Abstract
High-level quinolone resistance in Enterococcus faecium was associated with mutations in both gyrA and parC genes in 10 of 11 resistant strains. One low-level resistant strain without such mutations may instead possess an efflux mechanism or alterations in the other subunits of the gyrase or topoisomerase IV genes. These findings are similar to those for other gram-positive bacteria, such as Enterococcus faecalis.
Enterococci are important pathogens and a common cause of serious nosocomial infections such as bacteremia and endocarditis (21). Enterococcus faecalis is the most common isolate among enterococci. However, Enterococcus faecium has become increasingly important after the emergence of ampicillin and vancomycin resistance. Clinical isolates resistant to vancomycin are usually resistant to quinolones and almost all currently available antibiotics (1, 2, 10), but new fluoroquinolones may still have therapeutic value for enterococcal infections (12). At Huddinge Hospital, where this study was conducted, the frequency of quinolone-resistant enterococci has increased from 11% in 1994 to 25% in 1997.
Recent studies showed that fluoroquinolone resistance in gram-negative organisms is associated with mutations in the gyrA gene (subunit of DNA gyrase) or with a reduced accumulation of the drug (3, 9, 18, 22, 23, 29, 30). In gram-positive bacteria, fluoroquinolone resistance can be associated with mutations in the gyrA or parC (subunit of topoisomerase IV) gene (6, 7, 16, 17, 19, 26), and in some gram-positive organisms, such as Staphylococcus aureus, efflux pumps have been identified (6, 7, 13, 16, 17, 19, 26, 31).
The nucleotide sequence encoding 41 amino acids in the gyrase A protein, corresponding to Escherichia coli amino acids 67 to 106 in the GyrA protein (5, 8, 25, 27, 28), was identified in both gram-negative and gram-positive organisms as the quinolone resistance determining region.
In this study we have analyzed clinical quinolone-resistant E. faecium isolates for mutations in the genes encoding subunits of the quinolone target enzymes GyrA and ParC. Twelve clinical isolates of E. faecium, collected in different Swedish hospitals, were studied. The isolates were identified by using API 20 STREP (bioMérieux, Marcy l’Etoile, France). The MICs of ciprofloxacin and trovafloxacin were determined by using the E test (Biodisk, Solna, Sweden) on Iso-Sensitest agar (Oxoid) or, for those strains for which MICs of ciprofloxacin were ≥32 μg/ml, the agar dilution method on PDM-ASM agar (Biodisk) with 5% horse blood (4). The antibiotic susceptibilities are shown in Table 1. Of the 12 isolates, 10 were resistant (here defined as any strain for which the MIC of ciprofloxacin is >8 μg/ml), one was susceptible, and for another the MICs of both drugs were slightly higher than for the reference strain. The type strain E. faecium ATCC 19434 was used as a reference.
TABLE 1.
Alterations in gyrA and parC genes in clinical isolates of E. faceium
| ATCC strain | MIC (μg/ml)a
|
Amino acid (codon) at positionb
|
|||
|---|---|---|---|---|---|
| CIP | TRV | GyrA
|
ParC, 80 | ||
| 83 | 87 | ||||
| 19434 | 4 | 1 | Ser (AGT) | Glu (GAG) | Ser (AGC) |
| 3797 | 1 | 0.125 | |||
| 216 | 8 | 4 | |||
| 214 | 32 | 8 | Lys (AAG) | Ile (ATC) | |
| 211 | 32 | 8 | Lys (AAG) | Ile (ATC) | |
| 209 | 32 | 16 | Lys (AAG) | Ile (ATC) | |
| 210 | 256 | 8 | Lys (AAG) | Ile (ATC) | |
| 3784 | >256 | 4 | Lys (AAG) | Ile (ATC) | |
| 208 | 64 | 16 | Arg (CGT) | Ile (ATC) | |
| 221 | 256 | 32 | Ile (ATT) | Ile (ATC) | |
| 215 | 256 | 8 | Tyr (TAT) | Ile (ATC) | |
| 213 | >256 | 16 | Tyr (TAT) | Ile (ATC) | |
| 212 | >256 | 32 | Tyr (TAT) | Ile (ATC) | |
CIP, ciprofloxacin; TRV, trovafloxacin.
Positions correspond to E. coli. For those strains with no amino acid shown, the codon is identical to that of the type strain.
Genomic DNA was extracted from the 11 isolates and the type strain, by using the guanidium thiocyanate method (24). The target regions were amplified by using PCR with primers derived from E. faecalis sequences. A DNA fragment of 241 bp from the gyrA gene corresponding to the quinolone resistance determining region was amplified with the 23-mer oligonucleotide primers 5′-CGG GAT GAA CGA ATT GGG TGT GA-3′ and 5′-AAT TTT ACT CAT ACG TGC TTC GG-3′, equivalent to nucleotide positions 150 to 172 and 368 to 390 of the E. coli gyrA gene (15), respectively, and a 191-bp parC fragment was amplified with the 20-mer oligonucleotide primers 5′-AAT GAA TAA AGA TGG CAA TA-3′ and 5′-CGC CAT CCA TAC TTC CGT TG-3′ (positions 10 to 29 and 181 to 200 of the E. faecalis parC gene, respectively) (14). One-step PCR was performed for each gene in a 50-μl reaction mixture containing 1.25 U of Taq DNA polymerase, 200 μM concentrations of each deoxynucleoside triphosphate, 45 pmol of each primer, 1.5 mM MgCl2, and 10× PCR buffer (Sigma). Each reaction was run for 30 cycles with the following temperature profile: denaturation at 94°C for 1 min, annealing at 55°C for gyrA and 48.7°C for parC for 1 min, and then extension at 72°C for 1 min. The amplified fragments were processed for cycle sequencing by using the ABI PRISM Big-dye terminator kit, and sequences were then analyzed by capillary electrophoresis in an ABI PRISM 310 automated sequencer. Analysis for alteration in target position was carried out as described by Jalal and Wretlind (11).
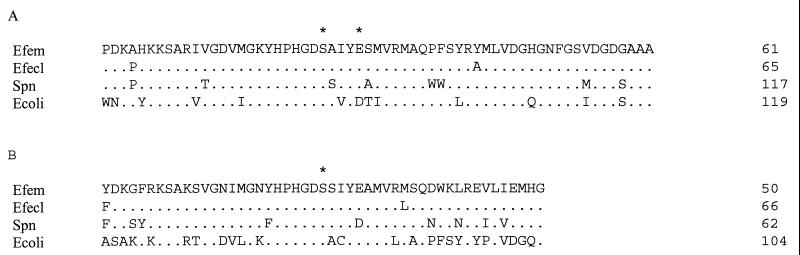
The nucleotide sequences of 195 bp of gyrA between the primers and 151 bp of parC between the primers were then determined and analyzed for alterations at the key amino acid positions. The E. faecium GyrA partial amino acid sequence showed 97, 88, and 63% identities with E. faecalis, Streptococcus pneumoniae, and E. coli, respectively. The corresponding identities for ParC were 92, 78, and 47% (Fig. 1).
FIG. 1.
E. faecium (Efem) GyrA (A) and ParC (B) partial gene sequences, compared with those of E. faecalis (Efecl), S. pneumoniae (Spn), and E. coli. The numbered amino acids start from the first amino acid in the complete sequence of E. coli and in partial sequences of the others. Only amino acids that differ from those of E. faecium are shown. Asterisks mark the mutation points.
In 10 of the strains GyrA showed single amino acid changes relative to strain ATCC 19434. The serine at position 83 (corresponding to E. coli) was changed to tyrosine in three strains, to isoleucine in one strain, and to arginine in another. At position 87, glutamate was changed to lysine in five isolates. In the parC gene, a single amino acid change was encoded, the serine at position 80 (corresponding to E. coli) to isoleucine in 10 strains (Table 1). One susceptible strain and one strain for which the MIC of ciprofloxacin was 8 μg/ml and that of trovafloxacin was 4 μg/ml had no alterations in gyrA or parC.
Two nucleotide substitutions were needed for the alteration of serine (AGT) to tyrosine (TAT). One possible explanation is that the parent strains had serine (TCT) in this position. Kanematsu et al. (14) found similar mutations with two nucleotide changes in E. faecalis at position 80 of the parC gene, where serine (AGT) was changed to arginine (CGC) in one strain and to isoleucine (ATC) in nine strains. Some of the strains in this study showed the same mutations in both gyrA and parC despite the fourfold difference in MICs of ciprofloxacin or trovafloxacin (Table 1). The most resistant strains may also have efflux systems and/or mutations in gyrB or parE.
Kanematsu et al. (14) found similar mutations in the gyrA and parC genes of E. faecalis, associated with resistance to fluoroquinolones. They detected one strain with a substitution in parC but not in gyrA. For this strain the MIC was between the MICs for those with no mutations and those with simultaneous mutations in both gyrA and parC; consequently they suggested that parC might be the primary target for quinolones as in other gram-positive bacteria such as S. pneumoniae and S. aureus (16, 17). In a previous study, Pan and Fisher (20) showed that the quinolone primary target can differ depending on the structure of the compound. They demonstrated that parC is the primary target for ciprofloxacin, whereas gyrA is the primary target for sparfloxacin in laboratory selected mutant strains of S. pneumoniae. However, in the present study we could not determine the quinolone primary target, since we found no isolates with mutations in only one of the genes. For E. faecalis and S. pneumoniae strains with substitutions only in either parC or gyrA, the MICs of at least one of the quinolones studied were eightfold higher or more (14, 20). For the low-level resistant strain in our study the MICs of quinolones were two- to fourfold higher than that for the type strain, and the strain may carry mutations in the other subunits of gyrase and topoisomerase IV or efflux system.
Nucleotide sequence accession numbers.
The gyrA and parC partial sequences of E. faecium appear in GenBank under accession no. AF060881 and AB017811, respectively.
REFERENCES
- 1.Bonilla H F, Zarins L T, Bradley S F, Kauffman C A. Susceptibility of ciprofloxacin-resistant staphylococci and enterococci to trovafloxacin. Diagn Microbiol Infect Dis. 1996;26:17–21. doi: 10.1016/s0732-8893(96)00146-0. [DOI] [PubMed] [Google Scholar]
- 2.Clark N C, Cooksey R C, Hill B C, Swenson J M, Tenover F C. Characterization of glycopeptide-resistant enterococci from U.S. hospitals. Antimicrob Agents Chemother. 1993;37:2311–2317. doi: 10.1128/aac.37.11.2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cullen M E, Wyke A W, Kuroda R, Fisher L M. Cloning and characterization of a DNA gyrase A gene from Escherichia coli that confers clinical resistance to 4-quinolones. Antimicrob Agents Chemother. 1989;33:886–894. doi: 10.1128/aac.33.6.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ericsson H M, Sherris J C. Antibiotic sensitivity testing. Report of an international collaborative study. Acta Pathol Microbiol Scand Sect B. 1971;217(Suppl.):1–90. [PubMed] [Google Scholar]
- 5.Everett M J, Jin Y F, Ricci V, Piddock L J V. Contributions of individual mechanisms to fluoroquinolone resistance in 36 Escherichia coli strains isolated from humans and animals. Antimicrob Agents Chemother. 1996;40:2380–2386. doi: 10.1128/aac.40.10.2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrero L, Cameron B, Manse B, Lagneaux D, Crouzet J, Famechon A, Blanche F. Cloning and primary structure of Staphylococcus aureus DNA topoisomerase IV: a primary target of fluoroquinolones. Mol Microbiol. 1994;13:641–653. doi: 10.1111/j.1365-2958.1994.tb00458.x. [DOI] [PubMed] [Google Scholar]
- 7.Ferrero L, Cameron B, Crouzet J. Analysis of gyrA and grlA mutations in stepwise-selected ciprofloxacin-resistant mutants of Staphylococcus aureus. Antimicrob Agents Chemother. 1995;39:1554–1558. doi: 10.1128/aac.39.7.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guillemin I, Cambau E, Jarlier V. Sequences of conserved region in the A subunit of DNA gyrase from nine species of the genus Mycobacterium: phylogenetic analysis and implication for intrinsic susceptibility to quinolones. Antimicrob Agents Chemother. 1995;39:2145–2149. doi: 10.1128/aac.39.9.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heisig P, Schedletzky H, Falkenstein-Paul H. Mutation in the gyrA gene of a highly fluoroquinolone-resistant clinical isolate of Escherichia coli. Antimicrob Agents Chemother. 1993;37:696–701. doi: 10.1128/aac.37.4.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herrera-Insúa I, Jacques-Palaz K, Murray B E, Rakita R M. Intracellular activities of RP 59500 (quinupristin-dalfopristin) and sparfloxacin against Enterococcus faecium. Antimicrob Agents Chemother. 1996;40:886–890. doi: 10.1128/aac.40.4.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jalal S, Wretlind B. Mechanisms of quinolone resistance in clinical strains of Pseudomonas aeruginosa. Microb Drug Resist. 1998;4:257–261. doi: 10.1089/mdr.1998.4.257. [DOI] [PubMed] [Google Scholar]
- 12.Jones R N, Johnson D M, Biedenbach D J, Marshall S A. Activity of two novel fluoroquinolones (DU-6859a and DV-7751a) tested against glycopeptide-resistant enterococcal isolates. Diagn Microbiol Infect Dis. 1995;23:123–127. doi: 10.1016/0732-8893(95)00168-9. [DOI] [PubMed] [Google Scholar]
- 13.Kaatz G W, Seo S M, Ruble C A. Efflux-mediated fluoroquinolone resistance in Staphylococcus aureus. Antimicrob Agents Chemother. 1993;37:1086–1094. doi: 10.1128/aac.37.5.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanematsu E, Deguchi T, Yasuda M, Kawamura T, Nishino Y, Kawada Y. Alterations in the GyrA subunit of DNA gyrase and the ParC subunit of DNA topoisomerase IV associated with quinolone resistance in Enterococcus faecalis. Antimicrob Agents Chemother. 1998;42:433–435. doi: 10.1128/aac.42.2.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Korten V, Huang W M, Murray B E. Analysis by PCR and direct DNA sequencing of gyrA mutations associated with fluoroquinolone resistance in Enterococcus faecalis. Antimicrob Agents Chemother. 1994;38:2091–2094. doi: 10.1128/aac.38.9.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muñoz R, de la Campa A G. ParC subunit of DNA topoisomerase IV of Streptococcus pneumoniae is a primary target of fluoroquinolones and cooperates with DNA gyrase A subunit in forming resistance phenotype. Antimicrob Agents Chemother. 1996;40:2252–2257. doi: 10.1128/aac.40.10.2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng E Y, Trucksis M, Hooper D. Quinolone resistance mutations in topoisomerase IV: relationship to flqA locus and genetic evidence that topoisomerase IV is the primary target and DNA gyrase is the secondary target of fluoroquinolones in Staphylococcus aureus. Antimicrob Agents Chemother. 1996;40:1881–1888. doi: 10.1128/aac.40.8.1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oram M, Fisher L M. 4-Quinolone resistance mutations in the DNA gyrase of Escherichia coli clinical isolates identified by using the polymerase chain reaction. Antimicrob Agents Chemother. 1991;35:387–389. doi: 10.1128/aac.35.2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan X-S, Ambler J, Mehtar S, Fisher L M. Involvement of topoisomerase IV and DNA gyrase as ciprofloxacin targets in Streptococcus pneumoniae. Antimicrob Agents Chemother. 1994;40:2321–2326. doi: 10.1128/aac.40.10.2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pan X-S, Fisher L M. Targeting of DNA gyrase in Streptococcus pneumoniae by sparfloxacin: selective targeting of gyrase or topoisomerase IV by quinolones. Antimicrob Agents Chemother. 1997;41:471–474. doi: 10.1128/aac.41.2.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patterson J E, Sweeney A H, Simms M, Carley N, Mangi R, Sabetta J, Lyons R W. An analysis of 110 serious enterococcal infections. Epidemiology, antibiotic susceptibility, and outcome. Medicine. 1995;74:191–200. doi: 10.1097/00005792-199507000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Piddock L J. Mechanism of quinolone uptake into bacterial cells. J Antimicrob Chemother. 1991;27:399–403. doi: 10.1093/jac/27.4.399. [DOI] [PubMed] [Google Scholar]
- 23.Piddock L J, Griggs D J, Hall M C, Jin Y F. Ciprofloxacin resistance in clinical isolates of Salmonella typhimurium obtained from two patients. Antimicrob Agents Chemother. 1993;37:662–666. doi: 10.1128/aac.37.4.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pitcher D G, Saunders N A, Owen R J. Rapid extraction of bacterial genomic DNA with guanidium thiocyanate. Lett Appl Microbiol. 1989;8:151–156. [Google Scholar]
- 25.Takenouchi T, Ishii C, Sugawara M, Tokue Y, Ohya S. Incidence of various gyrA mutants in 451 Staphylococcus aureus strains isolated in Japan and their susceptibilities to 10 fluoroquinolones. Antimicrob Agents Chemother. 1995;39:1414–1418. doi: 10.1128/aac.39.7.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tankovic J, Perichon B, Duval J, Courvalin P. Contribution of mutations in gyrA and parC genes to fluoroquinolone resistance of mutants of Streptococcus pneumoniae obtained in vivo and in vitro. Antimicrob Agents Chemother. 1996;40:2505–2510. doi: 10.1128/aac.40.11.2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Truong Q C, Nguyen Van J-C, Shlaes D, Gutmann L, Moreau N J. A novel, double mutation in DNA gyrase A of Escherichia coli conferring resistance to quinolone antibiotics. Antimicrob Agents Chemother. 1997;41:85–90. doi: 10.1128/aac.41.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waters B, Davies J. Amino acid variation in the GyrA subunit of bacteria potentially associated with natural resistance to fluoroquinolone antibiotics. Antimicrob Agents Chemother. 1997;41:2766–2769. doi: 10.1128/aac.41.12.2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoshida H, Nakamura M, Bogaki M, Nakamura S. Proportion of DNA gyrase mutants among quinolone-resistant strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1990;34:1273–1275. doi: 10.1128/aac.34.6.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoshida H, Nakamura M, Bogaki M, Ito H, Kojima T, Hattori H, Nakamura S. Mechanism of action of quinolones against Escherichia coli DNA gyrase. Antimicrob Agents Chemother. 1993;37:839–845. doi: 10.1128/aac.37.4.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoshida H, Bogaki M, Nakamura S, Ubukata K, Konno M. Nucleotide sequence and characterization of the Staphylococcus aureus norA gene, which confers resistance to quinolones. J Bacteriol. 1990;172:6942–6949. doi: 10.1128/jb.172.12.6942-6949.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]