Summary
Background
Several countries now have mandatory SARS-CoV-2 vaccination for healthcare workers (HCWs) or the general population. HCWs’ views on this are largely unknown. Using data from the nationwide UK-REACH study we aimed to understand UK HCW's views on improving SARS-CoV-2 vaccination coverage, including mandatory vaccination.
Methods
Between 21st April and 26th June 2021, we administered an online questionnaire via email to 17 891 UK HCWs recruited as part of a longitudinal cohort from across the UK who had previously responded to a baseline questionnaire (primarily recruited through email) as part of the United Kingdom Research study into Ethnicity And COVID-19 outcomes in Healthcare workers (UK-REACH) nationwide prospective cohort study. We categorised responses to a free-text question “What should society do if people do not get vaccinated against COVID-19?” using qualitative content analysis. We collapsed categories into a binary variable: favours mandatory vaccination or not, using logistic regression to calculate its demographic predictors, and its occupational, health, and attitudinal predictors adjusted for demographics.
Findings
Of 5633 questionnaire respondents, 3235 answered the free text question. Median age of free text responders was 47 years (IQR 36–56) and 2705 (74.3%) were female. 18% (n = 578) favoured mandatory vaccination (201 [6%] participants for HCWs and others working with vulnerable populations; 377 [12%] for the general population), but the most frequent suggestion was education (32%, n = 1047). Older HCWs (OR 1.84; 95% CI 1.44–2.34 [≥55 years vs 16 years to <40 years]), HCWs vaccinated against influenza (OR 1.49; 95% CI 1.11–2.01 [2 vaccines vs none]), and with more positive vaccination attitudes generally (OR 1.10; 95% CI 1.06–1.15) were more likely to favour mandatory vaccination, whereas female HCWs (OR= 0.79, 95% CI 0.63–0.96, vs male HCWs) and Black HCWs (OR=0.46, 95% CI 0.25–0.85, vs white HCWs) were less likely to.
Interpretation
Only one in six of the HCWs in this large, diverse, UK-wide sample favoured mandatory vaccination. Building trust, educating, and supporting HCWs who are hesitant about vaccination may be more acceptable, effective, and equitable.
Funding
MRC-UK Research and Innovation grant (MR/V027549/1) and the Department of Health and Social Care (DHSC) via the National Institute for Health Research (NIHR). Core funding was also provided by NIHR Biomedical Research Centres.
Research in context.
Evidence before this study
We searched the Pubmed database using the following search terms: ((vaccine OR vaccination OR immunisation) AND (Covid-19 OR Covid OR SARS-CoV-2 OR coronavirus) AND (healthcare worker OR health worker OR doctor OR nurse OR healthcare professional) AND (mandatory OR compulsory) AND (views OR opinions OR attitudes OR thoughts)), restricting the search to articles published between 1st January 2002 and 11th January 2022.
There were nine relevant studies, all cross-sectional surveys, and all but one found that around half or more of participants (HCWs or medical students from outside the UK) agreed with mandatory vaccination for HCWs. Lower agreement with mandatory vaccination was strongly associated with vaccine hesitancy and was associated with being in a non-medical (doctor) professional group.
Added value of this study
This is the largest study of HCW's views on strategies to address sub-optimal vaccine coverage, including mandatory vaccination. It is the only study from the UK, where a mandatory vaccination policy for most staff was voted into law on 6th January 2022 and then paused on 8th February 2022 subject to a Parliamentary consultation. One in six HCWs in our study favoured mandatory vaccination but twice as many favoured education and support. Mandatory vaccination was much less likely to be favoured among those hesitant about vaccination and among groups with lower vaccine uptake including HCWs of Black and Asian ethnicity.
Implications of all the available evidence
A mandatory vaccination policy could exacerbate existing inequalities among HCWs in England and add to workforce shortages. Greater efforts should be made to improve trust in vaccines to increase coverage.
Alt-text: Unlabelled box
Introduction
Vaccines against Coronavirus disease 2019 (COVID-19) were approved for emergency use in the United Kingdom (UK) in December 2020 and since then have been offered in a staggered manner to everyone aged 12 years and over.1 Figures released by the UK Government show that by 6th January 2022, 92% of adults in England had their first dose of a COVID-19 vaccine, 88% had a second dose and 68% had a booster or third dose.2 While these figures look promising, they mask considerable variations in vaccination uptake by region and demographics,3 with vaccine uptake lower in certain ethnic groups, among women, and in younger groups.4,5 This patterning of vaccine uptake is also observed among healthcare workers (HCWs).2,6
With COVID-19 cases surging and the emergence of the Omicron variant of concern, Italy, Greece and France have made COVID-19 vaccine compulsory for HCWs,7,8 and Austria and Greece have made vaccinations mandatory for the general population.9,10 The United States of America (USA) has mandated COVID-19 vaccination for all federal employees including healthcare personnel.11 In England, COVID-19 vaccination was made mandatory for social care workers in November 2021, and was due to become mandatory for HCWs working in other healthcare settings from April 2022, although the implementation of the legislation was paused on 8th February 2022 subject to a Parliamentary consultation.12, 13, 14
The introduction of strict measures to improve vaccine uptake has given rise to a variety of views, with some agreeing these measures are for ‘greater good’,15 while others fear they will deepen vaccine hesitancy and mistrust.16 Opinion polls from the UK demonstrate that the majority of the population agrees with mandatory COVID-19 vaccination for the general public and for National Health Service (NHS) or social care staff.17,18 By contrast, the World Health Organisation (WHO) has cautioned against mandatory vaccination, with the WHO Regional Director for Europe, Hans Kluge, stating that, “mandates should never contribute to increasing social inequalities in access to health and social services”.19 Several HCW regulators and representative bodies in the UK have stated concerns about mandatory vaccination for HCWs, including that it could erode trust and exacerbate existing workforce shortages.20, 21, 22, 23 The General Medical Council, UK have also identified that potential issues could arise among vaccinators if they feel that an individual's choice to receive a vaccination is unduly influenced by a deployment requirement.24
Previous research has demonstrated mixed views among HCWs regarding mandatory vaccinations against other diseases, particularly influenza, and support for mandatory vaccination varies by country, occupational group and vaccination status.25,26 At present there is little research on HCW views on compulsory COVID-19 vaccination. Understanding HCWs’ views on this topic (as well as on other potential ways of increasing COVID-19 vaccine uptake such as vaccine passports) is important as HCWs have considerable influence on the public's intention to get vaccinated27 and they also deliver vaccinations. Capturing HCWs’ suggestions for how to improve vaccine uptake could also help address vaccine hesitancy, shape policy and generate support for policy measures. In this study, we aimed to examine the views of HCWs in the UK about mandatory vaccination against COVID-19 for the UK population and/or for health and social care workers specifically, collected as part of the United Kingdom Research study into Ethnicity and COVID-19 outcomes among Healthcare workers (UK-REACH).
Methods
Overview and study design
UK-REACH is a programme of work aiming to determine the impact of the COVID-19 pandemic on UK HCWs, and to establish whether this differs according to ethnicity. This analysis uses data from the baseline questionnaire of the prospective nationwide longitudinal cohort study, administered between December 2020 and March 2021 and the first follow up questionnaire, administered by email to already recruited participants between 21st April 2021 and 26th June 2021. See study protocol28 for details.
Study population
We recruited individuals aged 16 years or over, living in the UK and employed as clinical or ancillary workers in a healthcare setting and/or registered with one of seven UK professional regulatory bodies. Recruitment into the study has been described extensively in previous work.6,28,29
This study used data from the second UK-REACH questionnaire, which was administered online by email to 17,891 participants who had already consented to participate in the study. HCWs were included in the analysed cohort if they answered both the baseline and the first follow up questionnaires.
Qualitative methods
In the follow-up questionnaire, participants could respond to a free text question: “What should society do if people do not get vaccinated against COVID-19?” We used the qualitative method of manifest content analysis,30,31 using an inductive (data-driven) approach to develop and assign codes to each response.
One researcher (KW) read through half of the responses and identified codes arising from the data, refining them iteratively throughout this process. When a participant's response included more than one code, we used the most socially restrictive code, for example, if a participant said that people should be educated and also that HCWs should have mandatory vaccinations, we coded this as mandatory vaccination for HCWs. This resulted in a dataset in which each participant's response had a single code. A second researcher (MG) then independently coded the remaining responses using the same coding framework, and double-coded 362 (25%) of KW's coded responses blindly. We assessed consistency and inter-coder reliability using the following formula32:
| reliability = number of agreements / (number of agreements + disagreements) |
Thereafter, both researchers discussed the coding framework, their interpretations of the codes, and the disagreements and finally arrived at an agreed code for each response.
Statistical analysis
Outcome measures
We used two outcome measures for the quantitative analysis. The first outcome measure was a multinomial categorical variable with one level for each code (see Table 1). For the second outcome measure we collapsed this into a binary outcome variable ‘favours mandatory vaccination’ (1=favours mandatory vaccination for the general public or for HCWs, 0=all other codes).
Table 1.
Description of the cohort stratified by the binary outcome of favouring mandatory vaccination or not and selected predictor variables, together with unadjusted and adjusted odds ratios for the association of predictor variables with the outcome.
| Variable | Totaln = 3235 | Does not Favour mandatory vaccinationn(%)2657 (82.1) | Favours mandatory vaccinationn(%)578 (17.9) | Unadjusted OR (95%CI) | P value | Adjusted OR (95%CI)* | P value |
|---|---|---|---|---|---|---|---|
|
Age (years) 16 to < 40 40 to < 55 ≥55 Missing |
1020 (31.5) 1239 (38.3) 963 (29.8) 13 (0.4) |
885 (33.3) 1019 (38.4) 743 (28.0) 10 (0.4) |
135 (23.4) 220 (38.1) 220 (38.1) 3 (0.5) |
Ref 1.42 (1.12–1.79) 1.94 (1.53–2.46) |
- 0.003 <0.001 |
Ref 1.40 (1.11–1.77) 1.84 (1.44–2.34) |
- 0.005 <0.001 |
|
Sex Male Female Missing |
824 (25.5) 2405 (74.3) 6 (0.2) |
653 (24.6) 1999 (75.2) 5 (0.2) |
171 (29.6) 406 (70.2) 1 (0.2) |
Ref 0.78 (0.64–0.95) |
- 0.01 |
Ref 0.79 (0.63–0.96) |
- 0.02 |
|
Ethnicity White Asian Black Mixed Other Missing |
2336 (72.2) 571 (17.7) 122 (3.8) 144 (4.5) 60 (1.9) 2 (0.1) |
1891 (71.2) 485 (18.3) 110 (4.1) 121 (4.6) 48 (1.8) 2 (0.1) |
445 (77.0) 86 (14.9) 12 (2.1) 23 (4.0) 12 (2.1) 0 (0.0) |
Ref 0.75 (0.59–0.97) 0.46 (0.25–0.85) 0.81 (0.51–1.28) 1.06 (0.56–2.02) |
- 0.03 0.01 0.36 0.85 |
Ref 0.77 (0.60–1.00) 0.46 (0.25–0.85) 0.84 (0.52–1.34) 1.07 (0.56–2.04) |
- 0.05 0.01 0.46 0.84 |
|
Migration status Born in the UK Born outside the UK Missing |
2356 (72.8) 791 (24.5) 88 (2.7) |
1925 (72.5) 657 (24.7) 75 (2.8) |
431 (74.6) 134 (23.2) 13 (2.3) |
Ref 0.91 (0.74–1.13) |
- 0.39 |
Ref 1.08 (0.84–1.38) |
- 0.56 |
|
IMD quintile 1 (most deprived) 2 3 4 5 (least deprived) Missing |
275 (8.5) 472 (14.6) 588 (18.2) 727 (22.5) 808 (25.0) 365 (11.3) |
230 (8.7) 388 (14.6) 474 (17.8) 607 (22.9) 654 (24.6) 304 (11.4) |
45 (7.8) 84 (14.5) 114 (19.7) 120 (20.8) 154 (26.6) 61 (10.6) |
Ref 1.11 (0.74–1.65) 1.23 (0.84–1.80) 1.01 (0.69–1.47) 1.20 (0.84–1.73) |
- 0.78 0.71 0.50 0.93 |
Ref† 1.06 (0.71–1.58) 1.08 (0.73–1.58) 0.88 (0.60–1.28) 1.02 (0.70–1.48) |
- 0.78 0.71 0.50 0.93 |
|
Job role Medical Nursing (inc Midwives + Health Care Assistants) AHPs (not inc scientists) Pharmacy Healthcare scientist Ambulance Dental Optical Admin/estates/other Missing |
778 (24.1) 698 (21.6) 917 (28.4) 62 (1.9) 146 (4.5) 94 (2.9) 93 (2.9) 82 (2.5) 184 (5.7) 103 (3.2) |
623 (23.5) 564 (21.2) 781 (29.4) 52 (2.0) 126 (4.7) 78 (2.9) 135 (5.1) 65 (2.5) 152 (5.7) 81 (3.1) |
155 (26.8) 134 (23.2) 136 (23.5) 10 (1.7) 20 (3.5) 16 (2.8) 36 (6.2) 17 (2.9) 32 (5.5) 22 (3.8) |
Ref 0.95 (0.74–1.24) 0.70 (0.54–0.90) 0.77 (0.38–1.56) 0.64 (0.39–1.06) 0.82 (0.47–1.45) 1.07 (0.71–1.61) 1.05 (0.60–1.84) 0.85 (0.56–1.29) |
- 0.73 0.006 0.47 0.08 0.50 0.74 0.86 0.44 |
Ref 0.84 (0.63–1.13) 0.66 (0.50–0.88) 0.81 (0.40–1.64) 0.57 (0.34–0.97) 0.72 (0.40–1.29) 0.96 (0.63–1.47) 0.95 (0.53–1.68) 0.79 (0.51–1.22) |
- 0.25 0.004 0.56 0.04 0.27 0.85 0.86 0.29 |
|
Exposure to patients with COVID-19 (at time of second questionnaire) No contact/remote contact only Face to face but no physical contact Physical contact Missing |
2518 (77.8) 149 (4.6) 377 (11.7) 191 (5.9) |
2062 (77.6) 132 (5.0) 312 (11.7) 151 (5.7) |
456 (78.9) 17 (2.9) 65 (11.3) 40 (6.9) |
Ref 0.58 (0.35–0.97) 0.94 (0.71–1.25) |
- 0.04 0.68 |
Ref 0.59 (0.35–1.00) 1.01 (0.75–1.35) |
- 0.05 0.97 |
|
Current or previous SARS-CoV-2 vaccine hesitancy Not hesitant Hesitant Missing |
2239 (69.2) 862 (26.7) 134 (4.1) |
1780 (67.0) 725 (27.3) 152 (5.7) |
459 (79.4) 92 (15.9) 27 (4.7) |
Ref 0.49 (0.39–0.63) |
- <0.001 |
Ref 0.56 (0.43–0.71) |
- <0.001 |
|
Number of influenza vaccines in previous 2 seasons 0 1 2 Missing |
456 (14.1) 515 (15.9) 2123 (65.6) 141 (4.4) |
397 (14.9) 428 (16.1) 1717 (64.6) 115 (4.3) |
59 (10.2) 87 (15.1) 406 (70.2) 26 (4.5) |
Ref 1.37 (0.96–1.96) 1.59 (1.19–2.14) |
- 0.09 0.002 |
Ref 1.35 (0.94–1.94) 1.49 (1.11–2.01) |
- 0.10 0.008 |
|
VAX score, med (IQR) Missing |
16 (14–17) 0 (0.0) |
16 (14–17) | 16 (15–18) | 1.11 (1.06–1.15) | <0.001 | 1.10 (1.06–1.15) | <0.001 |
|
Number of comorbidities 0 ≥1 Missing |
2465 (76.2) 249 (7.7) 521 (16.1) |
2033 (76.5) 201 (7.6) 423 (15.9) |
432 (74.7) 48 (8.3) 98 (17.0) |
Ref 1.12 (0.81–1.57) |
- 0.49 |
Ref 1.11 (0.79–1.56) |
- 0.54 |
|
Pregnant‡ Not pregnant Pregnant Missing |
2947 (91.1) 63 (2.0) 225 (7.0) |
2410 (90.7) 58 (2.2) 189 (7.1) |
537 (92.9) 5 (0.9) 36 (6.2) |
Ref 0.39 (0.15–0.97) |
- 0.04 |
Ref 0.60 (0.24–1.54) |
- 0.29 |
|
Previous COVID-19 Never tested Tested negative Tested positive Missing |
278 (8.6) 2181 (67.4) 763 (23.6) 13 (0.4) |
229 (8.6) 1798 (67.7) 620 (23.3) 10 (0.4) |
49 (8.5) 383 (66.3) 143 (24.8) 3 (0.5) |
1.00 (0.72–1.39) Ref 1.08 (0.88–1.34) |
0.98 - 0.46 |
1.00 (0.72–1.39) Ref 1.12 (0.91–1.39) |
0.99 - 0.29 |
|
Lives with a person ≥65 years old No Yes Missing |
2808 (86.8) 320 (9.9) 107 (3.3) |
2314 (87.1) 255 (9.6) 88 (3.3) |
494 (85.5) 65 (11.3) 19 (3.3) |
Ref 1.19 (0.89–1.59) |
- 0.23 |
Ref 0.97 (0.72–1.32) |
- 0.86 |
|
Lives with other key workers No Yes Missing |
1678 (51.9) 1444 (44.6) 113 (3.5) |
1378 (51.9) 1187 (44.7) 92 (3.5) |
300 (51.9) 257 (44.5) 21 (3.6) |
Ref 0.99 (0.83–1.20) |
- 0.95 |
Ref 1.02 (0.84–1.23) |
- 0.87 |
|
Trusts employing organisation to deal with concern about unsafe clinical practice Does not trust organisation Trusts organisation Missing |
844 (26.1) 2161 (66.8) 230 (7.1) |
673 (25.3) 1738 (65.4) 246 (9.3) |
164 (28.4) 350 (60.6) 64 (11.1) |
Ref 0.83 (0.67–1.02) |
- 0.07 |
Ref 0.82 (0.67–1.02) |
- 0.07 |
|
COVID-19 conspiracies score, med (IQR) Missing |
8 (7–10) 128 (4.0) |
8 (7–10) 107 (4.0) |
8 (7–10) 21 (3.6) |
0.94 (0.89–0.98) | 0.004 | 0.95 (0.91–1.00) | 0.05 |
|
UK region of work West Midlands South East England South West England + Channel Islands East of England East Midlands London North East England North West England + Isle of Man Yorkshire and the Humber Wales Scotland Northern Ireland Missing |
251 (7.8) 417 (12.9) 265 (8.2) 245 (7.6) 319 (9.9) 460 (14.2) 117 (3.6) 313 (9.7) 239 (7.4) 93 (2.9) 195 (6.0) 28 (0.9) 293 (9.1) |
208 (7.8) 349 (13.1) 218 (8.2) 205 (7.7) 272 (10.2) 357 (13.4) 87 (3.3) 257 (9.7) 201 (7.6) 73 (2.8) 164 (6.2) 25 (0.9) 241 (9.1) |
43 (7.4) 68 (11.8) 47 (8.1) 40 (6.9) 47 (8.1) 103 (17.8) 30 (5.2) 56 (9.7) 38 (6.6) 20 (3.5) 31 (5.4) 3 (0.5) 52 (9.0) |
Ref 0.94 (0.62–1.43) 1.04 (0.66–1.64) 0.94 (0.59–1.51) 0.84 (0.53–1.31) 1.40 (0.94–2.07) 1.67 (0.98–2.83) 1.05 (0.68–1.63) 0.91 (0.55–1.52) 1.33 (0.73–2.40) 0.91 (0.55–1.52) 0.58 (0.17–2.01) |
- 0.78 0.86 0.81 0.44 0.10 0.06 0.81 0.71 0.35 0.73 0.39 |
Ref 0.89 (0.59–1.36) 0.93 (0.59–1.48) 0.91 (0.56–1.46) 0.82 (0.52–1.29) 1.42 (0.95–2.11) 1.55 (0.91–2.65) 1.01 (0.65–1.57) 0.87 (0.54–1.40) 1.13 (0.61–2.07) 0.85 (0.51–1.41) 0.58 (0.17–2.03) |
- 0.60 0.77 0.69 0.39 0.09 0.11 0.97 0.56 0.70 0.52 0.40 |
*multivariable logistic regression adjusted for age, sex and ethnicity, †test for linear trend after multivariable regression was not significant.
‡Participants are coded as pregnant if they indicated they were pregnant at baseline or at follow up (i.e. this category includes participants who were pregnant at baseline and who may have delivered or any other reason leading to loss of pregnancy by the time of completing the follow up questionnaire).
Data in the first two columns are n(%) with percentages computed column-wise apart from the total number of those favouring/not favouring mandatory vaccination which are computed row wise. Due to including only complete cases in logistic regression models, multivariable models are based on fewer observations than univariable models. COVID-19 - coronavirus disease 2019; IMD – index of multiple deprivation; IQR – interquartile range; med – median; Ref – reference category for categorical variables in logistic regression analyses; SARS-CoV-2 – severe acute respiratory syndrome coronavirus-2.
Predictor variables
We chose the following predictor variables based on our previous analysis of the predictors of SARS-CoV-2 vaccine hesitancy6 together with a priori hypotheses about factors which might have an association with the outcome. These were as follows (see study protocol28 for details of each variable): demographics (ethnicity using Office for National Statistics categories,33 age (categorised as 16 to <40, 40 to < 55 and ≥ 55 years), sex, index of multiple deprivation (IMD) quintile of home postcode), migration status, job role, region of the UK in which the participant works, SARS-CoV-2 vaccine hesitancy as defined in our previous analysis,6 influenza (flu) vaccine uptake in the previous two seasons, attitudes towards vaccination generally (VAX scale),34 presence of comorbidities, previous COVID-19, pregnancy, living with someone over the age of 65, living with other key workers, trust in employer organisation (to deal with a concern about unsafe clinical practice), number of confirmed/suspected COVID-19 patients seen per week, and belief in COVID-19 conspiracies.35
Analysis
To assess response bias, we compared the demographic and occupational characteristics of those that responded to the free-text question with those that did not using chi-squared tests for categorical variable and Wilcoxon rank-sum tests for continuous variables.
We calculated the frequency and proportion of participants assigned to each code. We explored univariable relationships between predictor variables and the multinomial outcome variable using chi-squared tests for categorical variables and Kruskal-Wallis tests for continuous variables.
We used logistic regression to calculate the univariate association between the binary outcome variable and each predictor variable. We then calculated a base model by regressing age, sex and ethnicity on the binary outcome variable. We used logistic regression to examine the association of each of the other predictor variables in turn with the binary outcome, adjusted for age, sex and ethnicity.
We excluded participants with missing outcome data.
We used Stata 17 for all statistical analyses.36 P values <0.05 were considered statistically significant.
Ethical approval
Both studies were approved by the Health Research Authority (Brighton and Sussex Research Ethics Committee; ethics reference: 20/HRA/4718). All participants gave written informed consent.
Involvement and engagement
We worked closely with a Professional Expert Panel of HCWs from a range of ethnic backgrounds, occupations, and genders, as well as with national and local organisations (see study protocol).28
Role of the funding source
The funders had no role in study design, data collection, data analysis, interpretation, writing of the report. KW, MG, CAM and MP had access to all the data in the study and all authors accept responsibility to submit for publication.
Results
Description of the analysed cohort
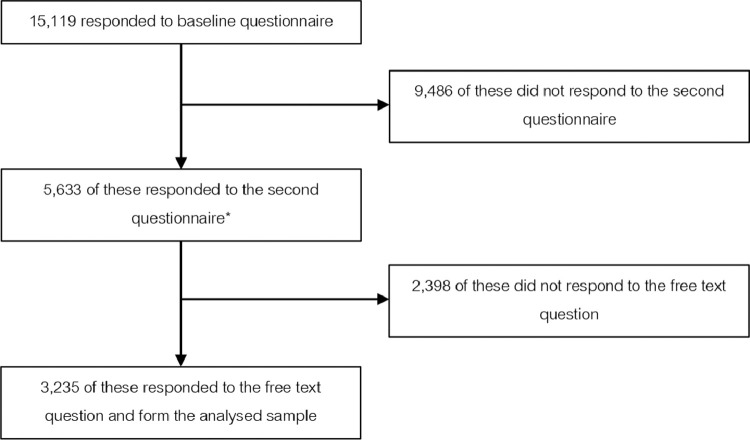
Of the 5633 respondents to both first and second questionnaires, 3235 (57.8%) gave a response to the free-text question that could be coded (see Figure 1). Of these, 2405 (74.3%) were female and 897 (27.7%) were from ethnic minority groups. The majority of participants worked in allied health professional (40.3%), medical (23.9%) or nursing/midwifery (21.6%) roles (Table 1).
Figure 1.
Formation of the analysed sample.
*These 5633 healthcare workers are included in the analysis of response bias (see Supplementary Table 1). Initial recruitment into the UK-REACH prospective longitudinal cohort study is described in greater detail in previous work.63
Assessment of response bias
Supplementary Table 2 shows a comparison of the demographic and occupational characteristics of those that did and did not respond to the free text question. Non-responders were significantly younger than responders (median [IQR] age in years 43 [34–57] vs 47[36–56], p < 0.001). There were no significant differences by sex, ethnicity or job role.
Inter-rater reliability of coding
Of the 362 double-coded responses, the researchers agreed on 334 and disagreed on 28, giving a reliability score of 92.2%. Following discussion and resolution of all discrepancies, one code with very few responses (“Change vaccines”) was subsumed in the code “Educate, increase access, incentivise”.
Qualitative description and frequency of codes
The analysis resulted in seven codes: Mandatory vaccination for the general population; Mandatory vaccination for HCWs; Do nothing; Specific restrictions for unvaccinated individuals; Maintain Covid-19 restrictions; Educate, increase access, incentivise; Do not know. Codes are described briefly in Table 2. More detailed descriptions of each code with exemplar quotes and frequencies are given below.
Table 2.
Description of codes used to analyse free-text responses to the question “What should society do if people do not get vaccinated against COVID-19?”
| Codes | Description of responses within code |
|---|---|
| Mandatory vaccination | Agreement with mandatory vaccination, either directly (e.g. by introducing a law) or via restrictions for unvaccinated individuals on access to essential services (work, education, healthcare), or by other severe restrictions such as isolating unvaccinated people completely and/or making them stay at home until they get vaccinated. |
| Mandatory vaccination for healthcare workers and social care staff | Agreement with mandatory vaccination for health and social care workers and those working with clinically vulnerable populations. |
| Specific restrictions for unvaccinated people | Vaccine passports and restricting access to leisure and travel but not to essential services (e.g. healthcare, work, education) and/or increased restrictions (e.g. wearing PPE, social distancing) for unvaccinated only. |
| Do nothing | Statements about freedom of choice being vital in a democracy, about it being immoral or undemocratic or against human rights to require people to be vaccinated. Statements that nothing can be done. |
| Educate, increase access or incentivise | Educate to improve understanding of the benefits and risks of vaccination. Encourage vaccine uptake (e.g. demonstrating empathy and listening). Providing positive incentives for vaccination (not restrictions on unvaccinated). Focus on improving uptake within marginalised groups by increasing confidence and knowledge (e.g. via relevant role models) and by tackling wider underlying societal causes of hesitancy (e.g. poverty and discrimination). Greater transparency about vaccine manufacture and roll-out. Improve access to vaccines or improving vaccines to make them more acceptable to some groups (e.g. vegans). |
| Maintain COVID-19 restrictions | Maintaining restrictions within society generally, not for unvaccinated people only (e.g. widespread use of PPE, social distancing, lockdowns). Consequences of higher levels of disease e.g. increased mortality within the population. |
| Do not know what to do | Statements about being unable to decide what to do e.g. “I really do not know”. Gives two opposing arguments (e.g. unable to do anything because of civil liberties, and mandatory vaccination for healthcare workers) without stating a preference for either. |
| Missing / not coded | Left blank. Unable to code because the response does not attempt to answer the question. |
Mandatory vaccination for the general population
Overall, 377 (12%) participants advocated mandatory vaccination for the general population and/or imposing serious sanctions on those who were eligible to be vaccinated but choose not to. This included fines and being shamed or isolated from society:
“Make it mandatory with meaningful penalties.”
“Identify & Isolate them”
“Shun them, and set them apart”
A number felt that vaccination was necessary to relieve some of the pressure faced by HCWs and the NHS due to COVID-19, and suggested individuals who chose not to get vaccinated should be refused healthcare on the NHS and made to pay:
“People need to realise that they put health care workers at risk would sign a disclaimer for reduced treatment”
“Make it mandatory or fine them, remove health services from them”
“If people have capacity and refuse then they should relinquish their right to NHS treatment if they catch COVID 19. They should be made to pay for their treatment if they require hospital admission”
Several also justified mandatory vaccination via the benefits to others and society from reducing the risk of transmission:
“Make them mandatory as part of our "social" and "national" responsibility to ourselves and others. Unless people cannot be vaccinated [sic] due to health reasons”
“I hope everyone should consider getting vaccine to reduce the risk to themselves and others, or government should make it compulsory”
Mandatory vaccination for HCW / social care staff
Overall, 201 (6%) participants specifically advocated mandatory vaccination for HCW and others working with vulnerable populations. Frequently this was described as an exceptional case that was necessary to protect the most vulnerable in society:
“Tough one. I think in certain roles this should be mandatory- healthcare workers, care home staff etc.”
“A really tricky one! I would support mandatory vaccination for people working in direct patient care roles (NHS/care sector) but not elsewhere”
Several mentioned that vaccination against Hepatitis B was already required for HCWs:
“Depends on the reason for not getting vaccinated and what the individual is hoping to do. In healthcare roles, vaccination should be mandatory (c.f Hep B). In general society there should not be a compulsion”
Specific restrictions for unvaccinated people
Overall, 17% (n = 547) participants advocated for specific restrictions for unvaccinated individuals. Responses described restrictions on travel, social and leisure activities for those who are unvaccinated, including use of vaccine passports and additional testing or use of protective personal equipment:
“I think there should be a requirement for proof of vaccination or a negative covid test result for access to indoor event such as theatres, concerts etc. and large scale outdoor events so that everyone can feel safe and confident. Those that refuse vaccination have the freedom and right to do so, but everyone has the right to feel safe”
“Restrict access to social gatherings, travel etc. if people choose not to get vaccinated”
Do nothing
Overall 18% (n = 580) had a response coded as “Do nothing”; a similar proportion as advocated mandatory vaccination. Common reasons in this category referred to the belief that the decision to be vaccinated was a personal choice that it was important to respect:
“Accept that this is a free country and people are capable of making their own decisions”
“No idea. Very hard to do as it is a choice and against human rights to enforce it”
“People should have a choice. They should not feel pressured into having something we still do not know a lot about.”
“It's a personal choice. We cannot force people to inject themselves with a substance. I think this could be considered as assault if we were made to.”
In contrast to the participants who felt vaccination should be mandatory to protect others, several participants in this category stated their opinion that unvaccinated people were only putting themselves at risk:
“Nothing - carry on. if people want the vaccine then that it ok but it is also ok not to have this. the vaccine reduces the symptoms if you get Covid, it does not stop you getting it or transmitting it.”
“Nothing much. If someone wishes to risk their life by not getting vaccinated, society cannot prevent this. Same applies to dangerous activities like mountaineering horse-riding etc.”
A few described how other vaccinations were not mandatory, so there was little justification for making Covid-19 vaccinations compulsory:
“People decline the flu vaccine and face no repercussions so I do not see how any sanctions can be placed on people not having the Covid vaccine”.
Some feared that making vaccination mandatory could have negative consequences:
“Best to careful - there are risks of creating a two tier society or driving the non-vaccinated underground”
“Just carry on and try not to use it as an excuse to argue and build bigger barriers”
A few mentioned that some people are clinically unable to be vaccinated:
“Respect people's wishes as it may be no fault of their own eg health or capacity reasons”
Several mentioned that herd immunity, either from vaccination or infection would be sufficient for tackling COVID-19:
“Allow choice, hope herd immunity overcomes”
“Return to normal as large numbers and vulnerable have been vaccinated.”
One participant stated a preference for “natural” immunity over vaccination:
“Cheer. Most people have a robust immune system. We will have been exposed to the usual coronaviruses/rhinoviruses during our lifetime and our t-cells and lymphocytes will recognise these again. Those with co morbidities should shield if they wish.”
Educate, increase access or incentivise
The most frequent code, chosen by almost a third of participants overall (1047/3229, 32%) was to educate, increase access to vaccines or incentivise vaccination. Many responses described the need to provide better information and support that would enable people to make decisions based on evidence and an assessment of the risks and benefits:
“Continue to encourage; ensure people aware of the evidence for vaccine and consequences of not doing it”
Several responses specifically mentioned the role of religious and ethnic minority community leaders in encouraging vaccination:
“Work with them and find out why they do not want it. Enlist community champions, e.g., religious leaders or other community leaders”
“Further support through campaigns, education and use of local champions or champions from same ethnicity.”
There were some calls for those spreading or allowing the spread of false information to be sanctioned:
“Media and social media should be held accountable for spreading false information”
Maintain COVID-19 restrictions
Overall, 10% (336) felt that society's response to suboptimal vaccination coverage would be to maintain COVID-19 restrictions, including for those shielding or especially vulnerable.
“Remain on specific lock downs or continue with strict social distancing measure[s]”
For some participants this may have been seen as a solution, but for others it reflected a feeling of resignation:
“More lockdowns will be inevitable”
“Prepare for another wave of infection!”
Do not know
A minority (147, 5%) acknowledged this is a difficult a question to answer or did not give a definitive answer:
“It's a difficult one. Everyone has a right to decline, but this risks the greater good for everyone. These people will get herd immunity. I do not have a real answer for this dilemma.”
Statistical associations of predictor variables with outcome measures
Overall 18% (n = 578) favoured mandatory vaccination (either in general or for HCWs specifically), whereas 82% favoured other options Table 1. shows the cohort stratified by the binary outcome variable and by the predictor variables with p values from univariable and multivariable tests of association. Supplementary Table 1 shows the cohort stratified by the seven-level categorical outcome variable and by the predictor variables with p values from univariable tests of association.
Univariable analyses indicated that favouring mandatory vaccination was associated with being older (OR 1.42; 95%CI 1.12–1.79 for those aged 40 to < 55 years and OR 1.94; 95%CI 1.53–2.46, for those aged ≥55years compared to those aged 16 to < 40 years), having been vaccinated against influenza in both the previous two seasons (OR 1.59; 95%CI 1.19–2.14, vs none), and with more pro-vaccine attitudes (OR 1.11; 95%CI 1.06–1.15); whereas not favouring mandatory vaccination was associated with female sex (OR 0.78; 95%CI 0.64–0.95, vs male), Black (OR 0.46; 95%CI 0.25–0.85, vs white) or Asian (OR 0.75; 95%CI 0.59–0.97, vs white) ethnicity, Allied Health Professional occupation (OR 0.70; 95%CI 0.54–0.90, vs Medical), hesitancy about SARS-CoV-2 vaccination (OR 0.49; 95%CI 0.39–0.64, vs not hesitant), pregnancy (current or recent, 0.39; 95%CI 0.15–0.97, vs not pregnant) and greater belief in COVID-19 conspiracies (OR 0.94; 95%CI 0.91–1.00).
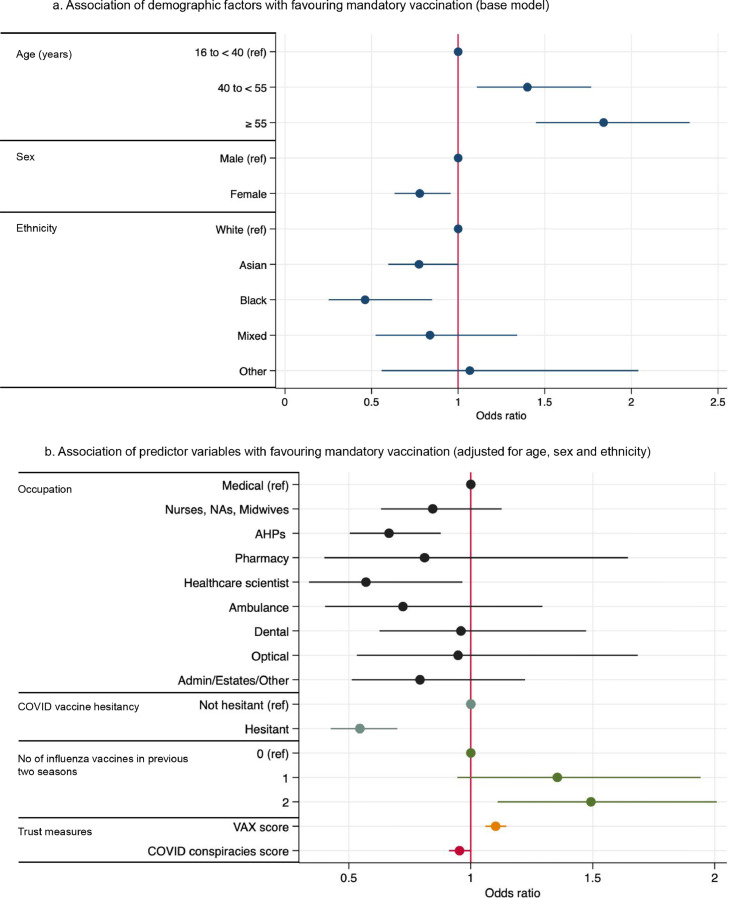
Multivariable analysis from the base model (Figure 2a) showed that older HCWs were more likely to favour mandatory vaccination (aOR 1.40; 95%CI 1.11–1.77 for those aged 40 to < 55 years and aOR 1.84; 95%CI 1.44–2.34, for those aged ≥55years compared to those aged 16 to < 40 years) whereas female HCWs (aOR 0.79, 95%CI 0.63–0.96, vs male) and HCWs of Black ethnicity (OR= 0.46, 95%CI 0.25–0.85, vs white) were less likely to. After adjusting for age, sex and ethnicity (Figure 2b), HCWs vaccinated against influenza in the previous two seasons (aOR 1.49; 95%CI 1.11–2.01, vs no influenza vaccine) and with more positive attitudes towards vaccination generally (aOR 1.10; 95%CI 1.06–1.15) were more likely to favour mandatory vaccination, whereas those hesitant about COVID-19 vaccination (aOR 0.56; 95% CI 0.43–0.71, vs not hesitant) and those who were in an Allied Health Profession (aOR 0.66; 95%CI 0.50––0.88, vs Medical) were less likely to favour mandatory vaccination.
Figure 2.
Significant findings from the multivariable logistic regression Figure 2 .a shows the base model. Associations of age, sex and ethnicity with an outcome of favouring mandatory vaccination are expressed as adjusted odds ratios and 95% confidence intervals. Regression analyses contained complete cases only, therefore, this analysis includes 3215 HCW Figure 2 .b shows the adjusted odds ratios and 95% confidence intervals for the association of predictor variables with an outcome of favouring mandatory vaccination. Only predictor variables with a statistically significant association are shown. Analyses are adjusted for age, sex and ethnicity. Regression analyses contained complete cases only, therefore, estimates for each predictor variable are based on different numbers of observations. Sample size for each predictor can be calculated by subtracting the number of observations with missing data (See Table 1) for the predictor from the number of observations in the base model (n = 3215). AHP – allied health professional; COVID-19 – coronavirus disease 2019; IMD – index of multiple deprivation.
Discussion
Only one in six HCWs in this large, diverse, UK-wide sample favoured mandatory vaccination as a strategy for dealing with suboptimal vaccination coverage; a third favoured education and support as a strategy. HCWs who were hesitant about vaccination generally and about COVID-19 vaccination specifically, as well as female HCWs, HCWs from some ethnic minority groups, younger HCWs, and Allied Health Professional occupational groups were less likely to advocate mandatory vaccination.
This is to our knowledge, the only large-scale national study of HCWs’ perceptions of mandatory vaccination. The size and the diversity of the sample (28% ethnic minority compared to 22% of NHS staff37 and 13% of the general population38), together with detailed information collected on participants from two waves of the UK-REACH longitudinal questionnaire, meant it was possible to examine differences in views by participant ethnicity, occupational group, age, health, and vaccination status.
Responses were collected in early Summer 2021, before mandatory vaccination for health and social care staff was announced in England on 9th November 2021,12 and before the classification by the UK Health Security Agency (UKHSA) of the Omicron variant of SARS-CoV-2 as a variant of concern on 27th November 202139 with greater transmissibility. This may have altered attitudes towards mandatory vaccination and vaccine passports. Data collection did however coincide with the classification by the UK Government of the Delta variant as a variant of concern on 7th May 2021, with the roll-out of vaccines to all eligible adults in the UK by July 2021, and the lifting of restrictions in June 2021 after a third national lockdown.40 Indeed, since the start of the vaccine roll-out increasing data on the vaccines has continued to emerge may have influenced and continue to influence participants’ views about mandatory vaccination in a variety of ways. This includes data on rare-side effects of the vaccines,41,42 the effectiveness of Covid-19 vaccination in pregnancy,43 the high efficacy of the vaccines against severe disease and hospitalisation44 and the impact of vaccination on reducing household transmission of Covid-19.45
The outcome variable data were gathered via a free-text question and we were therefore unable to explore attitudes and opinions in as much depth as would have been possible in a qualitative interview study. Our use of a free-text question rather than a multiple-choice question meant we could not capture what each participant thought about each code, including mandatory vaccination, however we were able to capture information that is potentially representative of participants’ priorities since they generated the responses themselves. The participant-generated responses to the free-text question also allowed us to capture new information about HCWs’ views not necessarily covered in the literature; however we have included a quantitative question about mandatory vaccination in a subsequent questionnaire. The trustworthiness of the results is also supported by the high inter-rater reliability of the double-coding of a large portion of responses. Our method of only allowing one code per response, and of choosing the most socially-restrictive code when there were multiple options, meant we did not examine the co-occurrence of codes within participants. This could also have resulted in an under-estimation of the endorsement of less restrictive options, such as Do nothing. The fact that respondents to the free-text question were slightly older than the cohort generally may have resulted in the over-estimation of the endorsement of more restrictive options such as mandatory vaccination for HCWs, which were more common among older participants. Our decision to undertake a complete case analysis could have introduced bias if data are not missing completely at random. However, the proportion of observations with missing data in selected predictor variables are low and ‘missingness’ does not seem to vary when the cohort are stratified by the outcome measure.
We found nine published studies that have examined HCW or medical student views on mandatory vaccination against COVID-19. None were from the UK. All were cross-sectional survey studies, and all asked participants a specific question about whether they agreed with mandatory vaccination for HCWs, and all but one46 found reasonably high levels support.47, 48, 49, 50, 51, 52, 53, 54 Our study used a different approach, asking participants to suggest solutions to sub-optimal SARS-CoV-2 vaccination coverage, and in our study a lower proportion of HCWs favoured mandatory vaccination as a strategy. This is likely to reflect that we did not directly ask participants about mandatory vaccination, as explained above. Similarly to our findings, two studies found higher rates of agreement with mandatory vaccination among doctors compared to other occupational groups.48,54 One found views on mandatory vaccination were not associated with age or sex48 and another found female and non-Hispanic White medical students were less likely to agree with mandatory vaccination for HCWs or patients and were also more vaccine hesitant.53 In our previous analysis we also found higher rates of hesitancy among allied health professionals compared to doctors.6 As with our study, several studies found that HCWs who were hesitant about vaccines were much less likely to agree with mandatory vaccination. Similarly, a mixed-methods study of health and social care workers in England published as a pre-print found that participants who agreed that they felt under pressure from their employer to get a vaccine were more likely to have declined vaccination, although the direction of causality is unclear.55
Other studies have assessed HCWs’ views on mandatory vaccination for non-COVID diseases, finding mixed levels of support. For example, a systematic review and meta-analysis of studies of HCW views on mandatory influenza vaccination found 61% agreeing with mandatory vaccination, but agreement varied between studies considerably, ranging from 15% to 90%. Rates of agreement were higher among vaccinated HCWs and among doctors (physicians and general practitioners) compared to nurses.25 A study of medical students at one Austrian university published in 2020 found 83% agreed with mandatory hepatitis B vaccination, whereas 40% agreed with mandatory influenza vaccination.26 A survey of English healthcare staff responsible for influenza vaccination campaigns conducted in 2017 found that 68% believed a mandatory campaign would increase uptake, but only 17% of those surveyed believed other HCWs would support mandatory vaccination, and qualitative interview and focus group results demonstrated “fairly consistent opposition” to mandatory vaccination.56
Only 12% of HCWs in our study proposed mandatory COVID-19 vaccination for the general public as a solution to sub-optimal vaccination rates, and half that number (6%) specifically proposed mandatory vaccination for HCWs. This suggests that the policy to introduce mandatory vaccination for frontline HCWs in England could be unpopular with the majority of HCWs, especially those who are already hesitant about vaccination against COVID-19 or against other diseases, as well as among female HCWs who make up the majority of NHS staff, and among Black and Asian ethnic groups as well as among Allied Health Professionals. If the introduction of mandatory vaccination does reduce trust in healthcare providers and employers among those groups, this could exacerbate existing health inequalities, and could be perceived as counteracting the ethical principle that individuals should be able to give true informed consent to a medical intervention.57
It is vital that strong efforts are made to build confidence in the safety and efficacy of vaccines among those who are hesitant.58 This includes vaccines against COVID-19, as well as vaccines against influenza and other vaccine-preventable diseases that compromise NHS staff health and patient safety. Building vaccine confidence among HCWs will not just increase uptake, but also enable HCWs to advocate for vaccination among patients59 and members of their own communities. This may support uptake among groups experiencing social and health inequalities who may be at greater risk of adverse effects from COVID-19 as well as other diseases.60
The findings of this study cast some doubt on the potential success of a mandatory vaccination policy for HCWs. The UK Government's own impact assessment for its proposed mandatory vaccination policy estimates that only a minority of currently unvaccinated HCWs would be vaccinated under the policy, which would leave 88,000 HCWs (5% of the workforce) unvaccinated and non-exempt, and therefore needing to be removed from patient-facing roles.12 Meanwhile the King's Fund has stated that NHS hospitals, mental health services and community providers reported a shortage of nearly 84,000 full-time equivalent staff in 2020, which might be exacerbated by enforcement of sanctions against unvaccinated HCWs.61
Future research should include evaluation of specific approaches for increasing vaccine uptake among HCWs, their colleagues, patients, families and communities.62 UK-REACH is currently analysing in-depth qualitative data on vaccine perceptions, and collecting longitudinal data on attitudes to vaccination policies and changes in vaccine hesitancy and uptake among diverse HCWs, which will help inform the best approaches to maximise uptake in this vital group.
The majority of UK HCWs did not propose mandatory Covid-19 vaccination as a solution to sub-optimal vaccine coverage. Mandatory vaccination was less favoured by those already hesitant about vaccination against Covid-19 and influenza, and among HCWs who are women, from some ethnic minority groups, younger, and in Allied Health Profession occupations. While compulsory vaccination is likely to increase coverage, a significant number of HCWs could remain unvaccinated and further research is required to understand the impact of compulsory vaccination policies in England, particularly on levels of trust among some minoritised groups, staff well-being, and shortages.
UK-REACH study collaborative group
Manish Pareek (Chief investigator), Laura Gray (University of Leicester), Laura Nellums (University of Nottingham), Anna L Guyatt (University of Leicester), Catherine John (University of Leicester), I Chris McManus (University College London), Katherine Woolf (University College London), Ibrahim Akubakar (University College London), Amit Gupta (Oxford University Hospitals), Keith R Abrams (University of Warwick), Martin D Tobin (University of Leicester), Louise Wain (University of Leicester), Sue Carr (University Hospital Leicester), Edward Dove (University of Edinburgh), Kamlesh Khunti (University of Leicester), David Ford (University of Swansea), Robert Free (University of Leicester)
Contributors
MP conceived of the idea for the study and led the application for funding with input from MDT, KK, ICM, KW, LBN, SC, LJG, ALG and CJ. The survey was designed by KW, MP, ICM, CMel, CJ, ALG, LBN, and CAM. Online consent and survey tools were developed by LB. The underlying data were verified by CAM, KW, MG and MP. KW, MG and CAM, wrote the first draft of the manuscript with input from MP, PP, and all co-authors. All authors confirm that they had full access to all the data in the study and accept responsibility to submit for publication. All authors approved the submitted manuscript. The lead authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Data sharing
To access data or samples produced by the UK-REACH study, the working group representative must first submit a request to the Core Management Group by contacting the UK-REACH Project Manager in the first instance. For ancillary studies outside of the core deliverables, the Steering Committee will make final decisions once they have been approved by the Core Management Group. Decisions on granting the access to data/materials will be made within eight weeks. Third party requests from outside the Project will require explicit approval of the Steering Committee once approved by the Core Management Group. Note that should there be significant numbers of requests to access data and/or samples then a separate Data Access Committee will be convened to appraise requests in the first instance.
Funding
MRC-UK Research and Innovation grant (MR/V027549/1) and the Department of Health and Social Care (DHSC) via the National Institute for Health Research (NIHR). Core funding was also provided by NIHR Biomedical Research Centres.
Declaration of Interests
KK is Director of the University of Leicester Centre for Black Minority Ethnic Health, trustee of the South Asian Health Foundation and chair of the Ethnicity Subgroup of the UK Government Scientific Advisory Group for Emergencies (SAGE). SC is Deputy Medical Director of the General Medical Council. MP reports grants from Sanofi, grants and personal fees from Gilead Sciences and personal fees from QIAGEN, outside the submitted work. KW declares honoraria from the Commission for Academic Accreditation UAE, Health Education England and King's College London and consultancy fees from the Federation of the Royal Colleges of Physicians of the UK outside of the submitted work. MDT reports a research collaboration with Orion Pharma unrelated to the research in this paper. SL is the Executive secretary of the Filipino Nurses Association-UK and Member of the Board International Forum of Headache nurses which is unrelated to the research in this paper. SL has received consultancy fees from Salvia BioElectronics and honoraria from Abbvie, Eli Lilly, TEVA and Novartis outside of the submitted work and participates on advisory boards for Abbvie, Eli Lilly, TEVA and Novartis. ALG participates in the Wellcome Longitudinal Population Studies COVID-19 questionnaire committee. The views expressed in the publication are those of the author(s) and not necessarily those of the National Health Service (NHS), the NIHR or the Department of Health and Social Care. This research was funded in whole, or in part, by the Wellcome Trust [WT204801/Z/16/Z and WT 202849/Z/16/Z]. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Acknowledgments
We would like to thank all the healthcare workers who took part in this study when the NHS was under immense pressure.
We wish to acknowledge the Professional Expert Panel group and the Steering and Advisory Group (see the cohort study protocol28 for details), and SERCO, as well as the following people for their support in setting up the study from the regulatory bodies: Kerrin Clapton and Andrew Ledgard (General Medical Council), Caroline Kenny (Nursing and Midwifery Council), Lisa Bainbridge (General Dental Council), Angharad Jones (General Optical Council).
We would also like to acknowledge the following trusts and sites who recruited participants to the study: Nottinghamshire Healthcare NHS Foundation Trust, University Hospitals Leicester, Lancashire Teaching Hospitals NHS Foundation Trust, Northumbria Healthcare, Berkshire Healthcare, Derbyshire Healthcare NHS Foundation Trust, South Tees NHS Foundation Trust, Birmingham and Solihull NHS Foundation Trust, Affinity Care, Royal Brompton and Harefield, Sheffield Teaching Hospitals, St George's Hospital, Yeovil District Hospital, Lewisham and Greenwich NHS Trust, Black Country Community Healthcare NHS Foundation Trust, Sussex Community NHS Foundation Trust, South Central Ambulance Service, University Hospitals Coventry and Warwickshire, University Hospitals Southampton NHS Foundation Trust, London Ambulance Trust, Royal Free, Birmingham Community Healthcare NHS Foundation Trust, Central London Community Healthcare, Chesterfield Royal Hospital, Bridgewater Community Healthcare, Northern Borders, County Durham and Darlington Foundation Trust, Walsall Healthcare NHS Trust.
KW was funded through an NIHR Career Development Fellowship (CDF-2017-10-008). CAM is an NIHR Academic Clinical Fellow (ACF-2018-11-004). LBN is supported by an Academy of Medical Sciences Springboard Award (SBF005\1047). ALG was funded by internal fellowships at the University of Leicester from the Wellcome Trust Institutional Strategic Support Fund (204801/Z/16/Z) and the BHF Accelerator Award (AA/18/3/34220). MDT holds a Wellcome Trust Investigator Award (WT 202849/Z/16/Z) and an NIHR Senior Investigator Award. KK and LJG are supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. KK and MP are supported by the NIHR Leicester Biomedical Research Centre (BRC). MP is supported by a NIHR Development and Skills Enhancement Award. CJ acknowledges funding from a MRC Clinical Research Training Fellowship (MR/P00167X/1). This work is carried out with the support of BREATHE -The Health Data Research Hub for Respiratory Health [MC_PC_19004] in partnership with SAIL Databank. BREATHE is funded through the UK Research and Innovation Industrial Strategy Challenge Fund and delivered through Health Data Research UK.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101346.
Appendix. Supplementary materials
References
- 1.National Health Service. Coronavirus (COVID-19) vaccines. 2021. https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine/. Accessed 29 November 2021.
- 2.National Health Service England. COVID-19 monthly announced vaccinations 09 September 2021. 2021. https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-vaccinations/. Accessed 7 October 2021.
- 3.de Figueiredo A. Forecasting sub-national trends in COVID-19 vaccine uptake in the UK. medRxiv 2021: 2020.12.17.20248382. [DOI] [PMC free article] [PubMed]
- 4.Freeman D., Loe B.S., Chadwick A., et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020:1–15. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robertson E, Reeve KS, Niedzwiedz CL, et al. Predictors of COVID-19 vaccine hesitancy in the UK Household Longitudinal Study. medRxiv 2021 : 2020.12.27.20248899. [DOI] [PMC free article] [PubMed]
- 6.Woolf K., McManus I.C., Martin C.A., et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: results from the UK-REACH prospective nationwide cohort study. Lancet Reg Health Europe. 2021 doi: 10.1016/j.lanepe.2021.100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wise J. British Medical Journal Publishing Group; 2021. Covid-19: France and Greece make Vaccination Mandatory for Healthcare Workers. [DOI] [PubMed] [Google Scholar]
- 8.Paterlini M. Covid-19: Italy makes vaccination mandatory for healthcare workers. Br Med J Publ Gr. 2021 doi: 10.1136/bmj.n905. [DOI] [PubMed] [Google Scholar]
- 9.Oltermann P. Austria plans compulsory Covid vaccination for all. The Guardian. 2021 19th November 2021.
- 10.News; B. Covid: Greece to fine over-60s who refuse Covid-19 vaccine. 30th November 2021 2021. https://www.bbc.co.uk/news/world-europe-59474808. Accessed 17 December 2021 2021.
- 11.Hagan K., Forman R., Mossialos E., Ndebele P., Hyder A.A., Nasir K. COVID-19 vaccine mandate for healthcare workers in the United States: a social justice policy. Expert Rev Vaccines. 2021:1–9. doi: 10.1080/14760584.2022.1999811. [DOI] [PubMed] [Google Scholar]
- 12.Care; DoHaS. Making vaccination a condition of deployment in the health and wider social care sector. 10th December 2021 2021. https://www.gov.uk/government/consultations/making-vaccination-a-condition-of-deployment-in-the-health-and-wider-social-care-sector/making-vaccination-a-condition-of-deployment-in-the-health-and-wider-social-care-sector. Accessed 17 December 2021.
- 13.Rimmer A. Covid vaccination to be mandatory for NHS staff in England from spring 2022. Br Med J Publ Group. 2021 doi: 10.1136/bmj.n2733. [DOI] [PubMed] [Google Scholar]
- 14.England; N. Vaccination as a condition of deployment (VCOD) for healthcare workers. Frequently Asked Questions. 8 February 2022 Version 1. NHS England; 2022.
- 15.Sokol D. Covid-19 vaccination should be mandatory for healthcare workers. BMJ. 2021:375. doi: 10.1136/bmj.n2670. [DOI] [PubMed] [Google Scholar]
- 16.Kmietowicz Z. Evidence is insufficient to back mandatory NHS staff vaccination, says House of Lords committee. Br Med J Publ Group. 2021 [Google Scholar]
- 17.YouGov. Opinion poll: Do you think it should or should not be compulsory for staff working in care homes for older people to be vaccinated against Covid-19? 16/06/2021 2021. https://yougov.co.uk/topics/politics/survey-results/daily/2021/06/16/986dc/1. Accessed 17 December 2021.
- 18.Hoffman N. Two thirds of people support compulsory Covid jabs for NHS and care staff. PoliticsHome. 2021 15/11/2021,. Accessed 17/12/2021) [Google Scholar]
- 19.United Nations in Western Europe. WHO: Mandatory vaccinations are a last resort. 7/12/2021 2021. https://unric.org/en/who-mandatory-vaccinations-are-a-last-resort/. Accessed 17 December 2021
- 20.Royal College of General Pracititioners. RCGP opposes mandatory Covid-19 vaccination for NHS workers. 09/11/2021 2021. https://www.rcgp.org.uk/about-us/news/2021/november/opposition-mandatory-vaccination-nhs-workers.aspx. Accessed 17 December 2021.
- 21.Royal College of Nursing. RCN position on mandating vaccination for health and social care staff. 11/11/2021 2021. https://www.rcn.org.uk/about-us/our-influencing-work/position-statements/rcn-position-on-mandating-vaccination-for-health-and-social-care-staff. Accessed 17 December 2021
- 22.Royal College of Midwives. Mandatory COVID vaccination for NHS staff. 10/11/2021 2021. https://www.rcm.org.uk/news-views/news/2021/november/mandatory-covid-vaccination-for-nhs-staff/. Accessed 17 December 2021.
- 23.NHS Employers . NHS Employers; 2021. Making Vaccination a Condition of Deployment in the Health and Wider Social Care Sector. London. [Google Scholar]
- 24.General Medical Council. GMC response to the Department for Health and Social Care Consultation on making vaccination against COVID-19 and influenza a condition of deployment in the health and wider social care sector. 2021. https://www.gmc-uk.org/-/media/documents/gmc-response-to-dhsc-consultation-on-making-vaccination-a-condition-of-deployment-health-an-88002576.pdf. Accessed 17 December 2021.
- 25.Gualano M.R., Corradi A., Voglino G., et al. Healthcare Workers’ (HCWs) attitudes towards mandatory influenza vaccination: a systematic review and meta-analysis. Vaccine. 2021;39(6):901–914. doi: 10.1016/j.vaccine.2020.12.061. [DOI] [PubMed] [Google Scholar]
- 26.Kunze U., Schweinzer H. Self-reported vaccination status and attitudes towards mandatory vaccinations for health care workers among medical students. Vaccine. 2020;38(35):5695–5699. doi: 10.1016/j.vaccine.2020.06.046. [DOI] [PubMed] [Google Scholar]
- 27.Li M., Luo Y., Watson R., et al. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. 2021 doi: 10.1136/postgradmedj-2021-140195. postgradmedj-2021-140195. [DOI] [PubMed] [Google Scholar]
- 28.Woolf K., Melbourne C., Bryant L., et al. Protocol: the United Kingdom Research study into Ethnicity And COVID-19 outcomes in Healthcare workers (UK-REACH): protocol for a prospective longitudinal cohort study of healthcare and ancillary workers in UK healthcare settings. BMJ Open. 2021;11(9) doi: 10.1136/bmjopen-2021-050647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin CA, Pan D, Nazareth J, et al. Access to personal protective equipment in healthcare workers during the COVID-19 pandemic in the United Kingdom: results from a nationwide cohort study (UK-REACH). medRxiv 2021. [DOI] [PMC free article] [PubMed]
- 30.Graneheim U.H., Lindgren B.M., Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34. doi: 10.1016/j.nedt.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 32.Miles MB, Huberman AM Qualitative data analysis: an expanded sourcebook: sage; 1994.
- 33.Service . Primary Principles: Ethnic Group; 2016. Harmonised Concepts and Questions for Social Data Sources. GS. [Google Scholar]
- 34.Martin L.R., Petrie K.J. Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med. 2017;51(5):652–660. doi: 10.1007/s12160-017-9888-y. [DOI] [PubMed] [Google Scholar]
- 35.Duffy B.A., D. Covid conspiracies and confusions: the impact on compliance with the UK's lockdown rules and the link with social media use: the Policy Institute, King's College London 2020.
- 36.StataCorp. Stata statistical software: release 17. College Station, TX: StataCorp LLC; 2021.
- 37.National Health Service. NHS Workforce. 2021. https://www.ethnicity-facts-figures.service.gov.uk/workforce-and-business/workforce-diversity/nhs-workforce/latest. Accessed 11 February 2021.
- 38.Government; U. Ethnicity Facts and Figures. 2022. https://www.ethnicity-facts-figures.service.gov.uk/. Accessed 4 February 2021.
- 39.UK Health Security Agency. SARS-CoV-2 variants of concern and variants under investigation in England. In: Care; DoHaS, editor.; 2021.
- 40.Institute for Government. Timeline of UK government coronavirus lockdowns. 2021. https://www.instituteforgovernment.org.uk/charts/uk-government-coronavirus-lockdowns. Accessed 22 December 2021.
- 41.Wise J. Covid-19: European countries suspend use of Oxford-AstraZeneca vaccine after reports of blood clots. BMJ. 2021;372:n699. doi: 10.1136/bmj.n699. [DOI] [PubMed] [Google Scholar]
- 42.Diaz G.A., Parsons G.T., Gering S.K., Meier A.R., Hutchinson I.V., Robicsek A. Myocarditis and pericarditis after vaccination for COVID-19. JAMA. 2021;326(12):1210–1212. doi: 10.1001/jama.2021.13443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dagan N., Barda N., Biron-Shental T., et al. Effectiveness of the BNT162b2 mRNA COVID-19 vaccine in pregnancy. Nat Med. 2021;27(10):1693–1695. doi: 10.1038/s41591-021-01490-8. [DOI] [PubMed] [Google Scholar]
- 44.Griffin S. Covid-19: AstraZeneca vaccine prevents 79% of symptomatic disease and 100% of severe disease, US study finds. BMJ. 2021;372:n793. doi: 10.1136/bmj.n793. [DOI] [PubMed] [Google Scholar]
- 45.Harris R.J., Hall J.A., Zaidi A., Andrews N.J., Dunbar J.K., Dabrera G. Effect of vaccination on household transmission of SARS-CoV-2 in England. N Engl J Med. 2021;385(8):759–760. doi: 10.1056/NEJMc2107717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ganslmeier A., Engelmann T., Lucke M., Täger G., Pfeifer M., Scherer M.A. [Attitude of health care workers towards SARS-CoV-2 vaccination] MMW Fortschr Med. 2021;163(Suppl 5):12–16. doi: 10.1007/s15006-021-0139-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aldosary A.H., Alayed G.H. Willingness to vaccinate against Novel COVID-19 and contributing factors for the acceptance among nurses in Qassim, Saudi Arabia. Eur Rev Med Pharmacol Sci. 2021;25(20):6386–6396. doi: 10.26355/eurrev_202110_27012. [DOI] [PubMed] [Google Scholar]
- 48.Craxì L., Casuccio A., Amodio E., Restivo V. Who should get COVID-19 vaccine first? A survey to evaluate hospital workers' opinion. Vaccines. 2021;9(3) doi: 10.3390/vaccines9030189. (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fotiadis K., Dadouli K., Avakian I., et al. Factors Associated with Healthcare Workers’ (HCWs) Acceptance of COVID-19 vaccinations and indications of a role model towards population vaccinations from a cross-sectional survey in Greece, May 2021. Int J Environ Res Public Health. 2021;18(19):10558. doi: 10.3390/ijerph181910558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gönüllü E., Soysal A., Atıcı S., et al. Pediatricians' COVID-19 experiences and views on the willingness to receive COVID-19 vaccines: a cross-sectional survey in Turkey. Hum Vaccin Immunother. 2021;17(8):2389–2396. doi: 10.1080/21645515.2021.1896319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jain J., Saurabh S., Kumar P., et al. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. 2021;149:e132. doi: 10.1017/S0950268821001205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maltezou H.C., Pavli A., Dedoukou X., et al. Determinants of intention to get vaccinated against COVID-19 among healthcare personnel in hospitals in Greece. Infect Dis Health. 2021;26(3):189–197. doi: 10.1016/j.idh.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mayan D., Nguyen K., Keisler B. National attitudes of medical students towards mandating the COVID-19 vaccine and its association with knowledge of the vaccine. PLoS One. 2021;16(12) doi: 10.1371/journal.pone.0260898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ulbrichtova R., Svihrova V., Tatarkova M., Hudeckova H., Svihra J. Acceptance of COVID-19 vaccination among healthcare and non-healthcare workers of hospitals and outpatient clinics in the Northern Region of Slovakia. Int J Environ Res Public Health. 2021;18(23) doi: 10.3390/ijerph182312695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bell S, Clarke RM, Ismail SA, et al. COVID-19 vaccination beliefs, attitudes, and behaviours among health and social care workers in the UK: a mixed-methods study. medRxiv 2021: 2021.04.23.21255971. [DOI] [PMC free article] [PubMed]
- 56.Stead M., Critchlow N., Eadie D., Sullivan F., Gravenhorst K., Dobbie F. Mandatory policies for influenza vaccination: views of managers and healthcare workers in England. Vaccine. 2019;37(1):69–75. doi: 10.1016/j.vaccine.2018.11.033. [DOI] [PubMed] [Google Scholar]
- 57.Khunti K., Kamal A., Pareek A., Griffiths A. Should vaccination for healthcare workers be mandatory? J R Soc Med. 2021 doi: 10.1177/01410768211013525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Papineni P.F., Martin I., Matharoo M., et al. Trusted messengers are key to encouraging vaccine uptake. BMJ Opin. 2021 S., BMJ. [Google Scholar]
- 59.Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. 2016 ; (1873-2518 (Electronic)). [DOI] [PubMed]
- 60.Pan D., Sze S., Minhas J.S., et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020:23. doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.The King's Fund. NHS workforce: our position. 26/02/2021 2021. https://www.kingsfund.org.uk/projects/positions/nhs-workforce2021).
- 62.Smith LE, Carter B. Parental preferences for a mandatory vaccination scheme in England; a discrete choice experiment. medRxiv 2021: 2021.12.22.21268231. [DOI] [PMC free article] [PubMed]
- 63.Martin CA, Pan D, Melbourne C, et al. Predictors of SARS-CoV-2 infection in a multi-ethnic cohort of United Kingdom healthcare workers: a prospective nationwide cohort study (UK-REACH). medRxiv 2021: 2021.12.16.21267934.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.