Abstract
Coronavirus Disease 2019 (COVID-19) is an evolving communicable disease caused due to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) which has led to a global pandemic since December 2019. The virus has its origin from bat and is suspected to have transmitted to humans through zoonotic links. The disease shows dynamic symptoms, nature and reaction to the human body thereby challenging the world of medicine. Moreover, it has tremendous resemblance to viral pneumonia or Community Acquired Pneumonia (CAP). Reverse Transcription Polymerase Chain Reaction (RT-PCR) is performed for detection of COVID-19. Nevertheless, RT-PCR is not completely reliable and sometimes unavailable. Therefore, scientists and researchers have suggested analysis and examination of Computing Tomography (CT) scans and Chest X-Ray (CXR) images to identify the features of COVID-19 in patients having clinical manifestation of the disease, using expert systems deploying learning algorithms such as Machine Learning (ML) and Deep Learning (DL). The paper identifies and reviews various chest image features using the aforementioned imaging modalities for reliable and faster detection of COVID-19 than laboratory processes. The paper also reviews and compares the different aspects of ML and DL using chest images, for detection of COVID-19.
Keywords: Artificial intelligence, COVID-19, Chest images, Image processing, Feature extraction, Classification
Introduction
The Coronavirus Disease 2019 (COVID-19) has globally emerged as a communicable disease caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The first case of COVID-19 was recognized on 12th December 2019 in Wuhan, the capital of Hubei Province, China. COVID-19 has been killing thousands and thousands of people and has thrown a challenge to the existence of human society. On 7th of January, 2020 the virus was recognized as a coronavirus based on >95% homology and > 70% similarity, with the bat coronavirus, and with the SARS-CoV, respectively [85]. Thus, World Health Organization (WHO) and International Committee on Taxonomy of Viruses (ICTV) has named this virus as SARS-CoV-2 [68] instead of 2019-nCoV [22, 26, 31, 35, 37, 46, 48, 56, 59, 91] based on the comparative study of their genomes. The first lethal case was reported on 11th of January, 2020 [76].
It was initially supposed that the colossal movement of Chinese during the Chinese New Year, may have fueled the widespread of the virus and then extended it towards a global pandemic [76]. The original event outside China was reported on 13th January 2020 in Thailand in a Chinese tourist. The initial human transmission of the virus was discovered in an epidemiologic examination performed on January 20, 2020, when two patients were detected COVID-19 positive in Guangdong Province and had no history of travel [15]. Subsequently, human transmission was reinforced by the reports of COVID-19, in hospital staffs [86]. The initial case in India was observed on 30th of January 2020 [32]. As of 27th of September, 2021 the world has recorded 231,703,120 confirmed cases of COVID-19, including 4,746,620 deaths, and has administered a total of 5,924,819,985 vaccine doses on 26th of September, 2021 [30]. India has recorded 33,678,786 confirmed cases of COVID-19 since January 2020 till 27th of September 2021, with 447,194 deaths, and has administered a total of 818,513,827 vaccine doses on 26th of September 2021 [36]. The recurrent advent and worldwide gauge of transmission, and deaths, and the emerging variants of the virus, have raised a global concern. An effective integrated early warning response system, to raise an opportune warning about these developing and re-emerging pathogens is required, to enable pre-emptive prediction of the disease. Various review works have studied and analysed the nature of the virus, the causes, symptoms, effects and precautionary actions to interrupt the spread of the virus [17, 24, 60, 76, 101].
The laboratory processes undertaken for the prognosis and recognition of COVID-19 such as the Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) consumes a lot of time, sometimes unreliable and is expensive. In lieu of this, many other processes of diagnoses are carried out for faster and reliable detection of COVID-19. The current swab tests are missing up to 30% of diseased people [12].
Hence, doctors have recommended the detection of COVID-19 using medical imaging such as chest Computed Tomography (CT) scans [68] or Chest X-Ray (CXR) images, especially for asymptomatic patients [9, 15, 20] or patients showing SARI symptoms or other pneumonia-like disease, for better prognosis, and for reliable and faster detection of COVID-19 [87]. The role of medical imaging is pivotal in the world of medicine, to view the anatomy of the human body, for early diagnosis, monitoring and treatment of diseases, at all major levels of health care such as respiratory diseases, lung(s) inflammation in COVID-19, etc. to drastically improve patient outcomes. The diagnostic imaging services are essential in assessing, confirming, documenting and decision making, in the course of diseases and effectiveness to treatment, thus providing patients with preventive and comprehensive care. Medical imaging such as CT scans for COVID-19 detection, can provide 3D imageries of the lungs and various cross-sectional views, for improved precision and accuracy when formulating to function on an area or whole, such as for lung transplantation in severe cases of COVID-19, thus supervising physicians through a subtle internal process. Thus, medical imaging has revolutionized the health care industry and allowed experts and researchers to absorb and analyze more, about the human body. Therefore, irrespective of the geography and location of the diseased patient(s), it is important to establish medical settings, services, and proper training and management in the use of medical imaging equipment, for improved diagnostic imaging services, for efficient and early detection of diseases such as COVID-19 [43, 78, 81]. Besides, medical imaging is less invasive with reduced in-patient procedures, painless, affordable, safe and effective with reduced complications and shorter recovery period. Additionally, with the file-sharing ecosystem and data privacy, patient data is not compromised and in due course the rate of patient exposure to radiations gets decreased due to availability of image datasets in authorized medical premises.
On March 16, 2020, the White House, teamed up with research institutions and technical companies, and called for global Artificial Intelligence (AI) researchers for development of novel techniques for COVID-19 research [6]. The use of AI and chest images will be helpful in detection of significant COVID-19 features such as hazy, patchy, ‘ground glass’ white spots in the lungs. It is found that Ground-Glass Opacities (GGOs) and consolidation with or without vascular enlargement, interlobular septal thickening and air bronchogram are the basic CT features of the disease [24]. In general, Radiologists examine the images/ chest CT scans to categorize the features of COVID-19 and to regulate the severity of the disease, which is however feasible but time consuming, unreliable, inefficient and highly prone to error. With intelligent systems, this process can be automated and intensive analysis and errors can be minimized. Thus, a faster, reliable and intelligent diagnosis and detection system can help experts and scientists in early detection of COVID-19, and thereby minimize the susceptibility of the disease and human-to-human transmission.
In this context, various works have proposed AI based models using Machine Learning and Deep Learning techniques upon high resolution chest CT scan images and chest X-Rays (CXR) images of COVID-19 patients, Community Acquired Pneumonia (CAP) patients and viral pneumonia patients, to improve diagnostic accuracy and minimize contagion. These works have preprocessed, interpreted and analyzed the images for identification of potential features of COVID-19, for feature learning, extraction and severity classification of candidate regions. Various intelligent and computer-assisted systems are proposed for COVID-19 detection using Machine Learning (ML) techniques such as Decision Tree [26], K-Means clustering [1], Support Vector Machine (SVM) [73], Neural Network, etc. Various Deep Learning(DL) techniques and architectures such as Convolutional Neural Network (CNN), Deep Convolutional Neural Network (DCNN), and Deep Neural Network (DNN) architectures such as AlexNet, Visual Geometry Group Network (VGG- 16, VGG-19), Inception V3, InceptionResNet V2, Residual Network -ResNet50, ResNet101, Densely Connected Network (DenseNet121), Autoencoder, Restricted Boltzmann Machine (RBM), Long Short-Term Memory (LSTM), Deep Reinforcement Learning (DRL) etc. are proposed for deep feature extraction and image classification, based on supervised and unsupervised approaches. Besides, hybrid models, Transfer Learning (TL) models, comprehensive and ensemble models, dimensionality reduction techniques, data balancing techniques etc. are also proposed to improve diagnostic accuracy.
This paper summarizes and introduces COVID-19 and its causes, clinical manifestations, treatment and diagnosis of COVID-19 using medical imaging, ML and DL models. The manuscript analyzes and compares different methodologies proposed for the early detection of COVID-19 and identifies various associated challenges. The paper reviews COVID-19 related medical imaging techniques, and identifies most common COVID-19 features based on diagnostic accuracy and model sensitivity. Based on the analysis, the paper identifies CT to be more reliable than CXR whereas CXR is more affordable and available than CT. In contrast to previous survey works which reviews various AI techniques for COVID-19 research and application for vaccine development, prediction and forecasting, stressing extremely less on diagnosis and early treatment using advanced techniques such as DL, this paper focuses on finding advanced solutions for early diagnosis and detection of COVID-19 based on the identification of significant and common features of COVID-19 using medical imaging, irrespective of age. The main contributions of the manuscript are:
To summarize the current state of COVID-19 and its variants worldwide, statistics of influence, choice of imaging modality, medical imaging and advancements in AI for early detection of COVID-19
To compare, identify and analyze the differences in usage of laboratory techniques such as RT-PCR, and medical imaging, and the significant reason for adoption, based on preferences and circumstances
To compare, identify and analyze the differences and the best in usage and performance, of imaging modalities such as CT and CXR for medical imaging of the lungs, consequent advantages and disadvantages in detection of COVID-19, and recognition of dissimilar as well as common and vital COVID-19 features, to prevent misclassification of lesions
To study and analyze the latest technical advancements made in detection of COVID-19 using AI such as DL techniques, hybrid mechanisms, ensemble techniques, attention mechanism etc. and identify loopholes and propose feasible solutions, on grounds of space and time complexity, model training and performance
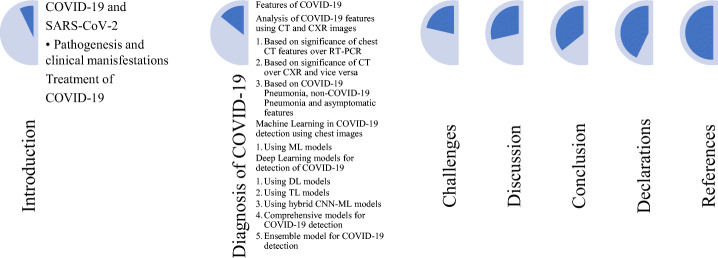
This paper is sectionalized in various sections, sub-sections and sub-sub sections. Section 1 itself gives a precise introduction on COVID-19, its inception, laboratory processes, computer-assisted diagnostic models, and medical imaging, and highlights the main contributions of the manuscript. Subsection 1.1 gives an introduction to COVID-19 and SARS-CoV-2. Subsection 1.2 states the clinical manifestations of COVID-19. Subsection 1.3 introduces various treatment adopted for detection of COVID-19. Section 2 introduces diagnosis of COVID-19 based on image features using imaging techniques such as CT and CXR, and analyzes those images to identify common as well as distinct COVID-19 features. It differentiates the two modalities to compare and identify the best medical imaging technique which can be adopted for the detection of COVID-19 using an AI-based computer-assisted intelligent system. It also highlights the importance of laboratory processes such as RT-PCR necessary for the confirmation of the disease. Section 2.1 introduces and analyzes different features of COVID-19 based on different imaging modality, and establishes the significance and choice/preference of the modality over each other based on specified situations, in different subsections. Section 2.2 introduces the significance, prevalence, and requirement for introduction and adoption of AI and advanced techniques in early detection of COVID-19. It introduces the importance of acquiring balanced image dataset for enhanced and improved ML models, hybrid models, DL models, Transfer Learning (TL) models, comprehensive evaluation models and ensemble models, proposed for the design and implementation of intelligent systems for COVID-19 detection, and compare them on the basis of performance. Section 3 identifies various challenges in diagnosis of COVID-19 using images and AI based learning models. Section 4 discusses the influence of related works in detection of COVID-19 to identify and improve the gaps so as to accelerate the performance and detection process, and analyze the importance of state-of-the-art techniques. The paper concludes on a firm note of employing DL techniques for large case studies over ML techniques, and highlights the importance of feature concatenation, deeper networks, and ensemble learning for deep image feature extraction and classification to achieve remarkable diagnostic performances using intelligent systems, for detection of COVID-19 at the earliest. The flowchart below depicts the direction and orientation of the manuscript.
COVID-19 and SARS-CoV-2
Coronaviruses are a gigantic family of viruses which can cause disease in animals and humans. Apart from SARS and MERS, the third instance of coronavirus affecting human through zoonotic transmission is the most recently discovered SARS-CoV-2 which has caused COVID-19 [44, 62]. The SARS-CoV-2 [76, 85] [33, 49, 55, 84] is a ß CoV of group 2B of the family of Coronaviridae [17] with 70% similarity in genetic sequence to SARS-CoV and > 95% homology with the bat coronavirus. Coronaviruses are enveloped positive sense Ribonucleic Acid (RNA) viruses in the range of 60 nm to 140 nm in diameter with prickle like projections on its exterior and a crown like appearance under the electron microscope [76]. The Basic Case Reproduction (BCR) rate of the SARS-CoV-2 virus, according to various modelling studies, has a range of 2 to 6.47 [76]. Today, this has an estimated median value of 5.8 within the CI range (4.7–7.3) in the USA and between 3.6–6.1 in European countries [42]. In India, BCR was 3.2 which started declining after the month of march,2020 to 1.3 and then to 1.09 and below in September 2020 [66]. At the onset of second wave, the value has started to increase again and today it has reached approximately to 1.37 [33, 57]. There is a alteration of five nucleotides between SARS and SARS-CoV-2 [68]. The variations at the level of spikes on receptor binding ligands [23, 33, 55, 85] is accountable for zoonotic spillover and crossing of the species barrier [2, 22, 24, 40, 51, 52, 56, 58, 68, 69, 76, 85, 92, 100]. The microscopic images of the structure of the SARS-CoV-2 approves the transformation in spike glycoprotein of SARS-CoV-2 [68]. Besides, there is about 89% resemblance with the genomic sequence of bat-SL-CoVZC45 and bat-SL-CoVZXC21, as consumption of game animals is traditionally acceptable in China, which may have also exemplified the existence of a bridging host to the spread of the virus from bats to human beings [8]. In the recent waves of COVID-19, SARS-CoV-2 has exhibited dynamic [71, 82] behaviour in the form of variants, which has caused more drastic effect.
Pathogenesis and clinical manifestations
The preliminary symptoms [24] at the onset of illness for the identification of COVID-19 are shortness of breath, loss of smell, loss of taste, fever (99%), fatigue (70%), dry cough (60%), myalgia (44%), chest pain, bluish skin, pharyngeal pain, abdominal pain, anorexia and dyspnoea. Majority of the cases have reported symptoms such as development to viral pneumonia, numerous organ failure, cytokine storm, liver damage, aches and pains, nasal congestion and conjunctivitis [76, 95, 99]. The most common complications of COVID-19 are arrhythmias, acute cardiac injury, shock, acute respiratory distress syndrome, and acute kidney injury [26, 31, 35]. Cytokine storm syndrome is related with widespread inflammation in response to SARS-CoV-2 infection, and is the principal reason of death of COVID-19 patients [18, 24, 35, 54]. SARS-CoV-2 infection in pregnant women may not cause intrauterine transmission but vertical transmission to neonates is probable [24, 70, 72, 88]. Amongst the laboratory identified abnormalities in chest/thorax of COVID-19 patients are bilateral patchy shadows [18] and Ground-Glass Opacities (GGO). Lung abnormalities such as desquamation of pneumocytes, hyaline membrane formation, bilateral diffused alveolar damage and presence of cellular fibromyxoid exudates [35] may indicate COVID-19 in patients.
Treatment of COVID-19
COVID-19 is contagious in nature. Today, we have various vaccines [61] and treatments [83] for the disease. However, there are numerous constant medical trials still assessing possible treatments for COVID-19 with emerging variants of SARS-CoV-2 [71, 82]. The treatment of COVID-19 diagnosed patients are carried out through proper maintenance of hygiene, body hydration and nutrition, and monitoring of oxygen levels, fever and cough [76]. The patients with severe symptoms and hypoxic patients are treated with oxygen through nasal prongs, face mask, High Flow Nasal Cannula (HFNC) oxygen therapy or non-invasive ventilation, intravenous methylprednisolone and intravenous adrenaline [68]. COVID-19 is a medical emergency which requires a reliable and intelligent diagnosis system for early detection using chest images, as manual analysis and examination of patients is feasible but time consuming. Thus, to identify features and patterns of COVID-19 prior to its formation and avoid severe impacts on lungs and other organs of the body, severity classification is necessary beforehand which can only be done using a smart, automated and intelligent system relying on medical images of the thorax and lungs.
Diagnosis of COVID-19
COVID-19 is commonly detected through molecular swab tests such as real-time Reverse Transcription Polymerase Chain Reaction (RT-PCR) [68]. The clinical sample constitutes nasopharyngeal swab or expectorated sputum, endotracheal aspirates and bronchoalveolar lavage fluid [76] or oropharyngeal swabs collected using Dacron swabs, to detect the coronavirus’s genome. The clinical samples are ensured with safety storage measurements to avoid contamination, minimize risks and ensure accuracy of diagnosis [44]. Additionally, and alternatively, medical imaging such as Computed Tomography (CT) scans and chest X-Ray (CXR) images are employed for the early detection of COVID-19 [13, 16, 21, 25, 93, 96, 97] to improve reliability and efficiency of outcomes. Besides, RT-PCR used for the diagnosis of COVID-19 has limitations such as lengthy turnaround times and variations in sensitivities. Thus, medical imaging can be useful for identification of distinctive features of COVID-19 in patients and for corresponding severity classification of the disease.
Features of COVID-19
Using CT scans and CXR images, various features are identified and taken into account for the detection of COVID-19. CT scan image features such as GGO, consolidation, number of lobes affected, pulmonary nodules, pleural effusion, occurrence of thoracic lymphadenopathy,airways abnormalities, axial distribution of disease, emphysema or fibrosis, lung cavitation, linear opacities, rounded morphology, ‘reverse halo’ sign, ‘crazy-paving’ pattern, reticulation/thickened interlobular septa, mixed pattern and honeycomb pattern, lesion distribution, peripheral distribution, vascular thickening, right or bilateral lungs and intralesional cavitation, subsegmental vessel enlargement, pleural and pericardial effusion, bilateral pneumonia, bilateral pulmonary, consolidative pulmonary opacities, parenchymal ground-glass, peripheral lung distribution, striking peripheral distribution, posterior or lower lobe involvement predilection -[1, 3, 5, 10, 11, 13, 14, 34, 53, 80, 89, 90, 93, 94, 98, 102] etc. In an asymptomatic case, patient has been identified with chest CT abnormalities resembling viral pneumonia, patchy bilateral GGO with peribronchial and peripheral/subpleural distribution, severe pneumonia, and acute respiratory distress syndrome [60].
Analysis of COVID-19 features using CT and CXR images
COVID-19 is a novel disease and identification of prominent features using medical imaging is important as well as challenging. The process of accurate image-based diagnosis of an ailment depends completely upon chest image data acquisition, analysis and interpretation. Image processing plays a vital role in preprocessing the high-dimensional image data through denoising, illumination correction, focus correction, image filtering, contrast enhancement, restoration, segmentation, thresholding, edge detection, region processing, point processing, math and statistical processing and color space conversions, etc. for better identification and extraction of local and global features. The following figures illustrate the different features present in CXR and CT scan images, obtained from analysis performed in earlier works. Figure 1 depicts normal chest X-Rays [29]. Figure 2 depicts CXR images of COVID-19 viral infection [89].
Flowchart 1.
Direction and Orientation of the manuscript
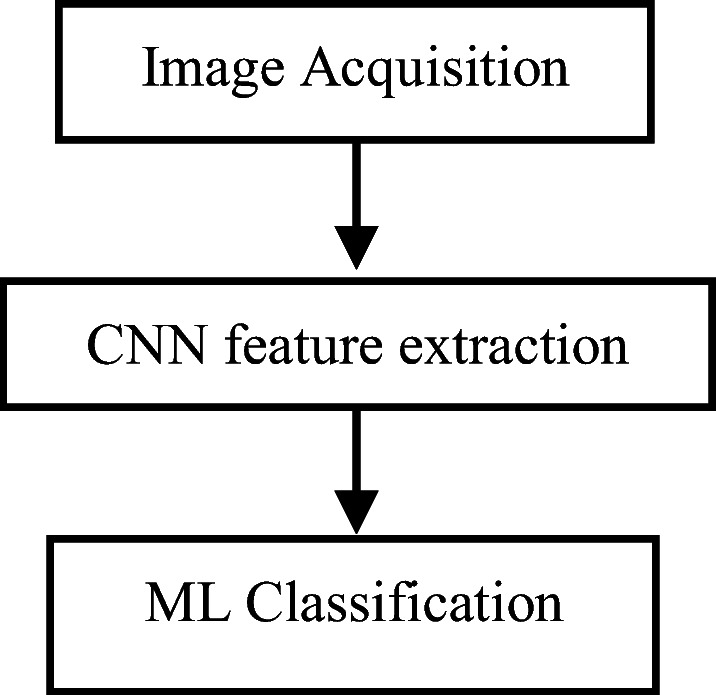
Block Diagram 1.
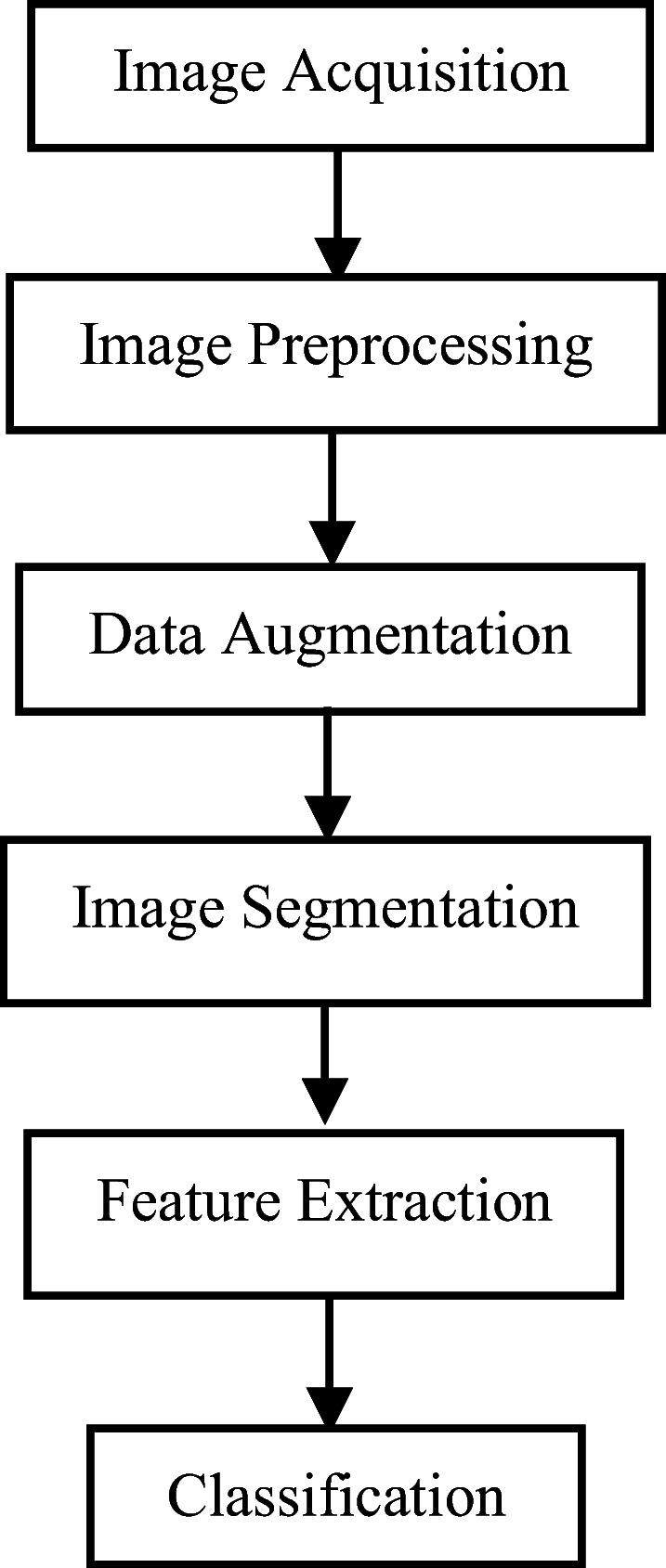
ML framework for COVID-19 detection
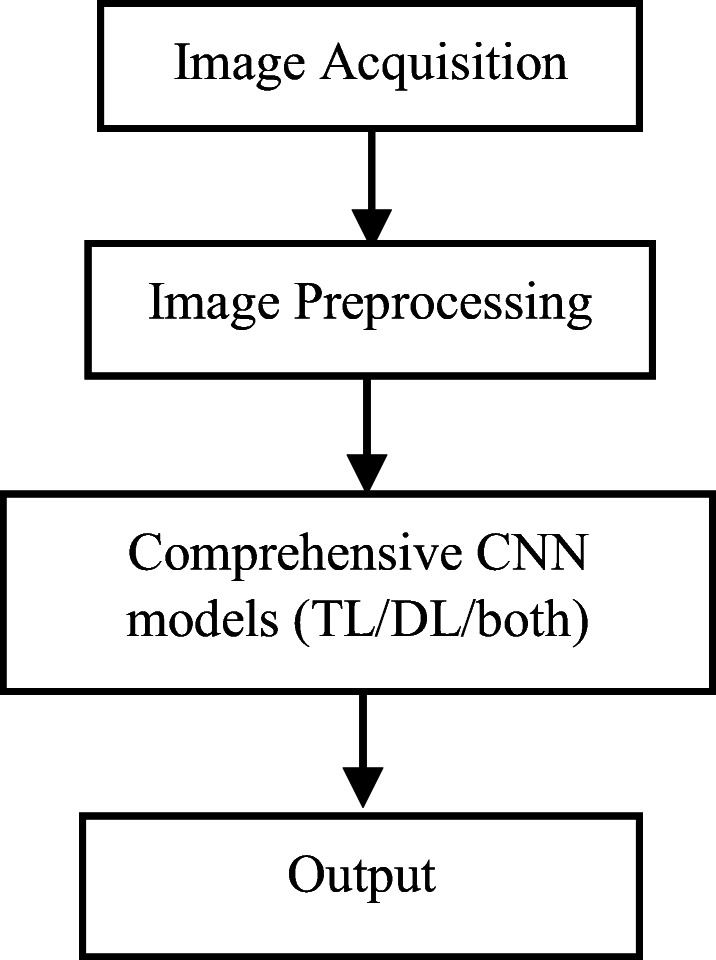
Block Diagram 2.
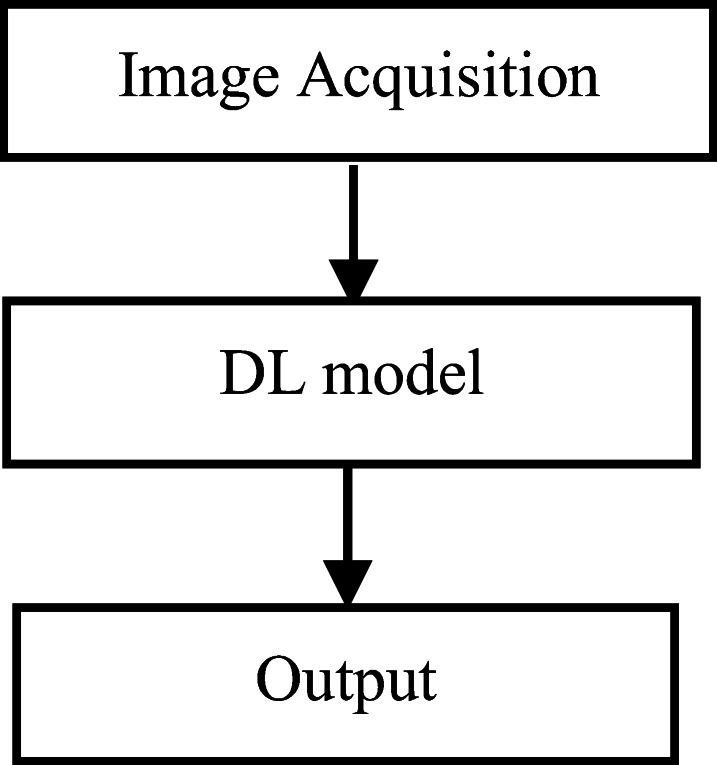
DL framework for COVID-19 detection
Fig. 1.

Example normal chest X-Rays [29]
Fig. 2.

CXR images of COVID-19 infection [89]
a. Based on significance of chest CT features over RT-PCR
The diagnosis process of COVID-19 using CT scans are described to be less precise than RT-PCR but it is estimated to have a high sensitivity in detecting COVID-19 and hence, it can play a fundamental role in the disease diagnosis/treatment [35]. Zu et al. [101] have investigated, reviewed and identified CT patterns for detection of COVID-19, such as posterior or lower lobe involvement predilection, peripherally distributed multifocal GGOs with patchy consolidations etc.
Bernheim et al. [13] have characterized chest CT findings in 121 confirmed COVID-19 diseased patients in China, in association to the time amid symptom commencement and the original CT scan. This study has recognized features such as Ground-Glass Opacities (GGO), consolidation, number of lobes affected, degree of involvement of each lung lobe, pulmonary nodules, pleural effusion, presence of thoracic lymphadenopathy, airways abnormalities, axial distribution of disease, lung disease such as emphysema or fibrosis, lung cavitation, linear opacities, rounded morphology, ‘reverse halo’ sign, ‘crazy-paving’ pattern and intralesional cavitation.
Ai et al. [3] have examined the diagnostic value and uniformity of chest CT in contrast to RT-PCR assay, on 1014 patients from Wuhan, China. This work has analyzed various features such as GGO, consolidation, nodules and lesion distribution in left, right or bilateral lungs, reticulation/thickened interlobular septa, etc. from the CT scans. The study has found 97% of cases have confirmed positive findings with chest CT, compared to RT-PCR with a positive rate of 59%. The study has reported errors encountered in RT-PCR due to sampling operations, specimens’ source, sampling timing and performance of detection kits. This work has reported CT images to be more efficient than RT-PCR.
Caruso et al. [14] have studied the chest CT features of 158 patients in Rome and Italy, and have compared the results with RT-PCR. The patients of COVID-19 pneumonia have shown continuous existence of peripheral GGO accompanying multilobe and posterior involvement, subsegmental vessel enlargement, bilateral distribution etc. The CT scans of 89% of COVID-19 pneumonia patients have reflected a common subsegmental vascular enlargement in areas of lung opacity having unclear etiology. This work has also identified various other CT features such as consolidation, cavitation, air bronchogram, interlobular septal thickening, pleural and pericardial effusion, pulmonary nodules, halo sign, bronchial wall thickening, perilesional vessel diameter, lymphadenopathy, bronchiectasis, using a significantly small dataset.
b. Based on significance of CT over CXR and vice versa
It is often not recommended to use CT scans as a first-line test without confirmed RT-PCR positive results and COVID-19 symptoms, out of concern for consequential health hazards. On the other hand, CXR is considered to have high sensitivity for significant clinical findings, less expensive than CT and hence are highly used for practice, in addition to its easy availability [46]. However, portable CXRs may incur a cost on radiological proficiency, often deficient in regions with inadequate resources. Therefore, computerized decision-making tools can be of value in making the diagnosis process feasible, for quantifying disease progression [35]. Qian et al. [63] have surveyed an early casualty caused by severe pneumonia and severe acute respiratory syndrome (SARS) disease in a 44-year-old Huanan Seafood Market worker. The Chest CT of the worker has shown features such as patchy bilateral GGO with peribronchial and peripheral/subpleural distribution. He was clinically diagnosed based on CXR images and was suspected as a case of COVID-19 infection. This study has recommended chest CT scan as an important diagnostic tool for confirmation of COVID-19 when real-time RT-PCR is unavailable or when CXR results are not promising. Another patient case visualization, has shown focal opacities and larger diffuse opacities using CXR images on feature identification of COVID-19 [69]. A transverse CT scan of a 68-year-old man with COVID-19 has shown ‘reversed halo’ sign in left lower lobe of the chest [50]. In another transverse CT scan of a 77-year-old woman with COVID-19 has shown multiple GGO and consolidation, with thickened intralobular and interlobular septum, air trapping and air bronchogram sign [50]. A minimum-intensity-projection CT image of a 66-year-old man with COVID-19 has shown strip like lesions and bronchus deformation due to fibrosis [50].
Table 1 gives an overview of earlier works on COVID-19 using RT-PCR and radiological images. It identifies and compares the most common features of COVID-19 along with the less likely features. It is observed that features such as GGO, consolidation, affected number & degree of lobes, interlobular septal thickening, pleural effusion (1:4), thoracic lymphadenopathy (1:2), posterior part or lower lobe involvement predilection, cavitation, opacities, lesion distribution, pulmonary nodules and vascular thickening are the most common features in CT imaging. In CXR and CT, GGO [13, 28] and pleural effusion are the common features of COVID-19. The fact that pleural effusion and thoracic lymphadenopathy, being less likely feature of COVID-19 is not justified as the ratio of being a less likely feature to that of being a more likely feature is 1:4 and 1:2 respectively, based on the study and analysis performed. Therefore, it can be established that pleural effusion identified using CT and CXR, and thoracic lymphadenopathy identified using only CT, are also amongst the most common imaging features of COVID-19. Based on the observations of CT scan images and CXR images for identification of COVID-19 features, CT images can quickly and efficiently detect the disease in comparison to CXR images.
Block Diagram 3.
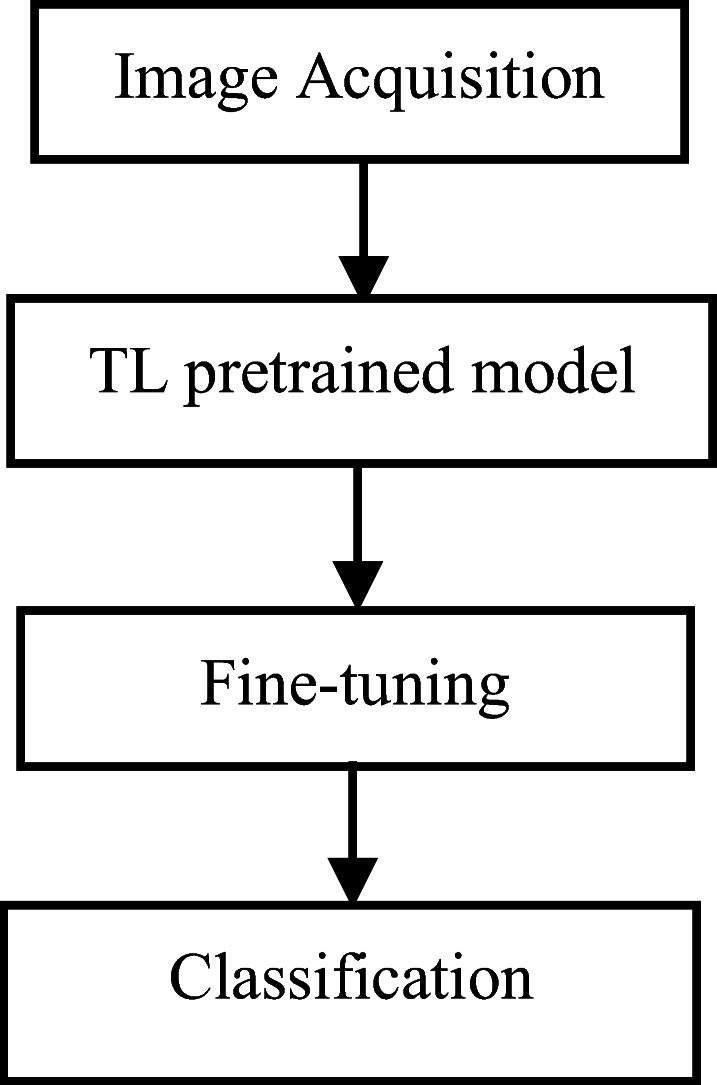
TL framework for COVID-19 detection
Table 1.
Detection of COVID-19 using CT scans and CXR images to identify common features
| Paper | Images | Features | Result | Inference |
|---|---|---|---|---|
| Ng et al. [60] | CT and Chest X-Ray (CXR) images from 21 cases | Patchy bilateral GGO with peribronchial and peripheral/subpleural distribution | CXR lack sensitivity than CT | Asymptomatic |
| Zu et al. [101] | CT | Peripherally distributed multifocal GGOs with patchy consolidations and posterior part or lower lobe involvement predilection | CT outperforms RT-PCR | ------ |
| Wang et al. [87] | 366 chest CT images from 90 patients | GGO, consolidation, reticular pattern, mixed pattern, honeycomb pattern,pleura effusion, pneumothorax and mediastinal emphysema | CT sensitivities increases from 84% to 99%. | ------ |
| Bernheim et al. [13] | 121 Chest CT images | GGO, consolidation, affected number & degree of lobes, pulmonary nodules, pleural effusion, thoracic lymphadenopathy, airways abnormalities, axial distribution, emphysema or fibrosis, lung cavitation, linear opacities, rounded morphology, ‘reverse halo’ sign, ‘crazy-paving’ pattern and intralesional cavitation. | RT-PCR is positive even in patients with normal chest CT | ------ |
| Ai et al. [3] | chest CT images of 1014 patients | GGO, consolidation, reticulation/thickened interlobular septa, nodules and lesion distribution in left, right or bilateral lungs | RT-PCR CI of 95%, sensitivity 97% | ------ |
| Bai et al. [10] | Chest CT images of 424 patients |
Peripheral distribution, GGO, fine reticular opacity, and vascular thickening Less likely features: central distribution, pleural effusion, lymphadenopathy |
High specificity but moderate sensitivity | Small cohort size, biased. |
| Caruso et al. [14] | Chest CT images of 158 patients | GGO, consolidation, multilobe involvement, bilateral distribution, pulmonary nodules, interlobular septal thickening, air bronchogram, halo sign, cavitation, bronchial wall thickening, bronchiectasis, perilesional vessel diameter, lymphadenopathy,pleural and pericardial effusion. | Sensitivity 97% | ------ |
Fig. 3 depicts a comparison of CXR (image A) and CT thorax coronal image (image B). The GGO in the right lower lobe periphery on the CT (red arrows) are not visible on the CXR, taken an hour apart from the first study [60].
Block Diagram 4.
Hybrid CNN-ML framework for COVID-19 detection
Fig. 3.
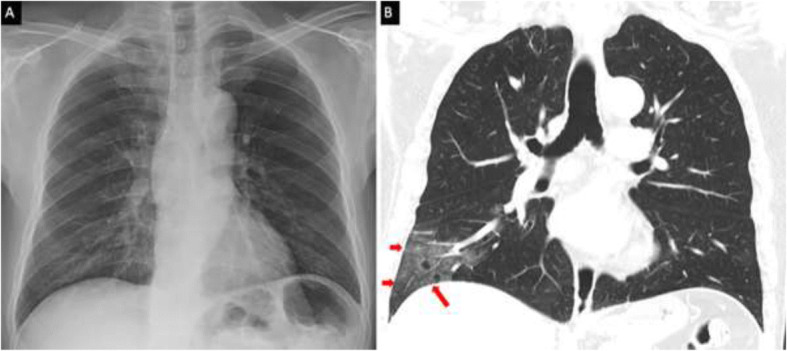
Comparison of Chest X-Ray (image A) and CT thorax coronal image (image B). The GGO in the right lower lobe periphery on the CT (red arrows) [21]
c. Based on COVID-19 pneumonia, non-COVID-19 pneumonia and asymptomatic features
Bai et al. [10] have reported a total of 424 patients which includes 205 non-COVID-19 pneumonia patients from the U.S. and 219 COVID-19 patients from China, using RT-PCR and abnormal chest CT findings. The study has compared the two cases and identified COVID-19 pneumonia features such as fine reticular opacity, GGO, peripheral distribution, and vascular thickening, and less likely features such as central and peripheral distribution, lymphadenopathy and pleural effusion. The study has certain limitations such as small cohort size and selection biasness. Another study using transverse-section of CT images has compared COVID-19, Influenza-A viral pneumonia and ‘no pneumonia’ manifestations [94]. Another study has confirmed COVID-19 manifestations such as consolidation in the left lower lobe apical segment, in a 10-year-old asymptomatic child [60].Wang et al. [87] have performed a study on 366 CT findings from 90 COVID-19 pneumonia patients and have assessed the presence of features such as GGO, consolidation, reticular pattern, mixed pattern, honeycomb pattern, pleura effusion, pneumothorax and mediastinal emphysema. The study has identified 94% of patients, who are discharged had insignificant to considerable residual lung aberrations (GGO). This work has highlighted the fact that patients can still have milder lung abnormalities while imaging and can show symptoms even after clinical recovery from COVID-19.
Machine learning (ML) in COVID-19 detection using chest images
The large-scale data of COVID-19 patients can be combined and analysed by cutting-edge ML algorithms to advance diagnostic rapidity and accuracy, for the development of effective therapeutic approaches, for potential identification of vulnerable people based on modified genetic and physiological characteristics. Fortunately, advanced ML techniques have found application in classification of COVID-19 genomes, discovering potential drug candidates against COVID-19, survival prediction, CRISPR-based COVID-19 detection assay, etc. [6]. Above all, ML techniques and advancements have made tremendous progress in medical imaging which has found a huge platform for application in detection of COVID-19 at an early stage with supportive RT-PCR results. ML advancements and applications have showcased state-of-the-art results in detection accuracy of COVID-19 and with newer architectures proposed in recent works done. Some of these recently proposed models are discussed below:
Using ML models
Various intelligent and computer-assisted systems are proposed for COVID-19 detection using ML techniques such as Decision Tree [26], K-Means clustering [50], SVM, Neural Network, etc. Elaziz et al. [27] have proposed a ML method for detection of COVID-19 using two CXR image-based dataset which consists of 216 COVID-19 positive images and 1675 COVID-19 negative images, and 219 COVID-19 positive images and 1341 COVID-19 negative images, respectively. The model has extracted the features using Fractional Multichannel Exponent Moments (FrMEMs), and has used a multi-core computational framework to accelerate large-dataset computational process. It has proposed a differential evolution based improved Manta-Ray Foraging Optimization method for selection of significant features, and KNN classifier for classification. The model has achieved accuracy of 96.09% and 98.09%, upon the respective datasets. The proposed approach is compared with the performance of MobileNet upon the same datasets, and has achieved comparatively better classification performance. Lalmuanawma et al. [45] have proposed a study on applications of ML and AI in the detection of COVID-19 for developmental studies and methodologies such as clinical decision support systems, diagnosis and treatment, contact tracing, and prediction and forecasting. The study has identified various learning paradigms such as SVMs, Deep Learning Neural Networks (DLNNs), regression, eXtreme Gradient Boosting machines (XGBoost), DL LSTM network, ensemble techniques, Random Forest algorithm etc. for diagnosis, prediction and forecasting of COVID-19. Block diagram 1 depicts the ML framework which clearly states that ML techniques are manual processes in each stage and has higher model training time. Since, traditional ML techniques are incompetent against real-time, large, complex, and high-dimensional data such as images, and lacks domain awareness and data representation, makes ML models computationally intensive and inflexible in performance. Therefore, DL models are proposed to overcome the limitations of ML models.
Deep learning (DL) models for detection of COVID-19
Manual process of analysis and detection of COVID-19 increases the spread and susceptibility of the disease. Therefore, fast growth of computerized diagnostic systems can contribute to augmented diagnostic accuracy and speed as well as shield health care workers and others by declining their interactions with COVID-19 patients [6]. Various DL techniques and architectures such as Convolutional Neural Network (CNN), Deep Convolutional Neural Network (DCNN), and Deep Neural Network (DNN) architectures such as AlexNet, Visual Geometry Group Network (VGG- 16, VGG-19), Inception V3, InceptionResNetV2, Residual Network -ResNet50, ResNet101, Densely Connected Network (DenseNet121), Autoencoder, Long Short-Term Memory (LSTM), Restricted Boltzmann Machine (RBM), Deep Reinforcement Learning (DRL) etc. are proposed for deep feature extraction and image classification, based on supervised and unsupervised approaches [4]. CNN-based structures are modelled and designed using multiple layers, pooling techniques, activation functions, dimensionality reduction techniques etc. for feature description, feature representation and parameter optimization. Therefore, intelligent systems can be designed on the basis of image processing and learning techniques for efficient feature extraction and classification, using small as well as large datasets, for the detection of COVID-19.
Using DL models
Jadhav et al. [37] have proposed an explainable DL platform using comprehensive data visualization techniques to incorporate a pipeline system for automatic lung and lesion segmentation using a pre-trained U-Net, to identify subtle lesions, ResNet18 based feature extraction, and multiple instance learning based classification, for the diagnosis and detection of COVID-19.
Lee et al. [47] have proposed an explainable DL model using fine-tuned VGG-16 and VGG-19 upon CXR images extracted from NIH CXR dataset and 1821 images extracted from RSNA Pneumonia Detection Challenge dataset, for detection of COVID-19 to establish a comparative evaluation and perform image classification. The model has used CLAHE for preprocessing followed by resizing, and visualization of the data using Gradient-weighted Class Activation Mapping (Grad-CAM). The model has compared the 6 fine-tuned sub-blocks of each of VGG-16 and VGG-19, in which block 2 of VGG-16 (VGG16-FT2) model has achieved comparatively maximum performance in COVID-19 classification with an accuracy of 95.9% and AUC of 0.950.
Rahimzadeh et al. [64] have proposed a feature concatenation method using Xception and ResNet50V2, for detection of COVID-19 using balanced datasets of pneumonia and normal cases, using 3783 CXR images. The proposed concatenated feature extraction network has performed better in detecting COVID-19 eliminating false cases, and outputs an overall better accuracy.
Dansana et al. [23] have proposed a CNN method for evaluation of a total of 360 CXR and CT scan images, and has evaluated the performances of VGG-19, Inception V2 and decision tree model, for detection of COVID-19. The fine-tuned VGG-19, Inception V2, and decision tree model employed have achieved a validation accuracy of 91%, 78% and 60%, respectively, upon the preprocessed image data and their corresponding vectorized feature maps.
Rajaraman et al. [65] have proposed an approach to train CNN-based algorithms to detect COVID-19 infections using weakly- labelled and augmented CXR images obtained from widely available databases namely Pediatric CXR dataset, Montreal COVID-19 CXR dataset, CheXpert CXR dataset, RSNA CXR dataset, Twitter COVID-19 CXR dataset, and NIH CXR-14 dataset. The model has used a discriminative training data augmentation strategy to expand the feature space and assess the performance of the randomly initialized Wide Residual CNN (WRCNN) for classification. The model has used preprocessing, Gradient-weighted Class Activation Maps (Grad-CAM) and U-Net for lung ROI visualization and segmentation, respectively. It has also evaluated pretrained and fine-tuned CNN models viz.VGG-16, Inception-V3, Xception, DenseNet-121 and NasNet-Mobile. On comparison, the proposed WRCNN has achieved an accuracy of 89.74% whereas VGG-16 has achieved an accuracy of 93.08%, and NasNet-Mobile has achieved the highest sensitivity of 97.53%, while classifying the Pediatric CXR dataset.
Shah et al. [74] have proposed a modified DL CNN named CTnet-10 for diagnosis of COVID-19 using 739 CT scan images and has achieved an accuracy of 82.1%. The model has comprehensively evaluated various other DL models such as DenseNet-169, InceptionV3, ResNet-50, VGG-16 and VGG-19. The model has used image augmentation and fine-tuning techniques, and has achieved a comparatively higher accuracy of 94.52% for VGG-19. The proposed model has achieved a lower execution time of 0.01233 s compared to VGG-19, InceptionV3 and DenseNet-169.
Tan et al. [79] have proposed a DL algorithm for diagnosis of COVID-19 based on super-resolution reconstructed images of 470 original chest CT images, and VGG-16 based image classification. The model has emphasized on improving the image data quality using pretrained Super Resolution Generative Adversarial Network (SRGAN) to enhance VGG-16 classification accuracy. The model has achieved an accuracy of 97.9% and sensitivity of 99%.
Shan et al. [75] have proposed to develop a DL-based 3-D CNN called VB-Net/combination of V-Net [94] for segmentation and quantification of infected regions from chest CT scans of 549 COVID-19 patients.
Wang et al. [89] have proposed COVID-Net, a Deep Convolutional Neural Network (DCNN) for the recognition of COVID-19 cases from 13,800 CXR images across 13,725 patient cases obtained from COVIDx dataset. The proposed, pretrained COVID-Net on ImageNet dataset, has used generative synthesis, and has achieved a Positive Predictive Value (PPV) of 96.4%.
Zhang et al. [98] have proposed to develop a ResNet18-based classification and an anomaly detection model for screening of COVID-19, using 1531 X-Ray images. The methodology has used Gradient-weighted Class Activation Mapping (Grad-CAM) method, to make predictions. The experimental results have shown that the developed model can distinguish COVID-19 cases with a sensitivity of 96%.
Li et al. [53] have proposed a COVID-19 detection neural network (COVNet) using ResNet50, which uses 4536 chest CT images and accurately detects and differentiates COVID-19, from Community Acquired Pneumonia (CAP) and other lung diseases. The model has performed U-Net based segmentation upon preprocessed CT scan for extraction of features. The methodology has obtained a sensitivity of 90% for the detection of COVID-19, and a sensitivity of 87% for the detection of CAP.
Xu et al. [94] have proposed a DL model to distinguish COVID-19 pneumonia from Influenza-A viral pneumonia and healthy cases, with a total of 618 pulmonary CT images, each. The methodology has used a Fully Convolutional Neural Network (FCNN) for volumetric medical image segmentation and classification. The model has identified features such as ground-glass appearance, striking peripheral distribution for the detection of COVID-19. The methodology has also used a classical ResNet-18 for image feature extraction and two 3-D Convolutional Neural Network (CNN) for classification. The model has achieved an overall accuracy of 86.7%.
Block Diagram 2 depicts a DL framework for detection of COVID-19 which takes the input image dataset and gives the output. The DL model is a complete black-box and all the operations such as preprocessing, feature extraction, classification, generalization on unseen data, fitting upon data, reducing dimensions of features for compact and simple representation, generation of feature vectors and probability maps, etc. are carried out transparently. Here, image processing and data augmentation phases can be introduced prior to DL for accelerating the performance of the model. The data can be visualized using data visualization techniques such as heatmaps and gradient mapping, to improve the explanation ability of the model. Such models have higher training time but produces efficient and reliable outcomes, when properly parameterized and tuned.
Using transfer learning (TL) models
Various pre-trained DL models also known as TL techniques have found application for early detection of COVID-19, using smaller datasets to minimize and handle dataset imbalance, and to overcome intensive training of DL architectures using larger datasets, for boosting the classification performance.
Narin et al. [59] have proposed a TL model for detection of COVID-19 using a pre-trained Deep Convolution Neural Network (DCNN) upon 100 CXR images. The study has employed ResNet50, InceptionV3 and Inception-ResNetV2 pre-trained models. The ResNet50 model has achieved the highest classification performance with 98% accuracy compared to InceptionV3 with an accuracy of 97% and Inception- ResNetV2 with an accuracy of 87%.
Jaiswal et al. [39] have proposed DenseNet201 based Deep Transfer Learning (DTL) model for detection of COVID-19 using chest CT images and extracts features using its individual learned weights on the ImageNet dataset, for efficient training and feature reuse. The proposed model is compared with VGG16, ResNet152V2, and Inception-ResNetV2, upon 2492 CT scans. The proposed DTL with DenseNet201 has achieved an AUC of 0.97.
Aslan et al. [7] have proposed an AlexNet (mAlexNet) based two DL pretrained architectures for automated detection of COVID-19 using 2905 CT images and performs ANN based lung segmentation trained using Levenberg–Marquardt backpropagation method upon 50 images. The model has proposed the latter from the two DL models as a hybrid ML-DL model containing two consecutive Bidirectional Long Short-Term Memories (BiLSTM1, BiLSTM2). The proposed model has achieved accuracy rates of 98.14% and 98.70% for mAlexNet and mAlexNet+BiLSTM, respectively.
Jain et al. [38] have proposed a two-stage modified pretrained TL model using ResNet50 and ResNet101, upon an augmented set of 1832 CXR images for the detection of COVID-19. The model performs resizing followed by preprocessing and augmentation of the original images, for deep feature extraction and classification. The model has achieved classification accuracy of 93.01% on test dataset using ResNet50, and a classification accuracy of 97.78% on test dataset using ResNet101.
Sitaula et al. [77] have proposed an attention-based end-to-end pretrained TL VGG-16 model and VGG-19 model, to obtain the spatial relationship between the ROIs in CXR images and perform fine-tuning in the classification process, for detection of COVID-19. The model has used 3255 CXR images of different categories such as Covid, Normal, No_findings, Pneumonia Bacteria, and Pneumonia Viral. The model results are compared with Inception-ResNetV2 and has achieved comparatively better performance with an accuracy of 87.49% for VGG-16 and an accuracy of 85% for VGG-19.
Wang et al. [90] have proposed a TL based Inception model and Decision tree-based ensemble to detect COVID-19 on radiographical changes in CT images. The methodology has used a total of 453 CT images of COVID-19 cases along with formerly identified viral pneumonia. The proposed model has achieved a sensitivity of 87.1%.
Block Diagram 3 depicts a pretrained TL framework for detection of COVID-19, to overcome data scarcity, computational constraints, larger parameters and larger training time of DL models. Such models can be used in lieu of DL models and need not require additional model building and training.
Using hybrid CNN-ML models
Sethy et al. [73] have proposed a DL-based CNN methodology and SVM-based classification for detection of coronavirus infected patient using CXR images available in the repository of GitHub, Kaggle and Open-i. The methodology has extracted deep features using 11 CNN-based DL architectures such as AlexNet, Visual Geometry Group Network −16 (VGG16), InceptionV3, InceptionResNetV2, ResNet50, GoogleNet, ResNet18, ResNet101, VGG19, DenseNet201 and Xception. The model has achieved higher accuracy using ResNet50 and SVM in comparison to other classification models.
Abbas et al. [1] have proposed a transfer learning model named DeTraC-ResNet18 based on their previous CNN model called Decompose, Transfer, and Compose (DeTraC), using pretrained ResNet18 for the detection of COVID-19 upon 80 CXR images, 105 samples of COVID-19 and 11 samples of SARS. The model has used pre-trained AlexNet for deep feature extraction along with Principal Component Analysis (PCA), and K-Means clustering based class decomposition task. The DeTraC-ResNet18 model has detected COVID-19 with an accuracy of 95.12%, whereas ResNet18 has achieved an accuracy of 92.5%.
Block diagram 4 depicts hybrid CNN-ML framework for detection of COVID-19. The phase of image processing is optional while using CNN. A hybrid model can employ ML classifier(s) as learning algorithm(s), thereby substituting fully connected dense classifiers, to reduce large number of training parameters.
Comprehensive models for COVID-19 detection
Kamal et al. [41] have proposed a TL model for recognition of COVID-19 using 760 CXR images and increased trainable parameters. The model has comprehensively evaluated CNNs such as VGG-19, InceptionV3, ResNet50, ResNet50V2, MobileNet, MobileNetV2, DenseNet121 and NasNetMobile. The finetuned DenseNet121 model performs better and has achieved 98.69% test accuracy and highest macro f1-score of 0.99, on CXR-B dataset.
Horry et al. [34] have proposed a DL based pretrained TL VGG-19 model using CXR, Ultrasound, and CT scan images upon comparison with VGG-16, Xception, InceptionResNet, Inception V3, NasNetLarge, DenseNet121 and ResNet50V2, for detection of COVID-19. The model concludes that ultrasound images provide superior detection accuracy compared to CXR and CT scans with a sensitivity of 100%, 86% and 83%, respectively. The model has used sampling, N-CLAHE and data augmentation for preprocessing. Besides, the model suffers from overfitting during the initial epochs of training while using the DL models except for VGG.
Ardakani et al. [5] have comprehensively evaluated pre-trained CNNs to detect COVID-19 such as ResNet-101, AlexNet, ResNet-18, MobileNet-V2, VGG-16, ResNet-50, SqueezeNet, VGG-19, GoogleNet, and Xception upon 1020 preprocessed CT images, of which two best-performing CNNs, ResNet-101 has achieved sensitivity of 100% and accuracy of 99.51% whereas Xception has achieved sensitivity of 98.04% and accuracy of 99.02%, compared to the radiologists’ sensitivity of 89.21% and accuracy of 86.27%.
Block Diagram 5 depicts a comprehensive model for evaluation and comparison of various DL or TL models upon a single dataset or upon various folds of dataset, and has analyzed the best performance of the model. However, such a model is time-consuming initially and requires proper tuning and modification, for each individual network.
Ensemble model for COVID-19 detection
An ensemble-based model is a group of weak as well as strong feature extractors or classifiers, which can be used to obtain multiple and new predictions, and perspectives to consider, analyze and interpret, the final average outcome. An ensemble model considers all pros and cons of a detection methodology, and identifies different perspectives to obtain and understand unknown predictions such that generalization is easy and overfitting of the model is comparatively less. It helps in eradication of misclassification and gives better and enhanced results. The motif of such a method is to boost the performance of the model through consideration and prediction of previously unseen behaviours, thereby overcoming the drawbacks of a single-classifier based classification system. It helps in exhaustive feature extraction and/or classification thereby enhancing domain knowledge of the model. It also helps in elimination of highly-parameterized dense classifiers and gives promising predictions, correct and better error rate, low bias, low variance and low generalization error. The main idea is to incorporate such ensemble DL techniques for exhaustive feature extraction and classification, to output efficient results for early detection of COVID-19.
Chowdhury et al. [19] have proposed a TL based ensemble of DCNNs based on EfficientNet named ECOVNet, to detect COVID-19 using a large CXR image dataset. The proposed model has compared and highlighted the importance and advantages of using data augmentation and an ensemble model for better prediction, low error rate and lower generalization error to that of a single model. The proposed model ECOVNet has achieved the highest accuracy of 96.26% with EfficientNet-B5 and data augmentation, and an accuracy of 94.68% with EfficientNet-B5 and without data augmentation.
Block diagram 6 depicts three different ensemble learning frameworks for detection of COVID-19. Block diagram 6(a) depicts a ML/CNN ensemble framework for feature concatenation, and predictions, using handcrafted ML algorithms or using DL CNN architectures for deep feature extraction and selection. The final predicted features may be given as input to a ML classifier such as SVM or a DL dense classifier such as Deep Neural Network (DNN) or Fully Connected Networks (FCN). Block diagram 6(b) depicts an ensemble classification framework which takes the input from a single CNN feature extractor and obtains multiple classification predictions on extracted features using different kinds of ML or DL classifiers, and then obtain the final average classification prediction. Block diagram 6(c) depicts concatenation of block diagram 6(a) and 6(b) which employs ML or DL based features extractors in an ensemble format and obtains multiple predictions on feature extraction. The linear average of all the predictions of the ensemble can be given as input to the ensemble classification framework. The ensemble classification framework similarly obtains multiple predictions on the ensemble feature output, to obtain the final linear average classification prediction. The analysis of all the three frameworks states that 6(b) may take the least time to train and develop the model and is less complex than 6(a) followed by 6(c). Experimental evaluation of 6(a) and 6(c) may demand huge number of resources and high computation. Besides, there are constraints of parameter optimization and feature incompatibility due to varied architectures, sample size incompatibility, and hence classification predictions may vary to that of estimated results. However, with such complex architectures and non-linearity in the problem, generalization rate can be improved and overfitting can be reduced.
Table 2 gives an overview of the works done in the detection of COVID-19 using ML-DL, DL, TL and ensemble techniques using CT scan images and CXR images. It is observed that ResNet101 has a better accuracy for detection of COVID-19 using both CT and CXR images [5, 38]. ResNet50 is highly sensitive towards detection of COVID-19 using both CT and CXR images [53, 73]. DL based segmentation architectures and data visualization techniques have shown the importance of similarity measurements in extraction and identification of features, respectively. Additionally, preprocessing of images and fine-tuning of the models have an impact in achieving better COVID-19 detection results.
Block Diagram 5.
Comprehensive CNN framework for COVID-19 detection
Table 2.
Detection of COVID-19 using ML-DL, DL, TL and ensemble techniques
| Paper | Model | Images | Methods | Result |
|---|---|---|---|---|
| Narin, Kaya and Pamuk [59] | DL | 100 CXR images | ResNet50, InceptionV3, Inception-ResNetV2 |
ResNet50 accuracy 98% InceptionV3 accuracy 97% Inception- ResNetV2 accuracy 87%. |
| Kamal et al. [41] | TL | 760 Chest X-Ray | Fine-tuned DenseNet121 | Accuracy 98.69% |
| Jaiswal et al. [39] | TL | CT images | DenseNet201 | AUC 0.97. |
| Aslan et al. [7] | DL and hybrid | 2905 CT images | mAlexNet and mAlexNet+BiLSTM, ANN segmentation |
mAlexNet accuracy 98.14% mAlexNet + BiLSTM accuracy 98.70% |
| Jain et al. [38] | TL | 1832 CXR images | ResNet50 and ResNet101 |
ResNet50 Accuracy 93.01% ResNet101 Accuracy 97.78% |
| Sitaula et al. [77] | TL | 3255 CXR images | VGG-16, VGG-19 | Accuracy 87.49% and 85% |
| Lee et al. [47] | DL | NIH chest X-ray dataset, RSNA Pneumonia Detection Challenge dataset | CLAHE, Grad-CAM, VGG-16 and VGG-19 | VGG-16 (VGG16-FT2) accuracy 95.9% and AUC 0.950 |
| Dansana et al. [23] | DL | 360 CXR and CT scan | VGG-19, Inception V2 and decision tree | Accuracy 91%, 78%, 60% |
| Rajaraman et al. [65] | DL | pediatric CXR dataset | CNN-based algorithms, Wide Residual CNN (WRCNN), Grad-CAM, U-Net | WRCNN accuracy 89.74% |
| Shah et al. [74] | DL | 739 CT scan images | CTnet-10, image augmentation and fine-tuning | Accuracy 94.52% |
| Tan et al. [79] | DL | 470 chest CT images | VGG-16, Super Resolution Generative Adversarial Network (SRGAN) |
Accuracy 97.9% Sensitivity 99%. |
| Elaziz et al. [27] | ML |
2 CXR image-based dataset |
Fractional Multichannel Exponent Moments (FrMEMs), KNN classifier | Accuracy 96.09% and 98.09% on datasets |
| Shan et al. [75] | ML | CT scans of 249 patients. | VBNet neural network to segment regions | Dice similarity coefficient of 91.6% ± 10.0% |
| Horry et al. [34] | TL | ultrasound images, CXR and CT scans | N-CLAHE, VGG-19 | Sensitivity 100%, 86% and 83% |
| Sethy et al. [73] | DL | CXR images collected from the repository of GitHub, Kaggle and Open-i. | InceptionResNetV2, AlexNet, GoogleNet, ResNet50, ResNet18, ResNet101, VGG16, InceptionV3, VGG19, DenseNet201 and Xception |
Accuracy of 95.38% (ResNet50 + SVM) VGGNet sensitivity 97.47% ResNet50 sensitivity 97.29%. |
| Wang and Wong [89] | DL | 13,800 CXR images from 13,725 cases | COVID-Net, a Deep Convolutional Neural Network (DCNN) |
Accuracy 92.6% Sensitivity 87.1% |
| Abbas, and Gaber [1] |
ML+ DL |
80 CXR images |
DeTraC-ResNet18 (pre-trained ResNet18) CNN-based AlexNet for deep feature extraction, Principal Component Analysis (PCA), K-means clustering for classification. |
Accuracy 92.5% Sensitivity 65% Specificity 94.3% Precision 94.5% |
| Zhang et al. [98] | DL | 1531 CXR images | ResNet18 | Sensitivity 96.00% |
| Wang et al. [90] | TL | 453 CT images | TL Inception network |
Accuracy 73.1% Specificity 67% Sensitivity 74%. |
| Li et al. [53] | DL | 4536 CT images | COVNet: RestNet50 |
Sensitivity 90% Specificity 96% |
| Ardakani et al. [5] | TL | 1020 preprocessed CT images | VGG-16, VGG-19, AlexNet, MobileNet-V2, ResNet-18, ResNet-50, SqueezeNet, GoogleNet, ResNet-101, and Xception |
ResNet-101 accuracy 99.51% Xception accuracy 99.02% |
| Xu et al. [94] | DL | 618 CT images | ResNet-18 | Accuracy 86.7% |
Challenges
High-dimensional data is a crucial challenge for ML models as it affects their training performance, whereas DL techniques [67] have effectively dealt with its volume, velocity, variety, and veracity. The performance of DL model increases with increase in data, unlike ML models. Nevertheless, big datasets are often imbalanced, and with larger architectures they require more time and high processing systems. Again, insufficient data can degrade the performance of a model and cause misclassification, thus making unreliable decisions. Therefore, sufficient amount of data and large case studies are necessary for a broader concept of the disease. Data privacy and scarcity of medical images is a concern for early diagnosis and treatment, leading to unavailability of medical data. This can be overcome with the help of different repositories available online [78, 89] and contains CT and CXR images of normal, non-COVID-19 pneumonia and COVID-19 pneumonia patients. Besides, images can also be collected from radiologists or from medical institutions, laboratories and organizations, on request. Various strategies can also be adopted for the creation and use of dataset such as undersampling and oversampling techniques, data augmentation and data preprocessing techniques. TL pre-trained models are also adopted to overcome problems associated with smaller datasets or data scarcity. However, adversarial attacks and biases may occur due to presence of artefacts and noise in datasets, or in the imaging modality or the device used for capturing the images, and additionally demands efficient dataset cleansing and interpretation expertise. Again, Generative Adversarial Networks (GANs) can also be adopted for data generation and discrimination in an unsupervised learning environment, to overcome the scarcity of large but balanced datasets. Thus, all these techniques can be used to mitigate data imbalance, data acquisition, privacy concern and noisy dataset for efficient feature extraction and corresponding image classification, for COVID-19 detection. Besides, feature representation and description of high-dimensional image data in a compact and understandable manner, for the predictive model, is another challenge often confronted while employing DL techniques. Thus, the need of dimensionality reduction techniques such as Principal Component Analysis (PCA), Singular Value Decomposition (SVD), Linear Discriminant Analysis (LDA), and Fully Convolutional Network (FCN), and others such as feature descriptors and attention-based mechanisms are necessitated for compact feature representation and efficient feature description of high-dimensional chest image data for better severity classification of COVID-19 using AI-based DL models.
Discussion
In various image related applications and tasks, traditional ML algorithms for image interpretation greatly rely upon handcrafted and expert-annotated features. Various Computer Vision (CV) techniques and ML models, are employed for better preprocessing, image analysis, feature extraction, feature representation and classification, upon the image dataset. However, the extensive variation of large medical imaging data, collected using sophisticated devices, and use of traditional ML models upon them takes more of model training time due to complex features and non-linear behaviour of the data. Such a process of manual analysis and interpretation is feasible but time consuming and inefficient, and highly prone to bias and error.
On the other hand, DL techniques can also adopt a few of the manual processing and analysis upon image data using Computer Vision (CV) techniques or can make use of its own inbuilt preprocessing functionalities, and down-sample the layers in the network to change the size of feature maps. They are complex and non-linear, and with deep architectures and multiple layers, such models are self-learners and robust in identifying features and human-level concepts, unlike conventional models. DL techniques have widened the scope of exploring the network connectivity patterns and behaviours, utilizing multi-level features, defining the convolutional layers to extract and interpret different and complicated features, strengthening the gradient through supervision of the hidden layers of the network, improve information flow by combining intermediate layers, minimize reconstruction losses etc. Besides, they can also perform high-level feature extraction and capture non-linear relationship, upon data using Representation Learning (RL), and can recreate new features from existing features to improvise model learning and generalization. Additionally, with better modelling measurements, a deep network can fundamentally learn probable mappings using domain knowledge, balanced dataset, skip-connections and make intellectual estimates such as interpolations and/or extrapolations, to ease the training of the network. The performance of DL models has increased with increase in data and number of layers in the network, but at one point it saturates and overfits due to high data skewness and failure in model convergence called degradation problem. Deeper networks are actually introduced by increasing the number of layers in the network, to easier the process of optimization and enhance accuracy, thereby enhancing deeper representations. However, the degradation problem due to increase in the number of layers of optimal deep networks can cause saturation in the accuracy of the model and higher training error. Thus, CNNs have undergone modifications to overcome the degradation problem caused as a result of deepness in structure, using short paths between layers, thus connecting and communicating more of high-dimensional details from lower layers to the upper layers, for e.g., ResNets and highway networks have introduced identity mappings, FractleNets combine parallel sequences with convolutional blocks etc. This avoids additional training parameters and high computational complexity. Thus, a good DL network initiates optimal reformation and preconditioning for simplification of optimization. This is the main reason why in most of the cases for developing an intelligent system for early COVID-19 detection, and various other image-based tasks, residual network and dense network have found tremendous applications because of lack of redundancy in network architecture which enabled them in achieving better performance in image classification and recognition tasks. Besides, CNNs such as DenseNets are considerably deeper, more precise, and effective to train for they contain petite networks between layers close to the input than those close to the output thus strengthening feature propagation, alleviating vanishing-gradient problem, encouraging feature reuse, and significantly reducing the number of parameters. The dense connectivity of such deeper networks enables feature reuse without any redundancy, improves flow of information and gradients, preserves state information, enables regularization and implicit deep supervision. The ability of compact internal representations and feature concatenation, growth rate marks the simplicity and efficiency of deep networks such as DenseNets. Additionally, orthogonal approaches such as increasing the network width, increasing the number of filters with sufficient depth can increase the performance of deeper networks. From Table 2 it can be concluded that ResNets have found immense application because of better performance in detection of COVID-19 [1, 5, 38, 53, 59, 73, 78, 94, 98] with consistently better accuracy and sensitivity irrespective of the amount of data used. However, the amount of data has an impact on the sensitivity of the model [1], but with smaller dataset these models have effectively overcome the data scarcity problem using various preprocessing [5], model optimization [53], crowdsourcing [73], and data generation techniques [71, 74]. Besides, dense networks [39, 41], VGG-16 [47, 77], VGG-19 [34, 47, 77], and comprehensive evaluation techniques [5, 73] have also found immense application in detection of COVID-19 because of better model learning and performance.
Block Diagram 6.
Ensemble learning frameworks for COVID-19 detection
The efficient utilization of image data has a very important role to play in model learning and training. The use of complex models upon smaller and/or skewed image datasets have shown high fine-grained variability which causes poor model performance, and hence complex model performance improvement can only be expected while using larger and balanced datasets [84]. The lack of balanced image data can be mitigated using domain adaptation, TL or using data augmentation techniques. DL can also be integrated with ML for designing a hybrid model to obtain a rich set of features and to minimize parameters, making interpretation of larger datasets and unknown patterns suitable, efficient and faster for traditional models, during training.
In recent state-of-the-art techniques attention mechanism in DL has also achieved greater significance. The importance of attention mechanism lies in its ability to focus on important and relevant features, learned from the given data and eradicating unwanted and irrelevant data. This is done with the motivation of reducing computational constraints, maximizing outcomes, minimizing resources and large training time. Thus, attention mechanism has also established a profound and significant importance to improve DL of features and minimize irrelevant information which otherwise causes high computational costs on being processed.
It is understood and realized that DL can be useful from the view point of detection of COVID-19, as medical imaging has incorporated the concept of DL, to assist physicians in learning and extraction of deep features for diagnosis of COVID-19 using chest CT scan images and CXR images. With the ever-increasing medical data, ML algorithms have shown poor performance during model training and generalization thus failing to output a better accuracy measurement. Besides, CT imaging features have more reliability in the detection of COVID-19 than CXR images, which is due to influence of external factors [60]. Thus, this study has analyzed various significant features of COVID-19 from earlier works and has interpreted and discussed the most common features of the disease, both in CXR and CT images. Various advantages and disadvantages are also identified in relation to detection of COVID-19. The main advantage of working with different kinds of AI-based intelligent models using ML, DL, TL and ensemble techniques upon chest images is that the process of detection of the disease can be made faster and efficient. The advantage of medical imaging and computer-assisted smart operations can make the task easier and faster for radiologists and doctors for early diagnosis and treatment of COVID-19 patients and eliminate emergency situations, in comparison to laboratory processes which are unreliable specially in asymptomatic cases. With intelligent systems, the progress of the disease and the patient’s health can be simultaneously visualized and monitored. The main disadvantage can be the lack of sufficient and balanced sample data which can cause higher detection error, and can demand huge computational resources which may not be available for treatment in remote areas.
Conclusion
The paper gives an elaborate description on the COVID-19 disease, its manifestations, and treatment and diagnosis of COVID-19 using radiology images, ML and DL techniques. Various features are identified and discussed in this manuscript, for the detection of COVID-19, using chest Computed Tomography (CT) and Chest X-Ray (CXR) images. It identifies RT-PCR to be less reliable in comparison to medical imaging of chest images for detection of COVID-19 and proposes computer-aided intelligent techniques such as ML and DL upon images, for early detection of the disease. Through this study, chest CT scan imaging modality is found to be more reliable than CXR imaging modality. In the near future, this work aims to extend the methodologies and frameworks of COVID-19 detection, proposed in this manuscript through implementation and evaluation. The review work aims to achieve a faster, easier, affordable and efficient learning system especially based on DL, to study, analyze and interpret large number of cases of COVID-19, for efficient outcomes, and for better identification and treatment of COVID-19 patients. It is believed that this manuscript will be helpful for various research works that are ongoing for early detection of COVID-19 and will be of interest to young scholars and researchers, in the field. It is also believed that this paper will be helpful in modelling the diagnostic pipeline efficiently, using ML and DL to identify and eradicate loopholes, for development of efficient, cost-effective and faster COVID-19 detection models.
Acknowledgements
I would like to thank my supervisor for the guidance throughout the preparation of this manuscript. I would like to thank my college for providing a platform, for creating opportunities necessary for research works.
Code availability
Not Applicable.
Funding
Not Applicable.
Data availability
Not Applicable.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dolly Das, Email: dolly_rs@cse.nits.ac.in.
Saroj Kumar Biswas, Email: saroj@nits.ac.in.
Sivaji Bandyopadhyay, Email: director@nits.ac.in.
References
- 1.Abbas A, Abdelsamea MM, Gaber MM. Classification of COVID-19 in chest X-ray images using DeTraC deep convolutional neural network. Appl Intell. 2021;51:854–864. doi: 10.1007/s10489-020-01829-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmad T, Khan M, Haroon THM, Nasir S, Hui J, Bonilla-Aldana DK, Rodriguez-Morales AJ. COVID-19: zoonotic aspects. Travel Med Infect Dis. 2020;36:101607. doi: 10.1016/j.tmaid.2020.101607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296(2):32–40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alom MZ, Taha TM, Yakopcic C, Westberg S, Sidike P, Nasrin MS, Hasan M, Van Essen BC, Awwal AAS, Asari VK (2019) A state-of-the-art survey on deep learning theory and architectures. 8(3):Electronics, 292 1-66. 10.3390/electronics8030292
- 5.Ardakani AA, Kanafi AR, Acharya UR, Khadem N, Mohammadi A. Application of deep learning technique to manage COVID-19 in routine clinical practice using CT images: results of 10 convolutional neural networks. Comput Biol Med. 2020;121:1–9. doi: 10.1016/j.compbiomed.2020.103795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aryal AS, Manandhar I, Munroe PB, Joe B, Cheng X. Artificial intelligence and machine learning to fight COVID-19. AI Mach Learn Understand Biol Processes. 2020;52(4):200–202. doi: 10.1152/physiolgenomics.00029.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aslan MF, Unlersen MF, Sabanci K, Durdu A. CNN-based transfer learning–BiLSTM network: a novel approach for COVID-19 infection detection. Appl Soft Comput. 2021;98:1–12. doi: 10.1016/j.asoc.2020.106912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China. Euro Surveill. 2020;25(5):2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, Wang M. Presumed asymptomatic carrier transmission of COVID-19. Jama. 2020;323(14):1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi LB, Wang DC, Mei J, Jiang XL, Zeng QH, Egglin TK, Hu PF, Agarwal S, Xie F, Li S, Healey T, Atalay MK. Performance of radiologists in differentiating COVID-19 from non-COVID-19 viral pneumonia at chest CT. Radiology. 2020;296(2):46–54. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barstugan M, Ozkaya U, Ozturk S (2020) Coronavirus (COVID-19) classification using CT images by machine learning methods. CoRR. Abs/2003.09424: 1-10
- 12.Sharon Begley (2020) Covid-19 testing issues could sink plans to re-open the country Might CT scans help? https://www.statnews.com/2020/04/16/ct-scans-alternative-to-inaccurate-coronavirus-tests/. Accessed on 30-4-2020
- 13.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M. Chest CT findings in coronavirus Disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3):685–691. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, Guido G, Bracci B, de Dominicis C, Laghi A. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020;296(2):79–85. doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, Xing F, Liu J, Yip CCY, Poon RWS, Tsoi HW, Lo SKF, Chan KH, Poon VKM, Chan WM, Ip JD, Cai JP, Cheng VCC, Chen H, … Yuen KY (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395(10223):514–523. 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed]
- 16.Chan JF, Yip CC, To KK. Tang TH, Wong SC, Leung KH, Fung AY, Ng AC, Zou Z, Tsoi HW, Choi GK, Tam AR, Cheng VC, Chan KH, Tsang OT, Yuen KY. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol. 2020;58(5):1–10. doi: 10.1128/JCM.00310-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chatterjee P, Nagi N, Agarwal A, Das B, Banerjee S, Sarkar S, Gupta N, Gangakhedkar RR. The 2019 novel coronavirus disease (COVID-19) pandemic: a review of the current evidence. Indian J Med Res. 2020;151(2–3):147–159. doi: 10.4103/ijmr.IJMR_519_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chowdhury NK, Kabir MA, Rahman M, Rezoana N (2020) Ecovnet: an ensemble of deep convolutional neural networks based on efficientnet to detect covid-19 from chest X-rays, arXiv:2009.11850v2 10.7717/peerj-cs.551, 7
- 20.Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance (2020). https://apps.who.int/iris/handle/10665/331446. Accessed on 01-05-2020
- 21.Corman VM, Eckerle I, Bleicker T, Zaki A, Landt O, Eschbach-Bludau M, Boheemen SV, Gopal R, Ballhause M, Bestebroer TM, Muth D, Müller MA, Drexler JF, Zambon MC, Osterhaus ADME, Fouchier RM, Drosten C. Detection of a novel human coronavirus by real-time reverse-transcription polymerase chain reaction. Euro Surveill. 2012;17(39):20285. doi: 10.2807/ese.17.39.20285-en. [DOI] [PubMed] [Google Scholar]
- 22.Coutard B, Valle C, de Lamballerie X, Canard B, Seidah NG, Decroly E. The spike glycoprotein of the new coronavirus 2019-nCoV contains a furin-like cleavage site absent in CoV of the same clade. Antivir Res. 2020;176:104742. doi: 10.1016/j.antiviral.2020.104742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dansana D, Kumar R, Bhattacharjee A, Hemanth DJ, Gupta D, Khanna A, Castillo O (2020) Early diagnosis of COVID-19-affected patients based on X-ray and computed tomography images using deep learning algorithm. Soft Comput 1-9. 10.1007/s00500-020-05275-y, 1, 9 [DOI] [PMC free article] [PubMed]
- 24.Dhama K, Patel SK, Pathak M, Yatoo MI, Tiwari R, Malik YS, Singh R, Sah R, Rabaan AA, Bonilla-Aldana DK, Rodriguez-Morales AJ. An update on SARS-CoV-2/COVID-19 with particular reference to its clinical pathology, pathogenesis, immunopathology and mitigation strategies. Travel Med Infect Dis. 2020;37:101755. doi: 10.1016/j.tmaid.2020.101755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, Singh KP, Chaicumpa W, Bonilla-Aldana DK, Rodriguez-Morales AJ (2020) Coronavirus disease 2019-COVID-19. Clin Microbiol Rev 33(4). 10.1128/CMR.00028-20 [DOI] [PMC free article] [PubMed]
- 26.Duan YN, Qin J. Pre-and posttreatment chest CT findings: 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):21. doi: 10.1148/radiol.2020200323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elaziz MA, Hosny KM, Salah A, Darwish MM, Lu S, Sahlol AT. New machine learning method for image-based diagnosis of COVID-19. PLOS ONE. 2020;15(6):e0235187 1-18. doi: 10.1371/journal.pone.0235187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evangelin MP, Krishna BG, Raga SY, Vamsi GK, Zakeer S, Raju KN (2020) A review: outbreak of Corona. Journal of medical biomedical and applied sciences. 8(4):354-357. 10.15520/jmbas.v8i4.217
- 29.Gaillard F, Normal chest x-ray. Case study, Radiopaedia.org. https://radiopaedia.org/cases/8304.Accessed on 27–09- 2021
- 30.Global Situation. World Health Organization (WHO) Coronavirus (COVID-19) Dashboard. https://covid19.who.int/. Accessed on 28-09-2021
- 31.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, … Zhong NS (2020) Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med 382(18):1708–1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed]
- 32.Gupta R, Pal SK (2020) Trend analysis and forecasting of COVID-19 outbreak in India. medRxiv 1-19. 10.1101/2020.03.26.20044511
- 33.Hoffmann M, Kleine-Weber H, Krüger N, Mueller MA, Drosten C, Pöhlmann S. The novel coronavirus 2019 (2019-nCoV) uses the SARS-coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells. Cell. 2020;181:1–23. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horry MJ, Chakraborty S, Paul M, Ulhaq A, Pradhan B, Saha M, Shukla N. COVID-19 detection through transfer learning using multimodal imaging data. IEEE Access. 2020;8:149808–149824. doi: 10.1109/ACCESS.2020.3016780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, … Cao B (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed]
- 36.India Situation. World Health Organization (WHO). https://covid19.who.int/region/searo/country/in . Accessed on 28-09-2021
- 37.Jadhav S, Deng G, Zawin M, Kaufman AE (2021) COVID-view: diagnosis of COVID-19 using chest CT. arXiv preprint arXiv:2108.03799 [DOI] [PMC free article] [PubMed]
- 38.Jain G, Mittal D, Thakur D, Mittal MK. A deep learning approach to detect Covid-19 coronavirus with X-ray images. Biocybernetics Biomed Eng. 2020;40(4):1391–1405. doi: 10.1016/j.bbe.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jaiswal A, Gianchandani N, Singh D, Kumar V, Kaur M. Classification of the COVID-19 infected patients using DenseNet201 based deep transfer learning. J Biomol Struct Dyn. 2020;39(15):5682–5689. doi: 10.1080/07391102.2020.1788642. [DOI] [PubMed] [Google Scholar]
- 40.Ji W, Wang W, Zhao X, Zai J, Li X. Cross-species transmission of the newly identified coronavirus 2019-nCoV. J Med Virol. 2020;92(4):433–440. doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamal KC, Yin Z, Wu M, Wu Z. Evaluation of deep learning-based approaches for COVID-19 classification based on chest X-ray images. SIViP. 2021;15:959–966. doi: 10.1007/s11760-020-01820-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ke R, Romero-Severson E, Sanche S, Hengartner N. Estimating the reproductive number R0 of SARS-CoV-2 in the United States and eight European countries and implications for vaccination. J Theor Biol. 2021;517:1–10. doi: 10.1016/j.jtbi.2021.110621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kitchener P (2013), Importance of medical imaging, vision XRay group. https://www.xray.com.au/importance-of-medical-imaging/. Accessed on: 09-09-2021
- 44.Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases (2020). https://www.who.int/publications/i/item/10665-331501. Accessed on 03-05-2020
- 45.Lalmuanawma S, Hussain J, Chhakchhuak L. Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: a review. Chaos, Solitons Fractals. 2020;139:1–12. doi: 10.1016/j.chaos.2020.110059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee PI, Hsueh PR. Emerging threats from zoonotic coronaviruses-from SARS and MERS to 2019-nCoV. J Microbiol Immunol Infect. 2020;53(3):365–367. doi: 10.1016/j.jmii.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee KS, Kim JY, Jeon ET, Choi WS, Kim NH, Lee KY. Evaluation of scalability and degree of fine-tuning of deep convolutional neural networks for COVID-19 screening on chest X-ray images using explainable deep-learning algorithm. J Pers Med. 2020;10(4):1–14. doi: 10.3390/jpm10040213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):18. doi: 10.1148/radiol.2020200236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Y, Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. Am J Roentgenol. 2020;214(6):1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 51.Li X, Song Y, Wong G, Cui J. Bat origin of a new human coronavirus: there and back again. Science China. Life Sci. 2020;63(3):461–462. doi: 10.1007/s11427-020-1645-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li X, Zai J, Zhao Q, Nie Q, Li Y, Foley BT, Chaillon A. Evolutionary history, potential intermediate animal host, and cross-species analyses of SARS-CoV-2. J Med Virol. 2020;92(6):602–611. doi: 10.1002/jmv.25731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li L, Qin L, Xu Z, Yin Y, Wang X, Kong B, Bai J, Lu Y, Fang Z, Song Q, Cao K, Liu D, Wang G, Xu Q, Fang X, Zhang S, Xia Juan, Xia Jia (2020) Artificial Intelligence Distinguishes COVID-19 from Community Acquired Pneumonia on Chest CT. Radiology 1–16. 10.1148/radiol.2020200905 [DOI] [PMC free article] [PubMed]
- 54.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020;80(6):14–18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, … Tan W (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395(10224):565–574. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed]
- 56.Malik YS, Sircar S, Bhat S, Sharun K, Dhama K, Dadar M, Tiwari R, Chaicumpa W. Emerging novel coronavirus (2019-nCoV)—current scenario, evolutionary perspective based on genome analysis and recent developments. Vet Q. 2020;40(1):68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marimuthu S, Joy M, Malavika B, Nadaraj A, Asirvatham ES, Jeyaseelan L. Modelling of reproduction number for COVID-19 in India and high incidence states. Clin Epidemiol Global Health. 2021;9:57–61. doi: 10.1016/j.cegh.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murdoch DR, French NP. COVID-19: another infectious disease emerging at the animal-human interface. New Zealand Med J (Online) 2020;133(1510):12–15. [PubMed] [Google Scholar]
- 59.Narin A, Kaya C, Pamuk Z. Automatic detection of coronavirus disease (covid-19) using x-ray images and deep convolutional neural networks. Pattern Anal Applic. 2021;24:1207–1220. doi: 10.1007/s10044-021-00984-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ng MY, Lee EY, Yang J, Yang F, Li X, Wang H, Lui MMS, Lo CSY, Leung B, Khong PL, Hui CKM, Yuen KY, Kuo MD. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol: Card Imaging. 2020;2(1):e200034. doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kirti Pandey (2021) COVID Vaccines approved in India: Covishield, Covaxin, Sputnik V, Moderna; here's all you wish to know. https://www.timesnownews.com/health/article/covid-vaccines-approved-in-india-covishield-covaxin-sputnik-v-moderna-heres-all-you-wish-to-know/778482. Accessed on 03-07-2021
- 62.Q&A Detail (2020). https://www.who.int/news-room/q-a-detail. Accessed on 30-4-2020
- 63.Qian L, Yu J, Shi H. Severe acute respiratory disease in a Huanan seafood market worker: images of an early casualty. Radiology: Cardiothoracic Imaging. 2020;2(1):1–2. doi: 10.1148/ryct.2020200033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rahimzadeh M, Attar A. A modified deep convolutional neural network for detecting COVID-19 and pneumonia from chest X-ray images based on the concatenation of Xception and ResNet50V2. Inform Med Unlocked. 2020;19:1–9. doi: 10.1016/j.imu.2020.100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rajaraman S, Antani S (2020) Training deep learning algorithms with weakly labelled pneumonia chest X-ray data for COVID-19 detection. medRxiv preprint. 10.1101/2020.05.04.20090803
- 66.Ranjan R, Sharma A, Verma MK (2021) Characterization of the second wave of COVID-19 in India, medRxiv 1-16. 10.1101/2021.04.17.21255665
- 67.Razzak MI, Naz S, Zaib A. Deep learning for medical image processing: overview, challenges and the future. In: Dey N, Ashour A, Borra S, editors. Classification in BioApps. Lecture notes in computational vision and biomechanics 26. Springer Cham; 2018. [Google Scholar]
- 68.Rodriguez-Morales A, Bonilla-Aldana DK, Tiwari R, Sah R, Rabaan AA, Dhama K (2020) COVID-19, an emerging coronavirus infection: current scenario and recent developments – An overview. Journal of pure and applied microbiology 14(1):6150. 10.22207/JPAM.14.1.02
- 69.Rodriguez-Morales AJ, Bonilla-Aldana DK, Balbin-Ramon GJ, Rabaan AA, Sah R, Paniz-Mondolfi A, Pagliano P, Esposito S. History is repeating itself: probable zoonotic spillover as the cause of the 2019 novel coronavirus epidemic. Infez Med. 2020;28(1):3–5. [PubMed] [Google Scholar]
- 70.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:1–4. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.SARS-CoV-2 Variant Classifications and Definitions (2021), Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html.Accessed on: 03-07-2021
- 72.Schwartz DA. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020;144(7):799–805. doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- 73.Sethy PK, Behera SK, Ratha PK, Biswas P (2020) Detection of coronavirus disease (COVID-19) based on deep features and support vector machine. MDPI AG 1-10
- 74.Shah V, Keniya R, Shridharani A, Punjabi M, Shah J, Mehendale N. Diagnosis of COVID-19 using CT scan images and deep learning techniques. Emerg Radiol. 2021;28:497–505. doi: 10.1007/s10140-020-01886-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shan F, Gao Y, Wang J, Shi W, Shi N, Han M, Xue Z, Shen D, Shi Y (2020) Lung infection quantification of COVID-19 in CT images with deep learning. Preprint arXiv: 200304655:1-19. 48:1633–1645. 10.1002/mp.14609
- 76.Singhal T. A review of coronavirus Disease-2019 (COVID-19) Indian J Pediatrics. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sitaula C, Hossain MB. Attention-based VGG-16 model for COVID-19 chest X-ray image classification. Appl Intell. 2021;51:2850–2863. doi: 10.1007/s10489-020-02055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Strengthening medical imaging (2021) https://www.who.int/activities/strengthening-medical-imaging. Accessed on: 09-09-2021
- 79.Tan W, Liu P, Li X, Liu Y, Zhou Q, Chen C, Gong Z, Yin X, Zhang Y. Classification of COVID-19 pneumonia from chest CT images based on reconstructed super-resolution images and VGG neural network. Health Inf Sci Syst. 2021;9(10):1–12. doi: 10.1007/s13755-021-00140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tang Z, Zhao W, Xie X, Zhong Z, Shi F, Liu J, Shen D (2020) Severity assessment of coronavirus disease 2019 (COVID-19) using quantitative features from chest CT images. Preprint arXiv:2003.11988 1-18
- 81.The Important Role Medical Imaging Plays in Diagnosis and Treatment, Peconic Bay Medical Center (2018). https://www.pbmchealth.org/news-events/blog/important-role-medical-imaging-plays-diagnosis-and-treatment. Accessed on: 09-09-2021
- 82.Tracking SARS-CoV-2 variants (2021). https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/. Accessed on: 03-07-2021
- 83.Treatments for COVID-19 (2021) Harvard Health Publishing, Harvard Medical School. https://www.health.harvard.edu/diseases-and-conditions/treatments-for-covid-19. Accessed on 03-07-2021
- 84.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94(7):e00127–e00120. doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, Shi H, Zhou M. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020;296(2):55–64. doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang L, Shi Y, Xiao T, Fu J, Feng X, Mu D, Feng Q, Hei M, Hu X, Li Z, Lu G, Tang Z, Wang Y, Wang C, Xia S, Xu J, Yang Y, Yang J, Zeng M, … Zhou W (2020) Working Committee on Perinatal and Neonatal Management for the Prevention and Control of the 2019 Novel Coronavirus Infection, Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection (First edition). Ann Transl Med. 8(3):47. 10.21037/atm.2020.02.20 [DOI] [PMC free article] [PubMed]
- 89.Wang L, Lin ZQ, Wong A. COVID-net: a tailored deep convolutional neural network design for detection of COVID-19 cases from chest radiography images. Nature research. Sci Rep. 2020;10(19549):1–12. doi: 10.1038/s41598-020-76550-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang S, Kang B, Ma J, Zeng X, Xiao M, Guo J, Cai M, Yang J, Li Y, Meng X, Xu B. A deep learning algorithm using CT images to screen for Corona virus disease (COVID-19) Eur Radiol. 2021;31:6096–6104. doi: 10.1007/s00330-021-07715-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Xiao K, Zhai J, Feng Y, Zhou N, Zhang X, Zou JJ, Li N, Guo Y, Li X, Shen X, Zhang Z, Shu F, Huang W, Li Y, Zhang Z, Chen RA, Wu YJ, Peng SM, Huang M, Xie WJ, Cai QH, Hou FH, Liu Y, Chen W, Xiao L, Shen Y (2020) Isolation and characterization of 2019-nCoV-like coronavirus from Malayan pangolins. bioRxiv 1-31. 10.1101/2020.02.17.951335
- 93.Xu YH, Dong JH, An WM, Lv XY, Yin XP, Zhang JZ, Dong L, Ma X, Zhang HJ, Gao BL. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect. 2020;80(4):394–400. doi: 10.1016/j.jinf.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xu X, Jiang X, Ma C, Du P, Li X, Lv S, Yu L, Chen Y, Su J, Lang G, Li Y, Zhao H, Xu K, Ruan L, Wu W. A deep learning system to screen novel coronavirus disease 2019 pneumonia. Engineering. 2020;6(10):1122–1129. doi: 10.1016/j.eng.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, Ng OT, Marimuthu K, Ang LW, Mak TM, Lau SK, Anderson DE, Chan KS, Tan TY, Ng TY, Cui L, Said Z, Kurupatham L, Cheng MI, … Lye DC (2020) Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 323(15):1488–1494. 10.1001/jama.2020.3204 [DOI] [PMC free article] [PubMed]
- 96.Yu L, Shanshan Wu, Xiaowen Hao, Xuelong Li, Xiyang Liu, Shenglong Ye, Han H, Dong X, Li X, Li J, Liu J, Liu N, Zhang W, Pelechano V, Chen W, Yin X (2020) Rapid colorimetric detection of COVID-19 coronavirus using a reverse transcriptional loop-mediated isothermal amplification (RT-LAMP) diagnostic platform: iLACO. Clinical Chemistry 1–19. 10.1093/clinchem/hvaa102 [DOI] [PMC free article] [PubMed]
- 97.Zhang N, Wang L, Deng X, Liang R, Su M, He C, Hu L, Su Y, Ren J, Yu F, Du L, Jiang S. Recent advances in the detection of respiratory virus infection in humans. J Med Virol. 2020;92(4):408–417. doi: 10.1002/jmv.25674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang J, Xie Y, Li Y, Shen C, Xia Y (2020) COVID-19 screening on chest X-ray images using deep learning based Anomaly Detection. arXiv preprint arXiv:2003.12338v1:1–6
- 99.Zhao D, Yao F, Wang L, Zheng L, Gao Y, Ye J, Guo F, Zhao H, Gao R (2020) Comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Oxford academic, clinical infectious diseases, article | WHO COVID | ID: covidwho-7938, 2020 [DOI] [PMC free article] [PubMed]
- 100.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, … Shi ZL (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270–273. 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed]
- 101.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020;296(2):15–25. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020;296(2):15–25. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not Applicable.