Abstract
Background
This is an update of a Cochrane Review first published in The Cochrane Library in Issue 4, 2007.
Poor voice quality due to a voice disorder can lead to a reduced quality of life. In occupations where voice use is substantial it can lead to periods of absence from work.
Objectives
To evaluate the effectiveness of interventions to prevent voice disorders in adults.
Search methods
We searched databases including CENTRAL, MEDLINE, EMBASE, CINAHL, PsycINFO and OSH Update to March 2010.
Selection criteria
Randomised controlled clinical trials (RCTs) evaluating interventions for preventing voice disorders in adults. For work‐directed interventions, interrupted time‐series and prospective cohort studies were also eligible.
Data collection and analysis
Two authors independently extracted data and assessed trial risk of bias. We performed meta‐analysis where appropriate.
Main results
We identified six randomised controlled trials including a total of 262 participants. Four studies were conducted with primary school or kindergarten teachers, one with student teachers and one with telemarketers.
Three studies found similar self‐reported vocal symptoms between those who attended direct voice training and those who were in a no intervention control group (standardised mean difference (SMD) 0.27; 95% CI ‐0.12 to 0.66).
Two studies found similar self‐reported vocal symptoms between those who attended indirect voice training and those who were in a no intervention control group (SMD 0.44; 95% CI ‐0.03 to 0.92).
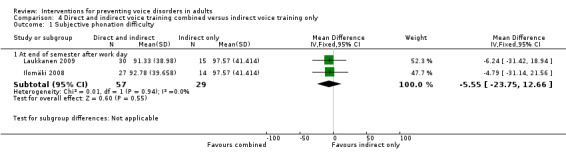
One study found similar scores on the Voice Handicap Index for those who had direct and indirect voice training combined and for those who had no intervention. Two studies compared a combination of direct and indirect voice training with indirect voice training only. Both studies found similar scores for self‐reported phonation difficulty (mean difference ‐5.55; 95% CI ‐23.75 to 12.66) in both groups.
The evidence for all comparisons was rated as low quality.
No work‐directed studies were found. No studies evaluated the effectiveness of prevention in terms of sick leave or number of diagnosed voice disorders.
Authors' conclusions
We found no evidence that either direct or indirect voice training or the two combined are effective in improving self‐reported vocal functioning when compared to no intervention. The current practice of giving training to at‐risk populations for preventing the development of voice disorders is therefore not supported by definitive evidence of effectiveness. Larger and methodologically better trials are needed with outcome measures that better reflect the aims of interventions.
Plain language summary
Interventions for preventing voice disorders in adults
People in occupations where voice use is central, such as teachers, are more at risk of developing voice disorders. The definition of voice disorders and their possible causes as well as the best methods for preventing them are still being debated. There is also no consensus on the best method of evaluating the voice, although many consider auditory voice quality assessment (where an expert judge listens to a recording of a participant's voice and makes his or her own judgment of its level of abnormality) as a gold standard measure. Voice training is used to prevent voice disorders. Voice training usually consists of a combination of 'direct' and 'indirect' treatment techniques. Direct techniques focus on the underlying physiological changes needed to improve an individual's technique in using the vocal system and may aim to alter vocal fold closure (adduction), respiratory patterns or resonance, pitch or articulatory tension. In practice this means training about how to achieve correct posture, breathing techniques and making various sounds like humming, singing musical scales or yawning. Indirect techniques, on the other hand, concentrate on contributory and maintenance aspects of the voice disorder and may involve relaxation strategies, counselling, explanation of the normal anatomy and physiology of the vocal tract, explanation of the causal factors of voice disorders and voice care and conservation.
We conducted a systematic search of the literature on preventing voice disorders in adults. We then appraised the quality of the studies found and combined their results. We found six studies which met our inclusion criteria. Four were conducted with teachers, one with student teachers and one with telemarketers.
We found no evidence that either direct or indirect voice training nor the two combined are effective in improving vocal functioning when measured using self‐reported outcomes and when compared to no intervention.
All the included studies were small and of low methodological quality. Given the extent of the problem and the widespread use of voice training, further research is warranted.
Background
This is an update of a Cochrane Review first published in The Cochrane Library in Issue 4, 2007.
In modern society, there is an increasing demand for oral communication in many occupations. It has been estimated that a well‐functioning voice is essential to one‐third of the labour force (Laukkanen 1995; Verdolini 2001; Vilkman 2004). Furthermore, it has been argued that the use of the voice in various professional and social contexts is constantly growing (Vilkman 2000b), due to the prevalence of new speech technology applications, such as mobile phones.
People who use their voice as a main tool in their work, i.e. professional voice users, often suffer from voice symptoms to a varying extent (Fritzell 1996; Scherer 1987; Smith 1998; Titze 1997). Teachers have been found to be the largest occupational group among those seeking medical help for voice problems (Fritzell 1996; Herrington‐Hall 1988). Between 20% to 80% of teachers have reported suffering from various voice symptoms (Sala 2001; Smith 1997). These studies have investigated voice symptoms rather than cases in which specific voice disorders have been diagnosed. The risk factors in voice‐utilising professions include background noise, poor room acoustics, long speaking distance, poor quality of air (dryness, dust), poor working posture and vocal loading itself from speaking or singing (Vilkman 1996). Vocal load is measured in terms of time and intensity: the longer and louder a person has to talk, the greater the strain on the voice will be and the more vocal capacity is required (Buekers 1998). Pre‐professional voice training can be advantageous for future occupational voice users, but it is often insufficiently organised and, as a result, fails to prevent voice problems (Ohlsson 1987; Vilkman 2000a). The educational programmes for singers and actors who are required to have a high quality of voice in their occupation include voice training. Other professionals also exposed to high vocal loading (teachers, salespersons, military, clergy), however, are only occasionally provided with training and usually on the worker's own initiative. For example, many teachers regard their vocal symptoms as inherent to their occupation and do not necessarily take appropriate countermeasures (Morton 1998).
Voice quality is a continuum between normal and abnormal extremes, which is why the differentiation of a disordered voice from a normal one is complicated. A person may produce a hoarse voice without any sign of abnormality in the larynx. On the other hand, people with certain laryngeal pathologies do not necessarily reveal appreciable vocal disturbances until a considerably advanced stage (Treole 1997). In this review we consider people with voice problems or symptoms as not having a voice disorder until they have been identified/diagnosed as such by an ear, nose and throat (ENT) specialist or a speech‐language pathologist (SLP). In the literature voice fatigue, voice symptoms, voice problems and voice disorders are all terms used when studying occupational voice and its loading. Vocal loading is a combination of prolonged voice use and "additional loading factors (e.g. background noise, acoustics, air quality) affecting the fundamental frequency, type and loudness of phonation or the vibratory characteristics of the vocal folds as well as the external frame of the larynx" (Vilkman 2004). There is usually no direct dose‐response relationship between vocal loading and self‐perceived voice problems as the threshold for seeking clinical help varies greatly between individuals. In this situation, prevention programmes that share knowledge or skills can help in preserving and improving the voice. However, when people suffering from voice problems seek clinical help for them, they are often diagnosed as having a voice disorder. Hence, instead of prevention they are offered voice therapy. Having a voice disorder always implies that voice symptoms are experienced as problems, but experiencing symptoms does not always mean that a person has a voice disorder. Usually the reported voice problems include self‐perceived voice symptoms and reductions in physical, social, emotional or professional well‐being (Verdolini 2001).
It has been stated that "in general, the goal of voice care, both prevention and treatment, is to restore the best voice possible, a voice that will be functional for purposes of employment and general communication" (Colton 2006). The educational approach can help individuals to identify factors that may contribute to a voice problem, alter and avoid them, and modify vocal behaviour before any damage occurs (Duffy 2003). Early identification of voice problems is also likely to reduce their severity and the time needed for recovery (Russell 1998). Proper care of the voice also plays a key role in restoring and preserving the individual's occupational capacity (Ramig 1998). Interventions directed toward preventing voice disorders can be divided into person‐directed interventions (e.g. voice training) and work‐ or environment‐directed interventions (e.g. ergonomic consultation/education and improving the acoustic conditions of the workplace).
We have defined prevention programmes as interventions which are offered to people at risk of voice disorders. In this review we chose self‐reported measures of voice handicap (participation restrictions), voice symptoms and voice‐related quality of life as primary indicators of the effectiveness of prevention activities. This is because of the variation between individuals in how a particular voice disturbance is perceived to affect their communication or ability to fulfil social and occupational responsibilities. All other measures of vocal or laryngeal performance are considered as secondary outcomes, along with measures of sickness absence and return to work.
Studies of the effectiveness of non‐surgical interventions for treating diagnosed voice disorders have also been conducted. They have been dealt with in a separate review (Ruotsalainen 2007).
Objectives
To evaluate the effectiveness of interventions aimed at preventing voice disorders or reducing the incidence of voice problems in adults in comparison to no intervention or other intervention methods.
To categorise interventions aimed at preventing voice disorders or reducing the incidence of voice problems in adults who due to their occupation, studies, hobby or lifestyle are at risk of developing a voice disorder.
Methods
Criteria for considering studies for this review
Types of studies
We considered for inclusion all randomised controlled studies or cluster‐randomised trials evaluating the effectiveness of interventions to prevent voice disorders in adults. For environmental or work‐related interventions, it is much more difficult to randomise when the intervention is applied at the group level. For this type of intervention we also considered for inclusion prospective cohort studies (otherwise known as controlled clinical trials, controlled before‐after studies or quasi‐experimental studies).
Types of participants
We included studies in which the participants were adults (16 or over), who due to their occupation, studies, hobby or lifestyle were at risk of developing a voice disorder but had not yet been identified/diagnosed as having one by an ear, nose and throat (ENT) specialist or a speech‐language pathologist (SLP). The voice changes throughout life. In childhood the morphology of vocal fold tissues keeps changing and during puberty the larynx grows (Titze 1994).The three connective tissue layers of the lamina propria, despite being apparent already during puberty, continue to become more differentiated until the age of 16 or 17 (Colton 2006). In advanced age some age‐related changes (e.g. ossification, atrophy, dystrophy and oedema) affect phonation (Jasper 2000). However, it is the physiological rather than the chronological age which has a strong impact on how well the larynx functions in phonation (Titze 1994). In this study we considered participants older than 16 years as adults.
Types of interventions
We included studies with any kind of intervention aimed at preventing voice problems or reducing the incidence of voice problems. We categorised interventions as:
direct voice training, i.e. training that is applied directly to the voice production apparatus;
indirect voice training, i.e. training that is applied to other functions (physical or cognitive) that influence voice production; and
the above combined.
We compared interventions with no intervention and, where possible, with alternative interventions.
Types of outcome measures
Primary outcomes
As primary outcomes we included patient‐reported measures of voice handicap, voice symptoms or voice‐related quality of life. Voice handicap is a measure of why patients with the same amount of voice disorder experience different levels of 'handicap' or 'disability' as defined by the WHO (Franic 2005).
Secondary outcomes
As secondary outcomes we included all other measurement techniques for establishing the state of vocal or laryngeal performance including:
aerodynamic measurements;
fundamental frequency and/or intensity (e.g. phonetography);
perceptual (visual or auditory) measurements (e.g. stroboscopy, GRBAS, etc.);
physiological measurements; and
acoustic voice analysis (e.g. perturbation measurements).
We intended to include studies measuring sickness absence or return to work but no studies were found using these outcomes.
Search methods for identification of studies
Electronic searches
We searched the literature for evaluation studies of interventions for functional voice disorders without restrictions on language or publication. Systematic search strategies were developed together with the Cochrane ENT Group Trials Search Co‐ordinator and the Cochrane Occupational Health Field Information Specialist.
For the original version of this review we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2006, Issue 2), MEDLINE (PubMed, 1950 to March 2006), EMBASE (embase.com, 1974 to March 2006), CINAHL (OVID, 1983 to March 2006), PsycINFO (webSPIRS, 1967 to February 2006), Science Citation Index (ISI Web of Science, Thomson, 1986 to March 2006) and the Occupational Health databases OSH‐ROM (webSPIRS, to February 2006). The search string for randomised controlled trials is based on Robinson 2002 and the string for non‐randomised studies on Verbeek 2005. Since the opportunities for naming and classifying voice disorders and their various treatments are so abundant, the searches were developed with the aim of maximum sensitivity at the expense of specificity. The date of the last search was the 5 April 2006. Details of the search strategies used can be found in Appendix 1, Appendix 2 and Appendix 3.
For the 2010 update of this review we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2010, Issue 1), MEDLINE (PubMed, 2006 to March 2010), EMBASE (embase.com, 2006 to March 2010), CINAHL (OVID, 2006 to 19 March 19 2010), PsycINFO (OVID, 2006 to 9 March 9 2010) and OSH Update (all databases, 2006 to March 2010). In addition, we searched the following databases in June 2009: the Cochrane ENT Group Trials Register, AMED, BIOSIS Previews, CAB Abstracts, ISI Web of Science, LILACS, KoreaMed, China National Knowledge Infrastructure, mRCT and ICTRP. The date of the last search was 19 March 2010. Details of the updated search strategies can be found in Appendix 4, Appendix 5, Appendix 6, Appendix 7, Appendix 8 and Appendix 9.
Searching other resources
We also carefully reviewed references from articles. We contacted authors of studies and other experts in the field for advice on further studies.
Data collection and analysis
Selection of studies
After employing the search strategies outlined above, three authors (JR, JS and LL) undertook study selection. Two authors independently assessed whether each of the studies found met the inclusion criteria. Disagreements were settled by consensus. We sought to obtain further information from the authors when a paper was found to contain insufficient information for reaching a decision on eligibility. The authors intend to perform a new search for trials every two years and to update the review accordingly.
Data extraction and management
Three authors (JR, JS and LL) extracted data. Two authors independently extracted data from each of the included trials regarding the country where the study was conducted, the type of study design used, characteristics of the study participants (as per study inclusion criteria) and types of interventions and outcomes. Results data (means and standard deviations) were also extracted for the purpose of meta‐analyses. We requested and received missing data from the following authors: Orla Duffy, Anne‐Maria Laukkanen and Andrea Gomes. Disagreements were settled by consensus.
Assessment of risk of bias in included studies
Three authors (JR, JS and LL) independently assessed the risk of bias in trials according to the guidance given in the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2008).
For the appraisal of cohort studies, we intended to use a validated instrument (Slim 2003). No cohort studies were, however, included in this review. Disagreements were settled through discussion.
Measures of treatment effect
The results of each trial were plotted as means and standard deviation (SD) for continuous outcomes and as odds ratios for dichotomous outcomes. In contrast to the previous version of the review, we also used standardised mean differences to be able to pool studies with similar outcomes measured with different scales. We felt that increasing power by combining small studies with non‐significant findings was important even though we know that standardised mean differences are more difficult for clinicians to interpret. We used the general assumption that an effect size of 0.2 indicates a small effect, 0.5 a moderate effect and 0.8 and beyond a big effect.
Unit of analysis issues
Two studies, Laukkanen 2009 and Ilomäki 2008, used the same control group. To avoid including the control group participants twice in the meta‐analysis we split the control group participants equally between the two studies.
Dealing with missing data
Where necessary, we sought missing statistical data (means and standard deviations) from trial authors. Since all studies had outcomes using continuous data, we were unable to conduct an intention‐to‐treat analysis. Results for the Bovo 2007 study were calculated from the raw patient data provided in the article because the reported figures were based on log‐transformed data. Bovo 2007 reported the scores separately for each participant. We then calculated means and standard deviations based on the reported data. Results for the Oliveira 2009 study were calculated from raw data obtained from the author because the voice symptom scores in the article were reported separately for men and women and they did not include standard deviations. In addition to the results of the voice symptom questionnaire, Oliveira 2009 also reported the same data as symptoms being absent or present and as improvement, worsening or no change. We did not use these data. The results for the Laukkanen 2009 study were obtained from the authors because they reported their results only in figures. This data set also contained the results for the self‐reported outcomes used in the Ilomäki 2008 study and so we used the results data obtained from the authors and not those presented in this article. This also enabled us to use only the after work day measurements because in Ilomäki 2008 the before and after work day measurements had been merged as means.
Assessment of heterogeneity
We tested for statistical heterogeneity by means of the I2 statistic in the meta‐analysis graphs. If this value is greater than 50% there is substantial heterogeneity between studies. When studies were statistically heterogeneous, we used a random‐effects model; otherwise we used a fixed‐effect model. All estimates included a 95% confidence interval (95% CI).
Assessment of reporting biases
We planned to assess publication bias by means of funnel plots. However, the small number of included studies did not enable this.
Data synthesis
For interventions directed at individuals, we used only randomised controlled trials to draw conclusions. For work‐ or environment‐directed interventions that are applied at the group level we intended to include also prospective cohort studies but none were identified that met our inclusion criteria.
The decision as to whether to perform quantitative pooling was based on clinical homogeneity. We defined clinically homogeneous studies as those with similar populations, interventions and outcomes measured at the same follow‐up point. The main problem in combining studies was the use of various outcome measures. We judged the Voice Handicap Index, vocal symptom score and questionnaire of vocal symptoms to be conceptually sufficiently similar to allow us to pool the results using standardised mean differences as implemented in the RevMan 5 software (RevMan 2008).
We rated the quality of evidence according to the GRADE system of high, moderate, low and very low quality as described in the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2008). For RCTs we started at the level of high quality of evidence and downgraded the quality by one or more levels depending on the number of qualifiers met.
Sensitivity analysis
We did not conduct any sensitivity analyses.
Results
Description of studies
Study selection
The original systematic searches yielded a set of 5937 references. From these, we identified a set of 46 potentially eligible studies based on title and abstract. These were then scrutinised further with regard to our inclusion and exclusion criteria. Altogether we excluded 44 studies leaving a total of two studies. The updated search strategies in March 2010 yielded a new set of 1696 references. From these, we identified a set of 48 potentially eligible studies. We then scrutinised the full‐text articles further with regard to our inclusion and exclusion criteria. Altogether we excluded 47 studies leaving a total of four new studies, out of which two publications (Ilomäki 2008; Laukkanen 2009) reported results based on overlapping samples. However, since the two studies reported on two different comparisons (Ilomäki 2008: voice training and voice hygiene lecture versus voice hygiene lecture alone; Laukkanen 2009: Voice Massage(TM) and voice hygiene lecture versus voice hygiene lecture alone) they are treated here as two separate studies. This brings the new total number of included studies to six.
Study designs
All of the included studies were randomised controlled trials. We were also aiming to include studies with interrupted time‐series and controlled before‐after designs for work‐directed interventions but the final sample contained none of these.
Country and time period
Four of the included studies were conducted in Europe: two in Finland (Ilomäki 2008 and Laukkanen 2009), one in the United Kingdom (Duffy 2004) and one in Italy (Bovo 2007). One study was conducted in Australia (Pasa 2007) and one in Brazil (Oliveira 2009). All the included studies are very recent.
Type of settings and participants
Interventions were conducted in occupational settings. In Ilomäki 2008, Laukkanen 2009 and Pasa 2007 the participants were primary school teachers. In Bovo 2007 the participants were kindergarten and primary school teachers and in Duffy 2004 they were student teachers. In Oliveira 2009 the participants were telemarketers.
Sample sizes
The total number of participants in the intervention groups was 147 and in the control groups 115.
Interventions
We found the following types of interventions:
1. Direct voice training
Three studies (Duffy 2004;Oliveira 2009;Pasa 2007) evaluated the effectiveness of training using direct intervention techniques alone compared to no intervention. In general, direct techniques focus on the underlying physiological changes needed to improve an individual's technique in using the vocal system. In Duffy 2004 this consisted of training focused on posture, respiration, release of tension in the vocal apparatus, resonance and voice projection. The authors do not provide any details regarding the type, length or frequency of vocal exercises. In Oliveira 2009 direct voice training consisted of vocal warm‐up and cool‐down as well as group activities regarding the psychodynamics of voice production. In order to promote vocal warm‐up, facilitating sounds, body movement techniques with sound production, overarticulation exercises, semi‐occluded vocal tract exercises (hand‐over‐mouth technique) and chant talk exercises were used in eight 30‐minute modules offered weekly. The facilitating sounds included humming sounds associated with chewing movements, fricatives and voice sounds associated with ascending musical scales (from C3 to C4) in staccato and legato. For cool‐down, voice sounds were also used, with descending musical scales (from G3 to C3), as well as the yawn‐sigh technique and laryngeal manipulation. In Pasa 2007 direct voice training consisted of warm‐up, stretching, contracting, and adductory strengthening exercises to be practised at home, twice each, twice per day, preferably morning and evening, for a six‐week period.
2. Indirect voice training
Two studies (Duffy 2004;Pasa 2007) looked at indirect voice training alone compared to no intervention. Indirect techniques concentrate on the contributory and maintenance aspects of the voice disorder (such as lack of knowledge). In Duffy 2004 this consisted of providing information on the mechanics of voice production, the amount and type of voice use, vocal behaviours thought to be phonotraumatic, hydration issues and lifestyle and diet factors that can support or interfere with a healthy voice. In Pasa 2007 participants were informed of the prevalence and impact of voice problems in teachers, basic anatomy and physiology of voice production, symptoms of voice disorders, strategies to reduce harmful vocal behaviours, managing and minimising health factors that contribute to the development and maintenance of voice problems, and changes to the speaking environment that increase vocal efficiency and reduce vocal harm. The training consisted of one two‐hour group session and three 30‐minute group sessions over ten weeks.
3. Direct and indirect voice training combined
Three studies (Bovo 2007; Ilomäki 2008; Laukkanen 2009) looked at direct and indirect voice training combined. In Bovo 2007 the intervention consisted of lectures and a practical session. The lecture concerned the anatomy and physiology of phonation, the causes of and predisposing factors to abnormal vocal fold pathology, the warning symptoms of vocal fatigue, voice ergonomics (i.e. vocal hygiene, strategies to reduce vocal demand in the classroom, and changing behaviour in daily life to reduce vocal abuse), classroom acoustics, and amplification systems. The practical session consisted of group voice therapy training: efficient respiratory behaviour; laryngeal muscle relaxation; manual circumlaryngeal therapy; relaxed voicing with elimination of hard glottal attack, chewing, voicing, yawn‐sigh, chant talk and pitch inflections; proper oral‐nasal resonance; and developing greater oral opening. The course had a duration of seven hours and consisted of two theoretical lectures each 90 minutes long and two sessions of group voice therapy each of 120 minutes. In Ilomäki 2008 the intervention consisted of a three‐hour lecture and five one‐hour voice training lessons during nine weeks. The lecture concerned the basics of voice and speech production, the main factors causing vocal loading in teachers, methods available to avoid overloading, and basics of economic versus non‐economic voice use. The voice training course was geared towards gaining ease and endurance in voice production, and getting rid of any poor vocal habits. The learning methods were introspections, discussions, voice exercises and individualised homework with a view to finding economic voice production, i.e. avoidance of excessive muscle tension of the larynx, deep breathing technique, firmness of phonation without effort, well‐resonating voice quality to improve audibility, and adequate individual pitch and loudness range and variation. In Laukkanen 2009 another randomly chosen group of 30 participants was added to the sample used in Ilomäki 2008. These participants also received the three‐hour voice hygiene lecture and in addition they were given Voice Massage(TM) in five one‐hour sessions over a period of 11 weeks. Voice Massage(TM) consists of manipulation of voice and speech production muscles of the larynx, respiration and articulation. It also includes some vocal and respiratory exercises during manipulation.
Outcomes measured
1. Primary outcomes: self‐report measures
Two studies (Duffy 2004;Bovo 2007) used the Voice Handicap Index (VHI) (Jacobson 1999). The VHI is a 30‐item five‐point Likert scale which assigns a number to how frequently the responder experiences particular problems described in the statements, with 0 = never and 4 = frequently. The scores have a potential range from 0 to 120 with the higher score correlating with a greater impact.
One study (Duffy 2004) used the Vocology Screening Profile (Hazlett 2001). This 18‐item questionnaire measures the frequency of the occurrence of vocal symptoms with a five‐point Likert scale, with 0 = never and 4 = frequently. The range of potential scores is 0 to 72.
One study (Pasa 2007) used the vocal use patterns at work questionnaire (13 items) and the vocal capabilities questionnaire (17 items). The former required participants to indicate how often they used particular negative vocal behaviours at work (e.g. throat clearing and shouting over large distances) by rating on a 100 mm visual analogue scale (VAS) ranging from "never" to "every time I use my voice" for every question. The results were reported as mean sums of ratings on a scale from 0 (no vocal misuse) to 1300 (greatest amount of vocal misuse). The latter questionnaire aimed to identify the extent to which participants experienced vocal symptoms associated with throat discomfort, breath control, pitch, loudness, voice quality and projection. For every question the participants rated their perception of their vocal abilities on a 100 mm VAS that ranged from "never" to "every time I use my voice". The results were reported as mean sums of ratings on a scale from 0 (no symptoms) to 1700 (most severe symptoms).
Two studies (Ilomäki 2008 and Laukkanen 2009) used three visual analogue scales for subjective evaluations: mean phonation difficulty (0 = particularly easy voice production; 100 = ordinary voice production; 200 = very difficult voice production), mean voice quality (0 = very good; 100 = ordinary quality; 200 = very poor quality) and mean throat tiredness (0 = no tiredness at all; 100 = very tired).
One study (Oliveira 2009) used the questionnaire of vocal symptoms (Lehto 2003) which is composed of 11 items. Responses to these items are given on a four‐point scale including: 1 = not even once a year or never, 2 = a few times a year or sometimes, 3 = approximately once a month or quite often, and 4 = almost every week or very often. The questionnaire results in composite scores that add up the individual scores for each item.
The study by Oliveira 2009 also used an adapted version of a questionnaire originally used by Lehto 2003 and named it the Benefits Obtained with Vocal Training (BVT) questionnaire. Of the 23 items in this questionnaire 11 were selected for use in this study. Two items were also added: "With the training my voice became clearer than before" and "With the training my voice became more resistant to fatigue than before". The adapted BVT questionnaire was scored: 1 = disagree, 2 = neither agree nor disagree, 3 = somewhat agree and 4 = agree. Items scored 3 or 4 were considered agreement. Results were reported as percentages of agreement to the 13 items of the questionnaire.
2.1. Secondary outcomes: observer‐rated measures
One study (Bovo 2007) measured voice quality with the GRBAS scale (Hirano 1989). In two studies (Ilomäki 2008; Laukkanen 2009), three experienced voice trainers evaluated text samples read out loud by the participants for voice quality and firmness of phonation using the Judge Program (Granqvist 2003) with a VAS ranging from 0 to 1000 units. Voice quality was assessed with a unipolar scale: 0 = very poor quality and 1000 = very good quality. Firmness of phonation was assessed with a bipolar scale: 0 = breathy phonation, 500 adequate firmness, and 1000 = strained voice. Results were reported as the mean of the three separate assessments.
2.2. Secondary outcomes: instrumental measures
One study (Duffy 2004) used the Dysphonia Severity Index (Wuyts 2000). Four studies (Bovo 2007; Ilomäki 2008; Laukkanen 2009; Pasa 2007) used one or more of the following measures: fundamental frequency (F0), jitter, shimmer, sound pressure level, alpha ratio (the ratio between the spectral energy below and above 1000Hz), maximum phonational frequency range or maximum phonation time (MPT) or normalised maximum phonation time (where the mean normative MPT for each participant's gender was subtracted from their longest MPT). One study (Bovo 2007) measured noise‐to‐harmonic ratio.
Type of control group
Four studies (Duffy 2004; Bovo 2007; Oliveira 2009; Pasa 2007) employed a no intervention control group. Two studies (Ilomäki 2008 and Laukkanen 2009) used a minimal intervention (a voice hygiene lecture) as the control group. Two studies (Duffy 2004; Pasa 2007) compared direct and indirect voice training.
Follow up
Duffy 2004 and Oliveira 2009 conducted only baseline and post‐intervention measurements. Pasa 2007 reported baseline, post‐intervention and a follow up of 10 weeks after the initial session. Bovo 2007 reported follow‐up scores for three and 12 months after intervention. However, the three‐month scores were the only post‐intervention measures available for both groups since the 12‐month follow up was completed only for the intervention group. In Ilomäki 2008 and Laukkanen 2009 measurements were made before and after a vocally loading working day and at the start and end of one school term. We used the measurements at the end of the working day.
Excluded studies
Reasons for excluding the 90 studies were as follows (see 'Characteristics of excluded studies'):
non‐randomised study design;
participants had dysphonia;
participants partly the same as in an already included study;
no self‐reported outcome; or
no intervention.
Risk of bias in included studies
Allocation
When it comes to the prevention of voice disorders the concealment of allocation into intervention and control groups is not an issue as participants cannot help but notice if they are involved in an active intervention. None of the studies reported the method of randomisation. However, four studies sought validation for the randomisation procedure by comparing groups after allocation. Duffy 2004 found no significant differences. Bovo 2007 reported the groups had been matched for age, working years, hoarseness grade and vocal demand. Ilomäki 2008 and Laukkanen 2009 found no significant differences in age, years taught, hours taught per week, hours taught during term or group size in the classroom. Pasa 2007 found no significant differences in age, years taught or hours taught per day.
Blinding
When the blinding of those assessing the outcome was an issue, i.e. with the secondary or observer‐rated outcomes like the GRBAS scale in the Bovo 2007 study, the voice samples were assessed blind by the first two authors of the study. We assume that this means that they were unaware of treatment allocation and participant identity. Ilomäki 2008 and Laukkanen 2009 did not report the blinding of their assessors.
Incomplete outcome data
The studies by Bovo 2007 and Oliveira 2009 suffered total losses of 36% and 52% of their initial samples respectively. Duffy 2004 reports that the training provided to the direct group required the most time, and due to this there was a drop‐out rate. This suggests that attrition may well have affected the results differentially. No numbers are given, however. Pasa 2007 reported no drop‐outs and only one participant from the shared control group was excluded from the analyses in the studies by Ilomäki 2008 and Laukkanen 2009 because of incomplete recordings. Oliveira 2009 reports that sample size was estimated according to a previously published study to allow for attrition. The study by Pasa 2007 is the only one to report having conducted a priori power calculations to ensure that even with attrition the study would have had adequate statistical power to detect significant differences. However, with the small number of participants in the study either the effect was overestimated or the variance was underestimated.
Selective reporting
The quality of reporting, especially of results, was poor in most studies and most of the reported comparisons were within and not between groups. The results figures reported in Bovo 2007 were based on log‐transformed data and not the reported raw data but this was not explained in the text. Results data for the Duffy 2004 and the Oliveira 2009 studies were obtained from the authors as standard deviations were not reported in the text. None of the authors reported that they had chosen primary outcomes a priori but all had included multiple outcomes. It is unclear whether studies reported all outcomes or only a selective proportion of those that were measured.
Effects of interventions
1. Direct voice training versus no intervention
1.1 Primary outcome self‐report measures
One study (Duffy 2004) found similar self‐reported vocal functioning as measured with the Voice Handicap Index in those who attended direct voice training and in the no intervention control group (mean difference (MD) 4.99; 95% CI ‐0.79 to 10.77). One study (Oliveira 2009) found similar self‐reported vocal functioning as measured with the questionnaire of vocal symptoms after direct voice training as in the no intervention control group (MD ‐1.11; 95% CI ‐5.11 to 2.89). One study (Pasa 2007) found a similar level of self‐reported vocal functioning as measured by the number of voice symptoms in the two groups (post‐intervention MD 143.6; 95% CI ‐65.57 to 352.77, follow up MD 88.69; 95% CI ‐100.76 to 278.14).
When combined in a meta‐analysis as standardised mean differences, the pooled estimate for these three studies for any voice problem is standardised mean difference (SMD) 0.27 (95% CI ‐0.12 to 0.66). Even though this is not significant it still includes an appreciable effect of fewer voice problems in the control group.
The numbers of vocal misuse behaviours after direct voice training were also similar to the no‐intervention control group in Pasa 2007 (post‐intervention MD 64.73; 95% CI ‐65.48 to 194.94, follow up MD 53.99; 95% CI ‐73.58 to 181.56).
The quality of the evidence from these three studies was downgraded two levels because of serious risk of bias in all three studies. Our conclusion that vocal functioning is similar after direct voice training compared to no intervention is based on low quality evidence. The 95% confidence interval indicates low precision because it still includes a moderate effect size of 0.40.
1.2 Secondary outcome instrumental measures
One study (Pasa 2007) found a similar maximum phonation time immediately after direct voice training and in the no intervention control group (MD 3.32; 95% CI ‐0.53 to 7.17) but at follow up the results favoured the intervention group (MD 3.17; 95% CI 0.24 to 6.10). The same study also found a similar maximum phonational frequency range after direct voice training and in the no intervention control group (post‐intervention MD ‐0.05; 95% CI ‐4.59 to 4.49, follow up MD ‐1.03; 95% CI ‐5.04 to 2.98).
2. Indirect voice training versus no intervention
2.1 Primary outcome self‐report measures
One study (Duffy 2004) compared indirect voice training and no intervention and found similar self‐reported vocal functioning as measured with the Voice Handicap Index (MD 5.47; 95% CI ‐1.42 to 12.36). One study (Pasa 2007) found similar numbers of vocal misuse behaviours after indirect voice training and no intervention (post‐intervention MD 59.24; 95% CI ‐52.76 to 171.24, follow up MD 3.94; 95% CI ‐115.66 to 123.54) and of voice symptoms (post‐intervention MD 104.62; 95% CI ‐94.71 to 303.95, follow up MD ‐25.9; 95% CI ‐215.10 to 163.30).
When both studies are combined in a meta‐analysis the effect size for any voice problem is SMD 0.44 with a 95% CI ‐0.03 to 0.92. Even though this is not significant it still includes an appreciable effect of fewer voice problems in the control group.
The quality of the evidence from these two studies was downgraded two levels because of serious risk of bias in both studies. We conclude that there is low quality evidence that vocal functioning is similar after indirect voice training compared to no intervention. However, the 95% confidence interval also included an appreciable adverse effect indicating more symptoms after voice training.
2.2 Secondary outcome instrumental measures
One study (Pasa 2007) compared indirect voice training and no intervention and found a similar maximum phonation time (post‐intervention MD 2.16; 95% CI ‐1.67 to 5.99, follow up MD 2.86; 95% CI ‐0.27 to 5.99) and a similar maximum phonational frequency range (post‐intervention MD 2.00; 95% CI ‐1.86 to 5.86, follow up MD 0.71; 95% CI ‐3.72 to 5.14).
3. Direct and indirect voice training combined versus no intervention
3.1 Primary outcome self‐report measures
One study (Bovo 2007) compared direct and indirect voice training combined with no intervention and found similar self‐reported vocal functioning as measured with the Voice Handicap Index (MD ‐7.35; 95% CI ‐15.07 to 0.37).
3.2 Secondary outcome instrumental measures
There is evidence from one study (Bovo 2007) that direct and indirect voice training combined is effective in improving vocal functioning as measured with maximum phonation time (MD 3.18 seconds; 95% CI 1.93 to 4.43) when compared to no intervention.
4. Direct and indirect voice training combined versus indirect voice training only
4.1 Primary outcome self‐report measures
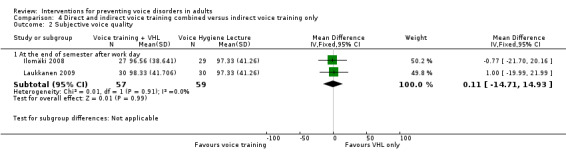
Two studies (Ilomäki 2008; Laukkanen 2009) compared direct and indirect voice training combined with indirect voice training only. Ilomäki 2008 compared voice training and a voice hygiene lecture to a voice hygiene lecture only and found similar self‐reported vocal functioning as measured with self‐reported phonation difficulty (MD ‐4.79; 95% CI ‐31.14 to 21.56), voice quality (MD ‐0.77; 95% CI ‐21.70 to 20.16) or throat tiredness (MD ‐0.93; 95% CI ‐12.88 to 11.02). Laukkanen 2009 compared Voice Massage(TM) and a voice hygiene lecture to a voice hygiene lecture only and found similar self‐reported vocal functioning as measured with self‐reported phonation difficulty (MD ‐6.24; 95% CI ‐31.42 to 18.94), voice quality (MD 1.00; 95% CI ‐19.99 to 21.99) or throat tiredness (MD ‐0.93; 95% CI ‐13.15 to 11.29).
When the two studies were combined in a meta‐analysis, the pooled mean difference for the phonation difficulty was MD ‐5.55; 95% CI ‐23.75 to 12.66.
The quality of the evidence from these two studies was downgraded two levels because of serious risk of bias. We conclude that there is low quality evidence that vocal functioning is similar after direct and indirect voice training combined and indirect voice training only.
4.2 Secondary outcome perceptual measures
One study (Ilomäki 2008) compared direct and indirect voice training combined with indirect voice training only and found similar scores in perceptually assessed voice quality (MD 19.00; 95% CI ‐41.53 to 79.53) and firmness of phonation (MD 16.00; 95% CI ‐38.32 to 70.32).
4.3 Secondary outcome instrumental measures
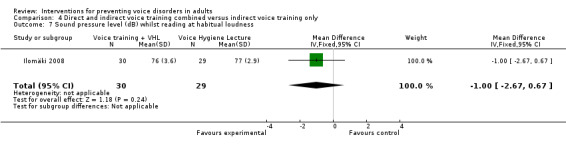
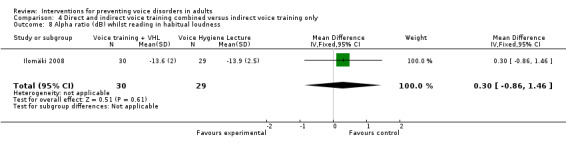
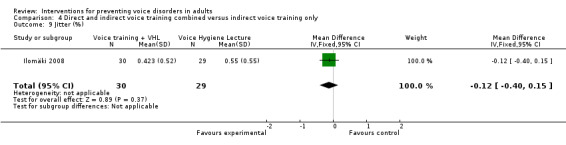
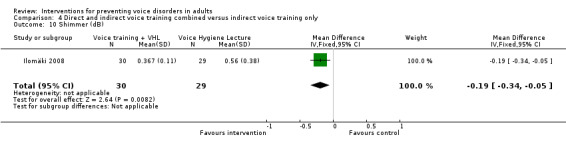
One study (Ilomäki 2008) compared direct and indirect voice training combined with indirect voice training only and found similar scores in average fundamental frequency (F0) (MD 3.00; 95% CI ‐5.38 to 11.38), sound pressure level (MD ‐1.00; 95% CI ‐2.67 to 0.67), alpha ratio (MD 0.30; 95% CI ‐0.86 to 1.46) and jitter (%) (MD ‐0.12; 95% CI ‐0.40 to 0.15) when reading at habitual loudness. The same study (Ilomäki 2008) found evidence that direct and indirect voice training combined is effective in improving shimmer (dB) (MD ‐0.19; 95% CI ‐0.34 to ‐0.05) when reading at habitual loudness, when compared to indirect voice training only.
Discussion
Summary of main results
In this review we did not find evidence for the effectiveness of direct or indirect voice training nor the two combined in improving vocal functioning when compared to no intervention as measured with any patient‐reported primary outcome measure. However, the 95% confidence intervals included appreciable effects especially in favour of the no intervention group. In terms of secondary outcomes, direct and indirect voice training combined was effective in increasing maximum phonation time and decreasing shimmer in two separate studies.
Overall completeness and applicability of evidence
The significant result of an increase in maximum phonation time found in one study (Bovo 2007) is an indication of compliance with the intervention as the phonation time increased by 30% in the intervention group and not in the control group. However, the baseline values were well below average and therefore the clinical relevance of this finding is probably low (cf. Raes 1996). The small decrease in shimmer found in another study (Ilomäki 2008) is also of questionable importance. A measurement of shimmer (dB) is an evaluation of the cycle to cycle variability of the amplitude of vocal fold vibration within the analysed voice sample. Lower or decreased values therefore suggest a better ability to maintain periodicity in vocal fold vibration. As the normal human voice is only quasiperiodic, any voice sample will contain some short‐term variability in both amplitude (i.e. shimmer) and pitch (i.e. jitter). Average values of shimmer for women without voice problems have been measured, in a range of studies, as lying somewhere between 0.24 dB and 0.48 dB when measured with the Multi‐Dimensional Voice Program (Kent 2003). According to the authors there are no normative data for the Intelligent Speech Analyser(TM) used in their study. Therefore it is difficult to say whether the measured 0.119 dB decrease from 0.486 dB to 0.367 dB in mean shimmer has any clinical relevance.
Objective measurements such as videolaryngoscopy, acoustical analysis (frequency, intensity and perturbation measures), maximum phonation time, etc. have also yet to yield recommendations for the ranges of a healthy voice, because the voice and its quality is a continuum unique to each person. Indirect measures, such as voice failures leading to sick leave or the number of diagnosed voice disorders, appear not to be used at all as measures of effectiveness.
The finding that participants tend to report more symptoms or increased voice handicap following intervention could be due to an increased awareness of the symptoms and is probably not due to a real increase in symptoms or handicap.
Apparently the effectiveness of voice training in preventing voice disorders has not been studied extensively, since we found so few randomised controlled trials despite our very extensive search strategy. Our search strategy was also designed to find non‐randomised studies and in so doing we made sure that we did not overlook any other relevant evidence. An overview of published non‐randomised controlled trials of person‐directed interventions for the prevention of voice problems is presented in Table 1. According to one study (Hackworth 2007) indirect voice training only compared with indirect voice training and additional information on behavioral modification/teaching techniques did not result in significant differences in vocal problems, water consumption, minutes of daily vocal warm up, number of vocal breaks taken, talking over noise or the use of non‐verbal commands. One study (Timmermans 2004b) compared direct and indirect voice training combined and no intervention and found that the groups scored similarly on the Voice Handicap Index. Another study (Chan 1994) found that direct and indirect voice training combined was effective in reducing Relative Average Perturbation when compared to no intervention. The results seem similar to the findings of our review, but they are difficult to compare because non‐randomised studies are more prone to bias. However, the non‐randomised studies do indicate that we did not overlook results that would put the review in a totally different perspective.
1. Controlled (non‐randomised) trials.
| Study ID | Methods | Participants | Interventions | Outcomes | Results |
| Chan 1994 | CT | 25 female kindergarten teachers | 1) Direct and indirect voice training (12) 2) No intervention (13) | 2) Relative average perturbation, ratio of energy below 1 kHz to energy above 1 kHz, Duty Cycle (an EGG parameter) | Significant improvement in RAP when compared to no intervention |
| Hackworth 2007 | CT | 76 general and/or vocal music teachers | 1) Indirect voice training (19) 2) Indirect voice training and additional information on behavioral modification/teaching techniques (11) 3) No intervention (46) | 1) Daily log for 8 weeks about vocal problems, water consumption, minutes of daily vocal warm‐up, number of vocal breaks taken (complete voice rest) and talking over noise and/or use of non‐verbal commands | No significant differences between intervention and control groups |
| Timmermans 2004a | CT | 68 students of a school for audiovisual communication | 1) Direct and indirect voice training (49) 2) No intervention (19) | 1) Voice Handicap Index 2) GRBAS, videolaryngostroboscopy, MPT, jitter, I‐low, Fo‐high, Dysphonia Severity Index | No significant differences between intervention and control groups |
| Timmermans 2004b | CT | 46 students of a school for audiovisual communication (same participants as in Timmermans 2004a) | 1) Direct and indirect voice training (23) 2) No intervention (23) | 1) Voice Handicap Index 2) GRBAS, videolaryngostroboscopy, MPT, jitter, I‐low, Fo‐high, Dysphonia Severity Index | No significant differences between intervention and control groups |
CT = controlled trial (i.e. allocation to groups was not randomised) EGG = electroglottographic RAP = relative average perturbation
Possible reasons for not succeeding in finding a significant positive prevention effect could be inadequacies in the duration of the training (the length in time and amount of the sessions) or in the formulation of the contents of the training. The results we found do not support the current practice of giving training to at‐risk populations for preventing the development of voice disorders. A clinically more relevant outcome would be the number of teachers that report having a current voice problem, such as in Roy 2004. We can take the figure of 11% for current voice problems from that study as an indication of the incidence of voice problems among teachers even though the real incidence would probably be lower. If we assume that training would be able to reduce voice problems by a quarter to 8%, then we would need about 1500 study participants for a sufficiently powered study.
We defined self‐reported measures of voice handicap or symptoms as our primary outcome, because this is the clinical problem that is most relevant to patients. For example the Voice Handicap Index (Jacobson 1999) estimates the psychosocial handicap caused by an already existing voice problem or disorder and it is a frequently used and validated questionnaire. However, it is difficult to say what constitutes a clinically relevant result in prevention studies since any decrease in voice handicap could be relevant at the population level. Since we do not have a clinical case definition or cut‐off point beyond which we can speak of dysphonia cases it is not possible to say how many cases have been prevented.
Quality of the evidence
The methodological quality of all included studies was poor. Even though all included studies were randomised controlled trials they were small and none of them reported the method of randomisation used or whether the process was concealed. It was also difficult to get a good impression of the concealment of allocation to researchers. We assumed that outcomes that were measured by questionnaire were reported blind to the researchers but we could not be certain about this assumption. Most studies suffered losses to follow up but took no action to deal with the attrition. The reporting of the studies was also of low quality, which is reflected in our having to contact the authors for further information.
The follow‐up time after the intervention was 10 months in one trial, one school term in one trial and three months in another. The last measurement time was directly after the intervention in the remaining three trials. In terms of long‐term prevention of voice disorders three months is a rather short follow‐up time.
Potential biases in the review process
The negative results of our review cannot be explained by language bias because we applied no language restrictions to the systematic search strategy. It is unlikely that colleagues who determined study inclusion for non‐English articles misunderstood their instructions and thereby excluded acceptable randomised trials.
Agreements and disagreements with other studies or reviews
A recent systematic review about preventative voice training (Hazlett (In Press)) concluded that: "voice training may be beneficial for professional voice users". This was, however, based on the conclusions of the authors of the included articles and not on a synthesis of the available evidence. The final conclusion of the authors was that evidence of preventative training still remains inconclusive because of methodological limitations of the included studies. This concurs partially with the conclusions of our review where we conclude that there is no evidence for effectiveness.
It is also noteworthy that we did not find any studies of work‐directed or environmental interventions that satisfied our inclusion criteria even though it is clear that a voice handicap develops as a result of the interaction between environmental factors and voice quality or vocal functioning. For this reason the improvement of environmental factors could be a fruitful preventive strategy.
Authors' conclusions
Implications for practice.
We did not find evidence to support the current practice of giving training to at‐risk populations for preventing the development of voice disorders. This absence of evidence does not necessarily mean that such training is ineffective. The extent of the problem and the widespread practice of training means that better quality studies are urgently needed to be able to give stronger recommendations.
Implications for research.
It is clear that larger and methodologically better trials are needed to establish whether the development of voice disorders can be prevented effectively and efficiently. In terms of study design this means comparing two groups of participants with high vocal load, one of which is not given the preventive training. The ethical dilemma thus produced can be overcome by employing a delayed treatment control or offering a minimal intervention to the control group. A randomised design is feasible and should be used to prevent bias. The follow‐up time should be at least one year but preferably longer to establish a long‐term effect. In addition to a reduction in self‐reported symptoms on validated questionnaires, it should also be noted whether participants go on to develop dysphonia. The varying use of terminology should be addressed by seeking consensus regarding meaning and usage.
What's new
| Date | Event | Description |
|---|---|---|
| 19 March 2010 | New search has been performed | New searches run. We identified and included four new studies. They did not, however, affect the conclusions of the review. We also adopted the Cochrane 'Risk of bias' method for quality assessment of studies. |
History
Protocol first published: Issue 1, 2007 Review first published: Issue 4, 2007
| Date | Event | Description |
|---|---|---|
| 23 October 2008 | Amended | Converted to new review format. |
Acknowledgements
Mari Qvarnström and Anita Länsivuori from Kuopio University Hospital provided valuable insight into the everyday practice of voice assessment and training. Anne‐Maria Laukkanen, Bernadette Timmermans and Roberto Bovo patiently answered all our questions regarding their studies and Orla Duffy, Anne‐Maria Laukkanen and Andrea Gomes sent us their results data. Merja Jauhiainen designed the original systematic search strategies in collaboration with the Cochrane ENT Group's Trials Search Co‐ordinator. Müge Filiz, Hamilton Lima Wagner and Piotr Sakowski performed study selection on articles written in Turkish, Portuguese and Polish respectively.
Appendices
Appendix 1. Search strategy for MEDLINE through PUBMED (2006)
#1 dysphoni*[tw] OR hoarseness[mh] OR phonastheni*[tw] OR trachyphoni*[tw] OR functional voice disorder*[tw] OR psychogenic voice disorder*[tw] OR ventricular phonation[tw] OR conversion voice disorder*[tw] OR functional aphonia[tw] OR conversion aphonia[tw] OR conversion dysphonia[tw] OR phonation break[tw] OR functional falsetto[tw] OR mutational falsetto[tw] OR puberphonia[tw] OR juvenile voice[tw] OR laryngeal myasthenia[tw] #2 phonation[tw] NEAR (disease*[tw] OR disorder*) #3 (voice[tw] OR vocal[tw] OR phonation[tw]) NEAR (problem*[tw] OR symptom*[tw] OR complaints[tw] OR hygiene[tw] OR disturbance*[tw] OR tremor*[tw] OR impair*[tw] OR handicap*[tw] OR tension*[tw] OR strain*[tw] OR abuse*[tw] OR fatigue*[tw] OR misuse*[tw] OR reduct*[tw]) #4 (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double‐blind method[mh] OR single‐blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR "clinical trial"[tw] OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind*[tw])) OR "latin square"[tw] OR placebos[mh] OR placebo*[tw] OR random*[tw] OR research design[mh:noexp] OR comparative study[mh] OR evaluation studies[mh] OR follow‐up studies[mh] OR prospective studies[mh] OR cross‐over studies[mh] OR control*[tw] OR prospectiv*[tw] OR volunteer*[tw]) NOT (animal[mh] NOT human[mh]) #5 (effect*[tw] OR control*[tw] OR evaluation*[tw] OR protect*[tw]) NOT (animal[mh] NOT human[mh]) #6 (#1 OR #2 OR #3) AND (#4 OR #5)
Appendix 2. Search strategy for EMBASE (2006)
#1 dysphonia/exp OR hoarseness/exp OR phonastheni* OR trachyphoni* OR "functional voice disorder*" OR "psychogenic voice disorder*" OR "ventricular phonation" OR "conversion voice disorder*" OR "functional aphonia" OR "conversion aphonia" OR "conversion dysphonia" OR "phonation break" OR "functional falsetto" OR "mutational falsetto" OR puberphonia OR "juvenile voice" OR "laryngeal myasthenia" #2 phonation AND (disease* OR disorder*) #3 (voice/exp OR vocal OR phonation) AND (problem* OR symptom* OR complaints OR hygiene/exp OR disturbance* OR tremor* OR impair* OR handicap* OR tension* OR strain* OR abuse* OR fatigue* OR misuse* OR reduct* #4 #1 OR #2 OR #3 #5 #4 AND [embase]/lim AND [article]/lim AND [human/]lim #6 #5 AND [randomized controlled trial]/lim #7 #5 AND [controlled clinical trial]/lim #8 randomized controlled trial/exp OR clinical trial/exp OR double blind procedure/exp OR single blind procedure/exp OR (singl* OR doubl* OR trebl* OR tripl*) AND (mask* OR blind*) OR placebo/exp OR placebo* OR random* OR comparative study/exp OR "evaluation study" OR evaluation studies/exp OR follow up/exp OR prospective study/exp OR crossover procedure/exp OR prospectiv* OR volunteer* #9 #5 AND #8 #10 #6 OR #7 OR #9
Appendix 3. Search strategy for CENTRAL (2006)
#1 dysphoni* (in Title, Abstract, Keywords) OR hoarseness (in Title, Abstract, Keywords) OR phonastheni* OR trachyphoni* OR functional voice disorder* OR psychogenic voice disorder* OR ventricular phonation OR conversion voice disorder* OR functional aphonia OR conversion aphonia OR conversion dysphonia OR phonation break OR functional falsetto OR mutational falsetto OR puberphonia OR juvenile voice OR laryngeal myasthenia #2 (voice OR vocal OR phonation) NEAR (problem* OR symptom* OR complaints OR hygiene OR disorder* OR disease* OR disturbance* OR tremor* OR impair* OR handicap* OR tension* OR strain* OR abuse* OR fatigue* OR misuse* OR reduct*) #3 #1 OR #2
Appendix 4. Updated search strategy for MEDLINE through PUBMED (2010)
#1 dysphoni*[tw] OR hoarseness[mh] OR phonastheni*[tw] OR trachyphoni*[tw] OR functional voice disorder*[tw] OR psychogenic voice disorder*[tw] OR ventricular phonation[tw] OR conversion voice disorder*[tw] OR functional aphonia[tw] OR conversion aphonia[tw] OR conversion dysphonia[tw] OR phonation break[tw] OR functional falsetto[tw] OR mutational falsetto[tw] OR puberphonia[tw] OR juvenile voice[tw] OR laryngeal myasthenia[tw] #2 phonation disease*[tw] OR phonation disorder*[tw] #3 voice problem*[tw] OR voice symptom*[tw] OR voice complaints[tw] OR voice hygiene[tw] OR voice disturbance*[tw] OR voice tremor*[tw] OR voice impair*[tw] OR voice handicap*[tw] OR voice tension*[tw] OR voice strain*[tw] OR voice abuse*[tw] OR voice fatigue*[tw] OR voice misuse*[tw] OR voice reduct*[tw] OR vocal problem*[tw] OR vocal symptom*[tw] OR vocal complaints[tw] OR vocal hygiene[tw] OR vocal disturbance*[tw] OR vocal tremor*[tw] OR vocal impair*[tw] OR vocal handicap*[tw] OR vocal tension*[tw] OR vocal strain*[tw] OR vocal abuse*[tw] OR vocal fatigue*[tw] OR vocal misuse*[tw] OR vocal reduct*[tw] OR phonation problem*[tw] OR phonation symptom*[tw] OR phonation complaints[tw] OR phonation hygiene[tw] OR phonation disturbance*[tw] OR phonation tremor*[tw] OR phonation impair*[tw] OR phonation handicap*[tw] OR phonation tension*[tw] OR phonation strain*[tw] OR phonation abuse*[tw] OR phonation fatigue*[tw] OR phonation misuse*[tw] OR phonation reduct*[tw] #4 (effect* [tw] OR control [tw] OR controls* [tw] OR controla* [tw] OR controle* [tw] OR controli* [tw] OR controll* [tw] OR control'* OR evaluation* [tw] OR program* [tw]) NOT (animals [mh] NOT humans [mh]) #5 (randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized [tiab] OR placebo [tiab] OR drug therapy [sh] OR randomly [tiab] OR trial [tiab] OR groups [tiab]) NOT (animals[mh] NOT humans[mh]) #6 (#1 OR #2 OR #3) AND (#4 OR #5) #7 #6 AND Entrez Date from 2006/01/01 to 2010
Appendix 5. Updated search strategy for EMBASE (2010)
#1 ('dysphonia'/exp OR 'hoarseness'/exp OR 'vocal cord disorder'/exp OR phonastheni* OR trachyphoni* OR 'functional voice disorder' OR 'psychogenic voice disorder' OR 'ventricular phonation' OR 'conversion voice disorder' OR 'functional aphonia' OR 'conversion aphonia' OR 'conversion dysphonia' OR 'phonation break' OR 'functional falsetto' OR 'mutational falsetto' OR puberphonia OR 'juvenile voice' OR 'laryngeal myasthenia' OR (('phonation'/exp OR 'phonation') AND (disease* OR disorder*)) OR ((('voice'/exp OR 'voice') OR vocal OR ('phonation'/exp OR 'phonation')) AND (problem* OR symptom* OR complaints OR ('hygiene'/exp OR 'hygiene') OR disturbance* OR tremor* OR impair* OR handicap*OR tension* OR strain* OR abuse* OR fatigue*OR misuse* OR reduct*)) AND [article]/lim AND [humans]/lim) AND ([randomized controlled trial]/lim OR [controlled clinical trial]/lim OR random* OR factorial OR crossover OR 'cross over'OR 'cross‐over' OR ('placebo'/exp OR 'placebo') OR 'double blind' OR 'single blind' OR assign* OR allocat* OR volunteer* OR 'crossover‐procedure'/exp OR 'double‐blind procedure'/exp OR ('single‐blind procedure'/exp) OR ('comparative study'/exp OR 'comparative study') OR 'evaluation study' OR ('evaluation studies'/exp OR 'evaluation studies') OR ('follow‐up'/exp OR 'follow‐up') OR 'prospective study'/exp OR prospectiv*) AND [2006‐2010]/py #2 #1 AND [embase]/lim AND [2006‐2010]/py
Appendix 6. Updated search strategy for CENTRAL (2010)
#1 (dysphoni*):ti,ab,kw or (hoarseness):ti,ab,kw or (phonastheni* OR trachyphoni* OR functional voice disorder* OR psychogenic voice disorder* OR ventricular phonation OR conversion voice disorder* OR functional aphonia OR conversion aphonia OR conversion dysphonia OR phonation break OR functional falsetto OR mutational falsetto OR puberphonia OR juvenile voice OR laryngeal myasthenia), from 2006 to 2010 in Clinical Trials #2 (voice OR vocal OR phonation) NEAR (problem* OR symptom* OR complaints OR hygiene OR disorder* OR disease* OR disturbance* OR tremor* OR impair* OR handicap* OR tension* OR strain* OR abuse* OR fatigue* OR misuse* OR reduct*), from 2006 to 2010 in Clinical Trials #3 #1 OR #2
Appendix 7. Search strategy for CINAHL (2010)
#1 dysphoni* OR hoarseness OR phonastheni* OR trachyphoni* OR functional voice disorder* OR psychogenic voice disorder* OR ventricular phonation OR conversion voice disorder* OR functional aphonia OR conversion aphonia OR conversion dysphonia OR phonation break OR functional falsetto OR mutational falsetto OR puberphonia OR juvenile voice OR laryngeal myasthenia #2 Phonation AND (disease* OR disorder*) #3 (voice OR vocal OR phonation) AND (problem* OR symptom* OR complaints OR hygiene OR disturbance* OR tremor* OR impair* OR handicap* OR tension* OR strain* OR abuse* OR fatigue* OR misuse* OR reduct*) #4 #1 OR #2 OR #3 #5 (effect* OR control* OR evaluation* OR program*) #6 (random* OR placebo OR drug therapy OR trial OR groups) #7 (singl* OR doubl* OR trebl* OR tripl*) AND (mask* OR blind*) OR comparative study OR comparative studies OR evaluation study OR evaluation studies OR follow up OR follow‐up OR prospectiv* OR crossover OR cross over OR cross‐overOR factorial OR allocat* OR volunteer* #8 #5 OR #6 OR #7 #9 #4 AND #8
Appendix 8. Search strategy for PsycINFO through OvidSP (2010)
1. exp dysphonia/ 2. limit 1 to (human and yr="2006 ‐Current") 3. (dysphoni* or hoarseness or phonastheni* or trachyphoni* or functional voice disorder* or psychogenic voice disorder* or ventricular phonation or conversion voice disorder* or functional aphonia or conversion aphonia or conversion dysphonia or phonation break or functional falsetto or mutational falsetto or puberphonia or juvenile voice or laryngeal myasthenia).mp. [mp=title, abstract, heading word, table of contents, key concepts] 4. limit 3 to (all journals and human and yr="2006 ‐Current") 5. (Phonation adj6 (disease* or disorder*)).mp. [mp=title, abstract, heading word, table of contents, key concepts] 6. limit 5 to (all journals and human and yr="2006 ‐Current") 7. ((voice or vocal or phonation) adj6 (problem* or symptom* or complaints or hygiene or disturbance* or tremor* or impair* or handicap* or tension* or strain* or abuse* or fatigue* or misuse* or reduct*)).mp. [mp=title, abstract, heading word, table of contents, key concepts] 8. limit 7 to (all journals and human and yr="2006 ‐Current") 9. 8 or 6 or 4 or 2 10. (randomized controlled trial* or controlled clinical trial or random allocation or double‐blind method or single‐blind method or clinical trials or clinical trial or ((singl* or doubl* or trebl* or tripl*) and (mask* or blind*)) or latin square or placebo* or random* or research design or comparative study or evaluation studies or follow‐up studies or prospective studies or cross‐over studies or control* or prospectiv* or volunteer*).mp. [mp=title, abstract, heading word, table of contents, key concepts] 11. limit 10 to (all journals and human and yr="2006 ‐Current") 12. (effect* or control* or evaluation* or protect*).mp. [mp=title, abstract, heading word, table of contents, key concepts] 13. limit 12 to (all journals and human and yr="2006 ‐Current") 14. 11 or 13 15. 9 and 14 16. from 15 keep 1‐108
Appendix 9. Search strategy for OSH Update (all databases) (2010)
#1 GW{dysphoni* OR hoarseness OR phonastheni* OR trachyphoni* OR "functional voice disorder*" OR "psychogenic voice disorder*" OR "ventricular phonation" OR "conversion voice disorder*" OR "functional aphonia" OR "conversion aphonia" OR "conversion dysphonia" OR "phonation break" OR "functional falsetto" OR "mutational falsetto" OR puberphonia OR "juvenile voice" OR "laryngeal myasthenia"} #2 GW{Phonation AND (disease* OR disorder*)} #3 GW{(voice OR vocal OR phonation) AND (problem* OR symptom* OR complaints OR hygiene OR disturbance* OR tremor* OR impair* OR handicap* OR tension* OR strain* OR abuse* OR fatigue* OR misuse* OR reduct*)} #4 #1 OR #2 OR #3 #5 GW{(effect* OR control* OR evaluation* OR program*)} #6 GW{(random* OR placebo OR drug therapy OR trial OR groups)} #7 GW{(singl* OR doubl* OR trebl* OR tripl*) AND (mask* OR blind*) OR "comparative stud*" OR "evaluation stud*" OR "follow up" OR "follow‐up" OR prospectiv* OR crossover OR "cross over" OR "cross‐over" OR factorial OR allocat* OR volunteer*} #8 #5 OR #6 OR #7 #9 #4 AND #8 #10 PY{2006 OR 2007 OR 2008 OR 2009 OR 2010} #11 #9 AND #10
Data and analyses
Comparison 1. Direct voice training versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any voice handicap | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention | 3 | 110 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.27 [‐0.12, 0.66] |
| 1.2 Follow up | 1 | 24 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.38 [‐0.44, 1.20] |
| 2 Amount of vocal misuse behaviours | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Post‐intervention | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 64.73 [‐65.48, 194.94] |
| 2.2 Follow up | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 53.99 [‐73.58, 181.56] |
| 3 Normalised maximum phonation time (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Post‐intervention | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 3.32 [‐0.53, 7.17] |
| 3.2 Follow up | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 3.17 [0.24, 6.10] |
| 4 Maximum phonational frequency range | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Post‐intervention | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐4.59, 4.49] |
| 4.2 Follow up | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.03 [‐5.04, 2.98] |
1.1. Analysis.
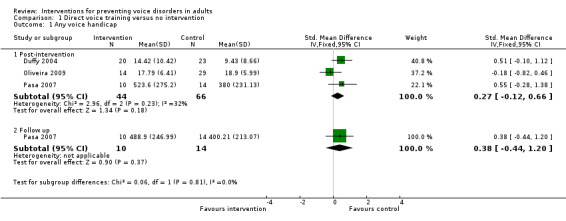
Comparison 1 Direct voice training versus no intervention, Outcome 1 Any voice handicap.
1.2. Analysis.
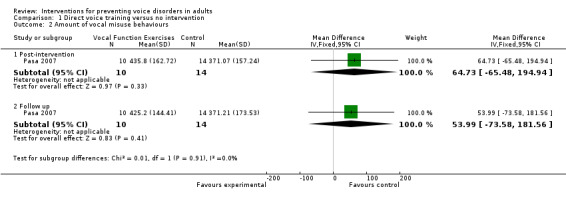
Comparison 1 Direct voice training versus no intervention, Outcome 2 Amount of vocal misuse behaviours.
1.3. Analysis.
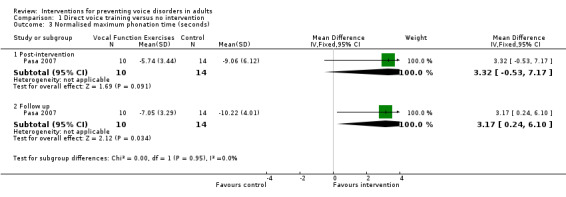
Comparison 1 Direct voice training versus no intervention, Outcome 3 Normalised maximum phonation time (seconds).
1.4. Analysis.
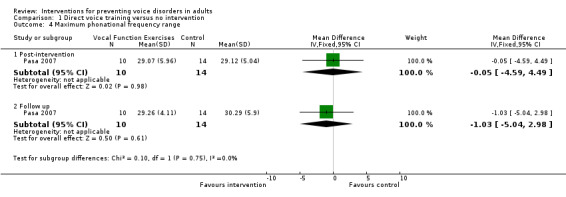
Comparison 1 Direct voice training versus no intervention, Outcome 4 Maximum phonational frequency range.
Comparison 2. Indirect voice training versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any voice handicap | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention | 2 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [‐0.03, 0.92] |
| 1.2 Follow up | 1 | 27 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.86, 0.65] |
| 2 Amount of vocal misuse behaviours | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Post‐intervention | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 59.24 [‐52.76, 171.24] |
| 2.2 Follow up | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 3.94 [‐115.66, 123.54] |
| 3 Normalised maximum phonation time (seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Post‐intervention | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 2.16 [‐1.67, 5.99] |
| 3.2 Follow up | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 2.86 [‐0.27, 5.99] |
| 4 Maximum phonational frequency range | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Post‐intervention | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [‐1.86, 5.86] |
| 4.2 Follow up | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 0.71 [‐3.72, 5.14] |
2.1. Analysis.
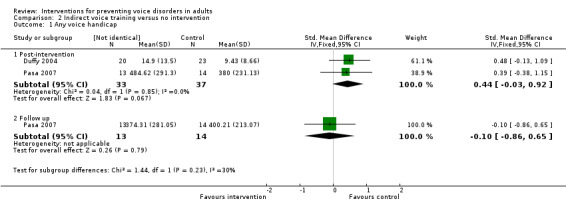
Comparison 2 Indirect voice training versus no intervention, Outcome 1 Any voice handicap.
2.2. Analysis.
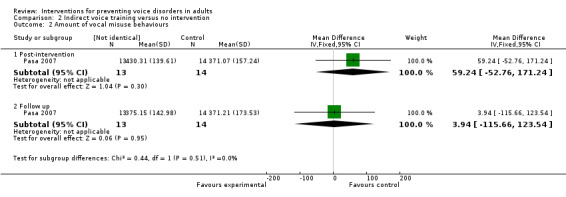
Comparison 2 Indirect voice training versus no intervention, Outcome 2 Amount of vocal misuse behaviours.
2.3. Analysis.
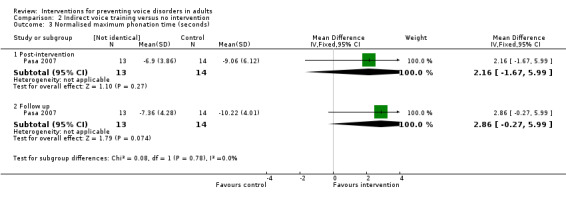
Comparison 2 Indirect voice training versus no intervention, Outcome 3 Normalised maximum phonation time (seconds).
2.4. Analysis.
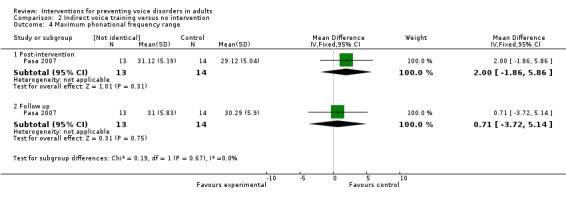
Comparison 2 Indirect voice training versus no intervention, Outcome 4 Maximum phonational frequency range.
Comparison 3. Direct and indirect voice training combined versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Voice Handicap Index | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐7.35 [‐15.07, 0.37] |
| 2 Maximum phonation time | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 3.18 [1.93, 4.43] |
3.1. Analysis.
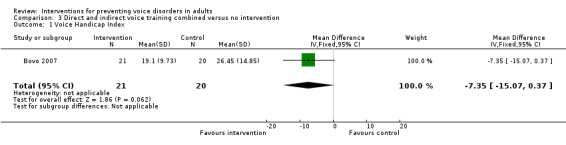
Comparison 3 Direct and indirect voice training combined versus no intervention, Outcome 1 Voice Handicap Index.
3.2. Analysis.
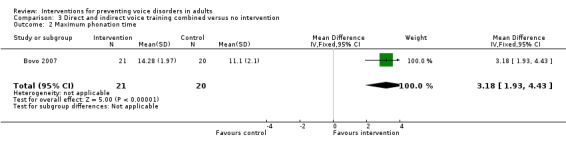
Comparison 3 Direct and indirect voice training combined versus no intervention, Outcome 2 Maximum phonation time.
Comparison 4. Direct and indirect voice training combined versus indirect voice training only.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective phonation difficulty | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 At end of semester after work day | 2 | 86 | Mean Difference (IV, Fixed, 95% CI) | ‐5.55 [‐23.75, 12.66] |
| 2 Subjective voice quality | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 At the end of semester after work day | 2 | 116 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐14.71, 14.93] |
| 3 Subjective throat tiredness | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 At the end of semester after work day | 2 | 116 | Mean Difference (IV, Fixed, 95% CI) | ‐0.93 [‐9.47, 7.61] |
| 4 Voice quality assessed by 3 vocologists | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 19.0 [‐41.53, 79.53] |
| 5 Firmness of phonation assessed by 3 vocologists | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 16.0 [‐38.32, 70.32] |
| 6 Average fundamental frequency (F0) whilst reading at habitual loudness | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 3.0 [‐5.38, 11.38] |
| 7 Sound pressure level (dB) whilst reading at habitual loudness | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐2.67, 0.67] |
| 8 Alpha ratio (dB) whilst reading in habitual loudness | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.86, 1.46] |
| 9 Jitter (%) | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.40, 0.15] |
| 10 Shimmer (dB) | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.34, ‐0.05] |
4.1. Analysis.
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 1 Subjective phonation difficulty.
4.2. Analysis.
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 2 Subjective voice quality.
4.3. Analysis.
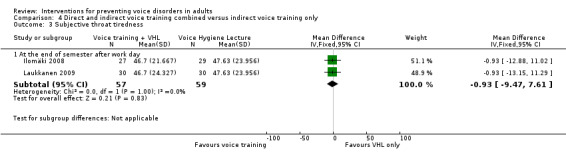
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 3 Subjective throat tiredness.
4.4. Analysis.
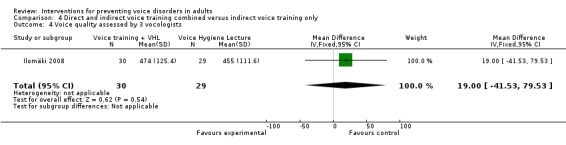
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 4 Voice quality assessed by 3 vocologists.
4.5. Analysis.
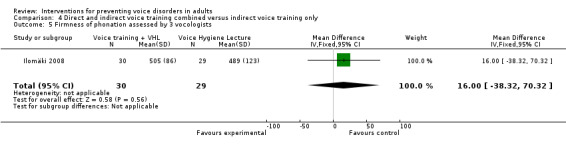
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 5 Firmness of phonation assessed by 3 vocologists.
4.6. Analysis.
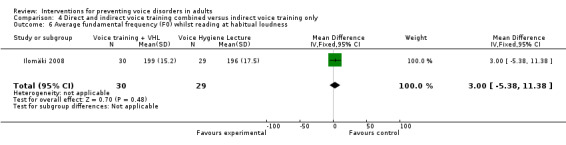
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 6 Average fundamental frequency (F0) whilst reading at habitual loudness.
4.7. Analysis.
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 7 Sound pressure level (dB) whilst reading at habitual loudness.
4.8. Analysis.
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 8 Alpha ratio (dB) whilst reading in habitual loudness.
4.9. Analysis.
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 9 Jitter (%).
4.10. Analysis.
Comparison 4 Direct and indirect voice training combined versus indirect voice training only, Outcome 10 Shimmer (dB).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bovo 2007.
| Methods | RCT | |
| Participants | 41 female kindergarten and primary school teachers in Italy Age: treatment group mean 39.38 (SD 9.0); control group mean 38.50 (SD 8.5) Both groups were matched for age, working years, hoarseness grade, and vocal demand | |
| Interventions | 1) Direct and indirect voice training (21)
The intervention consisted of a course, an educational pamphlet and exercises to be conducted at home. The course had a duration of 12 hours and consisted of 2 theoretical lectures each 90 minutes long and 2 sessions of group voice therapy each of 120 minutes. The lectures were conducted by two MD phoniatricians (the first 2 authors) and covered the following topics: anatomy and physiology of phonation, the causes and predisposing factors of vocal pathology, the warning symptoms of vocal fatigue, voice ergonomics (i.e. vocal hygiene, strategies to reduce vocal demand in the classroom, and changing behaviour in daily life to reduce vocal abuse), classroom acoustics and amplification systems. The practical session consisted of group voice therapy held by 4 speech‐language pathologists (SLP) with at least 15 years experience. During the voice therapy sessions, the participants were divided into groups of 20. The same techniques, as given below, were used by all SLPs and selected according to familiarity: (1) training of efficient respiratory behaviour through utilisation of low abdominal‐diaphragmatic breathing; (2) training of laryngeal muscle relaxation using Jacobson‐based whole‐body relaxation techniques; (3) manual circumlaryngeal therapy; (4) relaxed voicing with elimination of hard glottal attacks, chewing voicing, yawn‐sigh, chant talk and pitch inflections; (5) proper oral‐nasal resonance (Lessac‐based resonance therapy); and (6) exercises for developing greater oral opening. 2) No intervention (20) |
|
| Outcomes | 1) Voice Handicap Index 2) Videolaryngostroboscopy, Fo, jitter, shimmer, noise‐to‐harmonic ratio, maximum phonation time | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "On entry into the study, all 64 teachers gave consent for inclusion: 32 were randomized to the treatment group (ages 23–57, mean 39.38, SD 9.0) and 32 (ages 24–54, mean 38.50, SD 8.5) to no treatment. Both groups were matched for age, working years, hoarseness grade, and vocal demand." (p.4) No further details reported about the method of randomisation. |
| Allocation concealment? | Unclear risk | No details reported regarding whether allocation was concealed or not |
| Blinding? All outcomes | Low risk | "A blinded perceptive voice evaluation with global grade of dysphonia score ('GRBAS' scale) was made separately by the first two authors." (p. 7) |
| Incomplete outcome data addressed? All outcomes | High risk | The authors report that: "With regard to the drop out rate, the number of subjects who failed to attend the second clinical‐instrumental evaluation is indeed significant." (p. 15) The study suffered a total loss of 36% of the initial sample. No action was taken by the authors to address this in the results. |
| Free of selective reporting? | Unclear risk | The authors state that: "Mainly the data were analyzed with a repeated‐measures general linear model and an ordinal generalized linear model for multinomial data." (p. 8) However, they do not justify the need for such complicated analysis. |
Duffy 2004.
| Methods | RCT | |
| Participants | 55 teacher students in the UK The subjects' ages ranged from 21 to 39 years with an average age of 24.25 years. The subjects had no known hearing defects, and they self‐reported no voice or speech problems and had not attended training programmes for singing, voice care or stress management in the past. | |
| Interventions | 1) Indirect voice training (20)
Indirect training provided information on the mechanics of normal voice production, the amount and type of voice use, vocal behaviours thought to be phonotraumatic, hydration issues, and lifestyle and diet factors that can support or interfere with a healthy voice 2) Direct and indirect voice training (12) The second type, direct training, provided one of the groups with training to encourage healthy vocal behavior, modifying any inappropriate techniques or compensatory behaviours. More specifically, direct training focused on posture, respiration, release of tension in the vocal apparatus, resonance, and voice projection 3) No intervention (23) |
|
| Outcomes | 1) Voice Handicap Index, Vocology Screening Profile 2) Dysphonia Severity Index (Fo‐high, I‐low, maximum phonation time, jitter) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "The 55 subjects were randomly divided into three groups: 23 were in the control group, 20 in the indirect group, and 12 in the direct group." (p. 65). No further details reported about the method of randomisation. The authors do however state in the results that: "No significant differences between groups were found at the 0.05 level on any of the preintervention measures. Therefore, the randomization process is validated." (p. 67) |
| Allocation concealment? | Unclear risk | No details reported regarding whether allocation was concealed or not |
| Blinding? All outcomes | High risk | This study used self‐reported outcomes and instrumentally assessed outcomes and therefore blinding is not an issue |
| Incomplete outcome data addressed? All outcomes | High risk | "The training provided to the direct group required the most time, and due to this, there was a drop‐out rate. This resulted in unequal numbers and a smaller, direct group by comparison." (p. 68) The authors do not report any details on the drop‐outs or adjust for them in their results. |
| Free of selective reporting? | High risk | In the article the authors report the results only as means per groups in figures and as the results of ANOVAs. The authors however provided their raw data on request. |
Ilomäki 2008.
| Methods | RCT | |
| Participants | 59 female primary school teachers in Finland Mean age: 41.5 in the VHL group (control) and 42.2 in the VT group (intervention) Experience in years, mean: 15.8 in the VHL group (control) and 15.6 in the VT group (intervention) Vocal demands, mean: 23 teaching hours per week in the VHL group (control) and 24 hours in the VT group (intervention) Total hours taught during the autumn term: 420 in the VHL group and 439 in the VT group Class size: mean of 19 pupils in the VHL group and 20 in the VT group Differences between groups were non‐significant | |
| Interventions | 1) Indirect voice training (voice hygiene lecture only) (29)
After the first pre‐intervention recordings, all teachers attended a theoretical voice hygiene lecture lasting 3 hours. The course objectives of the lecture were to gain knowledge and awareness of the basics of voice and speech production, the main factors causing vocal loading in teachers, methods available to avoid overloading, and basics of economic versus non‐economic voice use 2) Direct and indirect voice training (voice training and voice hygiene lecture) (30) This group exercised their voices in 5 voice training lessons (each lesson 1 hour plus individualised homework) during 9 weeks. The course objectives of the voice training course were to gain ease and endurance in voice production, and getting rid of any poor vocal habits. The learning methods were introspections, discussions, voice exercises and individualised homework with a view to finding economic voice production, i.e. avoidance of excessive muscle tension of the larynx, deep breathing technique, firmness of phonation without effort, well‐resonating voice quality to improve audibility, and adequate individual pitch and loudness range and variation. |
|
| Outcomes | 1) Phonation difficulty, voice quality, throat tiredness 2) Voice quality, firmness of phonation, fundamental frequency (F0), sound pressure level, alpha ratio (the ratio between the spectral energy below and above 1000 Hz), jitter, shimmer | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "All 60 teachers attended a voice hygiene lecture at the beginning of term; 30 of them were randomly assigned to a voice training group" (p. 85). No further details reported about the method of randomisation. |
| Allocation concealment? | Unclear risk | No details reported regarding whether allocation was concealed or not |
| Blinding? All outcomes | Unclear risk | "Three experienced voice trainers evaluated the text samples for voice quality and firmness of phonation..." (p. 86). The authors do not report if the evaluators were blinded to the experimental conditions to which the participants had been assigned. |
| Incomplete outcome data addressed? All outcomes | High risk | "One of the teachers in the VHL group was excluded from the study at the end of the term because of incomplete recordings" (p. 85). However, in the raw data provided by the authors, three participants had dropped out of the experimental group and the control group somehow remained the same. |
| Free of selective reporting? | Low risk | The authors report results for each of the outcomes listed in the Methods section |
Laukkanen 2009.
| Methods | RCT | |
| Participants | 89 female primary school teachers, of whom 59 are the same as in Ilomäki 2008 Mean age: 41.1 (SD 8.5) Experience in years, mean: 15.3 (SD 8.8) Mean teaching hours per week: 24.3 (SD 4.4) | |
| Interventions | 1) Direct and indirect training (voice training and voice hygiene lecture) (30)
Same as in Ilomäki 2008 2) Direct and indirect training (Voice Massage(TM) and voice hygiene lecture) (30) Voice Massage(TM) is a Finnish method developed by massage therapist Leena Koskinen. It consists of manipulation of voice and speech production muscles of the larynx, respiration and articulation. It also includes some vocal and respiratory exercises during manipulation. 3) Indirect voice training (voice hygiene lecture only) (29) Same as in Ilomäki 2008 |
|
| Outcomes | 1) Phonation difficulty, voice quality, throat tiredness 2) Voice quality, firmness of phonation, fundamental frequency (F0), sound pressure level, alpha ratio (the ratio between the spectral energy below and above 1000 Hz), jitter, shimmer | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "In addition to the lecture, a randomly chosen group of 30 subjects received Voice Massage treatment (VM group) and another group of 30 subjects received Voice Training (VT group)" (p.58) |
| Allocation concealment? | Unclear risk | No details reported regarding whether allocation was concealed or not |
| Blinding? All outcomes | Unclear risk | "...perceptual voice analysis performed by three experienced speech trainers from 1‐min text reading samples recorded after the working day" (p. 60). The authors do not report if the evaluators were blinded to the experimental conditions to which the participants had been assigned. |
| Incomplete outcome data addressed? All outcomes | High risk | Group Ns reported in the article are 3 x 30 but the raw data provided by the authors indicated that there had been drop‐outs. Ns in the raw data were 30 and 27 for the intervention groups and 30 for the control group although in the Ilomäki 2008 study that reported on the same participants stated that one participant had been lost from the control group. |
| Free of selective reporting? | High risk | In the article, the authors do not report numerical results for their primary self‐reported outcomes. The authors however provided these on request. |
Oliveira 2009.
| Methods | RCT | |
| Participants | 43 telemarketers in Brazil Age: 18 to 55 Sex: intervention group 64% and control group 83% female | |
| Interventions | 1) Direct voice training (14)
The intervention group received an 8‐week training programme, including vocal warming‐up and cool‐down, as well as tasks to expand the psychodynamic aspects of voice production. In order to promote vocal warm‐up, facilitating sounds, body movement techniques with sound production, overarticulation exercises, semi‐occluded vocal tract exercises (hand‐over‐mouth technique) and chant talk exercises were used in 8 30‐minute modules offered weekly. The facilitating sounds included humming sounds associated with chewing movements, fricatives and voice sounds associated with ascending musical scales (from C3 to C4) in staccato and legato. For cool‐down, voice sounds were also used, with descending musical scales (from G3 to C3), as well as the yawn‐sigh technique and laryngeal manipulation. 2) No intervention (29) |
|
| Outcomes | 1) Vocal attrition symptoms, voice symptom score | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "A total of 100 telemarketers (83.3%) attended the lecture, of whom 92 (76.6%) consented to participate in the current study. Subjects were then randomly assigned to an intervention group (n = 44) and a control group (n = 48)" (p. 77) |
| Allocation concealment? | Unclear risk | No details reported regarding whether allocation was concealed or not |
| Blinding? All outcomes | High risk | This study used self‐reported outcomes only and therefore blinding is not an issue |
| Incomplete outcome data addressed? All outcomes | High risk | "Of the 44 telemarketers in the intervention group, 4 changed positions, were unavailable, 10 had over 25% absence and 12 did not show up. The intervention group was, therefore, comprised of 14 telemarketers. Of the 48 telemarketers in the control group, 39 attended the evaluations and 29 the re‐evaluations; this meant a loss of 19 telemarketers". (p. 78‐9). In other words, the intervention and control groups suffered losses of 68% and 40% respectively. No action was taken by the authors to address this in the results. |
| Free of selective reporting? | High risk | The authors reported the results the self‐reported outcome for males and females separately. This was not justified in advance. |
Pasa 2007.
| Methods | RCT | |
| Participants | 37 primary school teachers in Australia Mean age: 37 (SD 9.98) Sex: direct voice training group: 83%, indirect voice training group: 100% and control group: 93% female Teaching experience: 13.59 (SD 9.32) Mean number of teaching per day: 5.54 (SD 0.69) | |
| Interventions | 1) Direct voice training (10)
The exercises taught to the participants in this study were a modified version of Stemple's VFE. The VFE training the teachers received consisted of 4 exercises (warm‐up, stretching, contracting, and adductory strengthening exercises to be practiced at home, twice each, twice per day, preferably morning and evening, for a 6‐week period. The training session began with a brief discussion about the impact and prevalence of voice problems in teachers, and information about how the normal voice works. The participants in VFE group were then instructed how to perform VFE and how often the exercises need to be performed. The participants were encouraged to produce all the vocal exercises softly, with a frontal focus. The researchers demonstrated to the participants how the exercises were to be performed, instructed the them to produce the exercises themselves as a group, and finally divided the large group into smaller groups (2 or 3 people per group) to practice the exercises. Four student clinicians who were trained to perform VFE by the researchers directed each smaller group. 2) Indirect voice training (13) The vocal hygiene (VH) programme was adapted from the VH programme used by Roy et al. The aim of the VH training was to introduce healthy vocal behaviours into the participants' daily interactions, particularly in the school environment. The topics covered in the VH session were the prevalence and impact of voice problems in teachers, basic anatomy and physiology of voice production, symptoms of voice disorders, strategies to reduce harmful vocal behaviours, managing and minimising health factors that contribute to the development and maintenance of voice problems, and changes to the speaking environment that increase vocal efficiency and reduce vocal harm. 3) No intervention (14) |
|
| Outcomes | 1) Voice symptoms, vocal misuse behaviours 2) Maximum phonation time, maximum phonational frequency range | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | "The researchers decided a priori through random allocation that the teachers from the first school that agreed to participate would be allocated to the VH group. If less than 13 teachers decided to participate from this school (the required sample size for each group as determined through power analysis), then the teachers from the second school that volunteered to participate would also be allocated to the VH group. The next group to which a school (or schools) would be allocated was the VFE group, and the final group to which a school (or schools) would be allocated was the control group." (p. 130) |
| Allocation concealment? | Unclear risk | No details reported regarding whether allocation was concealed or not |
| Blinding? All outcomes | High risk | This study used self‐reported outcomes and instrumentally assessed outcomes and therefore blinding is not an issue |
| Incomplete outcome data addressed? All outcomes | High risk | "...at the commencement of the study there were 13 female participants in the VH group, 12 in the VFE group (10 females, 2 males), and 14 in the control group (13 females, 1 male). Two teachers from the VFE group completed the initial assessment but were unable to continue participating in the study... The number of participants in the VFE group was therefore reduced to 10." (p. 130). The authors do not report any details on the 8 individuals who volunteered to participate but could not or the 2 participants who dropped out after baseline measurements. The study suffered a total loss of 21% of the initial sample. |
| Free of selective reporting? | Low risk | The authors report the results for all the outcomes measured |
RCT = randomised controlled trial SD = standard deviation SLP = speech‐language pathologists VFE = vocal function exercises VH = vocal hygiene VHL = vocal hygiene lecture VT = voice training
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amir 2005 | STUDY DESIGN: No control group |
| Andersson 1998 | STUDY DESIGN: No control group |
| Andrews 1986 | STUDY DESIGN: No control group |
| Barrichelo 2007 | STUDY DESIGN: No control group |
| Barrichelo‐Lindstrom 2009 | STUDY DESIGN: No control group |
| Bassiouny 1998 | ALLOCATION:
Randomised PARTICIPANTS: All participants presented with a variety of vocal pathologies |
| Behrman 2008 | ALLOCATION:
Randomised PARTICIPANTS: All participants had benign vocal fold lesions |
| Bengisu 2008 | ALLOCATION:
Not randomised PARTICIPANTS: All intervention group participants had muscle tension dysphonia |
| Beranova 2003 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Berg 2008 | STUDY DESIGN: Retrospective case‐control study |
| Birkent 2004 | ALLOCATION: Not randomised but based on type of functional voice disorder PARTICIPANTS: Included participants with mutational falsetto (n = 16), vocal nodules (n = 17), and muscle‐tension dysphonia (n = 4) |
| Boominathan 2008 | STUDY DESIGN: No control group |
| Bouwers 2009 | STUDY DESIGN: Retrospective case‐control study |
| Broaddus‐Lawrence 2000 | STUDY DESIGN: No control group |
| Carding 1992 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Carding 1998 | ALLOCATION:
Randomised PARTICIPANTS: Included patients are in part the same individuals as in Carding 1999 |
| Carding 1999 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Chan 1994 | ALLOCATION:
Not randomised PARTICIPANTS: Kindergarten teachers INTERVENTIONS: Direct and indirect voice training OUTCOMES: No self‐reported outcome. Relative average perturbation, ratio of energy below 1 kHz to energy above 1 kHz, duty cycle |
| Chen 2007 | STUDY DESIGN: No control group |
| Dagli 2008 | STUDY DESIGN: No control group |
| Daniilidou 2007 | STUDY DESIGN: Consecutive cohort study |
| de Jong 2006 | STUDY DESIGN: No intervention |
| Demmink‐Geertman 2008 | STUDY DESIGN: Case‐control study |
| Fex 1994 | STUDY DESIGN: No control group |
| Fischer 2009 | ALLOCATION: Not randomised. Control group consisted of healthy volunteers |
| Fulljames 2006 | ALLOCATION: Not randomised but based on clinical need |
| Gamberini 2007 | STUDY DESIGN: Participants served as their own controls |
| Garcia Real 2002 | ALLOCATION:
Not randomised PARTICIPANTS: Professional voice users with a minimum of 4 hours of daily voice use and who had had in the past symptoms or signs of vocal damage due to voice use for a minimum of 6 months |
| Gibson 2009 | ALLOCATION:
Randomised PARTICIPANTS: "The study participants were adults with chronic cough (>2 months) that had persisted despite medical treatment according to the anatomic diagnostic protocol, including treatment for asthma, postnasal drip syndrome, gastro‐esophageal reflux and withdrawal of angiotensin‐converting enzyme inhibitors (if used). The severity of the cough was sufficient to seek medical attention from both a general practitioner and respiratory physician." (p.160) INTERVENTIONS: Education, vocal hygiene training, cough suppression strategies and psycho‐educational counselling OUTCOME: No self‐reported outcome. "Vocal function was assessed using a range of measures, including auditory perceptual voice analysis, acoustic analysis, and electroglottographic analysis." (p. 161). |
| Gillivan‐Murphy 2006 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Gorman 2008 | STUDY DESIGN: No control group |
| Guirro 2008 | STUDY DESIGN: No control group |
| Hackworth 2007 | ALLOCATION: Not randomised |
| Hakkesteegt 2010 | STUDY DESIGN: Clinical follow‐up study |
| Holbrook 1974 | STUDY DESIGN: No control group |
| Holmberg 2007 | STUDY DESIGN: No control group |
| John 2005 | STUDY DESIGN: No control group |
| Jones 2006 | STUDY DESIGN: No intervention |
| Jonsdottir 2001 | STUDY DESIGN: No control group |
| Jonsdottir 2002 | STUDY DESIGN: No control group |
| Ketelslagers 2007 | STUDY DESIGN: No intervention |
| Kirveskari 1988 | ALLOCATION:
Randomised PARTICIPANTS: Patients who had sought treatment for voice disorders INTERVENTION: Treatment for craniomandibular disorder (CMD) by elimination of occlusal and articular interferences, i.e. by adjustment of the teeth. "The occlusal adjustment consisted of elimination of the slide in centric (i.e., the retruded contact position was made stable) and of the removal balancing, working, and protrusive interferences. Removable dentures were adjusted according to the same principles. In two cases, new dentures were made. Placebo adjustment of the occlusion consisted of polishing occlusal surfaces with special attention to maintaining the occlusal contact relationships." (p. 328) OUTCOME: No self‐reported outcome. "The evaluation of the effects of treatment were made after two months by the phoniatrician and the dentists independently. Laryngeal status, voice status, and the subjective symptoms of CMD were evaluated by the phoniatrician, who was unaware of which group the subject belonged to." (p. 328). |
| Kizilay 2008 | STUDY DESIGN: No control group |
| Kotby 1991 | STUDY DESIGN: No control group |
| Laukkanen 2005 | STUDY DESIGN: No control group |
| Lehto 2003 | STUDY DESIGN: No control group |
| Lehto 2005 | STUDY DESIGN: No control group |
| MacKenzie 2001 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Malki 2008 | STUDY DESIGN: Case study |
| Mathieson 2009 | STUDY DESIGN: No control group |
| McCabe 2002 | STUDY DESIGN: No control group |
| Mendoza‐Lara 1990 | ALLOCATION:
Not randomised PARTICIPANTS: Intervention group participants had dysphonia |
| Milbrath 2003 | STUDY DESIGN: No control group |
| Morsomme 2010 | STUDY DESIGN: No control group |
| Motel 2003 | STUDY DESIGN: No control group |
| Nguyen 2009 | ALLOCATION:
Randomised PARTICIPANTS: All participants had an otolaryngologist's diagnosis of muscle tension dysphonia |
| Niebudek‐Bogusz 2007 | ALLOCATION:
Not randomised PARTICIPANTS: All participants had dysphonia |
| Niebudek‐Bogusz 2008 | ALLOCATION:
Not randomised PARTICIPANTS: All participants had dysphonia |
| Niebudek‐Bogusz 2008a | ALLOCATION:
Not randomised PARTICIPANTS: All participants had dysphonia |
| Oliveira 2005 | ALLOCATION:
Randomised PARTICIPANTS: Working telemarketers INTERVENTIONS: Vocal function exercises OUTCOME: No self‐reported outcome. "Deste modo, a efetividade do programa foi avaliada pela comparação de medidas acústicas e perceptivo‐auditivas pré e pós‐treinamento. A avaliação perceptivo‐auditiva foi realizada com a análise da qualidade vocal como un todo. Na avaliação acústica foram comparadas as medidas da F0, jitter, shimmer e os gráficos do diagrama do desvio fonatório." (p. 24) |
| Pedersen 2004 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Popovici 1993 | ALLOCATION:
Not randomised PARTICIPANTS: All participants had dysphonia |
| Portone 2008 | STUDY DESIGN: No intervention |
| Prosek 1978 | STUDY DESIGN: No control group |
| Rattenbury 2004 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Roy 1993 | STUDY DESIGN: No control group |
| Roy 1997 | STUDY DESIGN: No control group |
| Roy 2001 | ALLOCATION:
Randomised PARTICIPANTS: Included patients with self‐reported voice problems |
| Roy 2002 | ALLOCATION:
Randomised PARTICIPANTS: Included patients with self‐reported voice problems |
| Roy 2003 | ALLOCATION:
Randomised PARTICIPANTS: Included patients with self‐reported voice problems |
| Schaeffer 2007 | STUDY DESIGN: No control group |
| Seifert 2006 | STUDY DESIGN: No intervention |
| Sellars 2002 | STUDY DESIGN: Characterisation of the contents of voice therapy |
| Silverio 2008 | STUDY DESIGN: No control group |
| Simberg 2006 | ALLOCATION:
Randomised PARTICIPANTS: All participants had dysphonia |
| Simoes‐Zenari 2008 | STUDY DESIGN: No control group |
| Sinkiewicz 2006 | STUDY DESIGN: No control group |
| Sliwinska‐Kowalska 2002 | STUDY DESIGN: No control group |
| Sliwinska‐Kowalska 2003 | ALLOCATION:
Not randomised PARTICIPANTS: All participants had dysphonia including hyperfunctional dysphonia, insufficiency of glottis and vocal noduli |
| Sliwinska‐Kowalska 2006 | STUDY DESIGN: No intervention |
| Sulkowski 2005 | STUDY DESIGN: No intervention |
| Syed 2009 | STUDY DESIGN: No intervention |
| Timmermans 2004a | ALLOCATION:
Not randomised PARTICIPANTS: Students of a school for audiovisual communication INTERVENTIONS: Direct and indirect voice training OUTCOMES: Voice Handicap Index, GRBAS, videolaryngostroboscopy, maximum phonation time, jitter, I‐low, Fo‐high, Dysphonia Severity Index |
| Timmermans 2004b | ALLOCATION:
Not randomised PARTICIPANTS: Students of a school for audiovisual communication INTERVENTIONS: Direct and indirect voice training OUTCOMES: Voice Handicap Index, GRBAS, videolaryngostroboscopy, maximum phonation time, jitter, I‐low, Fo‐high, Dysphonia Severity Index |
| Timmermans 2005 | STUDY DESIGN: No control group |
| Van Lierde (in press) | STUDY DESIGN: No control group |
| Vertigan 2008 | ALLOCATION:
Randomised PARTICIPANTS: Persons with chronic cough that had persisted despite medical treatment INTERVENTIONS: SPEech Pathology Intervention Program for CHronic Cough (SPEICH‐C). "The SPEICH‐C involved four components including education about the nature of cough, strategies to control the cough, psychoeducational counseling, and vocal hygiene education to reduce laryngeal irritation" (p. 583) OUTCOME: No self‐reported outcome. Perceptual voice analysis: "Two experienced speech pathologists not connected to the study or to the assessment or treatment of the participants, served as listeners and conducted ratings on the speech samples. Listeners were blinded to the participant’s treatment allocation and whether the recording represented a pre‐ or postintervention condition." (p. 582) Acoustic and electroglottographic analysis: "Acoustic measures included maximum phonation time (MPT) measured in seconds, standard deviation of fundamental frequency (SDF0) measured in Hertz (Hz), jitter measured in percentage (%), and harmonic‐to‐noise ratio (HNR) measured in decibels (dB). The steady state vowel portion as judged by the fundamental frequency trace with a minimum of 3 seconds was chosen for each vowel. The average value of each measure across the three samples was calculated for every participant. A further measure, phonation range (PR) was calculated using a scale task whereby participants phonated an ascending scale on the phoneme /i/. Electroglottographic analysis was conducted on a 2‐minute sample of connected speech during a reading task. The data analyzed from this sample included fundamental frequency (Hz) in connected speech (DFx) and duration of the closed phase (%) in each cycle of vocal fold vibration (Qx)." (p. 582‐3) |
| Voerman 2009 | STUDY DESIGN: No intervention |
| Wingate 2007 | ALLOCATION:
Not randomised PARTICIPANTS: Half had complaints of throat pain or vocal fatigue and half were found to have benign vocal fold lesions |
| Yiu 2006 | ALLOCATION:
Randomised PARTICIPANTS: The majority of included patients had organic dysphonia |
| Zhao 2005 | ALLOCATION:
Not randomised PARTICIPANTS: Intervention group participants had mutational falsettos |
Characteristics of studies awaiting assessment [ordered by study ID]
Leppänen 2009.
| Methods | Randomised controlled trial |
| Participants | 60 female teachers in Finland |
| Interventions | 1) Direct and indirect voice training: Voice Hygiene Lecture and Voice Massage (TM) 2) Indirect voice training: Voice Hygiene Lecture only |
| Outcomes | 1) No subjective outcomes 2) Perceptual evaluation by 3 speech trainers, fundamental frequency (F0), equivalent sound level (Leq), alpha‐ratio, jitter and shimmer |
| Notes | It is unclear if the sample used in this study overlaps with that used in Ilomäki 2008 and/or Laukkanen 2009 |
Stemple 1994.
| Methods | Randomised controlled trial |
| Participants | 35 female adult graduate students in the USA |
| Interventions | 1) Direct voice training: sustaining musical notes and gliding from lowest to highest note and from highest to lowest in participant's frequency range 2) Placebo training: reading a short passage at comfortable pitch and chanting a series of sentences 3) No intervention |
| Outcomes | 1) No subjective outcomes 2) Fundamental frequency (F0), jitter, frequency range, phonation volume, flow rate, maximum phonation time, videolaryngostroboscopy |
| Notes | — |
Differences between protocol and review
This first update of this review differs in many ways from the original review. The systematic search was conducted in more databases. The studies' risk of bias was assessed more broadly than with just a brief mention of whether allocation was concealed or not. We also extracted more data from the new as well as the existing two studies.
Contributions of authors
Jani Ruotsalainen conceptualised the review jointly with JV and took the lead in writing the review and in managing the team of authors. He performed study selection and data extraction and performed the analyses. Jos Verbeek conceptualised the review jointly with JR, wrote the methods section of the protocol and commented extensively on all versions of the review. Leena Isotalo designed and conducted the updated systematic search strategies with additional help from Gemma Sandberg. Jaana Sellman and Laura Lehto performed study selection and data extraction and commented extensively on all versions of the review.
Sources of support
Internal sources
Finnish Institute of Occupational Health, Finland.
Ministry of Social Affairs and Health, Finland.
Cochrane Occupational Health Field, Finland.
External sources
Pension Fund Loyalis, Netherlands.
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bovo 2007 {published data only}
- Bovo R, Galceran M, Petruccelli J, Hatzopoulos S. Vocal problems among teachers: evaluation of a preventive voice program. Journal of Voice 2007;21(6):705‐22. [DOI] [PubMed] [Google Scholar]
Duffy 2004 {published data only}
- Duffy OM, Hazlett DE. The impact of preventive voice care programs for training teachers: a longitudinal study. Journal of Voice 2004;18(1):63‐70. [DOI] [PubMed] [Google Scholar]
Ilomäki 2008 {published data only}
- Ilomäki I, Laukkanen AM, Leppänen K, Vilkman E. Effects of voice training and voice hygiene education on acoustic and perceptual speech parameters and self‐reported vocal well‐being in female teachers. Logopedics, Phoniatrics, Vocology 2008;33(2):83‐92. [DOI] [PubMed] [Google Scholar]
Laukkanen 2009 {published data only}
- Laukkanen AM, Leppänen K, Ilomäki I. Self‐evaluation of voice as a treatment outcome measure. Folia Phoniatrica et Logopedica 2009;61(1):57‐65. [DOI] [PubMed] [Google Scholar]
Oliveira 2009 {published data only}
- Oliveira AGA, Behlau M, Gouveia N. Vocal symptoms in telemarketers: a random and controlled field trial. Folia Phoniatrica et Logopedica 2009;61(2):76‐82. [DOI] [PubMed] [Google Scholar]
Pasa 2007 {published data only}
- Pasa G, Oates J, Dacakis G. The relative effectiveness of vocal hygiene training and vocal function exercises in preventing voice disorders in primary school teachers. Logopedics, Phoniatrics, Vocology 2007;32(3):128‐40. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Amir 2005 {published data only}
- Amir O, Dukas M, Shnaps‐Baum R. The effect of a 'voice course' on the voices of people with and without pathologies: preliminary observations. Logopedics, Phoniatrics, Vocology 2005;30(2):63‐71. [DOI] [PubMed] [Google Scholar]
Andersson 1998 {published data only}
- Andersson K, Schalen L. Etiology and treatment of psychogenic voice disorder: results of a follow‐up study of thirty patients. Journal of Voice 1998;12(1):96‐106. [DOI] [PubMed] [Google Scholar]
Andrews 1986 {published data only}
- Andrews S, Warner J, Stewart R. EMG biofeedback and relaxation in the treatment of hyperfunctional dysphonia. British Journal of Disorders of Communication 1986;21(3):353‐69. [DOI] [PubMed] [Google Scholar]
Barrichelo 2007 {published data only}
- Barrichelo VMO, Behlau M. Perceptual identification and acoustic measures of the resonant voice based on "Lessac's Y‐Buzz" ‐ a preliminary study with actors. Journal of Voice 2007;21(1):46‐53. [DOI] [PubMed] [Google Scholar]
Barrichelo‐Lindstrom 2009 {published data only}
- Barrichelo‐Lindstrom V, Behlau M. Resonant Voice in Acting Students: Perceptual and Acoustic Correlates of the Trained Y‐Buzz by Lessac. Journal of Voice 2009;23(5):603‐609. [DOI] [PubMed] [Google Scholar]
Bassiouny 1998 {published data only}
- Bassiouny S. Efficacy of the accent method of voice therapy. Folia Phoniatrica et Logopedica 1998;50:146‐64. [DOI] [PubMed] [Google Scholar]
Behrman 2008 {published data only}
- Behrman A, Rutledge J, Hembree A, Sheridan S. Vocal hygiene education, voice production therapy, and the role of patient adherence: a treatment effectiveness study in women with phonotrauma. Journal of Speech, Language and Hearing Research 2008;51(2):350‐66. [DOI] [PubMed] [Google Scholar]
Bengisu 2008 {published data only}
- Bengisu S, Topbas S, Kocak I. The relationship between muscle tension dysphonia type 1 and soft phonation index and the effectiveness of voice therapy. Kulak Burun Bogaz Ihtisas Dergisi 2008;18(3):131‐8. [PubMed] [Google Scholar]
Beranova 2003 {published data only}
- Beranova A, Betka J. New opportunities in the treatment of dysphonia. Otorinolaryngologie a Foniatrie 2003;52:75‐9. [Google Scholar]
Berg 2008 {published data only}
- Berg EE, Hapner E, Klein A, Johns MM 3rd. Voice therapy improves quality of life in age‐related dysphonia: a case‐control study. Journal of Voice 2008;22(1):70‐4. [DOI] [PubMed] [Google Scholar]
Birkent 2004 {published data only}
- Birkent H, Akçam T, Gerek M, Ertas I, Ozkaptan Y. Results of voice therapy in functional voice disorders. Kulak Burun Bogaz Ihtisas Dergisi 2004;12:120‐7. [PubMed] [Google Scholar]
Boominathan 2008 {published data only}
- Boominathan P, Chandrasekhar D, Nagarajan R, Madraswala Z, Rajan A. Vocal hygiene awareness program for professional voice users (teachers): an evaluative study from Chennai. Asia Pacific Journal of Speech, Language & Hearing 2008;11(1):39‐45. [Google Scholar]
Bouwers 2009 {published data only}
- Bouwers F, Dikkers FG. A retrospective study concerning the psychosocial impact of voice disorders: Voice Handicap Index change in patients with benign voice disorders after treatment (measured with the Dutch version of the VHI). Journal of Voice 2009;23(2):218‐24. [DOI] [PubMed] [Google Scholar]
Broaddus‐Lawrence 2000 {published data only}
- Broaddus‐Lawrence PL, Treole K, McCabe RB, Allen RL, Toppin L. The effects of preventive vocal hygiene education on the vocal hygiene habits and perceptual vocal characteristics of training singers. Journal of Voice 2000;14(1):58‐71. [DOI] [PubMed] [Google Scholar]
Carding 1992 {published data only}
- Carding PN, Horsley IA. An evaluation study of voice therapy in non‐organic dysphonia. European Journal of Disorders of Communication 1992;27:137‐58. [DOI] [PubMed] [Google Scholar]
Carding 1998 {published data only}
- Carding PN, Horsley IA, Docherty GJ. The effectiveness of voice therapy for patients with non‐organic dysphonia. Clinical Otolaryngology and Allied Sciences 1998;23:310‐8. [DOI] [PubMed] [Google Scholar]
Carding 1999 {published data only}
- Carding PN, Horsley IA, Docherty GJ. A study of the effectiveness of voice therapy in the treatment of 45 patients with nonorganic dysphonia. Journal of Voice 1999;13(1):72‐104. [DOI] [PubMed] [Google Scholar]
Chan 1994 {published data only}
- Chan RW. Does the voice improve with vocal hygiene education? A study of some instrumental voice measures in a group of kindergarten teachers. Journal of Voice 1994;8(3):279‐91. [DOI] [PubMed] [Google Scholar]
Chen 2007 {published data only}
- Chen SH, Hsiao TY, Hsiao LC, Chung YM, Chiang SC. Outcome of resonant voice therapy for female teachers with voice disorders: perceptual, physiological, acoustic, aerodynamic, and functional measurements. Journal of Voice 2007;21(4):415‐25. [DOI] [PubMed] [Google Scholar]
Dagli 2008 {published data only}
- Dagli M, Sati I, Acar A, Stone R E Jr, Dursun G, Eryilmaz A. Mutational falsetto: intervention outcomes in 45 patients. Journal of Laryngology and Otology 2008;122(3):277‐81. [DOI] [PubMed] [Google Scholar]
Daniilidou 2007 {published data only}
- Daniilidou P, Carding P, Wilson J, Drinnan M, Deary V. Cognitive behavioral therapy for functional dysphonia: a pilot study. Annals of Otology, Rhinology and Laryngology 2007;116(10):717‐22. [DOI] [PubMed] [Google Scholar]
de Jong 2006 {published data only}
- Jong FI, Kooijman PG, Thomas G, Huinck WJ, Graamans K, Schutte HK. Epidemiology of voice problems in Dutch teachers. Folia Phoniatrica et Logopedica 2006;58(3):186‐98. [DOI] [PubMed] [Google Scholar]
Demmink‐Geertman 2008 {published data only}
- Demmink‐Geertman L, Dejonckere P H. Neurovegetative symptoms and complaints before and after voice therapy for nonorganic habitual dysphonia. Journal of Voice 2008;22(3):315‐25. [DOI] [PubMed] [Google Scholar]
Fex 1994 {published data only}
- Fex B, Fex S, Shiromoto O, Hirano M. Acoustic analysis of functional dysphonia: before and after voice therapy (accent method). Journal of Voice 1994;8(2):163‐7. [DOI] [PubMed] [Google Scholar]
Fischer 2009 {published data only}
- Fischer MJ, Gutenbrunner C, Ptok M. Intensified voice therapy: a new model for the rehabilitation of patients suffering from functional dysphonias. International Journal of Rehabilitation Research 2009;32(4):348‐55. [DOI] [PubMed] [Google Scholar]
Fulljames 2006 {published data only}
- Fulljames N, Harris S. Voice outcome measures: correlations with patients' assessment of their condition and the effectiveness of voice therapy. Logopedics, Phoniatrics, Vocology 2006;31(1):23‐35. [DOI] [PubMed] [Google Scholar]
Gamberini 2007 {published data only}
- Gamberini LJ, Carding PN, Drinnan MD. Comparing two models of voice care delivery. Clinical Otolaryngology 2007;32(2):122‐5. [DOI] [PubMed] [Google Scholar]
Garcia Real 2002 {published data only}
- Garcia Real T, Garcia Real A, Diaz RT, Canizo Fernandez RA. [The outcome of hydration in functional dysphonia]. Anales Otorrinolaringológicos Ibero‐americanos 2002;29(4):377‐91. [PubMed] [Google Scholar]
Gibson 2009 {published data only}
- Gibson PG, Vertigan AE. Speech pathology for chronic cough: a new approach. Pulmonary Pharmacology & Therapeutics 2009;22(2):159‐62. [DOI] [PubMed] [Google Scholar]
Gillivan‐Murphy 2006 {published data only}
- Gillivan‐Murphy P, Drinnan MJ, O'Dwyer TP, Ridha H, Carding P. The effectiveness of a voice treatment approach for teachers with self‐reported voice problems. Journal of Voice 2006;20(3):423‐31. [DOI] [PubMed] [Google Scholar]
Gorman 2008 {published data only}
- Gorman S, Weinrich B, Lee L, Stemple J C. Aerodynamic changes as a result of vocal function exercises in elderly men. Laryngoscope 2008;118(10):1900‐3. [DOI] [PubMed] [Google Scholar]
Guirro 2008 {published data only}
- Guirro RR, Bigaton DR, Silverio KC, Berni KC, Distefano G, Santos FL, et al. Transcutaneous electrical nerve stimulation in dysphonic women. Pró‐Fono 2008;20(3):189‐95. [DOI] [PubMed] [Google Scholar]
Hackworth 2007 {published data only}
- Hackworth RS. The effect of vocal hygiene and behavior modification instruction on the self‐reported vocal health habits of public school music teachers. International Journal of Music Education 2007;25(1):20‐30. [Google Scholar]
Hakkesteegt 2010 {published data only}
- Hakkesteegt MM, Brocaar MP, Wieringa MH. The applicability of the Dysphonia Severity Index and the Voice Handicap Index in evaluating effects of voice therapy and phonosurgery. Journal of Voice 2010;24(2):199‐205. [DOI] [PubMed] [Google Scholar]
Holbrook 1974 {published data only}
- Holbrook A, Rolnick MI, Bailey CW. Treatment of vocal abuse disorders using a vocal intensity controller. Journal of Speech and Hearing Disorders 1974;39(3):298‐303. [DOI] [PubMed] [Google Scholar]
Holmberg 2007 {published data only}
- Holmberg EB, Ihre E, Sodersten M. Phonetograms as a tool in the voice clinic: changes across voice therapy for patients with vocal fatigue. Logopedics, Phoniatrics, Vocology 2007;32(3):113‐27. [DOI] [PubMed] [Google Scholar]
John 2005 {published data only}
- John A, Enderby P, Hughes A. Comparing outcomes of voice therapy: a benchmarking study using the therapy outcome measure. Journal of Voice 2005;19(1):114‐23. [DOI] [PubMed] [Google Scholar]
Jones 2006 {published data only}
- Jones SM, Carding PN, Drinnan MJ. Exploring the relationship between severity of dysphonia and voice‐related quality of life. Clinical Otolaryngology 2006;31(5):411‐7. [DOI] [PubMed] [Google Scholar]
Jonsdottir 2001 {published data only}
- Jonsdottir V, Rantala L, Laukkanen AM, Vilkman E. Effects of sound amplification on teachers' speech while teaching. Logopedics, Phoniatrics, Vocology 2001;26(3):118‐23. [DOI] [PubMed] [Google Scholar]
Jonsdottir 2002 {published data only}
- Jonsdottir V, Laukkanen AM, Vilkman E. Changes in teachers' speech during a working day with and without electric sound amplification. Folia Phoniatrica et Logopaedica 2002;54(6):282‐7. [DOI] [PubMed] [Google Scholar]
Ketelslagers 2007 {published data only}
- Ketelslagers K, Bodt MS, Wuyts FL, Heyning P. Relevance of subglottic pressure in normal and dysphonic subjects. European Archives of Oto‐Rhino‐Laryngology 2007;264(5):519‐23. [DOI] [PubMed] [Google Scholar]
Kirveskari 1988 {published data only}
- Kirveskari P, Jaroma M, Laine T. Occlusal adjustment in the treatment of functional voice disorders. Cranio 1988;6(4):327‐9. [DOI] [PubMed] [Google Scholar]
Kizilay 2008 {published data only}
- Kizilay A, Firat Y. Treatment algorithm for patients with puberphonia. Kulak Burun Bogaz Ihtis Derg 2008;18(6):335‐42. [PubMed] [Google Scholar]
Kotby 1991 {published data only}
- Kotby MN, Elsady SR, Basiouny SE, Abourass YA, Hegazi MA. Efficacy of the accent method of voice therapy. Journal of Voice 1991;5(4):316‐20. [Google Scholar]
Laukkanen 2005 {published data only}
- Laukkanen AM, Leppanen K, Tyrmi J, Vilkman E. Immediate effects of 'voice massage' treatment on the speaking voice of healthy subjects. Folia Phoniatrica et Logopaedica 2005;57(3):163‐72. [DOI] [PubMed] [Google Scholar]
Lehto 2003 {published data only}
- Lehto L, Rantala L, Vilkman E, Alku P, Backstrom T. Experiences of a short vocal training course for call‐centre customer service advisors. Folia Phoniatrica et Logopaedica 2003;55(4):163‐76. [DOI] [PubMed] [Google Scholar]
Lehto 2005 {published data only}
- Lehto L, Alku P, Backstrom T, Vilkman E. Voice symptoms of call‐centre customer service advisers experienced during a work‐day and effects of a short vocal training course. Logopedics, Phoniatrics, Vocology 2005;30(1):14‐27. [DOI] [PubMed] [Google Scholar]
MacKenzie 2001 {published data only}
- MacKenzie K, Millar A, Wilson JA, Sellars C, Deary IJ. Is voice therapy an effective treatment for dysphonia? A randomised controlled trial. BMJ 2001;323(7314):658‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malki 2008 {published data only}
- Malki KH, Nasser NH, Hassan SM, Farahat M. Accent method of voice therapy for treatment of severe muscle tension dysphonia. Saudi Medical Journal 2008;29(4):610‐3. [PubMed] [Google Scholar]
Mathieson 2009 {published data only}
- Mathieson L, Hirani SP, Epstein R, Baken RJ, Wood G, Rubin JS. Laryngeal manual therapy: a preliminary study to examine its treatment effects in the management of muscle tension dysphonia. Journal of Voice 2009;23(3):353‐66. [DOI] [PubMed] [Google Scholar]
McCabe 2002 {published data only}
- McCabe DJ, Titze IR. Chant therapy for treating vocal fatigue among public school teachers: a preliminary study. American Journal of Speech‐Language Pathology 2002;11(3):356‐69. [Google Scholar]
Mendoza‐Lara 1990 {published data only}
- Mendoza‐Lara E. Behavioral treatment of professional dysphonias [Tratamiento conductual de las disfonias profesionales]. Análisis y Modificaión de Conducta 1990;16(48):275‐309. [Google Scholar]
Milbrath 2003 {published data only}
- Milbrath RL, Solomon NP. Do vocal warm‐up exercises alleviate vocal fatigue?. Journal of Speech, Language, and Hearing Research 2003;46(2):422‐36. [DOI] [PubMed] [Google Scholar]
Morsomme 2010 {published data only}
- Morsomme D, Bardonnie MF, Verduyckt I, Jamart J, Remacle M. Subjective evaluation of the long‐term efficacy of speech therapy on dysfunctional dysphonia. Journal of Voice 2010;24(2):178‐82. [DOI] [PubMed] [Google Scholar]
Motel 2003 {published data only}
- Motel T, Fisher KV, Leydon C. Vocal warm‐up increases phonation threshold pressure in soprano singers at high pitch. Journal of Voice 2003;17(2):160‐7. [DOI] [PubMed] [Google Scholar]
Nguyen 2009 {published data only}
- Nguyen DD, Kenny DT. Randomized controlled trial of vocal function exercises on muscle tension dysphonia in Vietnamese female teachers. Journal of Otolaryngology ‐ Head and Neck Surgery 2009;38(2):261‐78. [PubMed] [Google Scholar]
Niebudek‐Bogusz 2007 {published data only}
- Niebudek‐Bogusz E, Kuzanska A, Bloch P, Domanska M, Woznicka E, Politanski P, et al. Applicability of Voice Handicap Index to the evaluation of voice therapy effectiveness in teachers. Medycyna Pracy 2007;58(6):501‐9. [PubMed] [Google Scholar]
Niebudek‐Bogusz 2008 {published data only}
- Niebudek‐Bogusz E, Kotylo P, Politanski P, Sliwinska‐Kowalska M. Acoustic analysis with vocal loading test in occupational voice disorders: outcomes before and after voice therapy. International Journal of Occupational Medicine and Environmental Health 2008;21(4):301‐8. [DOI] [PubMed] [Google Scholar]
Niebudek‐Bogusz 2008a {published data only}
- Niebudek‐Bogusz E, Sznurowska‐Przygocka B, Fiszer M, Kotylo P, Sinkiewicz A, Modrzewska M, et al. The effectiveness of voice therapy for teachers with dysphonia. Folia Phoniatrica et Logopedica 2008;60(3):134‐41. [DOI] [PubMed] [Google Scholar]
Oliveira 2005 {published data only}
- Oliveira Gomes A. The effectiveness of a voice training for telemarketers [A efetividade de um programa de treinamento vocal para operadores de telemarketing]. Doctoral thesis. São Paulo: Universidade de São Paulo, Faculdade de Medicina. Departamento de Medicina Preventiva, 2005:59. [Google Scholar]
Pedersen 2004 {published data only}
- Pedersen M, Beranova A, Moller S. Dysphonia: medical treatment and a medical voice hygiene advice approach. A prospective randomised pilot study. European Archives of Oto‐rhino‐laryngology 2004;261(6):312‐5. [DOI] [PubMed] [Google Scholar]
Popovici 1993 {published data only}
- Popovici C. The role of psychotherapy in the treatment of voice disturbances [Aportul psihoterapiei de relaxare la ameliorarea tulburarilor vocale]. Rev Psih 1993;39(3):225‐37. [Google Scholar]
Portone 2008 {published data only}
- Portone C, Johns MM 3rd, Hapner ER. A review of patient adherence to the recommendation for voice therapy. Journal of Voice 2008;22(2):192‐6. [DOI] [PubMed] [Google Scholar]
Prosek 1978 {published data only}
- Prosek RA, Montgomery AA, Walden BE, Schwartz DM. EMG biofeedback in the treatment of hyperfunctional voice disorders. Journal of Speech and Hearing Disorders 1978;43(3):282‐94. [DOI] [PubMed] [Google Scholar]
Rattenbury 2004 {published data only}
- Rattenbury HJ, Carding PN, Finn P. Evaluating the effectiveness and efficiency of voice therapy using transnasal flexible laryngoscopy: a randomized controlled trial. Journal of Voice 2004;18:522‐33. [DOI] [PubMed] [Google Scholar]
Roy 1993 {published data only}
- Roy N, Leeper HA. Effects of the manual laryngeal musculoskeletal tension reduction technique as a treatment for functional voice disorders: perceptual and acoustic measures. Journal of Voice 1993;7(3):242‐9. [DOI] [PubMed] [Google Scholar]
Roy 1997 {published data only}
- Roy N, Bless DM, Heisey D, Ford CN. Manual circumlaryngeal therapy for functional dysphonia: an evaluation of short‐ and long‐term treatment outcomes. Journal of Voice 1997;11(3):321‐31. [DOI] [PubMed] [Google Scholar]
Roy 2001 {published data only}
- Roy N, Gray SD, Simon M, Dove H, Corbin‐Lewis K, Stemple JC. An evaluation of the effects of two treatment approaches for teachers with voice disorders: a prospective randomized clinical trial. Journal of Speech, Language, and Hearing Research 2001;44(2):286‐96. [DOI] [PubMed] [Google Scholar]
Roy 2002 {published data only}
- Roy N, Weinrich B, Gray SD, Tanner K, Toledo SW, Dove H, et al. Voice amplification versus vocal hygiene instruction for teachers with voice disorders: a treatment outcomes study. Journal of Speech, Language, and Hearing Research 2002;45:625‐38. [DOI] [PubMed] [Google Scholar]
Roy 2003 {published data only}
- Roy N, Weinrich B, Gray SD, Tanner K, Stemple JC, Sapienza CM. Three treatments for teachers with voice disorders: a randomized clinical trial. Journal of Speech, Language, and Hearing Research 2003;46(3):670‐88. [DOI] [PubMed] [Google Scholar]
Schaeffer 2007 {published data only}
- Schaeffer N. Speech breathing behavior and vocal fold function in dysphonic participants before and after therapy during connected speech: preliminary observations. Contemporary Issues in Communication Science & Disorders 2007;34:61‐72. [Google Scholar]
Seifert 2006 {published data only}
- Seifert E, Kollbrunner J. An update in thinking about nonorganic voice disorders. Archives of Otolaryngology Head and Neck Surgery 2006;132(10):1128‐32. [DOI] [PubMed] [Google Scholar]
Sellars 2002 {published data only}
- Sellars C, Carding PN, Deary IJ, MacKenzie K, Wilson JA. Characterization of effective primary voice therapy for dysphonia. Journal of Laryngology and Otology 2002;116(12):1014‐8. [DOI] [PubMed] [Google Scholar]
Silverio 2008 {published data only}
- Silverio KC, Goncalves CG, Penteado RZ, Vieira TP, Libardi A, Rossi D. Actions in vocal health: a proposal for improving the vocal profile of teachers. Pró‐Fono 2008;20(3):177‐82. [DOI] [PubMed] [Google Scholar]
Simberg 2006 {published data only}
- Simberg S, Sala E, Tuomainen J, Sellman J, Ronnemaa AM. The effectiveness of group therapy for students with mild voice disorders: a controlled clinical trial. Journal of Voice 2006;20(1):97‐109. [DOI] [PubMed] [Google Scholar]
Simoes‐Zenari 2008 {published data only}
- Simoes‐Zenari M, Latorre MR. Changes in behavior associated to the use of voice after a speech therapy intervention with professionals of child day care centers. Pró‐Fono 2008;20(1):61‐6. [DOI] [PubMed] [Google Scholar]
Sinkiewicz 2006 {published data only}
- Sinkiewicz A, Pruszewicz A, Obrebowski A, Wiskirska‐Woznica B, Wojnowski W. Subjective assessment of voice functions among teachers taking part in the rehabilitation program. Otolaryngologia Polska 2006;60(3):391‐5. [PubMed] [Google Scholar]
Sliwinska‐Kowalska 2002 {published data only}
- Sliwinska‐Kowalska M, Fiszer M, Kotylo P, Ziatkowska E, Stepowska M, Niebudek‐Bogusz E. Effect of voice emission training on the improvement in voice organ function among students attending the college of teachers. Medycyna Pracy 2002;53(3):229‐32. [PubMed] [Google Scholar]
Sliwinska‐Kowalska 2003 {published data only}
- Sliwinska‐Kowalska M, Fier M, Niebudek‐Bogusz E, Ziatkowska E, Kotylo P, Domatiska M. The effectiveness of voice therapy for teachers with voice disorders [Ocena Skuteczności Terapii Głosowej w Leczeniu Zaburzeń Głosuu Nauczycieli]. Medycyna Pracy 2003;54(4):319‐25. [Google Scholar]
Sliwinska‐Kowalska 2006 {published data only}
- Sliwinska‐Kowalska M, Niebudek‐Bogusz E, Fiszer M, Los‐Spychalska T, Kotylo P, Sznurowska‐Przygocka B, et al. The prevalence and risk factors for occupational voice disorders in teachers. Folia Phoniatrica et Logopedica 2006;58(2):85‐101. [DOI] [PubMed] [Google Scholar]
Sulkowski 2005 {published data only}
- Sulkowski WJ, Kowalska S. Occupational voice disorders: an analysis of diagnoses made and certificates issued in 1999‐2004. International Journal of Occupational Medicine and Environmental Health 2005;18(4):341‐9. [PubMed] [Google Scholar]
Syed 2009 {published data only}
- Syed I, Daniels E, Bleach NR. Hoarse voice in adults: an evidence‐based approach to the 12 minute consultation. Clinical Otolaryngology 2009;34(1):54‐8. [DOI] [PubMed] [Google Scholar]
Timmermans 2004a {published data only}
- Timmermans B, Bodt MS, Wuyts F, Heyning PH. Voice quality change in future professional voice users after 9 months of voice training. European Archives of Oto‐rhino‐laryngology 2004;261(1):1‐5. [DOI] [PubMed] [Google Scholar]
Timmermans 2004b {published data only}
- Timmermans B, Bodt MS, Wuyts FL, Heyning PH. Training outcome in future professional voice users after 18 months of voice training. Folia Phoniatrica et Logopaedica 2004;56(2):120‐9. [DOI] [PubMed] [Google Scholar]
Timmermans 2005 {published data only}
- Timmermans B, Bodt MS, Wuyts FL, Heyning PH. Analysis and evaluation of a voice‐training program in future professional voice users. Journal of Voice 2005;19(2):202‐10. [DOI] [PubMed] [Google Scholar]
Van Lierde (in press) {published data only}
Vertigan 2008 {published data only}
- Vertigan AE, Theodoros DG, Winkworth AL, Gibson PG. A comparison of two approaches to the treatment of chronic cough: perceptual, acoustic, and electroglottographic outcomes. Journal of Voice 2008;22(5):581‐9. [DOI] [PubMed] [Google Scholar]
Voerman 2009 {published data only}
- Voerman MS, Langeveld AP, Rossum MA. Retrospective study of 116 patients with non‐organic voice disorders: efficacy of mental imagery and laryngeal shaking. Journal of Laryngology and Otology 2009;123(5):528‐34. [DOI] [PubMed] [Google Scholar]
Wingate 2007 {published data only}
- Wingate JM, Brown WS, Shrivastav R, Davenport P, Sapienza CM. Treatment outcomes for professional voice users. Journal of Voice 2007;21(4):433‐49. [DOI] [PubMed] [Google Scholar]
Yiu 2006 {published data only}
- Yiu E, Xu JJ, Murry T, Wei WI, Yu M, Ma E, et al. A randomized treatment‐placebo study of the effectiveness of acupuncture for benign vocal pathologies. Journal of Voice 2006;20(1):144‐56. [DOI] [PubMed] [Google Scholar]
Zhao 2005 {published data only}
- Zhao YQ, Zhang LF, Li SQ, Sun YZ. Psycho‐intervention and speech training for mutational falsettos. Chinese Journal of Clinical Rehabilitation 2005;9(20):55‐7. [Google Scholar]
References to studies awaiting assessment
Leppänen 2009 {published data only}
- Leppänen K, Laukkanen AM, Ilomäki I, Vilkman E. A comparison of the effects of voice massage and voice hygiene lecture on self‐reported vocal well‐being and acoustic and perceptual speech parameters in female teachers. Folia Phoniatrica et Logopedica 2009;61(4):227‐38. [DOI] [PubMed] [Google Scholar]
Stemple 1994 {published data only}
- Stemple JC, Lee L, D'Amico B, Pickup B. Efficacy of vocal function exercises as a method of improving voice production. Journal of Voice 1994;8(3):271‐8. [DOI] [PubMed] [Google Scholar]
Additional references
Buekers 1998
- Buekers R. Voice performances in relation to demands and capacity: development of a quantitative phonometric study of the speaking voice. University of Maastricht, 1998. [Google Scholar]
Colton 2006
- Colton R, Casper J, Leonard R. Understanding Voice Problems. A Physiological Perspective for Diagnosis and Treatment. 3rd Edition. Baltimore Philadelphia: Lippincott Williams & Wilkins, 2006. [Google Scholar]
Duffy 2003
- Duffy VG. Effects of training and experience on perception of hazard and risk. Ergonomics 2003;46(1‐3):114‐25. [DOI] [PubMed] [Google Scholar]
Franic 2005
- Franic DM, Bramlett RE, Bothe AC. Psychometric evaluation of disease specific quality of life instruments in voice disorders. Journal of Voice 2005;19(2):300‐15. [DOI] [PubMed] [Google Scholar]
Fritzell 1996
- Fritzell B. Voice disorders and occupations. Logopedics, Phoniatrics, Vocology 1996;21:7‐12. [Google Scholar]
Granqvist 2003
- Granqvist S. Computer methods for voice analysis. Computer methods for voice analysis. Stockholm: Kungliga Tekniska Högskolan, 28 March 2003. [Google Scholar]
Handbook 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Hazlett (In Press)
Hazlett 2001
- Hazlett DE. An investigation into the prevalence and causes of occupational dysphonia in teachers. Jordanstown: School of Communication, Faculty of Social Sciences, University of Ulster, 2001. [Google Scholar]
Herrington‐Hall 1988
- Herrington‐Hall BL, Lee L, Stemple JC, Niemi KR, McHone MM. Description of laryngeal pathologies by age, sex, and occupation in a treatment‐seeking sample. Journal of Speech and Hearing Disorders 1988;53(1):57‐64. [DOI] [PubMed] [Google Scholar]
Hirano 1989
- Hirano M. Objective evaluation of the human voice: clinical aspects. Folia Phoniatrica (Basel) 1989;41(2‐3):89‐144. [DOI] [PubMed] [Google Scholar]
Jacobson 1999
- Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS, et al. The Voice Handicap Index: development and validation. American Journal of Speech‐Language Pathology 1999;6:66‐70. [Google Scholar]
Jasper 2000
- Jasper JK, Colton R. Current understanding and treatment of phonatory disorders in geriatric populations. Current Opinion in Otolaryngology & Head and Neck Surgery 2000;8:158‐64. [Google Scholar]
Kent 2003
- Kent RD, Vorperian HK, Kent JF, Duffy JR. Voice dysfunction in dysarthria: application of the Multi‐Dimensional Voice Program™. Journal of Communication Disorders 2003;36:281–306. [DOI] [PubMed] [Google Scholar]
Laukkanen 1995
- Laukkanen AM. On speaking voice exercises. Tampere, Finland: University of Tampere, 1995. [Google Scholar]
Morton 1998
- Morton V, Watson DR. The teaching voice: problems and perceptions. Logopedics, Phoniatrics, Vocology 1998;23:133‐9. [Google Scholar]
Ohlsson 1987
- Ohlsson AC, Löfqvist A. Work‐day effects on vocal behaviour in switchboard operators and speech therapists. Scandinavian Journal of Logopedics and Phonatrics 1987;12:70‐9. [Google Scholar]
Raes 1996
- Raes JP, Clement PA. Aerodynamic measurements of voice production. Acta Oto‐rhino‐laryngologica Belgica 1996;50(4):293‐8. [PubMed] [Google Scholar]
Ramig 1998
- Ramig LO, Verdolini K. Treatment efficacy: voice disorders. Journal of Speech, Language, and Hearing Research 1998;41(1):S101‐16. [DOI] [PubMed] [Google Scholar]
RevMan 2008 [Computer program]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2008.
Robinson 2002
- Robinson KA, Dickersin K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. International Journal of Epidemiology 2002;31(1):150‐3. [DOI] [PubMed] [Google Scholar]
Roy 2004
- Roy N, Merrill RM, Thibeault S, Gray SD, Smith EM. Voice disorders in teachers and the general population: effects on work performance, attendance, and future career choices. Journal of Speech, Language, and Hearing Research 2004;47(3):542‐51. [DOI] [PubMed] [Google Scholar]
Ruotsalainen 2007
- Ruotsalainen JH, Sellman J, Lehto L, Jauhiainen M, Verbeek JH. Interventions for treating functional dysphonia in adults. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD006373] [DOI] [PubMed] [Google Scholar]
Russell 1998
- Russell A, Oates J, Greenwood KM. Prevalence of voice problems in teachers. Journal of Voice 1998;12(4):467‐79. [DOI] [PubMed] [Google Scholar]
Sala 2001
- Sala E, Laine A, Simberg S, Pentti J, Suonpaa J. The prevalence of voice disorders among day care center teachers compared with nurses: a questionnaire and clinical study. Journal of Voice 2001;15(3):413‐23. [DOI] [PubMed] [Google Scholar]
Scherer 1987
- Scherer R, Titze IR, Raphael B, Wood R, Ramig L, Blager R. Vocal fatigue in a trained and an untrained voice user. In: Bear T, Sasakei C, Harris K editor(s). Laryngeal Function in Phonation and Respiration. Boston: Little, Brown and Company, 1987:533‐53. [Google Scholar]
Slim 2003
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non‐randomized studies (minors): development and validation of a new instrument. ANZ Journal of Surgery 2003;73(9):712‐6. [DOI] [PubMed] [Google Scholar]
Smith 1997
- Smith E, Gray SD, Dove H, Kirchner L, Heras H. Frequency and effects of teachers' voice problems. Journal of Voice 1997;11(1):81‐7. [DOI] [PubMed] [Google Scholar]
Smith 1998
- Smith E, Lemke J, Taylor M, Kirchner HL, Hoffman H. Frequency of voice problems among teachers and other occupations. Journal of Voice 1998;12(4):480‐8. [DOI] [PubMed] [Google Scholar]
Titze 1994
- Titze IR. Principles of voice production. Englewood Cliffs, New Jersey: Prentice‐Hall, Inc, 1994. [Google Scholar]
Titze 1997
- Titze IR, Lemke J, Montequin D. Populations in the U.S. workforce who rely on voice as a primary tool of trade: a preliminary report. Journal of Voice 1997;11(3):254‐9. [DOI] [PubMed] [Google Scholar]
Treole 1997
- Treole K, Trudeau MD. Changes in sustained production tasks among women with bilateral vocal nodules before and after voice therapy. Journal of Voice 1997;11(4):462‐9. [DOI] [PubMed] [Google Scholar]
Verbeek 2005
- Verbeek J, Salmi J, Pasternack I, Jauhiainen M, Laamanen I, Schaafsma F, et al. A search strategy for occupational health intervention studies. Occupational and Environmental Medicine 2005;62(10):682‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Verdolini 2001
- Verdolini K, Ramig LO. Review: occupational risks for voice problems. Logopedics, Phoniatrics, Vocology 2001;26(1):37‐46. [PubMed] [Google Scholar]
Vilkman 1996
- Vilkman E. Occupational risk factors and voice disorders. Logopedics, Phoniatrics, Vocology 1996;21:136‐41. [DOI] [PubMed] [Google Scholar]
Vilkman 2000a
- Vilkman E. A survey on the occupational safety and health arrangements for voice and speech professionals in Europe. In: Dejonckere PH editor(s). Occupational Voice ‐ Care and Cure. The Hague, The Netherlands: Kugler Publications, 2000:1‐9. [Google Scholar]
Vilkman 2000b
- Vilkman E. Voice problems at work: a challenge for occupational safety and health arrangement. Folia Phoniatrica et Logopedica 2000;52(1‐3):120‐5. [DOI] [PubMed] [Google Scholar]
Vilkman 2004
- Vilkman E. Occupational safety and health aspects of voice and speech professions. Folia Phoniatrica et Logopedica 2004;56(4):220‐53. [DOI] [PubMed] [Google Scholar]
Wuyts 2000
- Wuyts FL, Bodt MS, Molenberghs G, Remacle M, Heylen L, Millet B, et al. The Dysphonia Severity Index: an objective measure of vocal quality based on a multiparameter approach. Journal of Speech, Language, and Hearing Research 2000;43(3):796‐809. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Ruotsalainen 2008
- Ruotsalainen J, Sellman J, Lehto L, Verbeek J. Systematic review of the treatment of functional dysphonia and prevention of voice disorders. Otolaryngology ‐ Head and Neck Surgery 2008;138(5):557‐65. [DOI] [PubMed] [Google Scholar]


