Abstract
Objective:
To describe the correlation between the skeletal changes induced by maxillary protraction treatment and the sagittal airway dimension associated with tongue, soft palate, and hyoid bone position in skeletal Class III children.
Materials and Methods:
Twenty Class III patients (5 boys, 15 girls; mean age, 9.4 ± 1.8 years) treated with a maxillary protraction appliance were included in this study. Pretreatment and posttreatment cephalometric radiographs were analyzed; linear and angular measurements were performed by an expert orthodontist. The correlation between treatment changes in craniofacial morphology and those in upper airway, tongue, soft palate, and hyoid position was evaluated by Pearson's correlation analysis.
Results:
A significant increase in maxillary forward displacement, inhibition of mandibular forward growth, and clockwise rotation of the mandible were observed. Simultaneously, nasopharyngeal airway measurements PNS-ad1 and PNS-ad2 significantly increased by 1.4 mm and 1.9 mm, respectively. A correlation analysis revealed that maxillary protraction had a positive relationship with PNS-ad1 and PNS-ad2.
Conclusions:
The nasopharyngeal airway dimensions can be improved in the short term with maxillary protraction in skeletal Class III children.
Keywords: Maxillary protraction, Airway, Tongue, Soft palate
INTRODUCTION
Skeletal Class III malocclusion is associated with maxillary undergrowth, mandibular overgrowth, or the combination of both conditions. A maxillary protraction appliance (MPA) has been used for the treatment of Class III malocclusion of growing patients accompanying maxillary undergrowth.1,2 It was reported that the main effects of the treatment with an MPA include enhanced forward displacement of the maxilla, clockwise rotation of the mandible, counterclockwise rotation of the palatal plane, and labioversion of maxillary incisors.3–7 Despite several studies performed on skeletal and dental changes via the MPA, there have been few studies conducted on the correlation of the skeletal change with structures in the airway space via the MPA.
Airway space is divided into a nasopharynx, oropharynx, and hypopharynx and consists of hard tissues—such as maxilla, mandible, palatine bone, vomer, and cervical spine—and muscles of the tongue and soft palate, oral cavity, nasal cavity, and oral and retropharyngeal mucosa. The upper airway is closely related to the hyoid bone, as the hyoid bone is attached to the suprahyoid and infrahyoid muscles. The posture and position of the tongue are mainly regulated by the neuromusclature. As the genioglossus muscle is regulated by mechanoreceptors in the temporomandibular joint and contracts whenever the glossopharyngeal and nasopharyngeal nerves are stimulated, this muscle is associated with airway control. The soft palate, which is attached to the maxilla, can be affected by positional changes in the maxilla and the tongue due to its physical contact with the tongue.
It was reported that the skeletal change in skeletal Class III children via an orthopedic appliance changes the airway width.8–13 Kilinç et al.10 and Oktay and Ulukaya11 reported the significant change in the oropharynx and the nasopharynx after treatment with a maxillary protraction appliance. On the other hand, Sayinsu et al.9 and Kaygisiz et al.12 observed the significant change only in the nasopharynx. Hiyama et al.8 and Mucedero et al.13 reported no significant correlation of the skeletal change with change in the airway width.
The purpose of this study was to investigate the effects of the skeletal change by treatment with a maxillary protraction appliance on the airway width, tongue position, and soft palate, as well as their correlation. The research protocol was reviewed and approved by the institutional review board of the Kyung Hee University Medical Center (IRB No. KHD IRB 2009-14).
MATERIALS AND METHODS
The sample consisted of 20 patients (5 boys and 15 girls) who were treated in the Department of Orthodontics, Kyung Hee University Dental Hospital. The sample was collected based on the following inclusion criteria: anterior crossbite with a Class III molar relationship, accompanying maxillary skeletal retrusion, and no congenital anomalies or mandibular deviation. Of these patients, people who had been successfully treated using a maxillary protraction appliance (Delaire-type face mask) were chosen as subjects.
The lateral cephalometric radiograph was assessed on each patient at the first encounter (T1) and at the treatment completion of the first stage (T2). The mean age of the subjects at T1 was 9.4 ± 1.8 years, and the mean period of the treatment was 8.3 ± 3.8 months.
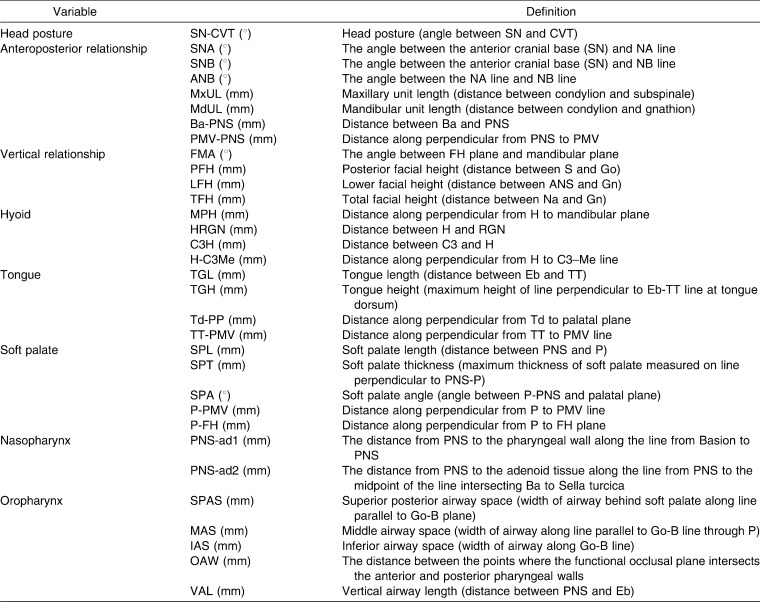
Lateral cephalometric radiographs were taken in the natural head position with CX-90SP (Asahi Roentgen, Kyoto, Japan) at 80 kVp, 20 mA, with occlusal position as after a usual swallow. A single orthodontist traced the lateral cephalometric radiograph using a pen (thickness 0.5 mm) on a 0.003-inch acetate film. Facial and airway measurements were also taken. Measurement points, lines, and items on the lateral cephalometric radiograph used in this study are presented in Figure 1 and Table 1.
Figure 1.
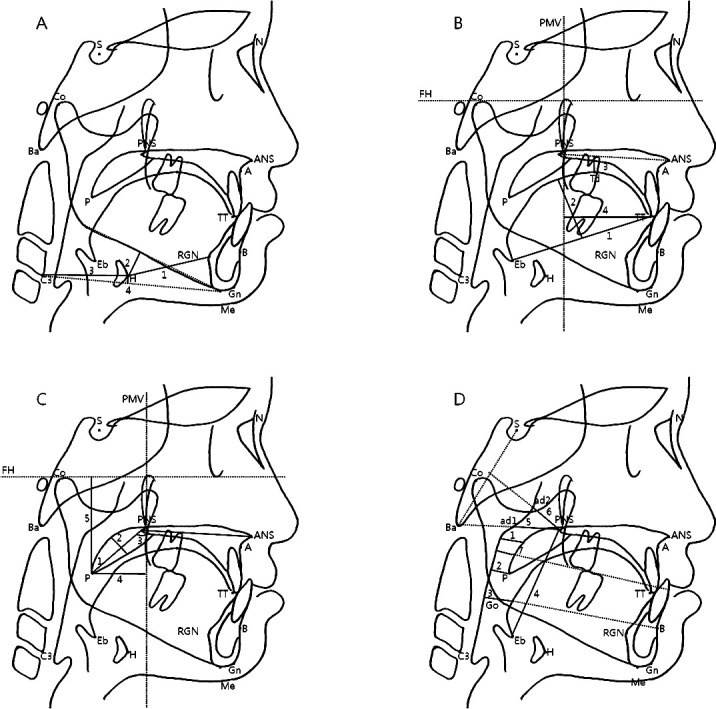
Cephalometric measurements. (A) Hyoid. (1) HRGN, (2) MPH, (3) H-C3, (4) H-C3Me. (B) Tongue. (1) TGL, (2) TGH, (3) Td-PP, (4) TT-PMV. (C) Soft Palate. (1) SPL, (2) SPT, (3) SPA, (4) P-PMV, (5) P-FH. (D) Airway. (1) SPAS, (2) MAS, (3) IAS, (4) VAL, (5) PNS-ad1, (6) PNS-ad2, (7) OAW.
Table 1.
Variables Used in Cephalometric Analysis
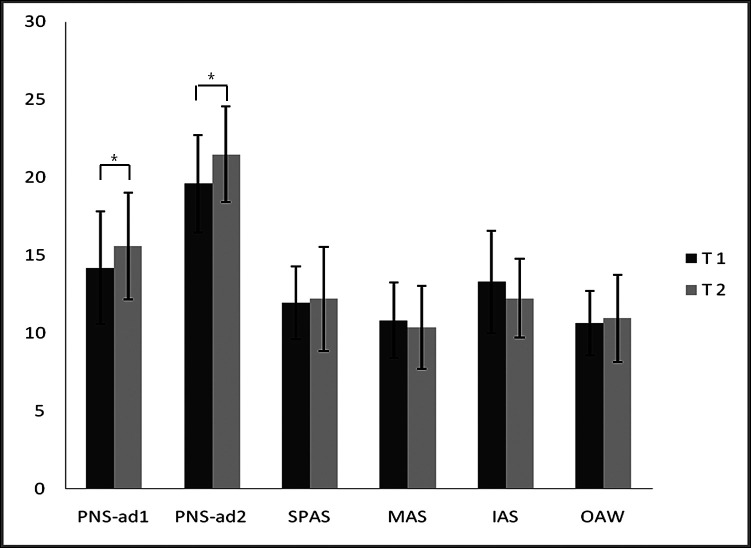
Figure 2.
Airway widths before and after maxillary protraction treatment.
Statistical Analysis
To estimate the reliability of a single measurer, measurement was repeatedly performed at 3-week intervals. A paired t-test with a significance level of ≤.01 was conducted on two measurements to check for any significant differences in the measured items as recorded in two different measurements. After no significant difference was confirmed, the mean values of the two measurements were adopted for statistical analyses.
All statistical analyses were performed using SPSS version 12.0 for Windows (SPSS Inc, Chicago, Ill). The result of the Shapiro-Wilk test confirmed that the variables followed normal distribution (P > .05). The pretreatment and posttreatment changes by maxillary protraction appliance were analyzed by paired t-test. To investigate the correlation between the skeletal changes and upper airway alterations, Pearson's correlation analysis was used. The level of significance was established as P < .05.
RESULTS
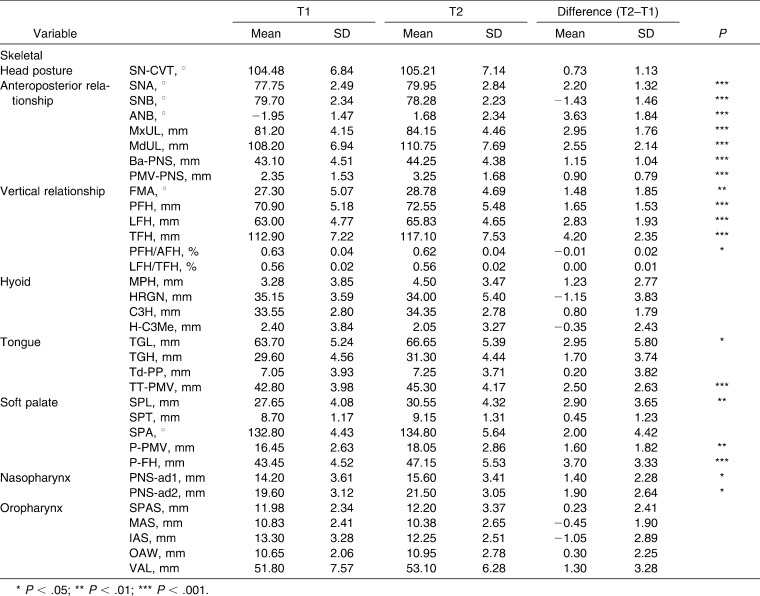
The mean and standard deviation at the first encounter (T1), at treatment completion (T2), and of the difference between them (T2–T1) were statistically analyzed using paired t-test, and the results are presented in Table 2 and Figure 2. As a result of the skeletal change by treatment with a maxillary protraction appliance, SNA increased by 2.20° ± 1.32°, ANB increased by 3.63° ± 1.84°, and FMA increased by 1.48° ± 1.85°, but SNB decreased by 1.43° ± 1.46°, which resulted in forward displacement on the maxilla and clockwise rotation of the mandible (P < .05). There was no observed change in the vertical or horizontal location of the hyoid bone. There was a significant increase in the measured length (TGL, SPL, TT-PMV, P-PMV, P-FH) in both the tongue and the soft palate. As for airway space measurements, PNS-ad1 increased by 1.40 ± 2.28 mm and PNS-ad2 increased by 1.90 ± 2.64 mm, which were statistically significant (P < .05). SPAS, VAL, and OAW increased, and MAS and IAS decreased, but the changes were not statistically significant.
Table 2.
Comparisons of the T1 to T2 Changes (Paired t-Test)
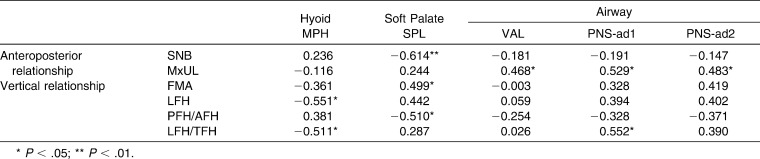
Presented in Table 3 are the results of the correlation analysis of the skeletal change with changes in the hyoid bone, the tongue, the soft palate, and the airway. The change in MPH showed a negative correlation with the change in LFH (r = −.551) and LFH/TFH (r = −.511). The change in SPL showed a negative correlation with the change in SNB (r = −.614) and PFH/AFH (r = −.510) and a positive correlation with the change in FMA (r = .499). The change in VAL (r = .468), PNS-ad1 (r = .529), and PNS-ad2 (r = .483), respectively, showed a positive correlation with the change in MxUL (P < .05).
Table 3.
Results of the Correlation Analysis Between the Craniofacial and Soft Tissue Variables
DISCUSSION
Orthodontic treatments, such as growth modification using a rapid palatal expander or an orthopedic appliance and orthognathic surgery, cause not only teeth movement but also a change in the skeletal dimension, leading to size and positional changes in the adjacent soft tissue. This study confirmed the effects of the skeletal change by the treatment with an MPA on the size changes in the airway, tongue, and soft palate.
The MPA affects both the maxilla and the mandible. Force anteroinferiorly exerted on the maxillary occlusal plane enhances the forward growth of maxilla and simultaneously causes the forward movement of the maxillary dentition and anterosuperior rotation of the palatal plane. Moreover, force posteriorly exerted on the mandible causes clockwise rotation of the mandible.3–7 In this study, the anteroposterior skeletal change caused by the MPA increased SNA and MxUL, enhancing the forward growth of the maxilla. In the mandible, SNB decreased but MnUL increased, showing the clockwise rotation of the mandible rather than the suppression of its growth. The vertical skeletal change increased FMA and decreased PFH/AFH, resulting in facial height increase by the clockwise rotation of mandible. The skeletal change shown in this study was consistent with the result of previous studies on the MPA.3–7
The changes in airway space components by the MPA were analyzed through measurements of the hyoid bone, soft palate, tongue, and airway. There was no anteroposterior or vertical positional change observed in the hyoid bone. There was an increased length without thickness change observed in both the tongue and the soft palate. Hiyama et al.8 reported that the tongue is positioned more anteriorly due to the increased space in the oral cavity caused by the forward growth of maxilla. They reported that the positional change in the tongue causes forward positioning of the soft palate, leading to increased upper airway width.14
This study of the measurements for airway space after the treatment with the maxillary protraction appliance showed PNS-ad1 (1.40 ± 2.28 mm) and PNS-ad2 (1.90 ± 3.64 mm) positioned relatively superiorly. This result is consistent with the result of studies by Sayinsu et al.9 and Kaygisiz et al.,12 which showed an increase in nasopharyngeal space rather than that of oropharyngeal space. Ceylan and Oktay15 reported that airway space size was affected by the change in the ANB angle. They also reported that oropharyngeal space decreased with the increase in the ANB angle. Akcam et al.16 reported that airway space decreased in patients with the clockwise rotation of the mandible. Kilinç et al.10 reported an increase in both nasopharyngeal and oropharyngeal space in the study using a maxillary protraction appliance, mentioning that the reason was the relatively small reduction of SNB angle and mandible rotation. In this study, the clockwise rotation of the mandible and increased ANB were the relative results of the forward growth of maxilla and did not cause the reduction of either oropharyngeal or hypopharyngeal space.
Changes in PNS-ad1 (r = .529) and PNS-ad2 (r = .483), respectively, showed a positive correlation with change in MxUL, indicating that maxillary growth by MPA caused increased nasopharyngeal space. In addition, in a rhinomanometric study, Ghoreishian and Gheisari17 reported that forward displacement on the maxilla via a maxilla surgery (Le Fort I) reduced intranasal resistance and improved the respiratory function by increasing air flow. In consideration of these facts, it is likely that maxillary protraction treatment in growing patients accompanying maxillary undergrowth improves their respiratory function by increasing upper airway space.
In a study on soft tissue growth in the oropharyngeal space, Taylor et al.18 reported that measurements in the soft tissue positioned at the posterior pharyngeal wall showed a big change in 6- to 9-year-old and 12- to 15-year-old subjects but showed less growth in 9- to 12-year-old subjects. In a study by Kilinç et al.,10 change in the upper airway space in the control group consisting of 17 nontreated Class III patients was trivial in during the follow-up of 9.8 months. In this study, the change in pharyngeal growth could be negligible because the mean age of subjects was 9.4 years and the mean treatment period was 8.3 months. Thus, a control group was not used.
Changes in pretreatment and posttreatment were measured using lateral cephalometric radiographs. Measurements in airway space, tongue, and hyoid bone using lateral cephalometric radiographs were known to have a correlation with those using CT19 and were reproducible at the natural head position.20 In addition, measurements in airway space were known to vary depending on the head positon.21 Therefore, the lateral cephalometric radiograph should be taken at the natural head position to ensure the exact evaluation of airway space components when using lateral cephalometric radiographs. SN-CVT was used to determine changes in the head position prior to treatment (T1) and after treatment (T2), showing no significant difference between T1 and T2. There was, however, limited evaluation of three-dimensional space as the lateral cephalometric radiograph is two-dimensional, whereas airway space is three-dimensional. In studies on upper airway space using the recently introduced cone-beam computed tomography (CBCT),22,23 space area, anteroposterior width, horizontal width, and upper airway volume can be measured. Therefore, it is likely that CBCT will be useful for the assessment of the effect on the airway of the treatment with a maxillary protraction appliance.
CONCLUSION
It is likely that forward movement of the maxilla through maxillary protraction treatment in Class III malocclusion in growing patients with maxillary undergrowth improves respiratory function by increasing upper airway space.
Acknowledgment
This study was supported by the Kyung Hee University program for the young researcher of medical science (2010).
REFERENCES
- 1.Mermigos J, Full C. A, Andreasen G. Protraction of the maxillofacial complex. Am J Orthod Dentofacial Orthop. 1990;98:47–55. doi: 10.1016/0889-5406(90)70031-7. [DOI] [PubMed] [Google Scholar]
- 2.Kapust A. J, Sinclair P. M, Turley P. K. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212. doi: 10.1016/s0889-5406(98)70141-6. [DOI] [PubMed] [Google Scholar]
- 3.Bacetti T, McGill J. S, Franchi L, McNamara J. A, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 4.Gallagher R. W, Miranda F, Buschang P. H. Maxillary protraction: treatment and posttreatment effects. Am J Orthod Dentofacial Orthop. 1998;113:612–619. doi: 10.1016/s0889-5406(98)70220-3. [DOI] [PubMed] [Google Scholar]
- 5.Yüksel S, Uçem T. T, Keykubat A. Early and late facemask therapy. Eur J Orthod. 2001;23:559–568. doi: 10.1093/ejo/23.5.559. [DOI] [PubMed] [Google Scholar]
- 6.Hwang C. J, Kyung S. H, Lim J. K. Treatment effect of protraction head gear on skeletal Class III malocclusion. Korean J Orthod. 1994;24:851–860. [Google Scholar]
- 7.Baik H. S, Sung S. J. Effects of maxillary protraction on growth in Class III malocclusion. Korean J Orthod. 1994;24:349–366. [Google Scholar]
- 8.Hiyama S, Suda N, Ishii-Suzuki M, Tsuiki S, Ogawa M, Suzuki S, Kuroda T. Effects of maxillary protraction on craniofacial structures and upper-airway dimension. Angle Orthod. 2002;72:43–47. doi: 10.1043/0003-3219(2002)072<0043:EOMPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Sayinsu K, Isik F, Arun T. Sagittal airway dimension following maxillary protraction: a pilot study. Eur J Orthod. 2006;28:184–189. doi: 10.1093/ejo/cji095. [DOI] [PubMed] [Google Scholar]
- 10.Kilinç A. S, Arslan S. G, Kama J. D, Özer T, Dari O. Effects on the sagittal pharyngeal dimensions of protraction and rapid palatal expansion in Class III malocclusion subjects. Eur J Orthod. 2008;30:61–66. doi: 10.1093/ejo/cjm076. [DOI] [PubMed] [Google Scholar]
- 11.Oktay H, Ulukaya E. Maxillary protraction appliance effect on the size of the upper airway passage. Angle Orthod. 2008;78:209–213. doi: 10.2319/122806-535.1. [DOI] [PubMed] [Google Scholar]
- 12.Kaygisiz E, Tuncer B. B, Yüksel S, Tuncer C, Yildiz C. Effects of maxillary protraction and fixed appliance therapy on the pharyngeal airway. Angle Orthod. 2009;79:660–667. doi: 10.2319/072408-391.1. [DOI] [PubMed] [Google Scholar]
- 13.Mucedero M, Baccetti T, Franchi L, Cozza P. Effects of maxillary protraction with or without expansion on the sagittal pharyngeal dimensions in Class III subjects. Am J Orthod Dentofacial Orthop. 2009;135:777–781. doi: 10.1016/j.ajodo.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 14.Özbek M. M, Memikoglu T. U. T, Gogen H, Lowe A. A, Caspian E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327–336. doi: 10.1043/0003-3219(1998)068<0327:OADAFO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Ceylan I, Oktay H. A study of the pharyngeal size in different skeletal patterns. Am J Orthod Dentofacial Orthop. 1995;108:69–75. doi: 10.1016/s0889-5406(95)70068-4. [DOI] [PubMed] [Google Scholar]
- 16.Akcam M. O, Toygar U, Wada T. Longitudinal investigation of soft palate and nasopharyngeal airway relations in different rotation types. Angle Orthod. 2002;72:521–526. doi: 10.1043/0003-3219(2002)072<0521:LIOSPA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Ghoreishian M, Gheisari R. The effect of maxillary multidirectional movement on nasal respiration. J Oral Maxillofac Surg. 2009;67:2283–2286. doi: 10.1016/j.joms.2009.04.064. [DOI] [PubMed] [Google Scholar]
- 18.Taylor M, Hans M. G, Strohl K. P, Nelson S, Broadbent B. H. Soft tissue growth of the oropharynx. Angle Orthod. 1996;66:393–400. doi: 10.1043/0003-3219(1996)066<0393:STGOTO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Lowe A. A, Fleetham J. A, Adachi S, Ryan C. F. Cephalometric and computed tomographic predictors of obstructive sleep apnea severity. Am J Orthod Dentofacial Orthop. 1995;107:589–595. doi: 10.1016/s0889-5406(95)70101-x. [DOI] [PubMed] [Google Scholar]
- 20.Malkoç S, Üsümez S, Nur M, Donaghy C. E. Reproducibility of airway dimensions and tongue and hyoid positions on lateral cephalograms. Am J Orthod Dentofacial Orthop. 2005;128:513–516. doi: 10.1016/j.ajodo.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Pracharktam N, Hans M. G, Strohl K. P, Redline S. Upright and supine cephalometric evaluation of obstructive sleep apnea syndrome and snoring subjects. Angle Orthod. 1994;64:63–74. doi: 10.1043/0003-3219(1994)064<0063:UASCEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Lee Y. S, Baik H. S, Lee K. J, Yu H. S. The structural change in the hyoid bone and upper airway after orthognathic surgery for skeletal Class III anterior open bite patients using 3-dimensional computed tomography. Korean J Orthod. 2009;39:72–82. [Google Scholar]
- 23.Kim Y. I, Kim S. S, Son W. S, Park S. B. Pharyngeal airway analysis of different craniofacial morphology using cone-beam computed tomography (CBCT) Korean J Orthod. 2009;39:136–145. [Google Scholar]