Abstract
Objective:
To evaluate whether plain lateral cephalometric radiographs in the neutral position could be used as a diagnostic tool to investigate changes in the cervical spine related to juvenile idiopathic arthritis (JIA).
Materials and Methods:
Lateral cephalometric radiographs of 82 subjects, 21 males and 61 females (8–25 years old), affected with JIA were revised and compared with 82 healthy control subjects matched in age and gender. Changes inspected in the cervical spine were erosions of the dens and fusion of the apophyseal joints. Anterior atlantoaxial subluxation of the first vertebra in relation to the second was examined by measuring the anterior atlanto-dens interval (aADI). Atlantoaxial impaction (AAI) was studied by using the Sakaguchi-Kauppi method.
Results:
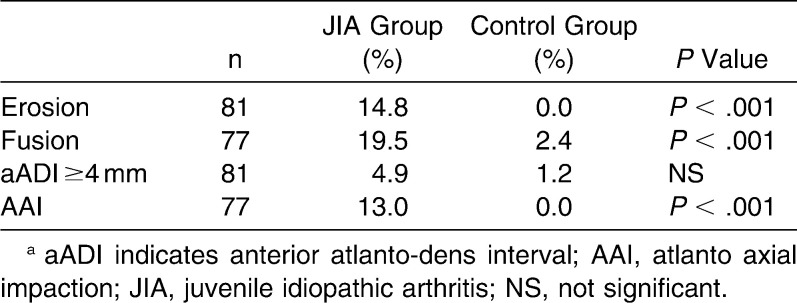
In the JIA sample, erosion was seen in 14.7%, (12 patients), of the patients and apophyseal joint ankylosis (fusion) in 18.3%, (15 patients). Three children and one adult had aADI more than 4.5 or 3 mm, respectively, which is considered to be abnormally increased, and AAI was noted in 13.0% of the subjects. In total, 35%, (29 children), of the children with JIA showed one or several radiographically visible changes as described earlier. Two of the control subjects showed ankylosis of the apophyseal joints, and one had aADI of 4 mm. Compared with the controls, significantly more changes were found in the JIA group.
Conclusion:
It can be concluded that arthritic changes in the cervical spine can be detected at a young age on plain lateral cephalometric radiographs and should be evaluated when available.
Keywords: Vertebrae, Radiological changes, Apophyseal join ankylosis, Anterior atlantoaxial subluxation
INTRODUCTION
Juvenile idiopathic arthritis (JIA) is a group of arthritic diseases of unknown etiology.1 In a very high percentage of the children, up to 87%, inflammatory signs can be detected in the condylar joints of newly diagnosed children.2 The arthritis might lead to severe destruction of the cartilage and underlying bone, which can result in a deviating growth of the face.3–9 To reduce these growth disturbances by early interventions, it is recommended that children with JIA be referred to a dentist for follow-up of facial growth and condylar destruction, especially as clinical and radiologic signs of inflammation are not always present, even though growth disturbances can be seen radiographically.6
On the radiographs taken to evaluate facial growth, at least four vertebrae of the upper part of the cervical spine are usually visible. Using lateral cephalometric radiographs could be a means to diagnose the upper part of the cervical spine, as it can be affected during the whole course of the rheumatoid disease, sometimes even at onset.10 Cervical spine involvement is seen in 21–77% of patients with JIA.10–16 The large range in frequencies depends on the severity of the disease of patients examined and the age of the patients when the radiographs were taken. Most previous studies investigating arthritic changes of the cervical spine have been done in adults or a mixed group of adults and adolescents. In older articles that describe the pathology of the spine, the medication differed notably compared with today's medical treatment regimen. It is thus reasonable to believe that the pattern of the spine's involvement looks different today.
The pathogenesis of JIA seen in the cervical spine is synovial inflammation, hyperemia, and pannus formation at the occipitoatlantoaxial joints resulting in characteristic craniovertebral junction findings.17 Of these findings, apophyseal joint ankylosis or fusion at C2–3 (vertebrae no. 2–3) level is the most frequently noted abnormality and constitutes a characteristic cervical spine change in JIA in 41–52% of patients with arthritis15,18 and might result in growth disturbances in the cervical spine,19 especially in patients with early onset.15
Less common findings are anterior atlantoaxial subluxation (aAAS), which is defined as an increase in the space between the arch of the atlas and the odontoid peg, subaxial subluxation (SAS) among the second and seventh cervical vertebrae, and erosions of the odontoid peg resulting in an “apple core” deformity.10,15,16
Soft-tissue calcification is frequent at levels of vertebral fusion, but calcification also occurs in the ligaments attached to the vertebrae, occurring in about 29% of patients.15
Cranial settling or atlantoaxial impaction (AAI) is another serious complication of long-standing rheumatoid arthritis.20–23 This occurs when the skull and C1 (first vertebrae) begin to settle down on the cervical spine, and the commonly eroded odontoid process comes to lie at an abnormally high location, often severely impinging the brainstem or the craniovertebral junction. Some believe the resultant compression of the medulla and vertebral arteries is the reason for sudden death among patients with rheumatoid arthritic patients who experience cranial settling.17
A potential risk of AAI is the difficulty that is often encountered when inducing general anesthesia. Both micrognathia and stiffness of the neck make intubation difficult, and care must be taken to avoid fracture of an already compromised odontoid process.10,24
The aim of this article, therefore, is to study whether one can detect arthritic changes in the cervical spines of children using plain lateral cephalometric radiographs commonly used in orthodontics. In addition, the cervical spines of the children with JIA were compared with those of healthy children with respect to these changes.
MATERIALS AND METHODS
In this retrospective study, lateral cephalometric radiographs from the records of children diagnosed with JIA at the Department of Pediatrics, Queen Silvia Children's Hospital Sahlgrenska, Gothenburg University, from 1984 to 2006 using the International League of Associations for Rheumatology1 criteria were examined. The children were referred to the Department of Orthodontics at the Institution of Odontology as part of their medical/dental care. In this health program a specialist in either stomatognathic physiology, orthodontics, or pediatric dentistry examines the patient. Lateral cephalometric radiographs are included in the examination.
A total of 82 patients with JIA (61 females, 21 males) were found. Mean age at the time of the lateral cephalometric radiograph was 13.9 years (range = 8 to 25 years). Mean age at onset of JIA was 7.4 years (range = 1 to 16 years), and the mean duration of the disease was 6.5 years (range = 1 to 23 years) (Figures 1, 2). Several patients had a series of radiographs. The most recent ones were included from these, which yielded radiographs from 17 patients taken after 16 years of age.
Figure 1.
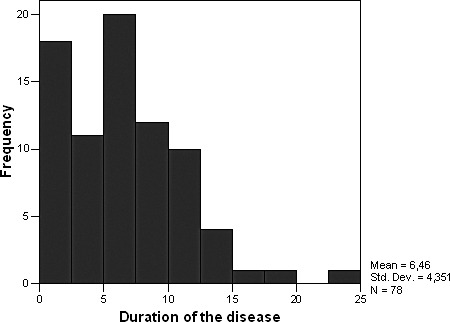
Duration of the disease of patients with JIA.
Figure 2.
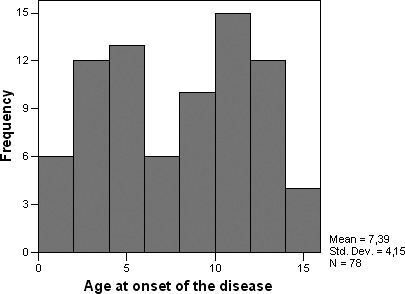
Age at onset.
Fifty-two patients were classified as having polyarthritis, 18 with oligoarthritis, 4 with psoriatic arthritis, 2 with enthesitis-related arthritis, and 6 with undifferentiated arthritis. The patients were matched in age and gender with lateral cephalometric radiographs of 82 healthy children who had been treated at the Department of Orthodontics at the University Clinic of Odontology in Gothenburg, Sweden.
The lateral cephalograms in all the children studied were taken in centric occlusion, with the head fixed in a cephalostat in a neutral position. The magnification in the different groups was adjusted to zero to allow comparisons. According to the Ethics Committee of Gothenburg University, there was no need for ethical approval owing to the retrospective character of the study.
The juvenile idiopathic arthritic changes studied in the lateral cephalometric radiographs were erosions of the dens, ankylosis of the apophyseal joints (fusion; Figure 3), anterior atlantoaxial subluxation (Figure 4), and atlantoaxial impaction (Figures 5, 6). Soft-tissue calcifications and growth disturbances were not investigated.
Figure 3.

Apophyseal joint ankylosis or fusion between C2, C3, C4, and C5.
Figure 4.

aAAS: aADI ≥4 mm (black arrow).
Figure 5.

AAI grade I (see Figure 6).
Figure 6.
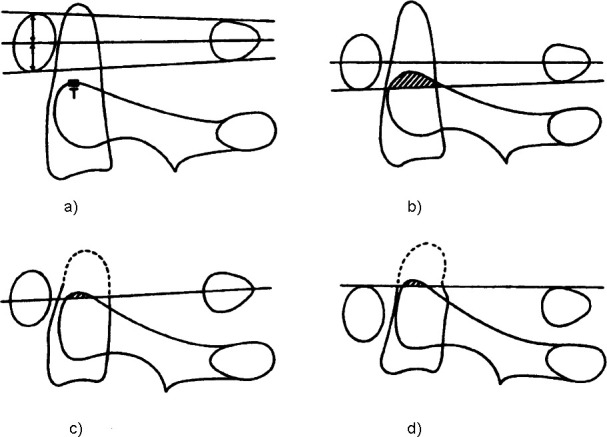
(a) Grade I: Normal. Inferior margin of C1 arch under the level of the C2 facet (top of C2 sclerotic ring). (b) Grade II: Inferior margin of the C1 arch reaches the level of the C2 facet. (c) Grade III: Midpoint of the C1 arch reaches the level of the C2 facet. (d) Grade IV: Superior margin of the C1 arch reaches the level of the C2 facet. AAI (ie, vertical subluxation or cranial settling) is diagnosed by the S-K method,27 which evaluates the position of the atlas (C1) in relation to the axis (C2). This study is age independent and therefore usable in children. In a lateral radiograph, the atlantoaxial facet joints are projected onto each other and form an easily visible curve on the side of the vertebral body of the axis. The most cranial tip of this curve is formed by the most cranial bony parts of the superior facets of the axis. If the cartilage layers of the facet joints are healthy, the tips of the bony facets of the axis are situated under the line that can be drawn form the lowest part of the anterior atlas arch to the lowest part of the posterior atlas arch (the lower atlas arch line). This is the normal situation, which is called grade I. (Figure used courtesy of Dr Kauppi.27)
Odontoid erosions were considered when changes in the normal contour of the anterior, superior and posterior aspects of the odontoid process were present.15 Apophyseal joint ankylosis was recorded when fusion was seen between the joints.16
The anterior aAAS is measured as the sagittal distance between the posterior aspect of the anterior arch of the atlas and the anterior aspect of the odontoid process, called the anterior atlanto-dens interval (aADI). In adults, aADI is considered normal when it is 3 mm in men and 2.5 mm in women.25 However, as the normal value in children is 4 mm, we considered an aADI as abnormal in adults and children when aADI was more than 3 mm and 4.5 mm, respectively.26
AAI (ie, vertical subluxation or cranial settling) is diagnosed by the Sakaguchi-Kauppi (S-K) method,27 which evaluates the position of the atlas in relation to the axis (Figure 6). This method is based on the relationship between the atlas and the axis and is independent of the growth of the patients. Growth disturbances were not measured.
Statistical Methods
The Wilcoxon rank sum test was used for testing differences in inflammatory involvements of the cervical spine between patients with JIA and control subjects.
Error of the Measurement
Twenty radiographs were randomly selected, 10 from the patients with JIA and 10 from the control group. The aADI was measured twice by one examiner at a 2-week interval.
Using Dahlberg's formula (Se2 = ∑d2/2n), the error of the measurement was found to be 0.43 mm. The radiographs were blindly checked for erosions and fusions and AAI once by both authors.
Inter- and intraexaminer reliability for evaluation of erosion, fusion, and AAI was evaluated using Kappa statistics. Disagreement was resolved by a common discussion to the satisfaction of both observers.
RESULTS
The interexaminer reliability Kappa value was 0.66 (good) for erosion, 0.74 (good) for fusion, and 0.75 (good) for AAI. The Kappa intraexaminer reliability was 0.75 (good) for erosion, 0.89 for fusion (very good), and 0.93 (very good) for AAI.
The JIA group showed significantly more radiographic features of inflammatory involvement, such as erosion, fusion, and AAI, compared with the control group (Table 1). The difference in aAAS was not significant compared with the control subjects. In total, 35% of the children with JIA showed one or several radiographically visible changes as described above.
Table 1.
Percentage Distribution of the Different Findings in the Cervical Spinea
DISCUSSION
This study shows that inflammatory changes in the cervical spine, as seen in children with JIA, can be diagnosed on cephalometric films taken primarily for growth analysis of the craniofacial complex or as an aid for orthodontic therapy planning. Significantly more skeletal changes were found in the JIA group than in controls (P < .001).
As mentioned earlier, changes seen in children with arthritis are aAAS, AAI, erosion, fusion, SAS, and growth disturbances. All radiographs were examined for the first four changes. In some radiographs, parts of the skull and cervical spine are cut off, causing dropouts in measurements. In most of the radiographs used in this study, only the first to the fourth vertebrae were pictured. This made it impossible to look for SAS among the second and seventh cervical vertebrae.
The reason for not measuring growth disturbances of the vertebrae is that they are preferably measured in adult patients with JIA.16 Most of our patients were young, and the spine was not yet fully developed.
The immature cervical spine was also an obstacle in our research as we sought the appropriate methods for use. Rheumatoid arthritis has primarily been studied in adults, and some measurements are not applicable in children. Several methods are also being used to define AAI in adult rheumatoid arthritis, but only the S-K method27 is independent of growth and could therefore be used in this study in children and adolescents.
To diagnose aAAS and fusion, it is recommended that two cephalometric radiographs be compared, one in extension and one in flexion of the neck. This is important first in order to check the consistency of the fusion of the vertebrae and second because it has been found that aADI increases in flexion and decreases in extension of the neck. It has been found that about 48% of aAASs are lost in the neutral position.2. For this reason, most studies in adults make measurements in flexion. In the present study, where we had access to radiographs only in normal position, the findings might be underestimated for aAAS and overestimated for apophyseal joint ankylosis.
The shortcomings of plain cephalometric radiographs in measuring erosions are clear, and computed tomography, and especially magnetic resonance imaging, are the methods of choice as concerns erosions. However, because of the expense and radiation load, these methods can only be used in certain cases.
The findings regarding cervical involvement differ depending on the age of the patients and the severity of the disease. Espada et al.15 found spinal changes in 60% of 120 patients examined with a more severe and polyarticular course of the disease, and Hensinger et al.10 found symptoms and signs only in patients with a polyarticular or systemic type of disease and radiographic changes only in one patient with oligorathritis. In the present study, however, 5 of 18 patients with oligoarthritis showed radiographic changes of the cervical spine, indicating that the spine might be involved even in young children with a minor number of joints involved. It is certain that the longer the duration of the disease, the more obvious the changes may become. Laiho et al.,16 aware of this, examined 159 patients with JIA at an adult age and found that significant changes with fusion were more often discovered (52%, 41 patients). Fried et al.24 demonstrated cervical spine involvement in 31% of 92 patients, most of them young. This figure is quite close to the results of the present study, with 35% involvement, showing that the radiographs we used for examination are probably sufficient for the purpose of finding pathology in the cervical spine.
Ankylosis of the apophyseal joints (fusion) was the most frequent involvement in the present study, as was also found in the investigations of Espada et al.15 and Hensinger et al.,10 with erosion and AAS the next most frequent. Fusion was also found in two patients in our control group. Fusion can indeed be found in healthy individuals,29 as can other anomalies of the odontoid process, such as congenital hypoplasia or aplasia, as Tetradis and Kantor30 showed in their case report. It is therefore important that an orthodontist, especially when dealing with patients with JIA, know how to diagnose all structures visible on radiographs that are taken, not only the craniofacial complex but also the part of the spine that is depicted.
Although plain radiographs have certain limitations in their diagnostic value for the spine, because these radiographs are frequently used by orthodontists they are an exceptional way of making a first survey of the cervical spine, especially in patients with JIA.
REFERENCES
- 1.Petty R. E, Southwood T. R, Manners P, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–392. [PubMed] [Google Scholar]
- 2.Kuseler A, Pedersen T. K, Herlin T, Gelineck J. Contrast enhanced magnetic resonance imaging as a method to diagnose early inflammatory changes in the temporomandibular joint in children with juvenile chronic arthritis. J Rheumatol. 1998;25:1406–1412. [PubMed] [Google Scholar]
- 3.Billiau A. D, Hu Y, Verdonck A, Carels C, Wouters C. Temporomandibular joint arthritis in juvenile idiopathic arthritis: prevalence, clinical and radiological signs, and relation to dentofacial morphology. J Rheumatol. 2007;34:1925–1933. Epub 2007 Aug 1. [PubMed] [Google Scholar]
- 4.Hu Y, Billiau A. D, Verdonck A, Wouters C, Carels C. Variation in dentofacial morphology and occlusion in juvenile idiopathic arthritis subjects: a case-control study. Eur J Orthod. 2009;31:51–58. doi: 10.1093/ejo/cjn085. [DOI] [PubMed] [Google Scholar]
- 5.Huntjens E, Kiss G, Wouters C, Carels C. Condylar asymmetry in children with juvenile idiopathic arthritis assessed by cone-beam computed tomography. Eur J Orthod. 2008;30:545–551. doi: 10.1093/ejo/cjn056. [DOI] [PubMed] [Google Scholar]
- 6.Twilt M, Schulten A. J, Nicolaas P, Dülger A, van Suijlekom-Smit L. W. Facioskeletal changes in children with juvenile idiopathic arthritis. Ann Rheum Dis. 2006;65:823–825. doi: 10.1136/ard.2005.042671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kjellberg H, Fasth A, Kiliaridis S, Wenneberg B, Thilander B. Craniofacial structure in children with juvenile chronic arthritis (JCA) compared with healthy children with ideal or postnormal occlusion. Am J Orthod Dentofacial Orthop. 1995;107:67–78. doi: 10.1016/s0889-5406(95)70158-3. [DOI] [PubMed] [Google Scholar]
- 8.Stabrun A. E, Larheim T. A, Höyeraal H. M, Rösler M. Reduced mandibular dimensions and asymmetry in juvenile rheumatoid arthritis. Pathogenetic factors. Arthritis Rheum. 1988;31:602–611. doi: 10.1002/art.1780310504. [DOI] [PubMed] [Google Scholar]
- 9.Stabrun A. E. Impaired mandibular growth and micrognathic development in children with juvenile rheumatoid arthritis. A longitudinal study of lateral cephalographs. Eur J Orthod. 1991;13:423–434. doi: 10.1093/ejo/13.6.423. [DOI] [PubMed] [Google Scholar]
- 10.Hensinger R. N, DeVito P. D, Ragsdale C. G. Changes in the cervical spine in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 1986;68:189–198. [PubMed] [Google Scholar]
- 11.Martel W, Holt J. F, Cassidy J. T. Roentgenologic manifestations of juvenile rheumatoid arthritis. Am J Roentgenol Radium Ther Nucl Med. 1962;88:400–423. [PubMed] [Google Scholar]
- 12.Grokoest A. W, Snyder A. I, Ragan C. Some aspects of juvenile rheumatoid arthritis. Bull Rheum Dis. 1957;8:147–148. [PubMed] [Google Scholar]
- 13.Schaller J, Wedgwood R. J. Juvenile rheumatoid arthritis: a review. Pediatrics. 1972;50:940–953. [PubMed] [Google Scholar]
- 14.Cassidy J. T, Martel W. Juvenile rheumatoid arthritis: clinicoradiologic correlations. Arthritis Rheum. 1977;20(2 suppl):207–211. [PubMed] [Google Scholar]
- 15.Espada G, Babini J. C, Maldonado-Cocco J. A, García-Morteo O. Radiologic review: the cervical spine in juvenile rheumatoid arthritis. Semin Arthritis Rheum. 1988;17:185–195. doi: 10.1016/0049-0172(88)90019-4. [DOI] [PubMed] [Google Scholar]
- 16.Laiho K, Savolainen A, Kautiainen H, Kekki P, Kauppi M. The cervical spine in juvenile chronic arthritis. Spine J. 2002;2:89–94. doi: 10.1016/s1529-9430(02)00151-1. [DOI] [PubMed] [Google Scholar]
- 17.Johnson M. H, Smoker W. R. Lesions of the craniovertebral junction. Neuroimaging Clin North Am. 1994;4:599–617. [PubMed] [Google Scholar]
- 18.Ziff M, Contreras V, McEwen C. Spondylitis in post-pubertal patients with rheumatoid arthritis of juvenile onset. Ann Rheum Dis. 1956;15:40–45. doi: 10.1136/ard.15.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Endén K, Laiho K, Kautiainen H, Arkela-Kautiainen M, Belt E, Kauppi M. Subaxial cervical vertebrae in patients with juvenile idiopathic arthritis—Something special? Joint Bone Spine. 2009;76:519–523. doi: 10.1016/j.jbspin.2008.10.009. Epub 2009 Feb 11. [DOI] [PubMed] [Google Scholar]
- 20.Boden S. D, Dodge L. D, Bohlman H. H, Rechtine G. R. Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am. 1993;75:1282–1297. doi: 10.2106/00004623-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Bland J. H. Rheumatoid subluxation of the cervical spine. J Rheumatol. 1990;17:134–137. [PubMed] [Google Scholar]
- 22.El-Khoury G. Y, Wener M. H, Menezes A. H, Dolan K. D, Kathol M. E. Cranial settling in rheumatoid arthritis. Radiology. 1980;137:637–642. doi: 10.1148/radiology.137.3.7444048. [DOI] [PubMed] [Google Scholar]
- 23.Casey A. T, Crockard H. A, Geddes J. F, Stevens J. Vertical translocation: the enigma of the disappearing atlantodens interval in patients with myelopathy and rheumatoid arthritis. Part I. Clinical, radiological, and neuropathological features. J Neurosurg. 1997;87:856–862. doi: 10.3171/jns.1997.87.6.0856. [DOI] [PubMed] [Google Scholar]
- 24.Fried J. A, Athreya B, Gregg J. R, Das M, Doughty R. The cervical spine in juvenile rheumatoid arthritis. Clin Orthop Relat Res. 1983;179:102–106. [PubMed] [Google Scholar]
- 25.Martel W. The occipito-atlanto-axial joints in rheumatoid arthritis and ankylosing spondylitis. Am J Roentgenol Radium Ther Nucl Med. 1961;86:223–240. [PubMed] [Google Scholar]
- 26.Locke G. R, Gardner J. I, Van Epps E. F. Atlas-dens interval (ADI) in children: a survey based on 200 normal cervical spines. Am J Roentgenol Radium Ther Nucl Med. 1966;97:135–140. doi: 10.2214/ajr.97.1.135. [DOI] [PubMed] [Google Scholar]
- 27.Kauppi M, Sakaguchi M, Konttinen Y. T, Hämäläinen M. A new method of screening for vertical atlantoaxial dislocation. J Rheumatol. 1990;17:167–172. [PubMed] [Google Scholar]
- 28.Kauppi M, Neva M. H. Sensitivity of lateral view cervical spine radiographs taken in the neutral position in atlantoaxial subluxation in rheumatic diseases. Clin Rheumatol. 1998;17:511–514. doi: 10.1007/BF01451289. [DOI] [PubMed] [Google Scholar]
- 29.Smoker W. R. Congenital anomalies of the cervical spine. Review. Neuroimaging Clin North Am. 1995;5:427–449. [PubMed] [Google Scholar]
- 30.Tetradis S, Kantor M. L. Anomalies of the odontoid process discovered as incidental findings on cephalometric radiographs. Am J Orthod Dentofacial Orthop. 2003;124:184–189. doi: 10.1016/s0889-5406(03)00394-9. [DOI] [PubMed] [Google Scholar]