Abstract
Objectives:
Socialization predicts cognitive aging outcomes. Neighborhoods may facilitate socially engaged aging and thus shape cognition. We investigated places where older adults socialized and whether availability of these sites was associated with cognitive outcomes.
Methods:
Qualitative analysis of interviews and ethnography with 125 older adults (mean age 71 years) in Minneapolis identified where participants socialized outside of home. This informed quantitative analysis of a national sample of 21,151 older Americans (mean age at baseline 67 years) from the Reasons for Geographic and Racial Differences in Stroke study. Multilevel generalized additive models described associations between access to key social places and cognitive function and decline.
Results:
Qualitative analysis identified eateries, senior centers, and civic groups as key places to socialize. We identified significant positive associations between kernel density of senior centers, civic/social organizations, and cognitive function.
Discussion:
Specific neighborhood social infrastructures may support cognitive health among older adults aging in place.
Keywords: environment, neighborhoods, social support, cognitive function, well-being
Introduction
Urban neighborhood environments are social determinants of cognitive aging. Increased density of infrastructure and destinations has been associated with better cognition in older adults (Besser et al., 2019; Besser et al., 2017). Neighborhood greenness (Brown et al., 2018) and access to a community center (Clarke et al., 2015) were associated with lower risks of Alzheimer’s disease and slower cognitive decline, respectively. A greater land use mix of residential and retail/commercial has been associated with lower odds of dementia (Wu et al., 2015) and access to coffee shops and fast-food restaurants associated with higher cognitive functioning among older adults (Finlay et al., 2020). Neighborhoods may be linked to cognition through effects on individual behaviors or exposures, such as walking, diet, mental stimulation, social engagement, and pollution. For example, access to nearby transit stops may increase physical activity (through active transit), diet (via access to grocery stores), and cognitive stimulation navigating the neighborhood environment (Besser et al., 2019). In sum, urban environments influence individual behaviors, constrain choices, and structure immediate access and exposure to shared resources and hazards, which may impact cognitive health among aging residents.
The potential role of neighborhood social infrastructure to boost cognitive function and protect against cognitive decline is not yet known. Sustained social engagement and strong social support networks are important predictors of health and well-being in later life. Conversely, loneliness and social isolation are linked to increased risk for depression (Cacioppo et al., 2010; Cacioppo et al., 2006), cardiovascular disease (Valtorta et al., 2016), and all-cause mortality (Blazer, 2020; Holt-Lunstad et al., 2015). Prior research finds that higher social participation and perceived support are linked to better cognitive function in older adults, whereas social isolation, loneliness, and poor social relationships are associated with cognitive decline, dementia, and Alzheimer’s disease (Evans et al., 2018; Kuiper et al., 2016; Sundstrom et al., 2020). There are multiple pathways through which social engagement may support cognitive functioning and protect against cognitive decline over time. Decreased engagement in everyday activities may result in disuse of the brain (Hultsch et al., 1999), which in turn may contribute to cognitive decline. Social support networks may prevent or modulate responses to stressful events that are damaging to health (Kawachi & Berkman, 2001), including the brain directly through inflammatory pathways (Sundstrom et al., 2020). Social engagement has also been proposed as a form of cognitive reserve as it may help older adults to maintain day-to-day cognitive function in the face of brain aging, pathology, or insults (Fancourt et al., 2018; Scarmeas & Stern, 2003; Stern et al., 2020). Furthermore, social networks may motivate positive health behaviors that are beneficial to cognitive functioning, such as regular exercise and non-smoking (Kuiper et al., 2016).
This study bridges neighborhood-health, environmental gerontology and cognitive aging literatures. We questioned where diverse older adults socialize outside of the home and whether availability of social places is associated with better cognitive function. Neighborhood contexts may be pivotal to supporting socially engaged aging in place (Finlay et al., 2018). “Third places” within neighborhoods facilitate social interaction, community building, inclusion, and social support (Oldenburg, 1999). These ordinary and often in-expensive places to “hang out” include formal organizations such as community centers and churches; and neighborhood public places such as parks, cafes, bars, and shopping malls. This social infrastructure (Klinenberg, 2018) may be particularly important to older adults who are at increased risk for social isolation and loneliness (Blazer, 2020; Finlay & Kobayashi, 2018). Older adults in urban areas may have unique opportunities for daily socialization in neighborhood places that can help buffer against loneliness (Torres, 2018), which by extension may support cognitive function and protect against cognitive decline.
In this mixed-methods study, thematic analysis of interviews and ethnographic fieldwork across the Minneapolis (MN) metropolitan area explored how and where older adults socialize and engage with others. The qualitative findings extend understanding of perceptions and usage of social infrastructure in a large, socioeconomically, and racially diverse sample of older adults living in a range of urban and suburban neighborhoods. The widespread popularity of both public and private local places such as coffee shops, senior centers, and civic groups to regularly gather and interact with others prompted new questioning into how social infrastructure might impact cognitive health in later life. The qualitative findings inspired novel exploratory investigation into whether access to these places was associated with cognitive functioning in a large, national sample of aging Americans in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. To our knowledge, this study is the first to examine potential links between avail-ability of social infrastructure and cognitive function by integrating evidence from qualitative fieldwork with quantitative survey data. It contributes new evidence to an emerging ecological model of cognitive health (Cerin, 2019) and highlights the importance of specific neighborhood amenities to support socially engaged aging in place.
Methods
We conducted an exploratory sequential mixed-methods study (Figure 1; Creswell et al., 2011). In Phase I, we analyzed qualitative data from the Aging in the Right Place study. The qualitative results generated the hypothesis that access to social places boosts socialization, which positively impacts cognitive function and protects against cognitive decline. In Phase II, we tested this hypothesis in a national sample of older Americans followed since 2003 in the REGARDS study. We examined whether residential proximity to and availability of senior centers, civic and social organizations, and food and drinking places (the three key qualitative themes) was associated with cognitive functioning and cognitive decline.
Figure 1.
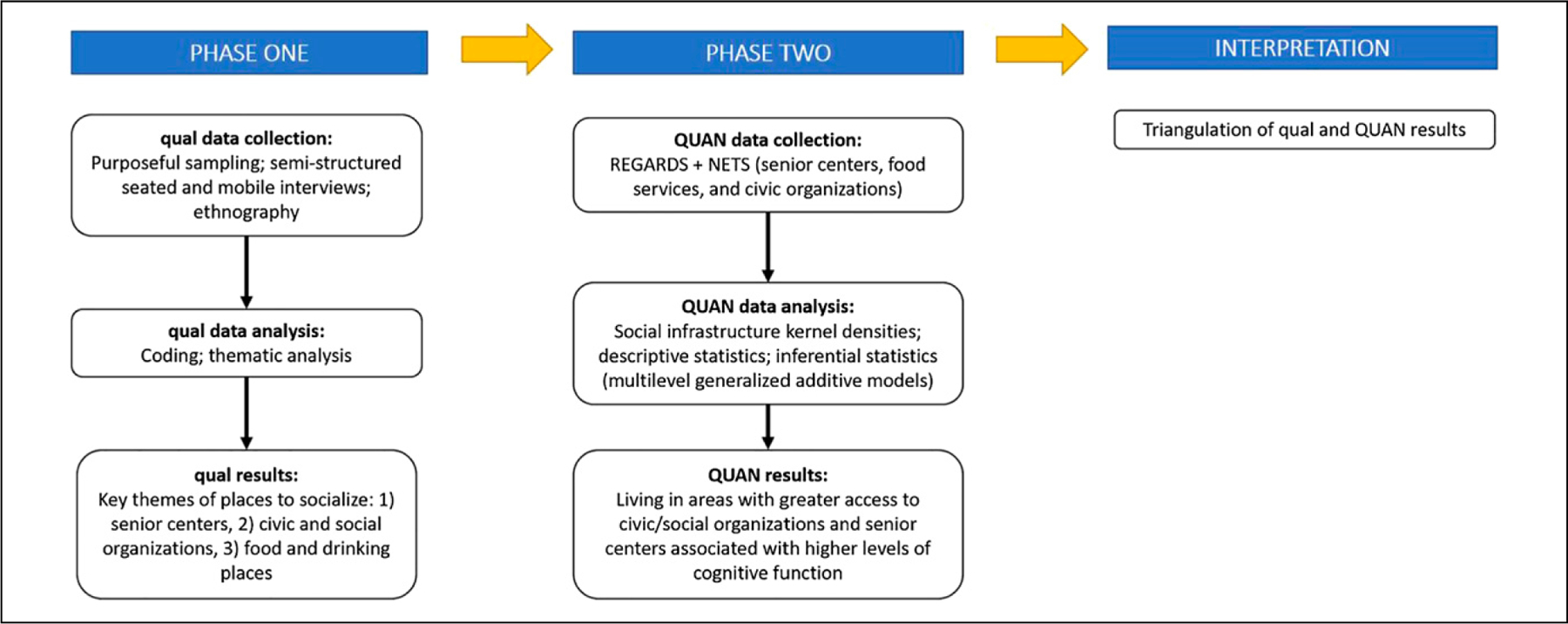
Exploratory sequential mixed-methods study design.
Phase I: Aging in the Right Place Study
This research aimed to examine how older adults perceive and navigate aging in place. Situated in the Minneapolis (MN) metropolitan area, the purposive design of three case study areas selected for sociodemographic and geographic variability (Supplementary Figure 1). Potential participants volunteered in response to project flyers placed in local shops, senior centers, residential buildings, newsletters, and health fairs. Eligibility included self-identifying as an older person and at least 55 years old, not institutionalized in a care setting, residence in a case study area, and demonstrated cognitive capacity to participate. The University of Minnesota Institutional Review Board approved study procedures, and all participants provided written informed consent.
Methods.
The lead author (JF) conducted semi-structured interviews with 125 older adults from June to October 2015. Questions probed for daily routines, social interactions, housing quality, service provision, and perceived well-being (details previously published: Finlay, 2017, 2018; Finlay & Kobayashi, 2018; Finlay et al., 2018, 2019; see Supplementary Table 1). Interviews were audio-recorded and ranged in duration from 30 to 90 minutes. Ninety-six participants volunteered to engage immediately afterward in a mobile interview (Finlay & Bowman, 2017), which were on average 17 minutes in duration and .86 km in length. Participants determined the route, mode of transit, and pace of movement to tour their home and neighborhood environments. This method produced spatially grounded and place-specific data, accessed subtler and more complex meanings of place, created opportunities for flexible and collaborative conversation with participants in situ, built rapport, and efficiently produced rich geographic data (Finlay & Bowman, 2017, p. 263). To capture broader spatial and temporal scales, a subset of six participants engaged in ethnographic fieldwork over 12 months (September 2015 to August 2016). Participants represented a variety of socioeconomic backgrounds, health statuses, and locations (details previously published: Finlay, 2018, 2021). At least once a month, JF spent time with participants at home, in grocery stores, senior centers, coffee shops, sites of worship, and parks. They conversed often between sessions by phone and email. JF employed unstructured interview techniques to seek personal accounts and perceptions and recorded notes in a small notebook and photography.
Qualitative analysis.
We organized qualitative material, including professionally transcribed audio files, in NVivo 12. The guiding research question for this analysis was: Where and how did participants socialize with others outside of their homes? We analyzed the qualitative data according to Braun and Clarke’s (2006) six steps of thematic analysis: familiarization, generation of initial codes, search for themes, review, define and name themes, and write-up. All authors first read through the material and generated initial codes. We met to compare interpretations and points of divergence in order to refine and clarify the coding structure. After test-coding and finalizing the codebook, the first author (JF) coded all material. The second and senior authors (ME and PC) reviewed all coding to ensure completeness and accuracy. The authorship team met to review the coding and define and name themes. JF wrote the results with substantive input from all coauthors. Regular debriefing among coauthors, negative case analysis, member checking, and audit trails enhanced transparency and credibility in identifying themes, linkages, and explanations (Marshall & Rossmann, 2016).
Phase II: REGARDS Study
The REGARDS study is an ongoing, national prospective cohort study. Investigators recruited community-dwelling adults aged 45 years or older from January 2003 to October 2007 by mail and telephone. The cohort includes 30,239 Black and white individuals with a mean baseline age of 64 years (details previously published: Howard et al., 2005). The baseline telephone interview collected demographics, behavioral and lifestyle information, and medical history. In 2006, a cognitive battery was implemented during follow-up. Investigators recorded and geocoded residential addresses over the follow-up period.
Measures
Cognitive Function.
Measures of verbal learning, memory, and executive function were administered biannually using the Consortium to Establish a Registry for Alzheimer’s Disease Word List Learning (WLL) and Word List Delayed Recall (WLD), as well as the Animal Fluency Test (AFT) and Letter Fluency Test (LFT) (Moms et al., 1989; Morris et al., 1989). These cognitive measures were validated for Black and white individuals (Lucas et al., 2005). In addition, a 5-minute battery was administered beginning in 2009, consisting of selected Montreal Cognitive Assessment ([MoCA] Nasreddine et al., 2005) items (see Supplementary Table 2).
We did not have a hypothesis for which specific cognitive function domains may be associated with frequenting social places. Therefore, to capture global cognitive function and use multiple sources of information from the REGARDS cognitive assessment with minimal measurement error, we used a factor score derived from a confirmatory factor analysis of all 5 cognitive tests (WLL, WLD, AFT, LFT, and MoCA) across all assessments in the REGARDS follow-up period. The model fits the data well (root mean square error of approximation = .013; comparative fit index= .999). Further details on the cognitive tests and the factor structure of the model are provided in Supplementary Table 2. We output standardized factor scores for each participant at each assessment to use in analyses.
Social Infrastructure.
The National Establishment Time-Series (NETS) database provides annual records of the US economy with detailed business microdata for more than 60 million private for-profit and nonprofit establishments, in addition to government agencies (Finlay et al., 2019; Hirsch et al., 2020; Walls, 2007). We selected establishments that were open from 2006 to 2017 belonging to three categories in the North American Industry Classification System ([NAICS] US Census Bureau, 2019) based upon the key qualitative themes: (1) civic and social organizations, such as clubs and veterans’ membership organizations; (2) food and drinking places, including restaurants and bars; and (3) services for the elderly and persons with disabilities, largely composed of senior centers (see Supplementary Table 3).
We created three measures to describe REGARDS participants’ annual social infrastructure environments through a kernel density method (Guagliardo, 2004). If a participant moved within the study period (2006–2017), we updated their social infrastructure kernel density measurements accordingly. Because participants in the qualitative analysis stated that residential proximity was important to usage, we fit a smoothly curved surface over each establishment location: the surface value was highest at the exact location and diminished over a 1-mile circular buffer to zero. Since qualitative results suggested that availability was also important (e.g., having multiple eateries to gather and socialize), we summed overlapping kernel values at each REGARDS participant’s home location. A high kernel value represented multiple sites in close proximity, while a kernel value of zero reflected the absence of such establishments within the participant’s surrounding area. Densities were cube-root transformed to help rein in potentially high-leverage values.
Covariates.
Control variables included individual-level characteristics associated with cognitive function, including: age (at first assessment; centered at 65 years), gender (male; female), race (Black; white), highest level of educational attainment (less than high school diploma; high school diploma; some college; college degree or more), marital status (single, divorced, or widowed; married), and years of follow-up from the first cognitive test. Neighborhood-level covariates—derived from the 2008–2012 and 2013–2017 5-year estimates from the American Community Surveys (US Census Bureau, 2013)—included census tract population density (log-transformed), proportion of a census tract population living below the poverty line, proportion of tract’s residents who were non-Hispanic Black, and pro-portion of housing units in a tract that were owner-occupied.
Analytical Sample.
REGARDS study respondents who participated in at least one data collection time point between 2006 and 2017 comprised our sample. Respondents varied in when they contributed their first cognitive test score within this period, with the majority (82%) contributing their first score between 2006 and 2008. Most respondents were tested 3–5 times over this interval. We included individuals with at least one cognitive test score and a valid kernel density score in the analyses. The years of follow-up from baseline test ranged from 0 years (among participants with only a baseline cognitive test) to 11.6 years. To match the qualitative data, we restricted the sample to individuals living in urban areas (identified as “urban core” or “other urban” by Rural-Urban Commuting Area Codes [United States Department of Agriculture, 2019]). Our final analytic sample included 21, 151 individuals with 73,228 observations.
Quantitative Analysis.
We used Gaussian generalized additive multilevel models to examine two ways in which neighborhood social infrastructure may be related to cognition: cognitive function and cognitive decline. All models were fit using gamm4 (Wood & Scheipl, 2017) in the R statistical programming language (R Core Team, 2020).
In the first set of models, we examined whether cognitive function varied between individuals who resided in neighborhoods with different levels of access to social infrastructure. For this analysis, we regressed respondents’ cognitive test scores on each of the social infrastructure density measures described above.1 To allow for nonlinear associations among neighborhood social resources and individual cognitive function, we fit each kernel density measure as a smooth term, using thin-plate regression splines (Wood, 2017). To assess whether social infrastructure kernel density was significantly associated with cognitive function, we calculated the p-values described in Wood (2012) for each of the focal smooth terms.
To help account for demographic and neighborhood features that might alternatively explain variation in cognitive function among REGARDS participants, we included the covariates described above (e.g., age, race, and neighborhood poverty) as controls in this analysis. Further, to account for the fact that observations were not independent—that is, respondents were both clustered within tracts and contributed multiple test scores to the sample across time—we included person-specific intercepts; person-specific time slopes; and census tract-specific intercepts as additional, random model parameters. Altogether, this analysis allowed us to investigate whether respondents who lived in neighborhoods that were densely populated by sites that facilitate social interaction experienced higher levels of cognitive function than adults who lived in areas that lacked said resources.
In the second set of models, we examined whether neighborhood social infrastructure was related to how individuals experienced cognitive decline. For this analysis, we fit two models for each social infrastructure measure: one that constrained cognitive trajectories across the course of the sample to be equal among all respondents, regardless of their neighborhood environment (i.e., Model 1); and one that allowed for cognitive trajectories to vary among individuals according to their access to neighborhood social infrastructure (i.e., Model 2). Model 1 was produced by regressing cognitive test scores on social infrastructure kernel density, years of follow-up from baseline test, and the controls and random terms described above. Model 2 was produced under a similar specification, except that we also fit an interaction among years from baseline test and social infrastructure kernel density. Interaction terms between time and social infrastructure densities were estimated as tensor-product smooths to allow for increased model flexibility (Wood, 2017).
We used Akaike information criterion (AIC) to assess which of the two model specifications better represented how cognitive function changed over time for REGARDS participants (Wood, 2017). A lower AIC generally indicates that a model more accurately reflects the true underlying data generating process; as such, a lower AIC for Model 2 would provide evidence to suggest that access to neighborhood social infrastructure played a meaningful role in shaping how respondents experienced cognitive decline over the course of the REGARDS study.
Results
Phase I: Qualitative
Characteristics of the qualitative sample are shown in Table 1. The average age at assessment was about 71 years, and 57% of participants were white. Two-thirds of the sample were female, about one-third were married, and 43% had at least some college education. Thematic analysis generated three main categories of social infrastructure that participants frequented to gather and interact with others outside of the home: senior centers, civic and social organizations, and food and drinking places. Additional sites among select participants included sites of worship, personal care, recreation, arts and culture, sports, and retail/services.
Table 1.
Descriptive Statistics for Qualitative Sample (n = 125): Aging in the Right Place Study (2015–2016).
| Measure | Mean ± SD or % |
|---|---|
| Age (years) | 71.3 (±7.8) |
| Female | 67 |
| Race/ethnicity: white | 57 |
| Race/ethnicity: Black | 25 |
| Race/ethnicity: other | 18 |
| Married | 34 |
| Education: high school or less | 57 |
Note. SD = standard deviation. “Other” self-identified races/ethnicities include (in alphabetical order) African, American Indian, Arabic, Asian, Bohemian, French, German, Hispanic/Latin American, Irish, Jewish, Norwegian, Polish, and Swedish.
Senior centers.
When asked who she talks to on a regular basis, Barbara (67 y)2—who lived alone and was not close to her family—replied that it was people in her local senior center:
It’s a very active senior center. We have our coffee every Monday. We have lunch every other Thursday. There’s lots of other things that go on there. When I retired a year ago, the senior center saved me. It really did. I went from all my friends being work friends to nobody in a day. I immediately started going to the coffee [group]. At least I had somebody to talk to once a week. Because when you first retire, the first week I had no one to talk to, not a soul.
Senior centers were often discussed as important places for regular social activities including cards and games, clubs, gatherings, and classes. As Denise (72 y) explained:
I do a lot of things with the senior center. I signed up for their memory class that’s coming up… I belong to the book club there, a wonderful group of really sharp women from all kinds of backgrounds.
Given that Denise could not drive following a stroke, she was happy to “pile into” the senior center’s van for outings. Isolated and lonely female participants like Barbara and Denise went two to five times a week to engage with others. Male participants often mentioned spending time “with the guys” at senior centers, such as David (75 y) who had attended a men’s coffee group for 10 years. Thomas (67 y) frequented a center’s woodshop daily and formed close relationships with the people there. During ethnographic sessions, JF listened to good-natured banter and witnessed strong social bonds between Thomas and his male woodshop friends. Thomas shared that he felt less lonely through daily social connection at the senior center.
Senior centers were low-cost spaces to socialize and spend time among both high- and low-income participants. For homeless and low-income participants, a downtown senior center anchored social connection, stability, and daily routine. Iris (68 y), Louis (57 y), Emma (58 y ), and Jim (55 y) countered insecure living situations and loneliness by focusing on positive connections formed through this place. They traveled there daily from homeless shelters to take advantage of free coffee and cookies, socialize with friends and staff, and enjoy a supportive environment. JF spent extended time in this senior center with Frank (77 y) and engaged regularly with fellow attendees of diverse ages, genders, racial and ethnic identities, and physical and cognitive abilities. For a breadth of participants, senior centers were valued places to make new friends and interact regularly with others.
Civic and social groups.
Affluent participants often discussed their involvement in committees and volunteer organizations such as parks and civic boards, planning advisory committees, neighborhood block groups, charities, political campaigns, and veterans’ organizations. Oliver (73 y) explained his involvement in multiple civic groups: “I like volunteering. You might say I am a volunteer junkie.” Aside from his wife, these groups contained the few people whom Oliver engaged with on a regular basis. For participants living alone and lonely such as Trudy (60 y), volunteering in a nearby center was an essential social activity and reason to get out the door: “I felt that it was better than me just sitting here all the time.” Nearby participant Joey (89 y) expressed:
I don’t do a lot here in the neighborhood—shopping and everything—but I belong to [a refugee committee]. I just came from a great meeting of theirs last week... Fantastic! I don’t do a lot down here other than that socially, but I like to go to these things.
In addition to providing opportunities to socialize, volunteering and participation in civic groups enabled a sense of purpose and regular activity.
Several low-income Black female participants residing in lower socioeconomic status (SES) areas expressed the importance of their neighborhood block clubs. They collectively watched local streets to enhance safety, fundraised for local improvements (e.g., speed bumps and park refurbishment), and organized neighborhood activities (e.g., street potluck barbeques and litter pickup). Multiple downtown-residing affluent participants belonged to a community aging organization providing social programs and classes for fee-paying members. Blanche (74 y) explained: “Intellectually they have things going on all the time that are wonderful.” Fellow members Cindy (72 y) and Bob (78 y) defined their neighborhood based upon the people they knew and regularly interacted with from this organization. Male participants such as William (71 y) sought out community and social opportunities through military and veteran associations. Overall, the breadth of civic and social organizations available nurtured social engagement among a wide range of participants by age, gender, race, income, and hobbies.
Food and drinking places.
Coffee shops, cafes, restaurants, and bars were highly discussed places to socialize. Participants such as Deborah (78 y) attended regular coffee gatherings with retired peers: “I got out to lunch maybe once a month. Coffee once a week, just to socialize and be with people my own age.” Fast-food restaurants and bars were multigenerational environments to meet up with younger family members, such as Ruth (70 y) and Harry (75 y): “There’s a real neat bar that has blues on Monday nights. They have a great group... and it’s just fun! Our daughter lives close to that, so we meet up with them and often go together.” Participants such as Warren (65 y) attended happy hours at local eateries to meet other single older adults. Fellow widow Nancy (77 y), a recent Minnesota transplant, went out regularly to make new friends and feel less lonely. Whether seeking new romantic relationships or friendships, meeting for snacks, meals, and beverages in local establishments was widely perceived as a low-pressure way to do so.
Both male and female participants also enjoyed socializing with staff and soaking up ambient contact. Cindy (72 y) related: “If you go into [the bar down the street], you’re going to run into people that are from all walks of life.” Though her husband could not travel far given severe disability, they enjoyed sitting in the local bar for impromptu encounters with neighbors, fellow customers, and staff. When Ellen (73 y) walked to the local shop for her daily coffee, ethnographic field notes reflect the welcoming social atmosphere:
The staff clearly knew her, and already had the coffee waiting for her by the time we got through the line to pay. They knew her regular routine, and were friendly and chatty. Ellen clearly enjoyed talking to them and being social with the young barista staff.
During Rachel’s (74 y) mobile interview, the local coffee shop staff greeted her with warmth and familiarity. While preparing her usual order, they inquired about upcoming medical appointments and art shows. Estranged from her children and living alone, this shop was an anchor of social connection and care and place to feel less lonely.
Black female participants residing in low SES neighborhoods, including Raquel (74 y), lamented the lack of such establishments:
There are a lot of seniors that are our friends who are isolated. I think it’s because we don’t have places where you can just go sit down, have a cup of coffee, see who comes in, visit with one another.
Local eateries represented comfortable, low-pressure, and affordable places to socialize for both high- and low-income participants. They represented generally welcoming multi-generational spaces to engage with others through both planned and impromptu social interactions.
Additional social places.
Sites of social engagement that were mentioned but less universal among participants (i.e., less frequent and generalizable by age, gender, race, and SES) included arts and culture venues (e.g., museums, theaters, and art galleries), sporting arenas (e.g., basketball and football games), and retail/service environments (e.g., grocery stores, bakeries, second-hand clothing stores, pharmacies, and post offices). Some participants shared encountering others and socializing in recreational amenities such as parks, gyms, pools, tennis courts, and golf courses. Susan (80 y) expressed: “I start out my week by walking [in a nearby park], and then we always stop and have coffee and catch up on everybody’s news and gossip.” Her husband Brad (81 y) played tennis several times a week with nine other men.
For religious participants, churches, synagogues, mosques, and temples were essential places for social well-being. Some participants worshiped at least once a week, in addition to attending choir, fellowship, Bible study, luncheons, and volunteer programs. Warren (65 y) attended his synagogue regularly, and labeled it as a major source of support and community throughout his life, including after his wife’s death. For Salma (67 y), the local church welcomed her family into a “big, big community” after immigrating to the US Brenda (73 y), who navigated chronic health conditions and had recently left an abusive relationship, expressed: “I’m dealing with [pain] without having a bunch of help. But I’ve got my Minister, we’ve talked about a lot of things.” Brenda was appreciative of the strong support system through her faith community and opportunities to leave home to engage with others. Ingrid (66 y) commented: “My church is here; my whole life is here.” For some, including Black female participants like Ingrid residing in a lower SES area, faith communities provided meaningful social connections and supportive long-term service networks.
Affluent female participants such as Michelle (74 y) regularly frequented hair salons: “I have a hair appointment once a week now, that’s one of my little indulgences.” She also took her teenage granddaughters to get manicures and pedicures together. Michelle lacked friends, felt lonely, and commented how much she enjoyed talking to her hairdresser and outings with her granddaughters. For male participants such as Timothy (77 y), the barbershop two blocks away was a regular spot to “hang out.” He socialized there with his barber and other customers in attendance, many of them regulars who had become friends. While overall not that many participants described personal care sites as places for socialization, for participants such as Michelle and Timothy they were anchors of social bonding, support, and care.
Phase II: Quantitative
Table 2 provides descriptive statistics for the REGARDS analytical sample. The mean cognitive score, averaged over time, was approximately .015 (SD = 2.335). Forty percent of the sample was Black; more than half identified as female; and the average respondent was about 67 years old (SD = 8.825) at the time of their first cognitive test. Two-thirds of the sample had at least some college education. Respondents were situated in 12,669 unique metropolitan census tracts with varying levels of social infrastructure.
Table 2.
Descriptive Statistics for Quantitative Sample (n = 21,151): Reasons for Geographic and Racial Differences in Stroke Study (2006–2017).
| Variable | Mean/proportion | SD |
|---|---|---|
| Cognitive test score | .015 | 2.335 |
| Senior center kernel density | .003 | .004 |
| Civic and social group kernel density | .007 | .005 |
| Food and drinking place kernel density | .011 | .007 |
| Age (at baseline test) | 67.00 | 8.825 |
| Black | .398 | — |
| Female | .556 | — |
| Married | .608 | — |
| Education: less than high school | .089 | — |
| Education: high school | .237 | — |
| Education: some college | .269 | — |
| Education: college degree or higher | .405 | — |
| Tract: proportion of housing owner occupied | .634 | .205 |
| Tract: proportion Black | .425 | .351 |
| Tract: proportion earning below poverty line | .188 | .133 |
| Tract: (log) population density | 7.433 | 1.564 |
| Years from baseline test | 3.445 | 3.177 |
Note. Respondents contributed 73,228 observations to the sample and were clustered within 12,669 unique census tracts. The years of follow-up from baseline test ranged from 0 years (among participants with only a baseline cognitive test) to 11.6 years.−
Cognitive function and neighborhood social infrastructure.
Table 3 displays parameter estimates for our analysis of between-person variation in cognitive function. The smooth terms in the bottom panel of Table 3 capture the association among social infrastructure kernel densities and cognitive function. While direct interpretation of these smooth terms is somewhat uninformative, their associated significance tests suggest that certain dimensions of the neighborhood social infrastructure environment are significantly associated with cognitive function. In particular, neighborhood civic and social organization kernel density (p-value ≤ .001) and senior center kernel density (p-value = .004) were estimated to be significantly associated with individuals’ overall level of cognitive function. Local access to eating and drinking establishments was not significantly associated with cognitive function (p-value = .996).
Table 3.
Relationship between Neighborhood Social Infrastructure and Cognitive Function: (Gaussian) Generalized Additive Multilevel Models.
| Parameter | Civic and social organizations |
Food and drinking establishments Parametric terms |
Senior centers |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Parametric terms | |||||||||
| β | SE | t-value | β | SE | t-value | β | SE | t-value | |
| Intercept | .13 | .11 | 1.18 | .01 | .11 | .10 | .05 | .11 | .46 |
| Age (at baseline test) | −.09 | .00 | −74.55 | −.09 | .00 | −74.46 | −.09 | .00 | −74.50 |
| Years from baseline test | −.07 | .00 | −33.65 | −.07 | .00 | −33.08 | −.07 | .00 | −33.00 |
| White | .93 | .03 | 30.63 | .92 | .03 | 30.30 | .92 | .03 | 30.40 |
| Male | −.39 | .02 | −16.22 | −.39 | .02 | −16.20 | −.39 | .02 | −16.20 |
| Education: college degree (ref.) | ― | ― | ― | ― | ― | ― | ― | ― | ― |
| Education: some college | −.68 | .03 | −24.38 | −.69 | .03 | −24.69 | −.69 | .03 | −24.67 |
| Education: high school | −1.18 | .03 | −40.21 | −1.19 | .03 | −40.57 | −1.19 | .03 | −40.56 |
| Education: less than high school | −1.77 | .04 | −43.16 | −1.78 | .04 | −43.40 | −1.78 | .04 | −43.37 |
| Married | .14 | .02 | 5.59 | .13 | .02 | 5.33 | .13 | .02 | 5.42 |
| Tract: (log) population density | .05 | .01 | 4.99 | .07 | .01 | 6.95 | .06 | .01 | 7.33 |
| Tract, proportion owner occupied housing | .27 | .07 | 3.78 | .20 | .07 | 2.74 | .22 | .07 | 3.13 |
| Tract, proportion Black | −.14 | .04 | −3.17 | −.16 | .05 | −3.49 | −0.16 | 0.04 | −3.59 |
| Tract, proportion below poverty line | −.35 | .11 | −3.22 | −.37 | .11 | −3.44 | −0.36 | 0.10 | −3.37 |
|
Random terms | |||||||||
| Parameter | SD | SD | SD | ||||||
|
| |||||||||
| Person-specific intercepts | 1.26 | 1.26 | 1.26 | ||||||
| Person-specific time slopes | .13 | .13 | .13 | ||||||
| Tract-specific intercepts | .26 | .26 | .26 | ||||||
|
Smooth terms | |||||||||
| Parameter | EDF | p-value | EDF | p-value | EDF | p-value | |||
|
| |||||||||
| Civic and social group kernel density | 5.13 | <.001 | ― | ― | ― | ― | |||
| Food and drinking place kernel density | ― | 2015 | 1.00 | .996 | ― | ― | |||
| Senior center kernel density | ― | ― | ― | ― | 1.00 | .004 | |||
Note: EDF denotes “effective degrees of freedom” and summarizes the number of parameters associated with each smooth. Ref. indicates “reference category.”
p-values for smooth terms are derived from the F-test described in Wood (2012).
To further unpack the associations implied by our models, we used the models presented in Table 3 to generate predicted cognitive test scores across a range of observed kernel density values, while holding all other variables in the model constant. Figure 2 displays these predictions, along with corresponding uncertainty intervals.
Figure 2.
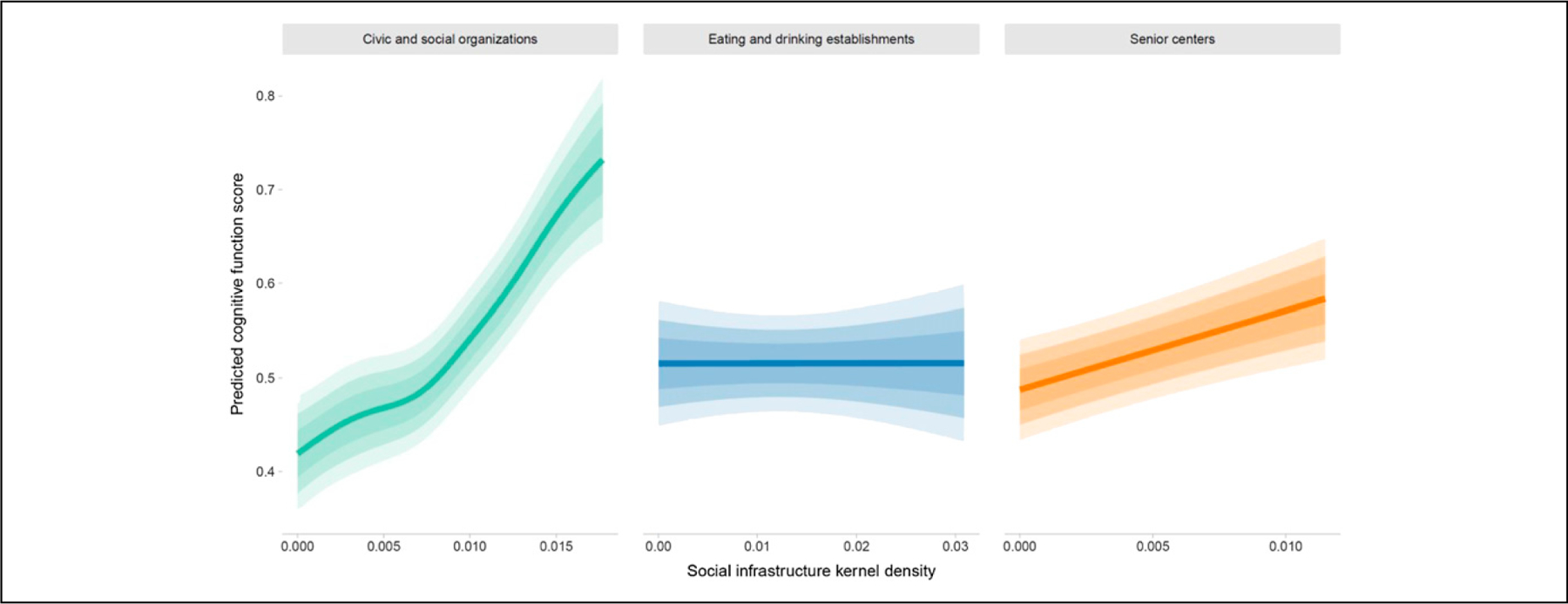
Predicted cognitive factor scores across a range of social infrastructure kernel densities. Note. Predictions are derived from the models presented in Table 3 and made for the 0–99th percentile of each observed kernel density score. All additional model covariates are held constant at their medians (for continuous features) or modes (for categorical features). The 50%, 75%, and 90% uncertainty intervals are marked by shaded regions.
The first panel in Figure 2 demonstrates a positive association between civic/social organization kernel density and cognitive function. Individuals residing in neighborhoods with little to no access to civic or social organizations (i.e., areas with kernel densities near 0) had predicted cognitive scores of approximately .42. In contrast, individuals residing in areas with high levels of access to civic and social organizations (i.e., areas at .018, the 99th percentile of civic/ social densities observed in the sample) had predicted scores of approximately .71. For context, this .29 difference in predicted cognitive scores among individuals residing in starkly different neighborhood environments was equivalent to a 3-year difference in age (1 year of age = an estimated .09-point difference in scores).
Figure 2 also demonstrates a moderate association among senior center infrastructure and cognitive function. Individuals living in areas with minimal levels of senior center infrastructure displayed predicted cognitive scores of .49, while individuals residing in areas with very high levels of infrastructure had estimated cognitive scores of approximately .57. Additionally, as indicated by the significance tests mentioned above, Figure 2 demonstrates a null association among eating and drinking establishment kernel density and cognitive function: individuals near the lowest and highest levels of this broad type of social infrastructure were predicted to have nearly identical cognitive test scores.
Cognitive decline and neighborhood social infrastructure.
We next present the results for our analysis of cognitive trajectories. For parsimony, we only display AIC scores for: (1) Model 1, which constrained the rate of cognitive decline across the length of the study to be identical across all respondents, and (2) Model 2, which allowed for the rate of cognitive decline to fluctuate across individuals who were situated in neighborhoods with varying levels of social infrastructure. Table 4 provides this summary information.
Table 4.
Fit Statistics for Gaussian Generalized Additive Multilevel Models for Rate of Change in Cognitive Function.
| Social infrastructure measure | AIC Model 1 | AIC Model 2 |
|---|---|---|
| Civic and social group kernel density | 286,792.2 | 286,797.4 |
| Food and drinking place kernel density | 286,802.0 | 286,803.9 |
| Senior center kernel density | 286,799.0 | 286,801.0 |
Note. AIC = Akaike information criterion. Model 1 represents a specification where rate of cognitive decline is independent of neighborhood-level social infrastructure. Model 2 represents a specification where rate of cognitive decline is dependent on the kernel density of social infrastructure sites in a respondent’s neighborhood.
As indicated in Table 4, the AICs of models with no interaction between years of follow-up time from baseline test and social infrastructure were universally smaller than models that incorporated this interaction. These results suggest that older adults’ rates of cognitive decline were independent of access to neighborhood social infrastructure sites in the REGARDS sample.
Discussion
This mixed-methods approach to understanding the potential role of neighborhood social infrastructure in later-life cognitive function and decline contributes novel evidence on contextual influences on cognitive health (Cerin, 2019). Consistent with prior research (Besser et al., 2019; Besser et al., 2017; Clarke et al., 2015; Finlay et al., 2020), our results suggest that urban infrastructure impacts cognitive health among older adults. By offering places to sustain positive social engagement and maintain social ties, neighborhood contexts appear implicitly involved in shaping cognitive function. Our results combine rich, subjective insights into complex urban realities and lived experiences from qualitative investigation with standardized and more generalizable findings derived through quantitative inquiry (Regnault et al., 2017). Mixing these data together generated novel inquiry and more comprehensive understanding of a multifaceted health research question (Creswell et al., 2011; Tariq & Woodman, 2013).
The qualitative analysis identified specific neighborhood places where urban older adults socialized. Senior centers were highly discussed places for connection to others, social support, and sense of community. This finding reflects previous research on organized institutional settings among older adults (Loe, 2011; Weil, 2014), in which senior centers structured social networks, routine interpersonal activities, cohesion, and opportunities for friendship. REGARDS respondents living in areas with greater access to senior centers demonstrated elevated levels of cognitive function relative to their peers, which confirmed our qualitatively derived hypothesis. We also observed strong convergence between the qualitative and quantitative results for civic and social organizations. In the qualitative results, local civic groups enabled participants to regularly engage with others (Greenfield et al., 2012), build a sense of community, and “get out the door.” These sites supported regular social activities, which can enhance cognitive reserve and improve cognitive function (Krueger et al., 2009; Kuiper et al., 2016). In subsequent quantitative analyses, the association between individual cognitive function and availability of local civic/social organizations was particularly pronounced. The convergent mixed-methods findings for both civic/social organizations and senior centers suggest that sites explicitly devoted to social interaction, relationships, civic engagement, and cohesion may protect cognitive functioning among older adults. These venues nurture social engagement, support, and connectedness among a breadth of older adults (Finlay et al., 2018) and thereby reduce risk for social isolation and associated poorer cognitive outcomes (Evans et al., 2018).
In the qualitative results, participants also valued coffee shops, restaurants, and bars as familiar third places to gather and “hang out,” Consistent with previous research among older adults (Torres, 2018; Broughton et al., 2016; Cheang, 2002; Finlay et al., 2020), eateries anchored social contact through planned gatherings with friends and family, informal interactions, and ambient contact with others. Eateries close to home were daily places to gossip with other regulars (Torres, 2018), seek laughter and fun (Cheang, 2002), be part of the community (Finlay et al., 2020), and engage in other forms of social support. Contrary to our initial predictions, local availability of food and drinking places played little to no role in shaping individual cognitive function in the quantitative analysis. Several factors may account for divergence between the qualitative and quantitative results. The NAICS codes we used to capture this social infrastructure category may be too broad. Qualitative participants discussed frequenting coffee shops and fast-food restaurants more often than bars and formal dining options, but our kernel density measure additionally incorporated full-service restaurants and bars to incorporate the full breadth of suggested social eating places. In previous research with REGARDS participants (Finlay et al., 2020), we found a positive association between the kernel density of coffee shops and fast-food restaurants with cognitive functioning. Further, some eateries may be less accommodating and comfortable to older adults, such as noisy and crowded restaurants and bars. They may also be too expensive for low-income individuals or not as supportive of social group gatherings around tables and booths.
We did not observe a relationship between social infrastructure and cognitive decline over time. This finding is consistent with those previously observed for education, which has been shown to play a strong role in shaping level of cognitive function in mid-to-later life, but not decline over time (Alley et al., 2007; Clouston et al., 2020; Zahodne et al., 2011). Future research should extend longitudinal follow-up to investigate whether the onset of rapid cognitive decline is delayed among those with greater access to neighborhood social infrastructure.
These results should be considered hypothesis-generating for further investigation. Both samples do not include rural perspectives, nor those living in residential long-term care. For the qualitative study, MN is generally supportive to older adults through investment in services and amenities such as parks, active transit, and care provision. The findings may not apply to other settings with distinct built, social, and natural environments. We did not explicitly ask participants about how neighborhood features impact lifestyle protective and risk factors for cognitive decline. Our exploratory analysis prompts future research directions into how these associations may further vary by person and place. The process by which adults maintain cognitive function as they age is heterogeneous and likely conditional on other social factors that confer power and privilege—such as gender, race, ethnicity, education, and income (Besser et al., 2019; Brewster et al., 2019; Lovden et al., 2020). While investigating these higher-order complexities is beyond the scope of the current manuscript, we strongly encourage future researchers to build upon our work and examine if and how the association between cognitive function and neighborhood social resources varies according to other social conditions. We provide a brief example of this line of investigation in the Supplementary Materials, drawing upon the qualitative results which suggested that SES shapes older adults’ abilities to use civic organizations for social support.
Several limitations of our quantitative analysis should be noted. Key confounding individual factors such as personal wealth—which may drive a participant’s place of residence, access to resource-rich environments, and level of cognitive functioning—are unavailable in REGARDS and thus un-accounted for in our models. Similarly, important measures of health and well-being that may jointly shape cognitive out-comes and influence how individuals engage with their surrounding environments (e.g., general health status; functional limitations; and living alone) are either not measured or only measured at the two in-home visits and are not available as repeat assessments across the period of observation in our analyses. As such, we caution readers to interpret our results as descriptive associations, rather than as causal processes. Additional concerns in this area involve selection and/or reverse causation: for instance, due to broad systems of overlapping inequality that govern both well-being and residential mobility, individuals that experience better overall cognitive health may be more readily able to select into neighborhood spaces with plentiful social resources (James et al., 2015). In future work, researchers might utilize REGARDS data with detailed information on the residential histories of respondents to better tease apart the process by which older adults come to live in different neighborhood environments as a function of their cognitive function over time—and make more definitive causal claims about how neighborhood social infrastructure is tied to cognitive outcomes.
Further, we could not determine REGARDS participants’ utilization of social infrastructure, so our results should be interpreted with respect to proximity and density of local infrastructure, as a marker of access. The kernel density method accounted for the proximity and density of nearby establishments, but nearby access to and options for socialization does not necessarily mean that participants frequented these establishments over time. Additional limitations of the quantitative analysis involve the coding of the NETS data. The NAICS categories chosen here may include a handful of organizations that are irrelevant to older adults, such as fraternities and sororities for civic/social organizations. Further, some businesses in the NETS data may be not included, misclassified, or inaccurately geocoded (Finlay et al., 2019; Hirsch et al., 2020). While we adjusted for neighborhood contextual variables, we did not account for some characteristics that may modify the effects of neighborhood social infrastructure, such as walkability, safety, business establishment quality, and proximity to other destinations (e.g., retail, healthcare providers, and recreational amenities).
Conclusions
Using an innovative mixed-methods approach, we identified that neighborhood social infrastructure is strongly related to level of cognitive function among older American adults but not change over time. Given that availability of civic/social organizations and senior centers was associated with higher cognitive functioning, future research investigating causal mechanisms can inform policy decisions and community interventions regarding resource allocation and urban development to support aging populations. Examples may include social programs for older adults hosted in coffee shops or eating establishments. Investment in neighborhood social infrastructure may help protect against cognitive impairment by promoting social engagement, physical and leisure activity, and intellectual stimulation among aging residents.
In 2019, nearly one-third of community-dwelling older adults in the United States lived alone, half for those aged over 85 (Kaplan & Berkman, 2020). It is important to conclude by noting that social isolation and loneliness have become increasingly common among older adults during the coronavirus disease 2019 (COVID-19) pandemic (Blazer, 2020; Morrow-Howell et al., 2020). As businesses and civic centers close or operate with tight restrictions, the temporary and permanent losses of community resources may further isolate older adults with adverse consequences for cognitive health. Virtual programs such as online religious services, civic groups, and coffee clubs are on the rise (Brooke & Jackson, 2020). While many older adults are proficient online, there remain disparities in access and ability. In the uncertainty of what lies ahead and potentially long-term social activity restrictions, it is critical for older adults to have access to local resources that facilitate connection and engagement with the outside world.
Supplementary Material
Acknowledgments
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIA. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy/
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this project was provided by NIH/NIA grant 1RF1AG057540–01 (Clarke), the Michigan Institute for Clinical and Health Research Postdoctoral Translational Scholar Program UL1 TR002240–02 (Finlay), and NIH/NIA Ruth L. Kirschstein National Research Service Award Individual Postdoctoral Fellowship F32 AG064815–01 (Finlay).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental material
Supplemental material for this article is available online.
We chose to fit separate models for each social infrastructure measure. In sensitivity analyses, we found that each kernel density measure was relatively highly correlated with one another, as well as with population density—which is a key feature to account for in the analysis. Models that simulta-neously included all three kernel densities measures and population density yielded nearly identical results to what is presented in the main results—save for the result around eating/ drinking establishment kernel density, which changed from sharing a null to a negative association with cognitive function. In the interest of being conservative, we attribute this change in signs to instability born from multicollinearity and/or concurvity, rather than to a true, substantively interesting description of the process linking cognition to social infrastructure (Gelman & Hill, 2007).
Bracketed information following participant pseudonyms represent age (in years) at time of interview.
References
- Alley D, Suthers K, & Crimmins E (2007). Education and cognitive decline in older Americans: Results from the AHEAD sample. Res Aging, 29(1), 73–94. doi: 10.1177/0164027506294245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besser L, Galvin JE, Rodriguez D, Seeman T, Kukull W, Rapp SR, & Smith J (2019). Associations between neighborhood built environment and cognition vary by apoli-poprotein E genotype: Multi-ethnic study of atherosclerosis. Health Place, 60, 102188. doi: 10.1016/j.healthplace.2019.102188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besser LM, McDonald NC, Song Y, Kukull WA, & Rodriguez DA (2017). Neighborhood environment and cognition in older adults: A systematic review. Am J Prev Med, 53(2), 241–251. doi: 10.1016/j.amepre.2017.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer D (2020). Social isolation and loneliness in older adults-a mental health/public health challenge. JAMA Psychiatry, 77, 990. doi: 10.1001/jamapsychiatry.2020.1054 [DOI] [PubMed] [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psy-chology. Qualitative Research in Psychology, 3(2), 77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Brewster P, Barnes L, Haan M, Johnson JK, Manly JJ, Napoles AM, & Mungas D (2019). Progress and future challenges in aging and diversity research in the United States. Alzheimers Dement, 15(7), 995–1003. doi: 10.1016/j.jalz.2018.07.221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke J, & Jackson D (2020). Older people and COVID-19: Isolation, risk and ageism. J Clin Nurs, 29, 2044. doi: 10.1111/jocn.15274 [DOI] [PubMed] [Google Scholar]
- Broughton KA, Payne L, & Liechty T (2016). An exploration of older men’s social lives and well-being in the context of a coffee group. Leisure Sciences, 39(3), 261–276. doi: 10.1080/01490400.2016.1178200 [DOI] [Google Scholar]
- Brown SC, Perrino T, Lombard J, Wang K, Toro M, Rundek T, Gutierrez CM, Dong C, Plater-Zyberk E, Nardi MI, Kardys J, & Szapocznik J (2018). Health disparities in the relationship of neighborhood greenness to mental health out-comes in 249,405 U.S. medicare beneficiaries. Int J Environ Res Public Health, 15(3), 430. doi: 10.3390/ijerph15030430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago health, aging, and social relations study. Psychol Aging, 25(2), 453–463. doi: 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA (2006). Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol Aging, 21(1), 140–151. doi: 10.1037/0882-7974.21.1.140 [DOI] [PubMed] [Google Scholar]
- Cerin E (2019). Building the evidence for an ecological model of cognitive health. Health Place, 60, 102206 doi: 10.1016/j.healthplace.2019.102206 [DOI] [PubMed] [Google Scholar]
- Cheang M (2002). Older adults’ frequent visits to a fast-food restaurant: Nonobligatory social interaction and the significance of play in a ‘‘third place’’. Journal of Aging Studies, 16, 303–321 doi: 10.1016/S0890-4065(02)00052-X [DOI] [Google Scholar]
- Clarke PJ, Weuve J, Barnes L, Evans DA, & Mendes de Leon CF (2015). Cognitive decline and the neighborhood environment. Ann Epidemiol, 25(11), 849–854. doi: 10.1016/j.annepidem.2015.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston SAP, Smith DM, Mukherjee S, Zhang Y, Hou W, Link BG, & Richards M (2020). Education and cognitive decline: An integrative analysis of global longitudinal studies of cognitive aging. J Gerontol B Psychol Sci Soc Sci, 75(7), e151–e160. doi: 10.1093/geronb/gbz053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW, Klassen AC, Plano Clark VL,& Smith KC (2011). Best practices for mixed methods research in the health sciences Office of Behavioral Social Sciences Research. [Google Scholar]
- Evans IEM, Llewellyn DJ, Matthews FE, Woods RT, Brayne C, & Clare L, on behalf of the CFAS-Wales research team (2018). Social isolation, cognitive reserve, and cognition in healthy older people. PLoS One, 13(8), e0201008. doi: 10.1371/journal.pone.0201008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D, Steptoe A, & Cadar D (2018). Cultural engagement and cognitive reserve: Museum attendance and dementia incidence over a 10-year period. Br J Psychiatry, 213(5), 661–663. doi: 10.1192/bjp.2018.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay J (2018). Cities of (In)Difference: A Mixed-Methods Analysis of Place and Wellbeing in Later Life (PhD), University of Minnesota, Minneapolis, MN. Retrieved from http://hdl.handle.net/11299/216152 University of Minnesota Digital Conservancy database [Google Scholar]
- Finlay J (2021). Intimately Old: From an Embodied to Emplaced Feminist Approach to Aging. Hypatia, 36(1), 80–100. doi: 10.1017/hyp.2020.51 [DOI] [Google Scholar]
- Finlay JM (2017). ‘Walk like a penguin’: Older Minnesotans’ experiences of (non)therapeutic white space. Soc Sci Med, 198, 77–84. doi: 10.1016/j.socscimed.2017.12.024 [DOI] [PubMed] [Google Scholar]
- Finlay JM, & Bowman JA (2017). Geographies on the move: a practical and theoretical approach to the mobile interview. The Professional Geographer, 69(2), 263–274. doi: 10.1080/00330124.2016.1229623 [DOI] [Google Scholar]
- Finlay J, Esposito M, Kim MH, Gomez-Lopez I, & Clarke P (2019). Closure of ‘third place’? Exploring potential consequences for collective health and wellbeing. Health Place, 60, 102225. doi: 10.1016/j.healthplace.2019.102225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay J, Esposito M, Tang S, Gomez-Lopez I, Sylvers D, Judd S, & Clarke P (2020). Fast-food for thought: Retail food environments as resources for cognitive health and wellbeing among aging Americans?. Health Place, 64, 102379. doi: 10.1016/j.healthplace.2020.102379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay JM, Gaugler JE, & Kane RL (2018). Ageing in the margins: expectations of and struggles for à good place to grow old’ among low-income older Minnesotans. Ageing & Society, 40(4), 759–783. doi: 10.1017/S0144686X1800123X [DOI] [Google Scholar]
- Finlay JM, & Kobayashi LC (2018). Social isolation and loneliness in later life: A parallel convergent mixed-methods case study of older adults and their residential contexts in the Minneapolis metropolitan area, USA. Soc Sci Med, 208, 25–33. doi: 10.1016/j.socscimed.2018.05.010 [DOI] [PubMed] [Google Scholar]
- Finlay JM, McCarron HR, Statz TL, & Zmora R (2019). A critical approach to aging in place: a case study comparison of personal and professional perspectives from the minneapolis metropolitan area. J Aging Soc Policy, 1–25. doi: 10.1080/08959420.2019.1704133 [DOI] [PubMed]
- Gelman A, & Hill J (2007). Data analysis using regression and multilevel/hierarchical models Cambridge University Press. [Google Scholar]
- Greenfield EA, Scharlach A, Lehning AJ, & Davitt JK (2012). A conceptual framework for examining the promise of the norc program and village models to promote aging in place. Journal of Aging Studies, 26(3), 273–284. doi: 10.1016/j.jaging.2012.01.003 [DOI] [Google Scholar]
- Guagliardo MF (2004). Spatial accessibility of primary care: Concepts, methods and challenges. International Journal of Health Geographics, 3(3), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JA, Moore KA, Cahill J, Quinn J, Zhao Y, Bayer FJ, Rundle A, & Lovasi GS (2020). Business data categorization and refinement for application in longitudinal neighborhood health research: A methodology. J Urban Health, 1–14. doi: 10.1007/s11524-020-00482-2 [DOI] [PMC free article] [PubMed]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, & Howard G (2005). The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology, 25(3), 135–143. doi: 10.1159/000086678 [DOI] [PubMed] [Google Scholar]
- Hultsch DF, Hertzog C, Small BJ, & Dixon RA (1999). Use it or lose it: Engaged lifestyle as a buffer of cognitive decline in aging? Psychology and Aging, 14(2), 245–263. doi: 10.1037/0882-7974.14.2.245 [DOI] [PubMed] [Google Scholar]
- James P, Hart JE, Arcaya MC, Feskanich D, Laden F, & Subramanian SV (2015). Neighborhood self-selection: The role of pre-move health factors on the built and socioeconomic environment. Int J Environ Res Public Health, 12(10), 12489–12504. doi: 10.3390/ijerph121012489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan DB, & Berkman BJ (2020). Older adults living alone Merck manual https://www.merckmanuals.com/professional/geriatrics/social-issues-in-older-adults/older-adults-living-alone
- Kawachi I, & Berkman LF (2001). Social ties and mental health. Journal of Urban Health, 78(3), 458–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinenberg E (2018). Palaces for the people: How social infrastructure can help fight inequality, polarization, and the decline of civic life Crown Publishing Group. [Google Scholar]
- Krueger KR, Wilson RS, Kamenetsky JM, Barnes LL, Bienias JL, & Bennett DA (2009). Social engagement and cognitive function in old age. Experimental Aging Research, 35(1), 45–60. doi: 10.1080/03610730802545028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiper JS, Zuidersma M, Zuidema SU, Burgerhof JG, Stolk RP, Oude Voshaar RC, & Smidt N (2016). Social relationships and cognitive decline: A systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol, 45(4), 1169–1206. doi: 10.1093/ije/dyw089 [DOI] [PubMed] [Google Scholar]
- Loe M (2011). Aging our way: Independent elders, interdependent lives Oxford University Press. [Google Scholar]
- Lovden M, Fratiglioni L, Glymour MM, Lindenberger U, & Tucker-Drob EM (2020). Education and cognitive functioning across the life span. Psychol Sci Public Interest, 21(1), 6–41. doi: 10.1177/1529100620920576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas JA, Ivnik RJ, Smith GE, Ferman TJ, Willis FB, Petersen RC, & Graff-Radford NR (2005). Mayo’s older African Americans normative studies: Norms for boston naming test, controlled oral word association, category fluency, animal naming, token test, wrat-3 reading, trail making test, stroop test, and judgment of line orientation. Clin Neuropsychol, 19(2), 243–269. doi: 10.1080/13854040590945337 [DOI] [PubMed] [Google Scholar]
- Marshall C, & Rossmann G (2016). Designing qualitative research (6th ed.). Sage. [Google Scholar]
- Moms JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, Mellits ED, & Clark C (1989). The consortium to establish a registry for Alzheimer’s disease (CE- RAD). Part I. Clinical and neuropsychological assesment of Alzheimer’s disease. Neurology, 39(9), 1159–1165. [DOI] [PubMed] [Google Scholar]
- Morris JC, Heyman A, Mohs RC, Hughes JP, Van Belle G, & Fillenbaum G (1989). CERAD investigators.The consortium to establish a registry for Alzheimer’s disease (CERAD): Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology, 39, 1159–1165. doi: 10.1212/WNL.39.9.1159 [DOI] [PubMed] [Google Scholar]
- Morrow-Howell N, Galucia N, & Swinford E (2020). Recovering from the COVID-19 pandemic: A focus on older adults. J Aging Soc Policy, 32, 1–9. doi: 10.1080/08959420.2020.1759758 [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, & Chertkow H (2005). The montreal cognitive assessment, moca: A brief screening tool for mild cognitive impairment. JAGS, 53, 695–699. doi: 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Oldenburg R (1999). The great good place: Cafes, coffee shops, bookstores, bars, hair salons, and other hangouts at the heart of a community (Third ed.). Marlowe & Company. [Google Scholar]
- R Core Team (2020). R: A language and environment for statistical computing R Foundation for Statistical Computing. http://www.R-project.org/ [Google Scholar]
- Regnault A, Willgoss T, & Barbic S, & International Society for Quality of Life Research Mixed Methods Special Interest Gruop (2017). Towards the use of mixed methods inquiry as best practice in health outcomes research. J Patient Rep Outcomes, 2(1), 19. doi: 10.1186/s41687-018-0043-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmeas N, & Stern Y (2003). Cognitive reserve and lifestyle. J Clin Exp Neuropsychol, 25(5), 625–633. doi: 10.1076/jcen.25.5.625.14576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern Y, Arenaza-Urquijo EM, Bartres-Faz D, Belleville S, Cantilon M, & Chetelat G (2020). Conceptual frameworks, W.Whitepaper: Defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimers Dement, 16(9), 1305–1311. doi: 10.1016/j.jalz.2018.07.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundstrom A, Adolfsson AN, Nordin M, & Adolfsson R (2020). Loneliness increases the risk of all-cause dementia and Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci, 75(5), 919–926. doi: 10.1093/geronb/gbz139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tariq S, & Woodman J (2013). Using mixed methods in health research. JRSM Short Rep, 4(6), 2042533313479197. doi: 10.1177/2042533313479197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres S (2018). Aging alone, gossiping together: Older adults’ talk as social glue. J Gerontol B Psychol Sci Soc Sci, 74(8), 1474–1482. doi: 10.1093/geronb/gby154 [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture (2019). Rural-urban commuting area codes https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- U.S. Census Bureau (2013). 2008–2012 American community survey 5-year estimates https://www.census.gov/programs-surveys/acs/data.html
- U.S. Census Bureau (2019). North American Industry classification system https://www.census.gov/eos/www/naics/
- Valtorta NK, Kanaan M, Gilbody S, Ronzi S, & Hanratty B (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart, 102(13), 1009–1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls DW (2007). National establishment time-series Data-base©: Data overview Paper presented at The Kauffman Symposium on Entrepreneurship and Innovation, November 2, 2007. [Google Scholar]
- Weil J (2014). The new neighborhood senior center: Redefining social and service roles for the baby boom generation Rutgers University Press. [Google Scholar]
- Wood SN (2012). On p-values for smooth components of an extended generalized additive model. Biometrika, 100(1), 221–228. doi: 10.1093/biomet/ass048 [DOI] [Google Scholar]
- Wood SN (2017). Generalized additive models: An introduction with R (Second ed.). CRC Press. [Google Scholar]
- Wood S, & Scheipl F (2017). gamm4: Generalized Additive Mixed Models using ‘mgcv’ and ‘lme4’. R package version 0.2–5 https://CRAN.R-project.org/package=gamm4
- Wu YT, Prina AM, Jones AP, Barnes LE, Matthews FE,, & Brayne C, & Medical Research Council Cognitive Function and Ageing Study (2015). Community environment, cognitive impairment and dementia in later life: Results from the cognitive function and ageing study. Age and Ageing, 44(6), 1005–1011. doi: 10.1093/ageing/afv137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Glymour MM, Sparks C, Bontempo D, Dixon RA, MacDonald SW, & Manly JJ (2011). Education does not slow cognitive decline with aging: 12-year evidence from the victoria longitudinal study. Journal of the International Neuropsychological Society: JINS, 17(6), 1039–1046. doi: 10.1017/S1355617711001044 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


