Abstract
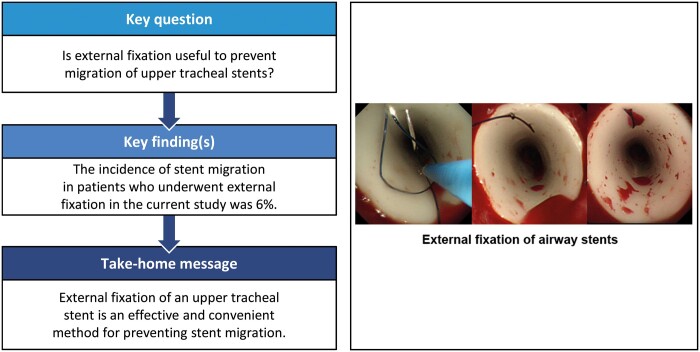
OBJECTIVES
Stent migration is a common complication of airway stent placement for upper tracheal stenosis and tracheoesophageal fistula. Although several researchers have reported that external fixation is effective in preventing stent migration, the usefulness and safety of external fixation have not been proved because their cohorts were small. We therefore investigated the efficacy and safety of external fixation during upper tracheal stenting.
METHODS
Records of patients who underwent airway stent placement from May 2007 to August 2018 in a single centre were retrospectively reviewed. We included only patients whose stent had been placed in the upper trachea with external fixation to the tracheal wall. The primary endpoint of this study was the rate of stent migration.
RESULTS
Altogether, 51 procedures were performed in 45 patients (32 males, 13 females; median age 60 years, range 14–91 years). The median follow-up period was 9 months (range 0.3–90 months). Among the procedures, 15 were performed for benign disease and 36 for malignancy. Stents were composed of either silicone (n = 42) or metal (n = 9). Stent migration occurred in 3 (6%) patients. The stents with migration were all composed of silicone. Other sequelae were granulation tissue formation in 10 (20%) patients, sputum obstruction in 6 (12%), cellulitis in 3 (6%) and pneumonia in 1 (2%).
CONCLUSIONS
External fixation was an effective method for preventing migration of airway stents placed for upper tracheal stenosis and tracheoesophageal fistula. The complications were acceptable in terms of safety.
Keywords: Airway stent, External fixation, Stent migration, Tracheal stenosis, Tracheoesophageal fistula
INTRODUCTION
Airway stenting for tracheal stenosis is an effective tool when providing palliative therapy [1]. Stent placement benefits patients with benign and malignant disease [2]. The effectiveness of tracheal stent placement for tracheoesophageal fistulas has been reported [3, 4], although there have been reports of complications associated with airway stenting. For example, respiratory movement, coughing or swallowing may cause stent migration [5], which in turn can result in relapse or exacerbation of the tracheal stenosis, causing further patient discomfort. Stent replacement is then required [6]. There have been several reports of tracheal stent migration, especially with subglottic or upper tracheal stenosis and fistula [7, 8]. Migration rates are 16–24% for silicone stents [5, 9] and 2.2–6.4% for metallic stents [10, 11]. Migration rarely occurs with the T-shaped stent. However, because the placement of a T-shaped stent requires an invasive procedure through an incision in the anterior neck and subsequent cosmetic problems, the straight stent is the first choice in our institution.
Several investigators have reported the effectiveness of external fixation of straight-type stents in preventing stent migration [12–15]. To date, however, studies have reported only relatively small numbers of patients who underwent this procedure. Hence, no standard procedure has been established for external fixation of airway stents to treat patients who require upper tracheal stenting. We therefore investigated the efficacy and safety of external fixation of airway stents in a relatively large cohort of patients undergoing stenting for disease in the upper trachea.
MATERIALS AND METHODS
Patients
In total, 739 airway stenting procedures were performed in 649 patients at National Hospital Organization Nagoya Medical Center between May 2007 and August 2018. The medical records of all patients who had undergone external fixation of tracheal stents for upper tracheal stenosis or tracheoesophageal fistula were retrospectively reviewed. The stents had been externally fixed to the tracheal wall.
Prior to the stenting procedure, anaesthetic tolerance was confirmed by the anaesthesiologist’s evaluation and several procedures, including electrocardiography, cardiac ultrasonography, pulmonary function testing and arterial blood gas analysis. The final adaptation of airway stenting with external fixation, including tolerance to the general anaesthesia, was assessed by the operator.
Before stent placement, written informed consent for the procedure was obtained from all patients. This study was approved by the institutional review board of National Hospital Organization Nagoya Medical Center (approval date: 23 April 2019; identifier: 2018–107). The need for informed consent for this study was waived because of its retrospective nature.
Bronchoscopic procedures
All bronchoscopic procedures were performed in an operating room under general anaesthesia. First, the airway was re-established using one or more of the following tools: argon plasma coagulation, electrocautery, cryosurgery, high-pressure balloon dilatation and/or rigid bronchoscopy (using the bevelled edge of the bronchoscope). Second, to determine the size of the stent, the diameter of the stenosis was measured using balloon-type radial probe endobronchial ultrasonography and flexible bronchoscopy. The operator then selected a Dumon™ silicone stent (Novatech SA, La Ciotat, France), an Ultraflex® metallic stent (Boston Scientific Corp., Natick, MA, USA), or an AERO® metallic stent (Merit Medical Systems, South Jordan, UT, USA). The selected airway stent was placed under fluoroscopic guidance.
External fixation techniques
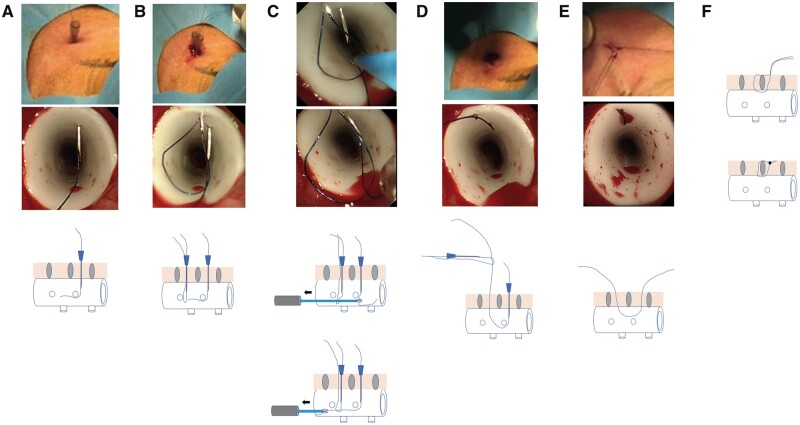
The first step of external fixation was to prepare two 22-gauge needles with a 3–0 nylon thread or a coated Vicryl® suture (Ethicon, Inc., Somerville, NJ, USA). A needle threaded for fixation was then inserted into the patient’s anterior neck and through the anterior aspect of the stent into the lumen (Fig. 1A). Then, a loop using a second thread was made inside the stent through the other needle (Fig. 1B). The thread for fixation was then guided through the fixation area with forceps under bronchoscopic control (Fig. 1C). Next, the thread was pulled out with the loop (Fig. 1D) and tied to fix the stent to the tracheal wall (Fig. 1E). Finally, the stent was secured with a buried suture (Fig. 1F). In some patients, the fixation technique reported by Miwa et al. [13] was performed with a device initially designed for gastropexy during endoscopic gastrostomy.
Figure 1:
(A) A needle, through which suture material for fixation was threaded, was inserted through the anterior neck of the patient into the stent lumen. (B) Using another needle, a second loop with suture material was made inside the stent. (C) The suture material for fixation was then threaded through the fixation area with forceps under bronchoscopic control. (D) The suture material was pulled out with the loop. (E) The suture material was tied to fix the stent to the tracheal wall. (F) The 2 threads were fixed using a buried suture.
Statistical analysis
The primary endpoint of this study was the incidence of stent migration in patients who underwent airway stenting with external fixation. Secondary endpoints included pulmonary function, need for supplemental oxygen and stent-related complications without migration. The complications included were limited to patients who required treatment with bronchoscopy (such as replacement of a stent or clearance of sputum).
Differences in pulmonary function before and after stenting (1–5 days after intervention) were analysed using the Wilcoxon signed-rank test. The results were considered statistically significant at 2-tailed P ≤ 0.05. Continuous variables were normally distributed and were expressed as mean ± standard deviation. Statistical analyses were performed using PASW Statistics for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Patients
During the study period, 51 airway stent procedures with external fixation were performed in 45 patients (32 males, 13 females). Median patient age was 60 years (range 14–91 years). Patients’ diagnoses and other characteristics are detailed in Table 1. The median follow-up period was 9 months (range 0.3–90.0 months). Of the 45 patients, 33 had malignant disease, with oesophageal cancer and lung cancer accounting for 26 of the 33 malignancies. Three patients with tracheoesophageal fistula were included in the group of patients with malignant disease. The 12 patients with benign disease had post-tracheostomy tracheal stenosis or granulation tissue (such as late effects of tuberculosis).
Table 1:
Patients’ characteristics
| Characteristic | Data | |
|---|---|---|
| Number of patients | 45 | |
| Number of procedures | 51 | |
| Median age, years (range) | 60 (14–91) | |
| Sex, male, number (%) | 32 (71) | |
| ECOG PS at time of procedure, number (%) | ||
| 1 | 25 | (49) |
| 2 | 13 | (25) |
| 3 | 4 | (8) |
| 4 | 9 | (18) |
| Airway stenosis/fistula | 42/3 | |
| Diagnosis, malignant/benign | 33/12 | |
| Malignant, number (%) | ||
| Lung cancer | 13 | (29) |
| Oesophageal cancer | 13 | (29) |
| Thyroid cancer | 3 | (7) |
| Tracheal cancer | 1 | (2) |
| Pharyngeal cancer | 1 | (2) |
| Lymphoma | 1 | (2) |
| Colon cancer | 1 | (2) |
| Benign, number (%) | ||
| Post-tracheostomy | 4 | (9) |
| Granulation tissue | 4 | (9) |
| Post-intubation | 2 | (4) |
| Benign tumour | 2 | (4) |
ECOG PS: Eastern Cooperative Oncology Group Performance Status.
Procedures
Table 2 summarizes the procedural details. Among the 51 stents placed, there were 42 silicone stents and 9 metallic stents (8 Ultraflex® and 1 AERO®). Nylon thread was used in all but one of the procedures (in which coated Vicryl® was used). Most of the procedures required 2 stitches for fixation. External fixation using a gastrostomy device was performed in 13 of the 51 procedures. The fixation sutures were placed at the stent site located the shortest distance from the anterior neck that the needle was able to reach, regardless of the lesion site.
Table 2:
Procedural details
| Parameter | Data |
|---|---|
| Stent type, silicone/metallic | 42/9 |
| Median stent outer diameter, mm (range) | 16 (11–20) |
| Median stent length, mm (range) | 50 (25–80) |
| Thread type, nylon/absorbable | 50/1 |
| Number of stitches, 2/1 | 45/6 |
Efficacy
Among the 51 patients, 12 (24%) received oxygen therapy, including 4 patients under mechanical ventilation; most of these patients (11 of 12, 92%) improved and no longer needed oxygen therapy. Pulmonary function test results were available before and after stenting for 21 patients. As shown in Table 3, the peak expiratory flow had significantly improved after stenting when compared with before stenting (P = 0.02), although there was no significant difference in the vital capacity or the forced expiratory volume in 1 s. Successful treatment with the stenting led to subsequent stent removal in 4 patients. The stent was removed using flexible bronchoscopy with a rigid bronchoscope under general anaesthesia; the nylon thread was first cut with scissors and then removed. Stent removal was performed without complications in all 4 cases.
Table 3:
Pulmonary function test results before and after stent placement (n = 21)
| Variable | Before stenting mean, SD | After stenting mean, SD | P-value |
|---|---|---|---|
| VC, l | 2.96, 0.30 | 2.85, 0.29 | 0.28 |
| FEV1, l | 1.86, 0.18 | 2.01, 0.18 | 0.24 |
| PEF, l/s | 2.62, 0.30 | 3.30, 0.30 | 0.02 |
FEV1: forced expiratory volume in 1 s; l: litre; l/s: litre/second; PEF: peak expiratory flow; SD: standard deviation; VC: vital capacity.
Safety
Stent-related complications occurred in 21 (41%) patients: migration in 3 (6%), granulation tissue formation in 10 (20%), sputum-related obstruction in 6 (12%), cellulitis due to thread infection in 3 (6%) and pneumonia in 1 (2%). Table 4 summarizes the data for the 3 patients with airway stent migration identified in our study. The stents with migration were all composed of silicone. Two patients required replacement of the stent and 1 underwent tracheotomy. Furthermore, 7 of the 10 patients with granulation tissue formation required replacement of the stent.
Table 4:
Characteristics of the 3 patients with stent migration
| Patient | Diagnosis | Age | Stent type | Outer diameter /length | Thread | Number of stitches | Follow-up, months | Treatment after migration |
|---|---|---|---|---|---|---|---|---|
| 1 | Post-intubation | 64 | Silicone | 16/50 | Nylon | 2 | 1.0 | Tracheostomy |
| 2 | Post-intubation | 19 | Silicone | 15/50 | Nylon | 2 | 2.0 | Stent replacement |
| 3 | Post-tracheostomy | 40 | Silicone | 14/35 | Absorbable | 2 | 1.5 | Stent replacement |
DISCUSSION
When placing a straight stent in the upper trachea, migration is a major stent-related complication that can lead to relapse of tracheal stenosis, which can cause significant discomfort. The risk of migration is high for silicone stents in the upper trachea without external fixation [7, 8]. To the best of our knowledge, our study cohort included a larger number of patients than the cohorts in previous studies evaluating external fixation of airway stents. Stent migration occurred in only 3 of 51 patients (6%), and we attributed this low incidence of stent migration to the external fixation.
Previous (including recent) studies have also evaluated the efficacy and safety of airway stenting with external fixation for upper tracheal stenosis [12–17]. Colt et al. [12] performed external fixation using 2 angiocatheters to fix the stent to a button. Their report stated that no migration had occurred in any of the 6 patients [12]. Granulation tissue had formed in 3 patients and cellulitis in 1 [12]. Majid et al. [14], who improved the method of Colt et al. [12], threaded an angiocatheter that was used to penetrate the stent and tracheal wall. Next, with an Endo Close® suturing device (used in endoscopic surgery) from another angiocatheter, the thread was picked up and sewn to the external button. External fixation was performed in 9 patients using this method [14]. Because the device enables remote suturing, the procedure was facilitated by passing an angiocatheter through the Endo Close® device. The reported complications were migration in 1 patient, granulation tissue formation in 2 patients, sputum obstruction in 2 patients and cellulitis in 1 patient [14]. In a recent study, Andreetti et al. [16] reported on 27 patients who underwent external fixation, also with angiocatheters. Their external fixation method was to tie a knot inside the trachea rather than using an external button [16]. The group did not report any specific complications, including stent migration [16]. Conversely, Miwa et al. [13] performed external fixation in 6 patients using a gastrostomy device; a recent report showed that this method resulted in no migration in 11 cases, including metallic stents [17].
The method used in our study (Fig. 1) follows the external fixation method of Miwa et al. [13] (Fig. 1). Although a gastrostomy device is used, the method of applying the suture is the same as in other reported techniques. The difference between previous studies using angiocatheters and the technique used for our 45 patients is that our procedure is relatively easy and can be performed safely. Furthermore, the 22-gauge needles used in our institution seem to result in a low risk of damage to the stent, blood vessels and trachea.
Table 4 summarizes the 3 instances of airway stent migration identified in our study. All 3 patients had benign disease and had undergone the 2-stitch method for stent fixation. The stents were all composed of silicone. In all patients, stent migration occurred within 2 months after stent placement. Patient 2 had post-tracheal intubation tracheal stenosis. In this patient, the suture was removed 3 weeks after stent placement to prevent cellulitis. One month after the suture was removed, migration developed and stent replacement was required. The suture used for stent fixation in patient 3 was coated with Vicryl®, which is an absorbable synthetic material. This patient was the only one in our study for whom absorbable suture material was used. This suture material is often used for ligating or fixing soft tissue. It retains its strength in the tissue for about 2–3 weeks and is hydrolyzed within 8–10 weeks. Because of its absorbency, coated Vicryl® does not appear to be suitable for external fixation. On the basis of this result, we use nylon suture and do not remove it in clinical practice. The causes of migration in patient 2 and patient 3 were thought to be the removed and absorbable sutures, respectively. The exact cause of stent migration in patient 1 was unknown. On the basis of these experiences, we believe that the likelihood of stent migration is reduced by using non-absorbable suture material and preventing suture removal by using buried sutures. In the present study, all 3 patients with stent migration had benign diseases; however, as 2 of these cases had clear reasons for stent migration (absorbable suture material in one case, and suture removal in another), it cannot be concluded that stent migration occurs because of benign disease.
In the study of Andreetti et al. [16], no migration was observed in 27 patients with tracheal stenosis who underwent stent placement with silicone stents and external fixation using absorbable thread. Their success may be due to their use of knots for fixation, even with the use of absorbable suture.
Cellulitis is a stent-related complication specific to external fixation. In our study, cellulitis occurred in 6% of patients. Majid et al. [14] reported an incidence of cellulitis of 11%, which was similar to our results. All patients with cellulitis in our study were cured with antibiotics and did not require stent replacement. Additionally, 10 patients (20%) experienced granulation tissue formation, 7 of whom required stent replacement. None of the other complications required replacement. Although there were 3 cases of cellulitis in our study, there was no skin irritation or necrosis due to suturing. Cellulitis was not found in the 4 cases in which the stent was removed. The incidence of stent replacement is acceptable compared with previous reports (22–50%) [12, 14].
With the exception a recent study, most previous studies on external fixation dealt with silicone airway stents, with a few focusing on metallic stents [12–16]. In general, metallic stents have a lower migration rate than silicone stents in the upper trachea [3, 10, 11], although metallic stent migration can occur. Our study included 9 patients with metallic stents (8 Ultraflex® and 1 AERO®). The metallic stent group experienced no stent migration, and none of the metallic stents were broken due to the sutures associated with external fixation. Others have also shown that, when placed in the upper trachea, metallic stents are less likely to migrate than silicone stents [5, 9–11]. Although we previously encountered cases in which there was migration of a metallic stent without external fixation [3], there was no such migration in the present study. These results, combined with ours, suggest that external fixation of a metallic stent may be beneficial for patients with upper tracheal stenosis or a tracheoesophageal fistula because of the low risk of stent migration. Although the metallic stent is made of monofilament, it was not particularly damaged and was treated in the same way as the silicone stent, which did not cause any problems in our study. We believe that external fixation of metallic stents further reduces the risk of migration.
In the present study, it was left to the operator’s discretion as to whether external fixation of the stent was accomplished with 1 or 2 stitches. In 6 patients, the operator judged that 1 stitch was sufficient to prevent stent migration and, indeed, no migration was observed in these patients. Furthermore, 3 of the 6 patients received metallic stents. Although our study was small, and the association was difficult to assess, the results suggest that there may be little correlation between the number of stitches used for external fixation and the prevention of stent migration. Future studies of external fixation of airway stents are needed, not only from the standpoint of the stent migration rate but also because of the sequelae due to suture infection and other invasive aspects.
Our study had several limitations. One was that it is a single-centre, retrospective study. It is unknown whether similar interventions can be undertaken at other institutions. However, the external fixation procedure presented in our study is simple and does not require special devices. Hence, the potential for its use at other institutions is promising. Additionally, although our study on external fixation is the largest in comparison with past studies, we think that the number of cases is insufficient to solve the subgroup questions of whether external fixation is required for placing a metallic stent and whether the appropriate number of stitches is 1 or 2.
CONCLUSION
External fixation of an upper tracheal stent is an effective, safe, and convenient method for preventing stent migration. Therefore, we propose that external fixation be performed when placing an airway stent in the upper trachea.
ACKNOWLEDGEMENTS
We thank Andrea Baird, MD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Conflict of interest: none declared.
Author contributions
Hideyuki Niwa: Conceptualization; Formal analysis; Project administration; Writing—original draft; Writing—review & editing. Masahide Oki: Conceptualization; Investigation; Project administration. Hideo Saka: Conceptualization; Investigation. Atsushi Torii: Data curation; Investigation. Arisa Yamada: Data curation; Investigation. Fumie Shigematsu: Data curation; Investigation. Akane Ishida: Data curation; Investigation. Yoshihito Kogure: Data curation; Formal analysis.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Khaled M. Al-Kattan, Claudio Andreetti, Rajashekara H.V. Reddy and the other anonymous reviewer(s) for their contribution to the peer review process of this article.
REFERENCES
- 1. Ost DE, Ernst A, Grosu HB, Lei X, Diaz-Mendoza J, Slade M, AQuIRE Bronchoscopy Registry et al. Therapeutic bronchoscopy for malignant central airway obstruction: success rates and impact on dyspnea and quality of life. Chest 2015;147:1282–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Puma F, Ragusa M, Avenia N, Urbani M, Droghetti A, Daddi N. et al. The role of silicone stents in the treatment cicatricial tracheal stenoses. J Thorac Cardiovasc Surg 2000;120:1064–9. [DOI] [PubMed] [Google Scholar]
- 3. Ishida A, Oki M, Saka H.. Fully covered self-expandable metallic stents for malignant airway disorders. Respir Investig 2019;57:49–53. [DOI] [PubMed] [Google Scholar]
- 4. Han X, Li L, Zhao Y, Liu C, Jiao D, Ren K. et al. Individualized airway-covered stent implantation therapy for thoracogastric airway fistula after esophagectomy. Surg Endosc 2017;31:1713–8. [DOI] [PubMed] [Google Scholar]
- 5. Noppen M, Meysman M, Claes I, D’Haese J, Vincken W.. Screw-thread vs Dumon endoprothesis in the management of tracheal stenosis. Chest 1999;115:532–5. [DOI] [PubMed] [Google Scholar]
- 6. Martínez-Ballarín JI, Díaz-Jiménez JP, Castro MJ, Moya JA.. Silicone stents in the management of benign tracheobronchial stenoses. Tolerance and early results in 63 patients. Chest 1996;109:626–9. [DOI] [PubMed] [Google Scholar]
- 7. Hervé D, Fabien M, Laroumagne S, Astoul P.. Silicone stents, the rigid bronchoscope, and the standard of care in central airway stenosis. Curr Respir Care Rep 2012;1:46–53. [Google Scholar]
- 8. Plojoux J, Laroumagne S, Vandemoortele T, Astoul PJ, Thomas PA, Dutau H.. Management of benign dynamic "A-shape" tracheal stenosis: a retrospective study of 60 patients. Ann Thorac Surg 2015;99:447–53. [DOI] [PubMed] [Google Scholar]
- 9. Olze H, Dörffel W, Kaschke O.. Endotracheal silicon stents in therapy management of benign tracheal stenoses. HNO 2001;49:895–901. [DOI] [PubMed] [Google Scholar]
- 10. Menna C, Poggi C, Ibrahim M, D'Andrilli A, Ciccone AM, Maurizi G. et al. Coated expandable metal stents are effective irrespective of airway pathology. J Thorac Dis 2017;9:4574–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lemaire A, Burfeind WR, Toloza E, Balderson S, Petersen RP, Harpole DH Jr. et al. Outcomes of tracheobronchial stents in patients with malignant airway disease. Ann Thorac Surg 2005;80:434–7. [DOI] [PubMed] [Google Scholar]
- 12. Colt HG, Harrell J, Neuman TR, Robbins T.. External fixation of subglottic tracheal stents. Chest 1994;105:1653–7. [DOI] [PubMed] [Google Scholar]
- 13. Miwa K, Takamori S, Hayashi A, Fukunaga M, Shirouzu K.. Fixation of silicone stents in the subglottic trachea: preventing stent migration using a fixation apparatus. Ann Thorac Surg 2004;78:2188–90. [DOI] [PubMed] [Google Scholar]
- 14. Majid A, Fernandez-Bussy S, Kent M, Folch E, Fernandez L, Cheng G. et al. External fixation of proximal tracheal airway stents: a modified technique. Ann Thorac Surg 2012;93:167–9. [DOI] [PubMed] [Google Scholar]
- 15. Spelsberg FW, Wollenberg B, Weidenhagen R, Lang RA, Winter H, Jauch K-W. et al. Tracheal stents for esophagotracheal fistula in laryngectomy patients. Safe fixation to the tracheostoma. HNO 2009;57:1065–9. [DOI] [PubMed] [Google Scholar]
- 16. Andreetti C, Menna C, D'Andrilli A, Ibrahim M, Venuta F, Santini M. et al. A modified technique to simplify external fixation of the subglottic silicone stent. Interact CardioVasc Thorac Surg 2018;27:878–80. [DOI] [PubMed] [Google Scholar]
- 17. Huang J, Zhang Z, Zhang T.. Suture fixation of tracheal stents for the treatment of upper trachea stenosis: a retrospective study. J Cardiothorac Surg 2018;13:111. [DOI] [PMC free article] [PubMed] [Google Scholar]