Background
As a foundation for all sensory development, the sense of touch develops prior to the 8th week of gestation and is the cornerstone of human experience and future development of verbal communication, learning, regulation, and social interaction.1–3 The normal developmental trajectory of touch is disrupted when infants are born premature (< 37 completed weeks gestation), separated from their mothers, and placed in a stressful neonatal intensive care unit (NICU) environment. Early disruption of gestation brings consequences during a time of critical fetal development when the brain is growing and organizing exponentially. Unfortunately, much of the touch infants receive in the NICU is related to procedural or unpleasant touch which is often over stimulating especially for infants born very preterm (≤30 weeks gestation), resulting in both adverse physiologic and behavioral state changes.4–6 Little is known about the type, timing, and amount of comforting touch appropriate for hospitalized infants born very preterm.6
For more than 3 decades, researchers have investigated the effects of different types of comforting touch strategies. These supplemental comforting touch techniques, specifically targeted at infants born very preterm, include therapeutic touch —a noncontact, energy balancing therapy;7 gentle human touch (GHT)—a still touch without stroking or massaging;8–12 “touch and caressing–tender in caring” therapy—a gentle/light systematic stroking touch;13–14 and infant massage with kinesthetic stimulation.15 While these studies have resulted in promising short-term outcomes, they have incorporated varying protocols resulting in limited or inconsistent results. Despite these inconsistencies, comforting touch remains essential for optimal growth and development and this touch must be based on each infant’s behavioral and physiological cues. Therefore, this pilot study employs a systematic, infant-driven, stress reducing supplemental touch intervention to fill the gap between what is known about the type, timing, and amount of comforting touch appropriate for hospitalized infants born very preterm.
Purpose and Working Hypothesis
In an attempt to use an infant-driven, gentle, systematic stroking technique (i.e., the M Technique—the ‘M’ stands for manual [a structured manual, method of touch] to separate it from massage) aimed at reducing stress and anxiety in fragile patients, our research team conducted one of the first studies to explore the feasibility and safety of the M Technique in hospitalized infants born very preterm.16 This promising feasibility study revealed improved physiological and behavioral effects of the M Technique on infants born very preterm after one session.16 To our knowledge, no studies have systematically examined the cumulative impact of the M Technique on infants born very preterm. Therefore, the purpose of this randomized-controlled trial (RCT) pilot was to investigate the cumulative effects of the M Technique on infant neurodevelopment in hospitalized very preterm infants. Our two specific aims were:
To examine the neurobehavioral and growth velocity impact of the M Technique for hospitalized very preterm infants. Our working hypothesis: Very preterm infants (≤30 weeks gestation) who receive the M Technique intervention will have improved (1) neurobehavioral development [NICU Network Neurobehavioral Scale (NNNS)];17 and (2) higher growth velocity (difference in infant weight at the beginning and end of protocol), compared to the control group.
To examine the physiological and behavioral state impact of the M Technique for hospitalized very preterm infants. Our working hypothesis: Very preterm infants who receive the M Technique intervention (experimental group only) will have improved physiologic stability (heart rate [HR], respiratory rate [RR], oxygen saturations) and behavioral state (e.g., Anderson Behavioral State Scale [ABSS])18 changes from baseline at 3 different time points over the course of the 5-week intervention.
In addition to our feasibility study, 16 our overall plan was to propose a rigorous study design of a novel intervention that will inform a larger, more definitive future, full-scale RCT.
Methods
Design
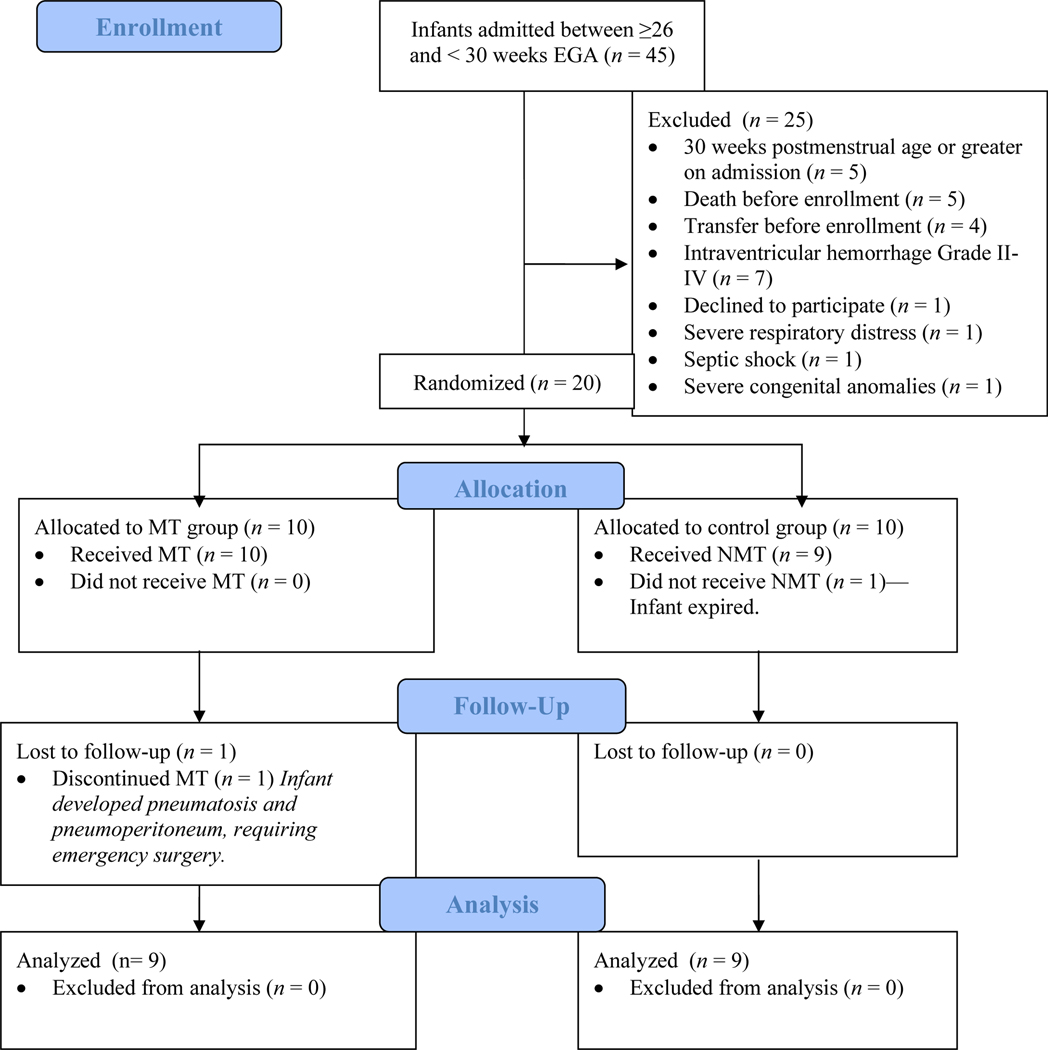
A RCT pilot design was employed using two groups of infants less than 30 weeks gestation. Eligible infants were randomized to the treatment or control groups (Figure 1).19
Figure 1.
Participant flow diagram. Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med 2010;152.
Setting
This RCT pilot study was conducted from September 2012 to May 2013 in the NICU of a 250-bed tertiary care academic pediatric hospital in the Midwest with a 75-bed level IV NICU that admits approximately 750 babies annually.
Sample
Infants between ≥ 26 and < 30 weeks estimated gestational age (EGA [determined by Ballard]) were excluded from the study if they had one of the following: (1) evidence of moderate to severe brain injury (e.g. Grade II-IV intraventricular hemorrhage), (2) septic shock, (3) non-intact skin, (4) respiratory failure (e.g., supplemental Fi02 requirement >75%), (5) severe congenital anomalies, (6) persistent tachycardia, (7) persistent bradycardia, or (8) those deemed unstable as determined clinically by the attending physician (no infants were excluded for instability based on each attending’s clinical judgment). Given the intended pilot nature of this study, a formal power analysis was not performed and a total of 20 subjects were selected based on our experience with our feasibility study.16
Intervention
The M Technique was originally developed by Dr. Jane Buckle as a method of relaxation touch and was used in infants following craniofacial surgery20 and eventually applied to hospitalized very preterm infants.16 The M Technique was provided according to a published detailed protocol from the investigative team’s feasibility study (Box 1).16 Infants in the experimental group received standard NICU care plus 7 minutes of the M Technique 6 times per week, for 5 weeks, for a total of 30 M Technique interventions. The M Technique intervention started once the infant reached 30 weeks postmenstrual age (PMA). This relaxation technique is a method of structured touch that follows a systematic set structure and distinctive pattern. Stroking was applied to the infant’s back using the pads of the 3rd and 4th fingers of both hands on each side of the infant’s spine. Each pattern consists of 3 strokes (e.g., from the nape of the neck to the base of the spine making the capital letter D or the shape of a diamond). There were a total of 8 distinctive patterns. The rationale for this set repetition is for the receiver to know what to anticipate and to avoid any unexpected stimulation. The M Technique uses a set pressure of 3 (more than a tickle) where 0 is no pressure and 10 is crushing pressure. The speed of the M Technique is slow, constant, rhythmical and repetitive. The M Technique can be provided to any part of the body but for this study the technique was delivered to the infant’s back while in a prone position. The duration of the intervention was based on the infant’s response and did not exceed a total of 7 minutes.
Box 1. M Technique Protocol.
Timing of M Technique therapy was based on a schedule that best supported each infant, generally at least, 1.5–2 hours post-feeding (if on a every 3 hour schedule).
Before, during, and after the M Technique administration, each infant’s behavioral and physiological cues and state were closely examined to avoid overstimulation. Administration of the technique was not commenced if the infant was in a quiet sleep state.
Before commencing the M Technique, the primary investigator confirmed with the attending physician and bedside nurse whether or not the infant was still considered a candidate to receive the M Technique. At this point, the nurse was instructed to place the infant in a midline prone position with extremities in flexion (supported by developmental positioning aids) after routine care.
Baseline data obtained.
Immediately prior to commencing the M Technique, the giver’s hands were warmed and Aquaphor applied to aid in reducing friction.
Confirmed infant was in a midline prone position and the upper half of the positioning aid was opened, keeping the lower extremities and buttocks in a well-supported flexed position.
Let your presence be known—hands cupped with one hand resting gently on the infant’s head and the other on the infant’s lower back/buttocks (offered gentle still touch/containment).
Stroking will using a pressure of 3 (0–10) with a set rhythmic sequence, each stroke repeated 3 times.
Stroking was applied to the infant’s back using the pads of the 3rd & 4th fingers of both hands
Total duration– 7 minutes (approximately 20 seconds per stroke)
Ended with still gentle touch/containment
Procedure
The Institutional Review Board at the university hospital approved the research protocol. A member of the research team obtained parental informed consent before enrollment. The study protocol began once the infants reached 30 weeks PMA.
Twenty very preterm infants ≥ 26 and < 30 weeks EGA were randomly assigned to experimental (M Technique) or control groups (n = 10 per group). Potential subjects were identified within the first 7 days of age after consulting with the attending physician. The randomization process used sequentially numbered, opaque sealed envelopes that contained an index card with the word treatment or control.21–22 Parents were provided the opportunity to select one of the envelopes that determined the infant’s allocation.
All infants, in the control and experimental groups, received neurodevelopmental and family-centered care strategies that’s part of this NICU’s standard of care and includes: Skin-to-skin care, parental presence, routine neurodevelopmental evaluation plans by trained physical and occupational therapists, routine positioning support to facilitate optimal physiological development, and an environment that optimizes developmental care consistent with supporting sleep cycles and neurodevelopment. In addition, infants in the experimental group received the M Technique intervention.
Each M Technique intervention was provided by the principal investigator (PI) or one other member of the research team who were trained extensively by Dr. Buckle, the M Technique developer. These two members of the research team also had a combined 60 years of clinical experience in assessing and reading very preterm infant cues. To ensure fidelity of the intervention performance, as part of the training, multiple return demonstrations were conducted on Dr. Buckle to achieve consistency and reduce variability between the M Technique givers. In addition, both trained givers met weekly to review and observe one another’s technique to ensure the intervention was being delivered as planned. Completing the M Technique training and gaining expertise in reading very preterm infant cues are vital before using this intervention.
Timing of each M Technique intervention session was guided by our experience with our feasibility study,16 the session lasted for 7 minutes and was coordinated with the bedside nurse based on a schedule that best supported each infant (Box 1). Each intervention session was performed in the infant’s room between 8:00 a.m. and 11:00 p.m. to allow flexibility for data collection around the infant and family schedule. Planned modification or termination of the stroke was only done if the infant demonstrated signs of physical or behavioral distress. Specific criteria were identified for the M Technique to be discontinued if the infant demonstrated signs of persistent physiologic distress (e.g., heart rate [HR] < 100 or > 200 beats per minutes for 15 seconds or more, or arterial oxygen saturations levels < 85% for longer than 30 seconds) or if the infant required an increase in supplemental FiO2 concentration during the M Technique administration.9, 16 Thus, the M Technique intervention was administered contingent on each very preterm infant’s behavioral and physiological cues.
Infant weights were collected twice as part of the infant’s routine nursing care: before (baseline/30 weeks PMA) the intervention started and again at the end of the 5-week intervention period (35 weeks PMA) for both the experimental and control groups. Infant neurobehavior was evaluated in the infant’s room by a trained research occupational therapist, who was blinded to subject allocation, at the end of the 5-week intervention period (35 weeks PMA) for both the experimental and control groups. Infant behavioral state was judged by a trained neonatal occupational therapist 5 minutes before the intervention (baseline) and recorded at the end of every minute throughout the 7-minute intervention, and up to 10 minutes after the intervention for infants in the experimental group. Infant heart rate (HR), respiratory rate (RR), and arterial oxygen saturation (SaO2) were obtained 5 minutes before the intervention continuously by the infant’s cardiorespiratory monitor and by a trained member of the research team who recorded these data on a separate sheet of paper at baseline, at the end of every minute throughout the 7-minute intervention, and up to 10 minutes after the intervention for infants in the experimental group.
Measures and Outcomes
Demographic Variables
A simple form to collect the demographic and descriptive variables data for each infant was developed by the primary investigator. In order to examine specific aim one, neurobehavioral outcomes and growth velocity; infant neurobehavior was measured using the NNNS and infant weight was measured using pre- and post-intervention weights for between group comparisons. Specific aim two, physiological and behavioral state responses of the M Technique over time, was addressed by measuring HR, RR, SaO2, and the ABSS.
Infant Neurobehavioral Measures:
The Neonatal Intensive Care Unit Network Neurobehavioral Scale (NNNS) is a valid and reliable comprehensive assessment of neurological integrity and behavioral function used specifically in at-risk, drug exposed and preterm infants and has shown long-term predictive ability.17, 23–28 The NNNS was administered at the end of the 5-week intervention period, once the infants reached 35 weeks PMA. All evaluations were performed by a single trained and certified occupational therapist with expertise in evaluating very preterm infant neurobehavior and who was blinded to subject allocation. Each NNNS evaluation started approximately 45 minutes to 1 hour prior to a scheduled feeding or hands-on care. The evaluations took approximately 25 to 30 minutes to complete.
The 115 NNNS items were scored manually and entered into a SPSS syntax (SPSS Inc, Chicago, Illinois) which gave a weight to each item and generated 12 summary scores including: orientation, tolerance of handling, quality of movement, self-regulation, nonoptimal reflexes, stress signs, arousal, hypertonia, hypotonia, asymmetry, excitability, and lethargy. Summary scores ranged from 0 to 13. Higher summary scores signified more types of neurobehavioral functions observed during the evaluation; lower scores, represented less types of neurobehavioral function observed.
Infant Weight:
Infant daily weights were collected at 30 weeks PMA and 35 weeks PMA. Daily weights were obtained on the night shift using the in-bed scale of the Giraffe Incubator (GE Healthcare, Laurel, MD) and, once the infant was in a crib, the Pediatric/Infant Scale-Tronix scale was used (White Plains, NY). These scales are regularly calibrated in line with the manufacturer’s standards and two nurses confirmed each weight for accuracy. Weight data were extracted from the infant’s electronic medical record (EMR) and compared to assess a difference in growth velocity between the two groups.
Infant Physiological Measures:
HR, RR, and SaO2 were measured continuously beginning 5 minutes before, during, and up to 10 minutes after the intervention. The HR, RR, and SaO2 measures were obtained via an IntelliVue MP70 patient monitor (Philips, Andover, MA) and Nellcor pulse oximeter (Nellcor Puritan Bennett, Inc, Pleasanton, CA) and confirmed by a member of the research team who separately tracked each physiological response.
Infant Behavioral State (IBS):
Twelve categories of infant behavioral state (e.g., quiet sleep, irregular sleep, active sleep, very active sleep, drowsy, alert inactivity, quiet awake, active, very active, fussing, crying, and hard crying) were measured using the Anderson Behavioral State Scale.18 The ABSS allows for classification of behavior into states from sleep to awake to crying. Rules for scoring as outlined by the originators were followed. Infant behavioral state was assessed and documented at baseline and every minute throughout the entire data collection period by an expert member of the research team. Prior to data collection, a second member of the research team independently judged behavioral states to ensure reliability. Inter-rater reliability was assured at a level > 95% throughout the study. State scores were recorded directly onto the ABSS and scores were entered into SPSS 18 software for later analyses.
Statistical Analysis
All data were analyzed using the SPSS 18 software (SPSS Inc, Chicago, Illinois). Descriptive statistics were used to describe infant characteristics, NNNS summary scores, and physiological and behavioral state scores. Due to the small sample size, non-parametric statistics were used. Mann-Whitney U statistical techniques were used to determine the equivalency of the two groups’ baseline characteristics at birth and at 30 weeks PMA (immediately prior to the intervention) and to determine differences between the two groups in NNNS summary scores and infant weights pre-and post-intervention. A level of significance at 0.05 was used for the statistical tests (2-tailed).
Physiological (HR, RR, O2 Saturations) and behavioral state (ABSS) data were collected continuously on the experimental group only and the data were averaged at baseline and during the M Technique at 1-minute intervals and then at 5 minutes and 10 minutes following the intervention at 3 different time points (beginning, midway and at the end of 5 weeks) to examine the cumulative effect of the M Technique over time. Due to the small sample size and insufficient degrees of freedom at the 3 different time points (30, 32, and 34 weeks PMA) for each infant, a typical RMANOVA could not be conducted. However, the 3 time points all had the same trend toward physiological and behavioral state stability and there were no differences between HR, RR, Sa02, and the ABSS for each infant between the 3 time points. Therefore, HR, RR, SaO2, and the ABSS at the 3 different time points were treated as independent measurements and the RMANOVA with a Greenhouse-Geisser correction was performed. Due to the advanced statistical methods of this analysis, an additional SAS mixed model statistical analysis was performed to confirm these results.29 Additional descriptive statistics were performed and graphs and figures were developed to provide visual illustration of trends over time.
Results
Infant Characteristics
Of the 20 infants enrolled in the study, one infant died prior to the data collection period (before 30 weeks PMA) and one infant developed necrotizing enterocolitis (NEC) with perforation of the gastrointestinal tract requiring emergency surgery and was withdrawn from the study. Therefore, data from a total of 18 infants (9 infants in each of the treatment and control groups) were analyzed for this study (Tables 1 & 2). Of the 18 infants, none of them exhibited signs of persistent physiologic or behavioral distress during the M Technique period; therefore, it was not necessary to discontinue the technique before the end of the 7-minute period.
Table 1.
| M Technique Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|
| Infant Characteristics | Mean | SE | Range | Mean | SE | Range | Significance 2-Tailedb |
|
| |||||||
| Birthweight, g | 970 | 71 | 630–1190 | 932 | 56 | 630–1250 | 0.72 |
| Gestational age, wk | 26.7 | 0.44 | 26–29 | 26.6 | 0.35 | 26–29 | 0.78 |
| Apgar score 1 min | 3.9 | 0.9 | 1–8 | 4.2 | 0.8 | 1–8 | 0.69 |
| Apgar score 5 min | 5.1 | 0.70 | 2–8 | 5.7 | 0.6 | 4–9 | 0.66 |
| CRIB II score | 5.1 | 1.4 | 1–13 | 3.6 | 1.3 | 1–12 | 0.30 |
| Genderc | Frequency (%) | Frequency (%) | |||||
| Male | 4 (44.4) | 6 (66.7) | |||||
| Female | 5 (55.6) | 3 (33.3) | |||||
| Racec | |||||||
| Black | 4 (44.4) | 4 (44.4) | |||||
| White | 5 (55.6) | 5 (55.6) | |||||
Note: SE=Standard Error of Mean. Wk=weeks. Min=Minute.
Infant characteristics between the M Technique and control groups were comparable.
Mann-Whitney U
Descriptive statistics of infant gender and race between the M Technique and control groups.
Table 2.
Descriptive-Categorical Variables of Participants at 30 weeks PMA (day 1 of study)
| Infant Characteristics | M Technique Group Frequency (%) | Control Group Frequency (%) |
|---|---|---|
|
| ||
| Assisted Ventilation | ||
| NC | 0 (0.0) | 1 (11.1) |
| HHNC | 4 (44.4) | 3 (33.3) |
| CPAP | 2 (22.2) | 1 (11.1) |
| SiPAP | 3 (33.3) | 3 (33.3) |
| Vent | 0 (0.0) | 1 (11.1) |
| Supplemental Oxygen | ||
| Yes | 8 (88.9) | 6 (66.7) |
| No | 1 (11.1) | 3 (33.3) |
| Patient Room Design | ||
| Single | 5 (55.6) | 6 (66.7) |
| Open Bay | 4 (44.4) | 3 (33.3) |
| Caffeine | ||
| Yes | 9 (100.0) | 9 (100.0) |
| No | 0 (0.0) | 0 (0.0) |
Note: NC=Nasal Cannula HHNC=High Humidity Nasal Cannula. CPAP=Continuous Positive Airway Pressure. SiPAP=Bi-level Continuous Positive Airway Pressure Vent=Ventilator.
Statistical differences not calculated because of categorical data.
There were no differences among the experimental and control groups in terms of birth weight, GA, clinical risk index for babies (CRIB)30 acuity score, and 1-minute and 5-minute Apgar scores. The majority of infants in both groups were white (55.6%), receiving caffeine (100%), and receiving assisted ventilation (100%). There were more females (55.6%) in the treatment group compared to males (66.7%) in the control group.
Neurobehavioral Outcome at 35 Weeks PMA
The results of the Mann-Whitney U analysis summarized in Table 3 did not reveal a significant difference in the 12 NNNS summary scores between the M Technique group and the non M Technique group. These neurobehavioral results do not support our working hypothesis for specific aim one.
Table 3.
Comparison of the Study Cohort NNNS Summary Scores at Term Equivalent
| Summary score | M Technique Group Meana (SE) | Control Group Meana (SE) | Significance 2-Tailedb |
|---|---|---|---|
|
| |||
| Attention | 3.32 (0.25) | 3.63 (0.49) | 0.83 |
| Handling | 0.61 (0.33) | 0.70 (0.06) | 0.25 |
| Quality of Movement | 3.14 (0.22) | 3.96 (0.37) | 0.08 |
| Regulation | 4.33 (0.24) | 4.05 (0.54) | 0.96 |
| Nonoptimal reflexes | 7.44 (0.84) | 7.33 (0.41) | 0.89 |
| Asymmetric reflexes | 2.89 (0.48) | 2.33 (0.53) | 0.36 |
| Stress abstinence | 0.37 (0.02) | 0.31 (0.03) | 0.17 |
| Arousal | 3.78 (0.32) | 3.06 (0.26) | 0.11 |
| Hypertonicity | 1.00 (0.33) | 1.33 (0.47) | 0.71 |
| Hypotonicity | 1.00 (0.29) | 0.56 (0.24) | 0.26 |
| Excitability | 4.89 (0.82) | 3.78 (0.81) | 0.37 |
| Lethargy | 5.78 (1.19) | 8.78 (0.88) | 0.10 |
Descriptive Statistics
Mann-Whitney U
Growth Velocity
The results of the Mann-Whitney U analysis summarized in Table 4 did not reveal a significant difference between the two groups at baseline (30 weeks PMA) (p = 0.790) and after the 5-week intervention at 35 weeks PMA (p = 0.171). However, a significant difference in body weight gain over the 5-week period was seen in the intervention group (1,163g +65g) compared to the control group (949g +43g) (p = 0.005). This almost 200g difference in body weight is a robust indication of enhanced growth velocity in infants born very preterm receiving the M Technique intervention which supports our working hypothesis for specific aim one.
Table 4.
Infant Weights Between the 2 groups at 30 weeks PMA (day 1 of study) and 35 weeks PMA (completion of study).
| Timepoints | M Technique Group Meana (SE/Range) | Control Group Meana (SE/Range) | Significance 2-Tailedb |
|---|---|---|---|
|
| |||
| Weight at 30 wk PMA, g. | 1171.67 (68.35/790–1470) | 1158.33 (46.44/910–1320) | 0.79 |
| Weight at 35 wk PMA, g. | 2335.00 (125.11/1780–3010) | 2107.44 (65.08/1830–2362) | 0.17 |
|
| |||
| Difference in weight from 30 weeks to 35 weeks PMA | 1163.33 (64.67/990–1540) | 949.11 (42.53/760–1202) | 0.005 |
Note: Wk=Weeks. PMA=Postmenstrual Age. SE=Standard Error of Mean.
Descriptive Statistics
Mann-Whitney U
Physiological Responses
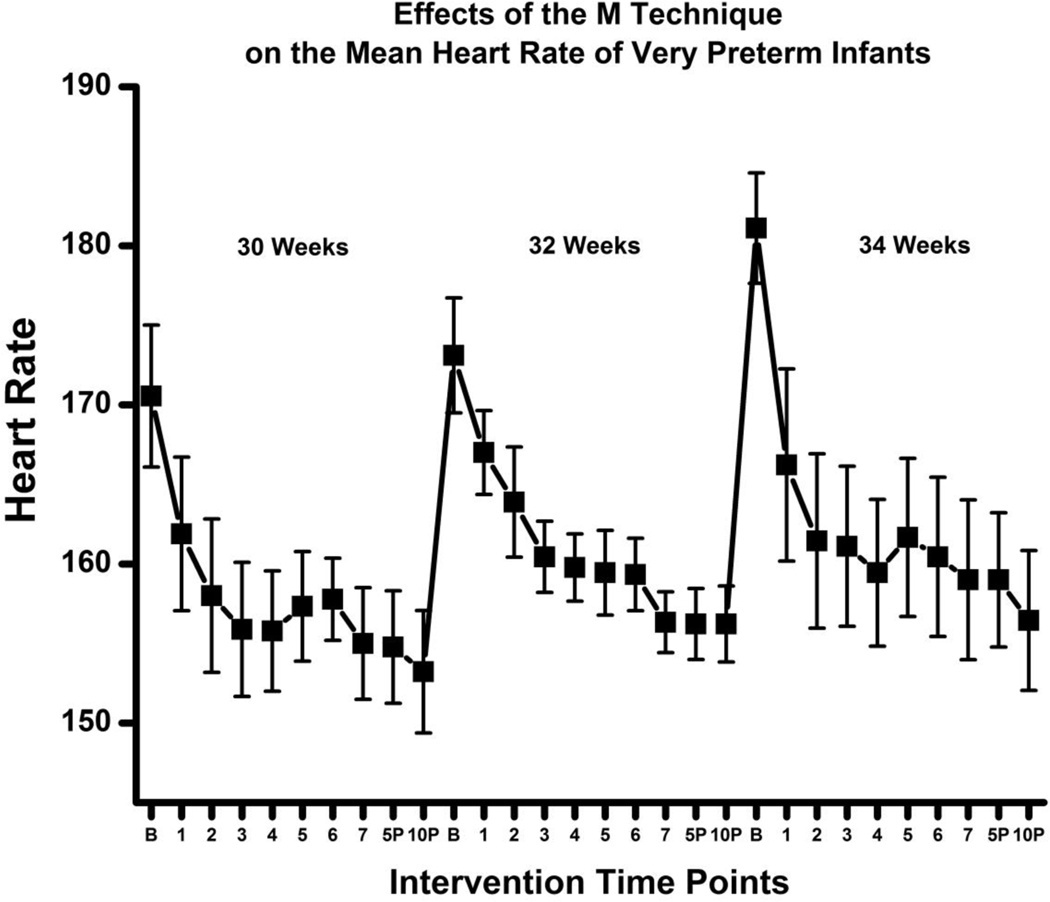
HR, RR, and SaO2 at the 3 different time points were treated as independent measurements and the RMANOVA with a Greenhouse-Geisser correction determined that mean HR, RR, and SaO2 differed significantly between from baseline to 10 minutes post the M Technique intervention (F = 41.116, p < 0.0005). These results were also confirmed after accounting for the repeated measurements from the 3 time periods (30, 32, and 34 weeks PMA) with the SAS mixed model statistical analysis.29 We can conclude that the M Technique elicits a statistically significant reduction in HR and RR and an increase in Sa02 over time, from baseline to 10 minutes post-intervention delivery, suggesting an improved physiologic stability in these high-risk infants born very preterm.
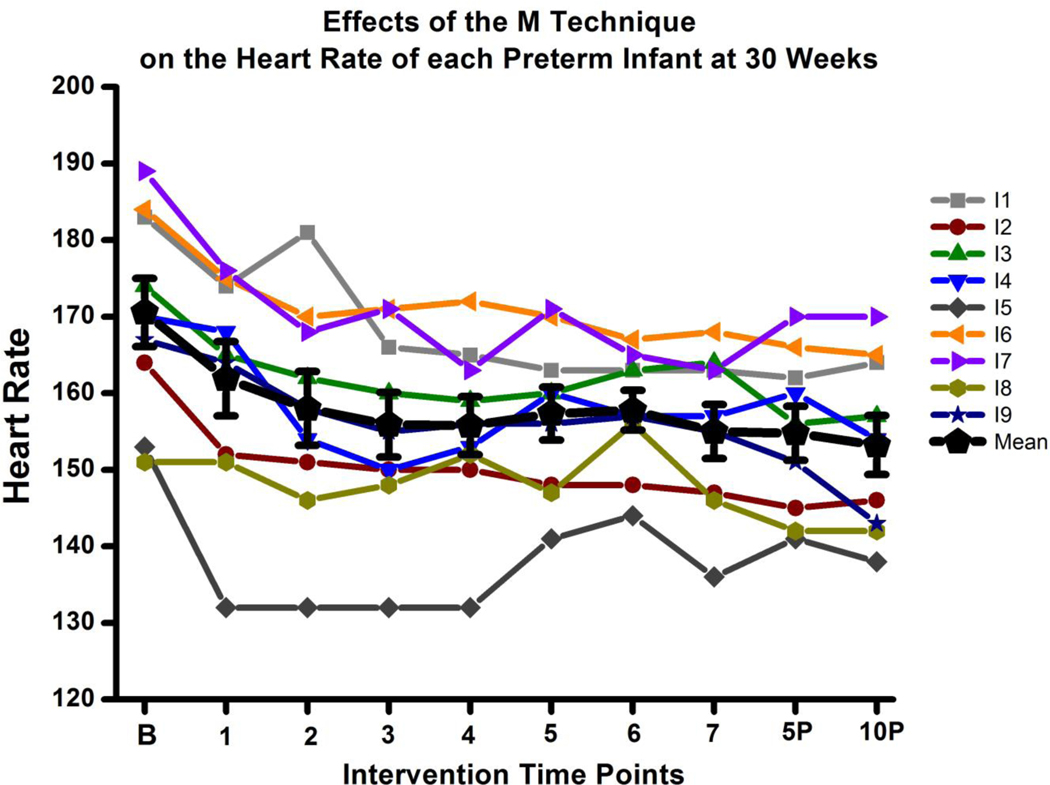
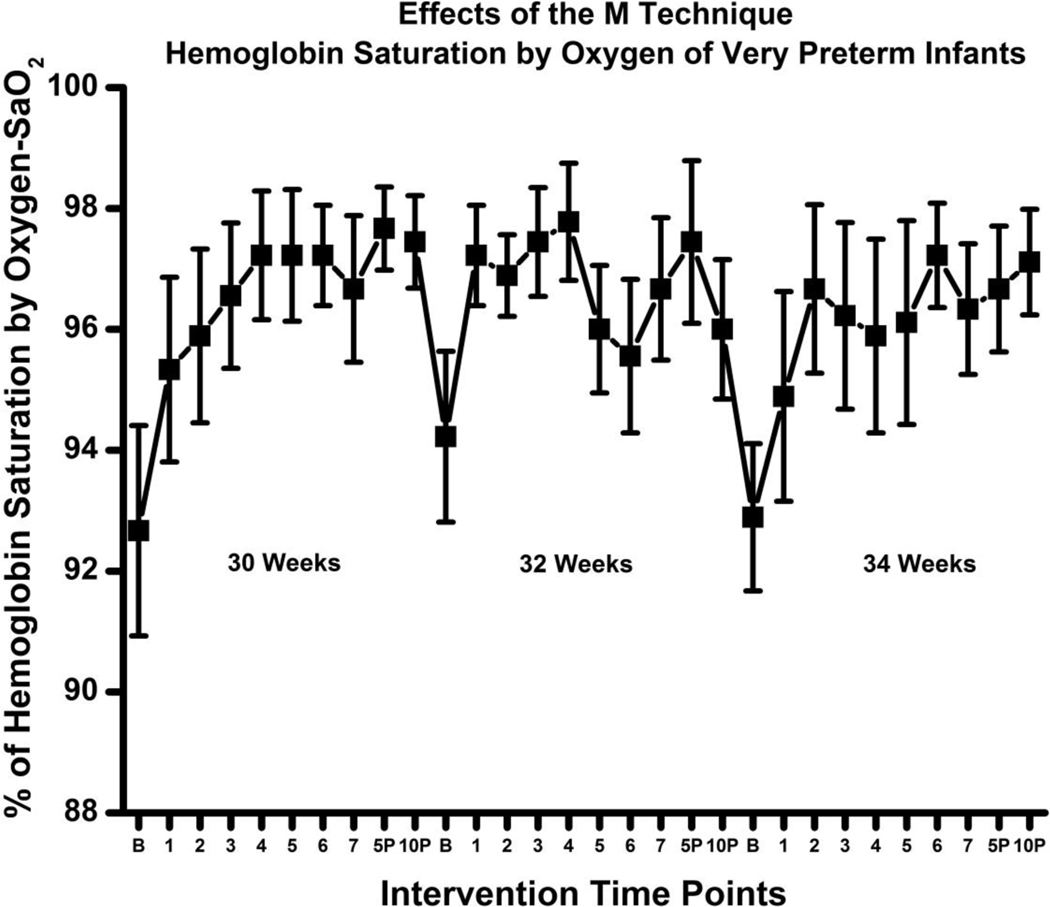
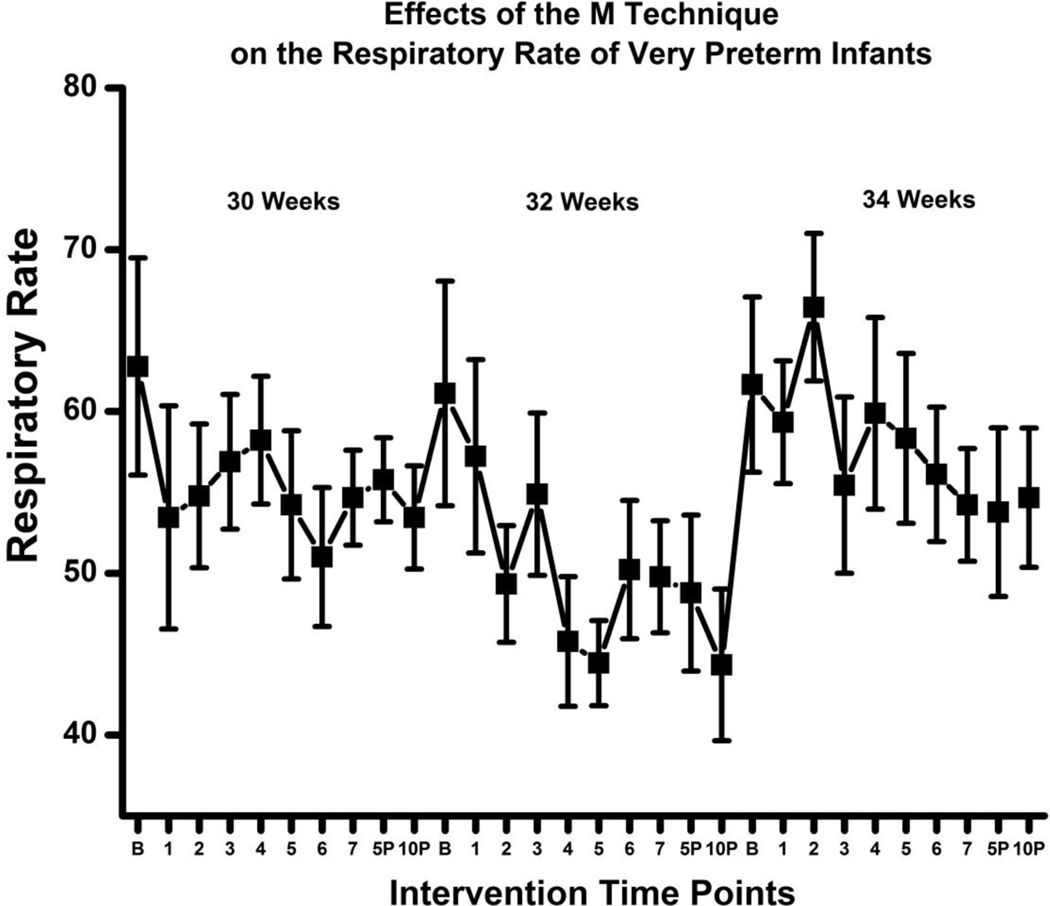
These physiologic changes over time are well illustrated in figures 2 – 5. Figure 2 provides a visual snapshot of each infant’s heart rate at 30 weeks PMA at each experimental time point controlled during these studies. The red line represents the group HR mean +/− standard errors (SE). Figures 3 – 5 illustrate the group HR, RR, and SaO2 means (+/− SE) over the 3 different time points for the treatment group at baseline and during the M Technique at 1-minute intervals and then at 5 minutes and 10 minutes after the M Technique. HR and RR progressively decreased throughout and up to 10 minutes following the M Technique intervention (Figures 3 – 4). Oxygen saturations increased over the course of the intervention and up to 10 minutes following the M Technique intervention (Figure 5).
Figure 2.
Line graph showing experimental subjects’ heart rate (HR) from baseline to 10 minutes post intervention at 30 weeks PMA. The black line indicates the group mean heart rate and standard error (SE) over time and clearly depicts the reduction of HR over time.
Figure 5.
Line graph showing shows the mean hemoglobin oxygen saturation percentage (SaO2 +/− SE) for experimental subjects from baseline to 10 minutes post intervention at 30, 32, and 34 weeks PMA making evident the increase in mean SaO2 over time at each PMA studied.
Figure 3.
Line graph shows the mean heart rate (HR +/− SE) for experimental subjects from baseline to 10 minutes post intervention at 30, 32, and 34 weeks PMA making evident the decrease in mean HR over time at each PMA studied.
Figure 4.
Line graph showing shows the mean respiratory rate (RR +/− SE) for experimental subjects from baseline to 10 minutes post intervention at 30, 32, and 34 weeks PMA making evident the decrease in mean RR over time at each PMA studied.
Behavioral State Responses
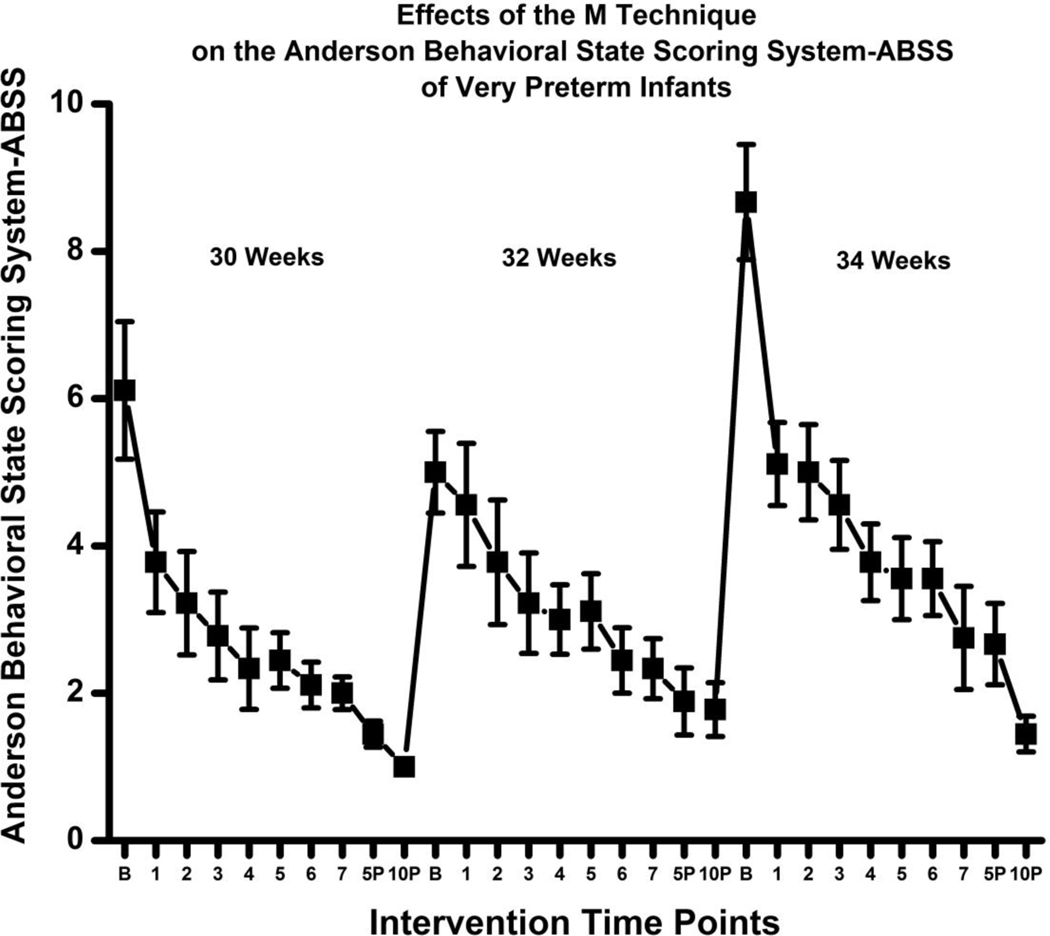
The majority of infants were in a drowsy to an active awake state at baseline with few crying at all 3 time points (Range = 3–11). None of the infants were awakened from a quiet sleep state to initiate the M Technique therapy. For the ABSS scoring the higher the behavioral state score, the more active the infant. The average behavioral state score decreased from baseline (Mean = 6.11) at all three time points resulting in infants being in a predominately quiet sleep state (Mean = 1.40) at completion through 10 minutes following the M Technique session.
The ABSS scores at the 3 different time points (30, 32, and 34 weeks PMA) were treated as independent measurements and the RMANOVA with a Greenhouse-Geisser correction determined that the mean ABSS differed significantly between time points from baseline to 10 minutes post the M Technique intervention (F = 38.564, p < 0.0005). These results were also confirmed after accounting for the repeated measurements from the three PMA periods (30, 32, and 34 weeks PMA) with the SAS mixed model statistical analysis.29 We can conclude that the M Technique elicits a statistically significant reduction in ABSS scores over time, from baseline to 10 minutes following the M Technique intervention, suggesting an improved behavioral state changes over time.
These behavioral state changes are illustrated in Figure 6 which represents the group ABSS means and SE over the 3 different time points for the treatment group at baseline and during the M Technique at 1-minute intervals and then at 5 minutes and 10 minutes after the M Technique. ABSS scores progressively decreased during, throughout and up to 10 minutes following the course of the M Technique, resulting in a more quiet sleep state.
Figure 6.
Line graph showing shows the mean Anderson Behavioral State Scoring System (ABSS +/− SE) for experimental subjects from baseline to 10 minutes post intervention at 30, 32, and 34 weeks PMA clearly illustrates the reduction in mean ABSS over time at each PMA studied.
Discussion
This study is one of the first to evaluate the effects of the M Technique on neurobehavioral development in infants born very preterm. It also demonstrates the feasibility and the potential utility of a repeated 7-minute M Technique session and the use of the NNNS in the NICU.
Very Preterm Infant Neurobehavior
Findings from this pilot study suggest a trend that multiple sessions of the M Technique do not influence neurobehavior in infants born very preterm when tested at 35 weeks PMA. Few massage or comforting touch studies have examined the effects of neurobehavioral development of high-risk, very preterm infants. The majority of touch studies examining neurobehavior have been conducted in healthy infants greater than 30 weeks GA with birth weights greater than 1,200 grams9, 31–33 and one study specifically examined cocaine exposed preterm infants.34 Similar to the present study, a recent meta-analysis concluded that neurobehavioral outcomes of these combined studies (excluding gentle human touch studies) yielded no significant differences between the massage and control groups.35 Because of the small number of studies, small sample sizes, and the heterogeneity that exists between the studies, the analysis was underpowered and the strength of the conclusion is weak. Gentle human touch (GHT) studies were not included in the meta-analysis because of the lack of evidence to support its effect on weight gain in preterm infants.35 However, consistent with the present study and the meta-analysis results, Harrison and colleagues9 did not observe a difference in the neurobehavioral subscales between the GHT and control groups.
NNNS Summary Score:
While there was a trend towards no differences observed between the treatment and control groups of this present study, this cohort of infants demonstrated less optimal neurobehavioral scores across all domains by near term equivalent which is consistent with other published NNNS mean summary scores of very preterm infants at term equivalent.23, 25–26 For example, when compared to previously reported NNNS summary scores of very preterm infant at term equivalent,23, 25 infants in this present study cohort had lower scores for attention, quality of movement, regulation, and arousal. These same infants had higher scores for handling, nonoptimal reflexes, asymmetric reflexes, stress abstinence, hypertonicity, hypotonicity, excitability and lethargy. However, it’s important to acknowledge that very preterm infants in these published reports23, 25 were evaluated closer to 40 weeks PMA (e.g., 40–44 weeks PMA) compared to this present study’s cohort at 35 weeks PMA, likely resulting in a difference in mean summary scores. According to Pineda and colleagues,26 significant changes in neurobehavior occur in the last six weeks of development, before term equivalent. Because of these rapid changes, a difference is likely to exist between infants born very preterm evaluated at near term (e.g., 35–36 weeks PMA) compared to term (e.g., 40–44 weeks PMA). This period of rapid brain growth provides a window of opportunity for health care professional to support infant development by maximizing early therapy interventions, such as occupational, physical, and speech therapies, to optimize neurodevelopment in these at-risk infants. Therefore, because of some of the trends observed in our study, it is hypothesized that if the M Technique intervention would have continued to discharge and the timing of the administration of the NNNS performed at term equivalent (40–44 weeks PMA), differences between the experimental and control groups may have reached significance and differences between this cohort and the published mean summary scores of infants born very preterm would not have differed. However, a further study is needed to validate this working hypothesis.
Growth Velocity
The effect of massage on daily weight gain in healthy preterm infants (greater than 30 weeks GA) is well reported.31–33, 36–39 However, similar to other studies examining the effects of massage on body weight in very-low-birth-weight infants (VLBW; <1500 g), our study found a trend towards no difference in body weight between the infants who received the M Technique and the control group at the end of the treatment period.15, 40 No difference in weight gain among infants born at very low birth weight has also been observed in infants who received gentle human touch and the control group.9, 12 However, unlike these studies, we did observe a trend towards a significant difference in body weight gain over the 5-week period between the two groups, infants born very preterm who received the M Technique gained more weight over time. The topic of infant nutrition is a complex phenomenon for infants born very preterm who are either VLBW or extremely-low-birth-weight (<1,000 g) (ELBW) and reside in the NICU. These infants are born at a time of rapid brain and body growth. Initiating and maintaining growth in these high-risk infants is often challenging and complicated due to their disease state. Often, growth rates lag behind resulting in extrauterine growth restriction because of their disease state, including pulmonary disease or sepsis. Due to the small sample size of this present study, it is difficult to predict or generalize these findings as it relates to growth and future research is needed with a larger sample.
Immediate Physiological Infant Response
This is the first comforting touch study to examine infant physiologic and behavioral state responses over a period of five weeks. The majority of massage or gentle human touch studies are conducted over a 5 to 10 day period. Similar to our feasibility study,16 findings from this present study suggest that infants born very preterm can tolerate an infant-driven systematic stroking touch method, the M Technique, that promotes physiologic stability and indications of relaxation. No studies have examined immediate physiologic responses in very preterm infants as a result of providing a 7-minute structured touch of stroking over a 5-week period. The majority of studies have examined slightly older gestational age infants and their response to gentle human touch (e.g., still touch, containment, no stroking) with the main outcomes resulting in no significant difference in oxygen saturation or heart rate before, during or after the intervention indicating no adverse effect.9, 12 These studies support the notion that gentle human touch for preterm infants does not cause changes in heart rate and oxygen saturation. However, in a larger randomized controlled trial, Harrison and colleagues10 reported a decrease in oxygen saturations across the 3 phases of GHT at baseline, during, and after the intervention and 19% of the infants in the GHT group had to have 1 or more GHT sessions terminated early because of a decrease in HR or a decrease in oxygen saturations. Preterm infants who received GHT and had decreased oxygen saturations were those infants who were lower in gestational age (GA range between 27 – 33 weeks) and birth weight (BW range between 796–1998 grams) and had higher morbidity levels (morbidity range not reported) than the infants who did not require early termination of the GHT sessions, suggesting the need for caution and close monitoring in these very small infants.10 This decrease in oxygen saturation did not occur in the present study, on the contrary, oxygen saturation improved under our experimental conditions.
Two studies have examined the immediate physiologic effects of the Touch and caressing-tender in caring (TAC-TIC) therapy, a systematic, sequence of stroking in ventilated very preterm infants.13–14 Intubated very preterm infants received a 3 to 4 minutes of systematic, sequenced stroking all over the body for an average of seven to nine sessions. Similar to our findings, de Roiste & Bushnell14 demonstrated a significant decrease in heart rate from the “during-to-after” stroking intervention but unlike our findings, these investigators did not observe a significant decrease in heart rate from “before-to-during” or “before-to-after” stroking intervention.14 In addition, these infants’ respiratory rates increased significantly from the “during to after” phases but no differences were found across the “before to during” and the “before to after” phases. These respiratory rate findings are different from the present study findings, which demonstrated a decrease in respiratory rates from baseline, during, and post M Technique intervention delivery. Both TAC-TIC therapy studies13–14 measured infants’ transcutaneous arterial oxygen tension (TcPO2) and found no difference in TcPO2 in any of the before, during, or after phases. These investigators also conclude that no change in TcPO2 indicates that this method of touch can be delivered without adverse effects and the unlikelihood of exacerbating infant distress.
The results of the present pilot study clearly suggest that the M Technique has positive immediate physiologic effects from baseline through 10 minutes post intervention, suggesting a relaxing and soothing effect, which is different from the aforementioned studies. Whether or not these positive physiologic responses have long-term implications needs further investigation.
Immediate Infant Behavioral State Response
To our knowledge, no infant massage or M Technique studies (except for our feasibility study) 16 have examined behavioral state outcomes in this population of infants born very preterm who receive the intervention beginning at 30 weeks PMA. Studies that have examined the immediate behavioral response to touch are restricted to gentle human touch, which include infants born at slightly older gestational ages and do not receive moderate pressure stroking.9–12 Similar to the GHT studies, infants in the present study had decreased levels of active sleep and motor activity during the touch intervention, however, these differences were significant in the present study from baseline up to 10 minutes following the M Technique intervention. In addition, infants in the present study also demonstrated consistent trends of increased periods of quiet sleep from baseline, during, and post-M Technique intervention which is different from the GHT studies that did not observe a significant increase in quiet sleep during this same time period.9–10, 12
Consistent with our feasibility study,16 infants born very preterm receiving the M Technique demonstrated positive ABSS scores over time suggesting a more quiet sleep state during and following the M Technique sessions. However, unlike our feasibility study, infants born very preterm in the present study received 30 applications of M Technique intervention over the course of 5 weeks, versus once in the feasibility study, and the behavioral state scores remained consistently low during and following the interventions. These study results suggest that a 7-minute infant-driven M Technique intervention can be delivered multiple times to hospitalized infants born very preterm beginning at 30 weeks PMA.
Conclusion
This RCT pilot study is one of the first to examine and support the cumulative effect of an infant-driven M Technique intervention that incorporates a series of stroking movements performed using a set pressure, sequence, and repetition in hospitalized infants born very preterm over a five-week period starting at 30 weeks PMA. Findings from this study build upon the science of touch for infants born very preterm and are important because much of the care delivered to this high-risk population includes minimal stimulation, resulting in limited comforting touch stimulation.6 This study demonstrates the utility and feasibility of multiple M Technique applications in high-risk infants in a level IV NICU beginning at 30 weeks PMA with notable evidence of positive physiological and behavioral state impact. These results indicate positive trends towards hospitalized very preterm infants being able to tolerate an infant-driven systematic stroking method of touch resulting in soothing or relaxing effects. Although no differences were found between the M Technique and control groups on neurobehavior, this study supports that the M Technique intervention does not adversely affect these at-risk infants and was deemed appropriate and beneficial for this small sample. Many infant massage protocols incorporate a 15–20 minute massage intervention (including kinesthetic activity), this study demonstrates that positive physiological and behavioral state changes occurred after only 7 minutes of the M Technique intervention, resulting in a lesser need of time commitment and effort by caregivers.
Limitations
The small sample size of this study limits the ability to generalize the findings. Our study was based on a practical, but relative small sample size of 9 infants per group, which may mask some of the additional differences that could exist between different groups of infants subjected or not to the M Technique intervention. Larger, well-designed studies with long-term follow-up are needed to examine the routine application of the M Technique in infants born very preterm. Only 2 ethnic groups were represented in this study with the majority being Caucasian. Since this was a small pilot study, it was important to obtain as homogenous a sample as possible to best detect between-group differences. For future studies, it will be important to compare the effects of the M Technique across the different races as such studies may offer insights into genetic influences on the response to touch therapy. We did not account for the neurodevelopmental support that’s part of this NICU’s standard of care (e.g., the number of skin-to-skin care sessions, the quantity or quality of parent-infant interactions, and the number of parent- or therapy-delivered massages). We believe that denying infants of these developmental- and family-centered care supportive strategies would be unethical.
Further, we did not account for the alterations in brain structure or white matter injury that are more accurately detected by MRI than cranial ultrasound, that may further explain poor neurobehavioral outcomes in the very preterm infant at term.41–42 We also did not account for perinatal (e.g., antenatal steroids) or neonatal factors (e.g., gender [even though both groups were well-matched] or disease state) that may have influenced neurobehavioral and growth velocity outcomes.
Although pilot studies may have a number of limitations, including small sample sizes, well constructed, a priori, pilot studies can inform investigators about the research process.43 Pilot studies include small sample sizes by design and are developed to test a novel concept or research method with the intent of conducting a larger, full-scale study to build upon the science.44–45 Given the at-risk population of this study, strong consideration of the sample size was important in order to balance between having a large enough sample to provide direction for next studies (e.g., establishing effect size) and small enough to expose unnecessary risks to a vulnerable population.45–46
Recommendations for Future Research
Future research with a larger diverse sample is needed to replicate these findings and to further evaluate the efficacy the M Technique intervention among hospitalized very preterm infants. In addition, a well constructed, RCT, should be designed to evaluate both short- and long-term effects of the M Technique as it relates to brain growth, neurobehavioral development, and stress reduction. To date, only one RCT trial has examined the long-term neurodevelopmental impact of massage and skin-to-skin care on infants born very preterm at two years of age.47 More research is needed to determine if this improved neurodevelopment is continued past 2 years of age and if the same effect can be seen with very preterm infants who receive the M Technique soon after birth through discharge.
Future research is also needed to evaluate the effectiveness of parent-delivered M Technique session and the potential impact on parent mental and emotional health and parent-infant synchrony. These future research studies should incorporate a modifiable infant-driven M Technique protocol starting prior to 30 weeks PMA to determine timing, duration, and frequency.
Ultimately, this pilot study design supports the need to further test this novel comforting touch intervention in a full-scale RCT. It is our goal that the next phase of study will be fruitful and foster new transformational knowledge that will be applied to the lives of infants born very preterm and their families.
Clinical Implications
Although no generalization can be applied from this small pilot study, these findings demonstrate that neonatal health care professionals can apply a potentially cost-effective, infant-driven comforting touch strategy, the M Technique, aimed at reducing stress and optimizing the sensory experience of very preterm infants. More importantly, neonatal health care professionals can teach parents to deliver the M Technique, which could ultimately have infant, parent, and infant-parent dyad implications.
Acknowledgements:
We thank Mary Raney, NNP-BC, Patricia Coffelt, MOT, OTR/L, and Sandy Conner, BS, PT, for actively participating in patient enrollment, intervention delivery and/or data collection. In addition, we thank the developer of the M Technique, Jane Buckle, PhD, RN, statistician An-Lin Cheng, PhD, from the University of Missouri Kansas City, School of Nursing, and the NICU families and staff for their willingness to participate.
Funding: Supported in part by the National Association of Neonatal Nurses Small Grants Award and St. Louis Children’s Hospital Foundation.
References
- 1.Montague A. Touching: The human significance of the skin. 1986. (3rd edition); Harper Row, Pulibhsers, Inc. NY. [Google Scholar]
- 2.Browne JV. Considerations for touch and massage in the neonatal intensive care unit. Neonatal Netw. 2000;19:61–4. [DOI] [PubMed] [Google Scholar]
- 3.Hertenstein MJ, Verkamp JM, Kerestes AM, Holmes RM. The communicative functions of touch in humans, nonhuman primates, and rats: a review and synthesis of the empirical research. Genet Soc Gen Psychol Monogr. 2006;132:35–42. [DOI] [PubMed] [Google Scholar]
- 4.Evans JC. Incidence of hypoxemia associated with caregiving in premature infants. Neonatal Netw. 1991;10:17–24. [PubMed] [Google Scholar]
- 5.Harrison LL. Tactile stimulation of neonatal intensive care unit preterm infants. In: Field T, ed. Touch and Massage in Early Child Development. San Francisco, CA: JJPI; 2004:139–161. [Google Scholar]
- 6.Smith JR. Comforting touch in the very preterm hospitalized infant: An integrative review. Adv Neonatal Care. 2012;12(6):349–365. doi: 10.1097/ANC.0b013e31826093ee [DOI] [PubMed] [Google Scholar]
- 7.Whitely JA, Rich BL. A double-blind randomized controlled pilot trial examining the safety and efficacy of therapeutic touch in premature infants. Adv Neonatal Care. 2008;8:315–333. [DOI] [PubMed] [Google Scholar]
- 8.Jay SS. The effects of gentle human touch on mechanically ventilated very short gestation infants. Matern Child Nurs J. 1982;11:199–259. [PubMed] [Google Scholar]
- 9.Harrison L, Olivet L, Cunningham K, Bodin MB, Hicks C. Effects of gentle human touch on preterm infants: pilot study results. Neonatal Netw. 1996;15:35–42. [PubMed] [Google Scholar]
- 10.Harrison L, Williams AK, Berbaum ML, Stem JT, Leeper J. Physiologic and behavioral effects of gentle human touch on preterm infants. Res Nurs Health. 2000;23:435–446. [DOI] [PubMed] [Google Scholar]
- 11.Harrison L, Williams AK, Berbaum ML, Stem JT, Leeper J. Effects of developmental, health status, behavioral, and environmental variables on preterm infants’ responses to a gentle human touch intervention. Int J Prenatal Perinatal Psychol Med. 2000;12:109–122. [Google Scholar]
- 12.Modrcin-Talbott MA, Harrison LL, Groer MW, Younger MS. The biobehavioral effects of gentle human touch on preterm infants. Nurs Sci Q. 2003;16:60–67. [DOI] [PubMed] [Google Scholar]
- 13.Adamson-Macedo EN, de Roiste A, Wilson A, de Carvalho FA, Dattani I. TAC-TIC therapy with high-risk, distressed, ventilated preterms. J Reprod Infant Psychol. 1994;12:249–252. [Google Scholar]
- 14.de Roiste A, Bushnell I. Cardiorespiratory and transcutaneous oxygen monitoring of high-risk preterms receiving systematic stroking. Int J Prenatal Perinatal Psychol Med. 2000;12:89–95. [Google Scholar]
- 15.Mendes EW, Procianoy RS. Massage therapy reduces hospital stay and occurrence of late-onset sepsis in very preterm neonates. J Perinatol. 2008;28(12):815–820. doi: 10.1038/jp.2008.108 [DOI] [PubMed] [Google Scholar]
- 16.Smith JR, Raney R, Conner S, Coffelt P, McGrath J, Brotto M, Inder T. (2012). Application of the M technique in hospitalized very preterm infants: A feasibility study. Adv Neonatal Care. 2012;12(5S):S10–S17. [DOI] [PubMed] [Google Scholar]
- 17.Lester BM, Tronick EZ, Brazelton B. (2004). The Neonatal Intensive Care Unit Network Neurobehavioral Scale procedures. Pediatr. 2004;113:641–667. [PubMed] [Google Scholar]
- 18.Gill NE, Behnke M, Conlon M, McNeely JB, Anderson GC. Effect of nonnutritive sucking on behavioral state in preterm infants before feeding. Nurs Res. 1988;37:347–50. [PubMed] [Google Scholar]
- 19.Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med 2010;152. [PMC free article] [PubMed] [Google Scholar]
- 20.de Jong M, Lucas C, Bredero H, van Adrichem L, Tibboel D, van Dijk M. Does postoperative “M” technique massage with or without mandarin oil reduce infants’ distress after major craniofacial surgery? J Adv Nurs. 2012;68:1748–1757. doi: 10.1111/j.1365-2648.2011.05861.x. [DOI] [PubMed] [Google Scholar]
- 21.Doig GS, Simpson F. Randomization and allocation concealment: A practical guide for researchers. J Crit Care. 2005;20(2):187–189. 10.1016/j.jcrc.2005.05.002 [DOI] [PubMed] [Google Scholar]
- 22.Viera AJ, Bangdiwala SI. Eliminating bias in randomized controlled trials: Importance of allocation concealment and masking. Fam Med. 2007;39(2):132–137. [PubMed] [Google Scholar]
- 23.Brown NC, Doyle LW, Bear MJ, Inder TE. Alterations in neurobehavior at term reflect differing perinatal exposures in very preterm infants. Pediatr. 2006;118(6):2461–2471. doi: 10.1542/peds.2006-0880 [DOI] [PubMed] [Google Scholar]
- 24.Sullivan MC, Miller RJ, Fontaine LA, Lester B. Refining neurobehavioral assessment of the high-risk infant using the NICU Network Neurobehavioral Scale. JOGNN. 2012;41(1):17–23. doi: 10.1111/j.1552-6909.2011.01322 [DOI] [PubMed] [Google Scholar]
- 25.El-Dib M, Massaro AN, Glass P, Aly H. Neurobehavioral assessment as a predictor of neurodevelopmental outcome in preterm infants. J Perinatol. 2012; 32(4):299–303. doi: 10.1038/jp.2011.100 [DOI] [PubMed] [Google Scholar]
- 26.Pineda RG, Tjoeng TH, Vavasseur C, Kidokoro H, Neil JJ, Inder T. Patterns of altered neurobehavior in preterm infants within the neonatal intensive care unit. J Pediatr. 2012;162(3):470–476. doi: 10.1016/j.jpeds.2012.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stephens BE, Liu J, Lester B, Lagasse L, Shankaran S, Bada H, … Higgins R. Neurobehavioral assessment predicts motor outcome in preterm infants. J Pediatr. 2010; 156:366–371. doi: 10.1016/j.jpeds.2009.09.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu J, Bann C, Lester B, Tronick E, Das A, Lagasse L, … Bada H. Neonatal neurobehavior predicts medical and behavioral outcome. Pediatrics. 2010;125(1):90–98. doi: 10.1542/peds.2009-0204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag. 2009. [Google Scholar]
- 30.The International Neonatal Network. The CRIB (Clinical Risk Index for Babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. Lancet 1993;342 : 193–98 [PubMed] [Google Scholar]
- 31.Arora J, Kumar A, Ramji S. Effect of oil massage on growth and neurobehavior in very low birth weight preterm neonates. Indian J Pediatr. 2005;42(11):1092–1100. Retrieved from http://www.indianpediatrics.net/nov2005/1092.pdf [PubMed] [Google Scholar]
- 32.Field T, Schanberg S, Scafidi F, Bauer CR, Vega-Lahr N, Garcia R, … Kuhn CM (1986). Tactile/kinesthetic stimulation effects on preterm neonates. Pediatr. 1986;77(5):654–658. [PubMed] [Google Scholar]
- 33.Scafidi FA, Field T, Schanberg SM. Factors that predict which preterm infants benefit most form massage therapy. J Dev Behav Pediatr. 1993;14(3):176–180. [PubMed] [Google Scholar]
- 34.Wheeden A, Scafidi FA, Field T, Ironson G, Bandstra E. Massage effects on cocaine-exposed preterm neonates. J Dev Behav Pediatr. 1993;14:318–322. [PubMed] [Google Scholar]
- 35.Wang L, He JL,Zhang XH. The efficacy of massage on preterm infants: A meta-analysis. Am J Perinatol. 2013;Epub. [DOI] [PubMed] [Google Scholar]
- 36.Diego MA, Field T, Hernandez-Reif M. Vagal activity, gastric motility, and weight gain in massaged preterm neonates. J Pediatr. 2005;147(1):50–55. doi: 10.1016/j.jpeds.2005.02.023 [DOI] [PubMed] [Google Scholar]
- 37.Dieter JN, Field T, Hernandez-Reif M, Emory EK, Redzepi M. Stable preterm infants gain more weight and sleep less after five days of massagetherapy. J Pediatr Psychol. 2003;28: 403–411. doi: 10.1093/jpepsy/jsg030 [DOI] [PubMed] [Google Scholar]
- 38.Ferreira AM, Bergamasco NH. Behavioral analysis of preterm neonates included in a tactile and kinesthetic stimulation program during hospitalization. Rev Bras Fisioter. 2010;14(2):141–148. 10.1590/S1413-35552010005000002 [DOI] [PubMed] [Google Scholar]
- 39.Gonzalez AP, Vasquez-Mendoza G, Garcia-Vela A, Guzman-Ramirez A, Salazar-Torres M, Romero-Gutierrez G. Weight gain in preterm infants following parent-administered Vimala massage: a randomized controlled trial. Am J Perinatol. 2009;26:247–252. [DOI] [PubMed] [Google Scholar]
- 40.Guzzetta A, Baldini S, Bancale A, et al. Massage accelerates brain development and the maturation of visual function. J Neurosci. 2009;29:6042–6051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Inder TE, Warfield SK, Wang H, Huppi PS, Volpe JJ. Abnormal cerebral structure is present at term in premature infants. Pediatr. 2005;115(2):286–294. Doi: 10.1542/peds.2004-0326 [DOI] [PubMed] [Google Scholar]
- 42.Inder TE, Anderson NJ, Spencer C, Wells S, Volpe JJ. White matter injury in the premature infant: a comparison between serial cranial sonographic and MR findings at term. AJNR Am J Neuroradiol. 2003;24(5):805–809. [PMC free article] [PubMed] [Google Scholar]
- 43.Teijlingen van E, Rennie AM, Hundley V, Graham W. The importance of conducting and reporting pilot studies: the example of the Scottish Births Survey. J Adv Nurs. 2001;34:289–295. [DOI] [PubMed] [Google Scholar]
- 44.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McGrath JM. Not all studies with small samples are pilot studies. J Perinat Neonatal Nurs. 2013;27(4):281–283..= doi: 10.1097/01.JPN.0000437186.01731.bc. [DOI] [PubMed] [Google Scholar]
- 46.Conn VS. Building a trajectory of research: editorial. West J Nurs Res. 2004;26(6):592–594. [DOI] [PubMed] [Google Scholar]
- 47.Procianoy RS, Mendes EW, Silveira RC. Massage therapy improves neurodevelopment outcome at two years corrected age for very low birth weight infants. Early Hum Dev. 2010;86:7–11. doi: 10.1016/j.earlhumdev.2009.12.001 [DOI] [PubMed] [Google Scholar]