Abstract
Objective:
To investigate the upper airways for anteroposterior width against different growth patterns and for alterations during various Class II treatments.
Materials and Methods:
Cephalograms from three treatment groups (headgear, activator, and bite-jumping appliance) were evaluated by a single investigator at baseline and at the end of orthodontic treatment. Cephalograms were used to determine upper airway width at different levels in the anteroposterior plane. Patients in the headgear group were additionally divided into six subsets on the basis of y-axis values to assess the influence of different growth patterns.
Results:
Small increases in pharyngeal width were noted at all vertical level segments, both at baseline and during orthodontic treatments. No significant differences in these small increases were noted across various treatment modalities and growth patterns.
Conclusion:
Upper airway changes did not significantly vary with the different treatment modalities investigated in the present study. Nevertheless, reductions in pharyngeal width potentially triggering or exacerbating obstructive sleep apnea syndrome (OSAS) are always possible in the headgear phase.
Keywords: Headgear, Growth pattern, Cephalometric analysis, Posterior airway space
INTRODUCTION
Along with exogenous factors such as alcohol or sedatives, the occurrence of the obstructive sleep apnea syndrome (OSAS) is favored by anatomic and pathologic alterations in the area of the upper airways.1 Thanks to its three-dimensional representation of anatomic structures, computed tomography (CT) is considered an excellent diagnostic tool to evaluate the width of the upper airways (along with magnetic resonance imaging). This width has been shown to correlate with the severity of OSAS.2
As far back as 1986, Riley et al.3 demonstrated a correlation between assessments based on CT scans and assessments based on cephalograms, which led them to conclude that the latter was appropriate for basic diagnostic purposes. More recently, some authors reported differences in anteroposterior distances in the pharyngeal space between patients with and without demonstrated OSAS at different vertical levels.4–11 Cephalography could be used to quantify successful treatments for OSAS by measures such as surgical advancement of the jaw (especially the mandible),6,12–16 surgical advancement of the geniohyoid muscle attachment,15,17,18 continuous positive airway pressure (cPAP) treatment,10 adenotomy,19 or advancement appliances.5
The limitations of analysis made themselves felt in the presence of specific muscle or hormonal diseases,20,21 or when attempts were made to predict OSAS on the basis of these values.22 However, patients with OSAS frequently showed other characteristics in connection with pharyngeal narrowness, including a retrognathic jaw position, dolichocephalic architecture of the facial skull, and a caudal position of the hyoid bone,1 such that the width of the pharyngeal space became relevant to a number of different orthodontic issues and treatments.23–25 With regard to prognathism, various study groups7,26–29 demonstrated increases in nasopharyngeal and oropharyngeal width during treatment with a maxillary expansion appliance and facemask. In skeletal Class II cases, pharyngeal narrowing was visible, especially the root-of-tongue level, which improved during treatment with functional orthodontic appliances.30 Hinz31 investigated children with abnormal sleeping patterns, finding that more of them required orthodontic than ear, nose, and throat (ENT) treatment and recommended that special attention should be paid in this respect.
A case was made against the use of a cervical headgear to treat Class II patients with OSAS after polysomnography showed that this approach was associated with exacerbation of the OSAS.32 On the other hand, Kirjavainen et al.33 investigated isolated treatments of skeletal Class II with a cervical headgear over a mean of 1.6 years, demonstrating only minor changes both regarding the initially higher values of the nasopharynx and regarding the initially lower values at the root-of-tongue level. As a rule, however, orthodontic treatment is not completed following the use of a cervical headgear; it will commonly involve a subsequent phase with a multibracket appliance and a phase of retention. It is therefore of clinical interest to obtain information about pharyngeal width during headgear-supported orthodontic treatment, particularly in connection with a risk assessment concerning the potential development of OSAS due to pharyngeal narrowness. Back in 1994, Hochban9 identified vertical growth patterns as a risk factor for OSAS, along with retrognathism. This prompted us to investigate whether pharyngeal narrowness should be expected in the presence of vertical growth patterns.
MATERIALS AND METHODS
The headgear group was compiled from the records of 209 patients available at a private orthodontic office. Patients with a history of sleep disorders were excluded from the study. All treatments involved a protocol with initial documentation based on casts and radiographs (lateral cephalograms and panoramic radiographs), followed by isolated headgear treatment for at least 6 months. The cervical headgear featured a nonangulated outer bow and an elastic strap. Traction force was adjusted to 350 to 400 g bilaterally, which improved Class II occlusal relations of the first molars by a minimum of 4 mm. Once the desired occlusal relation was established, the wearing cycle was reduced from 14 hours a day to overnight. Following complete eruption of the premolars and canines, intermediary documentation was collected and therapy continued by complete multibracket treatment and retentive treatment, including removable plates and fixed retainers.
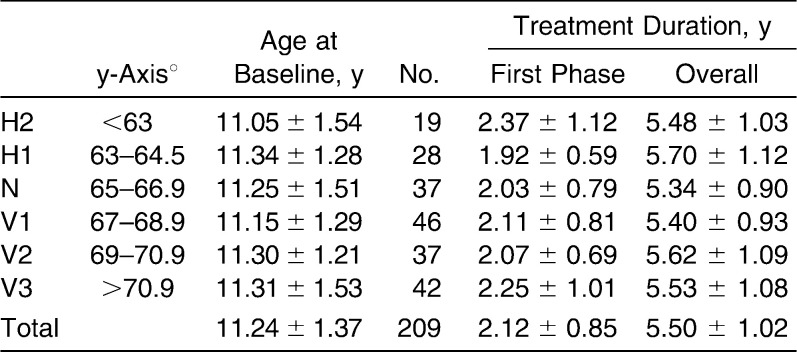
To appreciate the effects of growth patterns, patients in the headgear group were divided into six subgroups on the basis of y-axis values (Table 1).34,35
Table 1.
Overview of Subgroups Defined Within the Headgear Group of Patients
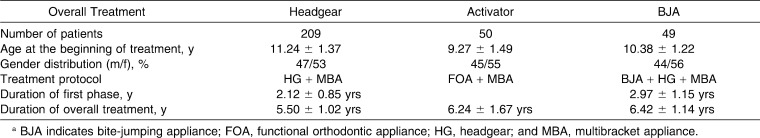
Patients treated with an activator and others treated with a bite-jumping appliance (BJA) were used for comparison with headgear-based treatment (ie, the headgear group as the total patient sample of subsets H2 to V3). The activator group included skeletal Class I and II patients who had been treated by an experienced orthodontist first using an activator as described by Andresen et al.36 and then a multibracket appliance, followed by a retention phase with removable plates and fixed retainers. The group treated with a BJA included cases that were consecutively retrieved by the same criteria and at the same orthodontic office as the headgear cases, the only difference being that these patients had received their BJA before receiving isolated headgear treatment (Table 2).
Table 2.
Overview of Demographic Data Across the Three Treatment Groupsa
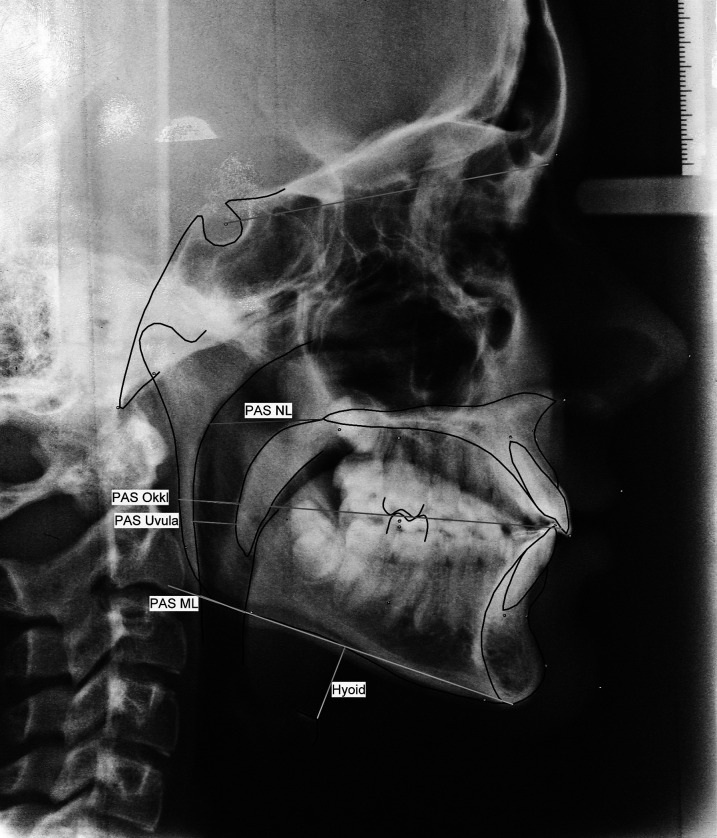
Analysis of the cephalograms was based on pharyngeal anteroposterior width and on sagittal (SNA, SNB) and vertical (y-axis) parameters (Figure 1). We determined the pharyngeal anteroposterior width at several vertical levels and refer to the majority of currently available studies5,23–28,33,37 as the “PAS (posterior airway space)” of each level. As an additional parameter, we evaluated the distance from the anterosuperior point to the mandibular base.1,9,33
Figure 1.
Overview of measured distances and angles.
To draw conclusions about the effects of various orthodontic treatments on the upper airways, a Tukey-Kramer test for multiple unconnected samples of different sizes was applied to compare baseline values obtained before treatment started vs subsequent measurements, thus evaluating alterations in the three main groups (activator, headgear, and BJA) during the first treatment phase and over the entire course of orthodontic treatment. No intermediate documents were produced for the activator group, meaning that no data were available for the first part of the treatment. Results were analyzed with JMP 7.0 statistics software (SAS Institute Inc., Cary, NC), and the level of significance was set to .05. Significant intergroup differences are represented by the characters “>” and “<” in the event tables provided (Tables 3 and 4). The same method was used for intergroup comparison of various subsets within the headgear group.
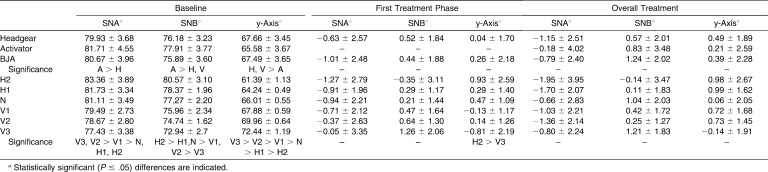
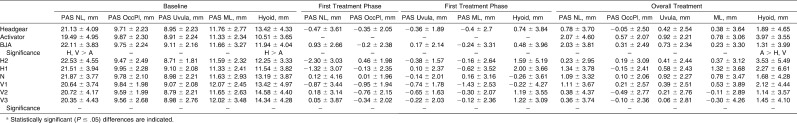
Table 3.
Results Obtained in the Three Treatment Groups (Headgear, Activator, Bite-Jumping Appliance) and Within the Growth Pattern–Related Subsets of the Headgear Group (HG) at the Outset of Treatmenta
Table 4.
Changes Observed in the Three Treatment Groups (Headgear, Activator, Bite-Jumping Appliance) and Within the Growth Pattern–Related Subsets of the Headgear Group (HG) During the First Treatment Phase and Over the Entire Course of Orthodontic Treatmenta
To calculate the measurement error, 30 cephalograms were evaluated twice by the same investigator at biweekly intervals or at longer intervals to avoid memory effects, using the formula sw2 = Σ di2/2n, introduced by Dahlberg.38 The values obtained were consistently less than 1 mm or 1 degree, the only exception with slightly higher values being the SNA (1.03 degrees) and SN-MeGo (1.08 degrees) angles.
RESULTS
Findings for the skeletal parameters (SNA, SNB, y-axis) were consistent with the typical results of Class II treatment obtained via various treatment concepts. Differences turned out to be small and did not reach the level of statistical significance. Those obtained for the first treatment phase for the headgear group divided on the basis of the y-axis were described previously.35 After that, reductions in SNA angles would diminish in the presence of progressively vertical growth patterns, SNB angles would increase more markedly, and y-axis angles would increase less markedly. Over the entire course of treatment, these differences were no longer found to be as pronounced (Table 3).
The nasopharynx was the only level (PAS NL) at which the upper airway widths in the activator group were significantly smaller than in the other groups at baseline; no such differences were observed at any of the other levels (Table 4). Also, increasingly lower values were obtained in the nasopharynx, with growth patterns exhibiting a more vertical orientation. At all other levels, the differences were minor.
During the first treatment phase, anteroposterior widths were found to be reduced at all levels in the headgear group. This finding was not related to different growth patterns. The preceding use of a BJA was effective in reducing this effect and in partially reversing it. However, no statistically significant difference was noted between groups.
In all treatment groups, increases in anteroposterior width were largest in the nasopharynx, and gains noted at all other levels averaged less than 1 mm throughout the entire treatment period of 5.2 to 6.4 years; within the activator group, the largest gains were recorded in the oropharynx. Distances from hyoid to mandibular base (hyoid) were significantly smaller in the activator group at baseline but then increased significantly more during treatment, such that intergroup differences in this respect were reduced to a minimum by the end of treatment.
Just as in the headgear group at large, upper airway widths (PAS NL = posterior airway space at nasal line; PAS OccPl = PAS Occlusion plane; PAS Uvula/PAS ML = PAS mandibular line) in the subgroups did not show an apparent trend related to growth patterns.
DISCUSSION
Hochban et al.1,8 investigated a series of adult patients with OSAS and identified a number of risk factors detectable on cephalograms (retrognathism, vertical growth pattern, caudal length of hyoid). The present study does not support the proposed correlation with pharyngeal anteroposterior width as measured at different vertical levels. In the BJA group with marked retrognathism (SNB <76 degrees) and vertically biased growth patterns, some of the values obtained for pharyngeal width even exceeded those obtained in the activator group without retrognathism. This statement also applies to growth patterns. The pharynx (except for the nasopharynx) was not narrower in the vertical than in the horizontal subset of the headgear group. This finding was demonstrated by Zhong et al.25 Two points can be made to explain this lack of agreement with the finding by Hochban et al.1,8
One point is that both Zhong et al.25 and the present authors investigated adolescents who did not have any known histories of OSAS, whereas Hochban et al.1,8 based their results on adults with diagnosed OSAS. The second point seems to be more important. As long ago as 1983, Riley et al.22 stated that it was impossible to prognosticate OSAS on the basis of cephalograms. Regarding the important question of dimensional changes in the pharyngeal area within the overall context of orthodontic treatment, only minor changes were observed, and even the differences noted between various treatment modalities were small.
These observations appear to be in contrast with those made by Özbek et al.,30 who reported that values would markedly increase during functional orthodontic treatment—by 2.15 mm at the uvula, and by 1.87 mm at the mandibular border, in comparison with an untreated control group. This apparent contradiction can be explained, however, by different treatment periods. The dimensional increases noted by Özbek et al.30 occurred within 1.5 years of active treatment, and overall treatment periods in the present investigation ranged from 5.2 to 6.4 years and involved smaller changes due to ongoing growth in the facial skull. Dimensional increases were most pronounced with very short-term treatment measures such as surgical advancement of one or both jaws2,12,16 or temporary use of an advancement appliance.39
The very small increases in pharyngeal width noticed in the oropharynx across all three treatment groups (not involving any significant intergroup differences) were in the range demonstrated by Kirjavainen and Kirjavainen33 on the basis of cross-sectional data. It can be concluded that Class II treatment of these patients, for whom no sleep-related breathing disorders were on record, had no or only minor effects on anteroposterior pharyngeal width. Different growth patterns were not shown to be a crucial factor.
In the nasopharynx, however, only the values of the activator group and the group that included a BJA were in the range of the cross-sectional data. Smaller increases observed in the headgear group can be explained by the distalizing force exerted by the cervical headgear. In the first treatment phase (isolated headgear treatment), more pronounced effects of the cervical headgear were obtained in terms of pharyngeal width reductions, not only in the nasopharynx but also at all other levels. These reductions are consistent with the observations made by Pirilä-Parkkinen et al.,32 who reported exacerbation of preexisting OSAS during treatment with a cervical headgear in the presence of significant mandibular retrusion. On the basis of this finding, they cautioned against using a cervical headgear in this situation. Kirjavainen and Kirjavainen,33 by contrast, did not demonstrate a pattern of pharyngeal width reductions in their sample of patients (also excluding known histories of OSAS) during headgear treatment. To summarize, a reduction in pharyngeal width must be expected, which might exacerbate any preexisting OSAS, or might result in decompensation of compensated OSAS. In this event, therapy should be interrupted and a switch made to other treatment modalities.
The functional orthodontic pretreatment applied in the BJA group was capable of diminishing width reductions, even eliminating them. No part of the results was shown to be influenced by different growth patterns.
CONCLUSIONS
Dimensional changes in the pharyngeal area within the overall context of orthodontic treatment were only minor, and even the differences noted between various treatment modalities were small.
Pharyngeal width reductions can occur in the phase of isolated headgear treatment. They may exacerbate any preexisting OSAS or may result in decompensation of compensated OSAS.
Pretreatment with a BJA can reduce headgear-related reductions in pharyngeal width.
REFERENCES
- 1.Hochban W, Brandenburg U, Peter J. H. Chirurgische Therapiemöglichkeiten der obstruktiven Schlafapnoe mittels Ober-und Unterkieferosteotomie. Fortschr Kiefer Gesichtschir. 1995;40:65–72. [PubMed] [Google Scholar]
- 2.Abramson Z, Susarla S, August M, Troulis M, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy in patients with obstructive sleep apnea. J Oral Maxillofac Surg. 2010;68:354–362. doi: 10.1016/j.joms.2009.09.087. [DOI] [PubMed] [Google Scholar]
- 3.Riley R, Powell N, Guilleminault C. Cephalometric roentgenograms and computerized tomographic scans in obstructive sleep apnea. Sleep. 1986;9:514–515. doi: 10.1093/sleep/9.4.514. [DOI] [PubMed] [Google Scholar]
- 4.deBerry-Borowieki B, Kukwa A, Banks R. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope. 1988;98:226–230. doi: 10.1288/00005537-198802000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Doff M. H, Hoekema A, Pruim G. J, van der Hoeven J. H, de Bont L. G, Stegenga B. Effects of a mandibular advancement device on the upper airway morphology: a cephalometric analysis. J Oral Rehabil. 2009;36:330–337. doi: 10.1111/j.1365-2842.2009.01946.x. [DOI] [PubMed] [Google Scholar]
- 6.Farole A, Mundenar M. J, Braitman L. E. Posterior airway changes associated with mandibular advancement surgery: implications for patients with obstructive sleep apnea. Int J Adult Orthodon Orthognath Surg. 1990;5:255–258. [PubMed] [Google Scholar]
- 7.Hiyama S, Suda N, Ishii-Suzuki M, Tsuiki S, Ogawa M, Suzuki S, Kuroda T. Effects of maxillary protraction on craniofacial structures and upper-airway dimension. Angle Orthod. 2002;72:43–47. doi: 10.1043/0003-3219(2002)072<0043:EOMPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Hochban W, Brandenburg U. Morphology of the viscerocranium in obstructive sleep apnoea syndrome—cephalometric evaluation of 400 patients. J Craniomaxillofac Surg. 1994;22:205–213. doi: 10.1016/s1010-5182(05)80559-1. [DOI] [PubMed] [Google Scholar]
- 9.Hochban W, Brandenburg U, Peter J. H. Surgical treatment of obstructive sleep apnea by maxillomandibular advancement. Sleep. 1994;17:624–629. doi: 10.1093/sleep/17.7.624. [DOI] [PubMed] [Google Scholar]
- 10.Kiely J. L, Deegan P. C, McNicholas W. T. Resolution of obstructive sleep apnea with growth in the Robin sequence. Eur Respir J. 1998;12:499–501. doi: 10.1183/09031936.98.12020499. [DOI] [PubMed] [Google Scholar]
- 11.Partinen M, Guilleminault C, Quera-Salva M, et al. Obstructive sleep apnea and cephalometric roentgenograms: the role of anatomic upper airway abnormalities in the definition of abnormal breathing during sleep. Chest. 1988;93:1199. doi: 10.1378/chest.93.6.1199. [DOI] [PubMed] [Google Scholar]
- 12.Conradt R, Hochban W, Brandenburg U, Heitmann J, Peter J. H. Long-term follow-up after surgical treatment of obstructive sleep apnoea by maxillomandibular advancement. Eur Respir J. 1997;10:123–128. doi: 10.1183/09031936.97.10010123. [DOI] [PubMed] [Google Scholar]
- 13.Kunkel M, Hochban W. The influence of maxillary osteotomy on nasal airway patency and geometry. Mund Kiefer Gesichtschir. 1997;1:194–198. doi: 10.1007/BF03043550. [DOI] [PubMed] [Google Scholar]
- 14.Lee K. W. Effect of orthognathic surgery on the posterior airway space (PAS) Ann Acad Med Singapore. 2008;37:677–682. [PubMed] [Google Scholar]
- 15.Riley R, Powell N, Guilleminault C. Current surgical concepts for treating obstructive sleep apnea syndrome. J Oral Maxillofac Surg. 1987;45:149–157. doi: 10.1016/0278-2391(87)90405-8. [DOI] [PubMed] [Google Scholar]
- 16.Riley R. W, Powell N. B, Guillemblault C. Maxillary, mandibular, and hyoid advancement for treatment of obstructive sleep apnea: a review of 40 patients. J Oral Maxillofac Surg. 1990;48:20–26. doi: 10.1016/0278-2391(90)90174-z. [DOI] [PubMed] [Google Scholar]
- 17.Riley R. W, Powell N. B, Guillemblault C. Inferior mandibular osteotomy and hyoid myotomy suspension for obstructive sleep apnea: a review of 55 patients. J Oral Maxillofac Surg. 1989;47:159–164. doi: 10.1016/s0278-2391(89)80109-0. [DOI] [PubMed] [Google Scholar]
- 18.Li K. K, Powell N. B, Riley R. W, Troell R, Guilleminault C. Overview of phase I surgery for obstructive sleep apnea syndrome. Ear Nose Throat J. 1999;78:854–857. [PubMed] [Google Scholar]
- 19.Woodside D. G, Linder-Aronson S, Lundstrom A, McWilliam J. Mandibular and maxillary growth after changed mode of breathing. Am J Orthod Dentofacial Orthop. 1991;100:1–18. doi: 10.1016/0889-5406(91)70044-W. [DOI] [PubMed] [Google Scholar]
- 20.Della Marca G, Pantanali F, Frusciante R, et al. Cephalometric findings in facioscapulohumeral muscular dystrophy patients with obstructive sleep apneas. Sleep Breath. 2010 Feb 20 doi: 10.1007/s11325-010-0330-y. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Hochban W, Ehlenz K, Conradt R, Brandenburg U. Obstructive sleep apnoea in acromegaly: the role of craniofacial changes. Eur Respir J. 1999;14:196–202. doi: 10.1034/j.1399-3003.1999.14a33.x. [DOI] [PubMed] [Google Scholar]
- 22.Riley R, Guilleminault C, Herran J, Powelh N. Cephalometric analysis and flow-volume loops in obstructive sleep apnea patients. Sleep. 1983;6:303–311. doi: 10.1093/sleep/6.4.303. [DOI] [PubMed] [Google Scholar]
- 23.Jena A. K, Singh S. P, Utreja A. K. Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage. Angle Orthod. 2010;80:1061–1067. doi: 10.2319/030210-125.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valiathan M, El H, Hans M. G, Palomo M. J. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010;80:1068–1074. doi: 10.2319/010810-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhong Z, Tang Z, Gao X, Zeng X. L. A comparison study of upper airway among different skeletal craniofacial patterns in nonsnoring Chinese children. Angle Orthod. 2010;80:267–274. doi: 10.2319/030809-130.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaygisiz E, Tuncer B. B, Yüksel S, Tuncer C, Yildiz C. Effects of maxillary protraction and fixed appliance therapy on the pharyngeal airway. Angle Orthod. 2009;79:660–667. doi: 10.2319/072408-391.1. [DOI] [PubMed] [Google Scholar]
- 27.Kılınc A. S, Arslan S. G, Kama J. D, Ozer T, Darı O. Effects on the sagittal pharyngeal dimensions of protraction and rapid palatal expansion in Class III malocclusion subjects. Eur J Orthod. 2008;30:61–66. doi: 10.1093/ejo/cjm076. [DOI] [PubMed] [Google Scholar]
- 28.Oktay H, Ulukaya E. Maxillary protraction appliance effect on the size of the upper airway passage. Angle Orthod. 2008;78:209–214. doi: 10.2319/122806-535.1. [DOI] [PubMed] [Google Scholar]
- 29.Sökücü O, Doruk C, Uysal ÖI. Comparison of the effects of RME and fan-type RME on nasal airway by using acoustic rhinometry. Angle Orthod. 2010;80:870–875. doi: 10.2319/120309-694.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Özbek M. M, Memikoglu T. U. T, Gogen H, Lowe A. A, Caspian E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327–336. doi: 10.1043/0003-3219(1998)068<0327:OADAFO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Hinz R. Differenzialdiagnose bei organisch bedingten schlafbezogenen Atmungsstörungen bei Kindern. J Orofac Orthop. 2008;69:497. [Google Scholar]
- 32.Pirilä-Parkkinen K, Pirttiniemi P, Nieminen P, Löppönen H, Tolonen U, Uotila R, Huggare J. Cervical headgear therapy as a factor in obstructive sleep apnea syndrome. Pediatr Dent. 1999;21:39–45. [PubMed] [Google Scholar]
- 33.Kirjavainen M, Kirjavainen T. Upper airway dimensions in Class II malocclusion: effects of headgear treatment. Angle Orthod. 2007;77:1046–1053. doi: 10.2319/081406-332. [DOI] [PubMed] [Google Scholar]
- 34.Godt A, Berneburg M, Kalwitzki M, Göz G. Bewegung der Molaren und Frontzähne im Rahmen einer zervikalen Headgeartherapie in Relation zum Wachstumsmuster—eine Fernröntgenseitenbildanalyse. J Orofac Orthop. 2008;69:189–200. [Google Scholar]
- 35.Godt A, Kalwitzki M, Göz G. Zervikaler Headgear in Relation zum Wachstumsmuster—eine Fernröntgenseitenbildanalyse. J Orofac Orthop. 2007;68:38–46. [Google Scholar]
- 36.Andresen V, Häupl K, Petrik L. Funktionskieferorthopädie. München, Germany: Johann Ambrosius Barth; 1957. [Google Scholar]
- 37.Muto T, Yamazaki A, Takeda S. A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int J Oral Maxillofac Surg. 2008;37:228–231. doi: 10.1016/j.ijom.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 38.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: Allen and Unwin; 1940. pp. 122–132. [Google Scholar]
- 39.Piskin B, Sentut F, Sevketbeyoglu H, Avsever H, Gunduz K, Kose M, Oguz D, Uyar S. Efficacy of a modified mandibular advancement device for a totally edentulous patient with severe obstructive sleep apnea. Sleep Breath. 2010;14:81–85. doi: 10.1007/s11325-009-0273-3. [DOI] [PubMed] [Google Scholar]