Abstract
COVID-19 has had a substantial impact on transit workers’ lives, especially among public-facing vehicle operators. The current project examined relationships between workers’ knowledge and perceptions of their employer’s COVID-19 safety responses, job attitudes, and health. We surveyed transit workers (N = 174) between July and August 2020 and followed up 3 months later. Fifty-seven workers responded to the follow-up survey. Surveys addressed workers’ knowledge and perceptions of their employer implementing Centers for Disease Control and Prevention (CDC)-recommended COVID-19 safety responses, COVID-19 risk perceptions, job attitudes, and health factors. Employees reported knowledge of their employer implementing ~8 of 12 CDC-recommended responses. The most reported response was informational poster placements; the least reported was designating a point-person for COVID-19 concerns. Significant associations were found between knowledge of employer safety responses and lower COVID-19 risk perceptions, better job attitudes, and greater mental and global health. Operators (i.e. public-facing workers) reported worse perceptions of employer responses, and higher COVID-19 risk perceptions, work stress, and turnover intentions, compared with non-operators. A time-lagged panel model found that COVID-19 risk perceptions significantly mediated the relationship between public-facing work status and follow-up depression, anxiety, stress, and global health. Results reveal opportunities for transit authorities to broaden and better communicate their responses to emergent occupational safety and health crises.
Keywords: COVID-19 risk perceptions, employer COVID-19 safety practices, occupational safety and health, safety communication, transit workers, transportation
What’s Important About This Paper?
Transit workers have performed a critical public service through the COVID-19 pandemic. This study found that transit workers’ knowledge and positive perception of their employer’s COVID-19 safety responses may have protected against negative job attitudes, stressors, and mental health impacts in the months after pandemic-related lockdowns. However, operators reported significantly worse perceptions and less knowledge of their employer’s responses, as well as higher COVID-19 risk perceptions, compared to non-operators. Effective communication about protective actions taken by transit employers to workers—particularly operators in public-facing positions—may have a notable, positive impact on transit workers’ risk perceptions at work, general job attitudes, and health factors.
Introduction
The COVID-19 pandemic has had substantial global occupational health impacts for workers. Specifically, public transportation workers have faced significant, early impacts from the pandemic, including heightened exposure to COVID-19 infection, as well as work disruptions and job insecurity associated with reduced ridership. The American Public Transportation Association reported that ridership reductions and increased costs for transit authorities associated with COVID-19 led to revenue losses of an estimated $32 billion or more (Impact of COVID-19, 2020). These economic consequences forced many transit authorities to reduce working hours or furlough employees. Beyond economic stressors resulting from uncertainty around the industry’s financial stability (Sinclair et al., 2020), transit employees have experienced additional COVID-19-related stress at work and other physical and mental health concerns, which may all negatively impact job attitudes. In a Washington Post article published in May 2020—only a few months after states began implementing shutdowns in response to the pandemic—George and Jaffe (2020) reported that over 10 000 transit workers in New York City alone had been quarantined, and that over 100 had died from the virus. George and Jaffe (2020) also reported many workers across the country were expressing high work stress, anger at their employers for poor safety responses, and heightened anxiety due to fears of contracting or spreading the virus.
Given their ‘essential worker’ status and frequent interactions with the general public, transit workers were classified early on by the World Health Organization (WHO) as having a medium exposure risk for contracting SARS-CoV-2, the virus that causes COVID-19 (WHO, 2020). Recent research has shown that transportation workers may have twice the risk of a severe COVID-19 case compared with non-essential workers [Risk Ratio = 2.20; 95% confidence interval (CI) 1.21–4.00], though this effect was attenuated after controlling for socioeconomic factors (Mutambudzi et al., 2021). In Washington state, the transportation and material moving sector had an estimated 416.2 COVID-19 cases per 100,000 employees—between the 50th (282.8) and 75th (508.0) percentiles across occupations measured (Zhang, 2021). In California, the transportation and logistics sector had the second highest mortality excess (31% increase) compared with other occupations (Chen et al., 2021). However, the relative risks of public transport operators, specifically, to other occupations, including other transportation industry jobs, are unknown. There is expanding evidence, however, that bus and other public transit environments may facilitate both contact and aerosol transmission of COVID-19 due to their confined spaces, increased physical proximity to others, and potentially poor ventilation (Luo et al., 2020; Tang et al., 2020; Moreno et al., 2021). However, these risk factors may have been attenuated during the pandemic by overall reductions in travel demands (Zhang, 2021), stringent cleaning protocols (Tang et al., 2020; Moreno et al., 2021), and agencies following governmental guidelines (e.g. Di Carlo et al., 2020), including COVID-19 safety recommendations from the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA) for workplaces. Indeed, in response to escalating health risks and impacts of the pandemic on transit workers, the CDC in April 2020, released recommendations for transit authorities to adopt specific COVID-19 safety responses to protect their employees (CDC, 2020). Examples of responses include providing hand sanitizer for operators, providing extra sick time to use if exposed to the virus, and hanging informational posters on hand hygiene (see Table 1 for the full list).
Table 1.
CDC-recommended employer COVID-19 safety responses.
| Employer Response | Participant Response | ||
|---|---|---|---|
| Yes (n, %) |
No (n, %) |
Don’t Know (n, %) |
|
| My employer has placed posters that encourage staying home when sick, covering coughs and sneezes, and washing hands often practices in common areas in the workplace. | 135 (95.7%) | 3 (2.1%) | 3 (2.1%) |
| My employer provides employees access to soap, clean running water, and drying materials and/or hand sanitizer. | 134 (95.0%) | 6 (4.3%) | 1 (0.7%) |
| My employer provides operators with sanitizing wipes to clean frequently touched areas of the bus. | 131 (92.9%) | 9 (6.4%) | 1 (0.7%) |
| My employer has encouraged sick employees to stay home and has provided information on who to call if sick. | 120 (85.1%) | 14 (9.9%) | 7 (5.0%) |
| My employer provides operators with gloves and has provided training on how to properly use them. | 107 (77.0%) | 19 (13.7%) | 13 (9.4%) |
| My employer has instituted measures to keep 6 ft of distance between operators and passengers. | 101 (72.7%) | 38 (27.3%) | 0 (0.0%) |
| My employer has provided employees with correct information on COVID-19, how it spreads, and risk of exposure. | 88 (62.9%) | 25 (17.9%) | 27 (19.3%) |
| My employer provides employees tissues and no-touch disposal receptacles. | 88 (62.9%) | 46 (32.9%) | 6 (4.3%) |
| My employer has given employees additional sick time and/or has made use of sick time more flexible so that employees can stay home if they’re experiencing respiratory symptoms. | 86 (61.0%) | 34 (24.1%) | 21 (14.9%) |
| My employer has provided employees with training on proper hand washing techniques and other infection control strategies to prevent the spread of disease. | 77 (54.6%) | 37 (26.2%) | 27 (19.2%) |
| My employer has conducted a worksite assessment to identify COVID-19 prevention strategies. | 61 (43.3%) | 24 (17.0%) | 56 (39.7%) |
| My employer has designated someone at work to be responsible for all COVID-19-related concerns at work. | 35 (24.8%) | 33 (23.4%) | 73 (51.8%) |
Note. Italics indicate a safety response that ≥25% of workers reported their employer did not implement (i.e. answered ‘No’). Proportions may not accurately reflect the overall sample N due to incomplete questionnaires.
Employers’ successful implementation and communication of CDC-recommended responses by transit authorities—measured by worker knowledge and perception of such responses being implemented—may not only play a role in the reduction of COVID-19 disease transmission, but may also impact transit operators’ perceptions of COVID-19-related risk, job attitudes (e.g. job satisfaction), and how they experience and cope with such extraordinary workplace stressors during an occupational health and safety crisis. This association would exist because these employer actions to reduce health hazards at work would indicate a true organizational commitment to safety (Kurtessis et al., 2017), which is associated with improved job attitudes (Huang et al., 2016) and psychological well-being (Nahrgang et al., 2010). In addition to employer actions, the specific job roles of transit workers themselves may impact their risk perceptions, job attitudes, and overall health.
It is well established that working conditions can influence employee job satisfaction, work-related stress, and well-being (e.g. Grawitch et al., 2006; Nahrgang et al., 2010). According to the organizational support theory (Eisenberger et al., 1986) and an associated meta-analysis (Kurtessis et al., 2017), work role characteristics (e.g. public-facing work) may affect one’s perceptions of organizational support and personal well-being. Recently, Sinclair et al. (2021) proposed a COVID-19-specific extension of organizational support theory, where occupational risk factors (e.g. essential working status, public-facing work) may impact workers’ physical and mental health via their influence on COVID-19 risk perceptions. Specifically, they posit that workers in public-facing work environments (e.g. transit operators)—considered medium risk by the WHO (WHO, 2020)—will have heightened COVID-19 risk perceptions because they are in regular contact with people whose COVID-19 infection status is unknown (i.e. the ambiguity of the situation may heighten their perceived risks; Viscusi et al., 1991). These greater perceptions of risk will then cause public-facing workers to have worse physical and mental health (e.g. exhaustion, stress, anxiety). Applied to the transit industry, it may be that those in vehicle operation occupations (e.g. bus operators), essential workers who must interact with the public on a regular basis, will have higher perceptions of COVID-19 risk and worse health compared with other transit workers (e.g. vehicle maintenance, office administration), and that risk perceptions may mediate the relationship between public-facing work status and health outcomes.
Our overarching goal of the present study was to better understand the COVID-19-related safety, health, and well-being impacts on transit workers and their associations with their employer’s responses to the pandemic and public-facing work status. Our first aim was to describe transit workers’ knowledge and perception of their organizations’ pandemic responses, personal COVID-19 risk perceptions, job attitudes, and mental and physical health. To accomplish this aim, we assessed proportions of employees aware of their employer implementing each CDC-recommended COVID-19 response; average levels of COVID-19 risk perceptions, job attitudes (e.g. job satisfaction, job insecurity), and mental (e.g. depressive symptoms) and physical (e.g. experience of COVID-19 symptoms) health; and associations among these factors.
Our second aim was to compare risk perceptions, job attitudes, and health factors between public-facing (viz. operators) and non-public-facing (e.g. office administration) transit workers using Sinclair et al.’s (2021) model of occupational risk factors, COVID-19 risk perceptions, and well-being as a guide. According to their model, employees working in public-facing environments are likely to have higher perceptions of COVID-19 risk (i.e. greater worry of contracting and/or transmitting the disease), which may negatively impact their job attitudes and mental and physical health. As such, we hypothesized transit operators to report greater worry about becoming infected with and spreading COVID-19, as well as worse job attitudes (e.g. greater work stress), mental health (viz. depressive and anxiety symptoms), global health, and experience of COVID-19 symptoms.
For our third aim, we assessed the indirect relationships between employees’ public-facing work status and their health factors, via their COVID-19 risk perceptions as a mediator. Sinclair et al. (2021) predict that public-facing workers will have heightened COVID-19 risk perceptions. These risk perceptions will then cause reductions in mental and physical health, serving as a mediator between public-facing work status and health outcomes. As such, we hypothesized that public-facing work status (operator versus non-operator) would predict higher risk perceptions at baseline. Then, we hypothesized COVID-19 risk perceptions to significantly predict health outcomes at a 3-month follow-up. Finally, we hypothesized a significant indirect effect of public-facing work status on follow-up health factors (viz. depressive symptoms, anxiety symptoms, experience of COVID-19 symptoms, and global health), via baseline risk perceptions as a mediator.
Methods
Participants and procedures
A total of nine transit authorities were contacted to participate in the study. Five declined to participate. Flyers describing the study were sent to two participating transit authorities, which were requested to be posted at all garage locations, and a third transit authority placed 260 individual flyers in employee mailboxes. Finally, a union local representing workers at the fourth and largest participating transit authority assisted with mailing 2605 recruitment flyers to their members directly. Flyers contained information about study participation and eligibility and included a link to the anonymous online survey. Interested workers followed the link to complete an eligibility screener and then completed the survey if they were eligible. The eligibility criterion was being currently employed at a transit agency. Lottery-style incentives were employed where a subsample of participants were randomly selected to receive either $50 (n = 20 at baseline; n = 10 at follow-up) or $100 (n = 10 at baseline; n = 5 at follow-up) for survey completion. Participants completed baseline surveys between 10 July and 30 August 2020, and follow-up surveys between 9 October and 1 December 2020. All procedures were reviewed and approved by the Human Subjects Institutional Review Board at Oregon Health & Science University (eIRB# 20047).
Two hundred and one individuals attempted the baseline survey (7.0% of total employees who were sent flyers). Of those, 197 consented to participate. After consenting, individuals filled out an eligibility survey to verify current transit agency employment. One hundred seventy-eight individuals were eligible and at least partially completed the baseline survey. Four participants were excluded from analyses—in order to avoid unintended time-related effects—because they filled out the initial survey after 30 August (total baseline N = 174). Ninety-five participants (54.6%) agreed to complete a follow-up survey, and 57 of those participants partially completed it (60.0% of those that agreed to the follow-up). The follow-up survey contained the same scales as at baseline excluding basic demographic information (e.g. race).
At baseline, participants (N = 174) were employees at transit authorities (k = 4) across three states in the Northwest USA. Most (n = 151; 86.8%) came from a single organization (n = 46; 80.7% at follow-up), which was the largest among all those participating in the study. Employees were predominately white (n = 108; 81.8%), male (n = 94; 71.2%), and averaged 50.7 years of age (SD = 10.8). Most participants were urban/mass transit operators (n = 117; 67.2%), but five other transit occupations, including other vehicle operators and workers in non-public-facing jobs, were represented (see Table 2 for more details). Job tenure ranged from 0 to 39 years (M = 7.4, SD = 8.0), and participants reported working an average of 39.6 h per week (SD = 10.1).
Table 2.
Demographic and work characteristics.
| Variable | Mean (SD) or n (%) |
|---|---|
| Age (years) | 50.7 (10.8) |
| Gender identity (% male) | 94 (71.2%) |
| Race | |
| American Indian/Alaskan Native | 4 (3.0%) |
| Asian | 4 (3.0%) |
| Black/African American | 3 (2.3%) |
| White | 108 (81.8%) |
| >1 race | 5 (3.8%) |
| Other | 8 (6.1%) |
| Ethnicity (% Hispanic) | 7 (5.4%) |
| Household | |
| Married or living with partner | 92 (69.2%) |
| Living with children aged 0–5 | 14 (10.8%) |
| Living with school-aged children | 37 (28.5%) |
| Education | |
| High-school diploma or GED | 14 (10.7%) |
| Some college or technical school (no degree) | 58 (44.3%) |
| Bachelor’s degree | 49 (37.4%) |
| Graduate or professional degree (e.g. MA, MD) | 10 (7.6%) |
| Transit occupation | |
| Building and grounds maintenance | 4 (2.3%) |
| Office and administrative support | 9 (5.2%) |
| Bus operator (urban/mass transit) | 117 (67.2%) |
| Other operator (e.g. rail, streetcar) | 14 (8.1%) |
| Transit operations, safety, or training | 13 (7.5%) |
| Vehicle maintenance and repair | 17 (9.8%) |
| Job tenure (years) | 7.4 (8.0) |
| Work hours per week | |
| Pre-COVID | 43.1 (10.2) |
| Currently | 39.6 (10.1) |
Note. Proportions were computed using available data for each individual question. As such, they may not accurately reflect the overall sample N due to incomplete questionnaires.
Measures
Knowledge of COVID-19 employer safety responses
Knowledge of COVID-19 safety responses was measured with a 12-item scale developed for this study focused on the list of CDC-recommended safety responses for transit employers in response to COVID-19 (CDC, 2020). Participants answered ‘Yes’, ‘No’, or ‘I Don’t Know’ to indicate whether their employer had implemented a particular safety practice (see Table 1 for all items). A composite score was computed by assigning a value of 1 for ‘Yes’ and 0 for ‘No’ and ‘I Don’t Know’ for each item and summing them (Cronbach’s α = 0.77).
Perceptions of pandemic response adequacy
Perceptions of employer pandemic response adequacy were measured with two items developed for this study. Items assessed to what extent participants felt their employers were prioritizing employee safety and health, and their satisfaction with their employer’s pandemic response. Participants responded on a 5-point Likert scale (1—‘Strongly Disagree’ to 5—‘Strongly Agree’).
Risk perceptions
COVID-19 risk perceptions were measured with three items developed for this study. Items assessed how often participants worried at work about becoming infected with COVID-19, infecting coworkers or the public, and infecting family members or others in their household. Participants responded to items on a 7-point Likert scale (1—‘Not at All’ to 7—‘Always’). Items were used individually in exploratory correlational analyses and averaged together for the planned mediation model (α = 0.88).
Job attitudes
Job attitudes were measured with three validated self-report scales. The 4-item Job Insecurity Scale (Vander Elst et al., 2014) was used to measure job insecurity on a 5-point Likert scale (1—‘Strongly Disagree’ to 5—‘Strongly Agree’) (α = 0.82). Three items adapted from Cammann et al.’s (1983) scale were used to measure job satisfaction on a 5-point Likert scale (1—‘Strongly Disagree’ to 5—‘Strongly Agree’) (α = 0.95). The 7-item Stress in General scale (Stanton et al., 2001) was adapted to measure work stress on a 7-point frequency-based Likert scale (1—‘Not At All’ to 7—‘Very Much’) (α = 0.91). An additional item assessed to what extent participants were considering leaving their job due to the COVID-19 pandemic (i.e. turnover intentions) on a 5-point Likert scale (1—‘Strongly Disagree’ to 5—‘Strongly Agree’).
Health factors
Mental health was measured with two validated self-report scales. The 2-item Patient Health Questionnaire (PHQ; Kroenke et al., 2003) measured depressive symptoms on a 4-point frequency-based Likert scale (0—‘Not at all’ to 3—‘Nearly Every Day’) (α = 0.82). The 2-item Generalized Anxiety Disorder scale (Kroenke et al., 2007) measured anxiety symptoms on the same Likert scale as the PHQ (α = 0.83). Additionally, a single item (‘In general, would you say your health is…’) from the Patient-Reported Outcomes Measurement Information System mental and physical health scales (Cella et al., 2007; Hays et al., 2009) measured global health on a Likert scale from 1—‘Poor’ to 5—‘Excellent’. Another item measured whether or not (‘Yes’, ‘No’, ‘I Don’t Know’) participants had experienced any COVID-19-related symptoms (e.g. cough, fever, shortness of breath, loss of taste or smell).
Data analysis
Analyses were conducted with SPSS version 27 (IBM Corp., 2020) and Mplus version 6.1 (Muthén and Muthén, 1998–2010). Descriptive statistics (frequencies, means, standard deviations, correlations) were computed for all main study variables at baseline and follow-up. Independent samples t-tests were computed for baseline comparisons of operators (viz. mass transit buses, school buses, light rails, and streetcars) and non-operators (i.e. public-facing versus non-public-facing work status). Finally, a structural equation model using full information maximum likelihood estimation was used to assess the time-lagged associations between operator public-facing work status, COVID-19 risk perceptions, and health factors. We assessed both direct and indirect effects in accordance with Sinclair et al.’s (2021) proposed model. [Note: P < 0.05 was used to determine significance in all analyses.]
Results
Aim 1 results: Describe transit workers’ perceptions of their organizations’ pandemic responses, personal COVID-19 risk perceptions, job attitudes, and health
See Tables 1–3 for descriptive statistics of all main study variables at baseline. According to employee knowledge, the most common employer-implemented COVID-19 safety practice was placing posters encouraging staying home when sick and washing hands frequently; the least common practice was designating someone to be responsible for all COVID-19 concerns at work (see Table 1). On average, workers reported knowledge of their employer implementing 8.3 (SD = 2.7) out of the possible 12 CDC-recommended safety responses. Job insecurity and job satisfaction were in normative ranges (Bowling and Hammond, 2008; Vander Elst et al., 2014). Sixteen participants (11.9%) met the cutoff for likely major depressive disorder (Kroenke et al., 2003), and 33 (24.3%) met the cutoff for likely generalized anxiety disorder (Kroenke et al., 2007). Finally, 34 participants (25.0%) reported having experienced symptoms of COVID-19 (only one reported being formally diagnosed).
Baseline correlations (see Supplementary Table 1, available at Annals of Work Exposures and Health online) revealed that age was negatively associated with symptoms of depression and anxiety, but not with job attitudes or risk perceptions. Males reported lower depressive symptoms and anxiety symptoms than females. Race had a few notable correlations. First, participants who are Black, Indigenous, and Other Peoples of Color (BIPOC) reported significantly higher work stress levels compared with white participants. Additionally, participants who are BIPOC had more frequent worries about becoming infected with COVID-19 and infecting others. Experiencing symptoms of COVID-19 was negatively associated with job satisfaction and positively associated with turnover intentions, depressive symptoms, and anxiety symptoms, but it was not related to risk perceptions or global health. Knowledge of employer’s responses to the pandemic (i.e. total number of known CDC-recommended safety responses implemented) and employee perceptions of employer’s pandemic responses were negatively correlated with risk perceptions, job insecurity, work stress, depressive symptoms, and anxiety symptoms, and they were positively associated with job satisfaction and global health.
Aim 2 results: Compare COVID-19 risk perceptions, job attitudes, and health factors between public-facing and non-public-facing transit workers
At baseline, there were some notable differences between public-facing operators and non-public-facing transit employees in knowledge of and perceived adequacy of their employer’s pandemic safety responses, risk perceptions, and certain work characteristics. As indicated in Table 3, operators (M = 8.0, SD = 2.7) reported knowledge of significantly fewer employer CDC-recommended safety responses than other employees (M = 9.0, SD = 2.5; P < 0.05). Only one specific employer response (knowledge of employers providing tissues and no-touch disposal receptacles) significantly differed proportionally between operators (n = 59; 56.2%) and non-operators (n = 29; 82.9%; P < 0.05); however, the proportion of operators aware of employer responses was generally lower than the proportion of non-operators. Relatedly, operators reported lower agreement with their employers prioritizing employee safety and health (M = 2.7, SD = 1.4) than non-operators (M = 3.4, SD = 1.5; P < 0.05) and satisfaction with employer’s pandemic responses (Moperator = 2.3, SDoperator = 1.4; Mother = 3.3, SDother = 1.5; P < 0.05).
Table 3.
Descriptive statistics at baseline and follow-up.
| Variable (possible range) | Operators (mean, SD) | Other Employees (mean, SD) | ||
|---|---|---|---|---|
| Baseline (n = 131)a | Follow-up (n = 42)a | Baseline (n = 43)a | Follow-up (n = 16)a | |
| Employer safety responses(0–12) | 8.0 (2.7) | 8.6 (2.4) | 9.0 (2.5) | 9.7 (2.2) |
| Employer prioritizing employee safety and health (1–5) | 2.7 (1.4) | 2.9 (1.4) | 3.4 (1.5) | 3.9 (1.3) |
| Satisfaction with employer COVID-19 response (1–5) | 2.3 (1.4) | 2.7 (1.4) | 3.3 (1.5) | 3.7 (1.4) |
| Considering leaving job due to COVID-19 (1–5) | 3.1 (1.5) | 3.4 (1.6) | 2.1 (1.4) | 1.3 (0.8) |
| Worry about contracting COVID-19 (1–7) | 5.8 (1.5) | 5.5 (1.7) | 4.4 (2.1) | 3.9 (1.9) |
| Worry about spreading COVID-19 to coworkers or public (1–7) | 5.3 (1.7) | 4.6 (2.2) | 3.9 (2.0) | 3.2 (1.7) |
| Worry about spreading COVID-19 to family or household (1–7) | 5.7 (1.8) | 5.4 (2.0) | 4.7 (2.1) | 3.5 (1.6) |
| Job insecurity (1–5) | 2.7 (1.0) | 2.8 (1.0) | 2.3 (0.8) | 2.0 (0.9) |
| Job satisfaction (1–5) | 3.8 (1.2) | 3.8 (1.3) | 4.2 (1.1) | 4.7 (0.5) |
| Work stress (1–7) | 4.9 (1.3) | 4.7 (1.5) | 4.4 (1.2) | 3.9 (1.1) |
| Depression (0–6) | 1.2 (1.6) | 1.4 (1.6) | 0.9 (1.3) | 0.5 (0.8) |
| Anxiety (0–6) | 1.8 (1.7) | 1.3 (1.2) | 1.2 (1.6) | 1.0 (1.5) |
| Global health (1–5) | 3.1 (0.9) | 3.2 (1.0) | 3.1 (0.9) | 3.2 (0.8) |
aSample size reflects number of participants that partially completed the survey at each time point, respectively.
Operators had substantially higher COVID-19 risk perceptions overall. They reported more frequently being concerned with becoming infected with COVID-19 (Moperator = 5.8, SD = 1.5; Mother = 4.4, SD = 2.1; P < 0.05), transmitting it to their coworkers or the public (Moperator = 5.3, SD = 1.5; Mother = 3.9, SD = 2.0; P < 0.05), and transmitting it to their families or households (Moperator = 5.7, SD = 1.5; Mother = 4.7, SD = 2.1; P = 0.05).
There were also several differences between operators and other transit employees in their work characteristics, work attitudes, and health. First, operators tended to have shorter tenure (M = 6.0 years, SD = 6.6) compared with non-operators (M = 11.8 years, SD = 10.3; P < 0.05). Additionally, operators reported greater reductions in work hours per week since COVID-19 began (MDiff = −4.7 h, SD = 9.1) compared with non-operators (MDiff = +0.1 h, SD = 3.5; P < 0.05). Operators reported significantly higher work stress (Moperator = 4.9, SD = 1.3; Mother = 4.4, SD = 1.2; P < 0.05), turnover intentions (Moperator = 3.1, SD = 1.5; Mother = 2.1, SD = 1.4; P < 0.05), and job insecurity (Moperator = 2.7, SD = 1.0; Mother = 2.3, SD = 0.8; P < 0.05). Additionally, operators reported slightly (though non-significantly) greater anxiety symptoms (M = 1.8, SD = 1.7) compared with non-public-facing employees (M = 1.2, SD = 1.6; P = 0.07). There were no differences in self-reported depressive symptoms, global health, or experience of COVID-19 symptoms (Ps > 0.05).
Aim 3 results: Assess the indirect effect of public-facing work status on health factors via COVID-19 risk perceptions as a mediator
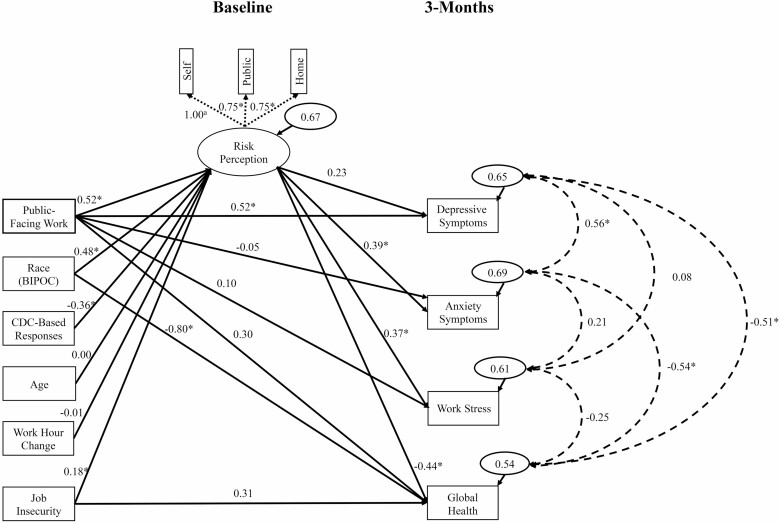
An initial time-lagged panel model was fit with all paths to the mediator and outcomes estimated, including all hypothesized covariates based on Sinclair et al.’s (2021) model (viz. age, race, employer safety responses, change in work hours since the pandemic, and job insecurity; see Supplementary Fig. 1, available at Annals of Work Exposures and Health online). This model fit the data well, χ2(21, N = 123) = 20.09, P = 0.52; CFI = 1.00; SRMR = 0.03; RMSEA = 0.00, 90% CI [0.00, 0.07]; however, many paths were non-significant (e.g. covariate paths to the outcome variables). As such, we fit a new model with just the hypothesized covariate paths to the mediator estimated (see Supplementary Fig. 2, available at Annals of Work Exposures and Health online). This model significantly reduced model fit, , P < 0.05, so we sequentially replaced two individual covariate-outcome paths (race and job insecurity to global health) based on modification indices. The final model fit was not significantly worse than the untrimmed model, , P = 0.08, and therefore used to interpret results (see Fig. 1 for partially standardized and fully standardized path coefficients). Controlling for age, employer safety responses, race, change in work hours, and job insecurity, operator status was significantly associated with risk perceptions at baseline (unstandardized b = 0.88, 95% CI [0.17, 1.59]). Further, baseline risk perceptions were significantly associated with greater anxiety symptoms (b = 0.30, 95% CI [0.08, 0.58]) and work stress (b = 0.31, 95% CI [0.02, 0.60]), and lower global health (b = −0.27, 95% CI [−0.49, −0.11]), but they were not associated with depressive symptoms (b = 0.21, 95% CI [−0.08, 0.46]). Significant covariate paths included race (b = 0.81, 95% CI [0.10, 1.41]) and job insecurity (b = 0.31, 95% CI [0.06, 0.61]) predicting greater risk perceptions at baseline; knowledge of employer’s CDC-recommended safety responses (b = −0.23, 95% CI [−0.31, −0.15]) predicting lower risk perceptions at baseline; and race predicting lower global health at follow-up (b = −0.82, 95% CI [−1.50, −0.11]).
Figure 1.
Final trimmed path model. Note. Values on solid lines represent standardized or partially standardized (in cases of binary independent variables) regression coefficients. Values on dashed lines represent correlation coefficients. Values in bubbles represent residual variances. Values on dotted lines originating from risk perceptions represent factor loadings. COVID-19 symptoms, though included in Sinclair et al.’s (2021) model was not included in our analysis because of low endorsement of the item at follow-up (n = 10). *Significant at P < 0.05. aDue to a non-significant negative residual variance, the residual variance for the item reflecting concern with becoming infected with COVID-19 was constrained to 0.
Indirect effects were evaluated using 95% bias corrected CIs computed from 1000 bootstrapped samples (see Table 4). Significant indirect effects of operator status were found on depressive symptoms, b = 0.18, 95% CI [0.01, 0.60], anxiety symptoms, b = 0.27, 95% CI [0.05, 0.70], work stress, b = 0.28, 95% CI [0.05, 0.78], and global health, b = −0.23, 95% CI [−0.57, −0.05], such that operator status predicted greater depressive symptoms, anxiety symptoms, work stress, and lower global health, via its association with greater COVID-19 risk perceptions as a mediator.
Table 4.
Total, direct, and indirect effects.
| Independent Variable | Outcomes | |||
|---|---|---|---|---|
| Depressive symptoms | Anxiety symptoms | Work stress | Global health | |
| Public-facing work status | ||||
| Total effect | 0.95 [0.30, 1.72] | 0.20 [−0.83, 0.97] | 0.42 [−0.48, 1.28] | 0.07 [−0.48, 0.59] |
| Direct effect | 0.77 [0.06, 1.65] | −0.07 [−1.08, 0.86] | 0.15 [−0.84, 1.05] | 0.31 [−0.23, 0.81] |
| Indirect effect | 0.18 [0.01, 0.60] | 0.27 [0.05, 0.70] | 0.28 [0.05, 0.78] | −0.23 [−0.57, −0.05] |
| Proportion mediated | 0.19 | —a | 0.67 | —a |
Note. COVID-19 risk perceptions were the mediator. Values were computed controlling for effects of age, race, knowledge of employer’s CDC-recommended safety responses, change in work hours since the pandemic began, and job insecurity on risk perceptions. For results of the model with all paths estimated on the outcomes as well, see Supplementary Table 2, available at Annals of Work Exposures and Health online. Proportion mediated was calculated by dividing the total effect by the indirect effect.
aProportion mediated should not be interpreted for these outcomes because of the sign change between the indirect, direct, or total effect.
Discussion
The goal of the present study was to understand the COVID-19-related safety, health, and well-being impacts on transit workers and examine associations between these factors and employee perceptions of employer’s safety responses to the pandemic based on public-facing work status. Along with initial news media reporting on the challenges facing public transit operators during the COVID-19 pandemic, empirical evidence suggests that public transit operators in a public-facing environment (with consequently heightened viral transmissibility) may be at elevated risk for contracting the SARS-CoV-2 virus (Tirachini and Cats, 2020; WHO, 2020; Moreno et al., 2021). Research was needed to understand how employers are responding to pandemic-related occupational hazards in order to reduce risk for their workers and protect their health. Such knowledge would help identify areas of success and areas that need to be addressed by employers to better protect these frontline workers currently and during future emergent safety and health crises. The present study addressed this need by measuring employee knowledge of their employer’s COVID-19 safety responses. Our evidence suggests that transit employers are providing their employees with certain COVID-19-relevant resources (e.g. information, hand sanitizer), but may not be communicating about organizational or structural changes they have made, which do not directly involve the employees (e.g. designating a COVID-19 resource person, conducting a workplace assessment to develop COVID-19 preventative strategies).
Aim 1: Describe transit workers’ perceptions of their organizations’ pandemic responses, personal COVID-19 risk perceptions, job attitudes, and health
Based on employee knowledge, transit employers were moderately responsive—implementing about 8 of 12 (~67%) of CDC-recommended responses on average—but there was a vast range in proportions of sample with knowledge depending on the employer practice (~25–95%). In addition, we found that the number of employer safety responses implemented (as observed by employees) was significantly correlated with job insecurity, job satisfaction, turnover intentions, perceptions of employer’s pandemic response, and mental and global health. It may be that if workers are aware of more effort put forth by their employers to prevent workers’ exposure to COVID-19 at work (i.e. greater perceived management commitment to safety), they will be more likely to perceive their employers as prioritizing their safety, be less frequently concerned about disease transmission, have more positive work attitudes (e.g. higher job satisfaction, lower turnover intention), and experience better mental and global health. Altogether, these results indicate that the more CDC-recommended safety responses transit employers implement in response to a health crisis, and the more effectively they communicate these changes, the better off their employees may be.
Additionally, our results suggest that communication of safety responses to employees could be improved across the board. Exploratory tests revealed that within each transit authority, there was inconsistency in employees’ knowledge of employer safety responses (i.e. participants from the same company would provide different responses to the same items). This finding is important because it indicates there may not be a uniform, effective way transit authorities are disseminating critical safety information across their organizations, or that communication methods are not reaching their employees who may be most at-risk (e.g. operators). Similarly, the differences found in perceptions of their employer’s pandemic responses indicate that transit authorities can work on revising what they do to protect and communicate with operators (e.g. making a concerted effort to notify operators about and provide them with tissues and no-touch disposal receptacles). It may be beneficial for employers to work closely with union locals, and also find direct or more effective ways to communicate with their operators, in order to identify current critical needs, form responses, and communicate about those responses and allocated resources. Such responses may be particularly beneficial at reducing operator turnover intentions, and improve operator experiences, during future emergent health crises.
The high rates of depressive and anxiety symptoms in our sample should be noted. Previous statistics have shown around 7% and 3% of US adults experiencing a major depressive episode or reporting a diagnosis of generalized anxiety disorder, respectively, in a given year (National Institute of Mental Health, n.d.). In our sample, we found substantially higher rates of likely major depression or other depressive disorder (~12%) [Note: The calculation of this rate may not be equivalent to the NIMH rate of experiencing a major depressive episode, because the former represents the proportion of participants that exceeded the cutoff point for likely major depression or some other depressive disorder based on the PHQ, rather than experience of a major depressive episode] and likely generalized anxiety disorder (~24%). Although there were no differences between operators and other transit workers, the relatively high observed prevalence of depressive and anxiety symptoms within our sample may indicate a general decrease in mental health as a result of pandemic in the general population (Pfefferbaum and North, 2020) and the prevalence may be comparable to other essential worker groups. For example, in a study of Australian workers, ‘other essential workers’ (including those in the logistics and transportation sector among others) had the highest average levels of anxiety compared with both healthcare workers (another industry greatly affected by the pandemic) and the general population (depression was also higher among other essential workers compared with healthcare workers, but no different from the general population; Toh et al., 2021). In a systematic review of healthcare workers’ mental health during the pandemic, Li et al. (2021) found depression (18.7%) and anxiety (14.8%) current prevalence in North America was substantially higher than the general population pre-COVID-19, and comparable to the rates found in our sample of transit workers (we found greater anxiety and lower depressive symptom prevalence). Essential workers’ mental health has been greatly impacted by COVID-19, even among those who may not have been public-facing, and as a result, it would be beneficial for transit employers to implement broader mental health initiatives as complements to their physical hazard related safety responses during a crisis.
Aim 2: Compare COVID-19 risk perceptions, job attitudes, and health factors between public-facing and non-public-facing transit workers
The public-facing context of operators’ work may not influence their job satisfaction during a crisis that is greatly affecting their industry. Similarly, although operators are at a greater risk for contracting the disease than non-public-facing workers (WHO, 2020), there were no differences in rates of COVID-19 symptoms between public-facing and non-public-facing work status. This result may indicate that employer safety responses are equally effective for all workers, or that the predicted higher infection risk due to public-facing exposures may not be present in our sample (though the single participant who reported being formally diagnosed with COVID-19 was an operator). However, the delay in survey administration may have played a role in these findings; individuals diagnosed with COVID-19 (or experiencing symptoms) or those deeply unsatisfied with their jobs as a result of COVID-19-related responses may have already left the workforce, producing a selection bias. Low cumulative testing rates in the Pacific Northwest (PNW) (CDC, 2021) in conjunction with the possibility for asymptomatic cases (an estimated 15.6% of individuals with COVID-19 are asymptomatic; He et al., 2021) may also explain the lack of symptom differences and single diagnosis. Additionally, strict cleaning protocols at the transit authority most represented in the present sample may have mitigated the spread of infection. However, there were a number of differences between operators and other employees, which should be noted.
Work stress, job insecurity, and turnover intentions were significantly higher among operators compared to non-operators. It is important to note that these differences may not be due to COVID-19 alone. Decades of research has found that bus operators experience unique and influential work stressors (e.g. cabin ergonomic issues, fluctuating shifts, aggressive passengers, time-based stressors, break time inadequacy), which can heighten overall stress felt at work and increase turnover (Tse et al., 2006). As such, public transit vehicle operation may be a more stressful position in the transportation industry both presently and in general, and these workers may feel more uncertain about their continued employment.
Aim 3: Assess the indirect effect of public-facing work status on health factors via COVID-19 risk perceptions as a mediator
Finally, results from our path analysis provided preliminary support for the model proposed by Sinclair et al. (2021). According to their model, public-facing occupations will have higher COVID-19 risk perceptions, which will reduce their mental and physical health. Our results partially support this hypothesis with the significant indirect effects of operator job role on depression and anxiety symptoms, work stress, and global health at the 3-month follow-up. However, the total effects were quite small, with three of four being non-significant. As such, though the public-facing work status of operators may reduce mental and physical health via greater COVID-19 risk perceptions, the overall impact may not be as large as hypothesized. It may be that other occupational risk factors (e.g. congregate work) have a stronger effect on risk perceptions and health outcomes than public-facing work. More research is needed to better evaluate health outcomes among different occupational groups with varying risk factors. During emergent occupational health and safety crises, transit employers would do well to take the differential effects of public-facing work into consideration, and tailor responses for their operators who may have worse psychological health due to their greater concerns of infection.
Strengths and potential limitations
A major strength of the present study is its timely assessment of how transit employees, an ‘essential’ population hit hard by the COVID-19 pandemic, perceived their employer’s responses to the pandemic and how such perceptions were associated with their risk perceptions, job attitudes, and health factors. We found that communication between employers and employees could be improved in terms of the specific actions transit authorities are taking to prioritize employee safety during the pandemic (particularly communicating actions that may not be explicitly known by employees). We also illustrated differing job attitudes, risk perceptions, and mental health between operators and other transit employees, indicating a need for employers to determine what critical resources and protections are needed by operators and communicate more effectively with them.
Potential limitations include individual-level analyses, potentially limited sample representation, and survey response rate, and low retention at follow-up. We also did not collect data from transit authority employers about their objective implementation of recommended COVID-19 safety practices and policies, which prevents us from comparing employee knowledge of employer responses to objective employer policies. As mentioned above, there were intraorganizational differences in the number of reported CDC-recommended safety responses implemented by an employer. Because of this variance, we cannot simply recommend transit authorities implement more responses to reduce hazard exposures; they may already have. Instead, we can only recommend that organizations communicate more consistently and effectively with all of their employees, particularly operators, about safety responses they have implemented. Future research should evaluate multilevel contexts to better understand the true consistency across levels of analysis (individual versus organizational) and the differing effects of an organization’s objective policies and safety responses (Level 2) and their employees’ knowledge/perceptions of them (Level 1) on workplace outcomes.
Our sample was also limited to urban transit employees in the PNW, with most coming from a single employer. Therefore, it is unknown whether results found are generalizable to other states with different COVID-19 experiences (e.g. differing incidence rates, state-mandated safety policies). Indeed, recent research has found starkly contrasting pictures of safety behaviors across states in the USA that varied in their macro-level COVID-19 responses (Probst et al., 2020). We also experienced a relatively low response rate to the survey. In total, the union that assisted with the recruitment mailers represents about 4366 workers; 151 of those responded to our survey (3.5% of total workers represented; 5.8% of the 2605 mailers sent). This is understandable given the many work, family, and societal changes occurring during the pandemic. However, our observed response rate does mean that the sample may not be wholly representative of workers employed at the agencies targeted. Furthermore, there were few responses from individuals who identified as BIPOC (18.2% of the current sample compared with national estimates in 2020 of 43.9% of transit bus operators and 26.0% of all transportation and material moving occupations; U.S. Bureau of Labor Statistics, 2021), which necessitated a dichotomization of the race variable for analyses. As such, though recent research has shown higher rates of COVID-19 infection and deaths for Black/African Americans compared with white Americans (Lopez et al., 2020), but not necessarily higher rates for other races (Bruine de Bruine and Bennett, 2020), we were unable to tease apart the associations of risk perceptions, job attitudes, and health across specific racial backgrounds. As noted above, the majority of the sample came from a single employer. In exploratory replications of the analyses, isolating data from the single largest employer and other transit authorities, respectively, several results changed (see Supplementary Tables 3–5, available at Annals of Work Exposures and Health online). Most notably, there were no differences among operators and non-operators with regard to COVID-19 risk perceptions, which consequently nullified all indirect effects. However, these nullified effects may have been due to reduced statistical power. Additionally, work stress was actually lower among operators compared with other employees at the other transit authorities, a reversal from the single largest employer. In any case, representation from many organizations on this topic is key, because the interorganizational variability illustrated indicates that what may be happening in general in the industry during a crisis may not necessarily be occurring in the same way for workers at each individual transit authority. Future studies should attempt to reach a wider variety of transit organizations, control for state-level initiatives, and improve the representation of individuals who are BIPOC.
Although we recruited a meaningful number of transit workers to participate at baseline, not all of those workers agreed to receive follow-up surveys. Of the 97 who agreed to follow-up, only 60% completed their follow-up survey (reflecting less than half of the original total baseline sample of 174). This attrition may have impacted the results of the path analysis. Indeed, only 10 participants at follow-up reported experiencing COVID-19 symptoms, which necessitated the variable being removed from the model altogether. Job insecurity was higher at baseline among drop-outs (the only significant difference), which could indicate job security concerns effecting disinterest in continuance, or perhaps individuals whose jobs were more tenuous did in fact lose those jobs (two individuals that attempted the follow-up survey were no longer eligible due to no longer working at a transit agency). We used full information maximum likelihood, which accounts for missing data at random (Newman, 2003); however, results may be less biased with a method to account for data missing not at random (Bartlett et al., 2014). Similarly, though mediation can be evaluated with only two waves of data (Cole and Maxwell, 2003), omitting autoregressive paths in our path model reduce our ability to make causal inferences. Future longitudinal studies should assess the effects of public-facing work on trajectories of risk perceptions, job attitudes, and health in order to elucidate causal relationships over time during emergent public health crises.
Conclusion
This study presents a timely and important inquiry into transit authorities’ implementation and communication of COVID-19 safety responses, transit workers’ knowledge and perceptions of their employer’s safety responses, and their relationships with risk perceptions, job attitudes, and health. It would be of high value for transit employers to utilize resources and recommendations provided by public health and safety entities (e.g. CDC, OSHA) and improve their communication with their workers—particularly operators—about responses they enact during emergent health and safety crises to reduce occupational health hazards. Employers may also wish to seek out feedback from employees who are BIPOC in order to address work stress and risk perception disparities. Although much of this work has focused on COVID-19 specifically, the implications of improving employer safety communication and tailoring safety responses to those at higher risk extend beyond the current pandemic and could benefit transit workers in future emergent health and safety crises.
Supplementary Material
Acknowledgements
We thank our labor union and transit agency partners for helping us reach and invite transit workers to participate in the study. These ongoing partner relationships were established through a separate project funded by a grant from the National Heart, Lung, and Blood Institute (NHLBI grant # R01 HL105495). We thank Nikolas Smart for his help developing and administering the survey. We would also like to express our appreciation for the workers who participated in the study, as well as transit workers more broadly for their dedicated service to the public during the pandemic. We wish to acknowledge all of the lives lost and those harmed by the pandemic within the transit industry and beyond.
Funding
This work was supported by the Oregon Institute of Occupational Health Sciences at Oregon Health & Science University via funds from the Division of Consumer and Business Services of the State of Oregon (ORS 656.630).
Conflict of interest
The authors declare no conflict of interest relating to the material presented in this article. Its contents, including opinions and/or conclusions expressed, are solely those of the authors.
Data availability
Requests for data from qualified researchers will be considered.
References
- Bartlett JW, Carpenter JR, Tilling Ket al. (2014) Improving upon the efficiency of complete case analysis when covariates are MNAR. Biostatistics; 15: 719–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling NA, Hammond GD. (2008) A meta-analytic examination of the construct validity of the Michigan Organizational Assessment Questionnaire Job Satisfaction Subscale. J Vocat Behav; 73: 63–77. [Google Scholar]
- Bruine de Bruine W, Bennett D. (2020) Relationships between initial COVID-19 risk perceptions and protective health behaviors: a national survey. Am J Prev Med; 59: 157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cammann C, Fichman M, Jenkins GDet al. (1983) Michigan Organizational Assessment Questionnaire. In Seashore SE, Lawler EE, Mirvis PH, Cammann C, editors. Assessing organizational change: a guide to methods, measures, and practices. Hoboken, NJ: Wiley-Interscience. pp. 71–138. ISBN 9780471894841 [Google Scholar]
- Cella D, Yount S, Rothrock Net al. ; PROMIS Cooperative Group. (2007) The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care; 45 (5 Suppl. 1): S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020) What transit workers need to know about COVID-19 [Flyer]. Available at https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/bus-transit-operator.html. Accessed 23 April 2020.
- Centers for Disease Control and Prevention . (2021) United States COVID-19 cases, deaths, and laboratory testing (NAATs) by state, territory, and jurisdiction. Available at https://covid.cdc.gov/covid-data-tracker/#cases_testsper100k. Accessed 15 June 2021.
- Chen YH, Glymour M, Riley Aet al. (2021) Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through November 2020. PLoS One; 16: e0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. (2003) Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. J Abnorm Psychol; 112: 558–77. [DOI] [PubMed] [Google Scholar]
- Di Carlo P, Chiacchiaretta P, Sinjari Bet al. (2020) Air and surface measurements of SARS-CoV-2 inside a bus during normal operation. PLoS One; 15: e0235943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger R, Huntington R, Hutchison S, Sowa D (1986) Perceived organizational support. J Appl Psychol; 71: 500–7. [Google Scholar]
- George J, Jaffe G. (2020) Transit workers are paying a heavy price during the pandemic. The Washington Post [online]. Available at https://www.washingtonpost.com/local/trafficandcommuting/transit-workers-are-paying-heavy-price-in-the-coronavirus-pandemic/2020/05/17/d7251b18-8edc-11ea-a9c0-73b93422d691_story.html. Accessed 17 May 2020. [Google Scholar]
- Grawitch MJ, Gottschalk M, Munz DC. (2006) The path to a healthy workplace: a critical review linking healthy workplace practices, employee well-being, and organizational improvements. Consult Psychol J Pract Res; 58: 129–47. [Google Scholar]
- Hays RD, Bjorner JB, Revicki DAet al. (2009) Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items. Qual Life Res; 18: 873–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Guo Y, Mao Ret al. (2021) Proportion of asymptomatic coronavirus disease 2019: a systematic review and meta-analysis. J Med Virol; 93: 820–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Lee J, McFadden ACet al. (2016) Beyond safety outcomes: an investigation of the impact of safety climate on job satisfaction, employee engagement and turnover using social exchange theory as the theoretical framework. Appl Ergon; 55: 248–57. [DOI] [PubMed] [Google Scholar]
- IBM Corp . (2020) IBM SPSS Statistics for Windows, version 27.0. Armonk, NY: IBM Corp. [Google Scholar]
- Impact of COVID-19. (2020) Impact of COVID-19 on the metropolitan transportation authority: hearing before the Senate Standing Committee on Transportation, New York State Legislature (2020) (testimony of Paul. P. Skoutelas). [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. (2003) The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care; 41: 1284–92. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBet al. (2007) Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med; 146: 317–25. [DOI] [PubMed] [Google Scholar]
- Kurtessis JN, Eisenberger R, Ford MTet al. (2017) Perceived organizational support: a meta-analytic evaluation of organizational support theory. J Manage; 43: 1854–84. [Google Scholar]
- Li Y, Scherer N, Felix Let al. (2021) Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLoS One; 16: e0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez MH, Rainie L, Budiman A. (2020) Financial and health impacts of COVID-19 vary widely by race and ethnicity [online]. Available at https://www.pewresearch.org/fact-tank/2020/05/05/financial-and-health-impacts-of-covid-19-vary-widely-by-race-and-ethnicity/. Accessed 22 March 2021.
- Luo K, Lei Z, Hai Zet al. (2020) Transmission of SARS-CoV-2 in public transportation vehicles: a case study in Hunan Province, China. Open Forum Infect Dis; 7: ofaa430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno T, Pintó RM, Bosch Aet al. (2021) Tracing surface and airborne SARS-CoV-2 RNA inside public buses and subway trains. Environ Int; 147: 106326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutambudzi M, Niedzwiedz C, Macdonald EWet al. (2021) Occupation and risk of severe COVID-19: prospective cohort study of 120075 UK Biobank participants. Occup Environ Med; 78: 307–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. (1998–2010) Mplus user’s guide. 6th edn. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nahrgang JD, Morgeson FP, Hofmann DA. (2010) Safety at work: a meta-analytic investigation of the link between job demands, job resources, burnout, engagement, and safety outcomes. J Appl Psychol; 96: 71–94. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health . (n.d.) Statistics. Available at https://www.nimh.nih.gov/health/statistics/index.shtml. Accessed 22 March 2021.
- Newman DA. (2003) Longitudinal modeling with randomly and systematically missing data: a simulation of ad hoc, maximum likelihood, and multiple imputation techniques. Organ Res Methods; 6: 328–62. [Google Scholar]
- Pfefferbaum B, North CS. (2020) Mental health and the Covid-19 pandemic. N Engl J Med; 383: 510–2. [DOI] [PubMed] [Google Scholar]
- Probst TM, Lee HJ, Bazzoli A. (2020) Economic stressors and the enactment of CDC-recommended COVID-19 prevention behaviors: the impact of state-level context. J Appl Psychol; 105: 1397–407. [DOI] [PubMed] [Google Scholar]
- Sinclair RR, Allen T, Barber Let al. (2020) Occupational health science in the time of COVID-19: now more than ever. Occup Health Sci; 4: 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair RR, Probst TM, Watson GPet al. (2021) Caught between Scylla and Charybdis: how economic stressors and occupational risk factors influence workers’ occupational health reactions to COVID-19. Appl Psychol Int Rev; 70: 85–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton JM, Balzer WK, Smith PCet al. (2001) A general measure of work stress: the Stress in General Scale. Educ Psychol Meas; 61: 866–88. [Google Scholar]
- Tang S, Mao Y, Jones RMet al. (2020) Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ Int; 144: 106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirachini A, Cats O. (2020) COVID-19 and public transportation: current assessment, prospects, and research needs. J Public Transport; 22: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toh WL, Meyer D, Phillipou Aet al. (2021) Mental health status of healthcare versus other essential workers in Australia amidst the COVID-19 pandemic: initial results from the collate project. Psychiatry Res; 298: 113822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse JLM, Flin R, Mearns K. (2006) Bus driver well-being review: 50 years of research. Transp Res F: Traffic Psychol Behav; 9: 89–114. [Google Scholar]
- U.S. Bureau of Labor Statistics . (2021) Labor force statistics from the current population survey. Available at https://www.bls.gov/cps/cpsaat11.htm. Accessed 15 June 2021.
- Vander Elst T, De Witte H, De Cuyper N. (2014) The Job Insecurity Scale: a psychometric evaluation across five European countries. Eur J Work Organ Psychol; 23: 364–80. [Google Scholar]
- Viscusi WK, Magat WA, Huber J. (1991) Communication of ambiguous risk information. Theory Decis; 31: 159–73. [Google Scholar]
- World Health Organization . (2020) Considerations for public health and social measures in the workplace in the context of COVID-19.World Health Organization. Available at https://apps.who.int/iris/rest/bitstreams/1277575/retrieve. Accessed 15 June 2021. [Google Scholar]
- Zhang M. (2021) Estimation of differential occupational risk of COVID-19 by comparing risk factors with case data by occupational group. Am J Ind Med; 64: 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Requests for data from qualified researchers will be considered.