Abstract
It is widely established that physical activity is associated with better cognitive outcomes, and accumulating evidence suggests that mind-body practice (MBP, e.g., movement therapies such as yoga) may yield similar benefits. Personality is related to both daily activities and cognition, but its role in the association between MBP and cognition is not well understood. Using data from waves 2 and 3 (2004–2014) of the Midlife in the United States (MIDUS) study, the current study examines bidirectional temporal associations between personality traits, MBP, and cognition in healthy adults (N = 2050). We applied a cross-lagged regression analysis to examine bidirectional effects between MBP, Big Five personality traits, and two cognitive domains (episodic memory and executive function) and controlled for relevant variables (sociodemographic factors, health, and functional status) at wave 2. MBP at baseline was independently associated with more favorable change in episodic memory, but not in executive function, both before and after including control variables. Also, episodic memory and executive function at baseline were related to increase in MBP. The findings show that MBP and cognitive function predict each other over time. There is also some evidence for cognition and personality associations over time; however, personality traits are not related to subsequent MBP.
Keywords: mind-body practice, personality traits, cognitive function, midlife in the United States, cross-lagged
Introduction
Due to population aging, cognitive decline is considered a major public health concern. Progressive deterioration of cognitive function can lead to further cognitive impairment and dementia. A large body of literature has established that performing intellectually demanding activities (Stine-Morrow et al., 2014) and physical activity (Brilliant et al., 2021; Colcombe & Kramer, 2003) may be beneficial for stimulating cognitive function. Because of the unavailability of medical treatments for age-related cognitive decline, mind-body practices (MBP), such as yoga, may be a useful option. Research has documented that personality is related to both daily activities (Lindner et al., 2021) and cognition (Graham & Lachman, 2012); still, its role in the association between MBP and cognition is not well understood. In this study, we examine bidirectional temporal associations between personality traits, MBP, and cognition in healthy adults.
Mind-Body Practices and Cognitive Function
MBP are considered to have beneficial effects on cognitive function in adulthood (Oken et al., 2006; Zhang et al., 2018). MBP can be performed through different physical activities or movement therapies (including meditative practices) that connect the body and the mind and impact both brain and behavior (Cramer et al., 2013). For example, yoga, an ancient Indian system of philosophy, commonly used as a mind-body interrelated practice, consists of physical movement (asanas), breathing exercises (pranayama), and meditation (dhyana) (Carim-Todd et al., 2013; Hariprasad et al., 2013). Tai chi is a Chinese martial art focused on the balance between the practitioner’s slow movement and deep breathing, used for its meditative health benefits (Carim-Todd et al., 2013; Hermanns et al., 2018). Pilates is another physical exercise method consisting of low-impact flexibility, postural balance, and muscular strength and endurance movements (Jung et al., 2020; Kloubec, 2011) and focusing on positive thoughts, Pilates promotes mental clarity and reduces stress (Lim & Park, 2019). All these movement therapies, as MBP, can be used primarily for managing the associated symptoms to improve the quality of life of persons with impaired cognitive functions (Farhang et al., 2019; Zhang et al., 2018). MBP, through its impact on vasomotor activities complexly mediated through the vagus nerve, increases the cerebral blood flow, and consequently affects the hypothalamus-pituitary-adrenal (HPA) axis, which in turn, reduces the production of inflammatory neurotransmitters and decreases the risk of inflammation-related disorders (Ulrich-Lai & Herman, 2009).
Researchers began studying yoga as an intervention to improve cognition (Hariprasad et al., 2013). However, research on the reverse direction, that is, cognitive function predicting MBP is rare. Regarding other physical activities, research has shown that the association between cognitive function and physical activities may be bidirectional (Daly et al., 2015); for example, Daly and colleagues (2015) found that poor executive function was related to reduced levels of physical activities among older adults over time. They also found evidence for the reverse association that physical activity predicted change in executive function over time; however, this effect was smaller in magnitude.
Personality Traits and Cognitive Function
On the other hand, personality traits are individual characteristics that reflect an individual’s patterns of thought processes, emotions, and behaviors. The Five-Factor Model (the “Big Five”) proposed by McCrae and Costa is currently the most widely used model of personality traits (McCrae & Costa, 1987, 1999). The five personality traits included in this model are extraversion, agreeableness, conscientiousness, openness, and neuroticism. According to McCrae and Costa (1999), extraversion is a personality trait related to engagement with the external world and the experience of gratification and other positive emotions. Agreeableness is a personality trait related to cooperation, social harmony, sympathy, altruism, and trustworthiness. Agreeable persons tend to have a kind, considerate, and optimistic view for others. Conscientiousness is a personality trait related to being organized, careful, persistent, achievement-focused, and diligent. Neuroticism is a personality trait related to the experience of negative emotions, such as anger, anxiety, or depression. Finally, openness is a personality trait related to intellectual curiosity, self-awareness, and active imagination (McCrae & Costa, 1987).
Although personality has been well documented as a significant correlate of cognitive performance across the adult life span (Baker & Bichsel, 2006; Graham & Lachman, 2012), there has been a long-standing debate about the degree to which personality and cognitive ability are associated. Ackerman (1996) pointed out that personality traits have a substantial impact on developing intellectual skills in adulthood. Lower levels of neuroticism and higher levels of openness are typically related to higher levels of cognitive function (Ackerman & Heggestad, 1997; Crowe et al., 2006; Rammstedt et al., 2016; Soubelet & Salthouse, 2011; von Stumm & Ackerman, 2013). Associations between conscientiousness and cognitive function are mixed (Rammstedt et al., 2016). Some studies find a negative correlation between conscientiousness and cognitive performance (Furnham et al., 2007; Rammstedt et al., 2016; Soubelet & Salthouse, 2011). However, other studies found positive associations between conscientiousness and cognitive performance in aging (Hülür et al., 2015; Sutin et al., 2018).
Research shows that personality is relatively stable in adulthood, yet there is some evidence for mean-level change (Roberts & DelVecchio, 2000; Schaie et al., 2004). For instance, agreeableness and conscientiousness increase, and neuroticism decreases with age (Cramer, 2003; Roberts et al., 2006). In addition to mean-level changes, research has also shown evidence for changes in rank order for personality traits (Graham & Lachman, 2012; Havlík et al., 2018). Analyses of cross-lagged associations suggest that cognitive decline may be related to an increase in neuroticism and a decline in openness (Aschwanden et al., 2017; Wettstein et al., 2020). Further, agreeableness has been found to reduce the association of social interaction with memory but not with executive functions (Segel-Karpas & Lachman, 2018). However, the association of conscientiousness and the cognitive decline shows a mixed result (Aschwanden et al., 2017), for instance, while some studies found a positive relationship between cognitive abilities and conscientiousness (Hülür et al., 2015), some found cognitive decline to be associated with an increase in conscientiousness due to compensatory mechanism (Rammstedt et al., 2016). Specifically, it is argued that people may use planning and organization to compensate for declines in cognition.
Personality Traits and Mind-Body Practices
Personality traits are related to a range of daily activities (Lindner et al., 2021), including health behaviors (Allen et al., 2019), physical activity (Saklofske et al., 2007), and MBP (Barkan et al., 2016; Jung et al., 2016). For example, Yu and colleagues found that personality traits have a significant positive effect on the amount of physical activity participation (Yu et al., 2014). In their study, the construct of five-factor personality traits jointly emerged as a significant determinant of frequency and amount of exercise participation, which further have a significant negative effect on stress and anxiety. In a study with 69 healthy adults, Elkana and colleagues (2018) found that individuals with a higher level of conscientiousness show better cognitive performance following a physical exercise program. However, evidence on the relationship between personality dimensions and the use of MBP is rare. In a mindfulness-based stress reduction (MBSR) intervention study with one hundred community-dwelling older adults, Barkan and colleagues (2016) found that agreeableness and openness predicted greater use of MBP both during and after the intervention. The authors also suggested that mental health practitioners tailor MBP to appeal to more individuals.
Also, regular MBP may lead to significant changes in personality traits (Delmonte, 1988; Jung et al., 2016; van den Hurk et al., 2011). For example, a study by Delmonte (1988) has shown that MBP through meditation was related to a decrease in self-reported neuroticism. Furthermore, in a study with 136 healthy adults, Jung and colleagues (2016) found that MBP was associated with increases in extraversion and openness and decline in neuroticism in the experimental group (n = 72) relative to the control group (n = 64). In another study, MBP in daily life was found to be positively associated with openness and extraversion and negatively associated with neuroticism and conscientiousness (van den Hurk et al., 2011).
The Present Study
The goal of the present study is to examine temporal associations between MBP, cognitive function, and personality in the Midlife in the United States (MIDUS) study, a large national probability sample of community-dwelling midlife and older adults. Specifically, using two waves of longitudinal data over 10 years, the current study appends to previous research by analyzing cross-lagged associations to examine whether baseline MBP has an effect on subsequent personality traits (agreeableness, extraversion, conscientiousness, neuroticism, and openness) and/or cognitive functions (episodic memory and executive function), and vice versa, while controlling for well-documented correlates of MBP, including sociodemographic and health factors. We hypothesized bidirectional associations between MBP and cognitive function over time. Furthermore, we expected a positive association of extraversion, agreeableness, conscientiousness, and openness with MBP and cognitive function, and a negative association of neuroticism with MBP and cognitive function.
Method
Participants and Procedure
We used data from the national survey of MIDUS, a large-scale, national probability sample of community-dwelling adults. The first study of this series (wave 1) was initiated in 1995-96 through random digit dialing of the US households in the 48 contiguous states, with 7108 English-speaking participants ranging in age from 24 to 75 years (M = 46, SD = 13) (Elliot et al., 2018). The current study uses data from waves 2 (2004–05) and 3 (2013–14) that included the cognitive functioning tests. Wave 2 included 75% of the original respondents in MIDUS 1, and wave 3 included 77% of MIDUS 2 participants (Hughes et al., 2018). In total, we used data from 2050 MIDUS participants who participated at both wave 2 and wave 3 and provided data on variables included in the present study.
Measures
Mind-Body Practices
MBP was assessed with the question “In the past 12 months, either to treat a physical health problem, to treat an emotional or personal problem, to maintain or enhance your wellness, or to prevent the onset of illness, how often did you use – exercise or movement therapy (yoga, pilates, tai chi, etc.)?” Participants provided their answer on a 5-point Likert scale ranging from 1 (“a lot”) to 5 (“never”). MBP was recoded as a binary variable, with responses indicating MBP (ranges from “a lot,” “often,” “sometimes” to “rarely”) coded as 1, and responses indicating no MBP (“never”) being coded as 0.
Cognitive Function
Cognitive function was assessed using the Brief Test of Adult Cognition by Telephone (BTACT), which included two measures of episodic memory (immediate and delayed free recall of 15 words), and five measures for executive function (number series completion, verbal ability and fluency in 60 seconds, backward digit span, 30-Second and Counting Task, Stop and Go Switch Task) (Lachman et al., 2010). The tests were z-scored (M = 0; SD = 1) according to means and standard deviations of the MIDUS II full sample. As per Lachman et al. (2010), composite scores for episodic memory and executive function were calculated as a standardized mean of the z-scored measures.
Personality Traits
In MIDUS, 25 self-descriptive adjective items were used to measure five-factor personality traits, including agreeableness (helpful, warm, caring, softhearted, and sympathetic), conscientiousness (organized, responsible, hardworking, and careless [reverse coded]), extraversion (outgoing, friendly, lively, active, and talkative), Openness (creative, imaginative, intelligent, curious, broadminded, sophisticated, and adventurous), and Neuroticism (moody, worrying, nervous, and calm [reverse coded]) (Lachman & Weaver, 1997; Zimprich et al., 2012). Responses were provided on a 1–4 Likert scale (1 = a lot, 2 = some, 3 = a little, and 4 = not at all) and averaged for each trait.
Covariates
Demographics
Demographic variables included baseline (wave 2) age (1 = <35, 2 = 35–44, 3 = 45–54, 4 = 55–64, 5 = 65–74, 6 = ≥75), gender (1 = male, 2 = female), race (1 = White, 2 = Black, 3 = others), and marital status (1 = married, 2 = separated/divorced, 3 = widowed, 4 = never married). Educational level was indicated by four categories (1 = no/some school, 2 = high school graduate/in college, 3 = graduated from college, 4 = having master’s/professional degree), and employment status was indicated by five categories (1 = currently working, 2 = self-employed, 3 = retired, 4 = unemployed, 5 = other).
Health and Functional Status
We used information obtained on health and functional status at wave 2. First, participants rated their current physical and mental health on a five-point scale ranging from 1 (excellent) to 5 (poor). Second, participants were asked if they have difficulty (functional limitations) in activities of daily living (ADL) and instrumental activities of daily living (IADL). Two dichotomous variables indicated whether participants had any difficulty with ADLs and IADLs, respectively (0 = no, 1 = yes). Third, participants were asked about their participation in vigorous and moderate physical activities (leisure). Vigorous physical activity was assessed with the question, “how often do you engage in vigorous physical activities that causes your heart to beat so rapidly that you can feel it in your chest and you perform the activity long enough to workup a good sweat and to breathe heavily?” Moderate physical activity was assessed with the question “how often do you engage in moderate physical activities, that is not physically exhausting, but it causes your heart rate to increase slightly and you typically workup a sweat?” Participants provided their answers on a 6-point Likert scale ranging from 1 (“several times a week or more”) to 6 (“never”). We coded the response as 1 (doing physical activities regularly, i.e., “several times a week or more” or “once a week”) or 0 (not doing physical activities regularly, i.e., either in lesser frequencies or “never”), for both summer and winter. We recoded those answers, whether performing physical activities regularly in one or both seasons, either with moderate or vigorous intensity (recoded as 1) or not (recoded as 0), to compare with MBP.
Other variables include body mass index (BMI; 1 = underweight [<18.5], 2 = normal [18.5–24.9], 3 = overweight [>24.9–29.9], and 4 = obese [>29.9]), smoking and alcohol history as health behavior (1 = regular tobacco/alcohol user currently, or 0 = not) and a count of the number of chronic conditions. Further, the participants also indicated (1 = yes, 2 = no) recent history (within the past 12 months) of high blood pressure, stroke, heart problems, diabetes, cancer, joint pain, and chronic sleep problem. Finally, participants were asked to respond to a 7-item DEPCON scale, administered by telephone, to assess whether they felt sad/depressed for more than two weeks in the past 12 months.
Statistical Analysis
Statistical analysis was conducted using Stata 15.1 (College Station, TX). Descriptive information and bivariate correlations between the independent, dependent, mediating, and all covariate variables were computed. We estimated cross-lagged multivariate regression analyses to examine associations between MBP, episodic memory, executive function, and personality traits over time while controlling for covariates at wave 2 (sociodemographic factors, health, and functional status). A p-value of .05 (two-sided) was used to evaluate statistical significance. Model fit was assessed by the indicators CFI and CD (equal to or higher than 0.90; Gerbing & Anderson, 1992), RMSEA (less than 0.05; Browne & Cudeck, 1992), and SRMR (less than 0.08, however, close to zero is considered as perfect fit; Hu & Bentler, 1998).
Results
Table 1 shows descriptive statistics for all variables included in this study. We reported the baseline (wave 2) characteristics of these individuals (N = 2050), aged 33–83 years (M = 55.0, SD = 10.8). Fifty-six percent of the sample were women, 94% were White, and 58% were employed at baseline. Participants’ educational levels were high, with 96% having at least graduated from high school and 19% having a master’s or professional degree. There were 13% who reported to be regular smokers, and 38% were regular alcohol users. The majority rated their physical (63%) and mental health (70%) as excellent or very good, even though 77% had at least one chronic disease, and 13% had five or more. A significant proportion of participants were overweight (39%) or obese (27%). 83% reported that they have never used MBP in the past 12 months, whereas 17% reported that they had used MBP (a lot 4%, often 3%, sometimes 6%, and rarely 4%) in the past 12 months.
Table 1.
Comparison of Respondent Characteristics of US Adults in Wave 2 (n = 2050).
| Variable | MIDUS 2 | |||
|---|---|---|---|---|
| Overall Status (n = 2050) | Based on Mind-Body Practice | |||
| Mind-Body Practice (n = 349; 17.0%) | No Mind-Body Practice (n = 1701; 83.0%) | p-value | ||
| Age mean year(sd) | 55.0(10.8) | 54.2(10.7) | 55.1(10.9) | .20 |
| <35 | 1.0 | 1.1 | 1.0 | |
| 35–44 | 18.1 | 20.6 | 17.5 | |
| 45–54 | 30.5 | 27.1 | 31.2 | |
| 55–64 | 29.3 | 32.4 | 28.7 | |
| 65–74 | 16.9 | 15.8 | 17.2 | |
| ≥75 | 4.2 | 2.6 | 4.5 | |
| Women | 55.5 | 73.1 | 51.9 | <.01 |
| Race/ethnicity | .93 | |||
| White | 94.0 | 93.7 | 94.1 | |
| Black | 2.3 | 2.3 | 2.4 | |
| Others | 3.7 | 4.0 | 3.6 | |
| Marital status | <.01 | |||
| Married | 73.9 | 66.2 | 75.5 | |
| Separated/divorced | 13.1 | 17.2 | 12.2 | |
| Widowed | 5.5 | 5.7 | 5.4 | |
| Unmarried | 7.6 | 10.9 | 6.9 | |
| Education | <.01 | |||
| No/some school | 3.8 | 1.4 | 4.3 | |
| Graduated from school/in college | 44.1 | 36.1 | 45.8 | |
| Graduated from college | 33.6 | 40.4 | 32.2 | |
| Master’s/professional degree | 18.5 | 22.1 | 17.8 | |
| Employment | .58 | |||
| Working | 57.8 | 55.9 | 58.1 | |
| Self-employed | 12.2 | 12.9 | 12.1 | |
| Retired | 20.1 | 19.5 | 20.2 | |
| Unemployed | 1.9 | 2.9 | 1.7 | |
| Other | 8.1 | 8.9 | 7.9 | |
| Health and functional status (past 12 months) | ||||
| BMI mean(sd) | 27.8(5.5) | 27.1(5.6) | 27.9(5.5) | <.01 |
| Underweight (<18.5) | 0.7 | 1.2 | 0.7 | |
| Normal (18.5–24.9) | 30.2 | 39.3 | 28.3 | |
| Overweight (25–29.9) | 38.8 | 33.8 | 39.9 | |
| Obese (>29.9) | 26.6 | 22.9 | 27.3 | |
| Missing | 3.7 | 2.8 | 3.9 | |
| Tobacco-user | 12.8 | 8.0 | 13.8 | <.01 |
| Alcohol-user | 37.7 | 38.7 | 37.5 | .67 |
| Regular physical activity | 47.3 | 64.8 | 43.7 | <.01 |
| Self-reported physical health | .02 | |||
| Excellent | 19.9 | 21.5 | 19.6 | |
| Very good | 43.7 | 49.0 | 42.6 | |
| Good | 27.6 | 23.5 | 28.5 | |
| Fair/poor | 8.8 | 6.0 | 9.4 | |
| Self-reported mental health | .25 | |||
| Excellent | 30.2 | 27.2 | 30.9 | |
| Very good | 39.7 | 43.8 | 38.9 | |
| Good | 25.7 | 23.5 | 25.7 | |
| Fair/poor | 4.5 | 5.4 | 4.5 | |
| Difficulty in ADL | 24.3 | 26.9 | 23.8 | .21 |
| Difficulty in IADL | 73.7 | 70.5 | 74.3 | .14 |
| Number of chronic condition/s mean(sd) | 2.0(1.7) | 2.3(1.7) | 1.9(1.6) | <.01 |
| 0 | 23.3 | 18.3 | 24.3 | |
| 1 | 21.6 | 18.9 | 22.1 | |
| 2 | 20.1 | 21.8 | 19.8 | |
| 3 | 14.0 | 12.6 | 14.3 | |
| 4 | 8.4 | 9.7 | 8.1 | |
| 5/more | 12.7 | 18.6 | 11.5 | |
| Had sleep problem | 9.7 | 14.3 | 8.7 | <.01 |
| Had diabetes | 7.5 | 7.5 | 7.5 | .99 |
| High blood pressure | 27.4 | 26.4 | 27.6 | .63 |
| Had stroke | 1.9 | 1.7 | 1.9 | .78 |
| Had cancer | 12.7 | 15.5 | 12.1 | .09 |
| Heart problem | 15.0 | 16.1 | 14.8 | .56 |
| Joint pain/joint stiffness | 85.1 | 86.5 | 84.8 | .40 |
| Felt sad/depressed for >2 weeks | 17.6 | 25.8 | 15.9 | <.01 |
| Personality traits mean(sd) | ||||
| Agreeableness | 3.4(0.5) | 3.5(0.5) | 3.4(0.5) | .34 |
| Conscientiousness | 3.5(0.4) | 3.5(0.4) | 3.5(0.4) | .82 |
| Extraversion | 3.1(0.6) | 3.2(0.5) | 3.1(0.6) | .27 |
| Neuroticism | 2.0(0.6) | 1.9(0.5) | 2.0(0.6) | .23 |
| Openness | 2.9(0.5) | 3.1(0.5) | 2.9(0.5) | <.01 |
| Episodic memory mean(sd) | 0.2(1.0) | 0.4(1.0) | 0.1(0.9) | <.01 |
| Executive functioning mean(sd) | 0.2(0.9) | 0.3(0.8) | 0.2(0.9) | .06 |
Note. All values are in percentage, unless otherwise specified. BMI = body mass index; ADL = activities of daily living; IADL = instrumental activities of daily living.
Table 1 also shows descriptive statistics for all variables included in this study stratified by engagement in MBP (wave 2). MBP was more prevalent among individuals aged 35–44 and 55–64 years, women, not married, and those with higher education (i.e., graduated from college and above). Body mass index (BMI) was significantly higher among those who did not engage in MBP. Only 8% of individuals engaged in MBP in the past 12 months were regular tobacco users, compared to 14% among those who did not engage in MBP. Those who engaged in MBP reported higher rates of regular physical activity and showed better self-reported health. At the same time, they were more likely to report sleep problems and feelings of depression. Participants who engaged in MBP showed higher levels of openness. Also, engagement in MBP was associated with higher scores in episodic memory. The current study also reported the wave 3 characteristics of these individuals (N = 2050), aged between 42–92 years (M = 64, SD = 11) (see Supplementary Table 1), where 19% reported that they had used MBP (a lot 4%, often 5%, sometimes 6%, and rarely 4%) in the past 12 months.
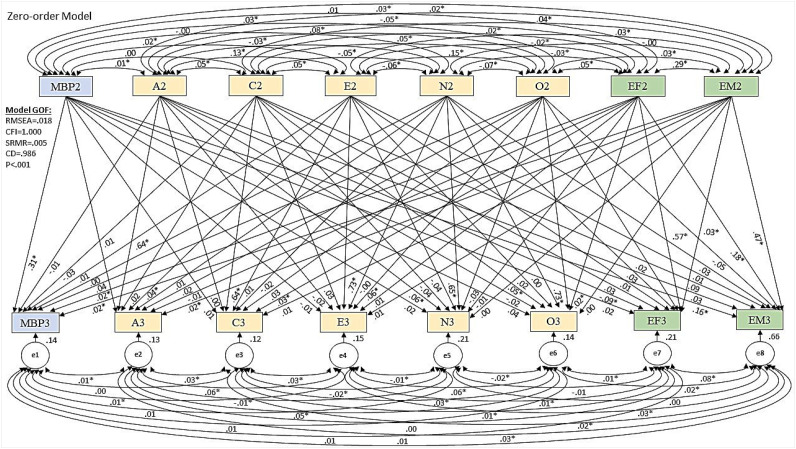
In the current study, the model fit was good for both the zero-order (CFI = 1.00, CD = 0.986, RMSEA = 0.018, and SRMR = 0.005) and full model (CFI = 1.00, CD = 0.991, RMSEA = 0.012, and SRMR = 0.002). Cross-lagged models examining associations between MBP, cognition, and personality over time are shown in Figures 1 and 2. Figure 1 shows the path diagram (zero-order model) for multivariable regression model estimating the effect of MBP, five-factor personality traits, and cognitive episodic memory and executive function (wave 2) on the same variables over time (wave 3), without involving the covariates. These regression results include the unstandardized regression coefficients (b values) and the significance level (p-value < .05). In this model, the MBP was independently associated with a more favorable change in episodic memory (b = 0.16, p < .001). However, the same effect was not found for executive function (b = 0.02, p = .43). Also, executive function was independently associated with a more favorable change in episodic memory (b = 0.18, p < .001) and vice versa (b = 0.03, p < .01). Episodic memory (wave 2) was related to an increase in MBP (b = 0.02, p = .01) and agreeableness (b = 0.02, p = .02) in wave 3. Executive function (wave 2) was related to increase in MBP (b = 0.02, p = .02), openness (b = 0.02, p = .02), and conscientiousness (b = 0.03, p < .01) in wave 3. Agreeableness was associated with a decline in executive function (b = −0.09, p < .001) over time.
Figure 1.
Crossed-lagged model (zero-order model) showing multivariable regression model estimating the effect of MBP, five personality traits, and cognitive functions of wave 2 on the same variables in wave 3, without involving covariates (n=2050; Model goodness of fit criteria: RMSEA = .02, CFI = 1.0, SRMR = .01, CD = .99). A = agreeableness, C = conscientiousness, E = extraversion, N = neuroticism, O = openness, EF = executive function, EM = episodic memory; Effects of covariates omitted from the illustration; *p<.05
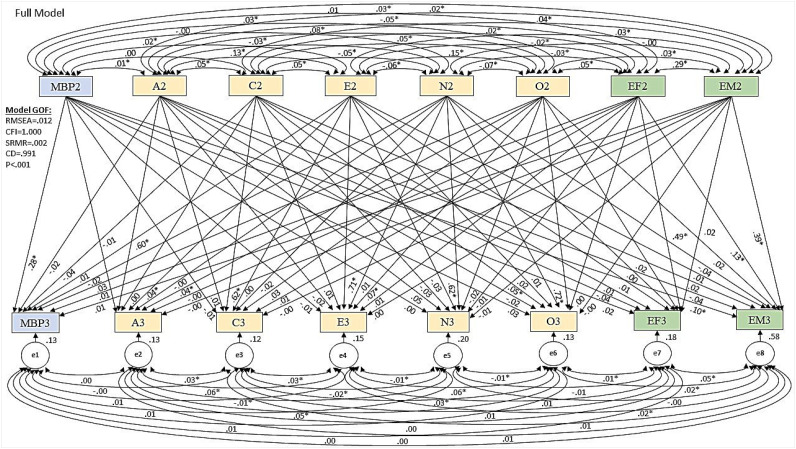
Figure 2.
Cross-lagged model (full model) showing multivariable regression model estimating the effect of MBP, five personality traits, and cognitive functions of wave 2 on the same variables in wave 3, controlling for covariates (n=2050; model goodness of fit criteria: RMSEA = .01, CFI = 1.0, SRMR = .00, CD = .99). A = agreeableness, C = conscientiousness, E = extraversion, N = neuroticism, O = openness, EF = executive function, EM = episodic memory; Effects of covariates omitted from the illustration; *p<.05.
Figure 2 shows the path diagram (full model) for the multivariable regression model, including covariates (sociodemographic factors and health at wave 2). After controlling for sociodemographic factors and health, MBP was independently associated with a more favorable change in episodic memory (b = 0.10, p = .04). However, the same effect was not found for executive function (b = 0.02, p = .44). Also, executive function had a significant positive effect on episodic memory (b = 0.13, p < .001) over time. Openness had a significant positive effect on extraversion (b = 0.07, p < .01) and agreeableness (b = 0.04, p = .02), and conscientiousness has significant positive effect on openness (b = 0.05, p = .03) over time. The results reveal no other interrelated changes over time.
Discussion
The present study evaluated bidirectional temporal associations between MBP, personality traits, and cognitive function in the MIDUS population-based sample of US adults, aged from the mid-thirties to the mid-eighties, over 10 years. The descriptive results show that even though there is literature to show health benefits to engaging in MBP, only a small percentage of the population studied have used MBP (17%). The cross-lagged multiple regression analysis showed that MBP and cognitive function predict each other over time: MBP at baseline was independently associated with a more favorable change in episodic memory in both sets of analyses before and after including control variables. However, it was unrelated to a change in executive function. Also, episodic memory and executive function at baseline were related to an increase in MBP in the zero-order model; however, these effects were no longer significant after including control variables. There is also some evidence for cognition and personality associations over time; for instance, episodic memory at baseline was related to an increase in agreeableness, while executive function at baseline was related to increase in openness and conscientiousness. In addition, agreeableness at baseline was related to a decline in executive function. However, the findings do not show any association between personality traits and subsequent MBP. The current study adds to previous research showing that habitual MBP in participants’ daily lives is associated with improvement in cognitive function at 10-year follow-up. While we found bidirectional temporal associations between cognition and personality over time, the findings do not show any bidirectional associations between personality traits and MBP.
Personality Traits and Cognitive Function
Earlier studies found associations between personality traits and cognitive functions (Hülür et al., 2015; Sutin et al., 2018). The current study corroborates and extends this previous research revealing that people high in executive function at baseline showed an increase in conscientiousness and openness. Higher executive functioning may allow individuals to be better organized at later ages, which may, in turn, result in increased conscientiousness. Higher executive functioning may also allow individuals to engage with new activities and areas of interest, which may result in increased openness. This finding corroborates earlier research (Rammstedt et al., 2016; von Stumm & Ackerman, 2013). The current study also found that a higher episodic memory at baseline was related to an increase in agreeableness over time. This finding may be related to older adults experiencing memory problems becoming irritable in social interactions, while older adults without memory problems may be relatively stable in agreeableness, thus social interactions that may contribute to their cognitive stimulation. This may explain that memories play an essential role in social interactions, and memory decline may lead to social withdrawal. This finding corroborates earlier research (Segel-Karpas & Lachman, 2018). However, the association of agreeableness with cognitive functions was not consistent. The result reveals that agreeableness at baseline was related to less favorable changes in executive function. However, baseline agreeableness was negatively associated with subsequent executive function.
Mind-body Practices and Cognitive Function
Research has widely documented the negative impacts of stress on cognition (Chen et al., 2018; Gómez-Gallego & Gómez-García, 2018). MBP seemed to affect structural and functional brain plasticity (Jung et al., 2016). Through its association with hippocampal volume, MBP impacts memory functions, attentional, and behavioral processes and thus may have a definite impact on cognition (Gómez-Gallego & Gómez-García, 2018). As a bridge between brain and body, MBP exhibits a down regulatory effect on the sympathetic nervous system and the hypothalamus-pituitary-adrenal axis in response to stress (Hariprasad et al., 2013; Ross & Thomas, 2010). Through complex neuronal circuits, MBP regulates the production of both pro-inflammatory neurotransmitters (e.g., dopamine) and inhibitory neurotransmitters (e.g., GABA) (Ross & Thomas, 2010; Ulrich-Lai & Herman, 2009). This physiological response is reported to reduce cortisol levels in plasma (Brand et al., 2012) and increase vagal activity (Carim-Todd et al., 2013). These effects reduce neuroinflammation and delay symptom onset, ultimately preventing further cognitive deterioration (Ross & Thomas, 2010). The current findings support the earlier studies showing the association of MBP and cognitive function predicting each other over time.
Further, the current study revealed a higher prevalence of sleep problems, depressive symptoms, and a number of chronic conditions among respondents who used MBP than those who did not use it. It is possible that these individuals may have been inclined to MBP for alleviation from these complaints. Similarly, knowledge of whether personality traits shape individuals’ propensity toward MBP may help healthcare providers tailor management for cognitive impairment. The current study specifies an increase in MBP as an increase from previously not using MBP to using it. Research has already documented that the participation rates of MBP, such as yoga, tai chi, and qigong, have increased from 6% (2002) to 15% (2017) (Wang et al., 2019). Our study corroborates this finding that the percentage of MBP users in wave 2 (17%) has increased to 19% in wave 3. We expected a positive association of agreeableness, conscientiousness, extraversion, and openness with MBP and a negative association of neuroticism with subsequent MBP (as per prevalence of personality traits among MBP users and non-users found in Table 1). However, we did not find any evidence for such associations.
Limitations
In closing, we note some limitations of the present study. First, in this study, we included mind-body practice as a one-item measure referring to various movement therapy/practices (in the MIDUS questionnaire, only three practices (yoga, tai chi, and Pilates) were provided as examples). Also, MIDUS did not assess how long the individuals were practicing MBP, which may affect health status. Many persons who practiced MBP might consider themselves deficient in health, thereby trying MBP to benefit as an alternative health approach. This motivation might be a reason that sometimes, our study did not yield predicted results. Second, the study participants were not initially screened for cognitive impairment. Though many individuals have various chronic diseases that might impact their cognitive function, it is still not possible to differentiate between individuals having cognitive decline beforehand or not. Third, based on available data, we were not able to differentiate between different MBP approaches. However, it can be assumed that a significantly larger proportion of participants used yoga because of its popularity among the general population than any other movement therapies mentioned in the study. For example, based on the National Health Interview Survey (NHIS), Clarke and colleagues (2015) found that although the use of yoga, tai chi, and qi gong as an alternative and complementary therapy has shown an increased prevalence between the years 2002 and 2012, yoga accounted for nearly four-fifths among all these approaches. Fourth, there may be potential limitations related to recall bias because responses were collected retrospectively and non-response and survivor biases because of the long gap between the two respective waves. Additionally, the makeup of the sample (94% white) may impact the findings as racial bias. Also, many more women practice MBP. Although we control for gender, this could affect generalizability bias. Further, MIDUS is an extensively used population dataset, where both wave 2 and wave 3 contain poststratification weights; however, this does not entirely address bias in longitudinal retention. Our study emphasizes retention (not attrition) and focuses on the characteristics of those respondents who remained in the study at the third wave. Finally, our dichotomizing a Likert scale measure on the self-report of MBP may be considered arbitrary. Sensitivity analyses using the Likert scale measure indicated that differences in episodic memory were primarily between those who endorsed categories “never” versus “some,” that is, those who reported some engagement in MBP showed a more favorable change in episodic memory compared with those who never used MBP (in both zero-order and full model). The same effect was not found in other associations. These additional analyses should be interpreted with the caveat that sample sizes per MBP category were small (i.e., between 4–6 % in each category of MBP other than “never”).
Conclusions
A wide body of research has demonstrated the beneficial effects of MBP on adult cognitive function. The current study reveals that MBP is related to better subsequent episodic memory over a decade; however, it was unrelated to subsequent executive function. Currently, with such a small percentage of the population engaging in MBP, healthcare providers could do more to educate their patients about the positive effects of MBP on cognitive performance to increase MBP use. In addition, the association between MBP and cognition was relatively independent of personality traits. One possible explanation may be that there is such an uneven distribution in the sample of those who did use MBP (only 17%) that could account for the lack of association. More research is needed to determine whether personality dispositions may protect community-dwelling older adults from cognitive declines through alternative and complementary practices and maintain and improve physical and cognitive health.
Supplemental Material
Supplement Material, sj-pdf-1-ggm-10.1177_23337214221083475 for Mind-Body Practice, Personality Traits, and Cognitive Performance: A 10-Years Study in US Adults by Kallol Kumar Bhattacharyya, Debra Dobbs and Gizem Hueluer in Gerontology and Geriatric Medicine
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Kallol Kumar Bhattacharyya https://orcid.org/0000-0003-0689-6592
References
- Ackerman P. L. (1996). A theory of adult intellectual development: Process, personality, interests, and knowledge. Intelligence, 22(2), 227–257. 10.1016/S0160-2896(96)90016-1 [DOI] [Google Scholar]
- Ackerman P. L., Heggestad E. D. (1997). Intelligence, personality, and interests: Evidence for overlapping traits. Psychological Bulletin, 121(2), 219–245. 10.1037/0033-2909.121.2.219 [DOI] [PubMed] [Google Scholar]
- Allen M. S., Laborde S., Walter E. E. (2019). Health-related behavior mediates the association between personality and memory performance in older adults. Journal of Applied Gerontology, 38(2), 232–252. 10.1177/0733464817698816 [DOI] [PubMed] [Google Scholar]
- Aschwanden D., Martin M., Allemand M. (2017). Cognitive abilities and personality traits in old age across four years: More stability than change. Journal of Research in Personality, 70, 202–213. 10.1016/j.jrp.2017.08.002. [DOI] [Google Scholar]
- Baker T. J., Bichsel J. (2006). Personality predictors of intelligence: Differences between young and cognitively healthy older adults. Personality and Individual Differences, 41(5), 861–871. 10.1016/j.paid.2006.02.017 [DOI] [Google Scholar]
- Barkan T., Hoerger M., Gallegos A. M., Turiano N. A., Duberstein P. R., Moynihan J. A. (2016). Personality predicts utilization of mindfulness-based stress reduction during and post-intervention in a community sample of older adults. Journal of Alternative and Complementary Medicine, 22(5), 390–395. 10.1089/acm.2015.0177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand S., Holsboer-Trachsler E., Naranjo J. R., Schmidt S. (2012). Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology, 65(3), 109–118. 10.1159/000330362 [DOI] [PubMed] [Google Scholar]
- Brilliant S. L., Claver M., LaPlace P., Schlesinger C. (2021). Physical activity and aging: Exploring motivations of masters swimmers. Gerontology and Geriatric Medicine, 7, 23337214211044656. 10.1177/23337214211044658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne M. W., Cudeck R. (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21(2), 230–258. 10.1177/0049124192021002005 [DOI] [Google Scholar]
- Carim-Todd L., Mitchell S. H., Oken B. S. (2013). Mind-body practices: An alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug and Alcohol Dependence, 132(3), 399–410. 10.1016/j.drugalcdep.2013.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Wang J., Liang Y., Sun F., Dong X. (2018). Perceived stress and cognitive functions among Chinese older adults: The moderating role of health status. Gerontology & Geriatric Medicine, 4, 2333721418778390. 10.1177/2333721418778390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke T. C., Black L. I., Stussman B. J., Barnes P. M., Nahin R. L. (2015). Trends in the use of complementary health approaches among adults: United States, 2002-2012. National Health Statistics Reports, (79), 1–16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4573565/. [PMC free article] [PubMed] [Google Scholar]
- Colcombe S., Kramer A. F. (2003). Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychological Science, 14(2), 125–130. 10.1111/1467-9280.t01-1-01430 [DOI] [PubMed] [Google Scholar]
- Cramer P. (2003). Personality change in later adulthood is predicted by defense mechanism use in early adulthood. Journal of Research in Personality, 37(1), 76–104. 10.1016/S0092-6566(02)00528-7 [DOI] [Google Scholar]
- Cramer H., Lauche R., Langhorst J., Dobos G. (2013). Yoga for depression: A systematic review and meta-analysis. Depression and Anxiety, 30(11), 1068–1083. 10.1002/da.22166 [DOI] [PubMed] [Google Scholar]
- Crowe M., Andel R., Pedersen N. L., Fratiglioni L., Gatz M. (2006). Personality and risk of cognitive impairment 25 years later. Psychology and Aging, 21(3), 573–580. 10.1037/0882-7974.21.3.573 [DOI] [PubMed] [Google Scholar]
- Daly M., McMinn D., Allan J. L. (2015). A bidirectional relationship between physical activity and executive function in older adults. Frontiers in Human Neuroscience, 8, 1044. 10.3389/fnhum.2014.01044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delmonte M. M. (1988). Personality correlates of meditation practice frequency and dropout in an outpatient population. Journal of Behavioral Medicine, 11(6), 593–597. 10.1007/BF00844908 [DOI] [PubMed] [Google Scholar]
- Elkana O., Krueger Bustanai N. Y., Louzia-Timen R., Kodesh E., Franco M., Doniger G. M. (2018). Conscientiousness is associated with improvement in visuospatial working memory and mood following acute physical exercise: A randomized controlled trial. Personality and Individual Differences, 132, 126–132. 10.1016/j.paid.2018.05.018. [DOI] [Google Scholar]
- Elliot A. J., Turiano N. A., Infurna F. J., Lachman M. E., Chapman B. P. (2018). Lifetime trauma, perceived control, and all-cause mortality: Results from the midlife in the United States study. Health Psychology, 37(3), 262–270. 10.1037/hea0000585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhang M., Miranda-Castillo C., Rubio M., Furtado G. (2019). Impact of mind-body interventions in older adults with mild cognitive impairment: A systematic review. International Psychogeriatrics, 31(5), 643–666. 10.1017/S1041610218002302 [DOI] [PubMed] [Google Scholar]
- Furnham A., Dissou G., Sloan P., Chamorro-Premuzic T. (2007). Personality and intelligence in business people: A study of two personality and two intelligence measures. Journal of Business and Psychology, 22(1), 99–109. 10.1007/s10869-007-9051-z [DOI] [Google Scholar]
- Gerbing D. W., Anderson J. C. (1992). Monte carlo evaluations of goodness of fit indices for structural equation models. Sociological Methods & Research, 21(2), 132–160. 10.1177/0049124192021002002 [DOI] [Google Scholar]
- Gómez-Gallego M., Gómez-García J. (2018). Effects of stress on emotional memory in patients with Alzheimer's disease and in healthy elderly. International Psychogeriatrics, 30(8), 1199–1209. 10.1017/S1041610217002642 [DOI] [PubMed] [Google Scholar]
- Graham E. K., Lachman M. E. (2012). Personality stability is associated with better cognitive performance in adulthood: Are the stable more able? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 67(5), 545–554. 10.1093/geronb/gbr149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariprasad V. R., Koparde V., Sivakumar P. T., Varambally S., Thirthalli J., Varghese M., Basavaraddi I. V., Gangadhar B. N. (2013). Randomized clinical trial of yoga-based intervention in residents from elderly homes: Effects on cognitive function. Indian Journal of Psychiatry, 55(Suppl 3), S357–S363. 10.4103/0019-5545.116308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havlík M., Mladá K., Fajnerová I., Horáček J. (2018). Do personality features influence our intuitions of the mind-body problem? A pilot study. Frontiers in Psychology, 9, 1219. 10.3389/fpsyg.2018.01219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermanns M., Haas B. K., Rath L., Murley B., Arce-Esquivel A. A., Ballard J. E., Wang Y. T. (2018). Impact of tai chi on peripheral neuropathy revisited: A mixed-methods study. Gerontology & Geriatric Medicine, 4, 2333721418819532. 10.1177/2333721418819532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L.-t., Bentler P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424–453. 10.1037/1082-989X.3.4.424 [DOI] [Google Scholar]
- Hughes M. L., Agrigoroaei S., Jeon M., Bruzzese M., Lachman M. E. (2018). Change in cognitive performance from midlife into old age: Findings from the midlife in the United States (MIDUS) study. Journal of the International Neuropsychological Society, 24(8), 805–820. 10.1017/S1355617718000425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hülür G., Hertzog C., Pearman A. M., Gerstorf D. (2015). Correlates and moderators of change in subjective memory and memory performance: Findings from the health and retirement study. Gerontology, 61(3), 232–240. 10.1159/000369010 [DOI] [PubMed] [Google Scholar]
- Jung Y. H., Lee U. S., Jang J. H., Kang D. H. (2016). Effects of mind-body training on personality and behavioral activation and inhibition system according to BDNF Val66Met polymorphism. Psychiatry Investigation, 13(3), 333–340. 10.4306/pi.2016.13.3.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung H., Miki Y., Tanaka R., Yamasaki M. (2020). The effects of a multicomponent lower extremity training technique on physical function in healthy older adults: A randomized controlled trial. Gerontology & Geriatric Medicine, 6, 2333721420935702. 10.1177/2333721420935702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloubec J. (2011). Pilates: How does it work and who needs it? Muscles, Ligaments and Tendons Journal, 1(2), 61–66. https://pubmed.ncbi.nlm.nih.gov/23738249/. [PMC free article] [PubMed] [Google Scholar]
- Lachman M. E., Agrigoroaei S., Murphy C., Tun P. A. (2010). Frequent cognitive activity compensates for education differences in episodic memory. The American Journal of Geriatric Psychiatry, 18(1), 4–10. 10.1097/JGP.0b013e3181ab8b62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman M. E., Weaver S. L. (1997). The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. https://www.brandeis.edu/psychology/lachman/pdfs/midi-personality-scales.pdf [Google Scholar]
- Lim E. J., Park J. E. (2019). The effects of Pilates and yoga participant’s on engagement in functional movement and individual health level. Journal of Exercise Rehabilitation, 15(4), 553–559. 10.12965/jer.1938280.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindner S., Aschwanden D., Zimmermann J., Allemand M. (2021). How do personality traits manifest in daily life of older adults? European Journal of Ageing, 19(1), 131–142. 10.1007/s10433-020-00598-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae R. R., Costa P. T. (1987). Validation of the five-factor model of personality across instruments and observers. Journal of Personality and Social Psychology, 52(1), 81–90. 10.1037/0022-3514.52.1.81 [DOI] [PubMed] [Google Scholar]
- McCrae R. R., Costa P. T., Jr. (1999). A five-factor theory of personality. In Pervin L. A., John O. P. (Eds.), Handbook of personality: Theory and research (2nd ed., pp. 139–153). New York, NY: Guilford Press. [Google Scholar]
- Oken B. S., Zajdel D., Kishiyama S., Flegal K., Dehen C., Haas M., Kraemer D. F., Lawrence J., Leyva J. (2006). Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Alternative Therapies in Health and Medicine, 12(1), 40–47. https://pubmed.ncbi.nlm.nih.gov/16454146/. [PMC free article] [PubMed] [Google Scholar]
- Rammstedt B., Danner D., Martin S. (2016). The association between personality and cognitive ability: Going beyond simple effects. Journal of Research in Personality, 62, 39–44. 10.1016/j.jrp.2016.03.005. [DOI] [Google Scholar]
- Roberts B. W., DelVecchio W. F. (2000). The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin, 126(1), 3–25. 10.1037/0033-2909.126.1.3 [DOI] [PubMed] [Google Scholar]
- Roberts B. W., Walton K. E., Viechtbauer W. (2006). Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin, 132(1), 1–25. 10.1037/0033-2909.132.1.1 [DOI] [PubMed] [Google Scholar]
- Ross A., Thomas S. (2010). The health benefits of yoga and exercise: A review of comparison studies. Journal of Alternative and Complementary Medicine, 16(1), 3–12. 10.1089/acm.2009.0044 [DOI] [PubMed] [Google Scholar]
- Saklofske D. H., Austin E. J., Rohr B. A., Andrews J. J. (2007). Personality, emotional intelligence and exercise. Journal of Health Psychology, 12(6), 937–948. 10.1177/1359105307082458 [DOI] [PubMed] [Google Scholar]
- Schaie K. W., Willis S. L., Caskie G. I. (2004). The seattle longitudinal study: Relationship between personality and cognition. Neuropsychology, Development, and Cognition. Section B, Aging, Neuropsychology, and Cognition, 11(2–3), 304–324. 10.1080/13825580490511134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segel-Karpas D., Lachman M. E. (2018). Social contact and cognitive functioning: The role of personality. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 73(6), 974–984. 10.1093/geronb/gbw079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soubelet A., Salthouse T. A. (2011). Personality-cognition relations across adulthood. Developmental Psychology, 47(2), 303–310. 10.1037/a0021816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stine-Morrow E. A. L., Payne B. R., Roberts B. W., Kramer A. F., Morrow D. G., Payne L., Hill P. L., Jackson J. J., Gao X., Noh S. R., Janke M. C., Parisi J. M. (2014). Training versus engagement as paths to cognitive enrichment with aging. Psychology and Aging, 29(4), 891–906. 10.1037/a0038244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Stephan Y., Terracciano A. (2018). Facets of conscientiousness and risk of dementia. Psychological Medicine, 48(6), 974–982. 10.1017/S0033291717002306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich-Lai Y. M., Herman J. P. (2009). Neural regulation of endocrine and autonomic stress responses. Nature Reviews. Neuroscience, 10(6), 397–409. 10.1038/nrn2647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Hurk P. A., Wingens T., Giommi F., Barendregt H. P., Speckens A. E., van Schie H. T. (2011). On the relationship between the practice of mindfulness meditation and personality-an exploratory analysis of the mediating role of mindfulness skills. Mindfulness, 2(3), 194–200. 10.1007/s12671-011-0060-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Stumm S., Ackerman P. L. (2013). Investment and intellect: A review and meta-analysis. Psychological Bulletin, 139(4), 841–869. 10.1037/a0030746 [DOI] [PubMed] [Google Scholar]
- Wang C. C., Li K., Choudhury A., Gaylord S. (2019). Trends in yoga, Tai Chi, and Qigong use among US adults, 2002-2017. American Journal of Public Health, 109(5), 755–761. 10.2105/AJPH.2019.304998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wettstein M., Tauber B., Wahl H. W. (2020). Associations between cognitive abilities and 20-year personality changes in older adults in the ILSE study: Does health matter? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 75(6), 1206–1218. 10.1093/geronb/gby155 [DOI] [PubMed] [Google Scholar]
- Yu C., Chao C., Cheng B. (2014). Effects of personality traits on the degree of exercise participation, physical self-description and social physique anxiety of hospital employees. Journal of Applied Sciences, 14(24), 3555–3562. 10.3923/JAS.2014.3555.3562 [DOI] [Google Scholar]
- Zhang Y., Li C., Zou L., Liu X., Song W. (2018). The effects of mind-body exercise on cognitive performance in elderly: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 15(12), 2791. 10.3390/ijerph15122791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimprich D., Allemand M., Lachman M. E. (2012). Factorial structure and age-related psychometrics of the MIDUS personality adjective items across the life span. Psychological Assessment, 24(1), 173–186. 10.1037/a0025265 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement Material, sj-pdf-1-ggm-10.1177_23337214221083475 for Mind-Body Practice, Personality Traits, and Cognitive Performance: A 10-Years Study in US Adults by Kallol Kumar Bhattacharyya, Debra Dobbs and Gizem Hueluer in Gerontology and Geriatric Medicine