ABSTRACT.
Despite reports of enterotoxigenic Bacteroides fragilis (ETBF) isolation from asymptomatic children, no reports exist regarding the possible association of ETBF with long-term complications such as development of environmental enteric dysfunction (EED) and subsequent linear growth faltering in childhood. We aimed to establish a potential association between the burden of asymptomatic ETBF infection and EED and linear growth at 24 months of age using the data collected from 1,715 children enrolled in the multi-country birth cohort study, known as the Etiology, Risk Factors, and Interactions of Enteric Infections and Malnutrition and the Consequences for Child Health study. Using Poisson regression models, we evaluated the site-specific incidence rate and, subsequently, identified the risk factors and assessed the association between the burden of ETBF infection and EED score and linear growth at 24 months of age. The overall incidence rate of ETBF infections per 100 child-months across all study sites was 10.6%, with the highest and lowest incidence of ETBF infections being reported in Tanzania (19.6%) and Peru (3.6%), respectively. Female gender, longer duration of breastfeeding, and improved water access, sanitation, and hygiene practices, such as improved drinking water source, improved sanitation, and improved floor material in households, along with enhanced maternal education and less crowding in the households were found to be protective against incidences of ETBF infection. The burden of ETBF infections was found to have significant associations with EED and linear growth faltering at 24 months of age across all the study sites. Our findings warrant regular clinical monitoring to reduce the burden of ETBF infections and diminish the burden of enteropathy and linear growth faltering in childhood.
INTRODUCTION
Childhood malnutrition accounts for approximately 45% of the cases of “under-five” mortality and has been reported to be associated strongly with a number of acute illnesses and severe damage to several physiological activities, including restricted mental growth and development in later life, cardiovascular and chronic respiratory illnesses, and compromised host immunity.1,2 Stunting or linear growth faltering (length-for-age z-score [LAZ] < 2 points of the WHO growth standard) is the most prevalent form of childhood malnutrition and affects an estimated 149 million children worldwide.3,4 The first 2 years of life are a critical window for long-term growth and development, and stunting has been reported to exhibit extremely serious and adverse consequences in children younger 2 years of age.5 Repeated exposure to fecal enteropathogens in early life and subsequent development of environmental enteric dysfunction (EED) are considered to be the primary factors attributing to linear growth failure in the early years of life.6
EED refers to functional changes in the gut, including influx of inflammatory cells to the intestine and consequent local and systemic inflammation resulting from damage to intestinal epithelial cells, increased permeability, and microbial translocation into the lamina propria as a result of a number of environmental determinants, which are often reversible.7 Chronic exposure to enteropathogens leading to persistent immune activation, increased intestinal permeability, and enteric inflammation are hallmarks of EED.8,9 Small intestine biopsy is considered to be the gold standard for the diagnosis of EED, but it is not feasible to perform in children because of the invasiveness protocols involved with the procedure.10 Consequently, several fecal biomarkers—namely, myeloperoxidase (MPO), neopterin (NEO), and α-1-antitrypsin (AAT)—have been reported to be associated with EED and have been proposed as noninvasive alternatives for the assessment of EED.11,12 Among these biomarkers in stool, MPO and NEO are markers of intestinal inflammation, whereas AAT indicates loss of serum proteins into the intestinal lumen as a result of altered intestinal permeability.13
Enterotoxigenic Bacteroides fragilis (ETBF) is an enteropathogen that causes diarrhea in both children and adults, and is one of the leading anaerobic isolates in clinical specimens.14 The prevalence of the association of ETBF with diarrhea has been reported to vary across geographic locations, ranging from 3.5% in Bangladesh to 28% in Italy.15 Sack et al.16 reported ETBF to be an important etiological agent in acute diarrhea in children older than 1 year in an age-structured case–control study. ETBF is known to produce a 20-kDa zinc-dependent, non-lethal, heat-labile metalloprotease known as “fragilysin,” which acts by cleaving the E-cadherin protein of zonula adherens and tight junctions, potentially leading to altered intestinal permeability.17,18 This toxin has been reported to result in swelling and rounding of the cultured enteric cell lines.19,20 Subsequent findings from a study conducted among children and adults with acute diarrheal illnesses in Dhaka, Bangladesh, indicate that ETBF induces intestinal inflammation.21 In one report, two to four sequential episodes of ETBF-associated diarrhea were reported for children in Bangladesh, suggesting that acquired immunity to ETBF is incomplete.22
Similar to the case for other enteric pathogens, asymptomatic ETBF colonization is common and the prevalence ranges from 4% to 20% for asymptomatic ETBF infection.15,23 Findings from an endoscopy-based study reported that ETBF was recovered from 35% of stool samples of control patients without diarrhea.24 However, the relationship between the burden of ETBF infection on the potential development of enteric inflammation and subsequent linear growth failure has not been reported. Therefore, we conducted this study using data from a multi-country birth cohort study to estimate incidence rates of ETBF infections across different geographic locations, and to establish a possible relationship between EED and linear growth among children at 24 months of age.
MATERIALS AND METHODS
Study design and ethical statement.
The study design of the multi-country birth cohort Etiology, Risk Factors, and Interactions of Enteric Infections and Malnutrition and the Consequences for Child Health (MAL-ED) study, conducted across eight sites (Bangladesh, Brazil, India, Nepal, Peru, Pakistan, South Africa, and Tanzania) in South America, sub-Saharan Africa, and Asia have been described previously.25 In short, 1,715 children were enrolled from November 2009 to February 2012 from the community within 17 days of birth at all eight sites and were monitored up to 24 months of age. The study was approved by the respective institutional review boards at each of the eight study sites.25 Written, informed voluntary consent was obtained from the parents or legal guardians of every child.
Collection of anthropometric, sociodemographic, and morbidity data.
Anthropometric indices of LAZ, weight-for-age z-score, and weight-for-length z-score were calculated according to 2006 WHO standards for children26 using data of monthly anthropometric measurements done up to the age of 24 months, using standard scales (seca GmbH & Co. KG, Hamburg, Germany). Sociodemographic data on the child’s birth, including birthweight, anthropometric indices at birth, presence of siblings, and other maternal characteristics, were collected at enrollment.25 A detailed account of any morbidity and child feeding practices was obtained during household visits, which were conducted twice weekly.27
Socioeconomic data were collected every 6 months, starting from 6 months of age of the participant. The water, sanitation, hygiene, asset, maternal education, and income index (WAMI), which ranges from 0 to 1 point, is an index of socioeconomic status of the households28 and was calculated subsequently. Greater socioeconomic status was indicated by a higher WAMI.29 WHO guidelines were followed to define improved water and sanitation,30 whereas treatment of drinking water was defined as filtering, boiling, or adding bleach.31
Collection of stool and blood samples.
Across all the study sites, non-diarrheal stool samples were collected each month (at least 3 days before or after a diarrhea episode) after enrollment and up to the age of 24 months. No diarrheal samples were analyzed in this study. Venous blood samples were collected at 7, 15, and 24 months of age.32 After collecting these biological samples, they were processed in the laboratories across all the sites according to the same standardized procedures and were stored in –80 °C freezers before subsequent laboratory analysis.33
Plasma zinc, a proxy marker that is also recommended for assessment of zinc status in children,34 was assessed at 7, 15, and 24 months using lame atomic absorption spectrophotometry (Shimadzu AA-6501S, Kyoto, Japan).35 α-1-Acid glycoprotein (AGP) in plasma, a biomarker for systemic inflammation,36 was assessed at 7, 15, and 24 months using an immunoturbidimetric assay with commercial kits from Roche Diagnostics on a Roche automated clinical chemistry analyzer (Hitachi-902, Boehringer Mannheim, Germany).
Evaluation of biomarkers of enteric inflammation and calculation of EED score.
Enteric inflammation was ascertained by measuring the levels of the inflammatory biomarkers MPO (Alpco, Salem, NH), NEO (GenWay Biotech, San Diego, CA), and AAT (Biovendor, Chandler, NC) in the stool samples collected from the study participants at 3, 6, 9, 15, and 24 months by quantitative ELISA using manufacturer guidelines.25 At each time point, the EED score, ranging from 0 to 10 points, was calculated from the three fecal markers, as described in previous studies.37,38 Categories were assigned the values 0 point (low), 1 point (medium), or 2 points (high). MPO, NEO, and AAT values were log‐transformed prior to subsequent analysis. The formula used for the calculation of the EED score is as follows:37
Assessment of enteropathogens by TaqMan array cards.
TaqMan array cards, customized multiplex quantitative polymerase chain reaction involving compartmentalized primer-probe assays, were used to detect a possible 29 pathogens from each of the samples, using protocols described elsewhere.39,40 The quantification cycle value of 35 was set as a threshold for analysis, as mentioned elsewhere.39 In our study, we investigated the occurrence of the bft gene of ETBF, and positive cases were analyzed further for co-infection for the presence of distinct other co-pathogens—namely, Campylobacter sp., enterotoxigenic Escherichia coli (ETEC), enteroaggregative E. coli (EAEC), typical enteropathogenic E. coli (tEPEC), Shigella/enteroinvasive E. coli, Cryptosporidium spp. and Giardia spp., as described previously.41
Statistical analysis.
All statistical analyses were performed using STATA V13 (Stata Corp. LLC, College Station, TX). Data were summarized as either the mean and sd or as the median with the interquartile range, depending on the distribution of the data. Poisson regression was used to calculate the incidence rates for ETBF infection, whereby the number of ETBF infections was considered the outcome variable and the log of several follow-ups was considered the offset variable.
Determinants for the monthly detection of ETBF in the stool samples were assessed using Poisson regression models, whereby the variables that were included in the final model, adjusting for all study sites and using stepwise forward selection, were gender of the participant, duration of exclusive breast feeding in months, LAZ at enrollment, maternal height, maternal age, maternal education, improved floor, access to an improved drinking water source, routine treatment of drinking water, lack of improved sanitation, more than two people living per room, mother having more than three living children, and household ownership of chicken or cattle.
The burden of ETBF infections was defined as the number of ETBF infections over the total number of follow-ups conducted throughout the study period. Associations between the burden of ETBF infection and linear growth and EED score at 24 months of age was determined using multivariate linear regression after adjusting for potential covariates—namely, gender of the participant, exclusive breast feeding, LAZ at enrollment, maternal age, maternal height, WAMI, more than two people living per room, mother having more than three living children, household ownership of chicken or cattle, plasma AGP level at 24 months, plasma zinc level at 24 months, and burden of other malnutrition associated co-pathogens during the study period (Campylobacter, ETEC, EAEC, tEPEC, Shigella sp., Cryptosporidium, and Giardia) for the overall estimate. For the growth analysis, we excluded the data collected from the participants enrolled at the Pakistan site because of bias noted at this site during the study period. Because the aim of our study was to analyze the possible association between burden of ETBF infection with enteric inflammation and linear growth at 24 months, we considered the plasma AGP and zinc levels at 24 months only.
The selection of the variables for the multivariate analysis was based on prior literature review,42 after which we prepared a conceptual framework for factors influencing enteric inflammation and subsequent linear growth from birth up until 2 years of life. Multicollinearity between the variables adjusted in the variance inflation factor was calculated, and no variable producing a variance inflation factor value of more than the threshold of five was found in the final model. The strength of association was evaluated by estimating the β-coefficient and its corresponding 95% CI. P < 0.05 was considered statistically significant during the analysis.
RESULTS
A total of 1,715 participants were enrolled across the eight different study sites, and a total of 34,622 monthly non-diarrheal stool samples were collected from the study participants throughout the entire study period, starting from their enrollment after birth. Table 1 shows the general characteristics of the study participants enrolled at each of the eight study sites.
Table 1.
General characteristics of the study participants enrolled at all the eight study sites
| Characteristics | Bangladesh (n = 210) | Brazil (n = 165) | India (n = 227) | Nepal (n = 227) | Peru (n = 194) | Pakistan (n = 246) | South Africa (n = 237) | Tanzania (n = 209) |
|---|---|---|---|---|---|---|---|---|
| Male gender (n, %) | 108 (51.4) | 89 (53.94) | 105 (46.3) | 122 (53.7) | 105 (54.1) | 120 (48.8) | 120 (50.6) | 105 (50.2) |
| Birthweight, kg | 2.8 ± 0.4 | 3.4 ± 0.5 | 2.9 ± 0.4 | 3.0 ± 0.4 | 3.1 ± 0.4 | 2.7 ± 0.4 | 3.2 ± 0.5 | 3.2 ± 0.5 |
| LAZ at enrollment | –1.0 ± 1.0 | –0.8 ± 1.1 | –1.0 ± 1.1 | –0.7 ± 1.0 | –0.9 ± 1.0 | –1.3 ± 1.1 | –0.7 ± 1.0 | –1.0 ± 1.1 |
| LAZ at 24 mo | –2.0 ± 0.9 | 0.0 ± 1.1 | –1.9 ± 1.0 | –1.3 ± 0.9 | –1.9 ± 0.9 | – | –1.7 ± 1.1 | –2.7 ± 1.0 |
| WAZ at enrollment | –1.3 ± 0.9 | –0.2 ± 1.0 | –1.3 ± 1.0 | –0.9 ± 1.0 | –0.6 ± 0.9 | –1.4 ± 1.0 | –0.4 ± 1.0 | –0.1 ± 1.1 |
| WAZ at 24 mo | –0.8 ± 0.9 | 0.5 ± 1.4 | –0.9 ± 0.9 | –0.3 ± 0.9 | 0.3 ± 0.9 | – | 0.5 ± 1.0 | 0.1 ± 1.0 |
| Days of exclusive breastfeeding | 143.2 ± 42.7 | 93.7 ± 57.8 | 105.4 ± 42.9 | 92.5 ± 54.5 | 89.5 ± 61.3 | 19.9 ± 22.7 | 38.6 ± 26.3 | 62.2 ± 35 |
| Maternal age during enrollment, y | 25 ± 5 | 25.4 ± 5.6 | 23.9 ± 4.2 | 26.6 ± 3.7 | 24.8 ± 6.3 | 28.1 ± 5.9 | 27 ± 7.2 | 29.1 ± 6.5 |
| Maternal BMI during enrollment | 22.3 ± 3.4 | 25.7 ± 4.4 | 22.0 ± 4.0 | 25.1 ± 3.2 | 24.9 ± 3.7 | 21.5 ± 3.8 | 27 ± 5.5 | 22.9 ± 3.2 |
| Maternal education > 6 y of schooling, n (%) | 77 (36.7) | 413 (86.7) | 147 (64.8) | 168 (74) | 150 (77.3) | 44 (17.9) | 233 (97.9) | 134 (64.1) |
| Presence of more than 3 living children at household during enrollment, n (%) | 160 (76.2) | 113 (68.5) | 157 (69.8) | 199 (87.7) | 111 (57.2) | 105 (42.7) | 141 (59.5) | 58 (27.8) |
| More than 2 people living per room, n (%) | 202 (96.2) | 24 (14.5) | 181 (79.7) | 101 (44.5) | 72 (37.1) | 219 (89.1) | 36 (15.2) | 114 (54.5) |
| Improved drinking water source, n (%) | 210 (100) | 165 (100) | 227 (100) | 227 (100) | 184 (94.9) | 246 (100) | 196 (82.7) | 89 (42.6) |
| Improved floor, n (%) | 204 (97.1) | 165 (100) | 222 (97.8) | 109 (48) | 69 (35.6) | 81 (32.9) | 231 (97.5) | 13 (6.2) |
| Average plasma zinc level, mmol/L; median (IQR) | 11.3 (10.6– 12.1) | 14 (13– 14.9) | 9.1 (8.6– 9.6) | 11.2 (10.4–12.2) | 14.8 (13.1–17.9) | 8.9 (7.7–10) | 22.9 (14.3–32.9) | 11.1 (9.9–12.3) |
| Average plasma AGP, mg/dL; median, (IQR) | 84.3 (71.5– 105.3) | 95.7 (81– 117) | 97 (83–110) | 117.7 (102.7– 139) | 115 (98– 130.3) | 93 (77.5– 111.8) | 126 (107.3–153.7) | 114.3 (97.7–138.7) |
AGP = α-1-acid glycoprotein; BMI = body mass index; IQR = interquartile range; LAZ = length-for-age z-score, WAZ = weight-for-age z-score, WHZ = weight-for-height z-score. Data are presented as mean ± sd unless otherwise mentioned.
The proportion of male participants was the highest in Peru and the lowest in India, whereas birthweight was the highest in Brazil and the lowest in Pakistan. The longest duration of exclusive breastfeeding was found in Bangladesh; the shortest duration was found in Pakistan. Maternal education (as defined by more than 6 years of schooling) was the highest in South Africa and lowest in Pakistan. Access to improved drinking water in the households of all enrolled study participants was reported in Bangladesh, Brazil, India, Nepal, and Pakistan. The highest average plasma zinc and plasma AGP levels throughout the study period was found in South Africa.
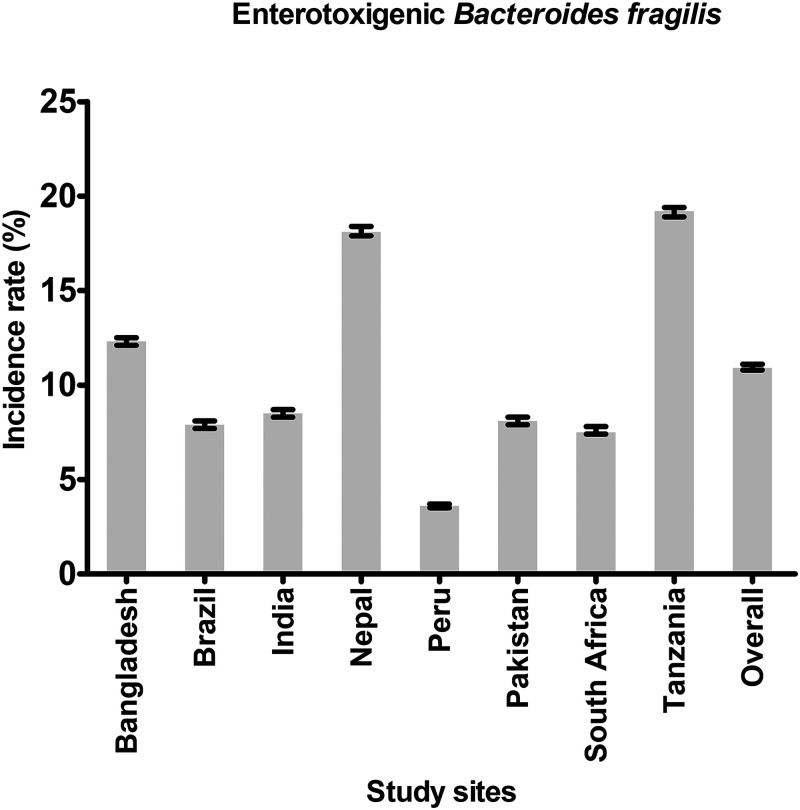
The incidence rates of ETBF infection per 100 child-months across each of the eight study sites over the 24-month study period is shown in Figure 1. The overall incidence rate of ETBF infection across all eight study sites was 10.9%. The highest incidence rate of ETBF infection per 100 child-months was found in Tanzania (19.2%); the lowest incidence rate was found in Peru (3.6%).
Figure 1.
Incidence rates of enterotoxigenic Bacteroides fragilis per 100 child-months among the participants enrolled at each of the eight study sites. Error bars = 95% CI.
Sociodemographic factors associated with ETBF infection.
Table 2 shows the relationship between different sociodemographic factors and ETBF infection across the eight different study sites. Female gender was found to have a significantly lower association with the incidence rate of ETBF infection per 100 child-months. Duration of exclusive breastfeeding, maternal height, maternal age, and routine treatment of drinking water did not have any association with the incidence rate of ETBF infection. However, increased maternal education, access to improved drinking water, and improved floor material in the households were found to be associated with a significantly lower incidence rate of ETBF infection per 100 child-months. Consequently, other sociodemographic factors such as lack of access to improved sanitation, more than two people living per room, mother having more than three living children, and household ownership of chicken or cattle were found to be significantly associated with an increased incidence rate of ETBF infection per 100 child-months.
Table 2.
Sociodemographic factors associated enterotoxigenic Bacteroides fragilis infection in each of the eight study sites
| Factors | Incidence rate ratio of B. fragilis detection per 100 child-months (95% CI) | P value |
|---|---|---|
| Female gender | 0.96 (0.94–0.97) | < 0.001 |
| Duration of exclusive breastfeeding, mo | 0.98 (0.96–0.99) | < 0.001 |
| LAZ at enrollment | 0.98 (0.97–0.99) | < 0.001 |
| Maternal height, cm | 1.0 (0.99–1.0) | 0.352 |
| Maternal age, y | 1.0 (0.99–1.0) | 0.004 |
| Maternal education > 6 y | 0.89 (0.88–0.91) | < 0.001 |
| Improved drinking water source | 0.92 (0.90–0.95) | < 0.001 |
| Routine treatment of drinking water | 1.0 (0.98–1.02) | 0.732 |
| Lack of improved sanitation | 1.21 (1.18–1.25) | < 0.001 |
| Improved floor material in households | 0.93 (0.90–0.95) | < 0.001 |
| More than 2 people living in a single room | 1.04 (1.02–1.05) | < 0.001 |
| Mother has more than 3 living children | 1.10 (1.07–1.11) | < 0.001 |
| Household ownership of chicken or cattle | 1.15 (1.13–1.17) | < 0.001 |
LAZ = length-for-age z-score. A Poisson regression model was used. The dependent variable was the number of infections during follow-up (1–24 months) and the offset variable was the log of the total number of follow-ups. All analyses were adjusted for different study sites and all variables included in the multivariable model.
Association between the burden of ETBF infection and enteric inflammation and linear growth at 24 months of age.
Table 3 shows the results of a separate analysis involving the association between the burden of ETBF infection with enteric inflammation and linear growth at 24 months of age. After adjusting for variables such as gender of the participant, exclusive breastfeeding, LAZ at enrollment, maternal age, maternal height, WAMI, more than two people living per room, mother having more than three living children, household ownership of chicken or cattle, plasma AGP level at 24 months, plasma zinc level at 24 months, and presence of other malnutrition associated co-pathogens (Campylobacter sp., ETEC, EAEC, tEPEC, Shigella sp., Cryptosporidium sp. and Giardia sp.), the burden of ETBF infection over the study period across all eight study sites was found to have a positive association with enteric inflammation at 24 months of age, as expressed by the EED score. Consequently, linear growth at 24 months as expressed by LAZ was found to be associated negatively with the burden ETBF infection over the study period across all eight study sites. Our findings indicate that with a 1-U increase in the burden of ETBF infection, the EED score at 24 months would be likely to increase by 0.256 U, and LAZ at 24 months would be likely to decrease by 0.155 U.
Table 3.
Association between burden of enterotoxigenic Bacteroides fragilis infection on enteric inflammation and linear growth at 24 months of age
| Outcome variable | EED score at 24 months | LAZ at 24 months | ||
|---|---|---|---|---|
| Adjusted β-coefficient, 95% CI | P value | Adjusted β-coefficient (95% CI) | P value | |
| Burden of ETBF infection | 0.256 | 0.024 | –0.155 (–0.22 to –0.083) | < 0.001 |
| Male gender | –0.275 | < 0.001 | –00.243 | < 0.001 |
| Exclusive breastfeeding | 0.026 | 0.024 | –00.051 | < 0.001 |
| LAZ at enrollment | –0.197 | < 0.001 | 0.298 | < 0.001 |
| Maternal age | 0.001 | 0.438 | 0.008 | 0.512 |
| Maternal body mass index | 0.170 | < 0.001 | 0.320 | < 0.001 |
| WAMI index | –0.458 | 0.007 | 0.946 | < 0.001 |
| Mother having more than 3 living children | 0.023 | 0.647 | –00.156 | < 0.001 |
| More than 2 people living in a room | 0.233 | < 0.001 | –0.120 | < 0.001 |
| Household ownership of chicken or cattle | 0.147 | 0.011 | –0.078 | < 0.001 |
| AGP level at 24 mo | 0.065 | < 0.001 | –0.111 | < 0.001 |
| Plasma zinc at 24 mo | –0.129 | < 0.001 | 0.083 | < 0.001 |
| Burden of Campylobacter infection | 0.712 | < 0.001 | –0.198 | < 0.001 |
| Burden of ETEC infection | 0.741 | < 0.001 | –0.244 | < 0.001 |
| Burden of EAEC infection | 1.108 | < 0.001 | –0.300 | < 0.001 |
| Burden of typical EPEC infection | 0.737 | 0.002 | –0.360 | < 0.001 |
| Burden of Shigella infection | 0.889 | < 0.001 | –0.419 | < 0.001 |
| Burden of Cryptosporidium infection | 0.865 | 0.005 | –0.320 | < 0.001 |
| Burden of Giardia infection | 0.387 | < 0.001 | –0.367 | < 0.001 |
AGP = α-1-acid glycoprotein; EAEC = enteroaggregative Escherichia coli; EED = environmental enteric dysfunction; EPEC = enteropathogenic Escherichia coli; ETBF = enterotoxigenic Bacteroides fragilis; ETEC = enterotoxigenic Escherichia coli; WAMI = water/sanitation, assets, maternal education, and income; LAZ = length-for-age z-score. The final regression model was adjusted for gender of the participant, exclusive breastfeeding, LAZ at enrollment, maternal age, maternal body mass index, WAMI index, more than two people living per room, mother having more than three living children, household ownership of chicken or cattle, plasma AGP level at 24 months, plasma zinc level at 24 months, and presence of co-pathogens (Campylobacter sp., ETEC, EAEC, typical EPEC, Shigella sp., Cryptosporidium sp., and Giardia sp.) for the overall estimate.
DISCUSSION
Findings from previous studies conducted in the settings of the MAL-ED study have reported that linear growth faltering at 24 months of life was attributed to asymptomatic infections by Shigella sp., EAEC, Campylobacter sp., Giardia sp., Cryptosporidium sp., and tEPEC.40 However, to the best of our knowledge, this is the first study that has aimed to estimate incidence rates of ETBF infections across different geographic locations and establish a possible association between EED and linear growth among children at 24 months of age. Diagnosis of ETBF infection from stool is difficult, with anaerobic stool culture for B. fragilis being delayed by the processing of stool samples, along with the general difficulty of anaerobic microbiology and fecal heterogeneity of B. fragilis strains, whereby both non-enterotoxigenic B. fragilis and ETBF may be detected in the stool samples.43–45 Thus, detection of the bft gene by polymerase chain reaction is recommended for accuracy in the diagnosis of ETBF infection.15
Reports from studies conducted in India, Bangladesh, and Brazil found that the prevalence of ETBF among acute diarrheal cases was between 2% and 4%.46–48 From our analysis, we report a 10.9% overall incidence rate of B. fragilis infection per 100 child-months across all eight study sites, with the highest incidence rate per 100 child-months in Tanzania (19.2%) and the lowest incidence rate per 100 child-months in Peru (3.6%). Findings from a case–control study conducted among children in India show that the prevalence of ETBF in asymptomatic cases was 7.2%.49 Reports from another study conducted in a rural area of Bangladesh show that approximately 16% of all children younger than 24 months of age were infected with ETBF at some time after birth.22 However, all these aforementioned studies were not longitudinal in design and did not involve monthly follow-ups for the assessment of the burden of enteropathogens and did not involve the use of such a sophisticated molecular diagnostic technique such as the TaqMan array cards, as did our study.
Reports involving the risk factors for ETBF are very limited. One study carried out in rural Bangladesh indicated that household ownership of cattle or poultry was a determinant of ETBF infection among children.22 Previous reports indicate that different domestic animals, including lambs and calves, can have ETBF-associated diarrhea.50,51 The results from our study show that the household ownership of chicken or cattle was significantly associated with a 15% higher incidence rate of ETBF infection. This finding is in agreement with reports from previous studies that indicated poultry or domestic cattle could act as reservoirs for ETBF, with ETBF being transmitted to human hosts through animal dung or poultry feces.22 The role of domestic animals in the transmission of enteropathogens to human hosts has been reported in previous studies.52
Additional findings from our study included lack of water access, sanitation, and hygiene (WASH) practices, lack of improved floor material in households, lack of improved drinking water, and lack of improved sanitation being associated with greater incidences of ETBF infection. Such findings were also evidenced in several other studies conducted in MAL-ED settings, where similar protective roles of improved WASH practices were found against infection by other enteropathogens.53,54 Moreover, increased maternal education and female gender were found to exert a protective role against ETBF infections, thus agreeing with reports from concurrent studies done in similar settings.49,54 Although enhanced maternal education may correspond to improved WASH practices and thereby reduce ETBF infections, the role of the female gender in reduced ETBF infections warrants further studies into the role of sex chromosomes in conferring protection against these enteropathogens, including ETBF.
In addition, we report a significant protective association of longer duration of breastfeeding with ETBF infections. Longer duration of breastfeeding is protective against the incidence of infections by other enteropathogens in studies carried out in similar settings.54 We hypothesize that human milk oligosaccharides, along with maternal antibodies and milk glycans, act in reducing infection by enteropathogens by promoting the growth of probiotic microbes in the gut, thus impeding the growth of pathogenic microorganisms.55,56 Also, increased crowding in households (more than two people living in a single room and mother having more than three living children) was found to be associated with the risk of incidence of ETBF infection, which could be explained by an increased fecal–oral transmission of enteropathogens, accentuated by the lack of access to proper sanitation, as evidenced in such settings.
In our study, we report a positive association between the burden of ETBF infection and EED score at 24 months of age. The relevance of an elevated EED score at 24 months of age with the burden of ETBF infection is yet to be elucidated, and there is no reported indication of enteric inflammation being associated with ETBF infection. However, it is well reported that the toxin secreted by ETBF, known as fragilysin, induces intestinal inflammation that activates β-catenin signaling and induces IL-8 secretion in colonic epithelial cells, leading to neutrophil infiltration in the small intestine and T-cell-mediated hyperstimulation of the gut immune system.21,57,58 Thus, persistent ETBF infection may lead to sustained secretion of fragilysin from birth over a period of 24 months, which may lead to continual inflammation of the gut epithelium, leading to a gradual change in the architecture of the small intestine.
Our study findings also demonstrate that the burden of ETBF infection was associated negatively with linear growth (LAZ) at 24 months of age. Although other studies conducted in MAL-ED settings reported that linear growth faltering at 24 months of age was associated with sub-clinical infections by certain other pathogens, none of those studies evaluated enteropathogen burden using the incidence rate of the enteropathogen infections at each successive follow-up over the entire study period.40 The effect size of the association of infection by other malnutrition-associated co-pathogens (Campylobacter, Shigella, ETEC, EAEC, tEPEC, and Giardia) with the outcome variables of EED score and LAZ at 24 months was greater than that of ETBF infection, as indicated in Table 3. Nevertheless, this is the first report to show a statistically significant association between the burden of ETBF infection and growth faltering at 24 months of age, thus warranting greater clinical vigilance in the management of ETBF infections to reduce the burden of enteropathy and linear growth faltering in childhood.
We can suggest that persistent ETBF infection leading to augmented enteric inflammation, as observed in our study, may have resulted in reduced intestinal barrier function and a decline in the surface area of the villi for absorption of nutrients, which—in conjunction with frequent diarrheal episodes during this period—may possibly have resulted in linear growth faltering at 24 months of age.59 Moreover, poor dietary protein quality during this critical period for growth and development, as evidenced in studies in low- to middle-income countries, may have led to a deficiency in circulating amino acids such as tryptophan.60–62 This phenomenon may have resulted in the suppression of intracellular master growth regulation or the mammalian target of rapamycin pathway, ultimately leading to a reduction in the rate of cell growth and proliferation, and linear growth faltering.60,63 However, such dietary data were unavailable for our analysis.
Despite the promising nature of our findings, there are some possible limitations associated with our analysis. First of all, we were unable to establish any conclusive causality between the burden of ETBF infection and EED and linear growth faltering. Thus, a definite biological explanation for our study findings cannot be drawn. In addition, small intestinal endoscopy, the gold standard for diagnosis of EED, was not performed, so we do not have any pertinent data regarding any possible molecular or immunological aberrations in the upper gastrointestinal biopsy specimens of the children in our study. Moreover, were unable to establish a temporal relationship between the ETBF infections and the final study outcomes, which would require structured longitudinal models.
CONCLUSION
The highest and lowest incidence of ETBF infection per 100 child-months was reported in Tanzania and Peru, respectively. Female gender, longer duration of breastfeeding, and improved WASH practices (such as improved drinking water source, improved sanitation, and improved floor material in households), along with enhanced maternal education and less crowding in the households (more than two people living in a single room and mother having more than three living children) were observed to be protective against incidences of ETBF infection. The burden of ETBF infections was observed to have significant associations with EED and subsequent growth faltering at 24 months of age across all study sites. Our study findings illustrate the clinical significance of ETBF infection, highlighting the long-term adverse effects exerted by asymptomatic gut colonization of ETBF in young children, and in turn may lead to greater monitoring and clinical vigilance in the management of ETBF infections during early childhood to avert the consequent long-term sequelae on a global scale.
ACKNOWLEDGMENTS
We acknowledge with gratitude the commitment of The Etiology, Risk Factors, and Interactions of Enteric Infections and Malnutrition and the Consequences for Child Health and Development Project (MAL-ED) as a collaborative project supported by the Bill & Melinda Gates Foundation, the Foundation for the National Institutes of Health, and the National Institutes of Health, Fogarty International Center. We are grateful to MAL-ED staff, parents, and children for their contributions. The International Center for Diarrheal Disease Research, Bangladesh is grateful to the governments of Bangladesh, Canada, Sweden, and the United Kingdom for providing unrestricted core support. We gratefully acknowledges these donors for their support and commitment to the endeavors of the International Center for Diarrheal Disease Research, Bangladesh. A publicly available MAL-ED data set was analyzed in this study. This data are available at: https://clinepidb.org/ce/app/record/dataset/DS_841a9f5259.
REFERENCES
- 1.Black RE et al. 2008. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371: 243–260. [DOI] [PubMed] [Google Scholar]
- 2.Ibrahim MK Zambruni M Melby CL Melby PC , 2017. Impact of childhood malnutrition on host defense and infection. Clin Microbiol Rev 30: 919–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization , 2021. Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition. Geneva, Switzerland: WHO.
- 4.De Onis M Branca F , 2016. Childhood stunting: a global perspective. Matern Child Nutr 12: 12–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olofin I et al. 2013. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS One 8: e64636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keusch GT et al. 2014. Environmental enteric dysfunction: pathogenesis, diagnosis, and clinical consequences. Clin Infect Dis 59: S207–S212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper KM Mutasa M Prendergast AJ Humphrey J Manges AR , 2018. Environmental enteric dysfunction pathways and child stunting: a systematic review. PLoS Negl Trop Dis 12: e0006205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kosek MN et al. 2017. Causal pathways from enteropathogens to environmental enteropathy: findings from the MAL-ED birth cohort study. EBioMedicine 18: 109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.George CM et al. 2018. Enteric infections in young children are associated with environmental enteropathy and impaired growth. Trop Med Int Health 23: 26–33. [DOI] [PubMed] [Google Scholar]
- 10.George CM et al. 2015. Fecal markers of environmental enteropathy are associated with animal exposure and caregiver hygiene in Bangladesh. Am J Trop Med Hyg 93: 269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCormick BJ et al. 2017. Dynamics and trends in fecal biomarkers of gut function in children from 1–24 months in the MAL-ED study. Am J Trop Med Hyg 96: 465–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iqbal NT et al. 2018. Promising biomarkers of environmental enteric dysfunction: a prospective cohort study in Pakistani children. Sci Rep 8: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fahim SM et al. 2018. Association of fecal markers of environmental enteric dysfunction with zinc and iron status among children at first two years of life in Bangladesh. Am J Trop Med Hyg 99: 489–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lassmann B Gustafson DR Wood CM Rosenblatt JE , 2007. Reemergence of anaerobic bacteremia. Clin Infect Dis 44: 895–900. [DOI] [PubMed] [Google Scholar]
- 15.Sears CL , 2009. Enterotoxigenic Bacteroides fragilis: a rogue among symbiotes. Clin Microbiol Rev 22: 349–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sack RB Albert MJ Alam K Neogi P Akbar M , 1994. Isolation of enterotoxigenic Bacteroides fragilis from Bangladeshi children with diarrhea: a controlled study. J Clin Microbiol 32: 960–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sears CL , 2001. The toxins of Bacteroides fragilis . Toxicon 39: 1737–1746. [DOI] [PubMed] [Google Scholar]
- 18.Obiso RJ Jr Azghani AO Wilkins TD , 1997. The Bacteroides fragilis toxin fragilysin disrupts the paracellular barrier of epithelial cells. Infect Immunol 65: 1431–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prindiville TP Sheikh RA Cohen SH Tang YJ Cantrell MC Silva J Jr , 2000. Bacteroides fragilis enterotoxin gene sequences in patients with inflammatory bowel disease. Emerg Infect Dis 6: 171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bressane MA Durigon LE Avila-Campos MJ , 2001. Prevalence of the Bacteroides fragilis group and enterotoxigenic Bacteroides fragilis in immunodeficient children. Anaerobe 7: 277–282. [Google Scholar]
- 21.Sears CL et al. 2008. Association of enterotoxigenic Bacteroides fragilis infection with inflammatory diarrhea. Clin Infect Dis 47: 797–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pathela P et al. 2005. Enterotoxigenic Bacteroides fragilis–associated diarrhea in children 0–2 years of age in rural Bangladesh. J Infect Dis 191: 1245–1252. [DOI] [PubMed] [Google Scholar]
- 23. Alouf JE, 2015. Bacterial protein toxins. Bacterial Toxins 1: 361–396. [Google Scholar]
- 24.Basset C Holton J Bazeos A Vaira D Bloom S , 2004. Are Helicobacter species and enterotoxigenic Bacteroides fragilis involved in inflammatory bowel disease? Dig Dis Sci 49: 1425–1432. [DOI] [PubMed] [Google Scholar]
- 25. The MAL-ED Network Investigators, 2014. The MAL-ED study: a multinational and multidisciplinary approach to understand the relationship between enteric pathogens, malnutrition, gut physiology, physical growth, cognitive development, and immune responses in infants and children up to 2 years of age in resource-poor environments. Clin Infect Dis 59: S193–S206. [DOI] [PubMed] [Google Scholar]
- 26.Onis Md Onyango AW Borghi E Siyam A Nishida C Siekmann J , 2007. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85: 660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richard SA Barrett LJ Guerrant RL Checkley W Miller MA , 2014. Disease surveillance methods used in the 8-site MAL-ED cohort study. Clin Infect Dis 59: S220–S224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Das R et al. , 2021. Evaluating association of vaccine response to low serum zinc and vitamin D levels in children of a birth cohort study in Dhaka. Vaccine 39: 59–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Das S Alam MA Mahfuz M El Arifeen S Ahmed T , 2019. Relative contributions of the correlates of stunting in explaining the mean length-for-age z-score difference between 24-month-old stunted and non-stunted children living in a slum of Dhaka, Bangladesh: results from a decomposition analysis. BMJ Open 9: e025439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. WHO/UNICEF Joint Water Supply, Sanitation Monitoring Programme, 2014. Progress on Drinking Water and Sanitation: 2014 Update. Geneva, Switzerland: World Health Organization.
- 31.Amour C et al. 2016. Epidemiology and impact of Campylobacter infection in children in 8 low-resource settings: results from the MAL-ED study. Clin Infect Dis 63: 1171–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogawski ET et al. , 2018. Use of quantitative molecular diagnostic methods to investigate the effect of enteropathogen infections on linear growth in children in low-resource settings: longitudinal analysis of results from the MAL-ED cohort study. Lancet Glob Health 6: e1319–e1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Houpt E et al. 2014. Microbiologic methods utilized in the MAL-ED cohort study. Clin Infect Dis 59: S225–S232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Benoist B Darnton-Hill I Davidsson L Fontaine O Hotz C , 2007. Conclusions of the joint WHO/UNICEF/IAEA/IZiNCG interagency meeting on zinc status indicators. Food Nutr Bull 28: S480–S484. [DOI] [PubMed] [Google Scholar]
- 35.Helrich K , 1990. AOAC official methods of analysis: vitamin C (ascorbic acid). Assoc Off Anal Chemists 2: 1058–1059. [Google Scholar]
- 36.Gannon BM Glesby MJ Finkelstein JL Raj T Erickson D Mehta S , 2019. A point-of-care assay for alpha-1-acid glycoprotein as a diagnostic tool for rapid, mobile-based determination of inflammation. Curr Res Biotechnol 1: 41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kosek M et al. 2013. Fecal markers of intestinal inflammation and permeability associated with the subsequent acquisition of linear growth deficits in infants. Am J Trop Med Hyg 88: 390–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arndt MB et al. 2016. Fecal markers of environmental enteropathy and subsequent growth in Bangladeshi children. Am J Trop Med Hyg 95: 694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu J et al. 2014. Development and assessment of molecular diagnostic tests for 15 enteropathogens causing childhood diarrhoea: a multicentre study. Lancet Infect Dis 14: 716–724. [DOI] [PubMed] [Google Scholar]
- 40.Rogawski ET et al. 2018. Use of quantitative molecular diagnostic methods to investigate the effect of enteropathogen infections on linear growth in children in low-resource settings: longitudinal analysis of results from the MAL-ED cohort study. Lancet Glob Health 6: e1319–e1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Houpt E et al. , 2014. Microbiologic methods utilized in the MAL-ED cohort study. Clin Infect Dis 59: S225–S232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanin KI et al. 2018. Micronutrient adequacy is poor, but not associated with stunting between 12– 24 months of age: a cohort study findings from a slum area of Bangladesh. PLoS One 13: e0195072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sack RB et al. 1992. Enterotoxigenic Bacteroides fragilis: epidemiologic studies of its role as a human diarrhoeal pathogen. J Diarrhoeal Dis Res 10: 4–9. [PubMed] [Google Scholar]
- 44.Sharma N Chaudhry R , 2006. Rapid detection of enterotoxigenic Bacteroides fragilis in diarrhoeal faecal samples. Indian J Med Res 124: 575. [PubMed] [Google Scholar]
- 45.Cohen SH Shetab R Tang-Feldman YJ Sarma P Silva J Jr Prindiville TP , 2006. Prevalence of enterotoxigenic Bacteroides fragilis in hospital-acquired diarrhea. Diagn Microbiol Infect Dis 55: 251–254. [DOI] [PubMed] [Google Scholar]
- 46.Niyogi S Dutta P Mitra U Pal D , 1997. Association of enterotoxigenic Bacteroides fragilis with childhood diarrhoea. Indian J Med Res 105: 167–169. [PubMed] [Google Scholar]
- 47.Albert MJ Faruque A Faruque S Sack R Mahalanabis D , 1999. Case–control study of enteropathogens associated with childhood diarrhea in Dhaka, Bangladesh. J Clin Microbiol 37: 3458–3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Krzyzanowsky F Avila-Campos MJ , 2003. Detection of non-enterotoxigenic and enterotoxigenic Bacteroides fragilis in stool samples from children in São Paulo, Brazil. Rev Inst Med Trop São Paulo 45: 225–227. [DOI] [PubMed] [Google Scholar]
- 49.Ramamurthy D et al. 2013. Case–control study on the role of enterotoxigenic Bacteroides fragilis as a cause of diarrhea among children in Kolkata, India. PLoS One 8: e60622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Myers L Shoop D Byars T , 1987. Diarrhea associated with enterotoxigenic Bacteroides fragilis in foals. Am J Vet Res 48: 1565–1567. [PubMed] [Google Scholar]
- 51.Border M Firehammer B Shoop D Myers L , 1985. Isolation of Bacteroides fragilis from the feces of diarrheic calves and lambs. J Clin Microbiol 21: 472–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fuhrmeister ER et al. 2019. Predictors of enteric pathogens in the domestic environment from human and animal sources in rural Bangladesh. Environ Sci Technol 53: 10023–10033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rogawski ET et al. 2017. Epidemiology of enteroaggregative Escherichia coli infections and associated outcomes in the MAL-ED birth cohort. PLoS Negl Trop Dis 11: e0005798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haque MA et al. 2019. Determinants of Campylobacter infection and association with growth and enteric inflammation in children under 2 years of age in low-resource settings. Sci Rep 9: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Plaza-Díaz J Fontana L Gil A , 2018. Human milk oligosaccharides and immune system development. Nutrients 10: 1038–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Atyeo C Alter G , 2021. The multifaceted roles of breast milk antibodies. Cell 184: 1486–1499. [DOI] [PubMed] [Google Scholar]
- 57.Wu S Lim K-C Huang J Saidi RF Sears CL , 1998. Bacteroides fragilis enterotoxin cleaves the zonula adherens protein, E-cadherin. Proc Natl Acad Sci USA 95: 14979–14984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu S Powell J Mathioudakis N Kane S Fernandez E Sears CL , 2004. Bacteroides fragilis enterotoxin induces intestinal epithelial cell secretion of interleukin-8 through mitogen-activated protein kinases and a tyrosine kinase-regulated nuclear factor-κB pathway. Infect Immunol 72: 5832–5839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Budge S Parker AH Hutchings PT Garbutt C , 2019. Environmental enteric dysfunction and child stunting. Nutr Rev 77: 240–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Semba RD et al. 2016. Child stunting is associated with low circulating essential amino acids. EBioMedicine 6: 246–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nuss ET Tanumihardjo SA , 2011. Quality protein maize for Africa: closing the protein inadequacy gap in vulnerable populations. Adv Nutr 2: 217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gazi MA et al. 2020. Plasma kynurenine to tryptophan ratio is negatively associated with linear growth of children living in a slum of Bangladesh: results from a community-based intervention study. Am J Trop Med Hyg 104: 766–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Semba RD et al. 2016. Perspective: the potential role of essential amino acids and the mechanistic target of rapamycin complex 1 (mTORC1) pathway in the pathogenesis of child stunting. Adv Nutr 7: 853–865. [DOI] [PMC free article] [PubMed] [Google Scholar]