Abstract
Background
Studies have reported the association between weight gain and nonalcoholic fatty liver disease (NAFLD) in the Asian population. We investigated the association between weight gain, NAFLD and significant fibrosis measured by transient elastography in a representative Unites States sample.
Methods
A cross-sectional study of 2849 participants was performed using the 2017-2018 National Health and Nutrition Examination Survey. We defined NAFLD by controlled attenuation parameter (CAP) scores and significant fibrosis (≥F2) by liver stiffness measurements using transient elastography, in the absence of other causes of chronic liver disease. A questionnaire that assessed weight change over 1 (short term) and 10 years (long term) was utilized.
Results
Age- and sex-adjusted odds ratios (OR) for NAFLD, comparing the third and fourth quartiles (weight-gain group) with the second quartile (weight-stable group, reference), were 1.61 (95% confidence interval [CI] 1.07-2.43) and 3.58 (95%CI 2.19-5.86), respectively. The association between weight gain and NAFLD remained significant after adjustment for demographic and metabolic risk factors (OR 1.87, 95%CI 1.19-2.95 for CAP score ≥263 dB/m; OR 2.23, 95%CI 1.48-3.35 for CAP ≥285 dB/m). In terms of significant fibrosis, multivariate-adjusted OR for significant fibrosis were 1.99 (95%CI 1.05-3.79 for the third quartile) and 3.12 (95%CI 1.46-6.65 for the fourth quartile), respectively. A statistically significant association between weight gain over 1 year and NAFLD was noted, whereas no such association was found between weight gain and significant fibrosis.
Conclusion
Weight gain over 10 years was associated with increased odds of NAFLD and significant fibrosis.
Keywords: Hepatic steatosis, weight, obesity, liver fibrosis, nonalcoholic fatty liver disease
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a growing healthcare burden worldwide, with an estimated global prevalence of 25% [1]. NAFLD comprises a broad spectrum of diseases, from nonalcoholic fatty liver to nonalcoholic steatohepatitis (NASH), significant fibrosis and end-stage liver disease, such as cirrhosis and hepatocellular carcinoma. Patients with NAFLD and fibrosis have a significantly increased risk of cardiovascular disease and liver-related mortality [2,3]. Hospitalization rates and the economic burden from NAFLD have increased compared to other etiologies of liver diseases in the United States (US) [4,5]. It is estimated that NAFLD is the most common cause of the rapidly increasing liver-related mortality worldwide [6].
Obesity has been identified as a risk factor in the pathogenesis of NAFLD and progression to NASH and fibrosis [7]. From 50-75% of obese individuals have NAFLD [7]. Obesity and weight gain were associated with the progression of liver fibrosis, defined by a noninvasive marker, in an Asian population with NAFLD [8]. It has been shown that fibrosis stage predicts severe liver disease and mortality in patients with NAFLD [9]. Although liver biopsy remains the gold standard for histological evaluation, transient elastography is a reliable noninvasive test to measure and monitor liver fibrosis, as well as to assess hepatic steatosis measured by the controlled attenuation parameter (CAP) [10]. A recent meta-analysis reported an association between weight loss interventions and improvement in NASH, but not in fibrosis [11]. Several studies have reported an association between weight gain and ultrasonography-diagnosed NAFLD, as well as fibrosis by noninvasive markers, in Asian control groups [8,12]. However, no studies have evaluated the impact of weight gain over 10 years on the risk of NAFLD as well as NAFLD-associated significant fibrosis, as measured by transient elastography, in the US population. Because of the lack of an approved pharmacologic treatment for NAFLD or fibrosis, there is a need to better understand modifiable risk factors for NAFLD as well as NAFLD-associated fibrosis to reduce the disease burden and associated healthcare costs. Therefore, we aimed to investigate the association between weight gain in the short- and long-term and NAFLD, as well as NAFLD-associated significant fibrosis measured by transient elastography, in the general US population.
Materials and methods
Study population
We analyzed data from the contemporary National Health and Nutrition Examination Survey (NHANES) 2017-2018. The NHANES dataset includes anthropometric measures as well as comprehensive questionnaires covering sociodemographic and lifestyle information, including weight history and detailed laboratory tests [13]. Ten-year data concerning weight were available for adults over 36 years; therefore, a total of 3843 participants were identified with a complete weight history. Five hundred forty-nine participants were excluded because of ineligible transient elastography or an incomplete examination. In addition, participants with viral hepatitis (presence of the hepatitis B surface antigen and/or hepatitis C virus RNA; n=62), exposure to steatogenic medications (such as amiodarone, corticosteroid, methotrexate, tamoxifen and valproate) for more than 6 months (n=69), significant alcohol consumption, defined as >30 g/day in men and >20 g/day in women [1], (n=83), and incomplete waist circumference data (n=114) were excluded. We also excluded participants with a medical history of fatty liver disease (n=79), medical history of other liver diseases (viral hepatitis, autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, a-1 antitrypsin deficiency, hemochromatosis, Wilson’s disease, alcohol related liver disease, liver cancer, liver fibrosis; n=32), and participants with HIV (n=6). Finally, a total of 2849 participants were included in this analysis (Fig. 1).
Figure 1.
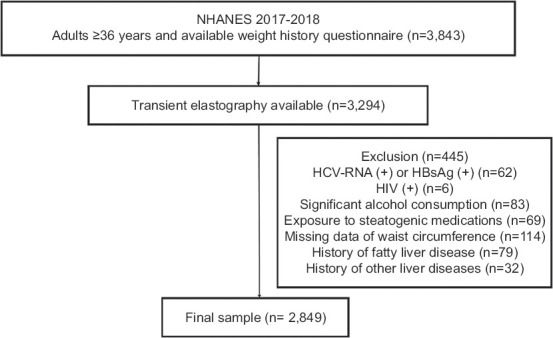
Flow chart showing cohort selection
Definition of NAFLD and significant fibrosis
We used previously proposed methods for the definition of NAFLD and significant fibrosis [14,15]. The FibroScan model 502 V2 Touch (Echosens, Waltham, MA) was equipped with medium or extra-large probes, which were used to estimate the CAP score and liver stiffness. Elastography results were considered as invalid and subsequently excluded if any of the following were present: <10 complete stiffness measurements out of up to 30 attempts, interquartile range/median ratio >30%, or <3 h of fasting before the examination [14,16,17]. We included individuals with serum aminotransferase <5 times the upper limit of the normal range. The interobserver reliability was 0.94 for CAP and 0.86 for liver stiffness [14,16]. We defined suspected NAFLD (≥S1) as CAP scores ≥263 dB/m (cutoff of sensitivity fixed at 90%) [14,18]. For the sensitivity analysis, we defined CAP scores ≥285 dB/m (cutoff optimizing sensitivity and specificity) as suspected NAFLD [14,18]. While most studies assign a cutoff of >250 dB/m for significant steatosis (>33% of hepatic steatosis), a prior study suggested a cutoff of 288 dB/m to detect >5% hepatic steatosis [19]. It should be noted that the CAP score can be affected by several factors, such as diabetes, body mass index, and NAFLD [19]. Liver stiffness of ≥8 kPa (≥F2) [10,19,20]. was used to define significant fibrosis in the cohort and among individuals with NAFLD.
Definition of weight changes
Weight changes over 10 years were calculated as the difference between present weight and weight 10 years before. Likewise, weight changes over a year were calculated as the difference between present weight and weight 1 year before. Weight changes were categorized into 4 weighted quartiles for 1 and 10 years, respectively. Weight changes over 10 years were categorized as follows: quartile 1, <-7 pounds (-3.18 kg); quartile 2, -7 pounds (-3.18 kg) to 6 pounds (2.72 kg); quartile 3, 6 pounds (2.72 kg) to 20 pounds (9.07 kg); and quartile 4, ≥20 pounds (9.07 kg). For the weight changes over a year, we categorized quartiles as follows: quartile 1, <-5 pounds (-2.27 kg); quartile 2, -5 pounds (-2.27 kg) to 0 pounds; quartile 3, 0-4 pounds (1.81 kg); and quartile 4, ≥4 pounds (1.81 kg). We used quartile 2 (weight-stable group) as the reference group. We categorized quartile 3 and quartile 4 as the weight-gain group and quartile 1 as the weight-loss group.
Statistical analysis
In view of the complex sampling design employed by the NHANES, we used appropriate sample weights to reconstruct representative data of the US population. According to quartiles for weight changes, baseline characteristics were compared using the c2 -test for categorical variables or linear regression for continuous variables. Data are shown as the weighted mean ± standard error or weighted frequency with 95% confidence intervals (CI), as appropriate. We used multivariate logistic regression analyses to determine the independent association between weight changes, NAFLD and NAFLD-associated fibrosis, after adjusting for multiple demographic and metabolic confounders, including age, sex, race/ethnicity, education level, marital status, smoking status, hypertension, diabetes, total cholesterol, high-density lipoprotein-cholesterol, physical activity, and weight circumference (model 2). We performed analyses using STATA 15.1 (StataCorp., College Station, Texas, USA).
Results
Weight changes over 10 years and NAFLD/significant fibrosis
As shown in Table 1, individuals in the weight-gain groups (quartiles 3 and 4) tended to be younger, female, Hispanic, non-Hispanic Black, current smokers, and more likely to have hypertension and diabetes compared to individuals in the weight-stable group. As expected, individuals in the weight-gain group had a higher body mass index, waist circumference, alanine aminotransferase, and gamma-glutamyl transferase than individuals in the weight-stable group. The prevalence of NAFLD (CAP scores of ≥263 dB/m) in the weight-gain group (68.8%, 95%CI 61.5-75.3 for quartile 4) was higher compared to the weight-stable group (44.4%, 95%CI 38.4-50.6 for quartile 2). Using another definition for NAFLD (CAP scores ≥285 dB/m), similar trends were noted (Table 1). The prevalence of NAFLD in the weight-loss group (quartile 1) was slightly higher than or comparable with that in the weight-stable group.
Table 1.
Characteristics of the study population according to weight change over 10 years. (n=2849)
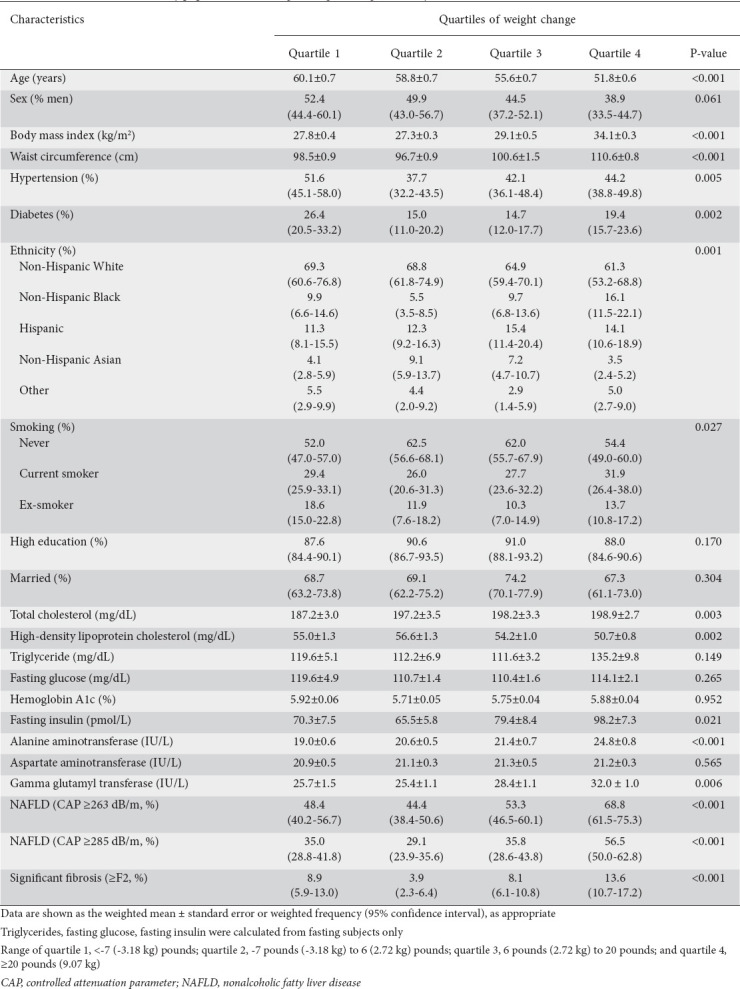
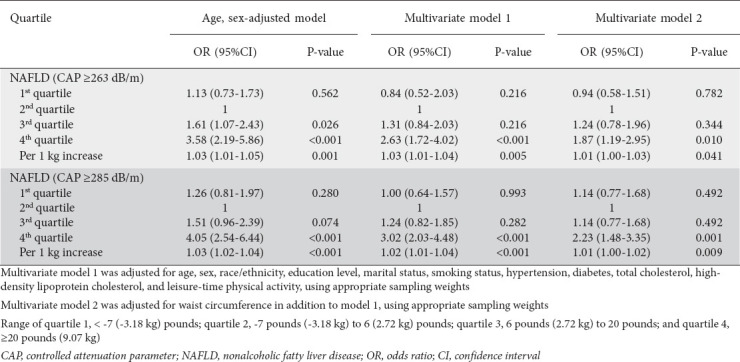
Table 2 shows univariate and multivariate analyses regarding the association between weight changes over 10 years and NAFLD. When NAFLD was defined as a CAP score of ≥263 dB/m, the weight-gain groups had increased odds of NAFLD compared to the weight-stable (reference) group in the age- and sex-adjusted model (odds ratio [OR] 1.61, 95%CI 1.07-2.43 for quartile 3; OR 3.58, 95%CI 2.19-5.86 for quartile 4). After adjustment for age, sex, race/ethnicity, education level, marital status, smoking status, hypertension, diabetes, total cholesterol, high-density lipoprotein cholesterol and physical activity, individuals who gained over 9.1 kg (20 pounds over 10 years) and composed quartile 4 had significantly greater odds of NAFLD (OR 2.63, 95%CI 1.72-4.02). For every kg gained, the odds of NAFLD increased by 3% (OR 1.03, 95%CI 1.01-1.04), after adjustment for multiple confounders. The addition of waist circumference to the model reduced the OR for NAFLD, but it remained significant (OR 1.87, 95%CI 1.19-2.95). This result suggests that the association between weight changes and NAFLD might be partly mediated by abdominal obesity. When sensitivity analyses were performed using a CAP score of ≥285 dB/m, similar and statistically significant associations between weight gain and NAFLD were observed in the univariate and multivariate models.
Table 2.
Multivariate odds ratio for NAFLD based on weight changes over 10 years
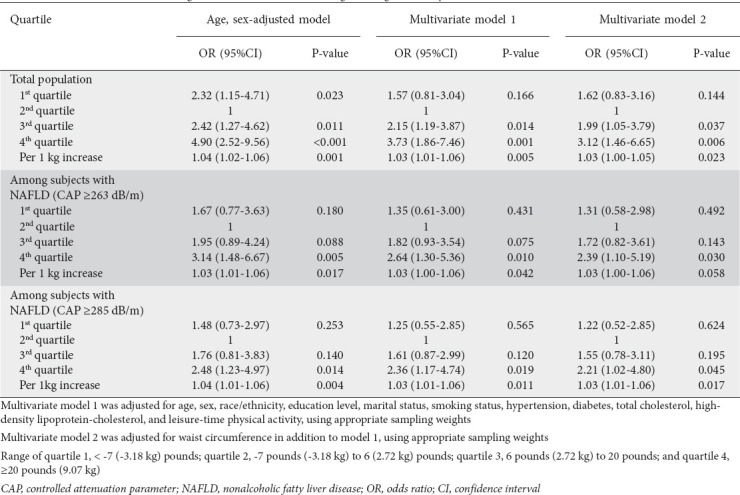
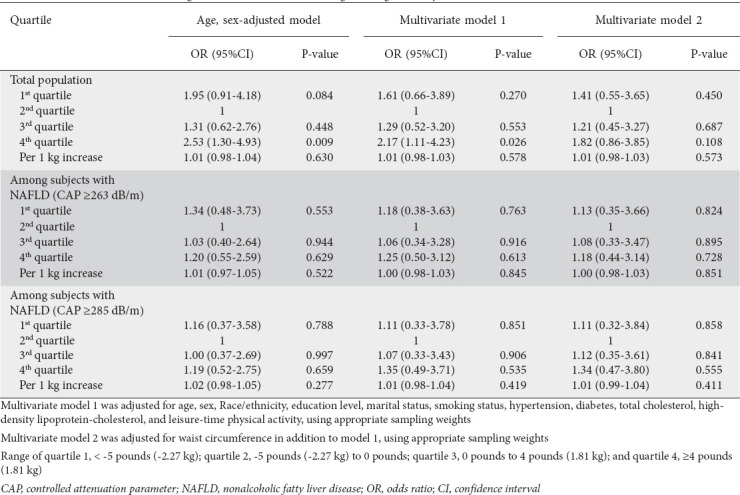
In terms of significant fibrosis (Table 3), the weight-gain groups had greater odds of significant fibrosis compared to the weight-stable group in the age- and sex-adjusted model (OR 2.42, 95%CI 1.27-4.62 for quartile 3; OR 4.90, 95%CI 2.52-9.56 for quartile 4). After adjustment for demographic and metabolic risk factors, the weight-gain groups had significantly greater odds of significant fibrosis compared to the weight-stable group (OR 2.15, 95%CI 1.19-3.87 for quartile 3; OR 3.73, 95%CI 1.86-7.46 for quartile 4). For every 1 kg of weight gain, the odds of significant fibrosis increased by 3% (OR 1.03, 95%CI 1.01-1.06). When waist circumference was included in the model, the association between weight changes and significant fibrosis was attenuated, but remained statistically significant. Sensitivity analyses were conducted among individuals with NAFLD using the different definitions of NAFLD based on different CAP score cutoff. Overall, the results were identical to those obtained using the cohort.
Table 3.
Multivariate odds ratio for significant fibrosis based on weight change over 10 years
Weight changes over 1 year and NAFLD/significant fibrosis
As shown in Supplementary Table 1 (189.9KB, pdf) , individuals in the weight-gain groups (quartiles 3 and 4) tended to be younger, more obese, female, Hispanic, non-Hispanic Black, current or ex-smokers, and more likely to have higher levels of liver enzymes compared to individuals in the weight-stable group. Consistent with previous results using weight changes over 10 years, the prevalence of NAFLD in the weight-gain group was higher than that in the weight-stable group, regardless of differences in the definition of NAFLD. Results of logistic regression analyses are presented in Table 4. Individuals who gained more than 1.81 kg (4 pounds; quartile 4) over a year had significantly greater odds of NAFLD (OR 3.55, 95%CI 2.31-5.47) in the age- and sex-adjusted model. When we considered demographic and metabolic risk factors (model 1) as well as waist circumference (model 2), the association between weight changes and NAFLD remained statistically significant (OR 3.91, 95%CI 2.32-6.58 for model 1; OR 3.15, 95%CI 1.76-5.67 for model 2). In addition, the odds of NAFLD increased significantly with every 1-kg increase over a year (OR 1.04, 95%CI 1.01-1.06). Sensitivity analyses were performed using a CAP score of ≥285 dB/m. Overall, the results were similar to those obtained using a CAP score of ≥263 dB/m. Regarding significant fibrosis in the total population (Table 5), individuals who gained more than 1.81 kg (4 pounds; quartile 4) over a year had greater odds of significant fibrosis in the age- and sex-adjusted model and multivariate model 1. However, this association became non-significant after waist circumference was taken into consideration. In addition, the odds of significant fibrosis were not linearly associated with weight gain (per 1-kg increase). Among individuals with NAFLD, weight gain of more than 1.81 kg (4 pounds; quartile 4) over a year was not associated with significant fibrosis in the age- and sex-adjusted model or in the multivariate models, regardless of the definition of NAFLD.
Table 4.
Multivariate odds ratio for NAFLD based on weight change over 1 year
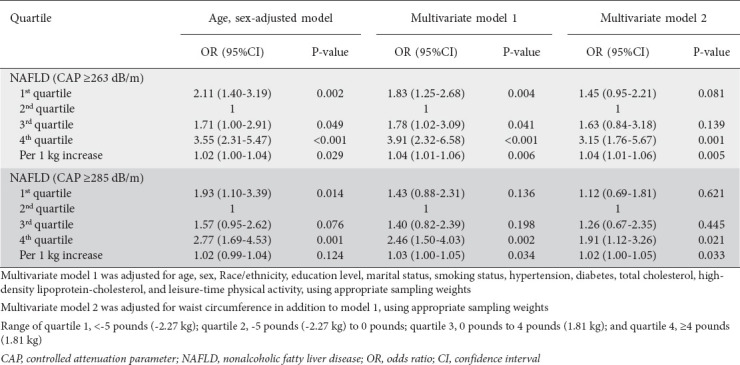
Table 5.
Multivariate odds ratio for significant fibrosis based on weight change over 1 year
Discussion
This study demonstrates the impact of weight gain over the short (1 year) and long (10 year) term on the risk of NAFLD and significant fibrosis, as measured by transient elastography. The current study found that adults who gained more than 9.07 kg (20 pounds) over 10 years had over 2-fold greater odds of NAFLD and an approximately 3-fold greater odds of significant fibrosis than those with stable weights. We found that weight gain over 10 years was associated with a greater risk of NAFLD and NAFLD-associated significant fibrosis, independently of demographic and metabolic risk factors. In addition, individuals who gained at least 1.81 kg (4 pounds) over a year had over 3-fold greater odds of NAFLD compared with those with stable weights.
A previous meta-analysis demonstrated a positive association between obesity and risk of NAFLD [21]. Several studies have demonstrated an association between weight gain, NAFLD and liver fibrosis in the Asian population [8,22,23]. Another study that evaluated 88 biopsy-proven patients with NAFLD over a 1-year follow up showed fibrosis progression in those with significant weight gain, defined as more than 5 kg [24]. The current study used a lower cutoff (1.81 kg, 4 pounds) over one year and did not demonstrate a significant association between weight gain and significant fibrosis. This may be explained by the fact that significant liver fibrosis takes time to progress or regress. However, our study found that weight gain over 10 years may increase the risk of NAFLD and significant fibrosis in a representative sample of the US general population, which is consistent with prior studies [8,21-24]. The fibrosis stage, not NASH, has been shown to predict mortality and the time for developing advanced liver disease in NAFLD [9]. As there are no approved pharmacologic treatments for NAFLD or fibrosis, avoiding weight gain may be another preventive option for NAFLD and significant fibrosis [25]. Thus, interventions aimed to prevent significant weight gain over a long-term period may prevent advanced liver disease in the general population and those with NAFLD.
Previous studies support the association between weight gain and the development of liver fibrosis and NAFLD [12,26-28]. Studies have demonstrated that short-term weight gain is an independent risk factor for NAFLD among nonobese Asian individuals [12,27]. However, no prior studies have investigated the long-term effect of weight gain in non-Asian populations. A recent prospective cohort study from Korea with a median follow up of 6 years reported that obesity and weight gain were associated with progression of liver fibrosis, assessed using the aspartate aminotransferase to platelet ratio index (APRI) [8]. However, that study had some limitations. The investigators used ultrasound for the diagnosis of NAFLD and APRI for the assessment of liver fibrosis. It has been shown that transient elastography is superior to ultrasound for detecting mild hepatic steatosis (>5% of hepatocytes) and superior to APRI for detecting significant fibrosis [29,30]. Thus, we used transient elastography in our study to diagnose NAFLD and significant fibrosis. In addition, the current study has long-term data on weight gain (over 10 years), which is a longer follow up than that in the recent prospective Korean study (6 years). Most of the studies that reported an association between weight gain, NAFLD and significant fibrosis were conducted in Asia (8,12,27). The current study used population-based data from the US, representing a more diverse race/ethnicity cohort.
The underlying mechanism behind the association between weight gain, NAFLD and liver fibrosis progression is not clearly understood. However, it is thought to be due to insulin resistance, inflammation, oxidative stress, and lipotoxicity that links to the progression of liver fibrosis [17,31-33]. However, one study showed a persistent, significant association between weight gain and noninvasive fibrosis assessment in NAFLD, after considering insulin resistance and high-sensitivity C-reactive protein [8]. This suggests multiple complex pathogenic mechanisms behind the association between weight gain and fibrosis in NAFLD. Some adipokines, such as leptin and adiponectin, may play a role in the pathogenesis of liver fibrosis progression in NAFLD [17]. Leptin is a pro-fibrogenic cytokine, while adiponectin has anti-fibrogenic and anti-inflammatory properties [34]. Thus, dysregulation of these adipokines may explain the risk of significant fibrosis in individuals with obesity and NAFLD [31,34,35].
The current study has several strengths. We used the CAP score to define NAFLD. The CAP score is a parameter with high accuracy for mild hepatic steatosis (>5% of hepatocytes) and has a higher sensitivity in identifying NAFLD than ultrasonography or noninvasive serum panels for NAFLD [36]. In addition, we defined significant fibrosis using transient elastography, not noninvasive serum panels [29,30]. To date, there have been no prior studies focusing on the US population that have investigated the association between weight changes over 10 years, NAFLD and significant fibrosis, measured by transient elastography. Therefore, the findings of this study may be generalizable to the Western world, which shares similar demographic, lifestyle, and behavioral health patterns with those of the US.
The current study has also several limitations. First, we used a weight history questionnaire, which is at risk of recall bias. Second, this study cannot offer definitive conclusions regarding causality. Third, we were unable to obtain transient elastography data at baseline prior to 1 and 10 years. Therefore, we were not able to provide NAFLD and significant fibrosis status at 1 and 10 years before, although we excluded participants with a medical history of fatty liver and liver fibrosis/cirrhosis. This may explain why weight loss was not inversely associated with NAFLD and significant fibrosis. The weight-loss group had a higher prevalence of diabetes, hypertension, NAFLD and significant fibrosis, and was older than the weight-stable group. In addition, because of limitations in the NHANES dataset, we were unable to obtain information regarding extrahepatic cholestasis or systemic diseases affecting the liver, which may be uncommon in the general population. Fourth, there is no universal cutoff to determine NAFLD using the CAP score or to determine significant fibrosis in NAFLD using liver stiffness by transient elastography. However, we used validated cutoff points for the CAP score and liver stiffness, based on previously published studies [10,19,20]. Fifth, our study design meant we were unable to retrieve medications that may affect the prevalence or the progression of NAFLD. Future studies will be needed to determine the impact of medication on the association between weight gain and NAFLD. Moreover, because of the complex survey design applied by the NHANES, we were unable to perform a post hoc analysis after adjustment for appropriate sample weights.
In conclusion, weight gain over 10 years is associated with greater odds of NAFLD and significant fibrosis in US adults, independently of known demographic and metabolic risk factors. In addition, weight gain over a year is closely associated with an increase in the odds of NAFLD.
Summary Box.
What is already known:
● Studies have reported an association between weight gain, nonalcoholic fatty liver disease (NAFLD), and liver fibrosis in the Asian population
● No studies have evaluated the impact of long-term weight gain on the risk of NAFLD and fibrosis in the Western population
● There is an urgent need to understand modifiable risk factors for NAFLD to reduce disease burden and associated healthcare costs
What the new findings are:
● This cross-sectional study showed that weight gain over 10 years was associated with a greater risk of NAFLD and significant fibrosis in United States adults
● Weight gain over a year was closely associated with an increase in the odds of NAFLD
Biography
University of Michigan, Ann Arbor, MI; University of Minnesota, Minneapolis, MN; Stanford University School of Medicine, Stanford, CA, USA
Footnotes
Conflict of Interest: Karn Wijarnpreecha received funding from the AASLD Advanced/Transplant Hepatology Award. Other coauthors have no conflict of interest
References
- 1.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease –meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Unalp-Arida A, Ruhl CE. Noninvasive fatty liver markers predict liver disease mortality in the U.S. population. Hepatology. 2016;63:1170–1183. doi: 10.1002/hep.28390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim D, Kim WR, Kim HJ, Therneau TM. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013;57:1357–1365. doi: 10.1002/hep.26156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim D, Cholankeril G, Li AA, et al. Trends in hospitalizations for chronic liver disease-related liver failure in the United States, 2005-2014. Liver Int. 2019;39:1661–1671. doi: 10.1111/liv.14135. [DOI] [PubMed] [Google Scholar]
- 5.Murag S, Ahmed A, Kim D. Recent epidemiology of nonalcoholic fatty liver disease. Gut Liver. 2021;15:206–216. doi: 10.5009/gnl20127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Changes in the global burden of chronic liver diseases from 2012 to 2017:the growing impact of NAFLD. Hepatology. 2020;72:1605–1616. doi: 10.1002/hep.31173. [DOI] [PubMed] [Google Scholar]
- 7.Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease:from pathophysiology to therapeutics. Metabolism. 2019;92:82–97. doi: 10.1016/j.metabol.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y, Chang Y, Cho YK, Ahn J, Shin H, Ryu S. Obesity and weight gain are associated with progression of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17:543–550. doi: 10.1016/j.cgh.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Hagström H, Nasr P, Ekstedt M, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67:1265–1273. doi: 10.1016/j.jhep.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 10.Eddowes PJ, Sasso M, Allison M, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1717–1730. doi: 10.1053/j.gastro.2019.01.042. [DOI] [PubMed] [Google Scholar]
- 11.Koutoukidis DA, Astbury NM, Tudor KE, et al. Association of weight loss interventions with changes in biomarkers of nonalcoholic fatty liver disease:a systematic review and meta-analysis. JAMA Intern Med. 2019;179:1262–1271. doi: 10.1001/jamainternmed.2019.2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamada G, Hagiwara Y, Kimura T, et al. Impact of body weight gain on the incidence of nonalcoholic fatty liver disease in nonobese Japanese individuals. Am J Gastroenterol. 2021;116:733–740. doi: 10.14309/ajg.0000000000001030. [DOI] [PubMed] [Google Scholar]
- 13.CDC National Health and Nutrition Examination Survey (NHANES) Liver ultrasound transient elastography procedures manual. 2018. [Accessed 15 January 2022]. Available from: https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/manuals/2018_Liver_Ultrasound_Elastography_Procedures_Manual.pdf .
- 14.Kim D, Cholankeril G, Loomba R, Ahmed A. Prevalence of fatty liver disease and fibrosis detected by fibroscan in adults in the United States, 2017-2018. Clin Gastroenterol Hepatol. 2020;19:1499–1501.e2. doi: 10.1016/j.cgh.2020.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Kim D, Cholankeril G, Loomba R, Ahmed A. Prevalence of nonalcoholic fatty liver disease and hepatic fibrosis among US adults with prediabetes and diabetes, NHANES 2017-2018. J Gen Intern Med. 2022;37:261–263. doi: 10.1007/s11606-021-06677-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CDC National Health and Nutrition Examination Survey. 2017-2018 Data documentation, codebook, and frequencies. Liver ultrasound transient elastography (LUX_J) 2020. [Accessed 15 January 2022]. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/LUX_J.htm .
- 17.Tilg H. Adipocytokines in nonalcoholic fatty liver disease:key players regulating steatosis, inflammation and fibrosis. Curr Pharm Des. 2010;16:1893–1895. doi: 10.2174/138161210791208929. [DOI] [PubMed] [Google Scholar]
- 18.Siddiqui MS, Vuppalanchi R, Van Natta ML, et al. NASH Clinical Research Network. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17:156–163. doi: 10.1016/j.cgh.2018.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1264–1281. doi: 10.1053/j.gastro.2018.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abeysekera KWM, Fernandes GS, Hammerton G, et al. Prevalence of steatosis and fibrosis in young adults in the UK:a population-based study. Lancet Gastroenterol Hepatol. 2020;5:295–305. doi: 10.1016/S2468-1253(19)30419-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li L, Liu DW, Yan HY, Wang ZY, Zhao SH, Wang B. Obesity is an independent risk factor for non-alcoholic fatty liver disease:evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016;17:510–519. doi: 10.1111/obr.12407. [DOI] [PubMed] [Google Scholar]
- 22.Du S, Wang C, Jiang W, et al. The impact of body weight gain on nonalcoholic fatty liver disease and metabolic syndrome during earlier and later adulthood. Diabetes Res Clin Pract. 2016;116:183–191. doi: 10.1016/j.diabres.2016.04.047. [DOI] [PubMed] [Google Scholar]
- 23.Zhang WJ, Chen LL, Zheng J, Lin L, Zhang JY, Hu X. Association of adult weight gain and nonalcoholic fatty liver in a cross-sectional study in Wan Song Community, China. Braz J Med Biol Res. 2014;47:151–156. doi: 10.1590/1414-431X20133058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 25.Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67:829–846. doi: 10.1016/j.jhep.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 26.Ratziu V, Giral P, Charlotte F, et al. Liver fibrosis in overweight patients. Gastroenterology. 2000;118:1117–1123. doi: 10.1016/s0016-5085(00)70364-7. [DOI] [PubMed] [Google Scholar]
- 27.Liu CJ. Prevalence and risk factors for non-alcoholic fatty liver disease in Asian people who are not obese. J Gastroenterol Hepatol. 2012;27:1555–1560. doi: 10.1111/j.1440-1746.2012.07222.x. [DOI] [PubMed] [Google Scholar]
- 28.Ting YW, Wong SW, Anuar Zaini A, Mohamed R, Jalaludin MY. Metabolic syndrome is associated with advanced liver fibrosis among pediatric patients with non-alcoholic fatty liver disease. Front Pediatr. 2019;7:491. doi: 10.3389/fped.2019.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Göbel T, Schadewaldt-Tümmers J, Greiner L, Poremba C, Häussinger D, Erhardt A. Transient elastography improves detection of liver cirrhosis compared to routine screening tests. World J Gastroenterol. 2015;21:953–960. doi: 10.3748/wjg.v21.i3.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang GL, Zhao QY, Lin CS, Hu ZX, Zhang T, Gao ZL. Transient elastography and ultrasonography:optimal evaluation of liver fibrosis and cirrhosis in patients with chronic hepatitis B concurrent with nonalcoholic fatty liver disease. Biomed Res Int. 2019;2019:3951574. doi: 10.1155/2019/3951574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fabbrini E, Sullivan S, Klein S. Obesity and nonalcoholic fatty liver disease:biochemical, metabolic, and clinical implications. Hepatology. 2010;51:679–689. doi: 10.1002/hep.23280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neuschwander-Tetri BA. Hepatic lipotoxicity and the pathogenesis of nonalcoholic steatohepatitis:the central role of nontriglyceride fatty acid metabolites. Hepatology. 2010;52:774–788. doi: 10.1002/hep.23719. [DOI] [PubMed] [Google Scholar]
- 33.Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic fatty liver disease:mechanisms and clinical implications. Semin Liver Dis. 2015;35:132–145. doi: 10.1055/s-0035-1550065. [DOI] [PubMed] [Google Scholar]
- 34.Park PH, Sanz-Garcia C, Nagy LE. Adiponectin as an anti-fibrotic and anti-inflammatory adipokine in the liver. Curr Pathobiol Rep. 2015;3:243–252. doi: 10.1007/s40139-015-0094-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Landecho MF, Tuero C, Valenti V, Bilbao I, de Higuera, Fruhbeck G. Relevance of leptin and other adipokines in obesity-associated cardiovascular risk. Nutrients. 2019;11:2664. doi: 10.3390/nu11112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karlas T, Petroff D, Sasso M, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–1030. doi: 10.1016/j.jhep.2016.12.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


