Abstract
In recent years, numerous studies have explored the quality of life (QoL) in those with diabetes mellitus. The aim of this scoping review was to explore the current state of knowledge on QoL and its various associated factors among people with diabetes in India. Three databases were searched (PubMed, Scopus, and Medline) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. A total of 41 articles were included in the review. The included studies were largely conducted in the Southern states and mainly investigated individuals with type 2 diabetes. The World Health Organization Quality of Life (WHOQOL-BREF) and Short Form Health Survey (SF-36) were the instruments used most often. In general, the studies showed that people with diabetes had poorer QoL than those without diabetes, and women with diabetes reported poorer QoL than men, consistent with findings across the world. However, the studies had significant methodological flaws which limit the validity and generalizability of the findings. Therefore, there is an urgent need to conduct high-quality QoL studies which are representative of all states of India as well as different types of diabetes in India in order to address this gap in the evidence.
Keywords: Diabetes, health-related quality of life, India, quality of life, scoping review
INTRODUCTION
Diabetes, a serious long-term condition, is considered one of the great global health challenges of the twenty-first century. An estimated 463 million people had diabetes in 2019, and this is expected to reach 578 million by 2030 and 700 million by 2045.[1] The countries with the highest number of adults with diabetes include China, India, and the USA.[1] Those living with diabetes are predisposed to complications such as retinopathy, neuropathy, cardiovascular disease, and diabetic foot disease. Moreover, psychological complications such as anxiety and depression are also common and impact psychosocial life and everyday functioning, contributing to poor quality of life [QoL].[2] The American Diabetes Association has classified diabetes into the following categories: 1. type 1 diabetes (T1D) “due to autoimmune beta cell destruction leading to absolute insulin deficiency” 2. type 2 diabetes (T2D) “due to progressive loss of beta-cell insulin secretion frequently on the background of insulin resistance” 3. Gestational diabetes mellitus (GDM) as “diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation” and 4. specific types of diabetes due to other causes (example- monogenic diabetes syndromes0).[3] It is important to understand the impact of each of these types of diabetes on QoL in order to achieve the best outcomes for all patients.
Quality of life (QoL)/Health-Related Quality of Life (HRQoL) and diabetes
The World Health Organisation (WHO) has defined QoL as “an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.”[4] QoL is considered an important health outcome, with good quality of life representing the ultimate therapeutic goal in chronic conditions.[5] The term was first used in medical literature in the 1960s and since then has gained considerable popularity in research and clinical practice. QoL includes four main components namely physical, psychological, social relationship, and environment.[6]
The term, “Health-Related Quality of Life (HRQoL)” is an inclusive term and is defined as the “physical, psychological and social domains of health, seen as distinct areas that are influenced by a person's experiences, beliefs, expectations, and perceptions.”[7] In the current literature, QoL and HRQoL are used interchangeably although each has its own meaning. In some definitions, HRQoL reflects health status, whereas in others it goes beyond health and encompasses concepts more consistent with QoL such as the environment.[8,9] QoL is a broader concept and covers all aspects of life, including education and social environment which reach beyond health. HRQoL, on the other hand, is used to measure self-perceived health or disease status and to understand the distinction between aspects of life related to health.[8]
QoL is decreased in patients with diabetes and becomes even worse when complications develop, or comorbidities exist.[6] Diabetes can negatively affect physical well-being in four major ways: 1) by leading to the development of long-term complications, 2) by being associated with short-term complications, 3) through the demands imposed by various treatment regimens, and 4) by affecting psychological functioning via its impact on mood.[10] For instance, persistent fatigue and tiredness can occur due to elevated blood glucose levels. Conversely, hypoglycemia (low glucose levels) symptoms can also be exhausting and discouraging.[10] Thus, both hypo- and hyperglycemia may affect the patient's overall sense of well-being. Lastly, social wellbeing is also compromised as diabetes can affect the patient's social relationships.[10]
The significant determinants shown to affect QoL among patients with diabetes include the type of diabetes, its duration, glycemic control, gender, complications, treatment regimen, and psychosocial factors.[11]
Tools used to measure QoL/HRQoL in patients with diabetes
Both generic and diabetes-specific instruments are widely used to measure the various domains of QoL. Overall, health and comorbidities are measured by generic tools, whereas diabetes-specific tools address diabetes-related aspects and the burden and impact of diabetes on an individual's lifestyle.[2] The most popular instrument used to measure general QoL is the WHO Quality of Life (WHOQoL) questionnaire. Among the diabetes-specific tools, the Diabetes Quality of Life (DQOL) and Audit of Diabetes-Dependent Quality of Life (ADDQoL) are the most popular.[12] In a recent scoping review, theme analysis of 30 diabetes-specific tools to measure QoL was undertaken and determined that tools often measured the impact of societal attitudes, public policies, and context on QoL in addition to mental, physical, and social health components.[2]
Quality of life and diabetes in India
India is currently second in the world in diabetes prevalence, with an estimated 77 million people affected in 2019, and this number is expected to reach 101 million by 2030.[1] The Indian Council of Medical Research (ICMR) - India DIABetes (ICMR-INDIAB) study has reported diabetes prevalence in 15 of the 31 states/union territories of India completed and published to date. The average prevalence was 7.3%; however, large differences in prevalence are observed between the states, indicating epidemiological transition.[13]
The earliest studies on diabetes QoL in India were conducted among T1D patients in 2007[14] and among T2D patients in 2009.[15] Since then, QoL assessment publications have increased however they are largely reported from tertiary care hospital settings and characterized by small sample sizes. Hence, the results of the studies cannot be generalized to the larger Indian population.[16] In addition to the existing drawbacks as stated above, more QoL assessment tools are being developed,[17,18,19] increasing the complexity of generalizing from multiple QoL tools. A recent article reported a scarcity of QoL studies among diabetic patients in India as a major limitation of the current literature.[16]
Hence, better recognition of the importance of the QoL construct in managing chronic conditions is important and a review of QoL studies, timely. Therefore, this scoping review aims to explore the current state of knowledge on QoL in people with diabetes in India. This paper also attempts to study the various factors associated with QoL in those with diabetes in India.
METHODS
This scoping review was based on the five stages outlined in the Arksey and O’Malley Framework[20] and guidelines from the Joanna Briggs Institute.[21] The Preferred Reporting Items for Systematic Review and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR)[22] were used. Registration on the International Prospective Register of Systematic Reviews (PROSPERO) was not possible as scoping reviews had not been accepted at the time of the review.
Stage 1: Identifying the research questions
What are the various measurement tools used to measure QoL/HRQoL status among patients with diabetes in India?
What are the various factors reported to be associated with quality of life and diabetes in India?
Stage 2: Identifying the relevant studies
Search strategy
The scoping review included all original studies published in English on QoL assessment and diabetes in India. The review included all types of diabetes including T1D, T2D, gestational diabetes, and other forms of diabetes. Grey literature including conference proceedings, dissertation, and thesis reports was included. The inclusion criteria contained “observational studies” and were not restricted to any type of diabetes and included adults and children. The exclusion criteria included “intervention studies” and “nondiabetic patients.” The keywords searched consisted of “Diabetes” AND “Quality of life OR health related quality of life” AND “India.” The search terms were intentionally kept broad and sensitive enough to include all relevant studies in the review. The search strategy used in PubMed is found in Table 1.
Table 1.
Search strategy used in PubMed
| # Search term |
| 1. #Diabetes AND |
| 2. #Quality of life/Health-related quality of life AND |
| 4. #India NOT |
| 5. #Intervention studies |
Databases used
The databases used for the review included PubMed, Scopus, and Medline and were searched between April and July 2020. The results were then imported to Covidence systematic review software, (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org), a web-based platform, which helps to streamline the collection of articles. The references of identified publications were screened for any additional relevant papers.
Stage 3: Study selection
Two independent investigators were involved in the study selection process. AR ran the searches in the individual databases and screened the titles in Covidence. The full-text review was conducted independently by AR and PR and, in case of disagreement, a third reviewer (VM) was consulted as a subject expert.
Stage 4: Charting the data
A template for data extraction is presented in Table 2.
Table 2.
Description of data extracted from each included study
| Study characteristics | Year of publication |
|---|---|
| Authors | |
| Place | |
| Study information | Design |
| Setting | |
| Recruitment | |
| Participant characteristics | Sample size |
| Age of the participants (Mean, median) | |
| Sex | |
| Sample size justification | |
| Measurement of QoL | A tool used for measurement |
| Result of the study | A total score of the tool used |
| Individual domain score | |
| Factors associated with QoL |
Stage 5: Collating, summarizing, and reporting the results
A PRISMA diagram showing the screening results is shown in Figure 1.
Figure 1.
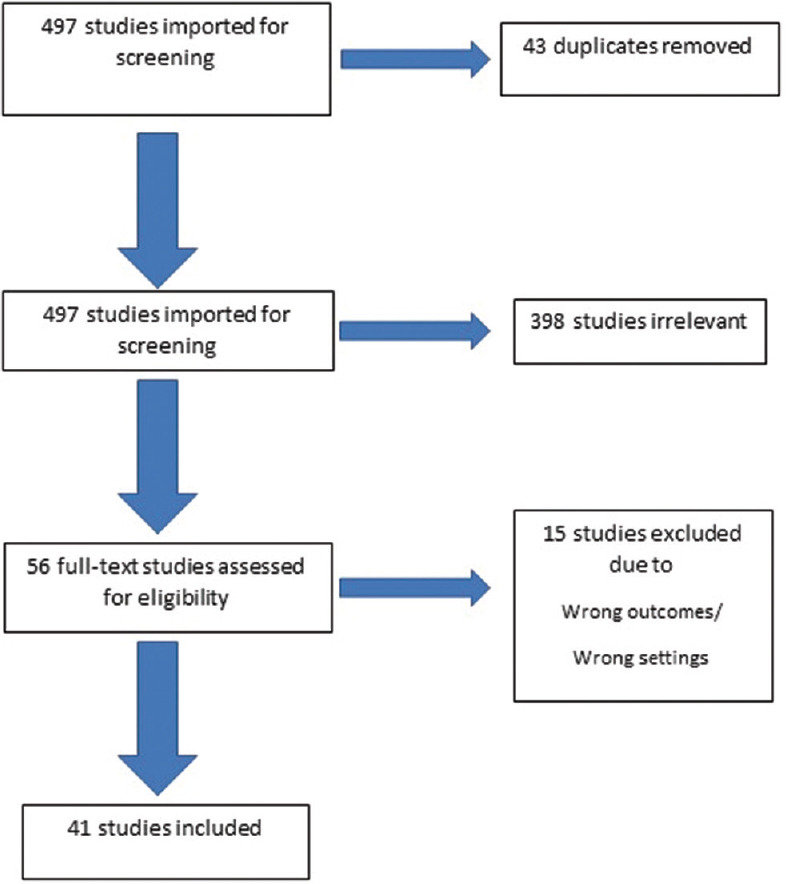
PRISMA flow diagram of study inclusion
RESULTS
General characteristics
Overall, 497 studies were imported for screening, of which 43 duplicate references were removed. A title/abstract screening of the remaining 454 articles was done, and 398 studies considered were removed due to nonrelevance of the subject to the objective of the review. After a full-text review of 56 articles, 15 studies were excluded due to having the wrong outcomes/settings and finally, 41 studies were included in the scoping review. A summary of the reviewed articles is in Appendix 1.
Of the 41 selected studies, one study was conducted in a community setting,[23] one study was conducted at primary health care center setting,[24] and another at secondary care facility,[25] with the 38 remaining studies conducted in tertiary health care facilities. The public health care system in India is a three-tier structure comprising primary, secondary, and tertiary levels. Primary health care centers are involved in providing primary care, whereas district hospitals and sub-divisional hospitals provide secondary care. Tertiary health care is delivered by medical college hospitals. The identified studies largely come from the southern part of India (19 studies) with thirteen studies reported from the state of Karnataka.
Most of the QoL assessment studies (39 studies) among diabetes patients in India have been published within the last decade. Overall, there were 31 studies that included T2D patients, four studies on T1D patients, one study on GDM, whereas five studies did not report their diabetes classification. The reviewed studies tended to have small sample sizes with sample size justification provided in only nine studies.[16,23,24,26,27,28,29,30,31] While four studies mentioned the use of convenience sampling,[25,32,33,34] 28 studies did not mention their sample design.
Five case-control studies where diabetes respondents were compared with nondiabetes patients were identified,[26,35,36,37,38] whereas the remainder of studies were cross-sectional.
Quality of life and type of diabetes
There were 29 studies with QoL assessment in T2D cohorts. Four studies reported QoL assessment among T1D patients.[14,27,39,40] A single study reported QoL assessment among mothers with gestational diabetes mellitus.[41] Seven studies have conducted QoL assessment among both T1D and T2D patients with diabetes.[15,25,32,36,38,42,43]
Only a few studies reported the mean QoL scores among T2D patients, and the scores varied drastically among different QoL assessment tools as seen in Appendix 1. The minimum score of 38.40 was reported from using the SF-36 tool,[31] and the maximum score of 86.83 was reported by QOLID.[44] Four studies reported scores that varied between 54.8 and 57.8.[25,33,36,45]
Among the T1D patients, the mean DAWN QoL scores reported were 35[39] and 29.3[40] which indicated a moderate QoL. The higher DAWN scoring indicates a greater impact on QoL.[40]
Quality of life and gender
Of the reviewed studies, only 14 reported gender and QoL. Poorer QoL in women than men were reported in nine studies on T2D[15,23,25,31,35,37,45,46,47] and in one study on T1D.[14] It is of interest that three studies had reported better QoL among female respondents with diabetes when compared to their male counterparts.[30,34,46]
Poor sleep quality was frequently reported among females as compared to men with T2D, which had detrimental effects on the HRQoL assessment.[48]
Quality of life and duration of diabetes
Of the 41 reviewed studies, seven studies reported a longer duration of diabetes to be associated with poorer QoL among T2D patients.[24,26,29,37,49,50,51] However, this factor was not reported in the T1D studies.
Quality of life and glycemic control
Not surprisingly, poor glycemic control was associated with impaired QoL in three studies among T2D patients.[30,34,37] Similarly, poor glycemic control was associated with poor QoL among T1D children in one article.[27]
Quality of life and diabetes-related complications
Of the 41 reviewed articles, four studies reported QoL assessment and diabetes-related complications. A cross-sectional study on QoL assessment among 382 T1D and T2D patients with different microvascular and macrovascular complications reported that diabetic complications were associated with reduced QoL. Neuropathy and nephropathy were associated with lower QoL as compared with other diabetic complications.[38]
A case-control study (100 cases and 100 controls) among T2D patients from Delhi reported lower mean values of WHO-QoL for all the domains in patients with complications of diabetes (more specific for nephropathy and neuropathy) as compared with patients without diabetes complications.[26]
Among the microvascular complications of diabetes, diabetic retinopathy (DR) and QoL assessment were reported in three studies.[42,52,53] One study reported lower QoL among patients with diabetes with diabetic retinopathy (DR) as compared to those without. The study participants included T1D and T2D patients. The lowest QOL scores were obtained from subjects with proliferative diabetic retinopathy (PDR).[52] The second was a cross-sectional study that reported poor QoL with proliferative diabetic retinopathy (PDR) as compared with nonproliferative DR (NPDR) in 250 T2D patients.[42] The third, a prospective, observational study among 189 T2D patients reported a significant reduction in HRQoL with the severity of retinopathy.[53]
Quality of life and treatment regimen
Better QoL was observed among patients receiving a single- or two-drug regimen as compared with patients receiving a combination regimen of oral hypoglycemic agents (metformin, glipizide, voglibose, repaglinide, sitagliptin, and vildaglitpin) and insulin in one study with T2D patients.[54] Treatment satisfaction of patients receiving metformin alone or in combination with glipizide was better than that of the patients receiving oral hypoglycemic agents and/or insulin.[54]
Quality of life and psychosocial factors
A study from Jaipur (n = 50) reported that more than half of patients with T2D noted impaired QoL.[37] In another cross-sectional study, among 300 T2D participants from Delhi, poor sleep quality was reported and associated with poor QoL.[48]
A case-control study showed that depression was significantly more prevalent among people with T2D than controls and was associated with poorer QoL.[26]
A study among T2D patients with and without depression reported that in the presence of depression, QOL deteriorated.[55]
Quality of life and comorbidities/metabolic syndrome
Of the 41 reviewed studies, only two assessed QoL among T2D patients with comorbidities[24] or metabolic syndrome.[56] A stroke had a high negative impact on the physical HRQoL. The presence of comorbidities affected the physical component summary (PCS) and the mental component summary (MCS) of the Short Form Health Survey-12. Subjects with visual impairment and stroke had significantly reduced quality of life.[24] Among T2D diabetes patients with metabolic syndrome, a greater significant decline is observed in PCS and MCS as compared to those without metabolic syndrome.[56]
Commonly used QoL measurement tools in Indian studies
The QoL assessment among T2D patients in India has been conducted using both generic and diabetes-specific instruments [Table 3]. Among the generic tools, the WHOQoL-BREF tool was employed in eleven studies and the SF-36 V2 questionnaire in nine studies. The diabetic-specific QOLID questionnaire tool was used in eight studies. Table 3 describes the commonly used QoL assessment tools used in India identified in the review.
Table 3.
Commonly used QoL assessment tools used in India identified in the review
| T2D | T1D | |
|---|---|---|
| Generic tool | WHOQOL-BREF | NIL |
| MOS SF36 V2 | ||
| Diabetes specific tool | QOLID (developed in India) | Diabetes Control and Complications Trial (DCCT)-modified to the Indian context |
| ADDQOL | DAWN Youth QoL | |
| Modified Diabetes Quality of life (developed in India) | Diabetes specific quality of life score (DSQoL) | |
| Appraisal of Diabetes Scale | QOLID (modified for T1D patients) |
The WHOQOL-BREF (10 studies)[25,26,29,30,35,36,57,58,59,60] and SF 36 (eight studies)[15,23,31,32,41,45,47,56] are the most commonly used generic instruments among T2D subjects in India. One study used both generic and diabetes-specific tools for QoL assessment and found that both instruments are equally effective and reliable in the evaluation of QoL among diabetes patients.[29]
In recent years, the QOLID questionnaire has been increasingly used among Indian researchers.[16,27,38,42,44,49,51,54] QOLID is specifically designed for an Indian population and has high internal consistency of 0.894 (identified using Cronbach's alpha) and discriminant validity which makes it popular among Indian researchers. Cronbach's alpha is provided as a measure of the internal consistency and expressed as a number between 0 and 1.[61]
For QoL assessment among T1D patients, four different questionnaires were used [Table 3] including Diabetes Control and Complications Trial (DCCT) (modified for the Indian context), DAWN Youth QoL, Diabetes specific quality of life score (DSQoL). In a recent study, the QOLID questionnaire mainly designed for the Indian diabetic adult population was translated into Hindi and modified with minor changes for T1D children.[27]
DISCUSSION
The present review is the first to our knowledge to collate articles related to QoL assessment in people living with diabetes in India. The review demonstrates that most evidence on QoL in India is available in individuals with T2D patients. The QoL assessment among T1D Indian children is scarce and needs to be investigated in future studies. In addition, there is little to no evidence of QoL in the Indian population for gestational diabetes mellitus (GDM) and monogenic forms of diabetes. As five million women have GDM in India[62] and new cases of monogenic diabetes are continually being reported due to advances in the field of molecular genetics,[63,64,65] QoL assessment needs to be urgently addressed in these subtypes of diabetes in order to be able to offer more support to these groups.
The largest number of studies (19 studies) were reported from southern states of India, many from teaching tertiary hospitals/institutions, especially from Karnataka as compared to other regions (North, East, West) of the country. One of the possible reasons could be that Karnataka has the largest number of teaching medical institutions in India. Notably, only a single study was reported from community settings. In the future, QoL assessment needs to be undertaken in large community settings with a proper sample size selection to understand the QoL status at the population level, which is currently missing. The presently available studies have small sample sizes, come from hospital settings, and have a short duration which makes it difficult to generalize the findings for a larger population.
During this review, it was observed that QoL is largely reported as being better among men as compared with women with diabetes, a consistent finding with studies conducted across the world.[11,66] A study was done in a secondary care setting highlighted the need to improve the QoL among women with diabetes.[25] Rubin et al.[11] in their review paper stated that men with diabetes have an advantage over women in HRQoL and recommended control for gender in future studies, which would be relevant to the Indian settings as well.
Though many studies in recent years have used QOLID as a measurement tool, generic questionnaires such as WHOQOL-BREF and SF-36 V2 continue to be used in India. The WHOQOL-100 was initially developed with international consensus but more recently a short form WHOQOL-BREF, with validity and reliability similar to the longer measure, has become available.[12] Many prefer to use the WHOQOL-BREF questionnaire as it is associated with a low time burden.[37] Though not diabetes-specific, it is largely applicable to people with diabetes and has been validated in Indian languages including Hindi.[67,68,69]
The SF-36 V2 questionnaire contains two components (Physical Component Summary and Mental Component Summary) and includes eight domains.[12] The questionnaire is available in Indian languages – Hindi and Kannada.[15,23] The Cronbach's alpha score for Hindi version is 0.70.[70] Though this tool is popular among Indian researchers, the reviewed studies have not stated the reasons behind selecting the tool.
QOLID is a reliable and valid questionnaire developed for Indian patients with diabetes. It contains eight domains with 34 questions and takes 7 min to complete.[18] The QOLID questionnaire is also now modified to measure QoL among Indian children.[27] The questionnaire has high internal consistency, discriminant validity, and has an overall Cronbach's alpha value of 0.894. However, the tool is designed for middle- and higher-income groups, and the authors suggest that the tool should be redeveloped for wider socio-economic groups and for community settings.[18] In the future, this questionnaire should be modified and validated for the Indian population across various socio-economic status levels. Socioeconomic status is defined as “a measure of an individual or family's economic and social position in relation to others, based on various variables for that like income, education, occupation, etc.”[71]
Table 4 illustrates the various domains of the commonly used questionnaire for QoL assessment.
Table 4.
Various domains used in the commonly used questionnaires
| Questionnaire | Number of questions | Domains measured |
|---|---|---|
| WHOQOL-BREF | 26 | Physical health, psychological health, social relationships, and environment plus two items measuring overall QoL and general health |
| SF-36 | 36 | a. Physical component summary containing: Physical functioning, body pain, general health, and role physical domains |
| b. A mental component summary containing vitality, mental health, social functioning, and role emotional domains | ||
| QOLID | 34 | Eight domains |
| 1. role limitation due to physical health, 2. physical endurance, 3. general health, 4. treatment satisfaction, 5. symptom botherness, 6. financial worries, 7. emotional/mental health 8. diet satisfaction. |
Newer questionnaires have also been developed to measure QoL, including MDQoL-17 which was developed and validated in 2010 and is available in local languages.[17] Another QoL assessment questionnaire was developed only for diabetic foot ulcer patients.[19] Though it is encouraging to have newer tools for QoL assessment available, these should be properly validated before entering common use. For example, one review paper identified Short Form -12 and Appraisal of Diabetes Scale as ideal and feasible tools for QoL assessment in busy clinical settings.[72]
The following section recommends several factors to be considered for the selection of QoL assessment tools in future research.
Guidelines to select the right tool for QoL assessment
With new tools being developed for Indian settings, care should be taken to select the right tool for assessment.[17,19] One of the best ways to avoid the unnecessary development of new instruments is to select an existing and validated measure. It is important to understand the various domains, the questionnaire will measure. It is also important to analyze the previous validation of the questionnaire and report psychometric properties. Cronbach's alpha is the most widely used objective measure of internal reliability and the acceptable value ranges from 0.70 to 0.95.[61] The WHOQOL-BREF, Appraisal of Diabetes Scale and QOLID have Cronbach's values of 0.78, 0.80, and 0.89, respectively, showing that they are all reliable tools.
It is also important to understand the purpose of the specific tool. Was it developed for clinical, research, or community settings? Is it patient-centered, treatment-centered, or diet-centered? The questionnaire should be made culturally appropriate to include patients’ needs and perspectives. It is crucial to consider the length of the questionnaire in order to avoid “questionnaire fatigue.” It has been suggested to keep shorter questionnaires for clinical screening and longer measures for researchers to gain further insights into the assessment of QoL.[2]
In addition, a few questions can be considered while selecting an ideal QoL measure as suggested by Speight et al.[12] They include the hypothesis and objective of the study, examination of the instrument and with each item and its response options, in case of generic measures are any relevant issues missed, response acceptance by the respondents, previous validation of the questionnaire in the given population/country/language, and analysis of data. If the clinician and researchers are not confident in such analysis, they can collaborate in a multidisciplinary team with a social scientist experienced in the development, use, and interpretation of measures in diabetes.
Limitations of the study
This study has some limitations. The quality of the reported studies is largely poor, with low homogeneity, and hence it was not possible to combine them into a meta-anlysis. Except for a few studies, most lacked a robust study methodology, many have not followed a scientific approach to sampling, relying on convenience sampling. Similarly, very few studies have mentioned the rationale as to why a particular QoL assessment questionnaire was preferred. In addition, several studies have not reported a thorough data analysis and interpretation.
Therefore, it is recommended that future research on QoL assessment in India should aim for better-designed studies with greater scientific rigor. Such studies would help in a better understanding of QoL and diabetes in India.
CONCLUSION
With the increased prevalence of diabetes in India and around the world, it is becoming even more important to assess the QoL as an outcome measure in long-term illness and management. The review is the first of its kind from India to review the various QoL assessment tools used. The current review showcased that poorer QoL was observed in people with diabetes as compared to those without diabetes. However, the reviewed studies were largely focused on T2D patients, with significant methodological issues, and small samples limiting their validity and generalizability. There is an urgent need to conduct extensive and high-quality QoL assessment studies with sample sizes representative of various groups and types of diabetes in India to address this gap in the evidence.
National recommendations are available in India for psychosocial management of diabetes, which provide practical guidelines to achieve qualitative improvement in diabetes management.[73] Similarly, a consensus statement has been issued to address the psychosocial challenges and management for South Asian women with diabetes.[74] However, as highlighted in this review, extensive research in this area is still required. Following this, further research on these guidelines should be updated to improve the psychosocial aspects of patients with diabetes in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Appendix
Appendix 1.
Summary of the articles reviewed
| Reference Author, year, city/state, area (North, East, South, West) | Study information Design; setting Recruitment | Participant characteristics (Sample size, study period median/mean age (years±SD) and sex) | Measurement of QoL | Results |
|---|---|---|---|---|
| [57] Laksita J et al., 2020 Mangalore Karnataka South India |
Cross-sectional. Tertiary teaching hospital. T2D patients diagnosed with duration of ≥1 year. |
n=190 Sample size justification: not provided Study period: 4 months mean age: 53.47±13.45 Male: 63.7% |
WHOQOL-BREFa | Mean score not provided. Only individual domain scores available. Factors associated with QoL: Increase in age has impaired QoL score Participants who had regular blood sugar and those who did daily exercise had better QoL. |
| [48] Azharuddin M et al., 2020 New Delhi North India |
Cross-sectional. Tertiary teaching hospital. Confirmed T2D patients as per medical records or having fasting plasma glucose level ≥126 mg/dL. |
n=300 Sample size justification: not provided Study period: 5 months mean age: 55.29±12.45 Male: 50.7% |
Health-related quality of life-EQ-5Db | EQ-5D index 0.79±0.22 EQ-5D VAS scores 77.50±23.42 Poor sleep quality reported among participants Poor sleeping resulted in lower HRQoL. |
| [42] Deswal J et al., 2020 Chandigarh North India |
Cross-sectional. Tertiary teaching hospital. Patients diagnosed with Diabetic Retinopathy (DR) for past 5 years. |
n=250 Sample size justification: not provided Study period-not provided mean age=57.13±9.7 Male- 54.4% |
QOLIDc- modified for DR | Diabetic Retinopathy has a significant effect of the QoL which increases with severity of the disease. Proliferative Diabetic Retinopathy (PDR) patients had poor QoL than non-proliferative diabetic retinopathy (NPDR) patients |
| [39] Kumar N et al., 2020 Sonipat Haryana North India |
Cross-sectional. Tertiary care hospital. 146 children with T1D were screened for study. Children on insulin therapy and ≥6 years of age were included. |
n=46 Sample size justification: not provided Study period-not mentioned mean age of onset of diabetes=9.9 ± (0.4) Male- 52% |
Down Quality of Life for youngd (published by the DAWN youth project) | Mean DAWN QoL score=35 |
| [28] Parashar A et al., 2019 Moradabad Uttar Pradesh North India |
Cross-sectional. Tertiary care hospital. T2D (in-patients and out-patients) |
n=196 Sample size justification: provided. Study period- 6 months (Jan-June, 2019) Mean age of the participants-not provided Male- 46.43% |
QOLID (of 8 domains only 4 were used) | Domain scores not mentioned |
| [16] John R et al., 2019 Pune Maharashtra West India |
Cross-sectional. T2D patients diagnosed for≥6 months. |
n=153 Sample size justification: provided Study period- not provided Mean age of the participants=61.23± (11.41) Male- 57.5% |
QOLID-Marati version (validated) | Mean QoL score- not mentioned. Only domain scores provided. Factors associated with QoL-Participants with positive family history had better QoL. Impaired QoL was observed among participants with higher BMI, Illiterates and primary educated participants, widowed or divorced patients, participants on treatment with insulin alone or in combination with OHA. |
| [44] Vas A et al., 2019 Udupi Karnataka South India |
Cross-sectional. Tertiary teaching hospital. Participants admitted with T2D aged ≥30 years and diagnosed with diabetes for >3 months and HbA1c ≥6%. |
n=180 Sample size justification: not provided Study period- 1 year Mean age of the participants not provided Male-67.2% |
QOLID | Mean QOLID instrument score- 86.83 ± (8.3) |
| [24] Pati S et al., 2020 Bhubaneshwar, Odisha |
Cross-sectional interview survey. 17 primary urban health centers in Bhubaneswar. Patients diagnosed with T2D by a physician for >6 months according to their personal health record. |
n=942 September 2014-February 2015 Sample size justification provided Male=63.1% Mean age of participants=55.3± (10.3) |
SF-12e | Overall Physical Component Summary=32.8±13.7 Overall Mental Component Summary=45.9±9.0 Presence of comorbid conditions associated with lower QoL values Significant reduction in HRQoL with increase in the number of comorbidities. Factors associated with QoL- duration of diabetes, use of insulin, obesity associated with poor QoL. |
| [38] Simon P et al., 2019 Mangalore Karnataka South India |
Cross-sectional. Tertiary care hospital. Patients aged ≥18 years and diagnosed with T1D and T2D. Other inclusion criteria mentioned. |
n=382 Sample size justification: not provided Study period- Jan-December 2012 Mean age of the participants not provided |
QOLID | Diabetic complications are associated with reduced QoL. Patients with diabetic neuropathy and nephropathy were associated with lower QoL in comparison with patients with retinopathy, foot complications and cardiac complications. |
| [27] Dayal D et al., 2019 Chandigarh North India |
Cross-sectional. Tertiary care hospital. Pediatric diabetes clinic. Children 4-15 years of age diagnosed with T1D for ≥6 months |
n=97 Sample size justification provided. Study period-January- December 2012 Mean age of participants=9.6 ± (2.6) Mean age of onset of T1D=7.2± (2.86) |
QOLID (Hindi)- validated | Total QOLID score=84.1 ± (6.8) Factors associated with QoL: Poor glycemic control and increased number of hospitalizations were related to poor QoL |
| [58] Bhattacharjee K et al., 2019 Kolkatta East India |
Cross-sectional. Tertiary care hospital. |
n=not mentioned Sample size justification: not provided Study period- June- October 2018 Mean age of the participants not provided |
WHOQOL-BREF | Physical domain, psychological, emotional, and social domain of QoL was significantly affected in diabetic persons. |
| [32] Goel M et al., 2019 New Delhi North India |
Cross-sectional. Tertiary care center. |
n=100 Convenience sampling technique mentioned. Male=36% Mean age of participants=51.95 ± (11.75) Mean age of participants=51.95 ± (11.75) |
SF-36 v2f (Hindi) | Mean scores not provided The study did not find any significant differences in HRQoL based on age, sex, and other co-existing diseases |
| [46] Parik P et al., 2019 Ahmedabad Gujarat Central India |
Cross-sectional descriptive study. Tertiary care teaching hospital. T2D patients aged ≥18 years attending tertiary care hospital for ≥1 month. |
n=358 Sample size justification: not provided Study period-not provided Male=39.7% Mean age of participants=60.71 ± (11.41) |
EQ 5D 5L (Gujarati) | Mean EQ VAS score=78.83±(15.02) Factors associated with QoL- Increased age, Male gender, uncontrolled disease, and presence of comorbidities decrease QoL score |
| [54] Chaturvedi R et al., 2018 Ahmedabad Gujarat Western India |
Cross-sectional. Tertiary care hospital at Western India. All patients diagnosed with T2D (treatment naïve or otherwise) attending clinic. Each patient evaluated at 3rd and 6th month of enrolment. |
n=200 Sample size justification: not provided Time period not mentioned Mean age of the participants=52.17 ± (8.2) |
QOLID (Gujarati version-validation not mentioned). Questionnaire administered at 0, 3, and 6 months | Better QoL was observed among patients receiving single or two-drug regimen as compared to patients receiving combination regimen of OHAs and insulin. The QoL parameters improved significantly at three and 6 months but was not statistically significant. |
| [41] Sasi Sekhar TVD et al., 2018 Chinoutpalli Krishna dt Andhra Pradesh South India |
Cross-sectional. Tertiary health care center. Pregnant women included by using OGTT (Carpenter and Coustans Criteria). |
n=150 Sample size justification: not provided Study period: June 2016 to May 2017 28 GDM (cases) and 118 GDM negative (controls) Mean age of cases=24.82 ± (3.9) Mean age of controls=23.31 ± (3.9) |
SF-36 V2 | Physical Component Score=42.6 ± (18) cases and 55.2 ± (19.1) (control) Mental Component Score=50 ± (14.7) cases and 62.2 ± (14.9) (control) Factors associated with QoL-Women with higher socioeconomic class had better QoL as compared to lower socioeconomic class. |
| [59] Gosain V et al., 2016 Mandya Karnataka South India |
Cross-sectional. Tertiary care hospital. Patients aged ≥20 years. Diagnosed with hypertension and/or T2D and on treatment for ≥1 year, attending the out-patient department. |
n=52 Sample size justification: not provided Study period-2 months Male=69% Mean duration of diabetes=7.8 |
WHOQOL-BREF | The mean QoL-BREF instrument score=Not mentioned. Factors affect QoL: Elderly people more than 60 years had a good quality of life in comparison to patients of age-group 40-49 yrs. |
| [34] PrasannaKumar HR et al., 2018 Mysore, Karnataka, South India. |
Prospective cross-sectional. Tertiary care multi-specialty hospital. Patients aged ≥18 years. |
n=200 Male=34% Convenience sampling technique mentioned. |
ADDQoLg | The mean QoL score=0.07 Diabetes-dependent QoL = -1.33 (0.58) 38% associated with poor health related QoL Factors associated with QoL Gender, age, domicile, education status, occupation, family structure, duration of T2D, HbA1c, insulin treatment and presence of comorbidities are positively correlated with QoL |
| [53] Radhakrishnan C et al., 2018 Kozhikode Kerala South India |
Prospective, observational study. Tertiary care referral hospital. Patients aged 33-76 years, suffering from T2D either with or without proliferative diabetic retinopathy or diabetic macular edema. |
n=189, Sample size justification: not provided Study period: not mentioned 94 were with Proliferative diabetic retinopathy or diabetic macular edema and remaining 95 were without PDR or DME. |
EQ 5D 5L | Severity of retinopathy significantly reduces health-related QoL. Presence of PDR or DME reduces vision related QoL significantly |
| [56] Rani M et al., 2018 Patiala Punjab North India |
Descriptive, observational study. Tertiary teaching hospital. T2D patients (screened as per American Diabetes Association) ≥ 18 years of age fulfilling NCEP-ATP III criteria (diagnosed with at least 3 components out of 5 components) |
n=100 (without metabolic syndrome) and 100 (with metabolic syndrome) Sample size justification: not provided Study period- October- March, 2017) |
SF-36 v2 | Patients with T2D with metabolic syndrome have overall poor HRQoL as compared with T2D without metabolic syndrome. |
| [26] Bahety P et al., 2017 New Delhi North India. |
Case-control study. Tertiary care hospital. Patients aged 30-80 years diagnosed with T2D for ≥1 year with absence of anxiety/depression before the diagnosis of diabetes based on history or previous records. |
n=100 cases and 100 control Sample size justification provided Male=48% Mean age of participants=56.0 ± (5.69) cases 56.1 ± (7.8) yrs controls |
WHOQOL-BREF | The mean QoL-BREF instrument score=not mentioned for cases and control The mean WHO-QOL for all domains was lower among cases when compared to controls. Depression was common cases as compared to controls. The mean WHO-QOL for all domains was lower among patients with nephropathy. |
| [37] Jain A et al., 2017 Jaipur Rajasthan West India |
Case-control study. Psychiatry department Secondary care referral hospital. Patients aged 18-70 yrs. Healthy controls were enrolled. Diabetes is defined as either requiring oral or injectable antidiabetic medication or having random blood glucose level >200 mg/dL |
n=50 cases and 50 control Sample size justification: not provided Study period not mentioned men=54% Mean age of participants=48.25 ± (19.06) Mean duration of diabetes=5.6 ± (2.3) |
WHO QOL-BREF (Hindi) | The QoL scores of all four domains were significantly lower among diabetic patients as compared to their controls. 62% of the patients with diabetes had insomnia Factors that affected QoL- women, poor glycemic control, insomnia, duration of illness for longer than 1-year and increased BMI had impaired QoL |
| [43] Kokiwar PR et al., 2017 Kokiwar PR et al., 2017 Hyderabad Telengana South India |
Cross-sectional study. Known case of diabetes >25 years of age. |
n=64 Sample size justification: not provided Study period-3 months Demographic details of the participants not available |
4 domains of QOLID questionnaire were used- a. Role limitation due to physical health b. Physical endurance c. General Health d. Symptom barrier |
Role limitation among participants was not much affected. |
| [52] Pereira DM et al., 2017 Mangalore Karnataka South India |
Case-control study. Tertiary teaching hospital. Patients>18 years of age with T1D and T2D. The cases and controls were selected using a fixed criterion. |
n=123 (97 cases with diabetic retinopathy (DR) and 26 control without DR) Sample size justification: not provided Study period- Jan- Dec, 2012 Male=57.1% Mean age of participants=55.09 ± (9.56) (cases) 54.12 ± (13.01) (cases) Mean duration of diabetes=10.98 ± (5.62) (cases) 6.69 ± (2.29) (cases) |
National Eye Institute 25- Item Visual Function Questionnaire (NEI-VFQ-25)h | Composite score (cases)= 73.93±25.55 Composite score (control)= 99.26±1.01 Quality of life was significantly lower in diabetics with DR as compared with those without DR. Maximum effect was seen on general health, general vision, and mental health Factors associated with QoL- Duration of retinopathy and severity of retinopathy decreased QoL |
| [50] Prajapati V et al. Manipal, 2017 Karnataka, South India. |
A prospective descriptive study. Tertiary care hospital. |
n=250 Sample size justification: not provided Study period Male=64% Mean age of participants=60.34 ± (12.04) |
Modified Diabetes Quality of Life (MDQoL)-17i | The average QoL score=65.47±15.07 Patients with complications had a decreased QoL The presence of comorbidity also decreased the QoL Factors associated with QoL-age, duration of diabetes history, HbA1c, number of complications, type of complication |
| [60] Swathi G KP et al., 2017 Warangal, Telangana, South India. |
Descriptive, observational study. Patients diagnosed with T2D and on anti-diabetic therapy for ≥6 months and aged ≥18 years. |
n=300 Sample size justification: not provided. Study period: not provided. Male=37% Mean age of participants=51.1± (9) |
WHOQOL-BREF | The mean QoL-BREF instrument score=not mentioned |
| [51] Mathew G et al., 2016 Thiruvalla Kerala South India |
Cross-sectional. Patients aged 35-65 years outpatient department patients with T2D of duration for more than a year. |
n=60 Sample size justification: not provided Mean age of the participants=54.85 Male=33.3% |
QOLID (Malayalam version) | Mean QOLID instrument score- 63.7 Factors associated with QoL- Increased body weight and females gender had impaired QoL scores |
| [23] Singh RK et al., 2015 Udupi Karnataka South India |
Cross-sectional. Diabetes patients of Udupi Taluk, Karnataka. Ten primary health centers (PHCs) were randomly selected. T2D patients registered in PHCs for treatment were included. |
n=138 Sample size justification provided Study period: not provided Male=46.4% Mean age of participants=57.40± (11.1) Mean duration of diabetes=9.29± (6.3) |
SF-36 v2 (Kannada version) | The total SF-36 score=43.12±(7.0) Factors associated with QoL- Men had better QoL scores than women |
| [31] Vaibhav et al. Jaipur, 2016 North India. |
Cross-sectional. Tertiary care center. T2D patients >25 years and on treatment for diabetes for <1 year attending the diabetic clinic were included. |
n=140 Sample size justification provided Study period: not provided Male=50% Mean age of participants=56.0 ± (11.6) Mean duration of diabetes=10.9± (8.3) |
SF-36 v2 | The total SF-36 score=38.40 ± (9.5) Factors associated with QoL- Men had better QoL as compared to women |
| [45] Santosh Kumar A et al., 2016 Shimoga, Karnataka, South India. |
Cross-sectional. Tertiary teaching hospital. Diabetes patients aged >20 years and on treatment for <6 months. |
n=100 Sample size justification: not provided. Study period: June- July, 2013 Male=55% Mean age of participants=54.45 ± (9.7) Mean duration of diabetes=5.78 ± (4.9) |
SF-36 v2 | Total score=57.15 ± (18.33) Factors associated with QoL- treatment for diabetes (patients who took only OHA), compliance to treatment (regular medications), physical activity, follow-up with doctor were significantly associated. |
| [49] Kumar P et al. Shivamogga, 2015 Karnataka, South India |
Cross-sectional. T2D patients at tertiary medical. Study participants >30 years of age. |
n=200 Sample size justification: not provided. Study period-December, 2014 (1 month) Male=52.5% Mean age of the participants: not provided |
QOLID | Mean QOLID instrument score for Male=108 Mean QOLID instrument score for Females=105 Factors affect QoL- Increase in age, years of diabetes, and lower-income class decreased the QoL |
| [36] Kumar P et al. Patna, 2015 Bihar, North India. |
Case-control. Diabetic camps conducted by tertiary teaching hospitals. |
n=85 (diabetes) and 85 (nondiabetes) age and sex matched. Sample size justification: not provided. Study period- March- April, 2013 Male=83.5% Mean age of the participants=49.5 |
WHOQOL-BREF (Hindi) | The mean QoL-BREF instrument score=57.80. |
| [47] Sindhu L et al., 2015 Thiruvananthapuram Kerala South India |
Cross-sectional study. Tertiary teaching hospital. T2D patients >25 years and on treatment for diabetes for <1 year attending the diabetic clinic. |
n=140 Sample size justification: not provided. Study period: not provided. Male=50% Mean age of the participants=56+11.6 |
SF-36 V2 | The mean QoL score=38.40+9.55. Factors identified with QoL -Males had higher QoL scores as compared to females. |
| [33] Mathew A et al. Mangalore, 2014 Karnataka South India |
Cross-sectional. Tertiary teaching hospital. T2D patients. |
n=100 Non-probability purposive sampling technique used. Time period not mentioned Mean age of the participants- not provided. Male- 53% |
QOLID | Mean QoL score=54.8 |
| [35] Jain V Wardha, 2014 Maharastra, Central India. |
Case-control. Rural medical college. Cases- T2D patients with diabetes. Controls- hospitals and community. |
n=70 cases 70 control Sample size justification- not provided. Study Period-not provided. Mean age of the participants=48.63± (10.6)-cases 49.21± (10.4)-control |
WHOQOL-BREF (Marati) | Mean score not provided. Only domain scores are given separately The overall QoL was poor among the study population. Factors associated with QoL- increased age, females, complications negatively affected QoL scores. |
| [25] Manjunath K et al. Vellore, 2014 Tamil Nadu, South India. |
Cross-sectional. Secondary care facility of rural tertiary medical college. Known T2D patients aged >30 and <60 years |
n=100 Convenience sampling justification was provided. Study period- June- September 2008 Male=36% Mean age of the participants=56 |
WHOQOL-BREF (Tamil) | The mean QoL-BREF instrument score=58.03±18.29 Factors associated with better QoL- married men and those with BMI more than 25. |
| [29] Patel B et al., Ahmedabad, Gujarat, 2014 Western India. |
Cross-sectional. Tertiary medical care center. T2D patients attending medicine clinics. |
n=140 Sample size justification provided. Study period: not mentioned. Male=42.1% Mean age of the participants=56.8± (10.5) Mean duration of diabetes=8.3± (9.4) |
1. WHOQOL-BREF 2. Appraisal of Diabetes Scale (ADS)j (Gujarati) |
1. Mean WHO BREF score=76.65± (8.29) 2. Mean ADS score=19.9± (3.4) Factors associated with QoL Age, duration of diabetes, number of symptoms, number of comorbidities, blood glucose level, and number of nonpharmacological measures were |
| [30] Somappa HK et al. Kolar, 2014 Karnataka, South India. |
Cross-sectional. T2D patients at rural tertiary care center. |
n=180 Sample size justification provided Study period-2 months Male=50% Mean age of the participants=59.56± (9.64) (male) 60.9± (7.51) (female) |
WHOQOL-BREF | Mean WHO BREF score=not mentioned. Females had higher mean scores of physical, psychological, social, and environmental domains of QoL compared to males. Quality of life decreased with an increase in age and irregular control of glucose (HbA1c). |
| [40] Puri K et al., 2013 New Delhi North Delhi |
Cross-sectional. Tertiary teaching hospital. T1D children/adolescents aged 6-18 yrs. |
n=49 Sample size justification- not provided. Study Period-not provided. Male=55% Mean age of the participants=11.7±3.1 |
DAWN Youth QoL questionnaire | DAWN QoL Score=29.3±15.8 |
| [55] Das R et al., 2013 Kolkata West Bengal Eastern India |
Cross-sectional. Tertiary teaching hospital. T2D patients. |
n=195 Sample size justification- not provided. Study Period-January 2011 to January 2012 Male=41.5% Mean age of the participants=44.21±6.39 (depressed) 45.68±6.2 (non-depressed) |
Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES)k SF-to evaluate the impact of depression on QoL | Depression has a negative impact on the QoL of the patient. Factors associated with QoL- Patients with poor blood control levels (HbA1c%) have worse QoL |
| [15] Gautam Y et al., 2009 New Delhi, North India. |
Cross-sectional. Tertiary teaching hospital. T1D and T2D patients included. |
n=260 Convenience sampling justification was provided. Study period- January- December 2006 Male=35% Mean age of the participants=49.7 Mean duration of diabetes=6.96± (6.08) |
MOS SF-36 v2 (Hindi version) | Total SF36 score=59.47±(18.70) Factors associated with QoL Females had lower QoL scores as compared with men. Patients with complications reported lower QoL scores as compared with patients without any complications. |
| [14] RT Varghese et al., 2007 Trivandrum, South India. |
Cross-sectional. Tertiary teaching hospital. T1D patients. |
n=200 Sample size justification: not provided Study period-February to March 2006. Male-72.5% Mean age of the participants- not mentioned. |
Diabetes Control and Complications Trial (DCCT)l questionnaire-questions deleted to fit Indian context and pertaining to T1D. | Total score not mentioned 62% of respondents were found to have a good quality of life. Factors associated with better QoL- Male gender, mixed diet, occupation with moderate physical activity, better education, family history of diabetes, having diabetic friends, better sex life, and absence of urinary incontinence. |
Footnotes: Sample size-n; QoL- Quality of Life; S. D- Standard Deviation; QOLID- Quality of Life Instrument for Indian Diabetic Patients; DR- Diabetic Retinopathy;
aWHOQOL-BREF- is a 26-item brief questionnaire over four major domains namely physical, psychological, social relationships, and environment. The responses of the WHOQOL-BREF are scored in a Likert scale fashion from 1 to 5. The total raw scores for these five dimensions will be transformed into 0 and 100 and then the analysis of the transformed score to be done with low score indicating poor QoL.
bHealth-related quality of life-EQ-5D or European Quality of Life- 5 Dimensions questionnaire consists of two parts- the first part is a health status categorized into five dimensions- mobility, self-care, usual activities, pain/discomfort, and anxiety/depression which scores from 0 (no problem) to 1 (extreme problems). The response to the first part is converted into an EQ-5D profile or EQ-5D index which ranges from -0.111 to 1, where 1 represents preferred health. The second part is a visual analog scale (VAS) to determine the overall health status and contains 20 cm scale to measure the patient's perception of quality of life on the day of the interview. The scale ranges from 0 to 100, 0 represents worst health, while 100 represents the best health.
cQOLID- developed in India consists of 34 items with eight domains on general health, role limitations due to physical health, symptom frequency, physical endurance, treatment satisfaction, financial worries, diet advice satisfaction, and mental health. The items were scored from 1 to 5, the maximum possible score is 169 and the minimum 34. The quality of life is classified into good (125-169), moderate (79-124), and poor (34-78).
dDown Quality of Life for young- is a 22-item validated questionnaire in six domains namely impact of symptoms related to diabetes, the impact of the treatment, impact on activities, parents’ issues, worry about the future, and perception of one's own health. Administered to subjects 10-18 years which each question having five possible responses ranging from ‘0’ (never) to ‘4’ (all the time) and the responses are added to get the total score for the subscale. Higher scores indicate a greater adverse impact on QoL
eSF-12 Short Form Health Survey 12 (SF-12) is a shorter version of the 36-item SF-36.
fSF-36 V2- It consists of 36 items covering eight domains: physical functioning (PF), role limitations caused by physical health problems (RP), bodily pain (BP), perception of general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional health problems (RE) and mental health (MH). The eight domains may be further grouped into two summary measures of the physical component summary (PCS) and the mental component summary (MCS). These aggregated scores are converted into norm-based scores (mean, 50; SD, 10), and higher scores indicate a more favorable physical functioning and psychological well-being.
gADDQoL-ADDQoL questionnaire is a third-generation individualized QoL instrument and contains 19 item domains. It evaluates the general QoL as well as the diabetes-dependent QoL. ADDQoL starts with two overview items assessing the patient's present global QoL (range + 3–−3) and the impact of diabetes on the QoL (range − 3–+3). For both items, lower scores indicate a poorer QoL. In the subsequent items, the respondent rates the impact of diabetes (range − 3 to + 3) and the importance of QoL (range 3–0) on 19 item domains.
hNational Eye Institute 25- Item Visual Function Questionnaire (NEI-VFQ-25)- The NEI-VFQ-25 consists of questions related to general health and vision, difficulties with activities and response to vision problems. To calculate an overall composite score for the VFQ-25, simply average the vision-targeted subscale scores, excluding the general health rating question. By averaging the sub-scale scores rather than the individual items, we have given equal weight to each sub-scale, whereas averaging the items would give more weight to scales with more items.
iModified Diabetes Quality of Life (MDQoL)-17- It consists of 17 questions that comprise seven domains, which include physical functioning, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and general health perceptions. All the contents are scored so that a high score depicts a more favorable health state. The possible scores are 0-100, 0 being the minimum and 100 being the maximum score. Scores represent the percentage of the total possible score achieved.
jAppraisal of Diabetes Scale (ADS)- is a seven-item diabetes-specific scale that attempts to assess patients’ feelings and attitudes about diabetes. It consists of items covering distress caused by diabetes, control over diabetes (two items), uncertainty due to diabetes, anticipated future deterioration, coping, and effect of diabetes on life goals. Each question in this scale uses Likert scale with five possible answers (1 - not at all, 2 - slight, 3 - moderate, 4 - very, and 5 - extremely). The total score can range from 0 (best level of health) to 35 (worst level of health). Thus, a lower score on the ADS scale suggests better QOL.
kQuality of Life Enjoyment and Satisfaction Questionnaire (Q-LES) SF- The raw scores on QLESQ-SF were converted to percentage maximum scores (QLESPER).
lDCCT- Diabetes Control and Complications Trial (DCCT) questionnaire, after deleting questions found irrelevant in Indian context and those pertaining only to type 1 diabetic subjects were used.
REFERRENCES
- 1.International Diabetes Federation Diabetes Atlas. 9th ed. Brussels, Belgium: 2019. IDF Atlas. Available from: https://diabetesatlas.org/data/en/ [Google Scholar]
- 2.Palamenghi L, Carlucci MM, Graffigna G. Measuring the quality of life in diabetic patients: A scoping review. J Diabetes Res 2020. 2020 doi: 10.1155/2020/5419298. 5419298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Classification and Diagnosis of Diabetes; Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S13–28. doi: 10.2337/dc19-S002. [DOI] [PubMed] [Google Scholar]
- 4.WHOQOL group. Development of the WHOQOL: Rationale and current status. Int J Mental Health. 1994;23:24–56. [Google Scholar]
- 5.Skevington S, Lotfy M, O’Connell KA WHOQOL Group. The World Health Organization's WHOQOL-BREF quality-of-life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 6.Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diabetes. 2017;8:120–9. doi: 10.4239/wjd.v8.i4.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Testa MA, Simonson DC. Assessment of quality of life outcomes. N Engl J Med. 1996;334:835–40. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 8.Karimi M, Brazier J. Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics. 2016;34:645–9. doi: 10.1007/s40273-016-0389-9. [DOI] [PubMed] [Google Scholar]
- 9.Post MWM. Definitions of quality of life: What has happened and how to move on. Top Spinal Cord Inj Rehabil. 2014;20:167–80. doi: 10.1310/sci2003-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Polonsky WH. Understanding and assessing diabetes specific quality of life. Diabetes Spectr. 2000;13:36–42. [Google Scholar]
- 11.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 12.Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome—A review of quality of life measurement in adults with diabetes. Diabetic Med. 2009;26:315–27. doi: 10.1111/j.1464-5491.2009.02682.x. [DOI] [PubMed] [Google Scholar]
- 13.Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, et al. Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585–96. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 14.Varghese RT, Salini R, Abraham P, Reeshma KK, Vijayakumar K. Determinants of the quality of life among diabetic subjects in Kerala, India. Diabetes & Metab Syndrome: Clin Res Rev. 2007;1:173–9. [Google Scholar]
- 15.Gautam Y, Sharma A, Agarwal A, Bhatnagar M, Trehan R. A cross-sectional study of QOL of diabetic patients at tertiary care hospitals in Delhi. Indian J Commun Med. 2009;34:346–50. doi: 10.4103/0970-0218.58397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.John R, Pise S, Chaudhari L, Deshpande PR. Evaluation of quality of life in type 2 diabetes mellitus patients using quality of life instrument for Indian diabetic patients: A cross-sectional study. J Midlife Health. 2019;10:81–8. doi: 10.4103/jmh.JMH_32_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Acharya L, Kareem S, Ashan F, Mallayasamy S. Development and validation of quality of life assessment instruments for diabetes patients. Asian J Pharm Health Sci. 2014;4:1114–20. [Google Scholar]
- 18.Nagpal J, Kumar A, Kakar S, Bhartia A. The development of ‘Quality of Life Instrument for Indian Diabetes patients (QOLID): A validation and reliability study in middle and higher income groups. J Assoc Physicians India. 2010;58:295–304. [PubMed] [Google Scholar]
- 19.Kateel R, Augustine AJ, Ullal S, Prabhu S, Bhat R, Adhikari P. Development and validation of health related quality of life questionnaire (Indian scenario) in diabetic foot ulcer patients. Diabetes & Metab Syndrome: Clin Res Rev. 2017;11:S651–S3. doi: 10.1016/j.dsx.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 20.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 21.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–6. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 22.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 23.Singh RK, Pattanshetty S, Nair S. Quality of life among type 2 diabetes patients in Udupi taluk: A cross-sectional study. Int J Med Sci Public Health. 2016;5:1846–50. [Google Scholar]
- 24.Pati S, Pati S, Akker MVD, Schellevis FFG, Jena S, Burgers JS. Impact of comorbidity on health-related quality of life among type 2 diabetic patients in primary care. Prim Health Care Res Dev. 2020;21:e9. doi: 10.1017/S1463423620000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manjunath K, Christopher P, Gopichandran V, Rakesh PS, George K, Prasad JH. Quality of life of a patient with type 2 diabetes: A cross-sectional study in rural South India. J Family Med Prim Care. 2014;3:396–9. doi: 10.4103/2249-4863.148124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bahety P, Agarwal G, Khandelwal D, Dutta D, Kalra S, Taparia P, et al. Occurrence and predictors of depression and poor quality of life among patients with type-2 diabetes: A Northern India perspective. Indian J Endocrinol Metab. 2017;21:564–9. doi: 10.4103/ijem.IJEM_123_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dayal D, Malhi P, Patodia J. Quality of life for Indian diabetic children. J Postgraduate Med Edu Res. 2019;5361:8. [Google Scholar]
- 28.Parashar A, Jha KK, Kumar A, Tomer SS, Yadav DS, Imran H. Assessment of quality of life of type-2 diabetes mellitus patients in tertiary care teaching hospital in North India. Int J Basic Clin Pharmacol. 2020;9:107–12. [Google Scholar]
- 29.Patel B, Oza B, Patel K, Malhotra S, Patel V. Health related quality of life in type-2 diabetic patients in Western India using World Health Organization Quality of Life –BREF and appraisal of diabetes scale. Int J Diabetes Dev Ctries. 2014;34:100–7. [Google Scholar]
- 30.Srinivas HK, Venkatesha M, Prasad R. Quality of life assessment among type 2 diabetic patients in rural tertiary centre. Int J Med Sci Public Health. 2014;3:415–7. [Google Scholar]
- 31.Vaibhav, Chahar B. A cross-sectional study to assess the quality of life in patients with type 2 diabetes mellitus. Indian J Forensic Community Med. 2016;3:3. [Google Scholar]
- 32.Goel M, Dhuldhule S, Prakash A, Ghotekar L. Assessing health-related quality of life in patients with diabetes mellitus at a Tertiary Care Center in Central Delhi. Indian J Community Med. 2019;44:171–2. doi: 10.4103/ijcm.IJCM_273_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathew A, Anusree TK, Mathew A, Archana S, Athira M, Sachina B, et al. Quality of Life amongType II diabetes mellitus patients in South India: A descriptive study. Am Int J Res Humanities Arts Soc Sci. 2014;7:4. [Google Scholar]
- 34.PrasannaKumar HR, Mahesh MG, Menon VB, Srinath KM, Shashidhara KC, Ashok P. Patient self-reported quality of life assessment in Type 2 diabetes mellitus: A pilot study. Niger J Clin Pract. 2018;21:343–9. doi: 10.4103/njcp.njcp_433_16. [DOI] [PubMed] [Google Scholar]
- 35.Jain V, Shivkumar S, Gupta O. Health-Related Quality of Life (Hr-Qol) in patients with type 2 diabetes mellitus. N Am J Med Sci. 2014;6:96–101. doi: 10.4103/1947-2714.127752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar P, Agarwal N, Singh CM, Pandey S, Ranjan A, Kumar D. Diabetes and quality of life—A pilot study. Int J Med Sci Public Health. 2015;5:4. [Google Scholar]
- 37.Jain A, Sharma R, Yadav N, Chaudhary P, Jainc G, Maanju M. Quality of life and its association with insomnia and clinical variables in type 2 diabetes. J Egypt Public Health Assoc. 2017;92:52–9. doi: 10.21608/epx.2018.7011. [DOI] [PubMed] [Google Scholar]
- 38.Simon P, Pereiera D, Mathai R, George T, Abraham S, D’Souza O, et al. Quality of life in diabetics with different complications: A cross-sectional study with patients visiting a hospital on an outpatient basis. Hamdan Med J. 2019;12:195–9. [Google Scholar]
- 39.Kumar N, Singh Y, Singh S, Rana V. Quality of life of type 1 diabetic Indian children and adolescents-Cross sectional study. Int J Health Sci Res. 2020;10:1–9. [Google Scholar]
- 40.Puri K, Sapra S, Jain V. Emotional, behavioral and cognitive profile, and quality of life of Indian children and adolescents with type 1 diabetes. Indian J Endocrinol Metab. 2013;17:1078–83. doi: 10.4103/2230-8210.122631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sasi Sekhar TVD, Meroz P, Ramadevi Ch, Mahesh T. Health related quality of life (HRQoL) in Gestational Diabetes Mellitus: A cross-sectional study in tertiary healthcare centre. Int J Sci Res. 2018;7:24–6. [Google Scholar]
- 42.Deswal J, Narang S, Gupta N, Jinagal J, Sindhu M. To study the impact of diabetic retinopathy on quality of life in Indian diabetic patients. Indian J Ophthalmol. 2020;68:848–53. doi: 10.4103/ijo.IJO_1553_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kokiwar PR, Reddy C. H. R, Reddy R. R.D, Reddy S. SR, N S, R S, et al. Quality of life and diabetes mellitus among diabetic adult patients in an urban slum area. Int J Community Med Public Health. 2017;4:4650–3. [Google Scholar]
- 44.Vas A, Devi ES. Quality of life of people with type 2 diabetes. Indian J Public Health Res Dev. 2019;10:47–50. [Google Scholar]
- 45.Santosh Kumar A, Koppad R, Chandrashekar S. Quality of life of type 2 diabetes patients in a tertiary care hospital in southern part of India, Shimoga, Karnataka: A cross-sectional study. Int J Community Med Public Health. 2016;3:1723–8. [Google Scholar]
- 46.Parik P, Patel V. Health-related quality of life of patients with type 2 diabetes mellitus at a tertiary care hospital in India using Eq 5D 5L. Indian J Endocrinol Metab. 2019;23:407–11. doi: 10.4103/ijem.IJEM_29_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sindhu L, Jayakumar B. Health-related quality of life in patients with type 2 diabetes mellitus: A cross-sectional survey. Indian J Public Health Res Dev. 2015;6:8–12. [Google Scholar]
- 48.Azharuddin M, Kapur P, Adil M, Ghosh P, Sharma M. Health related quality of life and sleep quality among North Indian type 2 diabetes mellitus patients: Evidence from a cross sectional study. Sleep Med. 2020;73:93–100. doi: 10.1016/j.sleep.2020.04.022. [DOI] [PubMed] [Google Scholar]
- 49.Kumar P, Krishna M. Quality of life in diabetes mellitus. Sci J Public Health. 2015;3:4. [Google Scholar]
- 50.Prajapati V, Blake R, Acharya L, Seshadri S. Assessment of quality of life in type II diabetic patients using the modified diabetes quality of life (MDQoL)-17 questionnaire. Braz J Pharm Sci. 2017;53 doi: 10.1590/s2175-97902017000417144. [Google Scholar]
- 51.Mathew G, Joseph L, Koshy LV. A study on quality of life assessment among patients with type 2 diabetes mellitus in a tertiary care hospital in Southern Kerala. Int J Pharm Pharm Res. 2016;6:39. [Google Scholar]
- 52.Pereira DM, Shah A, D’Souza M, Simon P, George T, D’Souza N, et al. Quality of life in people with diabetic retinopathy: Indian study. J Clin Diagn Res. 2017;11:NC01–6. doi: 10.7860/JCDR/2017/24496.9686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Radhakrishnan C, CK S, K S, S B. Quality of life in type 2 diabetic patients with and without proliferative retinopathy and macular edema. Diabetes. 2018;67(Suppl 1) doi: 10.2337/db18-2213-PUB. [Google Scholar]
- 54.Chaturvedi R, Desai C, Patel P, Shah A, Dikshit RK. An evaluation of the impact of antidiabetic medication on treatment satisfaction and quality of life in patients of diabetes mellitus. Perspect Clin Res. 2018;9:15–22. doi: 10.4103/picr.PICR_140_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Das R, Singh O, Thakurta RG, Khandakar MR, Ali SN, Mallick AK, et al. Prevalence of depression in patients with type II diabetes mellitus and its impact on quality of life. Indian J Psychol Med. 2013;35:284–9. doi: 10.4103/0253-7176.119502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rani M, Kumar R, Krishan P. Metabolic correlates of health-related quality of life in patients with type 2 diabetes mellitus. J Pharm Pract. 2018;32:422–7. doi: 10.1177/0897190018760622. [DOI] [PubMed] [Google Scholar]
- 57.Laksita J, Darshan B, Ramesh H, Vaman K, Bhaskaran U, Faizan M, et al. Quality of life and self-care behavior among people living with diabetes- A study from Coastal South India. Curr Diabetes Rev. 2020;16:1–6. doi: 10.2174/1573399816666200520101734. [DOI] [PubMed] [Google Scholar]
- 58.Bhattacharjee K, Naikwadi SS, Maiti A. Health related quality of life in patients with type-2 diabetes mellitus: An institutional cross-sectional descriptive study in Eastern India. Indian J Appl Res. 2019;9:17–19. doi: 10.36106/IJAR. [Google Scholar]
- 59.Gosain V, Rao C. A study on the quality of life of patients with type 2 diabetes mellitus and hypertension presenting to a tertiary care hospital in Southern India. J Soc Health Diabetes. 2016;4:45–7. [Google Scholar]
- 60.Swathi G, Kishore P, Venkateshwarulu S, Deepthi S. Evaluation of quality of life and medication adherence in type-II diabetic patients. J Med Sci Clin Res. 2017;5:10. [Google Scholar]
- 61.Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53–5. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morampudi S, Balasubramanian G, Gowda A, Zomorodi B, Patil AS. The challenges and recommendations for gestational diabetes mellitus care in India: A review. Front Endocrinol. 2017;8:56. doi: 10.3389/fendo.2017.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nair VV, Chapla A, Arulappan N, Thomas N. Molecular diagnosis of maturity onset diabetes of the young in India. Indian J Endocrinol Metab. 2013;17:430–41. doi: 10.4103/2230-8210.111636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Unnikrishnan R, Shah VN, Mohan V. Challenges in diagnosis and management of diabetes in the young. Clin Diabetes Endocrinol. 2016;2:18. doi: 10.1186/s40842-016-0036-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aarthy R, Aston-Mourney K, Mikocka-Walus A, Radha V, Amutha A, Anjana RM, et al. Clinical features, complications and treatment of rarer forms of maturity-onset diabetes of the young (MODY) A review. J Diabetes Complications. 2021;35:107640. doi: 10.1016/j.jdiacomp.2020.107640. [DOI] [PubMed] [Google Scholar]
- 66.Undén AL, Elofsson S, Andréasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend Med. 2008;5:162–80. doi: 10.1016/j.genm.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 67.Saxena S, Chandiramani K, Bhargava R. WOrld Health Organisation Quality of Life. WHOQOL Hindi: A questionnaire for assessing quality of life in health care settings in India. Natl Med J India. 1998;11:160–5. [PubMed] [Google Scholar]
- 68.Sreedevi A, Cherkil S, Kuttikattu DS, Kamalamma L, Oldenburg B. Validation of WHOQOL-BREF in Malayalam and determinants of quality of life among people with type 2 diabetes in Kerala, India. Asia-Pacific J Public Health. 2016;28(1 Suppl):62S–9S. doi: 10.1177/1010539515605888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kar N, Swain S, Patra S, Kar B. The WHOQOL-BREF: Translation and validation of the Odia version in a sample of patients with mental illness. Indian J Social Psychiatry. 2017;33:269–73. [Google Scholar]
- 70.Sinha R, van den Heuvel WJA, Arokiasamy P. Validity and reliability of MOS short form health survey (SF-36) for use in India. Indian J Community Med. 2013;38:22–6. doi: 10.4103/0970-0218.106623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ankitha C, Srivatava BK, Eshwar S, Jain V, Rekha K, Swamy MN. Overview of socio economic status scales in India. 2016;1:30–3. [Google Scholar]
- 72.Nair R, Kachan P. Outcome tools for diabetes-specific quality of life: Study performed in a private family practice clinic. Can Fam Physician. 2017;63:e310–5. [PMC free article] [PubMed] [Google Scholar]
- 73.Kalra S, Sridhar GR, Balhara YP, Sahay RK, Bantwal G, Baruah MP, et al. National recommendations: Psychosocial management of diabetes in India. Indian J Endocrinol Metab. 2013;17:376–95. doi: 10.4103/2230-8210.111608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bajaj S, Jawad F, Islam N, Mahtab H, Bhattarai J, Shrestha D, et al. South Asian women with diabetes: Psychosocial challenges and management: Consensus statement. Indian J Endocrinol Metab. 2013;17:548–62. doi: 10.4103/2230-8210.113720. [DOI] [PMC free article] [PubMed] [Google Scholar]


