Abstract
Objective:
To determine compliance with oral hygiene instructions (OHI) of adolescents receiving two-arch multibracket fixed appliances and identify its predictive factors.
Materials and Methods:
Forty-one patients in a longitudinal study were provided standardized OHI and assessed at baseline: before bonding (T0mo), approximately 30 days after bonding (T1mo), and approximately 150 days (T5mo) after bonding straight-wire appliances simultaneously in the maxillary and mandibular arches. Oral hygiene (OH) performance was measured using plaque and gingival indices. Compliance predictors were identified from questionnaires administered to patients and their parents and from patients' charts.
Results:
OH performance worsened from T0mo to T1mo but then improved from T1mo to T5mo. At T5mo, 73% of the sample had good OH. Univariate analyses found perceived severity of malocclusion, school performance, and parental marital status to be significant predictors of good OH performance at T5mo. Multiple logistic regressions identified having married parents and good academic performance in school as significant predictors.
Conclusions:
In the sample studied, after initially worsening, compliance with OHI improved at 5 months after bonding. Adolescents with married parents and those reporting good academic performance in school were found more likely to have complied with OHI provided at baseline and to perform better OH.
Keywords: Orthodontics, Oral hygiene, Compliance, Patient cooperation
INTRODUCTION
The insertion of multibracket fixed orthodontic appliances is associated with greater plaque build-up due to the difficulty in cleaning teeth, especially in the areas between brackets and around gingival margins.1 Plaque, if not removed, can lead to several adverse conditions, such as the occurrence of hyperplastic gingivitis, enamel decalcification and white spots, periodontal breakdown, and carious lesions.2 Continued plaque build-up may thus jeopardize the continuity and success of orthodontic treatment. It is estimated that 5%–10% of orthodontic patients do not complete treatment due to poor oral hygiene.3 Orthodontists routinely provide oral hygiene instructions (OHI) to their patients and motivate them to comply. This benefits patients during orthodontic treatment, and the benefits may continue well beyond orthodontic appliance removal.
Behavior, personality, and self-image are significantly developed during adolescence.4,5 However, stresses of adolescence make compliance more difficult. Compliance rates of long-term treatments have been reported to be as low as 50%,6,7 and orthodontic treatment also has been found to have such low compliance rates. To prevent adverse effects due to noncompliance, many studies have identified multiple demographic, psychosocial, psychologic, and behavioral factors to predict compliance.8 Demographic factors include gender, age, and socioeconomic status.7,8 Psychosocial and psychologic factors include the patients' personality traits; their relationship with their parents, peers, and the orthodontist; their performance in school; and external/internal locus of control.8,9 Behavioral factors (general and health related) are influenced by the psychologic and sociodemographic traits of the patients. Orthodontic treatment experience during the initial visits has also been considered a predictor for future compliance.10
Research on compliance with OHI in adolescent patients undergoing multibracket fixed orthodontic treatment is very limited, and variables predicting it are not well reported. This study was conducted to identify the level of compliance with OHI in adolescent patients scheduled to receive multibracket fixed appliances and identify the factors that predict it.
MATERIALS AND METHODS
After receiving approval from the research ethics board and obtaining informed consent from the participants and their parents, all 12- to 16-year-old healthy boys and girls who received two-arch fixed straight-wire orthodontic appliances (twin brackets) in the graduate orthodontic clinic at the Faculty of Dentistry, University of Toronto, during one academic year were followed during the course of the first 5 months of treatment. Patients were evaluated at baseline (T0mo; prior to appliance bonding), after approximately 30 days of bonding (T1mo), and then again after approximately 150 days of appliance bonding (T5mo). To be included, patients must have been able to perform their own OH activities. Patients with craniofacial anomalies or those with disabilities that restricted self-performed OH, or those scheduled to receive removable, functional, or self-ligating appliances were excluded. Of the 118 patients who fulfilled the age criterion, 41 patients (17 male, 24 female; mean age = 13.3 years, range 12–16 years) met the inclusion criteria and were included.
OH performance was measured objectively by the plaque index (PLI)11 and the gingival index (GI).12 The PLI and GI measure the thickness of the plaque accumulation and the severity and location of gingival inflammation, respectively. Both indices are objective, simple, and acceptable to patients.13 High levels of reliability in using both indices have been demonstrated in several studies.14,15 Four surface areas (buccal, mesial, lingual, distal) were examined on each of Ramfjord's six index teeth.16 Examination and recording of indices were performed at baseline T0mo, T1mo, and T5mo by the same investigator who had been trained and calibrated in the recording of PLI and GI in patients with and without fixed appliances. Standard OHI, which included verbal information on plaque, fixed appliances, and dietary advice, was given by the same investigator to each patient at the end of the T0mo PLI and GI recording appointment. Typodont demonstration of methods of plaque removal including brushing with a soft-bristled manual tooth brush and a fluoride-containing toothpaste, flossing, and using a Proxabrush were given. Each patient was also provided written information on OH maintenance and dietary advice. A clinical criterion based on experience in treating adolescent patients was proposed a priori and set at 20% of the maximum possible PLI score and 15% of the maximum possible GI score to distinguish patients with good compliance with OHI from those with poor compliance. Compliance with OHI has not been clearly defined in the literature. All patients had been provided the same OHI at baseline. This method therefore included those patients who improved their OH performance from baseline to this level by T5mo and those who may have maintained this level at both baseline and T5mo. A summary of the study procedures is presented in Table 1. Factors predicting compliance were obtained indirectly through questionnaires administered to the patients and their parents and by collecting data from the patients' charts. Each patient was asked to fill out two questionnaires (the first at T0mo, which asked about patient demographics, attitudes toward oral health, and current and past dental behavior; and the second at T5mo, which inquired about attitudes towards treatment, beliefs, psychologic, and psychosocial factors). Additionally, one parent of each patient was asked to provide family demographic information (eg, annual household income). Questionnaire items were adapted from different sources including the theory of reasoned action,17 orthodontic locus of control scale,18 need for peer approval scale (NPA),19 and the dental attitudes questionnaire.20 The questionnaires were pretested to assess their acceptability, ease of readability, and administration.
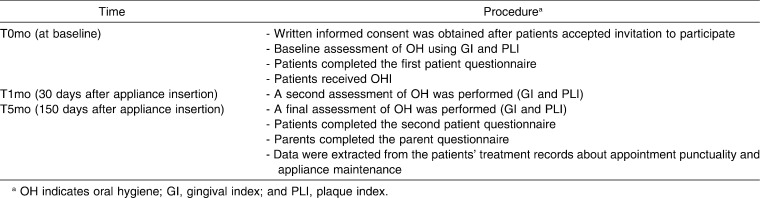
Table 1.
Study Procedures
Of the study variables, annual household income based on Statistics Canada's low income cut-off21 was categorized into “low” to describe incomes ≤$39,000, “middle” for incomes $40,000–$79,000, and “high” for incomes ≥$80,000. The history of patients' dental visits (excluding orthodontic visits) variable was categorized into, “within the last year” and “more than a year ago.” The appointment punctuality variable was obtained from the patients' charts and was defined as having attended all five scheduled orthodontic appointments during the study period: “Yes” if the patient attended all appointments (or cancelled and rescheduled before the day of the appointment), and “No” if the patient failed to show up or cancelled on the appointment day. The appliance maintenance variable was dichotomized into: “well maintained” to describe no broken brackets/bands and no or mild bends in the archwire, and “poorly maintained” to describe the presence of moderate to severe bends in the archwire and loose or broken brackets/bands. The patients' attitudes toward oral health were assessed at T0mo using a five-point Likert scale. Patients were asked about their attitudes towards brushing, flossing, periodic dental visits, and knowledge of poor oral health outcomes (tooth loss, gum bleeding). During the course of the treatment, the patients' attitudes toward wearing braces, the general health awareness, their interest in their teeth, the experience with follow-up appointments, and the perceived compliance with orthodontic instructions were recorded. Statements on internal and external locus of control,18 and reasoned action17 (behavioral beliefs, perceived behavioral control, and anticipated regret) were included. The self-reported school performance in the previous academic year variable was recorded into: “high” to describe those who obtained grade B or higher (70%–100%) according to the Ontario school grading system, and “low” to describe those who achieved grade C or lower (0%–69%). The NPA19 variable was assessed using nine (true or false) statements about the patients' feelings towards inclusions and approval by friends (eg, other children seldom ask my advice). The number of the total responses indicating an NPA was counted and ranged between 0 and 9. Higher scores suggested high NPA.
Data were analyzed using SPSS for Windows (version 15, SPSS Inc, Chicago, Ill). Descriptive statistics were initially conducted to explore the distribution of the data and to identify levels of OH at the three time points. Alpha factor analyses were conducted using Varimax rotation to reduce the number of attitude, psychologic, and psychosocial variables that were asked as part of the potential predictors of compliance in the two questionnaires. Univariate regression analysis was used to independently assess 23 potential predictors of compliance with OHI. Variables found to be significant at this level of analysis (P ≤ .05) and variables that were of borderline significance (P ≤ .1) were assessed simultaneously in a forward likelihood multiple logistic regression model. All statistical tests were two-tailed with 95% confidence intervals.
RESULTS
Analysis of the items inquired about in the questionnaires revealed the patients sought orthodontic treatment most frequently to straighten their teeth (73%) or to improve their facial appearance or profile (17%). Approximately 58% of the patients reported having performed well at school in the past year (Table 2). At baseline, 85% of the patients reported that they brushed their teeth more than once a day but only 46% used dental floss (Table 3). Eighty-five percent of the patients had received dental treatment in the preceding year. The most frequent reasons reported in the questionnaires for their dental visits were regular check-ups (56%), teeth cleaning (17%), tooth extraction (including teeth extracted for orthodontic purposes) (15%), and other reasons such as managing dental pain (12%). At T5mo, orthodontic appliance maintenance was deemed poor in over 50% of the patients, with each of these subjects having debonded at least one attachment by this time.
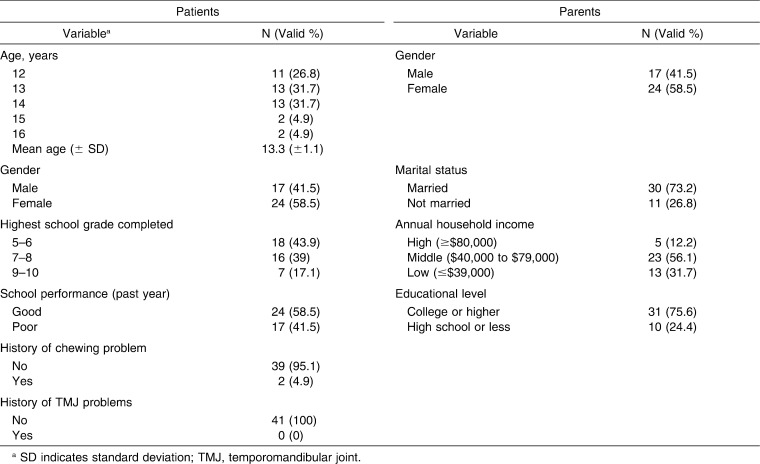
Table 2.
Sample Characteristics (N = 41)
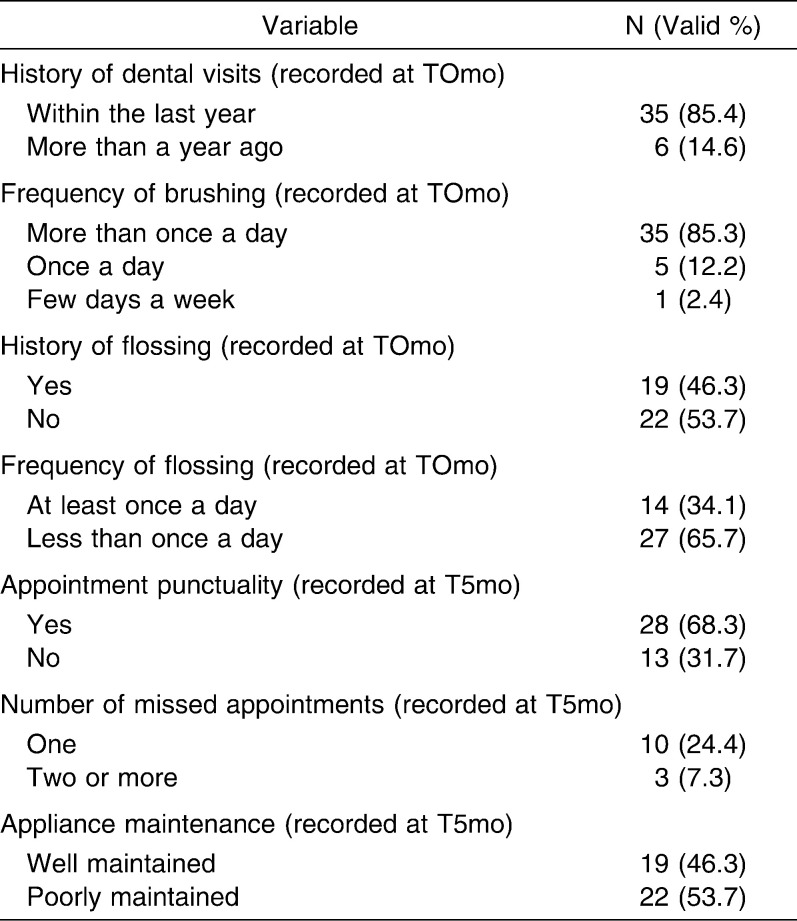
Table 3.
Oral Health Behavior of Adolescent Patients (N = 41)
Responses to the attitude statements asked at T0mo and T5mo showed that patients generally had positive attitudes towards oral health and their treatment. The patients' perceived severity of malocclusion revealed that 58% of the patients thought their teeth were somewhat crooked. Ninety percent of the patients indicated they had a good relationship with their orthodontist. Results of the NPA variable revealed that 93% of the patients scored between 0 and 4 out of 9 (mean ± SD = 2.3 ± 1.9). This indicated low NPA.
The first factor analysis reduced the attitude items in the first questionnaire to two factors. The first factor covered items related to brushing and flossing practices, and was therefore named “attitude toward oral health practices.” The second factor included items related to negative oral health outcomes and was labeled “attitudes toward poor oral health outcomes.” The second alpha-factor analysis of the categorical variables in the second questionnaire retained four factors: “relationship with orthodontist,” “general experience with follow-up appointments,” “locus of control,” and “planned behavior.” Retained factors in the first and second factor analyses accounted for 56% and 65% of the variability, respectively. Internal consistency of all items ranged from 0.6 to 0.9.
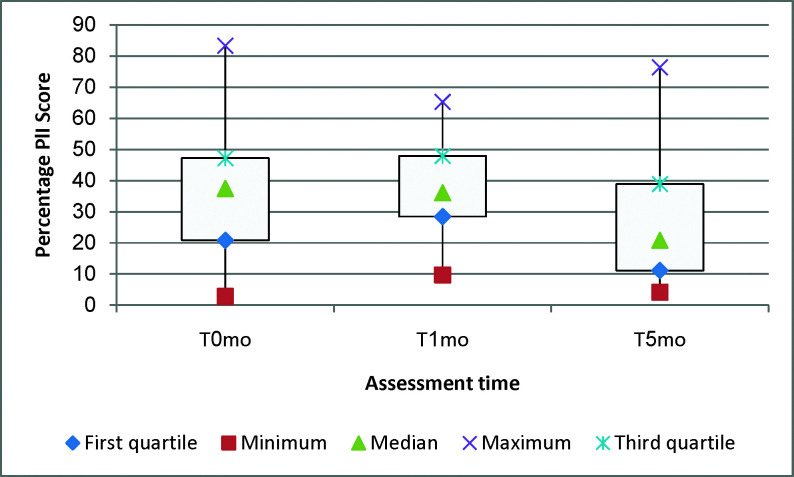
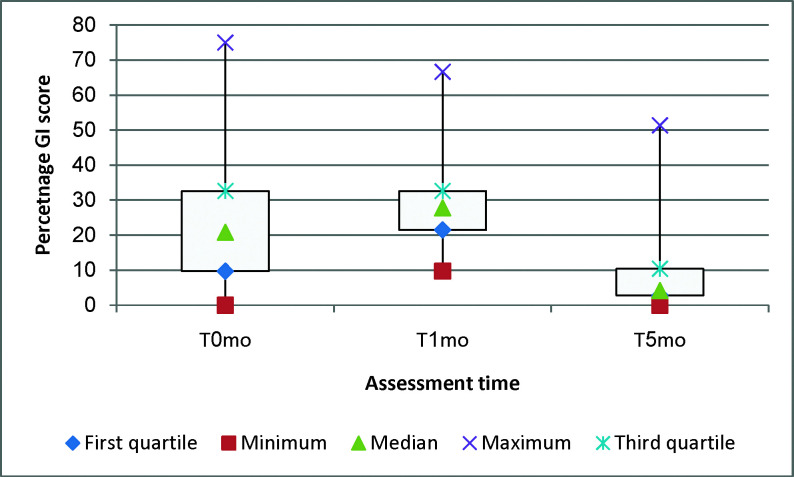
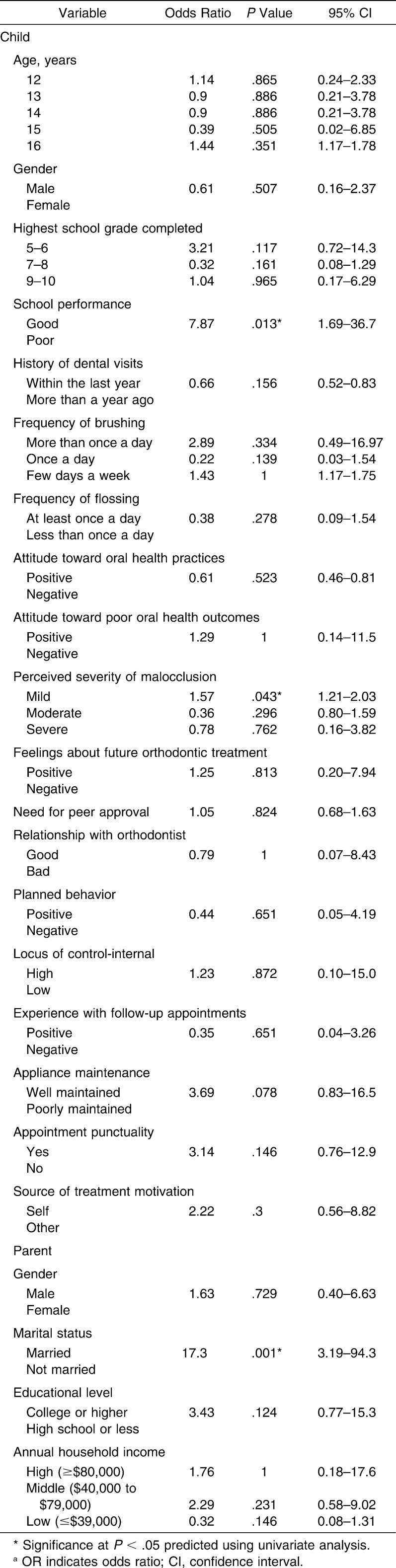
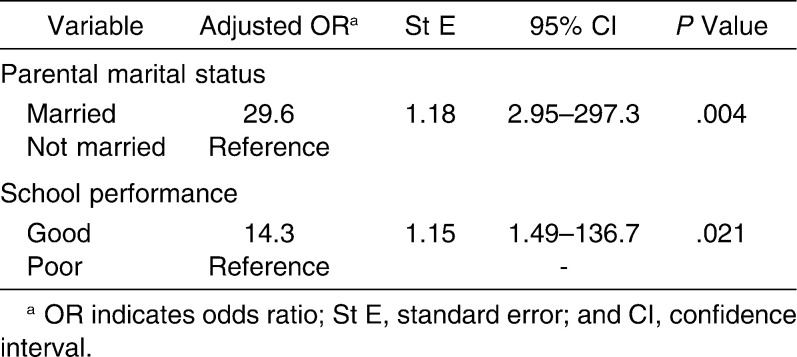
Figures 1 and 2 present the spread of the PLI and GI scores at T0mo, T1mo, and T5mo. Thirty patients who were classified as good compliers with OHI at T5mo by applying the criterion described earlier were compared to the 11 patients classified as poor compliers to identify predictors of compliance with OHI. The univariate analysis revealed three statistically significant variables: having achieved higher grades during the last academic year, perceived severity of malocclusion, and living in two-parent married families (Table 4). The multiple logistic regression model corroborated two variables to be significantly predictive of compliance (Table 5), having married parents and reporting good school performance in the past year. However, wide 95% confidence intervals were noted for the two significant variables.
Figure 1.
Distribution of PLI measurements at T0mo, T1mo, and T5mo.
Figure 2.
Distribution of GI measurements at T0mo, T1mo, and T5mo.
Table 4.
Univariate Regression Analyses of Compliance Levels With Oral Hygiene Instructions and Each Independent Variable
Table 5.
Predictive Multiple Logistic Regression Model of Compliance With Oral Hygiene Instructions During Fixed Orthodontic Treatment
DISCUSSION
Compliance in general remains a complex research topic, and evidence on factors predicting it is conflicting.10,22,23 Research on compliance with OHI during orthodontic treatment in particular is very limited. We found that OH performance of the sample in this longitudinal study first worsened within the first month of receiving fixed appliances but improved thereafter at T5mo, when 73% of the sample was assessed as having good OHI compliance. This improvement may be explained by the leveling and reduction in crowding commonly seen approximately 3 months into treatment, which have been shown to be associated with improved gingival health and OH.24 The Hawthorne effect may also have played a role as patients were aware they were being examined and evaluated, and this awareness could have influenced their behavior. This phenomenon indicates that study subjects' behavior can improve or get modified by their awareness that they are being observed as part of the study. Feil et al.6 studied the intentional use of the Hawthorne effect on OH compliance in orthodontic patients with history of poor OH in a 6-month single blinded quasi-randomized trial. They found significant improvement in OH compliance in the experimental group from their control group and significant quantitative differences between the two groups at the 3- and 6-month evaluation. They attributed the results to the Hawthorne effect. In addition, the repeated plaque and gingival index scoring may have served as a motivational factor. However, these factors were consistent for all patients, and perhaps made little impact on their performance at T1mo.
At T1mo, PLI and GI scores increased markedly, indicating poor OH performance. This is expected, since the initial period after bonding is associated with an increase in gingival bleeding in crowded dentitions.25 White26 described that pain and discomfort caused by the insertion of new appliances reduces the patients' initial acceptance of the appliances and worsens their OHI compliance. Also, in the present study, the T1mo evaluation was approximately 30 days after appliance bonding, at which time, they were still getting acquainted with their orthodontic appliance experience and the OH techniques required.
The multiple logistic regression model identified living with married parents and good school performance as significant predictors of good OH compliance. The small sample size probably contributed to the paucity of variables that could be isolated with confidence while maintaining a power of 80%. However, patients from two-parent families had 29 times higher odds to be compliant than patients from single-parent families. Earlier studies have shown that children of single-parent families have a higher risk of physical, social, and academic performance problems27,28 and also have a higher prevalence of dental caries and lower utilization of dental services than children of two-parent families.29 Good academic performers at school had 14 times higher odds to comply with the OHI. This factor has been explored in previous studies that found students with higher academic and social ratings by teachers,23 and higher grades were more compliant with orthodontic treatment than their scholastically lower grade achieving counterparts.8
This study was conducted on 12- to 16-year-old patients with straight-wire appliance twin brackets in a university setting, and 88% of the sample came from middle or low household income families. Our results may not be generalized to patients of other ages or those treated with other types of appliances or those from families with widely different incomes. Future studies should evaluate long-term compliance with OHI during orthodontic treatment, and extend the research question to study younger children and adults as well as other types of orthodontic appliances. Also, the ligation method in this study included one of the following: steel ties, elastomeric modules and/or chains applied at various stages of the treatment. Future studies could consider controlling for the ligation method.
CONCLUSIONS
OH performance worsened from the date of bonding to T1mo, but then improved significantly at T5mo.
Approximately 73% of the adolescent patients were assessed as good compliers with OHI when evaluated at T5mo.
At the univariate analysis level, perceived severity of malocclusion, school performance and parental marital status were found to be significant predictors of compliance with OHI.
Multiple logistic regression analysis identified living with married parents and good school performance as the two pretreatment predictors of compliance with OHI.
Acknowledgments
We thank James Leake, Jim Lai, and Derek Stephens for their advice; the Dental Research Institute at the Faculty of Dentistry, University of Toronto for partially funding the study; and the AAOF for the Eugene E. West Memorial Orthodontic Faculty Development Fellowship Award (2008) to Sunjay Suri during the time this work was undertaken.
REFERENCES
- 1.Alstad S, Zachrisson B. U. Longitudinal study of periodontal condition associated with orthodontic treatment in adolescents. Am J Orthod. 1979;76:277–286. doi: 10.1016/0002-9416(79)90024-1. [DOI] [PubMed] [Google Scholar]
- 2.Zachrisson B. U, Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Scand J Dent Res. 1971;79:394–401. doi: 10.1111/j.1600-0722.1971.tb02028.x. [DOI] [PubMed] [Google Scholar]
- 3.Mehra T, Nanda R. S, Sinha P. K. Orthodontists' assessment and management of patient compliance. Angle Orthod. 1998;68:115–122. doi: 10.1043/0003-3219(1998)068<0115:OAAMOP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Albino J. E, Lawrence S. D, Lopes C. E, Nash L. B, Tedesco L. A. Cooperation of adolescents in orthodontic treatment. J Behav Med. 1991;14:53–70. doi: 10.1007/BF00844768. [DOI] [PubMed] [Google Scholar]
- 5.Amado J, Sierra A. M, Gallon A, Alvarez C, Baccetti T. Relationship between personality traits and cooperation of adolescent orthodontic patients. Angle Orthod. 2008;78:688–691. doi: 10.2319/0003-3219(2008)078[0688:RBPTAC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Feil P. H, Grauer J. S, Gadbury-Amyot C. C, Kula K, McCunniff M. D. Intentional use of the Hawthorne effect to improve oral hygiene compliance in orthodontic patients. J Dent Educ. 2002;66:1129–1135. [PubMed] [Google Scholar]
- 7.Morris L. S, Schulz R. M. Patient compliance—an overview. J Clin Pharm Ther. 1992;17:283–295. doi: 10.1111/j.1365-2710.1992.tb01306.x. [DOI] [PubMed] [Google Scholar]
- 8.Sergel H. G, Zentner A. Predicting patient compliance in orthodontic treatment. Semin Orthod. 2000;6:231–236. [Google Scholar]
- 9.Nanda R. S, Kierl M. J. Prediction of cooperation in orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102:15–21. doi: 10.1016/0889-5406(92)70010-8. [DOI] [PubMed] [Google Scholar]
- 10.Albino J. E, Lawrence S. D, Lopes C. E, Nash L. B, Tedesco L. A. Cooperation of adolescents in orthodontic treatment. J Behav Med. 1991;14:53–70. doi: 10.1007/BF00844768. [DOI] [PubMed] [Google Scholar]
- 11.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 12.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 13.Bimstein E, Needleman H. L, Karimbux N, Van Dyke T. E. Periodontal and Gingival Health and Diseases children adolescents and young adults. London, UK: Martin Dunitz Ltd; 2001. [Google Scholar]
- 14.Eaton K. A, Rimini F. M, Zak E, Brookman D. J, Newman H. N. The achievement and maintenance of inter-examiner consistency in the assessment of plaque and gingivitis during a multicentre study based in general dental practices. J Clin Periodontol. 1997;24:183–188. doi: 10.1111/j.1600-051x.1997.tb00489.x. [DOI] [PubMed] [Google Scholar]
- 15.Kingman A, Loe H, Anerud A, Boysen H. Errors in measuring parameters associated with periodontal health and disease. J Periodontol. 1991;62:477–486. doi: 10.1902/jop.1991.62.8.477. [DOI] [PubMed] [Google Scholar]
- 16.Ramfjord S. P. Indices for prevalence and incidence of periodontal disease. J Periodontol. 1959;30:51–59. [Google Scholar]
- 17.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, New Jersey: Prentice Hall; 1980. [Google Scholar]
- 18.Wallston K. A, Wallston B. S. Health locus of control scales. In: Lefcourt H, editor. Research With the Locus of Control Construct Vol 1. New York, NY: Academic Press; 1981. [Google Scholar]
- 19.Lewit D. W, Virolainen K. Conformity and independence in adolescents' motivation for orthodontic treatment. Child Dev. 1968;39:1188–2000. [PubMed] [Google Scholar]
- 20.Bos A, Hoogstraten J, Prahl-Andersen B. A comparison of dental health care attitudes in the Netherlands in 1985, 1995, and 2001. Community Dent Oral Epidemiol. 2003;31:207–212. doi: 10.1034/j.1600-0528.2003.00038.x. [DOI] [PubMed] [Google Scholar]
- 21.Statistics Canada Low Income Cut-offs for 2006 and Low Income Measures for 2005. 2008 Statistics Canada, Income Research Paper Series, Catalogue no. 75F0002MIE – No. 004. [Google Scholar]
- 22.Sergel H. G, Klages U, Pempera J. On the prediction of dentist-evaluated patient compliance in orthodontics. Eur J Orthod. 1992;14:463–468. doi: 10.1093/ejo/14.6.463. [DOI] [PubMed] [Google Scholar]
- 23.Woolass K. F, Shaw W. C, Viader P. H, Lewis A. S. The prediction of patient co-operation in orthodontic treatment. Eur J Orthod. 1988;10:235–243. doi: 10.1093/ejo/10.3.235. [DOI] [PubMed] [Google Scholar]
- 24.Glans R, Larsson E, Ogaard B. Longitudinal changes in gingival condition in crowded and noncrowded dentitions subjected to fixed orthodontic treatment. Am J Orthod Dentofacial Orthop. 2003;124:679–682. doi: 10.1016/j.ajodo.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Addy M, Griffiths G. S, Dummer P. M, Kingdon A, Hicks R, Hunter M. L, Newcombe R. G, Shaw W. C. The association between tooth irregularity and plaque accumulation, gingivitis, and caries in 11-12-year-old children. Eur J Orthod. 1988;10:76–83. doi: 10.1093/ejo/10.1.76. [DOI] [PubMed] [Google Scholar]
- 26.White L. W. A new paradigm of motivation. J Clin Orthod. 1996;30:337–341. [PubMed] [Google Scholar]
- 27.Judge K, Benzeval M. Health inequalities: new concerns about the children of single mothers. BMJ. 1993;306:677–680. doi: 10.1136/bmj.306.6879.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moilanen I, Rantakallio P. The single parent family and the child's mental health. Soc Sci Med. 1988;27:181–186. doi: 10.1016/0277-9536(88)90327-9. [DOI] [PubMed] [Google Scholar]
- 29.Whittle J. G. Attendance patterns and dental health of parents and children. Community Dent Health. 1993;10:235–242. [PubMed] [Google Scholar]