Introduction
The novel coronavirus, or SARS-CoV-2, is a potentially deadly virus that causes COVID-19 disease and has led to the current pandemic.1 It has affected virtually everyone in the world since its emergence in 2019, with social, economic, and health effects that will probably last long past the end of the pandemic. In the long term, the impact of this health and social crisis may fall disproportionately upon children. This review will first highlight systemic/institutional inequities accentuated by the pandemic for subgroups of vulnerable children. These include Asian Americans and Pacific Islanders (AAPI), Black and Latinx, Indigenous populations, refugee communities, those with disability and LGBTQIA+ youth. It will then examine the impact of COVID-19 on the lives of American children including the effects on poverty, food insecurity and housing instability. It then explores the disruptions in health care access and utilization, childcare, and education. It will then review the overarching implications for childhood mental health and well-being. Finally, it will provide a series of recommendations on how best to achieve a just and equitable recovery for families and children.
Since the onset of the pandemic, over 12 million U.S. children have tested positive for COVID-19 as of January 2022, representing 18.9% of all COVID-19 cases.2 Children can become seriously ill, sometimes developing pulmonary illnesses that result in hospitalization and, infrequently, death. A small number of children develop Multisystem Inflammatory Syndrome-Child (MIS-C), presumed to be similar to the autoimmune Steven Johnson Syndrome.3 Despite uncertainty regarding the long-term effects of COVID-19 infections in children as well as the direct and indirect effects on children's well-being, children 5 years and older were not approved for vaccination until November 2021, and await approval for children under the age of 5 years.4
The pandemic has amplified multiple layers of entrenched health inequity, demonstrated by subgroups of vulnerable children that have been affected disproportionately. Health inequity is defined as differences in the health status of different population groups based on societal differences resulting in significant social and economic costs for individuals, families, communities and societies.5 Disparities frequently result in specific adverse health disparities that exist across sub-groups of the population.6 These disparities are frequently associated with specific demographic markers (e.g. income, race, ethnicity and gender), as well as with other social determinants such as access to care, housing instability, food insecurity, geography, transportation, and the built environment. Together they may affect families’ ability to secure adequate levels of shelter, nutrition, and health care for their children and to maintain adequate family income. Other factors that adversely affect children include violence against children, exposure to parental intimate partner violence, psychological distress, parental depression, and low self-esteem.7 Therefore, childhood health inequities need to be examined from the perspective of adverse health outcomes and the disproportionate burden placed on vulnerable families.
Systemic inequities accentuated by the pandemic
The COVID-19 pandemic has had a more significant negative effect on children in Black, Latinx, and Indigenous communities, as well as children with disabilities, and refugee or immigrant communities compared to more advantaged children.
Alt-text: Unlabelled box
This reflects persistent systemic inequities.8, 9, 10
The pandemic has amplified children's exposure to racism, xenophobia, and the negative effects of COVID-19 for a number of vulnerable communities and the children who are growing up within them.11 As the first cases of the novel coronavirus reached U.S. communities, suspicion of Asian Americans and Pacific Islanders (AAPI) followed close behind. With racialized language for the virus populating news (e.g., the “China Virus”) and political discourse from the local to the federal level the country's AAPI population suffered the economic consequences before the rest of the U.S. due to this xenophobia. By January of 2020, the earnings of New York's Chinatown neighborhoods dropped 50–70% compared to pre-pandemic earnings.12 In some cases, anti-AAPI discrimination has risen to the level of hate crime, with over 1700 such acts reported the first two months of American pandemic lockdowns.13 In addition, racialized vandalism, acid attacks, and even attempted murder of children occurred.14 In a 2020 survey of Chinese American parents and children, nearly half of participants reported concerns of racial discrimination and 71.1% of youth perceived bias against Chinese Americans related to COVID-19.15
Black and Latinx families and their children, owing to centuries of oppressive social, political, and economic practices, are less likely to own adequate health insurance and more likely to experience chronic health conditions that can worsen clinical COVID-19 outcomes.16 Native Americans experience COVID-intensifying chronic health conditions such as diabetes and asthma at rates much higher than those of their non-Indigenous counterparts in the U.S.17 In many places, individuals who live on reservations have also had limited ability to comply with CDC recommendations that limit viral transmission, perhaps owing to crowded multigenerational living situations that preclude social distancing and, in some cases, places disconnected from utilities and/or running water for hand-washing.18 Though, mistrust of federal health messaging has at times complicated communities’ efforts to limit the virus’ spread, many Indigenous communities have launched highly successful COVID-19 campaigns, relying on the principles of tribal sovereignty and protection of older community members.19 However, public health research tailored for indigenous communities is often hindered by misreporting and lack of transparency in research. For example, Indian Health Service (IHS) and tribal health authorities have often not been notified of COVID-19 community fatalities, because these deaths occurring in non-IHS hospitals. Non-HIS hospital staff may misreport Native patients’ race up to 50% of the time.20 The result of these errors is that tribal authorities often lack the data to understand the impact of the pandemic on their local communities.21 The impact is cumulative. For every additional percentile of a county's population that is Native American, the COVID-19 case fatality rate (CFR) is higher than the nation's average by a factor of 2.61.22 In Montana in 2020, Native American communities suffered COVID fatalities at 3.8 times the rate of White communities.23 In Native American cultures, households may contain multiple generations, with older family members often helping with childcare.24 Further, many American Indian communities place high value on physical proximity to loved ones and neighbors, and perceived social support appears to buffer the relationship between historical traumatic losses and current psychosocial stress.25 For children, the loss of social support and the presence of parental mental health issues can comprise insults to cognitive, physical, and social development.26 For Native American adolescents, a sense of cultural discontinuity has been associated with poorer wellbeing.27 In the post-COVID era, Native American children may face the challenge of navigating their own identity with fewer elders and other adults to offer culture and language education and foster their development.
Refugee and immigrant families face a unique set of challenges resulting from the pandemic. They are more likely than native-born citizens to live on incomes below the poverty line.28 COVID-19 causes substantial disruptions in resettlement supports, such as services that provide transportation, cultural brokering, and translation during health care visits.29 In addition, immigration detainees and asylum seekers in holding have had to wait in cramped detention centers for up to three times as long as before the pandemic and are exposed to cramped and unhygienic conditions that enable dramatic spread of COVID-19.30 Bond hearings and habeas petitions have frequently been delayed due to the pandemic, resulting in longer stays in detention facilities.31 Families may be separated for longer periods during or after detention, risking damage to children's physical and mental health. In addition, undocumented immigrant families are ineligible for COVID-19 relief and may be fearful of the consequences of applying for or accepting government support.
A number of factors interact to amplify the vulnerabilities of children with disabilities. First, they are more likely than their peers to live in lower-income families and to belong to ethnic and racial minorities.32 These markers can increase their risk of receiving less than optimal care in medical settings. Children with disabilities face a heightened risk of abuse in the home, and the loss of classroom time. Children with disabilities in rural areas who have complex or extensive medical needs are less likely to attend pediatrician appointments owing to cost, unavailability of care, and infrastructure challenges like limited broadband access and transportation.33 The pandemic has amplified these factors.
It is estimated that 30% of youth in foster care identify as LGBTQIA+, along with 40% of homeless youth. Functionally homeless teens in particular face elevated risks of experiencing trafficking or engaging in “survival sex”.34 The pandemic has simultaneously exacerbated the need for social and housing support for LGBTQIA+ teens while restricting their access to these services. For example, one Washington D.C. shelter for LGBTQIA+ youth reported a threefold increase in intake volume during the first month of shutdowns, at the same time that youth shelters across the country were compelled to reduce their capacity due to social distancing guidelines. Mental health care has been particularly challenging to access during COVID. Youth from gender or sexual minority groups who experience rejection within the home have higher risks of psychopathology and substance use. Such experiences are associated with a six-fold increase in LGBTQIA+ youth's rates of depression and an eight-fold risk of suicide attempts, compared to youth whose families provide greater acceptance of their children's identities.35 In addition, when parental mental illness goes untreated, children are at a higher risk of psychopathology, as well as poorer social and physical developmental outcomes.36
Inequities of basic needs & vital services for children
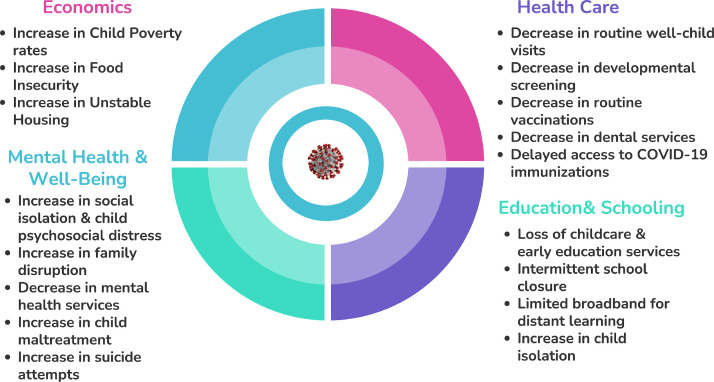
Inequities result in children being denied their basic needs and vital services such as economic security, health care access and utilization, providing education and schooling as well as support for mental health and psychosocial well-being of children.
Alt-text: Unlabelled box
Fig. 1 depicts inequities that threaten the health and well-being of children and youth in the United States.
Fig. 1.
COVID-19: Increasing child Inequities.
Economics: poverty, food insecurity and housing instability
The impact of the COVID-19 pandemic on the economic lives of families with children is very concerning. This is the third major economic downturn since the start of the 21st Century. The first recession began in 2001 and lasted for 10 months. The Great Recession, began in December of 2007 and lasted approximately 18 months, followed by a slow job recovery that persisted into the second decade of this century and an economic downturn that disproportionately affected children.37 Data from the Great Recession indicate that children whose parent's lost jobs have had lower earnings on average and are less likely to graduate from high school, with stronger effects on families with the lowest incomes.38
At the start of the Millennium the overall poverty rate for children less than 18 years of age in the United States was 16.2%; by 2009, it had increased to 20.7% due to the Great Recession.39 By 2019, the recovery had decreased he child poverty rate to 14.4%.40 Now families face yet another economic downturn brought on by the COVID-19 pandemic. Once again, there have been unusually high and rapid increases in unemployment. As of October 2020, more than 10 million unemployment cases had been filed in the United States.41 In addition, in December of 2021, 3.1 million persons reported that they had been unable to work because their employer had closed or lost business during the pandemic.42 It is estimated that the child poverty rate will increase to 17.1% in early 2022.43
In 2020, more than two thirds of COVID-19 fatalities in the U.S. occurred in households earning below median income.44 Adult unemployment and income loss during the pandemic may have adverse effects on children that last beyond the pandemic itself. Due in part to long-term systemic disparities in nutrition, housing quality, and insurance, the burden of the pandemic has fallen heavily on poorer Americans. COVID-19 has exacerbated the American wealth gap, with some estimates projecting an additional 7 million children experiencing food insecurity as a result of the crisis.45
COVID-19′s economic impact has been unevenly distributed in American society, with income loss resulting from shutdowns and illness particularly pronounced in families of color, such as Black and Hispanic adults and their children.46 In April 2020, Asian Americans with lower education attainment were 5.8% more likely than their low income White counterparts to have lost employment — a higher likelihood than any other racial subgroup measured — and alao experienced very slow employment regrowth, especially among lower-wage workers.47 , 48 These income losses exposed large groups of children to new and deeper family-level and community-level poverty.
Families living in poverty may have difficulty providing for needs like stable housing and food security — that is, access to enough food for active, healthy lives for all family members. For the 2.5% of children in the U.S. who face housing instability and homelessness, distance learning has often been impossible.49 In addition, families living in shelter environments often have limited ability to social distance, and therefore they have increased risk of infections and chronic conditions that may exacerbate the health consequences of the pandemic.50
Prior to the pandemic, there were more than 35 million persons living in food-insecure households, including 11 million children with Black families 2.4 times more likely to live in food insecure households as compared to White individuals (19.2% vs 8.1%).51 Black and Native communities experience higher rates of food insecurity compared to white families driven by higher levels of poverty and unemployment and inconsistent state policies. Due to the pandemic it was projected that there would be a significant increase in food insecure homes to 42 million homes including 13 million children experiencing food insecurity in 2021.52 Feeding America projected that 18 of the 25 counties with the highest food insecurity rates were in counties with predominant African Americans communities.53 Further, Black adults are more likely to have in-person employment that make them more vulnerable to the virus itself and the ensuing economic downturn.54 In addition, families face a culmination of multiple difficulties including not only job loss, but the need to care for children and ill family members.
The immediate rise in unemployment and income insecurity has placed a burden on families trying to maintain monthly rent and mortgage payments. It is well established that racial discrimination and economic disparities have long existed in the United States.55 Among families experiencing homelessness, 78% identify as non-white or Hispanic.56 In addition, persons with precarious housing situations who rely on “couch surfing”, that is individuals who find various couches to sleep on and homes to survive in until they are asked to leave (e.g., doubled-up housings where multiple families share a living space) are at particular risk during a pandemic.57 Families living in shelter environments frequently have limited ability to social distance, and they have heightened risk of infections and chronic conditions that may worsen the adverse health effects of the pandemic.58
To blunt the economic toll the pandemic has had on families with children, the Biden Administration and Congress passed the American Rescue Plan Act of 2021, with provisions to assist American families. The major anti-poverty provision was an increase in the Child Tax Credit, raising the amount from $2000 per child to $3000 for children between the ages of 6–17 years of age and $3600 per child for those under the age of 6.59 In addition, rather than a lump sum payment at the end of the year after annual taxes are completed, half of the amount is being distributed in monthly payments. More than 39 million households covering 90% of children in the United States are benefiting from this change. The renter eviction moratorium has also been a major policy initiative providing assistance for families. Initially put in place during the Trump Administration, it was extended by President Biden through July 2021 and then extended once again. Surveys show that 18.4% of all tenants owe back rent with the percentage of Black tenants at 32.9%.60
Undocumented immigrants and their 3.8 million U.S.-born children did not receive the COVID-19 emergency payment.61 Latina immigrant women born outside of the U.S. had unemployment rates over 22% in April 2020, experiencing a disproportionate rate of family income loss compared to non-immigrant families.62 Although they may be left out of federal financial stimulus programs, 74% of undocumented immigrants and 70% of refugees are “essential” workers, often incurring risk of virus transmission without receiving benefits such as hazard pay or guaranteed childcare.
Inequity in health care worsened by COVID
The pandemic has had a significant impact on both inpatient and outpatient healthcare utilization by children. Despite 95% of the 78 million children in the USA being insured through programs such as Medicaid, the Children's Health Insurance Program (CHIP), Tricare, and individual commercial health insurance, many children continue to lack comprehensive access to health services.63 This is due to either being uninsured and an increased number of children who are underinsuranced as the result of high deductibles, co-payments, and other out-of-pocket expenses.64 In addition, there are nonfinancial social factors such as lack of parental time to schedule routine visits, lack of transportation to health care appointments, lower health literacy levels and a paucity of clinics in nearby neighborhoods that limit access to care.65 The COVID-19 pandemic produced yet another hurdle to health care access for children who at baseline have barriers to routine preventive and acute care visits. Acute COVID symptoms, along with associated syndromes like Multisystem Inflammatory Syndrome in Children (MIS-C), are higher in Black and Latinx children than in their White counterparts, with 73.6% of MIS-C in the U.S. affecting Black and Latinx children.66 These youth are also disproportionately likely to be admitted to intensive care units.67
Due to the threat of COVID-19, parents and other caregivers continue to be faced with the challenging decision whether to delay acute care needs of their child or present to the hospital and risk exposure to this deadly virus. A recent study by Markham and colleagues examined inpatient hospitalizations pre-pandemic and during March-August 2020). The study documents a decrease in the median number of children's hospitalizations of 35.2%. In addition, disease specific rates decreased by 81.3% for asthma, 80.1% for bronchiolitis and 71.4% for pneumonia.68 A similar decrease has been observed for emergency visits with a decrease of 45.7% from pre-pandemic levels and a disease specific decrease in respiratory disorders by 70.0%.69
For low-income children on Medicaid and the Child Health Insurance Program (CHIP), the Centers for Medicare and Medicaid Services saw a significant reduction in outpatient services during the pandemic. Specifically, 69% fewer (7.6 million) dental services were rendered, as well as 44% fewer (3.2 million) child screening services that assess physical and cognitive development, 44% (6.9 million) fewer outpatient mental health services and 22% fewer (1.7 million) vaccinations up to age 2 years of age.70 Researchers have examined the impact of COVID-19 on childhood and adolescent vaccinations through review of the Vaccines for Children (VFC) program and by September 2020 reported a substantial decline in the routine ordering of pediatric vaccines.71 In addition, the CDC conducted a review of 10 states with high-performing immunization information systems and saw a significant decrease in the administration of routine and childhood and adolescent vaccines between March-September 2020.72 As of January 2022, COVID-19 immunization rates for children 5–11 years of age lagged significantly compared to older children 12–17 years and adults due to concerns for safety, necessity and efficaciousness.73 Only 5.7 million U.S. children ages 5–11 years or 20% are fully vaccinated.74
Virtual visits and remote care options were implemented in many practices, but internet access in the U.S. varies across social groups, further widening the care gap for those in disadvantaged circumstances. In addition, issues of privacy, safety and multilanguage interpretive services accentuate this gap.75
COVID-19 fatality rates increase with a county's rurality, largely due to a lack of infrastructure for disease surveillance and lower hospital resources, such as staff and ventilators.76 In 2020, case fatality ratios (CFR) were 1.79 standard deviations higher in rural counties than in the average American county.77 Before COVID, families in rural settings already reported practical barriers to obtaining healthcare for their children.78 Many children receive their primary care at school.79 The pivot to telehealth as the main means of healthcare delivery, necessitated by the shutdowns, decreased access to healthcare for families without adequate technology or internet access, many of whom already had to drive long distances to access public Wi-Fi for online learning.80
Child care and early childhood education
Quality childcare and early childhood education offer immediate and long-term benefits to children and their communities.81 In March 2020, 21 million children in the U.S. began staying home from daycares and preschools. For children of nearly all backgrounds, this represented a disruption to learning, since early cognitive development benefits from a diversity of stimulating environments.82 Many children are enrolled in programs such as Head Start, which aims to support the healthy welfare and development of children from lower-income families. Early childhood programs such as Head Start are associated with higher cognitive and socio-emotional functioning in children and improved mental health.83 Despite the best efforts of care providers to support children virtually, their service disruption in 2020–2021 is concerning for developmentalists.84
A significant portion of children under five in the U.S. receive “informal” childcare, such as through grandparents or neighbors, with infants and toddlers particularly likely to rely on informal caregivers as the primary source of nonparental care. Informal caregiving is often more affordable, accessible, and culturally harmonious, and has documented benefits for the employment trajectories of single mothers.85 However, many of these arrangements ceased in 2020–2021. Older adults and those from racial and ethnic minority groups faced heightened risk of COVID-19 complications, and many died or suffered long-term health effects from the virus, while others stopped providing informal care out of caution.86
With the loss of childcare, many parents reduced their work hours to care for young children at home, with the dual effects of lowering family income and also increasing the gender gap in wages.87 Meanwhile, Black Americans are overrepresented in industries deemed “essential” during the pandemic thus making it essential to find childcare while working from home during the pandemic.88 Parents obliged to work in person have faced the difficult choice of leaving their children with little or no adequate supervision. In addition to reducing children's exposure to developmentally critical stimuli and social interactions, insufficient supervision creates physical injury risks. Preliminary data on pediatric trauma admissions indicate that burn injuries have become more frequent across the U.S. during COVID-19 shutdowns.89
Education & schooling
American schools have a critical role in facilitating children's socialization, social mobility, and education and their contributions cannot be underestimated. First, schools directly support children's physical well-being. In 2018, 14% of families with children in the U.S. faced food insecurity.90 The National School Lunch and Breakfast Program served 31 million American children daily, providing them with more nutritious meals than their counterparts from low-income families who did not receive school lunch.91 Physical education programs at school are associated with reductions in children's cardiometabolic risk factors.92 , 93 School-based primary care clinics reach over six million children annually in the U.S. and school nurses provide monitoring of children's chronic health conditions and support compliance with immunizations and routine primary care.94 Households with children (especially young children) are at high risk of energy insecurity, and during periods of heat and cold, schools offer students eight or more hours of shelter from the elements.95 , 96 While American students may face dangers at school like bullying and gun violence,97 some students find that their classrooms are safer than their homes and neighborhoods. Further, when a child is unsafe at home, school staff are the most likely people in a child's life to report suspected abuse or neglect.98
Older children, for whom shutdowns brought more independent time at home, are exposed to an intensifying set of health risks. The pandemic saw heightened obesity rates across age groups widening disparities in terms of race and ethnicity, insurance, and neighborhood socioeconomic status widened.99 A confluence of factors contributed to these changes, such as lower parental supervision, disruption of school-delivered nutrition, more sedentary lifestyle, and higher amounts of media use. One commonality is that health behaviors during the past year have typically intensified the existing disparities among racial and socioeconomic groups. Obesity rates, for example, increased faster for children from lower-income backgrounds and those who are Hispanic and non-Hispanic Black.100 As early as preschool, black children are exposed to 50% more unhealthy food ads than their white counterparts.101 Black and Hispanic youth are exposed to almost twice as many advertisements for alcohol.102 There was also an increase in the rate of teens’ substance use.103 It has been estimated that between 232,000 and 1.1 million American high school students may be dropping out during the course of the pandemic due to the disruption in their schooling experience.104
Most parents, educators and clinicians are familiar with the “summer slide”, the loss of learning that many students display upon returning to school following summer vacation. Notably, the slide is steeper for children from materially disadvantaged families, such that the achievement gap widens following prolonged absence from school.105 In places where school closures (or voluntary remote learning) have been longest, COVID-19 is likely to result in the highest achievement gap for children from low-resourced compared to high-resourced families, with an average projected gap growth of 15–20%.106 Even when students are able to learn effectively remotely, they may lose exposure to experiences outside of their core curricula such as art and music.
One obvious factor in COVID-era educational disparities is a student's practical ability to attend class virtually. Many families face limitations in their home's floorspace, limiting children's privacy and focus.107 While 66% of people in the U.S. own smartphones, only an average of 61% of homes are fitted with high-speed internet access.108 The pivot to online learning in the spring of 2020 exposed a weakness in American infrastructure and brings to light the question of whether internet and technology access should be a public service or a service only available to those with adequate financial resources. Practical challenges often exist at the school level as well; only one in five American schools made plans for a prolonged closure by the outset of the pandemic and only 60% of schools with high student poverty had distributed electronic devices to children who needed them.109 In one study, 30.9% of teachers reported that their students lacked access to personal devices and lacked access to high-speed internet interfered with instruction.110 It is worth noting, though, that even when all students attend class virtually, the achievement gap may still widen. Due to the lack of immediate feedback in virtual classrooms, the students least resourced (nutritionally, materially, academically, emotionally) for a day's learning do not receive individualized support during class activities or instruction, and thus may fall behind.
As challenging as distance learning may be for any young child, it is especially difficult for children who would typically receive one-on-one visual, audio, processing, social, or attentional support in their classrooms, since online educational platforms may lack the capacity to deliver these services.111 Furthermore, many children, including 1.2 million under the age of six years, receive special education support, and many parents do not have the training or capacity to provide that support.112 Some children rely on specialty equipment for physical and occupational therapy and they stopped receiving those services in school during the outbreaks, while other families no longer have the means to afford these appointments in the private sector, owing to a loss of parental employment and insurance.113
Specific factors related to school closures have affected child development. The U.S. has suffered economic losses due to school closures. Preliminary estimates from the summer of 2020, informed by past school closures as well as those of 2020–2021, project that this current disruption will cost the U.S. $2.5 trillion in GDP, or $1337 annual loss in the future earnings of the average child who stayed at home during these two school years.114 As described above, school closures have direct effects on children's safety, mental health, and education. They also carry the risk of indirect developmental insults, through family- and community-level processes. When children are very young or otherwise unable to care for themselves, working parents may relinquish employment outside of the home to tend to children, which reduces earnings.115 Loss of childcare and schooling has had adverse outcomes on women's employment in particular, especially for families with low paternal involvement in child care work.116 The gender discrepancy in unemployment, most obvious at the outset of the pandemic in the U.S., is likely to continue for some time. This reflects a larger number of households with children experiencing income strain and poverty and, potentially, the developmental risks that accompany financial instability and family stress.117
As these children grow, they will enter a social and financial landscape that continues to reflect the effects of the pandemic. Positive neighborhood experiences predict higher future earnings and socioemotional competence.118 but when poverty and disorganization concentrate in a neighborhood, children face more barriers to academic achievement and higher risks of internalizing psychopathology, above and beyond the effects of family income. Neighborhood poverty has been associated with an increase in COVID-19 incidence, severity, and fatality, so communities already affected by poverty have seen more social and economic disruption during the pandemic.119
School closures have made it more challenging for recently arrived refugee children to access resources such as language-learning, social support, and acculturation experiences that might help them navigate the transition to life in the U.S. For youth in particular, school-based supports such as affirming teachers, clubs, and friend groups are likely to be primary loci of resilience outside the home.120 For the two thirds of LGBTQIA+ youth who do not receive identity-affirming support from their immediate families, school closures bear dual risks: First, closures isolate them from these social networks, and second, school closures result in more time spent at home with the stressors of family rejection.121
Child mental health & psychosocial well-being
Concomitant with the changes discussed above regarding the care and education of young children there has also been a profound impact on their mental health and psychosocial wellbeing. Although most new studies that examined COVID-19 have focused on its clinical characteristics and epidemiology, comparatively fewer publications have analyzed the psychosocial impact of the virus, and most of those have focused on adults. Recently, two survey studies from China found that 35–54% of respondents reported the impact of COVID-19 as moderate-to-severe with respect to psychosocial distress.122 , 123
Recent decades have seen a renewed investment by educators, researchers, and policy makers in schools’ role in supporting positive emotional and social growth trajectories in their pupils.124 To date, 29 U.S. states have established standards for social and emotional learning in schools.125 Even when schools do not explicitly implement social and emotional learning curricula, classrooms often offer students an education in these principles simply by situating a child in a network of peer and adult relationships in which they learn norms of emotion regulation and social awareness.126 A sense of belonging at school is associated with a range of positive academic and psychosocial outcomes, such as lower risk-taking behavior and higher self-esteem.127 When schools function as intended they improve children's social skills, identity formation, and mental health.128 When schools closed during the COVID-19 pandemic, 78 million children in the U.S. were suddenly estranged from these developmental resources.
A growing body of research that supports the importance of positive childhood experiences has emerged. Adverse childhood experiences (ACE), as described by the Kaiser Permanente trial in 1998, are related to the later development of negative mental and physical health outcomes.129 Since many of the ACE's are immutable, positive experiences is a focus for children and youth at home and school.130 The impact of pandemic shutdowns and community lockdowns has severely disrupted extracurricular activities and social gatherings that could offer these positive experiences to children. Even the mandates to “stop singing” due to aerosolized viral particles interferes with the positive day-to-day life of children.131
The plethora of family and individual stressors make careful monitoring of child and family well-being a priority during and following the pandemic. Economic and financial disruptions are also common during viral outbreaks with loss of income related to work closures or illness resulting in a major source of psychological distress. In a recent study from Canadian province of New Brunswick, 33% of the families reported that financial situation was significantly negatively affected by the pandemic.132
A major concern regarding child wellbeing during the pandemic is the potential increase in child maltreatment. Researchers recently analyzed data from nine pediatric trauma centers between March and September of 2020 and reported that physical abuse of school-aged children tripled during the early months of the pandemic.133 The most common injury identified was head injury, followed by a mix of chest, abdomen, extremity and burn injuries. Preliminary results show that the incidence of child sexual abuse may have increased 85% during school closures, and that child maltreatment has occurred at a higher frequency and acuity.134 In addition, intimate partner violence has increased in frequency during the pandemic, with more time at home, children have more exposure to adults’ conflicts.135 It is also suspected that owing to increased family stress, the incidence of abuse and neglect has increased during this period, but reports and allegations have declined substantially. This may be due to the fact that during school closures, children lack interaction with mandatory reporters such as teachers and school social support personal suggesting a staggering number of children whose experiences of maltreatment go unnoticed.
The early adolescent period is one of heightened vulnerability to psychopathology, and it is estimated that half of lifetime mental health conditions are diagnosable by age 14 years.136 Approximately 20% of adolescents show signs of intense emotional difficulty. Support from and connectedness to peers is associated with lower symptoms of depression and other disorders for adolescents, so youth at risk for clinical disorders may have suffered particularly from the relational distance of the COVID-19 pandemic.137 Furthermore, school counselors are typically mental health support counselors, and in rural areas, they may be a child's source of clinical care. The experience of quarantine and shutdown is itself traumatic for youth. For example, during the SARS outbreak in Canada, children who underwent quarantine had PTSD rates that were four times higher than those of their peers.138
One of the most alarming trends has been the increase in youth suicide attempts during the pandemic, especially among adolescent females.139 The CDC has reported that emergency room mean number of visits for suicide attempts increased by 26.2% for girls aged 12–17 in the summer of 2020 compared to 2019. In addition, in March of 2021, mean weekly ED visits for suspected suicide attempts was 50.6% higher compared to the same period in 2019.140 Adolescents may be particularly affected by an increase in anxiety and decrease in social connectedness to peers and teachers and a decrease in access to mental health services as a result of the pandemic. Finally, the loss of a loved ones places a significant burden on the well-being of children.
It has been estimated that one U.S. child loses a parent or caregiver for every four COVID-19 associated deaths. Between April 2020 to June 2021, over 140,000 children in the U.S. lost a parent or grandparent caregiver as a result of the pandemic.
Alt-text: Unlabelled box
The magnitude of the mental health impact of the pandemic has resulted in the U.S. Surgeon General, the American Academy of Pediatrics and other child health organizations recently declaring a mental health crisis for children, in large part due to the adverse impact of the pandemic.142 , 143
Creating an equitable & just recovery for children & youth
With a new surge in infection starting in the late summer of 2021 and extending into 2022, it is not obvious when the U.S. will be free from this illness. More than 4 million lives have been lost globally and this is probably an underestimate. The recovery should include efforts to minimize the damage that has occurred and to set a path for restoration for the lives of the children affected, particularly those most vulnerable.
Table 1 provides an overview of some of the strategies that will contribute to an equitable and just recovery for our children.
Table 1.
COVID-19: Recommendations for an equitable & just recovery.
| Family Economic Security |
|---|
|
|
|
| Health Care Access & Utilization |
|
|
|
|
|
| Education & Schooling |
|
|
|
|
|
|
|
| Mental Health & Psychological Well-Being |
|
|
|
|
Economic stability
The economic burden placed on families with children has been deleterious for their short- and long-term financial security and well-being. Federal and state governments should expand access to unemployment insurance for part-time, low-wage, and student workers. Leaders should consider eliminating barriers to accessing Temporary Assistance for Needy Families (TANF) to encourage people who are pursuing an education or job training to qualify and by remove limits on assistance to children born to parents already enrolled in the program. Maintaining and expanding the refundable Child-Dependent Tax Credit and make those changes permanent will support low resource families financially. Expand unemployment access to part-time, low wage & student workers. A livable wage that meets the basic needs facing families with children is an important factor in achieving and maintaining a family's economic stability.
Health care access & quality
There are millions of children who have missed vaccines and preventive well child visits. Families should be counselled on the need for scheduled well child visits and immunizations and prioritize catch-up visits for routine scheduled visits & recommended vaccinations. Providing safe environments to avoid exposure to COVID-19 during visits will be important. Of course, if large numbers of children remain unvaccinated for common childhood diseases (e.g., measles and pertussis) then community outbreaks could occur. A sudden increase in the need for vaccines may strain the vaccine supply chain. As discussed, the pandemic has adversely affected the development, mental health, and social circumstances of many children. Developmental and social/emotional screening tools may need to be re-supplied with training and support of newly hired staff.
Disparities in children's healthcare access, unmasked by the pandemic, can inform infrastructure changes. The identification of community-specific barriers that children and families face when accessing care continue to be an important area of child health research. This may include mapping primary care clinic sites to foster equitable distribution to primary care services. Primary care clinicians and community organizations can work together to educate families on the importance of routine preventive visits, immunizations, and age appropriate developmental and socio-emotional screening.144
The social disruptions over the last several years have been immense. Infrastructure that supports children remotely will help to minimize and protect them from future disruptions. The expansion of internet services to resource poor communities will improve access to virtual medical services. The rapid transition of health care system's capacity to shift to online and virtual medical services has been, in one sense, a triumph because it enabled virtual child health visits during the pandemic.145 However, it also widened the access gap among children and families with limited access to internet and personal electronic devices.146 Increasing families’ access to technology and in particular internet services may prove a potent public health intervention. Of course, in person child health visits remain critically important for child health. Finally, primary clinicians can work with other community leaders to dispel parents’ vaccine misconceptions.
Education & schooling
The impact of the pandemic on the schooling of America's children has been enormous, from the early care of infants and toddlers through primary and secondary education. Legislation that supports universal preschool for all 3- and 4-year-olds would be transformative. The cohort of young children whose preschool education was paused or never begun due to COVID closures may benefit from re-entering preschool programs and delaying kindergarten matriculation. Expanding eligibility and enrollment for quality early childhood programs following the COVID pandemic will greatly benefit young children.147
Summer school opportunities that promote catch-up learning can be effective. In 2020, New York quadrupled summer school access, and Tennessee has begun to recruit college-aged tutors for youth who are struggling academically on their return to school. In addition, children returning from shutdowns may benefit from a number of nonacademic resources, such as renewed attention to mental health and nutrition support. Public health experts have also suggested keeping buildings open for children whose caregiving, nutrition, and safety needs during the workday exceed families’ capacity.148
Mental health & wellbeing
The mental health and psychosocial wellbeing of children during the pandemic is a major concern. School staff can be instrumental in identifying nutritional or mental health needs and implementing trauma-informed classroom practices.149 There is a need to expand community based mental health services with greater access to screening and treatment for children's mental health and emotional problems. In both the classroom and community trauma informed practice includes utilizing a strength-based approach for vulnerable subgroups of children and youth. Trauma informed practice promotes trusting relations, acknowledges the widespread impact of trauma, recognizes the signs and symptoms of trauma in patients, families, and staff and actively attempts to avoid re-traumatization.150 Maintaining access to activities outside of school is also important to promote strong mental health in childhood.
Conclusion
While COVID-19 has had a relatively low mortality rate in our children and youth, the immediate and long-term effects should not be underestimated. In addition to illuminating the inequities that have existed in the past, the pandemic has increased the stress and strain on families, systems, and existing resources more than ever imagined. Future waves of the pandemic and post-pandemic recovery for our children will need caring adults promoting children's access to quality health care, education, and safe environments to foster the physical and mental health of all children regardless of ethnicity.
Declaration of Competing Interest
The authors do not have any conflicts to declare.
References
- 1.Lee E.C., Wada N., Grabowski K., Gurley E.S., Lessler The engines of SARS-CoV-2 spread. Science. 2020;370:406–407. doi: 10.1126/science.abd8755. DOI: 10.1126/science.abd8755. [DOI] [PubMed] [Google Scholar]
- 2.Children and COVID-19: State-Level Data Report. American Academy of Pediatrics. 2022. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/.
- 3.Katlan B, Nakip O, Kesici S, Bayrakci B. Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 infection presenting with Steven Johnson Syndrome. Pediatric Critical Care Medicine, 2021; 22(Issue Supplement 1 3S:357. 10.1097/01.pcc.0000741300.46124.ac [DOI]
- 4.COVID-19 vaccines for children and teens. Center for Disease Control and Prevention, 2022 @ https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/children-teens.html?s_cid=11370:covid%20vaccine%20approved%20for%20children:sem.ga:p:RG:GM:gen:PTN:FY21
- 5.Health Inequities and their Causes. World Health Organization, 2018, @ https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes
- 6.Oberg C.N., Colianni S., King-Shultz L. Child Health Disparities in the 21st Century. Curr Prob Pediatr Adolesc Health Care. 2016;46:291–312. doi: 10.1016/j.cppeds.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Oberg C.N., Nathawad R., Raman S., Goldhagen J. Violence against children recognition, rights, responses. Pediatr Clin North Am. 2021;68:357–369. doi: 10.1016/j.pcl.2020.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Ismail S.J., Tunis M.C., Zhao L., et al. Navigating inequities: a roadmap out of the pandemic. BMJ Global Health. 2021;6 doi: 10.1136/bmjgh-2020-004087. 10.1136/bmjgh-2020-004087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Addressing Inequities in Education: Considerations for Black Children and Youth in the Era of COVID-19. Society for Research in Child Development (SRCD) Statement of the Evidence, 2020
- 10.Bhaskar S, Rastogi A, Menon KV, Kunheri B, Balakrishnan S. & Howick J. Call for action t address equity and justice divide Durint COVID-19. Frontiers in Psychiatry-Policy and Practice Reviews, 2020. 10.3389/fpsyt.2020.559905 [DOI] [PMC free article] [PubMed]
- 11.Marron Jonathan M. Structural Racism in the COVID-19 Pandemic: don't Forget about the Children! Am J Bioethics. 2021;21(3):94–97. doi: 10.1080/15265161.2020.1871114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen JA, Zhang E, & Liu CH. (2020). Potential impact of COVID-19–related racial discrimination on the health of Asian Americans, 2020; 110: 1624–1627. 10.2105/AJPH.2020.305858. [DOI] [PMC free article] [PubMed]
- 13.Choi C, & Kulkarni MP. (2020). For immediate release press statement In Six Weeks, STOP AAPI HATE Receives Over 1700 Incident Reports of Verbal Harassment, Shunning and Physical Assaults. www.a3pcon.org/stopaapihate.
- 14.Tessler H., Choi M., Kao G. The anxiety of being Asian American: hate crimes and negative biases during the COVID-19 Pandemic. Am J Criminal Justice. 2020;45(4):636–646. doi: 10.1007/S12103-020-09541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheah C.S.L., Wang C., Ren H., Zong X., Cho H.S., Xue X. COVID-19 racism and mental health in Chinese American Families. Pediatrics, 2020. 2020;2020021816:146. doi: 10.1542/PEDS.2020-021816. [DOI] [PubMed] [Google Scholar]
- 16.Racial and ethnic and ethnic disparities in access to health insurance and health care A Publication of the UCLA Center for Health Policy Research and the Theory J. Kaiser Family Foundation. Policy Research Report. 2000 [Google Scholar]
- 17.Villrroel M., Tainya C., Norris T. Health of American Indian and Alaska native adults, by urbanization level: united States, 2014-2018. NCHS Data Brief. 2020 no. [PubMed] [Google Scholar]
- 18.Hedgpeth D., Fears D., Scruggs G. Native Americans suffer the highest rates of diseases that make coronavirus lethal - The Washington Post. Washington Post. 2020 https://www.washingtonpost.com/climate-environment/2020/04/04/native-american-coronavirus/ [Google Scholar]
- 19.Burki T. COVID-19 among American Indians and Alaska Natives. Lancet Infect Dis 2021. 2021;21:325–326. doi: 10.1016/S1473-3099(21)00083-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bigback K.M., Hoopes M., Dankovchik J., et al. Using record linkage to improve race data quality for American Indians and Alaska Natives in Two Pacific Northwest State Hospital Discharge Databases. Health Serv Res. 2015;50(Suppl 1):1390. doi: 10.1111/1475-6773.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagle R. Native Americans being left out of US coronavirus data and labelled as “other” | Native Americans | The Guardian. Guardian. 2020 https://www.theguardian.com/us-news/2020/apr/24/us-native-americans-left-out-coronavirus-data. [Google Scholar]
- 22.Iyanda A.E., Boakye K.A., Lu Y., Oppong J.R. Racial/ethnic heterogeneity and rural-urban disparity of COVID-19 case fatality ratio in the USA: a negative binomial and GIS-based analysis. J Racial Ethn Health Disparities. 2021:1–14. doi: 10.1007/S40615-021-01006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williamson L.L., Harwell T.S., Koch T.M., et al. COVID-19 incidence and mortality among American Indian/Alaska Native and White Persons — Montana, March 13–November 30. Morbidity Mortality Weekly Rep. 2020;70:510. doi: 10.15585/MMWR.MM7014A2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kakol M., Upson D., Sood A. Susceptibility of Southwestern American Indian Tribes to Coronavirus Disease 2019 (COVID-19) J Rural Health, 2021. 2021;37:197–199. doi: 10.1111/JRH.12451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.John-Henderson N.A., Ginty A.T. Historical trauma and social support as predictors of psychological stress responses in American Indian adults during the COVID-19 pandemic. J Psychosom Res. 2020;139 doi: 10.1016/J.JPSYCHORES.2020.110263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manning C., Gregoire A. Effects of parental mental illness on children. Psychiatry, 2006. 2006;5:10–12. doi: 10.1383/PSYT.2006.5.1.10. [DOI] [Google Scholar]
- 27.Tlanusta Garrett M. Vol. 11. Perspectivas Sociales = Social Perspectives; 2009. pp. 41–67. (Acculturation and Wellness of Native American Adolescents in the United States of North America). ISSN-e 2007-9265, Vol. 11, No. 1-2Págs41–67. https://dialnet.unirioja.es/servlet/articulo?codigo=3651010&info=resumen&idioma=ENG. [Google Scholar]
- 28.Kerwin D, & Warren R. (2020). US Foreign-Born Workers in the Global Pandemic: essential and Marginalized, 2020; 8(3): 282–300. 10.1177/2331502420952752. [DOI]
- 29.Brickhill-Atkinson M., Hauck F.R. Impact of COVID-19 on Resettled Refugees. Prim Care. 2021;48:57. doi: 10.1016/J.POP.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marouf F.E. The impact of COVID-19 on immigration detention. Front Hum Dyn, 2021. 2021 doi: 10.3389/FHUMD.2020.599222. April 8, 2021. [DOI] [Google Scholar]
- 31.COVID-19 Habeas Litigation. National Immigration Justice Center. 2020. https://immigrantjustice.org/court_cases/covid-19-habeas-litigation.
- 32.van Dyck P.C., Kogan M.D., McPherson M.G., Weissman G.R., Newacheck P.W. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004;158:884–890. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- 33.Skinner A.C., Slifkin R.T. Rural/urban differences in barriers to and burden of care for children with special health care needs. J Rural Health. 2007;23:150–157. doi: 10.1111/J.1748-0361.2007.00082.X. [DOI] [PubMed] [Google Scholar]
- 34.Cohen R.I.S., Bosk E.A. Vulnerable youth and the COVID-19 pandemic. Pediatrics. 2020;146 doi: 10.1542/PEDS.2020-1306. [DOI] [PubMed] [Google Scholar]
- 35.Summers-Gabr N.M. Rural–urban mental health disparities in the United States during COVID-19. Psychol Traumay. 2020;12(S1):S222. doi: 10.1037/TRA0000871. [DOI] [PubMed] [Google Scholar]
- 36.Reupert A., Maybery D. Families affected by parental mental illness: a multiperspective account of issues and interventions. Am J Orthopsychiatry. 2007;77(3):362–369. doi: 10.1037/0002-9432.77.3.362. [DOI] [PubMed] [Google Scholar]
- 37.Oberg C.N. The great recession's impact on children. Matern Child Health J. 2011;15:553–554. doi: 10.1007/s10995-011-0807-8. [DOI] [PubMed] [Google Scholar]
- 38.Kalil A. Effects of the great recession on child development on JSTOR. Ann Am Acad Pol Soc Sci. 2013;650:232–249. https://www-jstor-org.ezp2.lib.umn.edu/stable/24541684?seq=6#metadata_info_tab_contents. [Google Scholar]
- 39.DeNavas-Walt C., et al. Income, Poverty, and Health Insurance Coverage in the United States: 2009. U.S. Government Printing Office; Washington, DC: 2010. U.S. Census Bureau, Current Population Reports, P60-238; p. 14. [Google Scholar]
- 40.Income, poverty, and health insurance coverage in the United States: 2019. September 15, 2020. Release number CB20-145
- 41.Jobless claims jump, hitting highest level since mid-August. CNBC, October 15, 2020. Accesses at https://www.cnbc.com/2020/10/15/weekly-jobless-claims.html.
- 42.Economic News Release-Employment Situation Summary. U.S. Bureau of Labor Statistics. 2022. https://www.bls.gov/news.release/empsit.nr0.htm.
- 43.Parolin Z., Collyer S., Curran M.A. Sixth Child Tax Credit Payment Kept 3.7 million Children out of Poverty in December. Child Poverty set to spike in January 2022 after expiration of monthly payments. Poverty Social Policy Brief. 2022;6:1–6. https://www.povertycenter.columbia.edu/publication/monthly-poverty-december-2021. [Google Scholar]
- 44.Seligman B., Ferranna M., Bloom D.E. Correction: social determinants of mortality from COVID-19: a simulation study using NHANES. PLoS Med. 2022;18 doi: 10.1371/journal.pmed.1003490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gundersen C., Hake M., Dewey A., Engelhard E. Food Insecurity during COVID-19. Appl Econ Perspect Policy. 2021;43:153–161. doi: 10.1002/AEPP.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parolin Z, Curran M, Matsudaira J, Waldfogel J, & Wimer C. (2020). Monthly poverty rates in the United States during the COVID-19 Pandemic.
- 47.Bartik AW, Bertrand M, Lin F, Rothstein J, & Unrath M. (2020). Measuring the labor market at the onset of the COVID-19 crisis. https://doi.org/10.3386/W27613
- 48.Kim A.T., Kim C.H., Tuttle S.E., Zhang Y. COVID-19 and the decline in Asian American employment. Res Soc Stratif Mobil. 2021;71 doi: 10.1016/J.RSSM.2020.100563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Haskett M.E., Armstrong J.M. APA Handbook of Contemporary Family psychology: Applications and Broad Impact of Family Psychology. American Psychological Association; 2019. The experience of family homelessness; pp. 523–538. In B. H. Fiese, M. Celano, K. Deater-Deckard, E. N. Jouriles, & M. A. Whisman (Eds.) [Google Scholar]
- 50.Perri M., Dosani N., Hwang S.W. COVID-19 and people experiencing homelessness: challenges and migration strategies. Can J Med Assoc J. 2020;192:E716–E719. doi: 10.1503/cmaj.200834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.The Impact of the Coronavirus on Food insecurity in 2020. Feeding America, Updated October 2020.
- 52.The Impact of the Coronavirus on Food Insecurity (2020 & 2021) Feeding America. 2021. https://www.feedingamerica.org/sites/default/files/2021-03/National%20Projections%20Brief_3.9.2021_0.pdf.
- 53.Coleman-Jensen Alisha, Rabbitt Matthew, Gregory Christian, Singh Anita. U.S. Department of Agriculture, Economic Research Service; 2020. Household Food Security in the United States in 2019, ERR-275. [Google Scholar]
- 54.Weller C.E. African Americans face systematic obstacles to getting good jobs. Center Am Progr. 2019 [Google Scholar]
- 55.Coughlin C.G., Sandel M., Stewart A.M. Homelessness, Children, and COVID-19: a looming crisis. Pediatrics. 2020;146(2) doi: 10.1542/peds.2020-1408. [DOI] [PubMed] [Google Scholar]
- 56.US Interagency Council on Homelessness . US Interagency Council on Homelessness; Washington, DC: 2018. Homelessness in America: Focus on Families with Children. [Google Scholar]
- 57.Wilson, P. Couch surfing the waves of American Poverty, Current Affairs, November 2020, https://www.currentaffairs.org/2020/11/couch-surfing-the-waves-of-american-poverty.
- 58.Coughlin C.G., Sandel M., Homelessness Stewart AM. Children, and COVID-19: a Looming Crisis. Pediatrics. 2020;146 doi: 10.1542/PEDS.2020-1408. [DOI] [PubMed] [Google Scholar]
- 59.Fact Sheet: Biden-Harris Administration Announces Child Tax Credit Awareness Day and Releases Guidance for Unprecedented American Rescue Plan Investment to Support Parents and Health Child Development. White House, 2011. https://www.whitehouse.gov/briefing-room/statements-releases/2021/06/11/fact-sheet-biden-harris-administration-announces-child-tax-credit-awareness-day-and-releases-guidance-for-unprecedented-american-rescue-plan-investments-to-support-parents-and-healthy-child-dev/.
- 60.Ban on renter evictions during COVID-19 pandemic is extended. Associated Press, 2021. https://apnews.com/article/ban-renter-evictions-extended-coronavirus-covid-19-8bcf2635ef149b01f1c8aed69238b30f
- 61.Saenz R., Sparks C. The inequities of job loss and recovery amid the COVID-19 pandemic. Carsey Sch Publ Policy Scholars’ Repository. 2020 https://doi.org/https://dx.doi.org/10.34051/p/2021.3. [Google Scholar]
- 62.Capps R, Batalova J, and Gelatt J. COVID-19 and Unemployment: assessing the Early Fallout for Immigrants and other U.S. Workers. Migration Policy Institute Fact Sheet. 2020. https://www.migrationpolicy.org/research/covid-19-unemployment-immigrants-other-us-workers https://www.childrenshospitals.org/Issues-and-Advocacy/General/Fact-Sheets/Health-Care-Coverage-Sources-for-Americas-Children
- 63.Yu Justin, Perrin James M., Hagerman Thomas, Houtrow; Amy J. Underinsurance Among Children in the United States. Pediatrics. 2022;149 doi: 10.1542/peds.2021-050353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yu Justin, Perrin James M., Hagerman Thomas, Houtrow; Amy J. Underinsurance Among Children in the United States. Pediatrics. 2022;149 doi: 10.1542/peds.2021-050353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pascoe J.M., Wood D.L., Duffee, Kuo Mediators and adverse effects of child poverty in the United States. Pediatrics. 2016;137 doi: 10.1542/peds.2016-0340. [DOI] [PubMed] [Google Scholar]
- 66.Godfred-Cato S., Bryant B., Leung J., et al. COVID-19–associated multisystem inflammatory syndrome in children — United States, March–July 2020. Morbidity Mortality Weekly Rep. 2020;69:1074. doi: 10.15585/MMWR.MM6932E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Leeb R.T., Price S., Sliwa S., et al. COVID-19 Trends Among School-Aged Children — United States, March 1–September 19, 2020. Morbidity Mortality Weekly Rep. 2020;69:1410. doi: 10.15585/MMWR.MM6939E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Markham J.L., Richardson T., DePorre A., et al. Inpatient use and outcomes at children's hospitals during the early COVID-19 pandemic. Pediatrics. 2021;147 doi: 10.1542/peds.2020-044735. [DOI] [PubMed] [Google Scholar]
- 69.DeLaroche A.M., Rodean J., Aronson P.L., et al. Pediatric emergency department visits at US children's hospitals during the COVID-19 pandemic. Pediatrics. 2021;147 doi: 10.1542/peds.2020-039628. [DOI] [PubMed] [Google Scholar]
- 70.care Delayed. AAP responds to report on drop in pediatric visits in Medicaid. CHIP. AAP News. 2020 [Google Scholar]
- 71.Santoli J.M., Lindley M.C., DeSilva M.B., et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration— United States. MMWR 2020. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. PMID:32407298 https://doi.org/10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 72.Murphy B.P., Zell E., Kirtland K., et al. Impact of the COVID-19 Pandemic on Administration of selected routine childhood and adolescent vaccinations-10 US Jurisdictions. March-September 2020. MMWR. 2021;70:840–845. doi: 10.15585/mmwr.mm7023a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Suran M. Why parents still hesitate to vaccinate their children against COVID-19. JAMA. 2022;327:23–25. doi: 10.1001/jama.2021.21625. doi:10.1001/jama.2021.21625. [DOI] [PubMed] [Google Scholar]
- 74.Summary of data publicly reported by the Centers for Disease Control and Prevention. Children and COVID-19 vaccination trends. American Academy of Pediatrics, 1/26/2022. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends. 2022
- 75.Eyrich N.W., Andino J.J., Fessell D.P. Bridging the digital divide to avoid leaving the most vulnerable behind. JAMA Surg. 2021;156:703–704. doi: 10.1001/jamasurg.2021.1143. [DOI] [PubMed] [Google Scholar]
- 76.Pro G., Hubach R., Wheeler D., et al. Differences in US COVID-19 case rates and case fatality rates across the urban-rural continuum. Rural Remote Health. 2020;20:6074. doi: 10.22605/RRH6074. https://doi.org/10.22605/RRH6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Iyanda A.E., Boakye K.A., Lu Y., Oppong J.R. Racial/ethnic heterogeneity and rural-urban disparity of COVID-19 case fatality ratio in the USA: a negative binomial and GIS-Based Analysis [published online ahead of print, 2021 Feb 26] J Racial Ethn Health Disparities. 2021:1–14. doi: 10.1007/s40615-021-01006-7. doi:10.1007/s40615-021-01006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marcin J.P., Shaikh U., Steinhorn R.H. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79:169–176. doi: 10.1038/pr.2015.192. [DOI] [PubMed] [Google Scholar]
- 79.Hoffman J.A., Miller E.A. Addressing the consequences of school closure due to COVID-19 on children's physical and mental well-being. World Med Health Policy. 2020;12:300–310. doi: 10.1002/WMH3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Francom GM, Lee SJ, & Pinkney H. Technologies, Challenges and Needs of K-12 Teachers in the Transition to Distance Learning during the COVID-19 Pandemic. https://doi.org/10.1007/s11528-021-00625-5/Published 2022 [DOI] [PMC free article] [PubMed]
- 81.Heckman J.J. American Educator, Spring; 2011. The Economics of Inequality: The Value of Early Childhood Education. . https://eric.ed.gov/?id=EJ920516. [Google Scholar]
- 82.Anders Y., Rossbach H.G., Weinert S., et al. Home and preschool learning environments and their relations to the development of early numeracy skills. Early Childhood Res Q. 2012;27:231–244. doi: 10.1016/J.ECRESQ.2011.08.003. [DOI] [Google Scholar]
- 83.Harden B.J., Sandstrom H., Chazan-Cohen R. Early Head Start and African American families: impacts and mechanisms of child outcomes. Early Childhood Res Q. 2012;27:572–581. doi: 10.1016/J.ECRESQ.2012.07.006. [DOI] [Google Scholar]
- 84.Atiles JT, Dunlap RL, & Tester M. (2021). How Head Start Addressed COVID-19 Challenges. 2021, 97, 60–65. 10.1080/00094056.2021.1930931. [DOI]
- 85.Brady M. (2016). Gluing, catching and connecting: how informal childcare strengthens single mothers’ employment trajectories. 2016; 30: 821–837. 10.1177/0950017016630259. [DOI]
- 86.Pennington A.F., Kompaniyets L., Summers A.D., et al. Risk of Clinical Severity by Age and Race/Ethnicity Among Adults Hospitalized for COVID-19—United States, March–September 2020. Open Forum Infect Dis. 2021;8 doi: 10.1093/OFID/OFAA638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Collins C., Landivar L.C., Ruppanner L., Scarborough W.J. COVID-19 and the gender gap in work hours. Gender Work Org. 2021;28(S1):101–112. doi: 10.1111/GWAO.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Poteat T., Millett G.A., Nelson L.R.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann Epidemiol 2020. 2020;47:1–3. doi: 10.1016/J.ANNEPIDEM.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sanford E.L., Zagory J., Blackwell J.M., Szmuk P Ryan M., Ambardekar A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg 2021. 2021;56:918–922. doi: 10.1016/J.JPEDSURG.2021.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lancker W.V., Parolin COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Publ Health. 2020;5:e243. doi: 10.1016/S2468-2667(20)30084-0. https://doi.org/10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vernarelli J.A., O'Brien B. A vote for school lunches: school lunches provide superior nutrient quality than lunches obtained from other sources in a nationally representative sample of US children. Nutrients. 2017;9:924. doi: 10.3390/NU9090924. Vol. 9, Page 924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pozuelo-Carrascosa D.P., Cavero-Redondo I., Herráiz-Adillo Á., Díez-Fernández A., Sánchez-López M., Martínez-Vizcaíno V. School-based exercise programs and cardiometabolic risk factors: a meta-analysis. Pediatrics. 2018;142 doi: 10.1542/PEDS.2018-1033. [DOI] [PubMed] [Google Scholar]
- 93.Song J.H., Song H.H., Kim S. Effects of school-based exercise program on obesity and physical fitness of urban youth: a quasi-experiment. Healthcare 2021. 2022;9(3):358. doi: 10.3390/HEALTHCARE9030358. Vol. 9, Page 358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hoffman J.A., Miller E.A. Addressing the consequences of school closure due to COVID-19 on children's physical and mental well-being. World Med Health Policy. 2020;12:300–310. doi: 10.1002/WMH3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Harker Steele A.J., Bergstrom J.C. Brr! It's cold in here” measures of household energy insecurity for the United States. Energy Res Soc Sci. 2021;72 doi: 10.1016/J.ERSS.2020.101863. [DOI] [Google Scholar]
- 96.Koball H, & Jiang Y. (2018). Basic facts about low-income children: children under 9 years, 2016. 10.7916/D8-T97P-BF73. [DOI]
- 97.Rowhani-Rahbar A., Moe C. School shootings in the U.S.: what is the state of evidence? J Adolescent Health. 2019;64(6):683–684. doi: 10.1016/j.jadohealth.2019.03.016. https://doi.org/10.1016/J.JADOHEALTH.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 98.Baron E.J., Goldstein E.G., Wallace C.T. Suffering in silence: how COVID-19 school closures inhibit the reporting of child maltreatment. J Public Econ. 2020;190 doi: 10.1016/J.JPUBECO.2020.104258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jenssen B.P., Kelly M.K., Powel M., Bouchelle Z., Mayne S., Fiks A.G. COVID-19 and changes in child obesity. Pediatrics. 2021;147 doi: 10.1542/peds.2021-050123. /doi.org/10.1542/peds.2021-050123. [DOI] [PubMed] [Google Scholar]
- 100.Jenssen B.P., Kelly M.K., Powell M., Bouchelle Z., Mayne S.L. & Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021;147 doi: 10.1542/PEDS.2021-050123. [DOI] [PubMed] [Google Scholar]
- 101.Fleming-Milici F., Harris J.L. Television food advertising viewed by preschoolers, children and adolescents: contributors to differences in exposure for black and white youth in the United States. Pediatr Obes. 2018;13:103–110. doi: 10.1111/IJPO.12203. [DOI] [PubMed] [Google Scholar]
- 102.Collins RL, Martino SC, Kovalchik SA, Becker KM, Shadel WG, & D'Amico EJ. Alcohol advertising exposure among middle school–age youth: an assessment across all media and venues. 2016, 77, 384–392. 10.15288/JSAD.2016.77.384. [DOI] [PMC free article] [PubMed]
- 103.Dumas T.M., Ellis W., Litt D.M. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolescent Health. 2020;67:354–361. doi: 10.1016/j.jadohealth.2020.06.018. https://doi.org/10.1016/J.JADOHEALTH.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dorn, E, Hancock B, Sarakatsannis J, & Viruleg E. (2020). COVID-19 and student learning in the United States: the hurt could last a lifetime.
- 105.Alexander K.L., Entwisle D.R., & Olson L.S. Lasting consequences of the summer learning gap, 2016; 72: 167–180. 10.1177/000312240707200202. [DOI]
- 106.Kuhfeld M., Soland J., Tarasawa B., Johnson A., Ruzek E., Liu J. Projecting the Potential Impact of SOVID-19 School Closures on Academic Achievement. Educ Res. 2020;49:549–565. DOI: 10.3102/0013189X20965918. [Google Scholar]
- 107.Montacute R. (2020). Implications of the Covid-19 crisis for educational inequality.
- 108.Chiou L., Tucker C. Social distancing, internet access and inequality. Natl Bureau Econ Res. 2020 doi: 10.3386/W26982. [DOI] [Google Scholar]
- 109.Diliberti M., Schwartz H., Hamilton L., Kaufman J. Prepared for a Pandemic? How Schools’ Preparedness Related to Their Remote Instruction During COVID-19. Prepared for a Pandemic? How Schools’ Preparedness Related to Their Remote Instruction During COVID-19. 2020 doi: 10.7249/RRA168-3. [DOI] [Google Scholar]
- 110.Francom G.M., Lee S.J., & Pinkney H.Technologies, Challenges and Needs of K-12 Teachers in the Transition to Distance Learning during the COVID-19 Pandemic. https://doi.org/10.1007/s11528-021-00625-5/Published [DOI] [PMC free article] [PubMed]
- 111.Patel K. Mental health implications of COVID-19 on children with disabilities. Asian J Psychiatr. 2020;54 doi: 10.1016/J.AJP.2020.102273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Houtrow A., Harris D., Molinero A., Levin-Decanini T., Robichaud C. Children with disabilities in the United States and the COVID-19 pandemic. J Pediatr Rehabil Med. 2020;13:415–424. doi: 10.3233/PRM-200769. [DOI] [PubMed] [Google Scholar]
- 113.Warner-Richter M., & Lloyd C.M. (2020, August 6). Considerations for Building Post-COVID Early Care and Education Systems that Serve Children with Disabilities. Child Trends. Augusy 2020. https://www.childtrends.org/publications/considerations-for-building-post-covid-early-care-and-education-systems-that-serve-children-with-disabilities
- 114.Donohue J.M., Miller E. COVID-19 and School Closures. JAMA. 2020;324(9):845–847. doi: 10.1001/jama.2020.13092. https://doi.org/10.1001/JAMA.2020.13092. [DOI] [PubMed] [Google Scholar]
- 115.Armitage R., Nellums L.B. Considering inequalities in the school closure response to COVID-19. Lancet Global Health. 2020;8:e644. doi: 10.1016/S2214-109X(20)30116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Petts R.J., Carlson D.L., & Pepin J.R. A gendered pandemic: childcare, homeschooling, and parents’ employment during COVID-19. Gender, Work & Organization. 2021, https://doi.org/10.1111/GWAO.12614
- 117.Kalil A. Effects of the Great Recession on Child Development on JSTOR. Ann Am Acad Pol Soc Sci. 2013;650:232–249. https://www-jstor-org.ezp2.lib.umn.edu/stable/24541684?seq=6#metadata_info_tab_contents. [Google Scholar]
- 118.Shonkoff J., & Phillips D. (2000). From Neurons to Neighborhoods: the Science of Early Childhood Development - National Research Council, Institute of Medicine, Board on Children, Youth, and Families, Committee on Integrating the Science of Early Childhood Development - Google Books. [PubMed]
- 119.Thompson C.N., Baumgartner J., Pichardo C., et al. COVID-19 Outbreak — New York City, February 29–June 1, 2020. Morbidity Mortality Weekly Rep. 2020;69:1725. doi: 10.15585/MMWR.MM6946A2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Salerno J.P., Devadas J., Pease M., Nketia B., & Fish J.N. (2020). Sexual and Gender Minority Stress Amid the COVID-19 Pandemic: implications for LGBTQ Young Persons’ Mental Health and Well-Being, 2020; 135: 721–727. 10.1177/0033354920954511. [DOI] [PMC free article] [PubMed]
- 121.DeMulder J., Kraus-Perrotta C., Zaidi H. Sexual and gender minority adolescents must be prioritized during the global COVID-19 public health response. Sexual Reprod Health Matt. 2020;28:1. doi: 10.1080/26410397.2020.1804717. DOI: 10.1080/26410397.2020.1804717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Qiu J., Shen B., Zhao M., et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang C., Pan R., Wan X., et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hamilton L., Doss C. Supports for social and emotional learning in American Schools and Classrooms: findings from the American Teacher Panel. Supp Soc Emotional Learn Am Schools Classrooms. 2020 https://doi.org/10.7249/RRA397-1. [Google Scholar]
- 125.Positive Action. (n.d.). Social-Emotional Learning (SEL) Standards in All 50 States. Retrieved July 12, 2021, from https://www.positiveaction.net/blog/sel-standards.
- 126.Tom K. & Tom K. Measurement of Teachers’ Social-Emotional Competence: development of the Social-Emotional Competence Teacher Rating Scale. 2020, https://scholarsbank.uoregon.edu/xmlui/handle/1794/12351.
- 127.Allen K., Kern M.L., Vella-Brodrick D., Hattie J., Waters L. What schools need to know about fostering school belonging: a meta-analysis. Educ Psychol Rev. 2016;30:1–34. doi: 10.1007/S10648-016-9389-8. 1, 30. [DOI] [Google Scholar]
- 128.Clark H., Coll-Seck A.M., Banerjee A., et al. A future for the world's children? A WHO–UNICEF–Lancet Commission. Lancet. 2020;395:605–658. doi: 10.1016/S0140-6736(19)32540-1. https://doi.org/10.1016/S0140-6736(19)32540-1. [DOI] [PubMed] [Google Scholar]
- 129.Felitti V.J., Anda R.F., Nordenberg D., et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults-The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 130.Bethell C., Jones J., Gombojay N., Linkenback J., Sege R. Positive childhood experiences and adult mental and relational health in statewide sample. Jama Pediatric. 2019;173 doi: 10.1001/jamapediatrics.2019.3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.COVID-19 Scientific Advisory Group Rapid Evidence Reports. Topic: singing as a risk for transmission of SARS-CoV-2. Alberta Health Services, COVID-19 Scientific Advisory Group. 2020.
- 132.COVID-19 Survey . Personal communications Nb Social Pediatrics; 2022. New Brunswick, Canada. [Google Scholar]
- 133.Child Study: Abuse Rose During COVID Pandemic. U.W. News World Rep. 2021 [Google Scholar]
- 134.Salt E., Wiggins A.T., Cooper G.L., et al. A comparison of child abuse and neglect encounters before and after school closings due to SARS-Cov-2. Child Abuse Negl. 2021;118 doi: 10.1016/J.CHIABU.2021.105132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Piquero A.R., Jennings W.G., Jemison E., Kaukinen C., Knaul F.M. Domestic violence during the COVID-19 pandemic - Evidence from a systematic review and meta-analysis. J Crim Justice. 2021;74 doi: 10.1016/j.jcrimjus.2021.101806. https://doi.org/10.1016/J.JCRIMJUS.2021.101806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Knopf D., Park M.J., & Mulye, T.P. (n.d.). The Mental Health of Adolescents: a National Profile, 2008. Retrieved July 12, 2021, from http://www.forumfyi.org/Files/FF_
- 137.Roach A. Supportive Peer Relationships and Mental Health in Adolescence: an Integrative Review. 2018, https://doi.org/10.1080/01612840.2018.1496498 [DOI] [PubMed]
- 138.Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7:105–110. doi: 10.1017/DMP.2013.22. [DOI] [PubMed] [Google Scholar]
- 139.Hill R.M., Katrina Rufino, Kurian S., Saxena J., Saxena K., Williams L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. 2021; 147: e2020029280. 10.1542/peds.2020-029280 [DOI] [PubMed]
- 140.Yard E., Radhakrishnan L., Ballesteros M.F., et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12-25 Years Before and During the COVID-19 Pandemic—United States, January 2019-May 2021. Morb Mortal Wkly Rep. 2021;70:888–894. doi: 10.15585/mmwr.mm7024e1. DOI: http://dx.doi.org/10.15585/mmwr.mm7024e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hillis S.D., Blenkinsop A., Villaveces A., et al. COVID-19–associated orphanhood and caregiver death in the United States. Pediatrics. 2021;148(6) doi: 10.1542/peds.2021-053760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Protecting youth mental health, The U.S. Surgeon General's Advisory, 2021. Accessed @ https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
- 143.AAP A.A.C.A.P. CHA declares national emergency in children's mental health. AAP NEWS. 2021 Accessed @ https://publications.aap.org/aapnews/news/17718. [Google Scholar]
- 144.Henize A.W., Beck A.F., Klein M.D., Adams M., Kahn R.S. A road map to address the social determinants of heath through community collaboration. Pediatrics. 2015;136:e993–e1001. doi: 10.1542/peds.2015-0549. /doi.org/10.1542/peds.2015-0549. [DOI] [PubMed] [Google Scholar]
- 145.Curfman A., S McSwain S.D., Chuo J., et al. Pediatric telehealth in the COVID-19 pandemic era and beyond. Pediatrics. 2021;148 doi: 10.1542/peds.2020-047795. e2020047795. 10.1542/peds.2020-047795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Early J., Hernandez A. Digital disenfranchisement and COVID-19: broadband internet access as a social determinant of health. Health Promot Pract. 2021;22(5):605–610. doi: 10.1177/15248399211014490. [DOI] [PubMed] [Google Scholar]
- 147.Building a National Early Childhood Education System that Works. Learning policy institute, 2021. https://learningpolicyinstitute.org/sites/default/files/product-files/LPI_Early_Childhood_Education_2021_BRIEF.pdf
- 148.Schwabish J., Joo N., Spievack N., Waxman E. Urban Institute; April 2020. Strategies and Challenges in Feeding Out-Of-School Students.https://www.urban.org/sites/default/files/publication/102095/strategies-and-challenges-in-feeding-out-of-school-students.pdf [Google Scholar]
- 149.Cavanaugh, B. (2016). Trauma-informed classrooms and schools, 2016; 25: 41–46. 10.1177/107429561602500206. [DOI]
- 150.Griffin G. Defining trauma and a trauma-informed COVID-19 response. Psycholo Trauma. 2020;12(S1):S279–S280. doi: 10.1037/tra0000828. [DOI] [PubMed] [Google Scholar]