Abstract
Background
Dental trauma is common especially in children and young adults. One group of dento‐alveolar injuries is classified as luxation. This group includes a subgroup of severe injuries where the tooth is displaced from its original position. These injuries are classified further by the direction in which the tooth has been displaced, namely: intrusion, extrusion and lateral luxation.
Objectives
To evaluate the effects of a range of interventions for treating displaced luxated permanent front teeth.
Search methods
Search strategies were developed for MEDLINE via OVID and revised appropriately for the following databases: Cochrane Oral Health Group's Trials Register (to 20 August 2012), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 8), MEDLINE via OVID (1966 to August 2012), EMBASE via Elsevier (1974 to August 2012), and LILACS via BIREME (1982 to August 2012). Dissertations, Theses and Abstracts were searched as were reference lists from articles. There were no language restrictions.
Selection criteria
Randomised or quasi‐randomised controlled trials of treatment interventions for displaced luxated permanent front teeth. Included trials had to have a minimum follow‐up period of 12 months.
Data collection and analysis
Two review authors independently and in duplicate assessed the eligibility of all reports identified in the searches. Authors were contacted for additional information where required.
Main results
No randomised or quasi‐randomised controlled trials were found.
Authors' conclusions
We found no randomised or quasi‐randomised trials of interventions to treat displaced luxated permanent front teeth. Current clinical guidelines are based on available information from case series studies and expert opinions. Randomised controlled trials in this area of dental trauma are required to robustly identify the benefits of different treatment strategies.
Keywords: Child, Humans, Young Adult, Incisor, Incisor/injuries, Tooth Avulsion, Tooth Avulsion/therapy
Plain language summary
Interventions for treating traumatised permanent front teeth: luxated (dislodged) front teeth
Traumatic injuries to upper front teeth in children and young adults are common. The Cochrane Oral Health Group conducted this review to look at interventions to treat the front permanent (adult) tooth or teeth when they have been displaced from their original position following injury. This review does not include teeth that have been completely knocked out (avulsion).
The latest search of relevant studies was carried out on 20th August 2012.
There are various causes of this kind of traumatic injury including falls, blows, accidents and assaults. Studies have shown that the majority of cases involve boys and young men (60% to 70%).
There are three main kinds of displacement.
‐ Lateral, where the tooth has been forced sideways (either back or forwards) in the socket and is immobile. ‐ Extrusion, where the tooth has become loosened and begins to come out of the socket. ‐ Intrusion, where the tooth has been forced into the bone of the jaw.
After the injury, the teeth may be repositioned into their original position or allowed to spontaneously return to their original position (appropriate for some types of intrusion injury). Repositioning can be undertaken either manually by the dentist or using orthodontic braces. Once the tooth is returned to its original position, splinting may be used to maintain its position. A large variety of splinting techniques have been reported in the literature. An ideal splint should be passive (i.e. it should not cause the tooth to move away from its original position), allow physiological movement (e.g. allow very minor movements of the tooth while maintaining its original position) and be simple to handle during application and removal. From the patient's perspective, the splint should not interfere with biting, cleaning or speech. The length of time the splint should stay in position depends on the injury, the mobility of the tooth and the tissues affected. The injured tooth or teeth will then require long term (at least 12 months) monitoring to assess healing, particularly of the gum and soft tissues around the tooth and crucially the pulp inside it which keeps the tooth alive. Where indicated (i.e. if the pulp inside the tooth dies), further treatment may be required such as root canal treatment.
This Cochrane review investigated what treatments are beneficial for these kinds of injuries including:
‐ the role of antibiotics and their different types; ‐ the role of splints, their differing types, and the optimum length of time for their use; and ‐ the role of repositioning techniques (e.g. the use of orthodontic braces or surgery).
Out of 548 studies identified in the search, no studies were found which met the inclusion criteria. There is therefore no high quality evidence available on which to base an assessment of interventions to treat these injuries. Current treatment guidelines are based on studies with a greater risk of bias using study designs such as case series, animal studies and laboratory‐based cellular studies. High quality studies are therefore urgently needed.
Background
Description of the condition
Dental trauma is common (Chadwick 2006; Hamilton 1997) and occurs mainly in children and young adults (Petersson 1997). One group of injuries is classified as luxations. This group encompasses a range of injuries; this review will be limited to injuries where the tooth is displaced from its original position. These injuries are further subclassified into: intrusion, extrusion and lateral luxations according to the direction of displacement. Where the tooth is completely knocked out of the socket and the mouth, this is called an avulsion and is discussed in a different Cochrane review (Day 2010).
The definition of each injury is defined as.
A lateral luxation injury produces a displacement of the tooth in a direction other than an axial direction. It occurs in conjunction with comminution or fracture of the alveolar socket, and renders the tooth immobile (Andreasen 1985b).
An extrusive luxation (or extrusion) is characterised by partial extrusive displacement of a tooth from its socket. Clinically, the tooth will be excessively mobile and radiographically the injured tooth will appear elongated. Further there will be a widening of the periodontal ligament space and an intact alveolar bone (Andreasen 2001). Finally where the tooth is luxated palatally or buccally a diagnosis of extrusive luxation is made if the tooth is mobile.
An intrusive luxation (or intrusion) is the apical displacement of the tooth into the alveolar bone with comminution or fracture of the alveolar socket (Welbury 2002).
There are multiple causes for luxation injuries (e.g. falls, blows, accidents, assaults). All these involve a sudden collision against a hard object (Andreasen 1972; Crona‐Larsson 1989). As with all types of trauma, males are more likely to be involved (60% to 70%) (Andreasen 1970; Caldas 2001; Moura 1994; Nicolau 2001; Rocha 2001) and the central maxillary incisor is the most frequent tooth involved (Andreasen 1985b).
Although the incidence of luxations is low compared to fractures of the tooth, the consequences are frequently more severe. Treatment and follow‐up care can require multiple hours in the dental chair for the patient (Glendor 2000) and ultimately the tooth may be lost especially following intrusive injuries. Following a luxation injury the following tissues are injured: the periodontal ligament surrounding the tooth, the alveolar (bony) socket and the vascular and nervous supply to the tooth. Treatment can be provided for all these tissues and can be split into two phases.
Initial or emergency care: administered to improve aesthetics and function. Teeth may be repositioned, either surgically or utilising orthodontic forces, into their original position or in some cases allowed to re‐erupt. Following repositioning the tooth frequently requires holding in the correct position e.g. splinting. A large variety of fixation or stabilisation techniques have been reported in the literature. An ideal splint should be passive (e.g. cause no orthodontic tooth movement), allow physiological movement of the injured tooth and be easy to apply and remove. From the patient's perspective, the splint should not interfere with the occlusion, oral hygiene or speech. Duration of splinting can depend on the injury, mobility of the tooth and the tissues affected.
Medium and long term follow‐up is aimed at monitoring the type of healing seen in these different tissues; treatment is provided to prevent further complications.
Monitoring for at least 12 months is required to assess pulpal healing. The evaluation of pulpal health requires: vitality testing, radiographs, evaluation of any symptoms and clinical monitoring for changes in colour and the development of a sinus or swelling or tenderness to pressure (Andreasen 1985; Andreasen 1985b; Andreasen 1989b).
The damage caused to the periodontal tissues can lead to different types of resorption of the root surface. These include repair‐related resorption, infection‐related resorption or replacement resorption. Treatment is provided with the aim of preventing infection‐related resorption. Where replacement resorption occurs, ultimately the tooth will be lost over a period of years depending the speed of bone turnover and age of the patient (Andersson 1989; Barrett 1997). For some injuries especially intrusion there can be long term loss of supporting alveolar bone with associated gingival recession.
Description of the intervention
Treatment of permanent teeth extruded or dislocated laterally, when seen immediately after the trauma, consists of careful manual repositioning through firm finger pressure, often necessitating a regional anaesthetic block. The optimal treatment for intruded teeth has not yet been determined (Al‐Badri 2002; Andreasen 2006b; Humphrey 2003; Jacobsen 1986; Kinirons 1991; Tsilingaridis 2012; Vinckier 1989; Wigen 2008). Guidelines (Albadri 2010; Diangelis 2012) describe three potential interventions ‐ no treatment and allow for spontaneous eruption or surgical repositioning or orthodontic repositioning.
Where surgical repositioning is undertaken, the tooth will require splinting in order to maintain its correct position. An atraumatic physiological splint is required (Andreasen 2001; Barrett 1997; Drago 1991; Trope 2002) to stabilize the tooth for sufficient time to ensure that there is no further injury and allow repair of the injured tissues. The splint should not interfere with the occlusion or function, be atraumatic to the adjacent soft tissues, allow adequate oral hygiene (Trope 2002; von Arx 2001b) and may be retained in situ for 1 to 6 weeks depending on the severity of the injury.
Various root canal medicaments have been used to ensure disinfection of the root canal prior to definitive obturation. These include calcium hydroxide and antibiotic‐steroid combination pastes. Currently there is uncertainty over the supplemental use of systemic antibiotics and the decision to prescribe them is left to the individual circumstances (Diangelis 2012).
How the intervention might work
Interventions are aimed at minimising the chance of infection and allowing injured tissues to heal. In some cases, such as teeth with complete root development and intrusion injuries, elective pulp extirpation is recommended to prevent infection‐related resorption. Where there is a chance of pulpal healing, such as lateral luxation or extrusive luxations or intruded teeth with immature root development, careful monitoring of pulpal healing is required.
Healing of the periodontal tissues can take place by either repair‐related resorption or ankylosis.
Why it is important to do this review
The effects of luxation injuries and their subsequent healing have a significant long term consequence for the individual and family involved, as well as the costs incurred by healthcare funders.
Objectives
To evaluate the effects of a range of interventions for treating displaced luxated permanent front teeth.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials or quasi‐randomised controlled trials that included a minimum follow‐up period of 12 months were eligible for inclusion.
Types of participants
Participants with a history of dental trauma and a diagnosis of luxations of permanent front teeth (attending a dental clinic (for diagnosis, treatment or observation)).
Only subjects with luxated anterior permanent teeth were included.
Any studies which involved patients with specific medical histories or disabilities would require further correspondence with the authors if this is not discussed in original paper. For example cardiac patients who are at risk of infective endocarditis or patients with significant learning difficulties may necessitate clinicians to provide a specific treatment and therefore may make them ineligible for a trial. Correspondence would therefore ask about how many patients fitted into these categories and how the trial dealt with them.
Types of interventions
All interventions for treating luxated teeth were considered, this included.
Types of antibiotics: the effect of using no antibiotics, a placebo or different types of antibiotics.
Types and duration of fixation: the effect of using no splint or different types of splints and their duration.
Types of dental repositioning: to compare spontaneous re‐eruption, orthodontic repositioning or surgical repositioning.
Types of root canal medicaments: this was compared with no medicaments, placebo and different types of medicaments.
Types of outcome measures
Primary outcomes
Pulp survival.
Tooth survival.
Function: eating, speech.
Pain.
Periodontal ligament healing.
Mobility.
Secondary outcomes
Cost: financial, clinic cost, dentist time, number of visits, time in chair, patient's time off work/school, post‐operative complications.
Ease of cleaning of splint, aesthetics, comfort, patient satisfaction.
Quality of life.
Search methods for identification of studies
Electronic searches
The following were searched for relevant trials:
The Cochrane Oral Health Group's Trials Register (Appendix 1);
the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 8) (Appendix 2);
MEDLINE via OVID (1966 to August 2012) (Appendix 3);
EMBASE via Elsevier (1974 to August 2012) (Appendix 4);
LILACS via BIREME (1982 to August 2012) (Appendix 5);
Dissertation, Theses and Abstracts (1981 to August 2012) (Appendix 6).
For the identification of studies included or considered for this review, detailed search strategies were developed for each database searched. These were based on the search strategy developed for MEDLINE but revised appropriately for each database. The search strategy for MEDLINE was combined with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as detailed in Box 6.4.c, Chapter 6, of the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (updated March 2011) (Higgins 2011).
The subject search used a combination of controlled vocabulary and free text terms based on the search strategy for searching MEDLINE via OVID presented in Appendix 3, and revised appropriately for each database.
Language
Studies in all languages were considered for translation.
Cross‐checking references
Reference lists of identified studies were cross‐checked for additional studies.
Unpublished studies
Authors of relevant studies were written to in order to obtain further information about ongoing or unpublished randomised controlled trials. Manufacturers of different splinting materials or root canal materials were written to. Unfortunately no replies were received.
Data collection and analysis
Selection of studies
Two review authors (Flavia Belmonte (FMB) and Cristiane Rufino Macedo (CRM)) independently and in duplicate assessed the titles and abstracts (when available) of all reports identified by the search strategy as being of potential relevance to the review. No blinding with respect to institutional affiliations or site of publication was undertaken. The full report was obtained for all studies appearing to meet the inclusion criteria or in instances where there was insufficient information from the title, keywords and abstract to make a clear decision. All studies were assessed independently for eligibility by both review authors. Instances of disagreement in the study selection process were referred to another member (Virginia Trevisani (VFT)) of the review team and ultimately resolved by discussion among all review team members.
Data extraction and management
In future updates if studies are eligible for inclusion, data will be extracted by two review authors (FMB, CRM) independently using specially designed data extraction forms according to the checklist table 7.3.a of the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (Higgins 2011). The following data will be collected from each included study.
Study eligibility.
Study methods: design, duration, randomisation procedure, blinding, allocation concealment.
Study participants: inclusion and exclusion criteria, diagnosis, sample size, setting, country, age of participants, gender.
Interventions: type of splint, length of splinting, other treatment, provider of intervention (training of provider in delivery of intervention, continuity of carer), details of the control group.
Outcomes: type of outcome, measurement tool (including validity), timing and frequency of assessment.
Results.
Conclusions: as stated by the study authors.
Miscellaneous: limitations of study, funding source and other remarks.
Characteristics of the trial participants, interventions and outcomes for the included trials will be presented in the included studies table. Authors will be contacted for clarification or for further information.
Assessment of risk of bias in included studies
In future updates if studies are eligible for inclusion, bias will be assessed independently and in duplicate using the tools described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (Higgins 2011). The domains investigated will be:
sequence generation;
allocation concealment;
blinding of participants
blinding of assessors;
incomplete outcome data addressed;
selective outcome reporting; and
other sources of bias.
A 'Risk of bias' table would be completed for each domain in each included study. Possible judgements would be 'Low risk of bias', 'High risk of bias' or 'Unclear risk of bias'. Results would be presented graphically by study and by domain over all studies.
Measures of treatment effect
In future updates if studies are eligible for inclusion, they will be analysed by FMB and CRM according to the criteria described in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (Higgins 2011). For dichotomous data risk ratios will be applied and for continuous data the mean difference or standardized mean difference will be used when different methods for measuring effects are used. Estimate of effects will be presented with 95% confidence intervals.
Unit of analysis issues
In future updates if studies are eligible for inclusion, participants will be the primary unit of analysis. Where participants have multiple teeth injured then full reporting of the outcomes for each tooth will be expected. Only when multi‐level modelling has been undertaken to identify the effect of the intervention at both patient and tooth level can the data be fully explored. Otherwise secondary analysis will be undertaken which examines the best and worst outcomes at a tooth level for each intervention.
Multi‐arm studies may be considered for inclusion in the review and, in accordance with recommendations in the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (Higgins 2011), all relevant experimental groups will be combined and considered as a single group and compared to a combined group of all control groups, if present.
Given the nature of the conditions and interventions under review, it is highly unlikely cluster trials will be a likely study design.
Dealing with missing data
In future updates if studies are eligible for inclusion, the authors will be contacted to clarify missing or confusing data. Where studies are identified, intention‐to‐treat analysis will be carried out where subjects are lost to follow‐up.
Assessment of heterogeneity
In future updates if studies are eligible for inclusion, statistical heterogeneity will be assessed using a Chi2 test and I2 statistic.
Assessment of reporting biases
In future updates if sufficient number of studies (greater than 10) are eligible for inclusion, a funnel plot (Egger 1997) will be used to assess publication bias.
Data synthesis
In future updates if studies are eligible for inclusion, dichotomous data will be reported using risk ratios and 95% confidence intervals (CI). Continuous data will be reported by calculating the mean differences and 95% CI. If continuous data are measured with different instruments (different and not interchangeable units of measure) the standardized mean difference will be used. For all statistical methods when pooling data, 95% CI will be reported. A random‐effects meta‐analysis will be performed if more than three studies are identified. In case of only two studies identified, a fixed‐effect model meta‐analysis will be performed.
Subgroup analysis and investigation of heterogeneity
In future updates if sufficient studies (greater than 10) are eligible, subgroup analyses according to age, gender and length of the follow‐up will be performed.
Sensitivity analysis
In future updates if sufficient studies are eligible for inclusion, sensitivity analyses to assess the robustness of the results, excluding the studies in which a high risk of bias is detected, will be performed. Furthermore, sensitivity analyses to examine the effect of randomised or quasi‐randomised trials will be undertaken.
Presentation of main results
In future updates if sufficient studies are eligible for inclusion, the main findings of the review will be presented in a 'Summary of findings' table according to Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (Higgins 2011). The quality of evidence will be graded using the GRADE system. The table will provide information concerning the main outcomes, number of participants, magnitude of effect of the examined interventions and the quality of the evidence.
Results
Description of studies
The search strategy retrieved 679 records (50 Cochrane Oral Health Group's Trials Register, 113 CENTRAL, 420 MEDLINE, 66 EMBASE and 30 LILACS) and one additional report was obtained through another source. This number was reduced to 548 potentially eligible studies once duplicated publications were removed. All titles and abstracts were assessed by two review authors (Flavia Belmonte (FBM) and Cristiane Rufino Macedo (CRM)) and 542 were excluded. Six studies were identified as potentially meeting the inclusion criteria. They were excluded for the following reasons: case series (Caprioglio 1990; Ebeleseder 2000; Qin 2002), studies of splints on uninjured teeth (Filippi 2002; von Arx 2001) and short follow‐up (Liang 2008). The study flow diagram (Figure 1) provides further details of the literature search.
1.
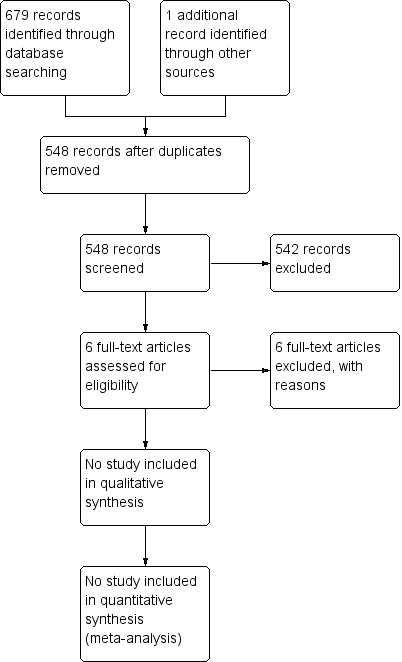
Study flow diagram.
Risk of bias in included studies
No study was included in this review.
Effects of interventions
No study was included in this review.
Discussion
The search strategy identified three case series studies describing treatment interventions for displaced luxated permanent front teeth. The review was unable to identify any randomised controlled trials in this subject area.
One of the main implications resulting from this systematic review is the need for further research to investigate the effects of different treatment interventions for displaced luxated permanent front teeth. Researchers designing studies in the area of dento‐alveolar trauma should pay particular consideration to a number of complicating factors:
the rarity of the different types of displaced luxation injury;
the variability of emergency presentation of patients following a displaced luxation injury to a permanent front tooth and the different dental and/or medical specialities who may be involved in the acute management of these injuries;
the failure of patients to present with sufficient speed following injury to the treatment centre while all treatment options are still appropriate;
the ethical problem of obtaining informed consent in an emergency situation.
This list of problems does not mean that good quality research is impossible for displaced luxated permanent front teeth. It does, however, require good planning and feasibility studies to ensure these complicating factors can be accommodated. Furthermore good quality randomised controlled trials require the appropriate financial sponsorship to maintain the enthusiasm of centres to recruit and retain sufficient patients to ensure the study reaches its power calculation and therefore that a valid conclusion can be drawn from the results.
Authors' conclusions
Implications for practice.
We found no randomised or quasi‐randomised trials of interventions to treat displaced luxated permanent front teeth. Current clinical guidelines are based on available information from case series studies and expert opinions.
Implications for research.
The relative effectiveness and safety of different treatment interventions for displaced luxated anterior permanent teeth has not been evaluated by robust clinical research. Conducting randomised controlled trials in this area of dento‐alveolar trauma needs to overcome a number of specific difficulties. It does not however mean that such trials are impossible. Researchers should collaborate to conduct well designed clinical trials to address important primary outcomes from both a clinical and patient perspective.
What's new
| Date | Event | Description |
|---|---|---|
| 11 March 2014 | Review declared as stable | This empty review will not be updated until a substantial body of evidence on the topic becomes available. If trials are conducted and found eligible for inclusion in the future, the review would then be updated accordingly. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 4, 2013
| Date | Event | Description |
|---|---|---|
| 3 September 2008 | Amended | Converted to new review format. |
Acknowledgements
The review authors would like to thank Luisa Fernandez Mauleffinch (Managing Editor), Anne Littlewood (Trials Search Co‐ordinator), Philip Riley (Deputy Managing Editor), and the Cochrane Oral Health Group editorial team (Professors Helen Worthington and Jan Clarkson).
Appendices
Appendix 1. Cochrane Oral Health Group's Trials Register search strategy
#1 (splint* or reposition* or realign* or "re‐erupt*" or "root canal" or endodontic* or pulpectom* or pulpotomy or "pulp devitali*" or antibiotic or antibacterial or penicillin or amoxicil* or amoxil or BR‐2333 or clamoxyl or clariana or hydroxyampicillin or penamox or polimox or trimox or wymox or erthromycin* or erycette or erymax or "ilotycin t‐stat"):AB
#2 (splint* or reposition* or realign* or "re‐erupt*" or "root canal" or endodontic* or pulpectom* or pulpotomy or "pulp devitali*" or antibiotic or antibacterial or penicillin or amoxicil* or amoxil or BR‐2333 or clamoxyl or clariana or hydroxyampicillin or penamox or polimox or trimox or wymox or erthromycin* or erycette or erymax or "ilotycin t‐stat"):TI
#3 ((intrusi* or extrusi* or lateral or dental or tooth or teeth or incisor* or incisal* or "partial axial" or apical or palat* or buccal*)):TI AND ((injur* or avuls* or trauma* or displac* or dislodg* or luxat*)):TI
#4 ((intrusi* or extrusi* or lateral or dental or tooth or teeth or incisor* or incisal* or "partial axial" or apical or palat* or buccal*)):AB AND ((injur* or avuls* or trauma* or displac* or dislodg* or luxat*)):AB
#5 (#1 or #2)
#6 (#3 or #4)
#7 (#5 and #6)
Appendix 2. CENTRAL search strategy
#1. exp Tooth Injuries/
#2. ((intrusi$ or extrusi$ or lateral or dental or tooth or teeth or incisor$ or incisal or "partial axial" or apical or palat$ or buccal$) adj5 (injur$ or avuls$ or trauma$ or displac$ or dislodg$ or luxat$)).tw.
#3. 1 or 2
#4. exp Periodontal Splints/
#5. periodontal splint$.tw.
#6. exp Splints/
#7. (splint$ or fixat$ or stabili$).tw.
#8. ((bi‐digital or orthodontic or surgical or dental) adj5 (reposition$ or realign)).tw.
#9. dental re‐eruption.tw.
#10. exp "Root Canal Therapy"/
#11. (("root canal" or endodontic) adj5 (treatment or therap$ or medicament$ or prepar$ or obturat$)).tw.
#12. exp Pulpectomy/
#13. exp Pulpotomy/
#14. exp dental pulp devitalization/
#15. (pulpectomy or pulpotomy or pulp devitali$).tw.
#16. exp Anti‐Bacterial Agents/
#17. anti?bacterial agent$.tw.
#18. anti?bacterial$.tw.
#19. anti?biotic$.tw.
#20. exp Penicillins/
#21. (penicillin$ or amoxicil$ or amoxil or actimoxi or BR‐2333 or clamoxyl or clariana or hydroxyampicillin or penamox or polimox or trimox or wymox or erythromycin$ or erycette or erymax or llotycin T‐Stat).tw.
#22. or/4‐21
#23. 3 and 22
Appendix 3. MEDLINE (OVID) search strategy
#1. exp Tooth Injuries/
#2. ((intrusi$ or extrusi$ or lateral or dental or tooth or teeth or incisor$ or incisal or "partial axial" or apical or palat$ or buccal$) adj5 (injur$ or avuls$ or trauma$ or displac$ or dislodg$ or luxat$)).tw.
#3. 1 or 2
#4. exp Periodontal Splints/
#5. periodontal splint$.tw.
#6. exp Splints/
#7. (splint$ or fixat$ or stabili$).tw.
#8. ((bi‐digital or orthodontic or surgical or dental) adj5 (reposition$ or realign)).tw.
#9. dental re‐eruption.tw.
#10. exp "Root Canal Therapy"/
#11. (("root canal" or endodontic) adj5 (treatment or therap$ or medicament$ or prepar$ or obturat$)).tw.
#12. exp Pulpectomy/
#13. exp Pulpotomy/
#14. exp dental pulp devitalization/
#15. (pulpectomy or pulpotomy or pulp devitali$).tw.
#16. exp Anti‐Bacterial Agents/
#17. anti?bacterial agent$.tw.
#18. anti?bacterial$.tw.
#19. anti?biotic$.tw.
#20. exp Penicillins/
#21. (penicillin$ or amoxicil$ or amoxil or actimoxi or BR‐2333 or clamoxyl or clariana or hydroxyampicillin or penamox or polimox or trimox or wymox or erythromycin$ or erycette or erymax or llotycin T‐Stat).tw.
#22. or/4‐21
#23. 3 and 22
Appendix 4. EMBASE (Elsevier) search strategy
#1. 'tooth injury'/exp
#2. ((intrusi* OR extrusi* OR lateral OR dental OR tooth OR teeth OR incisior* OR incisal OR 'partial axial' OR apical OR palat* OR buccal*) NEAR/5 (injur* OR avuls* OR trauma OR displac* OR dislodg* OR luxat*)):ab,
#3. 1 OR 2
#4. 'periodontic device'/exp
#5. (periodont* NEAR/1 (device* OR splint*)):ab,ti
#6. 'splint'/exp
#7. splint*:ab,ti OR fixat*:ab,ti OR stabili*:ab,ti
#8. (('bi digital' OR orthodontic OR surgical OR dental) NEAR/5 (reposition* OR realign)):ab,ti
#9. 'root canal therapy':ab,ti
#10. (('root canal' OR endodontic) NEAR/5 (treatment OR therap* OR medicament* OR prepar* OR obturat*)):ab,ti
#11. pulpectomy:ab,ti OR pulpotomy:ab,ti OR 'pulp devitalization':ab,ti OR 'pulp desvitalisation':ab,ti
#12. 'antibiotic agent'/exp
#13. 'antibiotic agent':ab,ti OR antibiotic*:ab,ti
#14. 'penicillin derivative'/exp
#15. penicillin*:ab,ti OR amoxicil*:ab,ti OR amoxil:ab,ti OR actimoxi:ab,ti OR 'br 2333' OR clamoxyl:ab,ti OR clariana:ab,ti OR hydroxyampicillin:ab,ti OR penamox:ab,ti OR polimox:ab,ti OR ortrimox:ab,ti OR orwymox:ab,ti OR erythromycin*:ab,ti OR erycette:ab,ti OR erymax:ab,ti OR llotycin T‐Stat:ab,ti
#16. or/4‐15
#17. 3 and 16
Appendix 5. LILACS (BIREME) search strategy
(((MH:C07.793.850) OR (MH:C26.900) OR (TW:Tooth Injuries) OR (TW:Traumatismos de los Dientes) OR (TW:Traumatismos Dentários)) OR ((TW:intrusi$) OR (TW:extrusi$) OR (TW:lateral) OR (TW:dental) OR (TW:tooth) OR (TW:teeth) OR (TW:incisor$) OR (TW:incisal) OR (TW:partial axial) OR (TW:apical) OR (TW:palat$) OR (TW:buccal$) AND (TW:injur$) OR (TW:avuls$) OR (TW:trauma$) OR (TW:displac$) OR (TW:dislodg$) OR (TW:luxat$))) AND ((MH:E06.721.721.680) OR (TW:Periodontal Splints) OR (TW:Ferulas Periodontales) OR (TW:Contenções Periodontais) OR (TW:Splints, Periodontal) OR (TW:periodontal splint$) OR (MH:E07.858.690.650.845) OR (MH:E07.858.442.660.845) OR (TW:Splints) OR (TW:Ferulas) OR (TW:Contenções) OR (TW:splint$) OR (TW:fixat$) OR (TW:stabili$)) OR ((TW:bi‐digital) OR (TW:orthodontic) OR (TW:surgical) OR (TW:dental) AND (TW:reposition$) OR (TW:realign)) OR (TW:dental re‐eruption) OR (MH:E06.397.778) OR (TW:Root Canal Therapy) OR (TW:Tratamiento del Conducto Radicular) OR (TW:Tratamento do Canal Radicular) OR ((TW:root canal) OR (TW:endodontic) AND (TW:treatment) OR (TW:therap$) OR (TW:medicament$) OR (TW:prepar$) OR (TW:obturat$)) OR ((MH:E06.397.633) OR (TW:Pulpectomy) OR (TW:Pulpectomía) OR (TW:Pulpectomia) OR (MH:E06.397.695) OR (TW:Pulpotomy) OR (TW:Pulpotomía) OR (TW:Pulpotomia) OR (MH:E06.397.778.377) OR (TW:Dental pulp devitalization) OR (TW:Desvitalización de la Pulpa Dental) OR (TW:Desvitalização da Polpa Dentária) OR (TW:Pulpectomy) OR (TW:Pulpotomy) OR (TW:pulp devitali$) OR (MH:D27.505.954.122.085) OR (MH:SP4.011.102.088) OR (MH:VS2.002.001.012) OR (TW:Anti‐Bacterial Agents) OR (TW:Antibacterianos) OR (TW:Antibiotics) OR (TW:antibacterial agent$) OR (TW:anti‐bacterial agent$) OR (TW:anti bacterial$) OR (TW:antibiotic$) OR (MH:D02.065.589.099.750) OR (MH:D02.886.108.750) OR (MH:D03.438.260.825) OR (MH:D03.605.084.737) OR (MH:D04.075.080.875.099.221.750) OR (TW:Penicillins) OR (TW:Antibiotics, Penicillin) OR (TW:Penicilina$) OR (TW:penicillin$) OR (TW:amoxicil$) OR (TW:amoxil) OR (TW:actimoxi) OR (TW:BR‐2333) OR (TW:clamoxyl) OR (TW:clariana) OR (TW:hydroxyampicillin) OR (TW:penamox) OR (TW:polimox) OR (TW:trimox) OR (TW:wymox) OR (TW:erythromycin$) OR (TW:erycette) OR (TW:erymax) OR (TW:llotycin T‐Stat)))
Appendix 6. Dissertations/Theses/Abstracts search strategy
Keyword CONTAINS: "injúria dental" or "avulsão dental" or "intrusão dental" or "extrusão dental" or "trauma dental" or "trauma axial" or "deslocamente dental" or "deslocamente axila" or "deslocamento lateral" or "luxação dental" or "luxação axial"
AND
"splints periodontais" or "contenções periodeontais" or "reposição dental" or "reerupção dental" or "traumatismos dental" or "tratamento dental" or "tratamento do canal radicular" "obturação endodontica" or "obturação do canal dentário" or "pulpotomia" or "pulpectomia" or "intrusão dental" or "intrusão lateral" or "canal radicular" or "dislocamento lateral" or "desvitalização pulpar dental" or "desvitalização pulpar" or "antibiotico" or "agentes antibióticos" or "antibactericida" or amoxilina or "eritromicina" or "amoxilina" or "actimoxi" or "clamoxyl" or "penamox"
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Caprioglio 1990 | Case series. |
| Ebeleseder 2000 | Case series. |
| Filippi 2002 | Study of healthy volunteers with uninjured teeth. |
| Liang 2008 | Short follow‐up time (3 to 6 months). |
| Qin 2002 | Case series. |
| von Arx 2001 | Study of healthy volunteers with uninjured teeth. |
Contributions of authors
Developing search strategy: Cristiane Rufino Macedo. Study selection: Flavia Belmonte, Cristiane Rufino Macedo. Designing the review: Virginia Trevisani, Humberto Saconato. Writing the review: Flavia Belmonte, Cristiane Macedo. Critical revision: Cristiane Macedo, Peter F Day.
Sources of support
Internal sources
Brazilian Cochrane Center, Brazil.
Leeds Dental Institute, University of Leeds, UK.
External sources
-
Cochrane Oral Health Group Global Alliance, UK.
All reviews in the Cochrane Oral Health Group are supported by Global Alliance member organisations (British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; Canadian Dental Hygienists Association, Canada; National Center for Dental Hygiene Research & Practice, USA and New York University College of Dentistry, USA) providing funding for the editorial process (http://ohg.cochrane.org).
-
National Institute for Health Research (NIHR), UK.
CRG funding acknowledgement: The NIHR is the largest single funder of the Cochrane Oral Health Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Declarations of interest
None known.
Stable (no update expected for reasons given in 'What's new')
References
References to studies excluded from this review
Caprioglio 1990 {published data only}
- Caprioglio D, Ronchin M, Zappa G. Splinting technique for traumatic luxation of anterior permanent teeth [Tecniche di splintaggio nelle lussazioni traumatiche dei denti permanenti anteriori]. Rivista Italiana di Odontoiatria Infantile 1990;1(3):21‐6. [PUBMED: 2076432] [PubMed] [Google Scholar]
Ebeleseder 2000 {published data only}
- Ebeleseder KA, Santler G, Glockner K, Hulla H, Pertl C, Quehenberger F. An analysis of 58 traumatically intruded and surgically extruded permanent teeth. Endodontics & Dental Traumatology 2000;16(1):34‐9. [PUBMED: 11202854] [DOI] [PubMed] [Google Scholar]
Filippi 2002 {published data only}
- Filippi A, Arx T, Lussi A. Comfort and discomfort of dental trauma splints ‐ a comparison of a new device (TTS) with three commonly used splinting techniques. Dental Traumatology 2002;18(5):275‐80. [PUBMED: 12427202] [DOI] [PubMed] [Google Scholar]
Liang 2008 {published data only}
- Liang FZ, Lei RC, Zhang LH, Ma WT. Self‐etching adhesive versus traditional wire‐ligated techniques in fixation of traumatized teeth and periodontal index changes. Journal of Clinical Rehabilitative Tissue Engineering Research 2008;12(52):10313‐6. [Google Scholar]
Qin 2002 {published data only}
- Qin M, Ge L, Bai R. Use of a removable splint in the treatment of subluxated, luxated and root fractured anterior permanent teeth in children. Dental Traumatology 2002;18(2):81‐5. [PUBMED: 12184217] [DOI] [PubMed] [Google Scholar]
von Arx 2001 {published data only}
- Arx T, Filippi A, Lussi A. Comparison of a new dental trauma splint device (TSS) with three commonly used splinting techniques. Dental Traumatology 2001;17(6):266‐74. [DOI] [PubMed] [Google Scholar]
Additional references
Al‐Badri 2002
- Al‐Badri S, Kinirons M, Cole B, Welbury R. Factors affecting resorption in traumatically intruded permanent incisors in children. Dental Traumatology 2002;18(2):73‐6. [PUBMED: 12184215] [DOI] [PubMed] [Google Scholar]
Albadri 2010
- Albadri S, Zaitoun H, Kinirons MJ. UK National Clinical Guidelines in Paediatric Dentistry: treatment of traumatically intruded permanent incisor teeth in children. International Journal of Paediatric Dentistry 2010;20 Suppl 1:1‐2. [PUBMED: 20718877] [DOI] [PubMed] [Google Scholar]
Andersson 1989
- Andersson L, Bodin I, Sorensen S. Progression of root resorption following replantation of human teeth after extended extraoral storage. Endodontics & Dental Traumatology 1989;5(1):38‐47. [DOI] [PubMed] [Google Scholar]
Andreasen 1970
- Andreasen JO. Etiology and pathogenesis of traumatic dental injuries. A clinical study of 1,298 cases. Scandinavian Journal of Dental Research 1970;78(4):329‐42. [DOI] [PubMed] [Google Scholar]
Andreasen 1972
- Andreasen JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. International Journal of Oral Surgery 1972;1(5):235‐9. [DOI] [PubMed] [Google Scholar]
Andreasen 1985
- Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth‐the development of pulp necrosis. Endodontics & Dental Traumatology 1985;1(6):207‐20. [DOI] [PubMed] [Google Scholar]
Andreasen 1985b
- Andreasen FM, Andreasen JO. Diagnosis of luxation injuries: the importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Endodontics & Dental Traumatology 1985;1(5):160‐9. [DOI] [PubMed] [Google Scholar]
Andreasen 1989b
- Andreasen FM. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endodontics & Dental Traumatology 1989;5(3):111‐31. [DOI] [PubMed] [Google Scholar]
Andreasen 2001
- Andreasen JO, Andreasen FM. Textbook and Color Atlas of Traumatic Injuries of the Teeth [Texto e Atlas Colorido de Traumatismo Dental]. 3rd Edition. Porto Alegre: Artmed Editora, 2001. [Google Scholar]
Andreasen 2006
- Andreasen JO, Bakland LK, Andreasen FM. Traumatic intrusion of permanent teeth. Part 2. A clinical study of the effect of preinjury and injury factors, such as sex, age, stage of root development, tooth location, and extent of injury including number of intruded teeth on 140 intruded permanent teeth. Dental Traumatology 2006;22(2):90‐8. [PUBMED: 16499632] [DOI] [PubMed] [Google Scholar]
Andreasen 2006b
- Andreasen JO, Bakland LK, Andreasen FM. Traumatic intrusion of permanent teeth. Part 3. A clinical study of the effect of treatment variables such as treatment delay, method of repositioning, type of splint, length of splinting and antibiotics on 140 teeth. Dental Traumatology 2006;22(2):99‐111. [PUBMED: 16499633] [DOI] [PubMed] [Google Scholar]
Barrett 1997
- Barrett EJ, Kenny DJ. Survival of avulsed permanent maxillary incisors in children following delayed replantation. Endodontics & Dental Traumatology 1997;13(6):269‐75. [DOI] [PubMed] [Google Scholar]
Caldas 2001
- Caldas AF Jr, Burgos ME. A retrospective study of traumatic dental injuries in a Brazilian dental trauma clinic. Dental Traumatology 2001;17(6):250‐3. [DOI] [PubMed] [Google Scholar]
Chadwick 2006
- Chadwick BL, White DA, Morris AJ, Evans D, Pitts NB. Non‐carious tooth conditions in children in the UK, 2003. British Dental Journal 2006;200(7):379‐84. [PUBMED: 16607325] [DOI] [PubMed] [Google Scholar]
Crona‐Larsson 1989
- Crona‐Larsson G, Norén JG. Luxation injuries to permanent teeth‐ a retrospective study of etiological factors. Endodontics & Dental Traumatology 1989;5(4):176‐9. [DOI] [PubMed] [Google Scholar]
Day 2010
- Day P, Duggal M. Interventions for treating traumatised permanent front teeth: avulsed (knocked out) and replanted. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD006542.pub2] [DOI] [PubMed] [Google Scholar]
Diangelis 2012
- Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dental Traumatology 2012;28(1):2‐12. [PUBMED: 22230724] [DOI] [PubMed] [Google Scholar]
Drago 1991
- Drago CJ. Splinting of compromised teeth with composite resin. WDA Journal 1991;67(1):9‐11, 50. [PUBMED: 1997037] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [PUBMED: 9310563] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glendor 2000
- Glendor U, Halling A, Bodin L, Andersson L, Nygren A, Karlsson G, et al. Direct and indirect time spent on care of dental trauma: a 2‐year prospective study of children and adolescents. Endodontics & Dental Traumatology 2000;16(1):16‐23. [DOI] [PubMed] [Google Scholar]
Hamilton 1997
- Hamilton FA, Hill FJ, Holloway PJ. An investigation of dento‐alveolar trauma and its treatment in an adolescent population. Part 1: The prevalence and incidence of injuries and the extent and adequacy of treatment received. British Dental Journal 1997;182(3):91‐5. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Humphrey 2003
- Humphrey JM, Kenny DJ, Barrett EJ. Clinical outcomes for permanent incisor luxations in a pediatric population. I. Intrusions. Dental Traumatology 2003;19(5):266‐73. [PUBMED: 14708651] [DOI] [PubMed] [Google Scholar]
Jacobsen 1986
- Jacobsen I. Long term evaluation, prognosis and subsequent management of traumatic tooth injuries. Proceedings of the International Conference on Oral Trauma. Chicago: American Association of Endodontics Endowment and Memorial Foundation, 1986:129.
Kinirons 1991
- Kinirons MJ, Sutcliffe J. Traumatically intruded permanent incisors: a study of treatment and outcome. British Dental Journal 1991;170(4):144‐6. [PUBMED: 2007085] [DOI] [PubMed] [Google Scholar]
Moura 1994
- Moura A, Prokopowitsch I, Dawidowicz H. Etiology and pathogenesis of traumatic dental injuries of patients of endodontic medical department of the University of São Paulo. Endodontics & Dental Traumatology 1994;10(1):45‐8. [Google Scholar]
Nicolau 2001
- Nicolau B, Marcenes W, Sheiham A. Prevalence, causes and correlates of traumatic dental injuries among 13‐year‐olds in Brazil. Dental Traumatology 2001;17(5):213‐7. [DOI] [PubMed] [Google Scholar]
Petersson 1997
- Petersson EE, Andersson L, Sorensen S. Traumatic oral vs non‐oral injuries. Swedish Dental Journal 1997;21(1‐2):55‐68. [PubMed] [Google Scholar]
Rocha 2001
- Rocha MJ, Cardoso M. Traumatized permanent teeth in Brazilian children assisted at the Federal University of Santa Catarina, Brazil. Dental Traumatology 2001;17(6):245‐9. [DOI] [PubMed] [Google Scholar]
Trope 2002
- Trope M. Clinical management of the avulsed tooth: present strategies and future directions. Dental Traumatology 2002;18(1):1‐11. [PUBMED: 11841460] [DOI] [PubMed] [Google Scholar]
Tsilingaridis 2012
- Tsilingaridis G, Malmgren B, Andreasen JO, Malmgren O. Intrusive luxation of 60 permanent incisors: a retrospective study of treatment and outcome. Dental Traumatology 2012;28(6):416‐22. [PUBMED: 22107160] [DOI] [PubMed] [Google Scholar]
Vinckier 1989
- Vinckier F, Lambrechts W, Declerck D. Intrusion of the definitive incisors [Intrusion de l'incisive definitive]. Revue Belge de Médecine Dentaire 1989;44(3):99‐106. [PUBMED: 2697043] [PubMed] [Google Scholar]
von Arx 2001b
- Arx T, Filippi A, Buser D. Splinting of traumatized teeth with a new device: TTS (Titanium Trauma Splint). Dental Traumatology 2001;17(4):180‐4. [PUBMED: 11585145] [DOI] [PubMed] [Google Scholar]
Welbury 2002
- Welbury R, Kinirons MJ, Day P, Humphreys K, Gregg TA. Outcomes for root‐fractured permanent incisors: a retrospective study. Pediatric Dentistry 2002;24(2):98‐102. [PubMed] [Google Scholar]
Wigen 2008
- Wigen TI, Agnalt R, Jacobsen I. Intrusive luxation of permanent incisors in Norwegians aged 6‐17 years: a retrospective study of treatment and outcome. Dental Traumatology 2008;24(6):612‐8. [PUBMED: 19021652] [DOI] [PubMed] [Google Scholar]


