Abstract
Objectives
To investigate the prevalence of, and the factors associated with, long-term sick leave in working-age patients diagnosed with COVID-19 in general practices in Germany.
Methods
Patients aged 18–65 years diagnosed with COVID-19 in any of 1255 general practices in Germany between March 2020 and February 2021 were included in the study. Long-term sick leave was defined as sick leave of at least 4 weeks. The association between predefined independent variables and long-term sick leave was studied using an adjusted logistic regression model.
Results
This study included 30 950 patients diagnosed with COVID-19 (51.7% women, mean (standard deviation) age 41.5 (±13.0) years). The prevalence of long-term sick leave was 5.8%. Female sex, older age, and several conditions (noninfective enteritis and colitis; reaction to severe stress, and adjustment disorders; atopic dermatitis; mononeuropathies; reflux diseases; diabetes mellitus; and hypertension) were positively and significantly associated with long-term sick leave.
Conclusion
Long-term sick leave was relatively rare in COVID-19 patients followed in general practices in Germany. These results should be confirmed or invalidated in other settings and countries.
Keywords: long-term sick leave, COVID-19, coronavirus disease, general practices, Germany
Introduction
COVID-19 is a respiratory infection that emerged in China in December 2019 (Zu et al., 2020) and was declared a global pandemic in March 2020 (Cucinotta and Vanelli, 2020). Common clinical manifestations include fever, cough, dyspnoea, malaise, and fatigue (da Rosa Mesquita et al., 2020). As of June 24, 2021, more than 179 million individuals had contracted COVID-19, and approximately 3.9 million related deaths had been recorded (World Health Organization, 2021). In Germany, the number of confirmed cases and deaths is approximately 3.7 million and 90 500, respectively (World Health Organization, 2021). In this context, research is required to better characterize the epidemiology and the consequences of COVID-19 in this country.
For a substantial proportion of COVID-19 patients, symptoms may last more than 3 weeks. This persistence of symptoms is referred to as post-COVID syndrome. It is estimated that between 10% and 35% of individuals will develop post-COVID syndrome, with fatigue being the most frequent symptom (Pavli et al., 2021). Interestingly, COVID-19 is not only associated with a wide range of symptoms of a potentially chronic nature but is also a risk factor for poor physical health (Tanji et al., 2021), impaired mental well-being (Xiong et al., 2020), and increased disability (Pizarro-Pennarolli et al., 2021). Taken together, these various complications of COVID-19 may negatively impact the ability of working-age patients to work; in fact, a large number of studies have reported high rates of sick leave in workers affected by COVID-19 (Alquézar-Arbé et al., 2020; Calvo-Bonacho et al., 2020; Carvalho-Schneider et al., 2021; COVIDSurg Collaborative, 2021; Groenewold et al., 2020; Khorasanee et al., 2021; Merkin et al., 2020; Prezant et al., 2020; Suárez-García et al., 2020). For example, 1 study using data collected in a UK medical centre in March and April 2020 found that 39% of physicians were absent at least once due to sickness and that absences due to sickness amounted to 1240 days in the overall sample (Khorasanee et al., 2021). Despite this extensive literature, however, little is known about long-term COVID-19 sick leave (i.e., sick leave lasting for at least several weeks) and the populations at particular risk.
Therefore, the goal of our study was to investigate the prevalence of, and the factors associated with, long-term COVID-19 sick leave in working-age patients followed in general practices in Germany.
Materials and methods
Database
Data from the Disease Analyzer database (IQVIA) were used for this study. Details on this database are available in the literature (Rathmann et al., 2018). To summarize, the Disease Analyzer database contains demographic, diagnosis, and prescription data collected in general and specialized practices in Germany, with 3% of all practices in the country included in the database. Diagnosis data are coded using the German adaptation of the International Classification of Diseases, 10th revision (ICD-10), and prescription data using the European Pharmaceutical Marketing Research Association's Anatomical Therapeutic Chemical classification system. Assessment of data quality includes criteria such as completeness of documentation and linkage between diagnoses and prescriptions. Finally, previous research has shown that the Disease Analyzer database offers a representative panel of practices in Germany (Rathmann et al., 2018).
Study population
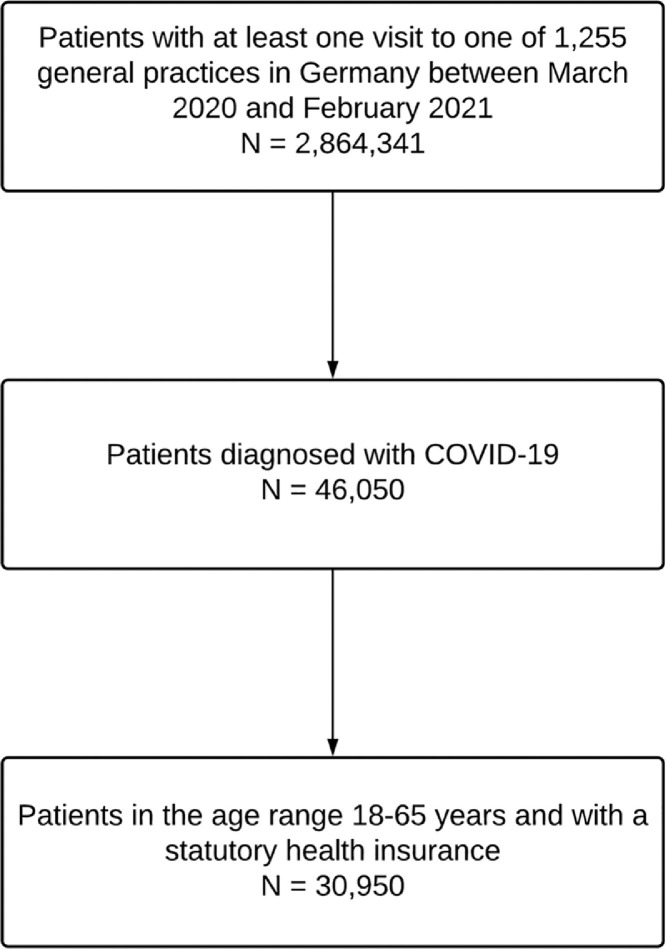
Our study included patients diagnosed with COVID-19 in any of 1255 general practices in Germany between March 2020 and February 2021. Given that the population of interest of this study corresponded to working-age adults, participants had to be aged 18–65 years. Moreover, participants had to have statutory health insurance. Data on those with private health insurance were not included in the analysis, as self-employed people frequently opt for private health insurance (Busse and Blümel, 2014), and sick leave may not be necessary for this group of workers. The selection of study patients is displayed in Figure 1 .
Figure 1.
Selection of study patients
Long-term sick leave
As there is no clear consensus on the definition of long-term sick leave, for the purposes of this study, it was defined as sick leave of at least 4 weeks.
Demographic and clinical variables
Demographic variables included sex and age. Clinical variables included all disorders diagnosed in at least 3% of patients within 12 months prior to COVID-19 diagnosis. These disorders were: hypertension (ICD-10: I10); depression (F32 and F33); gastritis and duodenitis (K29); thyroid gland disorders (E00-E07); atopic dermatitis (L20-L30); reaction to severe stress, and adjustment disorders (F43); lipid metabolism disorders (E78); chronic sinusitis (J32); somatoform disorders (F45); sleep disorders (F51 and G47); chronic headache (G43 and G44); obesity (E66); osteoarthritis (M15-M19); reflux diseases (K20-K22); asthma (J45 and J46); allergic rhinitis (J30); noninfective enteritis and colitis (K50-K52); diabetes mellitus (E10-E14); phlebitis and thrombosis (I80-I84); cardiac arrhythmias (I76-I79); anxiety disorders (F41); mononeuropathies (G56-G59); spondylitis (M47); and vitamin D deficiency (E55).
Statistical analyses
The demographic and clinical characteristics of the study population were studied. The prevalence of long-term sick leave was estimated by dividing the number of patients on long-term sick leave by the total number of patients. Finally, the association of demographic and clinical variables with long-term sick leave was analysed using an adjusted logistic regression model. The results are presented as odds ratios (ORs) and 95% confidence intervals (CIs). P-values <0.05 were considered statistically significant. All analyses were performed using SAS 9.4.
Results
This study included a total of 30 950 patients diagnosed with COVID-19. Of these patients, 51.7% were women, and the mean (standard deviation) age was 41.5 (±13.0) years (Table 1 ). The most common conditions were hypertension (13.5%), depression (12.2%), and gastritis and duodenitis (11.7%). The prevalence of long-term sick leave (i.e., sick leave lasting at least 4 weeks) was 5.8% in the overall sample. Finally, the results of the adjusted logistic regression analysis are displayed in Table 2 . In terms of demographic characteristics, female sex (OR = 1.19; male sex: reference) and older age (36–45 years: OR = 1.84; 46–55 years: OR = 2.68; 56–65 years: OR = 3.71; 18–25 years: reference) were positively and significantly associated with the odds of taking long-term sick leave. In terms of clinical characteristics, there was a significant relationship between long-term sick leave and noninfective enteritis and colitis (OR = 2.02), reaction to severe stress, and adjustment disorders (OR = 1.68), atopic dermatitis (OR = 1.27), mononeuropathies (OR = 1.27), reflux diseases (OR = 1.24), diabetes mellitus (OR = 1.21), and hypertension (OR = 1.19).
Table 1.
Demographic and clinical characteristics of the study population (N = 30 950)
| Variable | Value |
|---|---|
| Sex | |
| Women | 51.7 |
| Men | 48.3 |
| Age (in years) | |
| Mean (standard deviation) | 41.5 (±13.0) |
| 18-25 | 14.3 |
| 26-35 | 22.5 |
| 36-45 | 21.6 |
| 46-55 | 23.2 |
| 56-65 | 18.4 |
| Disorders diagnosed within 12 months prior to the diagnosis of COVID-19 | |
| Hypertension | 13.5 |
| Depression | 12.2 |
| Gastritis and duodenitis | 11.7 |
| Thyroid gland disorders | 11.4 |
| Atopic dermatitis | 9.5 |
| Reaction to severe stress, and adjustment disorders | 9.3 |
| Lipid metabolism disorders | 8.2 |
| Chronic sinusitis | 7.4 |
| Somatoform disorders | 7.2 |
| Sleep disorders | 6.5 |
| Chronic headache | 6.4 |
| Obesity | 6.1 |
| Osteoarthritis | 6.1 |
| Reflux diseases | 6.1 |
| Asthma | 5.2 |
| Allergic rhinitis | 4.7 |
| Noninfective enteritis and colitis | 4.6 |
| Diabetes mellitus | 4.3 |
| Phlebitis and thrombosis | 4.0 |
| Cardiac arrhythmias | 3.8 |
| Anxiety disorders | 3.7 |
| Mononeuropathies | 3.5 |
| Spondylitis | 3.4 |
| Vitamin D deficiency | 3.0 |
Abbreviation: COVID-19 coronavirus disease.
Table 2.
Association between demographic and clinical variables and long-term sick leave in COVID-19 patients followed in general practices in Germany
| Variable | Proportion of patients on long-term sick leave (%) | OR (95% CI) | P value |
|---|---|---|---|
| Total | 5.8 | ||
| Sex | |||
| Female | 6.5 | 1.19 (1.07-1.31) | <0.001 |
| Male | 5.1 | Reference | |
| Age (in years) | |||
| 18–25 | 2.6 | Reference | |
| 26–35 | 2.9 | 1.10 (0.87-1.39) | 0.429 |
| 36–45 | 5.1 | 1.84 (1.48-2.29) | <0.001 |
| 46–55 | 7.5 | 2.68 (2.17-3.29) | <0.001 |
| 56–65 | 10.7 | 3.71 (3.01-4.58) | <0.001 |
| Disorders diagnosed within 12 months prior to the diagnosis of COVID-19a | |||
| Noninfective enteritis and colitis | 12.3 | 2.02 (1.70-2.40) | <0.001 |
| Reaction to severe stress, and adjustment disorders | 11.6 | 1.68 (1.46-1.92) | <0.001 |
| Atopic dermatitis | 9.2 | 1.27 (1.10-1.47) | 0.001 |
| Mononeuropathies | 11.1 | 1.27 (1.04-1.57) | 0.022 |
| Reflux diseases | 11.2 | 1.24 (1.05-1.47) | 0.013 |
| Diabetes mellitus | 11.3 | 1.21 (1.00-1.48) | 0.048 |
| Spondylitis | 12.3 | 1.21 (0.99-1.49) | 0.063 |
| Hypertension | 10.5 | 1.19 (1.04-1.36) | 0.010 |
| Chronic headache | 8.2 | 1.19 (1.00-1.42) | 0.056 |
| Phlebitis and thrombosis | 11.0 | 1.17 (0.96-1.42) | 0.114 |
| Somatoform disorders | 9.9 | 1.13 (0.96-1.34) | 0.132 |
| Sleep disorders | 10.1 | 1.11 (0.94-1.32) | 0.218 |
| Chronic sinusitis | 7.7 | 1.11 (0.94-1.32) | 0.218 |
| Allergic rhinitis | 7.6 | 1.11 (0.89-1.37) | 0.360 |
| Obesity | 9.1 | 1.08 (0.90-1.29) | 0.433 |
| Asthma | 8.8 | 1.06 (0.87-1.30) | 0.540 |
| Depression | 8.6 | 1.05 (0.91-1.21) | 0.506 |
| Gastritis and duodenitis | 8.1 | 1.05 (0.91-1.21) | 0.534 |
| Lipid metabolism disorders | 9.9 | 1.04 (0.89-1.21) | 0.638 |
| Vitamin D deficiency | 8.9 | 1.03 (0.81-1.31) | 0.823 |
| Osteoarthritis | 11.2 | 1.02 (0.87-1.21) | 0.784 |
| Cardiac arrhythmias | 8.4 | 1.02 (0.81-1.27) | 0.892 |
| Anxiety disorders | 8.8 | 1.02 (0.73-1.15) | 0.469 |
| Thyroid gland disorders | 8.1 | 0.99 (0.86-1.14) | 0.910 |
OR: odds ratio.
The adjusted logistic regression model included all demographic and clinical variables displayed in the table.
Long-term sick leave corresponded to sick leave of at least 4 weeks.
The reference column corresponds to patients without the disorder of interest.
Discussion
Main findings
This cross-sectional study, including almost 31 000 patients with COVID-19 from across more than 1250 general practices in Germany, found that 5.8% of patients were on long-term sick leave between March 2020 and February 2021. It was also observed that female sex, older age, and several conditions (i.e., noninfective enteritis and colitis; reaction to severe stress, and adjustment disorders; atopic dermatitis; mononeuropathies; reflux diseases; diabetes mellitus; and hypertension) were positively and significantly associated with the risk of long-term sick leave. To the best of the authors’ knowledge, this is one of the largest studies to have investigated the prevalence of long-term sick leave in people affected by COVID-19.
Interpretation of findings
One major finding of this study is that the rate of long-term sick leave in COVID-19 patients followed in general practices in Germany was slightly higher than 5%. To date, only 1 other study has analysed the prevalence of long-term sick leave in individuals diagnosed with COVID-19. This study of 150 patients with noncritical COVID-19 in France revealed that 19.7% and 11.2%, respectively, were on sick leave for 30 and 60 days after the onset of the disease (Carvalho-Schneider et al., 2021). Although they do not directly assess the proportion of patients on long-term sick leave, other pieces of research have focused on the mean or median period of sick leave. For example, a study including 1911 healthcare workers living in Spain found a median sick leave period of 20 days (Suárez-García et al., 2020). Another study of 4408 emergency medical system responders and 11 230 firefighters from the United States estimated that the mean duration of medical leave was 19.8 days for those with suspected COVID-19 and 25.3 days for those with confirmed COVID-19 who later returned to work (Prezant et al., 2020). The discrepancy between the findings of the previous French study (Carvalho-Schneider et al., 2021) and the present German study's findings may be due to the different settings in which these studies were carried out. Patients included in the French study were treated for COVID-19 in an academic university hospital, whereas our study included individuals followed in general practices. Thus, it is likely that the proportion of participants with severe COVID-19 was lower in the German sample than in the French one.
Interestingly, sex, age, and several chronic disorders were positively and significantly associated with long-term sick leave. First, women were more likely to take long-term sick leave than their male counterparts. This finding is relatively unexpected because previous research suggests that male sex is a risk factor for severe COVID-19 and COVID-19 complications (Vahidy et al., 2021). That being said, persistent fatigue after COVID-19 is more common in women than in men (Townsend et al., 2020), which might explain why the prevalence of long-term sick leave was higher in women than in men. Second, there was a positive relationship between increasing age and long-term sick leave. A systematic review and meta-analysis of 12 studies (N = 3064 COVID-19 patients) revealed that older age increases the risk of several COVID-19 complications (i.e., acute respiratory distress syndrome, acute kidney injury, acute cardiac injury, and shock) (Tiruneh et al., 2021) and thus return to work might be more difficult in older adults than in younger populations. Third, several conditions (noninfective enteritis and colitis; reaction to severe stress, and adjustment disorders; atopic dermatitis; mononeuropathies; reflux diseases; diabetes mellitus; and hypertension) were associated with increased odds of long-term sick leave. Since noninfective enteritis and colitis, atopic dermatitis, mononeuropathies, and reflux diseases involve immunological dysregulations (Elzinga et al., 2019; Lee et al., 2018; Miraglia del Giudice et al., 2006; Rieder et al., 2010), some of which may require the use of immunotherapies (Catalan-Serra and Brenna, 2018; Léger et al., 2016; Werfel and Biedermann, 2015), people affected by these conditions may display a disrupted immunological response when exposed to a pathogen and may be at particular risk of severe COVID-19 and COVID-19 complications. Furthermore, there is some evidence that both diabetes mellitus and hypertension are associated with severe COVID-19 and related complications (Abdi et al., 2020; Lippi et al., 2020), suggesting that these diseases could have long-lasting effects on ability to work following COVID-19 diagnosis. Finally, there was a significant association between reaction to severe stress, and adjustment disorders, and long-term sick leave. One hypothesis is that individuals with this psychiatric condition may have more difficulty adjusting to a COVID-19 diagnosis than the general population, resulting in a delayed return to work after the acute phase of the disease.
Public health implications and directions for future research
Our study found that the vast majority of working-age adults followed in general practices in Germany returned to work in the month following their COVID-19 diagnosis. Nonetheless, barriers to return to work should be identified in people on long-term sick leave, and public health measures reducing these barriers should be implemented. These measures may include the possibility to work from home or to work flexible hours. In terms of future research, long-term sick leave in adults with COVID-19 should be studied in other settings and countries. In addition, further studies are needed to gain a better understanding of the factors that significantly impact the odds of long-term sick leave.
Strengths and limitations
The large sample size and the use of data collected in general practices are 2 major strengths of this study. However, this study is also subject to several limitations. First, sick leave may have been initiated in other settings (e.g., pulmonology practices and hospitals), and sick leave-related data may have been undocumented in some general practices, indirectly leading to an underestimation of the prevalence of long-term sick leave. Second, there is no consensus on the definition of long-term sick leave, and the use of a cut-off of 4 weeks may have impacted the results of this study. Third, no information was available on COVID-19 severity and COVID-19 complications, although these variables likely help predict the odds of taking long-term sick leave.
Conclusion
The prevalence of long-term sick leave was 5.8% in this sample of approximately 31 000 COVID-19 patients followed in general practices in Germany. Sex, age, and several disorders (noninfective enteritis and colitis; reaction to severe stress, and adjustment disorders; atopic dermatitis; mononeuropathies; reflux diseases; diabetes mellitus; and hypertension) were significantly associated with the risk of long-term sick leave. Further research is warranted to corroborate or invalidate the study results in other settings and countries.
Acknowledgments
Conflicts of interest
The authors declare no competing financial interests.
Funding source
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
German law allows the use of anonymous electronic medical records for research purposes under certain conditions. According to this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data. Because patients were only queried as aggregates and no protected health information was available for queries, no Institutional Review Board approval was required for the use of this database or the completion of this study.
Author contributions
Louis Jacob contributed to the design of the study, managed the literature searches, wrote the first draft of the manuscript, and corrected the manuscript. Ai Koyanagi, Lee Smith, Christian Tanislav, Marcel Konrad, and Susanne van der Beck corrected the manuscript. Karel Kostev contributed to the design of the study, performed the statistical analyses, and corrected the manuscript. All authors contributed to and have approved the final manuscript.
References
- Abdi A, Jalilian M, Sarbarzeh PA, Vlaisavljevic Z. Diabetes and COVID-19: A systematic review on the current evidences. Diabetes Res Clin Pract. 2020;166 doi: 10.1016/j.diabres.2020.108347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alquézar-Arbé A, Piñera P, Jacob J, Martín A, Jiménez S, Llorens P, et al. Impact of the COVID-19 pandemic on hospital emergency departments: results of a survey of departments in 2020 - the Spanish ENCOVUR study. Emergencias. 2020;32:320–331. [PubMed] [Google Scholar]
- Busse R, Blümel M. Germany: Health system review. Health Syst Transit. 2014;16:1–296. xxi. [PubMed] [Google Scholar]
- Calvo-Bonacho E, Catalina-Romero C, Fernández-Labandera C, Fernández-Meseguer A, González-Quintela A, Martínez-Muñoz P, et al. COVID-19 and Sick Leave: An Analysis of the Ibermutua Cohort of Over 1,651,305 Spanish Workers in the First Trimester of 2020. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.580546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho-Schneider C, Laurent E, Lemaignen A, Beaufils E, Bourbao-Tournois C, Laribi S, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2021;27:258–263. doi: 10.1016/j.cmi.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalan-Serra I, Brenna Ø. Immunotherapy in inflammatory bowel disease: Novel and emerging treatments. Hum Vaccin Immunother. 2018;14:2597–2611. doi: 10.1080/21645515.2018.1461297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVIDSurg Collaborative COVID-19-related absence among surgeons: development of an international surgical workforce prediction model. BJS Open. 2021;5 doi: 10.1093/bjsopen/zraa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elzinga S, Murdock BJ, Guo K, Hayes JM, Tabbey MA, Hur J, et al. Toll-like receptors and inflammation in metabolic neuropathy; a role in early versus late disease? Exp Neurol. 2019;320 doi: 10.1016/j.expneurol.2019.112967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groenewold MR, Burrer SL, Ahmed F, Uzicanin A, Free H, Luckhaupt SE. Increases in Health-Related Workplace Absenteeism Among Workers in Essential Critical Infrastructure Occupations During the COVID-19 Pandemic - United States, March-April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:853–858. doi: 10.15585/mmwr.mm6927a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khorasanee R, Grundy T, Isted A, Breeze R. The effects of COVID-19 on sickness of medical staff across departments: A single centre experience. Clin Med (Lond) 2021;21:e150–e154. doi: 10.7861/clinmed.2020-0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SH, Kwon JE, Cho M-L. Immunological pathogenesis of inflammatory bowel disease. Intest Res. 2018;16:26–42. doi: 10.5217/ir.2018.16.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Léger J-M, Guimarães-Costa R, Muntean C. Immunotherapy in Peripheral Neuropathies. Neurotherapeutics. 2016;13:96–107. doi: 10.1007/s13311-015-0401-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G, Wong J, Henry BM. Hypertension in patients with coronavirus disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020;130:304–309. doi: 10.20452/pamw.15272. [DOI] [PubMed] [Google Scholar]
- Merkin R, Kruger A, Bhardwaj G, Kajita GR, Shapiro L, Galen BT. Internal Medicine Resident Work Absence During the COVID-19 Pandemic at a Large Academic Medical Center in New York City. J Grad Med Educ. 2020;12:682–685. doi: 10.4300/JGME-D-20-00657.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miraglia del Giudice M, Decimo F, Leonardi S, Maioello N, Amelio R, Capasso A, et al. Immune dysregulation in atopic dermatitis. Allergy Asthma Proc. 2006;27:451–455. doi: 10.2500/aap.2006.27.2887. [DOI] [PubMed] [Google Scholar]
- Pavli A, Theodoridou M, Maltezou HC. Post-COVID syndrome: Incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch Med Res. 2021 doi: 10.1016/j.arcmed.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizarro-Pennarolli C, Sánchez-Rojas C, Torres-Castro R, Vera-Uribe R, Sanchez-Ramirez DC, Vasconcello-Castillo L, et al. Assessment of activities of daily living in patients post COVID-19: a systematic review. PeerJ. 2021;9 doi: 10.7717/peerj.11026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prezant DJ, Zeig-Owens R, Schwartz T, Liu Y, Hurwitz K, Beecher S, et al. Medical Leave Associated With COVID-19 Among Emergency Medical System Responders and Firefighters in New York City. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.16094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathmann W, Bongaerts B, Carius H-J, Kruppert S, Kostev K. Basic characteristics and representativeness of the German Disease Analyzer database. Int J Clin Pharmacol Ther. 2018;56:459–466. doi: 10.5414/CP203320. [DOI] [PubMed] [Google Scholar]
- Rieder F, Biancani P, Harnett K, Yerian L, Falk GW. Inflammatory mediators in gastroesophageal reflux disease: impact on esophageal motility, fibrosis, and carcinogenesis. Am J Physiol Gastrointest Liver Physiol. 2010;298:G571–G581. doi: 10.1152/ajpgi.00454.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Rosa Mesquita R, Francelino Silva LC, Junior, Santos Santana FM, Farias de Oliveira T, Campos Alcântara R, Monteiro Arnozo G, et al. Clinical manifestations of COVID-19 in the general population: systematic review. Wien Klin Wochenschr. 2020:1–6. doi: 10.1007/s00508-020-01760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suárez-García I, Martínez de Aramayona López MJ, Sáez Vicente A, Lobo Abascal P. SARS-CoV-2 infection among healthcare workers in a hospital in Madrid. Spain. J Hosp Infect. 2020;106:357–363. doi: 10.1016/j.jhin.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanji Y, Sawada S, Watanabe T, Mita T, Kobayashi Y, Murakami T, et al. Impact of COVID-19 pandemic on glycemic control among outpatients with type 2 diabetes in Japan: A hospital-based survey from a country without lockdown. Diabetes Res Clin Pract. 2021;176 doi: 10.1016/j.diabres.2021.108840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiruneh SA, Tesema ZT, Azanaw MM, Angaw DA. The effect of age on the incidence of COVID-19 complications: a systematic review and meta-analysis. Syst Rev. 2021;10:80. doi: 10.1186/s13643-021-01636-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Dyer AH, Jones K, Dunne J, Mooney A, Gaffney F, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahidy FS, Pan AP, Ahnstedt H, Munshi Y, Choi HA, Tiruneh Y, et al. Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: Cross-sectional analysis from a diverse US metropolitan area. PLoS One. 2021;16 doi: 10.1371/journal.pone.0245556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werfel T, Biedermann T. Current novel approaches in systemic therapy of atopic dermatitis: specific inhibition of cutaneous Th2 polarized inflammation and itch. Curr Opin Allergy Clin Immunol. 2015;15:446–452. doi: 10.1097/ACI.0000000000000199. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard 2021. https://covid19.who.int/.
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;296:E15–E25. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]