Abstract
Introduction:
Systemic sclerosis is an autoimmune disease that characteristically presents with fibrosis and vasculopathy. In Latin America, the information on the epidemiology of this disease is scarce and records are essential to know its behavior in the populations. In Colombia, the Ministry of Health uses the SISPRO tool to collect information on the unified national health system which offers nearly universal coverage (around 95%). This public information makes it possible to perform epidemiological studies on different diseases.
Objectives:
Using the SISPRO data corresponding to the years 2012–2016, we analyzed the prevalence and characteristics of patients with systemic sclerosis.
Methods:
A descriptive cross-sectional study was performed based on the SISPRO data; we used as keywords the diagnoses of the International Classification of Diseases related to the diagnosis of systemic sclerosis.
Results:
A total of 11,300 individuals diagnosed with systemic sclerosis were documented. The estimated prevalence was 23.7 cases per 100,000 inhabitants (based on a total population of 47,663,162); this disease is more frequent in the age group of 65–69 years in females (77%), and has a female:male ratio of 3.27:1.
Conclusion:
This study describes the epidemiological characteristics of systemic sclerosis in Colombia, based on official statistics from the Ministry of Health. The results provide a new vision of this disease in Latin America and open the door to future research, in order to better understand the particular characteristics of this disease in our country and our region.
Keywords: Systemic sclerosis, epidemiology, Colombia, Latin America, registries
Introduction
Systemic sclerosis (SSc) is an autoimmune disease with high morbidity and mortality due to its multiple clinical manifestations, with potential fatal outcomes, and deterioration in quality of life, due to fibrosis and a characteristic vasculopathy. 1 Although classic clinical manifestations are frequent in this disease, such as skin fibrosis and Raynaud’s phenomenon, there are other clinical manifestations that make it difficult to diagnose it and require experienced centers to confirm the diagnosis and initiate treatment. 1 There are no studies describing the epidemiology of SSc in Colombia, and its prevalence and distribution are unknown. Due to this, in this work we present the SSc epidemiological data taken from the official statistics of the Ministry of Health.
Materials and methods
The Colombian health system is based on public financing from a single payer and a mixed public and private provisions, with a nearly universal coverage (around 95%). 2 The Ministry of Health has developed an information collection and storage tool, called the Comprehensive Social Protection Information System (SISPRO), which has four components: health, pensions, occupational risks, and social promotion. In the first component, the basic and minimum data that the General Social Security System in Health (SGSSS) requires for management, regulation, and control processes are stored and processed. These data are taken from the Individual Health Services Delivery Registry (RIPS). The information contained in these databases is accessible to the public. The data to carry out this study were obtained by consulting the online dynamic tables of the Ministry of Health. We obtained information about the period between 1 January 2012 and 31 December 2016, for which we conducted an analysis of RIPS databases, using the codes of the International Statistical Classification of Diseases and Related Health Problems (10th revision; ICD-10) for SSc (M340, M341, M342, M348, and M349). Following the “Strengthening the Reporting of Observational studies in Epidemiology (STROBE)” guidelines for observational studies (see checklist in Supplementary material), we analyzed variables such as gender, type of insurance (there is different financial scheme for the poor), and distribution in 5-year age groups according to the official projections of the National Administrative Department of Statistics (DANE), based on the projections of the last 2005 national census. 3 Prevalence was adjusted by gender and age group to the 2014 Colombian population using the direct method, for each of the 32 Colombian political divisions (departments), during the 5-year period analyzed, using the average population of the period. Diagnostic criteria for SSc in the SISPRO database are clearly not standardized and depend on each physician. In addition, only the “main diagnosis” is included, which could potentially lead to underreporting in patients with multiple diagnoses, but we could assume SSc should classify as main diagnosis in most, if not all, cases. It is important to note that the Colombian health system is one with the highest coverage in Latin America (45.2 million; the Colombian population is estimated at 47.6 million), according to the Ministry of Health’s latest measurement in 2017. 2
Results
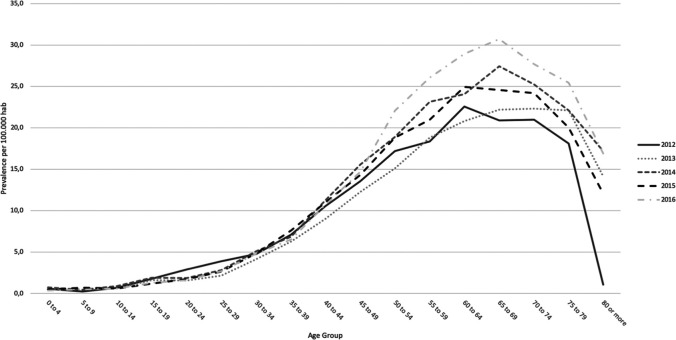
We identified 11,300 cases (“people attended”) with a main diagnosis of SSc, which allowed us to calculate a prevalence of 23.7 cases per 100,000 inhabitants. We could also establish that SSc occurs more frequently in females (77% of cases), with a female:male ratio of 3.27:1. When performing an analysis of the prevalence of SSc by 5-year age groups, we observed a higher prevalence in the 65–69 years age group (see Table 1 and Figure 1). Table 2 shows the number of patients according to gender and age group.
Table 1.
Patients with a main diagnosis of systemic sclerosis according to age group between 2012 and 2016.
| Age group (years) | 2012 | 2013 | 2014 | 2015 | 2016 | Total patients a | Prevalence b |
|---|---|---|---|---|---|---|---|
| 0–4 | 23 | 23 | 31 | 20 | 15 | 106 | 2.5 |
| 5–9 | 10 | 18 | 19 | 28 | 20 | 90 | 2.1 |
| 10–14 | 30 | 25 | 38 | 25 | 26 | 124 | 2.9 |
| 15–19 | 77 | 70 | 82 | 52 | 54 | 300 | 6.9 |
| 20–24 | 120 | 65 | 78 | 74 | 68 | 357 | 8.4 |
| 25–29 | 145 | 82 | 109 | 104 | 107 | 458 | 11.8 |
| 30–34 | 161 | 142 | 177 | 171 | 173 | 659 | 18.9 |
| 35–39 | 213 | 192 | 215 | 244 | 212 | 807 | 25.7 |
| 40–44 | 306 | 260 | 323 | 317 | 312 | 1091 | 37.8 |
| 45–49 | 384 | 351 | 448 | 413 | 422 | 1464 | 51.1 |
| 50–54 | 423 | 384 | 494 | 504 | 603 | 1664 | 63.8 |
| 55–59 | 361 | 386 | 494 | 465 | 600 | 1645 | 77.0 |
| 60–64 | 346 | 332 | 399 | 431 | 521 | 1445 | 86.9 |
| 65–69 | 238 | 265 | 343 | 321 | 419 | 1154 | 92.2 |
| 70–74 | 178 | 193 | 225 | 224 | 268 | 793 | 88.1 |
| 75–79 | 116 | 146 | 149 | 137 | 178 | 538 | 80.0 |
| 80 or above | 66 | 92 | 115 | 83 | 120 | 379 | 56.6 |
| Total | 3086 | 2954 | 3607 | 3455 | 3895 | 11300 | 23.7 |
Number of people attended at some point in the 5-year period.
Calculated with the average population of the period as denominator per 100,000 population.
Figure 1.
Age-specific prevalence of patients with systemic sclerosis during the years 2012–2016. Prevalence calculated with the average population of the period as denominator per 100,000 population.
Table 2.
Patients with a main diagnosis of systemic sclerosis by gender and age group in the period 2012 and 2016.
| Age group (years) | Male |
Female |
||
|---|---|---|---|---|
| Patients | Prevalence a | Patients | Prevalence a | |
| 0–4 | 56 | 0.3 | 50 | 2.4 |
| 5–9 | 44 | 2.0 | 46 | 2.2 |
| 10–14 | 49 | 2.2 | 75 | 3.6 |
| 15–19 | 101 | 4.5 | 199 | 9.3 |
| 20–24 | 94 | 4.3 | 263 | 12.7 |
| 25–29 | 121 | 6.2 | 337 | 17.5 |
| 30–34 | 158 | 9.3 | 501 | 28.2 |
| 35–39 | 179 | 11.8 | 628 | 38.9 |
| 40–44 | 258 | 18.6 | 833 | 55.5 |
| 45–49 | 295 | 21.6 | 1169 | 78.0 |
| 50–54 | 293 | 23.6 | 1371 | 100.3 |
| 55–59 | 303 | 30.0 | 1342 | 119.2 |
| 60–64 | 277 | 35.3 | 1168 | 132.9 |
| 65–69 | 259 | 44.4 | 895 | 134.1 |
| 70–74 | 167 | 40.8 | 626 | 127.7 |
| 75–79 | 128 | 43.8 | 410 | 108.0 |
| 80 or above | 112 | 40.4 | 267 | 68.0 |
| Total | 2645 | 11.2 | 8655 | 35.9 |
Calculated with the average population of the period as denominator per 100,000 population.
When analyzing the type of coverage that patients have according to the health system affiliation regime, we found that the majority of SSc patients belong to the contributory regime (62%), followed by the subsidized regime (31%), complementary plans (5%), and special regimes (1%).
Regarding the distribution of SSc by departments of the country, we found a range of adjusted prevalence of 0–59.86 per 100,000 inhabitants, a male-adjusted prevalence ranges from 0 to 21.8 per 100,000 population, and female-adjusted prevalence from 0 to 96.4 per 100,000 population (see Figure 2). The regions with the highest prevalence are Bogotá, Quindío, Caldas, and Risaralda. The areas with the highest number of reported cases are Bogotá (3731 cases), Antioquia (1532 cases), and Valle del Cauca (956 cases).
Figure 2.
Geographic distribution of the prevalence of systemic sclerosis for the period by departments by gender and age groups adjusted to Colombian population. Prevalence is calculated with the average population of the period as denominator per 100,000 population: (a) global, (b) female, and (c) male.
Discussion
This work on the prevalence of SSc in Colombia from official statistics allows us to have an approach on the distribution of this entity, which adds to the scarce literature on the topic in Latin America. It is important to emphasize the fact that, as the region is experiencing a population transition, with greater industrialization, economic development and aging of the population, the prevalence of chronic entities such as the SSc is increasing, a disease that has traditionally been described in more industrialized countries4,5 and in regions with some particular characteristics. 6 It should also be noted that this and other autoimmune diseases have a considerable burden of environmental factors that impact prognosis, morbidity, and mortality. 7 Also intriguing is that three of the highest prevalent departments correspond to the Colombian coffee triangle, which share a common ancestry, and environmental similarities that could explain a similar prevalence of SSc.
A recent study carried out in Colombia with Community Oriented Program for Control of Rheumatic Diseases (COPCORD) methodology, showed that the prevalence of SSc in the general population was 20 per 100,000 inhabitants, with a prevalence in females of 40 per 100,000 inhabitants. 8 This is very similar to our results from the official data of the Ministry of Health. However, in the Latin American context, studies such as the one carried out in Mexico in 2011 with COPCORD methodology, show a similar prevalence of SSc, of 20 per 100,000 inhabitants, but with a higher prevalence in males (100 per 100,000 inhabitants) than in females (20 per 100,000 population). This is striking, since a higher prevalence has generally been described in women. 9 Another study carried out in the Dominican Republic shows a lower prevalence than that of our study, of only 0.93 per 100,000 inhabitants, with a female:male ratio of 2.7:1. This prevalence is much lower than ours, but shows a similar female:male ratio. 10 A study conducted in Brazil showed a prevalence of 10.5 per 100,000 inhabitants. 11 Another study carried out in Buenos Aires showed data very similar to ours, since they found a global prevalence of 29.6 per 100,000 inhabitants, with a prevalence in the female population of 47.7 per 100,000 inhabitants, and 2.8 per 100,000 inhabitants in the male population, as well as an average age at diagnosis of 66 years. 12
Another study that yielded similar results is the one conducted in Lugo, Spain, with a global prevalence of 27.7 per 100,000 inhabitants, 77% females. 13 A review made in Australia by Morrisroe et al. 14 showed a prevalence of 23.3–86 per 100,000 inhabitants, with female predominance, with a maximum female:male ratio of 5:1. In Detroit (USA), a prevalence of 27.6 per 100,000 inhabitants was estimated, being more frequent in women than in men, with a 4.6:1 ratio. 15
Reviews such as those made by Fautrel et al. 6 show that the overall prevalence of SSc varies between 0.7 and 48.9 per 100,000 inhabitants; it also shows a greater predominance in the female population and an age-related effect in the White female population, with a greater prevalence between 65 and 74 years, similar to the findings of our study. The SSc prevalence data from our study and from most of the previously cited studies are within the prevalence range in most of Europe, as compiled by Shapira et al. 16 (prevalence of 3.1–33.9 per 100,000 inhabitants). A summary of the SSc global prevalence is presented in Figure 3.
Figure 3.
World prevalence of systemic sclerosis. Prevalence is calculated with the average population of the period as denominator per 100,000 population.9–13,17,18
The fact that most of the patients (62%) belong to the contributory regime, which roughly covers half of the population (the better well-off), could perhaps reflect the lower possibility to access a rheumatologist in the other half of the population. This could lead to subdiagnosis in the most vulnerable part of the Colombian population.
The main limitation of our study is the possible underreporting or wrong reporting by physicians at the moment of entering the ICD-10 code in the medical records, and the fact that the diagnostic criteria used for each case are unknown. The smaller number of patients in the subsidized regime, which covers close to half of the whole Colombian population, could be explained by the barriers to specialized care of this financial scheme. Due to the characteristics of the registry and the fact that there is no criterion to determine which is the “main diagnosis” from 1 year to another, a variation in the registry could occur; for this reason it is not possible to calculate the incidence or duration of the disease. 19 Likewise, due to the limited information available, it is not possible to establish the time of evolution of the disease, the specific clinical characteristics of the patients, their response to treatment, the severity of the disease, or the mortality. Our study shows information taken from the database of the Colombian Ministry of Health, information that is used to make demographic and epidemiological analyzes, and projections for the care of patients with SSc in our country.
Conclusion
This study analyzes the prevalence of SSc in Colombia based on official statistics; it shows a global prevalence similar to that described in other regions of the world, with the female population being the most affected by this disease. The data presented in this work will open the door to future research, in order to better understand the particular characteristics of SSc in different regions of Colombia.
Supplemental Material
Supplemental material, STROBE_checklist for Prevalence of systemic sclerosis in Colombia: Data from the National Health Registry 2012–2016 by Daniel G Fernández-Ávila, Santiago Bernal-Macías, Juan M Gutiérrez, Diana N Rincón and Diego Rosselli in Journal of Scleroderma and Related Disorders
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: All procedures performed in this study were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Santiago Bernal-Macías  https://orcid.org/0000-0002-7010-8338
https://orcid.org/0000-0002-7010-8338
Supplemental material: Supplemental material for this article is available online.
References
- 1. Denton CP, Khanna D. Systemic sclerosis. Lancet 2017; 390: 1685–1699. [DOI] [PubMed] [Google Scholar]
- 2. Ministerio de Salud y Protección Social de Colombia. Cobertura sistema de salud en Colombia, 2019, https://www.minsalud.gov.co/proteccionsocial/Paginas/cifras-aseguramiento-salud.aspx
- 3. Departamento Administrativo Nacional de Estadística DANE. Proyecciones de población, 2014, https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion
- 4. Albala C, Vio F, Yanez M. Epidemiological transition in Latin America: a comparison of four countries. Rev Med Chil 1997; 125(6): 719–727. [PubMed] [Google Scholar]
- 5. Rose NR. Prediction and prevention of autoimmune disease in the 21st century: a review and preview. Am J Epidemiol 2016; 183(5): 403–406. [DOI] [PubMed] [Google Scholar]
- 6. Fautrel B, Sibilia J, Chifflot H, et al. Incidence and prevalence of systemic sclerosis: a systematic literature review. Semin Arthritis Rheum 2008; 37(4): 223–235. [DOI] [PubMed] [Google Scholar]
- 7. Anaya JM, Ramirez-Santana C, Alzate MA, et al. The autoimmune ecology. Front Immunol 2016; 7: 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. González C, Ballesteros JG, Londoño J, et al. Prevalencia de la enfermedad reumática en Colombia, según estrategia COPCORD-Asociación Colombiana de Reumatología. Estudio de prevalencia de enfermedad reumática en población Colombiana mayor de 18 años. Rev Colomb Reumatol 2018; 25(4): 245–256. [Google Scholar]
- 9. Pelaez-Ballestas I, Sanin LH, Moreno-Montoya J, et al. Epidemiology of the rheumatic diseases in Mexico. A study of 5 regions based on the COPCORD methodology. J Rheumatol Suppl 2011; 86: 3–8. [DOI] [PubMed] [Google Scholar]
- 10. Gottschalk P, Vásquez R, López PD, et al. Esclerodermia en el Caribe: Características en una serie de casos dominicana. Reumatol Clin 2014; 10(6): 373–379. [DOI] [PubMed] [Google Scholar]
- 11. Horimoto AMC, Matos ENN, Costa MR, et al. Incidence and prevalence of systemic sclerosis in Campo Grande, State of Mato Grosso do Sul, Brazil. Rev Bras Reumatol Engl Ed 2017; 57(2): 107–114. [DOI] [PubMed] [Google Scholar]
- 12. Rosa JE, Soriano ER, Narvaez-Ponce L, et al. Incidence and prevalence of systemic sclerosis in a healthcare plan in Buenos Aires. J Clin Rheumatol 2011; 17(2): 59–63. [DOI] [PubMed] [Google Scholar]
- 13. Arias-Nunez MC, Llorca J, Vazquez-Rodriguez TR, et al. Systemic sclerosis in northwestern Spain: a 19-year epidemiologic study. Medicine 2008; 87(5): 272–280. [DOI] [PubMed] [Google Scholar]
- 14. Morrisroe K, Stevens W, Proudman S, et al. A systematic review of the epidemiology, disease characteristics and management of systemic sclerosis in Australian adults. Int J Rheum Dis 2017; 20(11): 1728–1750. [DOI] [PubMed] [Google Scholar]
- 15. Mayes MD, Lacey JV, Jr, Beebe-Dimmer J, et al. Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large US population. Arthritis Rheum 2003; 48(8): 2246–2255. [DOI] [PubMed] [Google Scholar]
- 16. Shapira Y, Agmon-Levin N, Shoenfeld Y. Geoep-idemiology of autoimmune rheumatic diseases. Nat Rev Rheumatol 2010; 6(8): 468–476. [DOI] [PubMed] [Google Scholar]
- 17. Barnes J, Mayes MD. Epidemiology of systemic sclerosis: incidence, prevalence, survival, risk factors, malignancy, and environmental triggers. Curr Opin Rheumatol 2012; 24(2): 165–170. [DOI] [PubMed] [Google Scholar]
- 18. Ingegnoli F, Ughi N, Mihai C. Update on the epidemiology, risk factors, and disease outcomes of systemic sclerosis. Best Pract Res Clin Rheumatol 2018; 32(2): 223–240. [DOI] [PubMed] [Google Scholar]
- 19. Mendez-Ayala A, Narino D, Rosselli D. Burden of epilepsy in Colombia. Neuroepidemiology 2015; 44(3): 144–148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, STROBE_checklist for Prevalence of systemic sclerosis in Colombia: Data from the National Health Registry 2012–2016 by Daniel G Fernández-Ávila, Santiago Bernal-Macías, Juan M Gutiérrez, Diana N Rincón and Diego Rosselli in Journal of Scleroderma and Related Disorders