Abstract
Objective.
To provide a conceptual framework to guide investigations into burdens of noncancerous genitourinary conditions (NCGUCs), which are extensive and poorly understood.
Methods.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) convened a workshop of diverse, interdisciplinary researchers and health professionals to identify known and hidden burdens of NCGUCs that must be measured to estimate the comprehensive burden. Following the meeting, a subgroup of attendees (authors of this article) continued to meet to conceptualize burden.
Results.
The Hidden Burden of Noncancerous Genitourinary Conditions Framework includes impacts across multiple levels of well-being and social ecology, including individual (i.e., biologic factors, lived experience, behaviors), interpersonal (e.g., romantic partners, family members), organizational/institutional (e.g., schools, workplaces), community (e.g., public restroom infrastructure), societal (e.g., health care and insurance systems, national workforce/economic output), and ecosystem (e.g., landfill waste) effects. The framework acknowledges that NCGUCs can be a manifestation of underlying biological dysfunction, while also leading to biological impacts (generation and exacerbation of health conditions, treatment side effects).
Conclusions.
NCGUCs confer a large, poorly understood burden to individuals and society. An evidence-base to describe the comprehensive burden is needed. Measurement of NCGUC burdens should incorporate multiple levels of well-being and social ecology, a life course perspective, and potential interactions between NCGUCs and genetics, sex, race, and gender. This approach would elucidate accumulated impacts and potential health inequities in experienced burdens. Uncovering the hidden burden of NCGUCs may draw attention and resources (e.g., new research and improved treatments) to this important domain of health.
Keywords: noncancerous genitourinary conditions, benign genitourinary conditions, urologic conditions, bladder health, urologic methods, conceptual framework, research framework, research modeling, social ecological model, burden
Noncancerous genitourinary conditions (NCGUCs, Table 1) encompass conditions of the urinary and genital systems not directly caused by cancer, or indirectly caused by cancer or its treatment. NCGUCs are prevalent and lead to significant burden across all stages of life and genders. In the United States (U.S.), 1 of 2 women and 1 of 6 men report urinary incontinence (UI), with the highest prevalence at older ages.1 Overactive bladder (OAB), characterized by frequency, nocturia, and urgency, with or without UI, is estimated to affect over 1 in 10 women and men worldwide.2 Infants and young children can develop vesicoureteral reflux, which occurs in one-third of children with febrile urinary tract infections (UTIs).3 Neurogenic bladder, stemming from causes as varied as spinal cord injury, spina bifida, diabetes mellitus, stroke, and traumatic brain injury, can lead to a wide array of urinary issues.4 In addition to being a possible manifestation of other health conditions, NCGUCs can generate or exacerbate coexisting health conditions.5–8 Timely identification and treatment of NCGUCs may thus contribute to the prevention and management of multiple chronic conditions, a U.S. national health priority.9
Table 1.
Selected noncancerous genitourinary conditions.
| Bladder Outlet Obstruction | |
| Chronic Pelvic Pain | |
| Congenital Conditions (e.g., Hypospadias Vesicoureteral reflex, Ureteropelvic junction obstruction) | |
| Dysfunctional Voiding | |
| ♂ | Ejaculatory Dysfunction |
| ♂ | Erectile Dysfunction |
| Fecal Incontinence | |
| ♀ | Female Genital and Reproductive Conditions* |
| Interstitial Cystitis | |
| ♂ | Genitourinary Syndrome of Menopause |
| Neurogenic Bladder | |
| Nocturia | |
| Overactive Bladder | |
| ♀ | Pelvic Organ Prolapse |
| ♂ | Peyronies Disease |
| ♂ | Priapism |
| ♂ | Prostate Enlargement (Benign Prostatic Hyperplasia) |
| ♂ | Prostate Infection |
| Sexual Development Disorders | |
| Sexually Transmitted Diseases | |
| ♂ | Scrotal Masses |
| Urolithiasis | |
| Urosepsis | |
| Underactive Bladder | |
| Urinary Incontinence | |
| Urinary Tract Infections |
Female genital and reproductive conditions (e.g., endometriosis, vaginal atrophy) may also be considered NCGUCs. Although they were not within the scope of the NIDDK workshop that led to this manuscript, we wished to acknowledge the importance of these conditions.
Previous efforts to describe the burden of NCGUCs have typically focused on individual burdens (e.g., reduced quality of life)10 or societal burdens (e.g., health care expenditures).11 While these contributions to the literature are noteworthy, they are incomplete. We argue that the comprehensive burden of NCGUCs is largely hidden. NCGUCs pose non-trivial, potentially life-altering problems not only for affected individuals, but also for their families and caregivers. These problems may be compounded within populations that experience a variety of health inequities due to unjust distribution of social determinants of health (i.e., structurally determined resources for health).12 Less recognized and understudied burdens of NCGUCs also include lost work productivity and reduced economic outputs, reduced contributions to the different communities to which affected members belong, and the environment (e.g., ecosystem strains). It is vital to create a framework for identifying and raising awareness of the comprehensive burden of NCGUCs. By doing so, we may increase perceived importance of these conditions among public health practitioners and policymakers, accelerate improvements in access to care, make available resources for affected populations, and stimulate transdisciplinary NCGUC research.
This article provides a conceptual framework for approaching investigations into the comprehensive burden of NCGUCs. To our knowledge, such an effort to broadly conceptualize the hidden burden of NCGUCs has not been undertaken within the field of urology. The Hidden Burden of NCGUCs Framework, described in this article, can be applied to the design of research that both exposes and better characterizes the burden of NGUCs. The framework may not only shape future research, but also support ongoing advocacy efforts to increase demand for needed research. This research may in turn inform future efforts to prevent and treat both NCGUCs and their many consequences. Exposing previously unrealized and underappreciated impacts of NCGUCs represents one paradigm shift in terms of appreciating the importance of NCGUCs. A second paradigm shift is a proposed change in terminology. While the scientific literature often uses the term “benign” to describe NCGUCs, the term in this context is a misnomer. Use of the term “benign” to describe NCGUCs may have unintended consequences, such as implying the conditions are “mild” or “insignificant” and contributing to a general sense that they are less important than other health conditions. Based on prevalence and impact, NCGUCs should be considered a public health priority. For this reason, we reject the descriptor, “benign,” and instead use the term, “noncancerous genitourinary conditions,” consistent with terminology used by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).13
Material and Methods
To better understand the comprehensive burden of NCGUCs, NIDDK convened a workshop in October 2019.14 Attendees comprised a diverse and interdisciplinary group of researchers and health professionals—including urologists and urogynecologists working across traditional NCGUC silos, primary care providers, nurses, measurement and data scientists, basic scientists, environmental scientists, economists, policy experts, public health professionals, and others. Attendees also included people with NCGUCs. Meeting attendees were charged to answer the following key questions: (1) What data are needed to understand the hidden burden of NCGUCs? (2) How can these data be captured in a feasible manner to build a complete picture of NCGUC burden? (3) Are new tools needed for data capture? In order to answer these questions, participants agreed upon the importance of first developing a conceptual framework to understand the comprehensive burden of NCGUCs. The purpose of this article is to present the resulting conceptual framework.
A research-oriented conceptual framework encapsulates what is possible to study and is intentionally broad.15 In the field of public health, social ecological frameworks recognize that individuals are embedded within larger social systems; these frameworks represent characteristics of individuals and environments that interact to influence health outcomes.16 A traditional public health approach would identify “upstream” risk factors (e.g., obesity, parity) that may influence the development and maintenance of NCGUCs, as well as protective factors that may influence health maintenance or NCGUC resolution. In contrast, the focus of this article is on “downstream” effects. Participants of the NIDDK workshop reversed the focus of a traditional social ecological framework by focusing on how NCGUCs may influence broad categories and domains of individuals’ well-being and their social ecology (Figure 1). Following the NIDDK workshop, several subgroups were assembled to continue answering questions posed during the meeting and exploring key needs—including the need to further refine the framework representing hidden burdens of NCGUCs. Outputs of other subgroups are detailed in this special issue.17, 18
Figure 1.
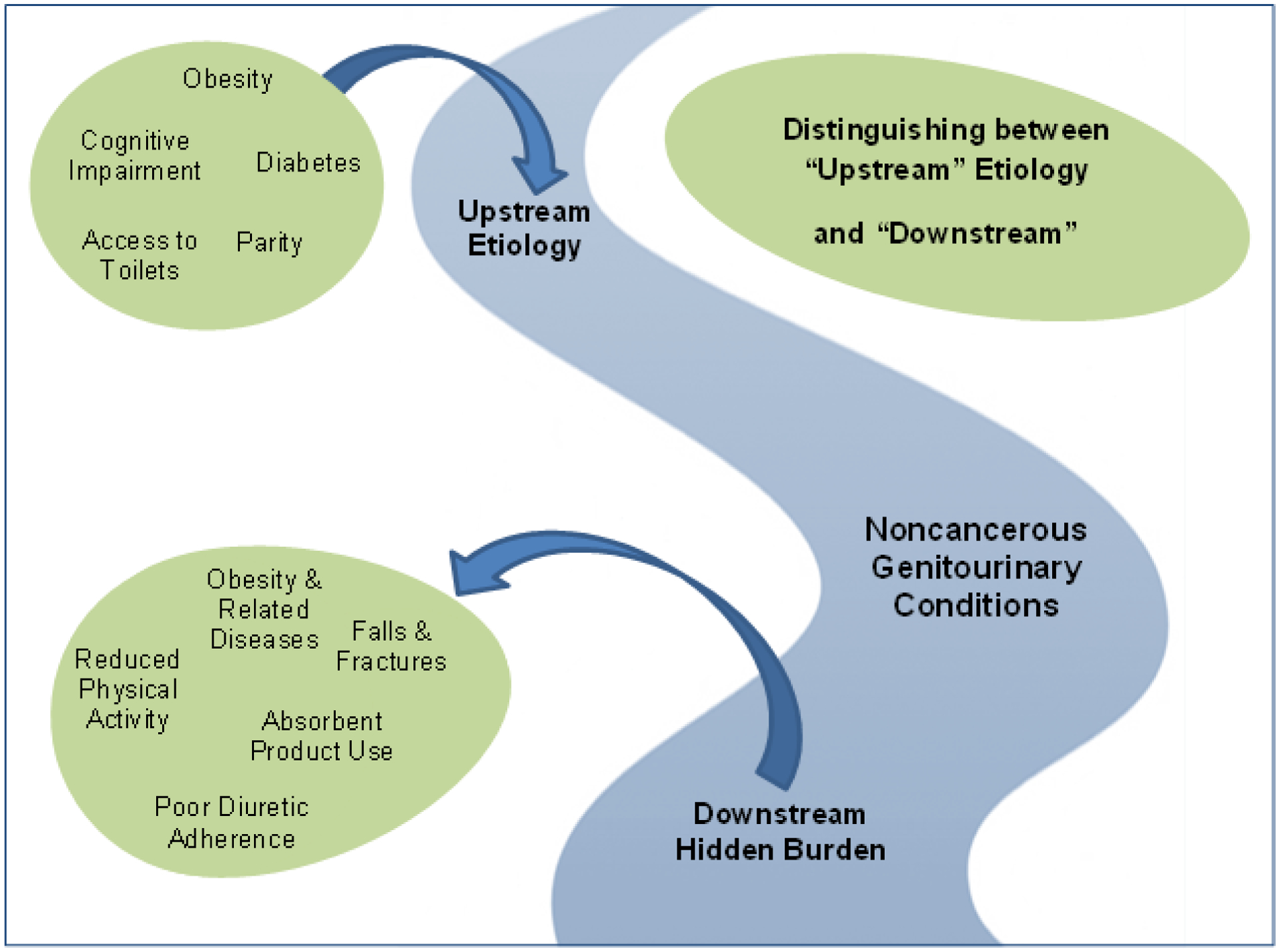
Distinguishing between upstream and downstream factors in relation to NCGUCs.
Below, we present the Hidden Burden of NCGUCs Framework (Figure 2) and review evidence demonstrating the impact NCGUCs can have on the biological systems, lived experience, and behaviors of individuals, as well as the social ecology that surrounds them. Presented evidence is not the result of a systematic review of the literature. Instead, authors with expertise at specific levels of our framework have referenced well-known impacts within their disciplinary fields. The intentional breadth of our framework led to investigating potential impacts of NCGUGs at levels of social ecology beyond authors’ disciplinary training (i.e., environmental and ecosystem impacts). Across all levels, an evidence base to represent the comprehensive burden of NCGUCs is lacking, and this is particularly marked at some levels of our framework. Potential impacts are identified not only from existing literature, but also from clinical observation and the lived experience of people with NCGUCs.
Figure 2.
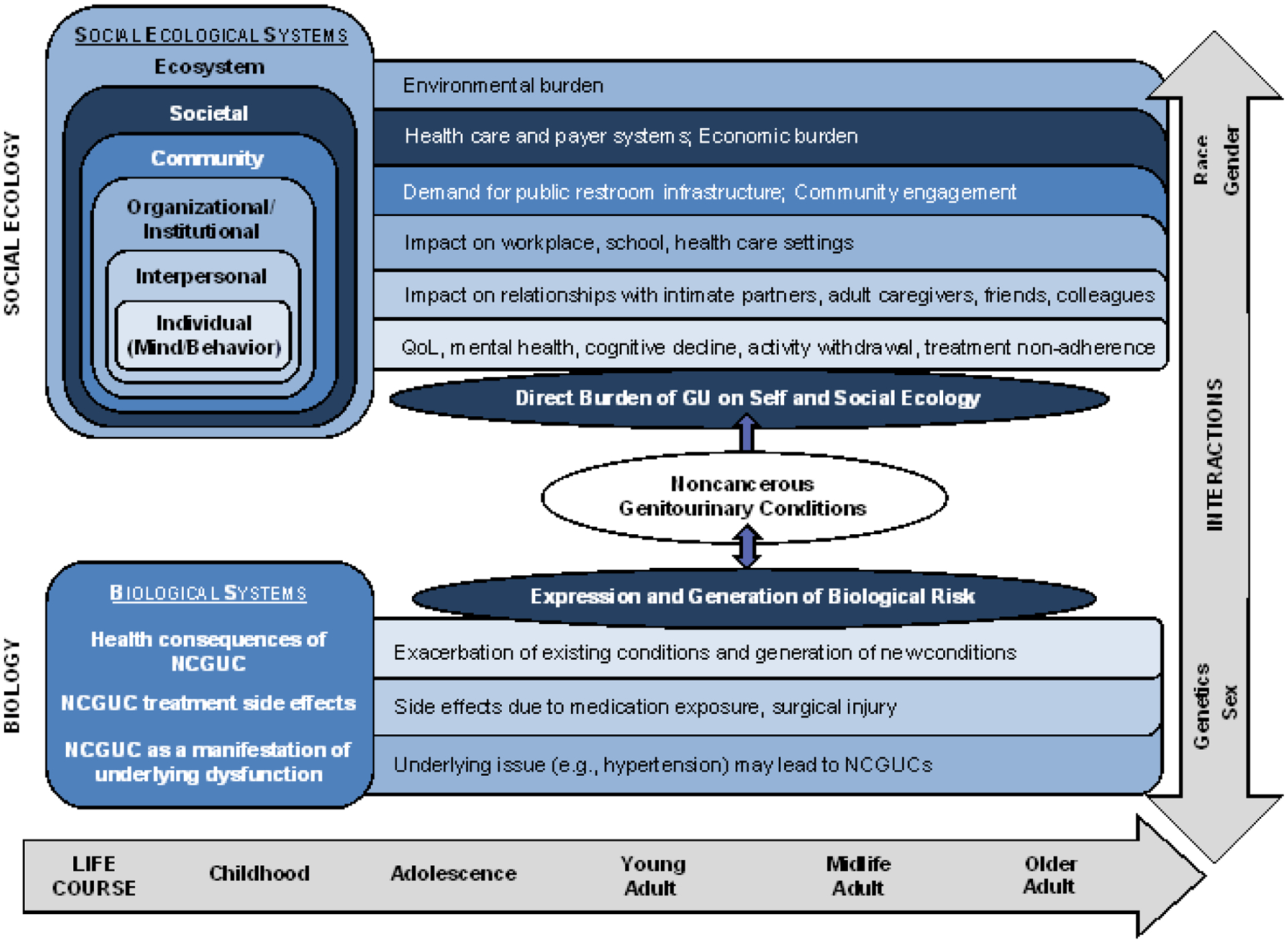
Hidden Burden of Noncancerous Genitourinary Conditions (NCGUCs) Framework. (Adapted from Glass & McAtee, 2006)
Results
Conceptualizing the Hidden Burden.
Figure 2 is a conceptual framework intended to stimulate further inquiry into the hidden burden of NCGUCs. Adapted from Glass and McAtee’s19 Society-Behavior-Biology Nexus, this framework focuses on the downstream hidden burden of NCGUCs instead of upstream etiology. The top portion of Figure 2 shows how NCGUCs can impact the lived experience and behaviors of individuals, as well as the multiple levels of social ecology that surrounds individuals, including interpersonal, organizational and institutional, community, societal, and ecosystem effects. The bottom portion of Figure 2 shows bidirectional associations between NCGUCs and the biological systems of individuals. The upward portion of the bidirectional arrow (see center of figure) recognizes that NCGUCs may first develop due to underlying biological dysfunction; the downward portion of the bidirectional arrow recognizes that once NCGUCs have developed, they may have health consequences or treatment side effects. For this reason, the biological systems portion of Figure 2 is divided into three sections that correspond to common clinical presentations: health consequences of NCGUC, including the generation or exacerbation of other illnesses; NCGUC treatment side effects; and NCGUC as a manifestation of underlying biological dysfunction.
A “life course” arrow underlies the impacts of NCGUCs on social ecological and biological systems. A life course perspective recognizes that NCGUCs may develop at any point across the life course and that the impacts of NCGUCs can accumulate over time. Impacts may be chronic or sporadic in nature and likely exacerbate with age. An “interactions” arrow at the right of Figure 2 recognizes that the type and severity of social ecological and biological impacts of NCGUCs may vary according to genetics, sex (i.e., differences in anatomy, chromosomal composition, and hormonal exposures), gender (i.e., differences in social roles, expectations, and experiences), race (i.e., a proxy for differences in social determinants of health engendered by structural racism), and other biological and societal constructs. This perspective encourages researchers and clinicians to investigate and address health disparities and inequities in the burden of NCGUCs that may differentially impact populations.
Individual Level Impacts – Biological Consequences of NCGUCs on other Health Conditions.
One of the most potentially serious NCGUCs is the inability to empty the bladder (i.e., urinary retention). Neurological or idiopathic urinary retention can lead to kidney failure and subsequent death.5 Kidney failure was once the leading cause of death subsequent to spinal cord injury.20 Today, the use of clean intermittent catheterization to drain urine from the bladder has dramatically reduced bladder related mortality. However, intermittent catheterization can be uncomfortable and may cause injuries. Indwelling catheters have their own negative impacts, such as increased risk of UTIs and bladder cancer.21 An inability to volitionally empty the bladder increases the risk of autonomic dysreflexia (increases in blood pressure that can cause stroke, seizure, and death), a risk that is lessened by emptying the bladder at regular intervals using intermittent catheterization.22
An inability to properly empty the bladder (e.g., due to outlet obstruction) or an inability to store normal amounts of urine may lead to nocturia, a common NCGUC.6 Nocturia is complex with multiple etiologies including not only bladder dysfunction, but also sleep disorders and cardiopulmonary disease. Nocturia is characterized by frequent and bothersome nighttime urination and is the leading cause of sleep disturbance in older adults.23 Loss of sleep is a serious health condition that increases the risk of developing depression,24 type 2 diabetes,25 cardiovascular disease,26 and mortality.27 Those with NCGUCs, notably nocturia and incontinence, are at increased risk of falls.7 Falling can be extremely dangerous in older persons, leading to hip fractures, loss of mobility and independence, and increased mortality risk.28
UTIs, another set of NCGUCs, are the most common type of bacterial infection, resulting in over 1 million emergency department visits and 100,000 hospitalizations per year.29 UI is a risk factor for UTIs,30 illustrating how one NCGUC can increase the risk for another. UTIs are particularly dangerous to pregnant women and are associated with an increased risk of pyelonephritis (kidney infections with potential for kidney damage), pre-eclampsia (indicated by high blood pressure, which can lead to seizures), pre-term delivery, and intrauterine growth restriction (poor fetus growth, which can negatively impact the health of the fetus).8
Individual Level Impacts – Treatment Side Effects.
Medication to treat NCGUCs can often lead to side effects. For example, treatment of OAB with anticholinergic medications can cause dry mouth and constipation. In severe cases, anticholinergic use can lead to urinary retention (primarily in men), delirium, and gait instability and falls.31 Older adults, who are most likely to have OAB symptoms, are most susceptible to these severe side effects, especially delirium.31 Because of these side effects, the American Geriatrics Society Beers Criteria strongly recommends against anticholinergic use in older adults.32 Although uncommon, use of 5-alpha reductase inhibitors to treat benign prostatic hyperplasia (BPH) in men can lead to decreased libido, decreased ejaculate, and erectile dysfunction.33 Alpha-blockers are a second class of medications used to treat BPH; while they are widely used and generally well tolerated, they can cause retrograde ejaculation with associated infertility, as well as orthostatic hypotension, which can lead to falls and fractures.34 Treatment for recurrent UTIs with serial courses of antibiotics can contribute to multidrug resistant organisms and also have adverse impacts to the gastrointestinal microbiome.35, 36 Because most medications are used to control symptoms, but do not resolve the NCGUC, side effects can become chronic.
Surgical treatment of NCGUCs can also lead to severe side effects that have both short- and long-term health impacts. For example, although bladder outlet procedures to treat BPH have high overall patient satisfaction, some individuals may experience retrograde ejaculation or incontinence.37 Endoscopic procedures, such as transurethral procedures or ureteroscopy, carry a low, but noteworthy risk of strictures.37, 38 Strictures can lead to additional LUTS and kidney function deterioration, requiring additional surgical procedures to treat obstruction or symptoms.39 Patients undergoing surgery for prolapse or incontinence may develop additional urinary or pelvic symptoms, sexual dysfunction, or pain. Surgical mesh-related complications include erosion/extrusion and infection,40 particularly for specific surgical procedures. In 2019, the U.S. Food and Drug Administration ordered the use of transvaginal mesh for the treatment of pelvic organ prolapse to be withdrawn from the market due to safety concerns.41 Although the use of synthetic mesh for stress urinary incontinence carries some risks (e.g., low rates of urinary retention, mesh erosion, and pelvic pain that require surgical revision or removal),42 extensive data exists to support its safe use, and the procedure is recommended by the FDA and multiple professional societies.43
Individual Level Impacts – Mind and Behavior.
An individual’s lived experience is “housed” in the brain and can impact brain development, stress physiology, and central nervous system function across the lifespan.44 For this reason, stressors have the potential to impact a wide range of mental and physical health problems, including those that emerge later in life. For example, research suggests that childhood adversity increases the risk for lower urinary tract symptoms (LUTS) in adult women through alterations in stress physiology.45 Stress is not only an “upstream” risk factor for NCGUCs, but also a “downstream” consequence of NCGUCs. NCGUCs negatively impact self-esteem; affect; and perceptions of overall health, imposition on family members, and one’s work or professional life.46, 47 One systematic review and several population-based studies have found that NCGUCs can reduce quality of life and increase symptoms of depression and anxiety, particularly among those who experience bother or functional loss.10, 47–49 Some studies have observed effects on incident depression or anxiety across 10 or more years.48, 49 In one study of men, the presence of LUTS was not only associated with greater risk of depression, but also suicidal ideation.50 While treatments for LUTS may ameliorate both physical and psychological symptoms, some treatments may exacerbate psychological symptoms for a small subset of patients. For example, initiation of 5α reductase inhibitor increased risk for depression and self-harm in the first 18 months of treatment in a population-based, retrospective cohort study of older men; however, the authors concluded that potential benefits of treatment likely outweighed potential risks for most patients.51
In addition to effects on the mind, NCGUCs commonly lead to changes in behavior that can severely impact health and well-being. Withdrawal from activities and social isolation are common among individuals with UI.52 Social isolation is a major health problem, leading to cognitive decline, nutritional deficits, cardiovascular disease, falls, hospital readmittance, and mortality.53 Some conditions such as OAB are associated with lower levels of physical activity, likely due to fear of urine leakage.54 This change in behavior can lead to an increasingly sedentary lifestyle, which can in turn lead to numerous serious medical conditions including cardiovascular disease, breast cancer, and colon cancer.55 Many individuals cope with NCGUCs (e.g., urgency, frequency, incontinence) by restricting fluid intake. Fluid restriction may increase the likelihood of experiencing UTIs or kidney injury.56 Finally, diuretics can worsen NCGUCs. This can lead individuals with cardiovascular or kidney disease to avoid taking critical blood pressure medications,57, 58 potentially leading to serious health consequences.
Broadening the Focus from Individual-Level Impacts to Social Ecology.
Individuals with NCGUCs are embedded within a social ecology comprised of close interpersonal relationships (e.g., families, peers, intimate partners); organizations and institutions (e.g., schools, workplaces); communities (e.g., neighborhoods, groups united through shared social identities); their larger society (e.g., economic systems; healthcare infrastructure); and the broader ecosystem (e.g., natural resources within the environment).59 Each level of social ecology is impacted by NCGUCs, particularly when one considers the high prevalence of conditions within the population.
Interpersonal Level Impacts.
NCGUCs impact interpersonal relationships with spouses/intimate partners, family members, friends, colleagues/co-workers, and adult caregivers.60, 61 Among both men and women, NCGUCs can have a profound impact on sexual function, sexual satisfaction, and intimacy.62, 63 Perceptions of masculinity, such as “feeling less of a man,” can negatively impact men’s intimate relationships.64 Individuals living with NCGUCs also describe reducing, avoiding, and withdrawing from friendships that were once a source of joy.65, 66 Recurrent UTIs can have a significant social impact, particularly among pre-menopausal, working women.67 Several studies have focused on the impact of NCGUCs on a person’s ability to engage in productive work.61, 66, 68 However, whether and how UTIs or other NCGUCs impact relationships with colleagues and co-workers is an area in need of further exploration. Although minimally addressed in the literature, studies examining the perspectives of informal caregivers identify decreased quality of life, emotional distress, and social isolation as consequences of caring for a person with LUTS or UI; recommendations include acknowledging the burden of caregiving, implementing strategies for increasing support, and providing education and other resources for caregivers.69, 70
Organizational and Institutional Level Impacts.
Little research has examined the impact of NCGUCs on organizations and institutions, with the exception of health care settings such as hospitals and nursing homes. Incontinence can impede independence among older adults; when combined with other factors, incontinence can lead to caregiver burden and transfer to nursing homes. Incontinence in nursing homes is managed using a variety of urinary collection devices, including absorbent products, intermittent straight catheterization, condom catheters, and indwelling urethral catheters. The annual cost of managing UI in nursing homes is estimated to be more than five billion dollars, including labor, laundry, and supplies.71 Effectively preventing and managing incontinence requires time and collaboration on the part of nursing home employees, who are often overtaxed.72 Primary genitourinary system disease, including UTI and related sepsis, is a major preventable reason for hospitalization.73 Thus, NCGUCs can have a significant impact on the ability of nursing homes to provide optimal care.
Workplaces and schools are likely to be key institutions impacted by NCGUCs, although research is needed to support this premise.10 Many workplaces are ill-equipped to handle the toileting needs of individuals with NCGUCs. Over one-third of employed women in the U.S. report having UI in the last month,74 but the Occupation Safety and Health Administration (OSHA) standard for employers is only one toilet per 15 persons.75 Nearly 90% of employed women with severe incontinence use pads/incontinence products,74 yet such products are not offered in public restrooms. The norms of some workplaces are characterized by restricted time for toileting or access to amenities. Studies demonstrate that such norms can have an impact on individuals, and findings hint at impacts on the institutions themselves. For example, one cross-sectional observational study examined associations between nurses’ workplace bladder practices, urinary symptoms, and work productivity. Nurses often experienced restricted access to amenities due to job demands and workplace environments.76 Most nurses delayed voiding and many purposefully limited fluid intake at work. This, in turn, impacted nurses’ reported ability to concentrate at work and manage time, respectively. In other studies, individuals with Interstitial cystitis/bladder pain syndrome or UTIs have reported reduced work productivity.61, 66, 68 In the aggregate, the productivity of workplaces may similarly be reduced, although research is necessary to support this point. Additional areas of inquiry include absenteeism and loss of talent because employees have changed professions or exited the workforce due to NCGUCs.
Reduced ability to manage time, concentrate, and produce work may conceivably extend to children and adolescents in the school setting. Research has found that the school toileting environment (e.g., bullying; long lines; lack of privacy, cleanliness, toilet paper, soap, or towels/hand dryers) is linked to NCGUCs among students;77 other research suggests that students’ infrequent voiding can explain this association.78 Qualitative research demonstrates that teachers often restrict students’ toileting access because they do not recognize students’ biological need to void and assume that students are intending to misbehave if they ask to leave the classroom.79 What remains to be established are whether students’ NCGUCs impact the teaching mission of schools. Potential areas of inquiry include aggregate measures of student concentration and academic performance, as well as absenteeism and truancy.
Community Level Impacts.
Research is needed to determine whether there is adequate public restroom infrastructure and supplies for individuals with NCGUCs, as well as the consequences for communities when these resources are insufficient. In addition to challenges in finding readily available facilities, women with incontinence report using larger handicap restrooms to change clothing after an incontinence episode.80 Often only one toilet in a facility is handicap accessible, further limiting toileting access. Public restrooms do not typically provide receptacles for the disposal of incontinence containment products. Women with incontinence in Australia described carrying bags to discreetly dispose of their used products.80 Research on public restroom infrastructure and supplies is not only essential to meet the needs of the general population, but also vulnerable populations that may be depend upon communities for amenities. For example, in the U.S., San Francisco has one of the nation’s largest populations of people living in homelessness; in response to a rise in complaints about human waste on streets, the city implemented the Pit Stop program, which provides staffed public restrooms in critical areas throughout the city to ensure safety and cleanliness of restrooms.81 Research on infrastructure should consider key locations, including commercial businesses, community parks and recreation, and transportation corridors (e.g., public highway systems). In addition to impacts on the community built environment, NCGUCs likely impact community social systems. Although the evidence-base is limited on this point, NCGUCs could conceivably impact participation in and service to community organizations, including volunteering. At least one study examined and did not find support for this impact, however.82
Societal Level Impacts.
At the societal level, NCGUCs have a pronounced impact on healthcare and insurance systems. Individuals who seek treatment create a demand for services. Access to care may be inequitably distributed due to factors including race, education, health literacy, and distance from quaternary care facilities.83, 84 Greater institutionalization in nursing homes due to NCGUCs has been observed over time as the population ages.85 Caring for individuals with NCGUCs in acute and chronic care settings places a greater burden on the overall healthcare system.11 Patients, providers, and payers are engaged in a debate over who will pay for products and services, with differing incentives and abilities to pay.86 Many individuals do not realize that NCGUCs can be treated or choose to manage conditions on their own;87, 88 this represents unmet health care and social service needs that would strain systems further if individuals sought the care to which they are entitled.
NCGUCs also have a pronounced impact on the productivity and economic systems of a society. The economic burden of urge UI in the U.S., for example, was estimated to be $65.9 billion in 2007 with greater than 20% growth projected by 2020.89 Aging of the U.S. population and economic inflation that has occurred since this estimate may mean the cost is substantially higher today. The impact of obesity and diabetes, together with population growth, is expected to incur an additional $1.24 billion per year in healthcare spending for urolithiasis alone by 2030.90 The economic burden of NCGUCs are further discussed by Kim and colleagues91 in this issue.
Ecosystem Level Impacts.
At the broadest level of social ecology, the ecosystem, NCGUCs may have an impact on the natural environment. According to the U.S. Environmental Protection Agency (EPA), disposable infant diapers and adult incontinence products resulted in 4.1 million tons of municipal solid waste in the U.S. in 2018, and accounted for 1.4% of all municipal solid waste that year. Most of this waste was sent to landfills and a smaller percentage (approximately 20%) was combusted with energy recovery.92 One group has estimated that one third of absorbent product waste is related to adult incontinence products,93 which can range from absorbent pads for mild incontinence to adult diapers for individuals with severe incontinence and those who are bed-ridden.94 Once deposited into landfills, absorbent products are believed to take over 500 years to degrade,95 an estimate that has motivated the absorbent product industry to develop smaller products with a greater proportion of biodegradable materials, and the waste management industry to explore recycling and composting of absorbent products.94 NCGUCs are likely to have other costs to the natural environment. In addition to disposal of absorbent products, disposal of other single-use products necessary for the treatment of NCGUCs (e.g., catheters, surgical instruments) may strain the ecosystem; the burden of manufacturing these products also is not well understood. In addition, it is unclear whether water consumption from frequent toilet flushes or laundering linked to NCGUCs has an impact on the natural environment. Research is needed to better understand the total ecosystem burden of NCGUCs.
Individual Level – NCGUCs as Manifestations of Underlying Dysfunction.
In the previous sections, we enumerated downstream biological and social ecological consequences of NCGUCs to highlight the seriousness of these conditions and their burdens to individuals and society. A discussion of the importance of NCGUCs would be incomplete without also highlighting that NCGUCs may serve as early warning signs or manifestations of other health conditions.
For example, the genitourinary system is dependent upon proper cardiovascular (CV) function and is the terminal excretory point for fluid waste from the circulatory system. Therefore, NCGUCs may serve as early indicators of CV dysfunction. Nocturia is associated with an increased risk of hypertension.96 Nocturia is also associated with measures of subclinical atherosclerosis such as aortic calcification and increased arterial stiffness,97, 98 both early steps in the pathogenesis of CV disease. In addition, nocturia can be a sign of sleep apnea,99 which also has a major impact on cardiovascular function.100 In a recent study of African American men surveyed at their barbershop, the presence and severity of nocturia was found to be predictive of undiagnosed hypertension and suboptimal blood pressure control, making nocturia a useful screening tool in the community setting.101 As with nocturia, it is believed that erectile dysfunction is an early manifestation of underlying CV dysfunction.102 Erectile dysfunction is a sign of increased risk for CV disease, coronary heart disease, stroke, and mortality.103
NCGUCs are also associated with neurological dysfunction.104 NCGUCs are known to occur prior to neurological diagnosis in some patients with multiple sclerosis, multiple system atrophy, normal pressure hydrocephalus, early dementia, Parkinson’s disease, and spinal cord disorders.105 NCGUCs could conceivably serve as an early indicator of neurological dysfunction or as a sign of undiagnosed neurological dysfunction that has been advancing for some time. In addition to neurological dysfunction, NCGUCs are associated with diabetes106 Although urinary abnormalities such as sweet-smelling urine or excessive urination are telltale signs of diabetes, less is known about the utility of routinely screening patients seeking NCGUC treatment for diabetes.
Therefore, ascertaining a clinical history of NCGUCs, regardless of whether patients present with this problem, can provide insights as to the potential presence of underlying CV, neurological, and potentially even diabetic disease, as well as risk for future dysfunction. By properly educating medical professionals as to the importance of NCGUCs, we may be able to improve our treatment of other health conditions through earlier detection, prevention, and treatment.
Comment
NCGUCs confer a large, yet poorly understood burden to individuals and society. Many of these burdens are “hidden” from the awareness of researchers, practitioners, policymakers, and the general public. This may be true because of disciplinary specialization and resultant silos of research and treatment; public health priorities that are more visible than NCGUCs with respect to communication campaigns and advocacy; and stigmatization of those who experience NCGUCs. In this article, we have presented evidence to support the premise that NCGUCs should become a public health priority. We have also presented a conceptual framework for approaching investigations into additional burdens of NCGUCs.
Research to describe the comprehensive burden of NCGUCs is needed. Measurement of burdens should incorporate multiple levels of well-being and social ecology. While some consequences of NCGUCs on other health conditions are well documented (e.g., risk of additional NCGUCs, kidney injury, autonomic dysreflexia, sleep loss, falls), a comprehensive understanding of the systemic effects of NCGUCs on the body is lacking. Although medications and procedures to treat NCGUCs have well documented benefits, the degree to which side effects and short- and long-term complications are experienced within specific populations, particularly those that are more vulnerable to health inequities, is poorly documented. In addition, treatment choices may yield benefits or burdens beyond the individual level of social ecology, including impacts felt by caregivers and other family members and changes to the environment. Impacts of NCGUCs on individuals’ lived experience, behaviors, and interpersonal relationships are well documented, though perhaps underappreciated by members of society that are not intimately acquainted with the conditions. A largely understudied domain of research is the impact of NCGUCs and their treatments on the broader social ecology of individuals, including organizations and institutions (e.g., productivity in workplaces and schools), communities (e.g., unmet demand for public restroom infrastructure and supplies for individuals with NCGUCs), society (e.g., economic output) and ecosystem (e.g., landfill waste, water consumption). The adoption of a social ecological perspective in studying NCGUC impact may inform the development of treatments that confer more benefits and fewer burdens across levels of social ecology.
Measurement of NCGUC burdens should incorporate a life course perspective. Different methods may be used to accomplish this goal. For example, medical records may be reviewed to evaluate NCGUC impacts that led to treatment at different stages of the life course (e.g., childhood, older adulthood) or after specific life events (e.g., pregnancy, cancer treatment). Within some medical systems, records may also be reviewed to determine accumulated impacts of NCGUCs over time. Other methods of data collection include qualitative interviews, cross-sectional surveys, retrospective or prospective cohort studies, and economic analyses, particularly to evaluate impacts on levels of ecology not well represented in the literature. While it is not feasible for a single study to address every aspect of burden or stage of the life course depicted by the Hidden Burden of NCGUCs Framework, the framework may encourage researchers to expand their scope of study when possible, even by considering burden at one additional level of social ecology. Thus, the Hidden Burden of NCGUCs Framework provides a map for different routes of study within the field of urology research. It also may stimulate transdisciplinary collaborations.
A life course approach would acknowledge the accumulation of impacts over time and identify potential points for prevention and intervention. In this special issue, Norton and colleagues18 identify “inflection points” – sensitive time periods across the life course of individuals for identification and response to NCGUCs. Early identification and response may minimize burdens and maximize benefits to both individuals and society. For this reason, providers who do not normally focus on NCGUCs should proactively screen for a history of NCGUCs among patients and make referrals, as appropriate. Providers should also be aware of life events that may serve as inflection points. For example, gynecologists and obstetricians can prepare women for the possibility that they may experience LUTS as a result of pregnancy and childbirth; routinely screen for LUTS; and make referrals for primary, secondary, and tertiary prevention strategies, as appropriate (e.g., pelvic floor exercises). In this article, we have noted that NCGUCs may be a manifestation of underlying biological dysfunction. The utility of screening for other disorders when patients present with NCGUCs (e.g., early identification and treatment of other costly health conditions) is an understudied domain of research. It is possible that early identification and response to NCGUCs may not only aid in the resolution of these conditions, consistent with Norton and colleagues’ Inflection Point Model,18 but also other health conditions (e.g., hypertension).
Research should also examine whether burdens of NCGUCs vary by genetics, sex, race, and gender. This approach would expose potential health inequities in burden experienced by different populations and social groups, given the presence of a specific NCGUC. For example, cisgender women are more likely than cisgender men to experience challenges in accessing public restroom facilities,79 as are transgender individuals.106 Implicit or explicit bias may influence the health care of racial and ethnic minorities and result in disproportionate burden of NCGUCs.107
Conclusions.
Exposing the hidden burden of NCGUCs may increase perceived importance of these conditions among public health practitioners and policymakers, accelerate improvements in care, make available resources for affected populations, and stimulate transdisciplinary NCGUC research. An enhanced focus on NCGUCs may improve the lives of millions who bear the hidden burden of NCGUCs.
Acknowledgements
Dr. Hokanson’s work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (K01DK121866). Dr. Hsi’s work was supported by NIDDK (R21DK127075). Dr. Liu’s work was supported by the Boston University School of Medicine (Department of Medicine Career Investment Award) and the National Institute of Aging (1K23AG057813). Dr. Reynolds’ work supported by NIDDK (1K23DK103910). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, NIDDK, or the National Institute of Nursing Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest
There are no reported financial or personal relationships that could bias this work.
Financial and Personal Disclosures
Sonya S. Brady: None
Tamara G. Bavendam: None
Christine K. Bradway: None
Britt Conroy: None
Annemarie Dowling-Castronovo: None
C. Neill Epperson: Asarina Pharma (advisory board); Sage Therapeutics (consultant, advisory board, site principle investigator Sage 217-PPD-301 and Sage 547-PPD-304)
Adonis K. Hijaz: Collamedix Inc (equity) and Astellas (speaker).
Ryan S. Hsi: None
Karen Huss: None
Michelle Kim: None
Jason Lazar: None
Richard K. Lee: None
Christine K. Liu: AgeBold (consultant)
Christine N. Loizou: None
Saadia Miran: None
Lona Mody: None
Jenna M. Norton: None
W. Stuart Reynolds: None
Siobhan Sutcliffe: None
Nicole Zhang: None
James Hokanson: None
References
- 1.Markland AD, Richter HE, Fwu CW, Eggers P, Kusek JW. Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. J Urol. 2011;186(2):589–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU international. 2011;108(7):1132–1138. [DOI] [PubMed] [Google Scholar]
- 3.Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER. Imaging studies after a first febrile urinary tract infection in young children. The New England journal of medicine. 2003;348(3):195–202. [DOI] [PubMed] [Google Scholar]
- 4.Stöhrer M, Blok B, Castro-Diaz D, et al. EAU guidelines on neurogenic lower urinary tract dysfunction. European urology. 2009;56(1):81–88. [DOI] [PubMed] [Google Scholar]
- 5.Hernández Hernández D, Tesouro RB, Castro-Diaz D. Urinary retention. Urologia. 2013;80(4):257–264. [DOI] [PubMed] [Google Scholar]
- 6.Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2010;184(2):440–446. [DOI] [PubMed] [Google Scholar]
- 7.Gibson W, Hunter KF, Camicioli R, et al. The association between lower urinary tract symptoms and falls: forming a theoretical model for a research agenda. Neurourology and urodynamics. 2018;37(1):501–509. [DOI] [PubMed] [Google Scholar]
- 8.Kalinderi K, Delkos D, Kalinderis M, Athanasiadis A, Kalogiannidis I. Urinary tract infection during pregnancy: current concepts on a common multifaceted problem. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2018;38(4):448–453. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. Multiple chronic conditions: A strategic framework – Optimum health and quality of life for individuals with multiple chronic conditions. Accessed 3/15/21, https://www.hhs.gov/sites/default/files/ash/initiatives/mcc/mcc_framework.pdf
- 10.Coyne KS, Wein A, Nicholson S, Kvasz M, Chen CI, Milsom I. Comorbidities and personal burden of urgency urinary incontinence: a systematic review. Int J Clin Pract. 2013;67(10):1015–1033. [DOI] [PubMed] [Google Scholar]
- 11.Morris AR, Ho MT, Lapsley H, Walsh J, Gonski P, Moore KH. Costs of managing urinary and faecal incontinence in a sub-acute care facility: a “bottom-up” approach. Neurourology and urodynamics. 2005;24(1):56–62. [DOI] [PubMed] [Google Scholar]
- 12.Tellechea L, Zuo S, Kohn JR, et al. The effect of social determinants of health on overactive bladder symptom severity. J Urol. 2020:101097ju0000000000001545. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Urologic diseases. Accessed 3/15/21, https://www.niddk.nih.gov/about-niddk/research-areas/urologic-diseases
- 14.National Institute of Diabetes and Digestive and Kidney Diseases National Institutes of Health. Final Meeting Summary. Paper presented at: Uncovering the Hidden Burden of Benign Genitourinary Conditions 2019; Bethesda, MD. [Google Scholar]
- 15.Brady SS, Bavendam TG, Berry A, et al. The Prevention of Lower Urinary Tract Symptoms (PLUS) in girls and women: Developing a conceptual framework for a prevention research agenda. Neurourology and urodynamics. Nov 2018;37(8):2951–2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golden SD, Earp JA. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ & Behav. Jun 2012;39(3):364–372. [DOI] [PubMed] [Google Scholar]
- 17.Kim M, Harvey J, Gusev A, Norton J, Miran S, Bavendam T. A scoping review of the economic burden of non-cancerous GU conditions. 2021. [DOI] [PubMed]
- 18.Norton JM, Dowling-Castronovo A, Conroy B, et al. Capturing the hidden burdens of non-cancerous genitourinary conditions through inflection point modeling. 2021. [DOI] [PubMed]
- 19.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650–1671. [DOI] [PubMed] [Google Scholar]
- 20.Hackler RH. A 25-year prospective mortality study in the spinal cord injured patient: comparison with the long-term living paraplegic. J Urol. 1977;117(4):486–488. [DOI] [PubMed] [Google Scholar]
- 21.Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010;184(1):213–217. [DOI] [PubMed] [Google Scholar]
- 22.Furusawa K, Tokuhiro A, Sugiyama H, et al. Incidence of symptomatic autonomic dysreflexia varies according to the bowel and bladder management techniques in patients with spinal cord injury. Spinal cord. 2011;49(1):49–54. [DOI] [PubMed] [Google Scholar]
- 23.Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med Rev. 2009;10(5):540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mezick EJ, Hall M, Matthews KA. Are sleep and depression independent or overlapping risk factors for cardiometabolic disease? Sleep Med Rev. 2011;15(1):51–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 22 2008;105(3):1044–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calhoun DA, Harding SM. Sleep and hypertension. Chest. 2010;138(2):434–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30(10):1245–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyé ND, Van Lieshout EM, Van Beeck EF, Hartholt KA, Van der Cammen TJ, Patka P. The impact of falls in the elderly. Trauma. 2013;15(1):29–35. [Google Scholar]
- 29.Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. JAMA. 26 2014;311(8):844–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu KK, Boyko EJ, Scholes D, et al. Risk factors for urinary tract infections in postmenopausal women. Arch Intern Med. 10 2004;164(9):989–993. [DOI] [PubMed] [Google Scholar]
- 31.Collamati A, Martone AM, Poscia A, et al. Anticholinergic drugs and negative outcomes in the older population: from biological plausibility to clinical evidence. Aging Clin Exp Res. 2016;28(1):25–35. [DOI] [PubMed] [Google Scholar]
- 32.American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–694. [DOI] [PubMed] [Google Scholar]
- 33.Hirshburg JM, Kelsey PA, Therrien CA, Gavino AC, Reichenberg JS. Adverse effects and safety of 5-alpha reductase inhibitors (Finasteride, Dutasteride): A systematic review. J Clin Aesthet Dermatol. 2016;9(7):56–62. [PMC free article] [PubMed] [Google Scholar]
- 34.Lepor H Alpha blockers for the treatment of benign prostatic hyperplasia. Rev Urol. 2007;9(4):181–190. [PMC free article] [PubMed] [Google Scholar]
- 35.Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host-pathogen interactions and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.U.S. Department of Health and Human Services Centers for Disease Control. Antibiotic resistance threats in the United States. 2019. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
- 37.Sun F, Sun X, Shi Q, Zhai Y. Transurethral procedures in the treatment of benign prostatic hyperplasia: A systematic review and meta-analysis of effectiveness and complications. Medicine. 2018;97(51):e13360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cooper JL, François N, Sourial MW, et al. The impact of ureteral access sheath use on the development of abnormal postoperative upper tract imaging after ureteroscopy. J Urol. Nov2020;204(5):976–981. [DOI] [PubMed] [Google Scholar]
- 39.Lu C, Zhang W, Peng Y, et al. Endoscopic balloon dilatation in the treatment of benign ureteral strictures: A meta-analysis and systematic review. J Endourol. 2019;33(4):255–262. [DOI] [PubMed] [Google Scholar]
- 40.Shah HN, Badlani GH. Mesh complications in female pelvic floor reconstructive surgery and their management: A systematic review. Indian J Urol. 2012;28(2):129–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ray S, Clifton MM, Koo K. Inaccuracies in news media reporting about the 2019 US Food and Drug Administration ban on transvaginal mesh for pelvic organ prolapse repair. Urology. 2021;150:194–200. [DOI] [PubMed] [Google Scholar]
- 42.Unger CA, Rizzo AE, Ridgeway B. Indications and risk factors for midurethral sling revision. Int Urogynecol J. 2016;27(1):117–122. [DOI] [PubMed] [Google Scholar]
- 43.Ugianskiene A, Davila GW, Su TH. FIGO review of statements on use of synthetic mesh for pelvic organ prolapse and stress urinary incontinence. Int J Gynaecol Obstet. Nov 2019;147(2):147–155. [DOI] [PubMed] [Google Scholar]
- 44.Bale TL, Epperson CN. Sex differences and stress across the lifespan. Nat Neurosci. 2015;18(10):1413–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Epperson CN, Duffy KA, Johnson RL, Sammel MD, Newman DK. Enduring impact of childhood adversity on lower urinary tract symptoms in adult women. Neurourol Urodyn. 2020;39(5):1472–1481. [DOI] [PubMed] [Google Scholar]
- 46.Dmochowski RR, Newman DK. Impact of overactive bladder on women in the United States: results of a national survey. Curr Med Res Opin. 2007;23(1):65–76. [DOI] [PubMed] [Google Scholar]
- 47.Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012;80(1):90–96. [DOI] [PubMed] [Google Scholar]
- 48.Bogner HOD AJ; de Vries HF; Northington GM; Joo JH. The temporal relationship between anxiety disorders and urinary incontinence among community-dwelling adults. J Anxiety Disord. 2011;25(2):203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Felde G, Ebbesen MH, Hunskaar S. Anxiety and depression associated with urinary incontinence. A 10-year follow-up study from the Norwegian HUNT study (EPINCONT). Neurourol Urodyn. 2017;36(2):322–328. [DOI] [PubMed] [Google Scholar]
- 50.Breyer BN, Kenfield SA, Blaschko SD, Erickson BA. The association of lower urinary tract symptoms, depression and suicidal ideation: data from the 2005–2006 and 2007–2008 National Health and Nutrition Examination Survey. J Urol. May 2014;191(5):1333–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Welk B, McArthur E, Ordon M, Anderson KK, Hayward J, Dixon S. Association of suicidality and depression with 5α-reductase inhibitors. JAMA Int Med. 2017;177(5):683–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yip SO, Dick MA, McPencow AM, Martin DK, Ciarleglio MM, Erekson EA. The association between urinary and fecal incontinence and social isolation in older women. Amer J Obstet Gynecol. 2013;208(2):146.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nicholson NR. A review of social isolation: an important but underassessed condition in older adults. J Prim Prev. 2012;33(2–3):137–152. [DOI] [PubMed] [Google Scholar]
- 54.Coyne KS, Sexton CC, Clemens JQ, et al. The impact of OAB on physical activity in the United States: results from OAB-POLL. Urology. 2013;82(4):799–806. [DOI] [PubMed] [Google Scholar]
- 55.Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124(5):799–815. [DOI] [PubMed] [Google Scholar]
- 56.Lean K, Nawaz RF, Jawad S, Vincent C. Reducing urinary tract infections in care homes by improving hydration. BMJ Open Qual. 2019;8(3):e000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hwang R, Chuan F, Peters R, Kuys S. Frequency of urinary incontinence in people with chronic heart failure. Heart Lung. 2013;42(1):26–31. [DOI] [PubMed] [Google Scholar]
- 58.Patel M, Vellanki K, Leehey DJ, et al. Urinary incontinence and diuretic avoidance among adults with chronic kidney disease. Int Urol Nephrol. 2016;48(8):1321–1326. [DOI] [PubMed] [Google Scholar]
- 59.Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health. 2011;32:307–326. [DOI] [PubMed] [Google Scholar]
- 60.Bradway C, Miller E, Heivly A, Fleshner I. Continence care for obese nursing home residents. Urol Nurs. 2010;30(2):121–129. [PubMed] [Google Scholar]
- 61.Hakimi Z, Houbiers J, Pedersini R, Vietri J. The burden of bladder pain in five european countries: A cross-sectional study. Urology. 2017;99:84–91. [DOI] [PubMed] [Google Scholar]
- 62.Mendes A, Hoga L, Gonçalves B, Silva P, Pereira P. Adult women’s experiences of urinary incontinence: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep. 2017;15(5):1350–1408. [DOI] [PubMed] [Google Scholar]
- 63.Schultheiss D Urogenital infections and male sexuality: effects on ejaculation and erection. Andrologia. 2008;40(2):125–129. [DOI] [PubMed] [Google Scholar]
- 64.Kong EH, Deatrick JA, Bradway CK. Men’s experiences after prostatectomy: A meta-synthesis. Int J Nurs Studies. 2017;74:162–171. [DOI] [PubMed] [Google Scholar]
- 65.Moriarty HJ, Robinson JP, Bunting-Perry L, Bradway CW. Cognitive, affective, and behavioral dimensions of the lower urinary tract symptom experience in men with Parkinson’s Disease. J Wound Ostomy Continence Nurs. 2016;43(1):80–87. [DOI] [PubMed] [Google Scholar]
- 66.Wild DJ, Clayson DJ, Keating K, Gondek K. Validation of a patient-administered questionnaire to measure the activity impairment experienced by women with uncomplicated urinary tract infection: the Activity Impairment Assessment (AIA). Health Qual Life Outcomes. 2005;3:42. doi: 10.1186/1477-7525-3-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Health Qual Life Outcomes. 2019;11:1756287219832172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vasudevan V, Moldwin R. Addressing quality of life in the patient with interstitial cystitis/bladder pain syndrome. Asian J Urol. 2017;4(1):50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Santini S, Andersson G, Lamura G. Impact of incontinence on the quality of life of caregivers of older persons with incontinence: A qualitative study in four European countries. Arch Gerontol Geriatr Suppl. 2016;63:92–101. [DOI] [PubMed] [Google Scholar]
- 70.Moriarty H, Bunting-Perry L, Robinson JP, Bradway CW. The experience of women who care for spouses with Parkinson’s Disease and lower urinary tract symptoms. .JOGNN-J Obst Gyn Neo. 2016;45(5):737–748. [DOI] [PubMed] [Google Scholar]
- 71.Hu TW, Wagner TH, Bentkover JD, Leblanc K, Zhou SZ, Hunt T. Costs of urinary incontinence and overactive bladder in the United States: a comparative study. Urology. 2004;63(3):461–465. [DOI] [PubMed] [Google Scholar]
- 72.McDaniel C, Ratnani I, Fatima S, Abid MH, Surani S. Urinary incontinence in older adults takes collaborative nursing efforts to improve. Cureus. 12 2020;12(7):e9161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rogers MA, Fries BE, Kaufman SR, Mody L, McMahon LF Jr., Saint S Mobility and other predictors of hospitalization for urinary tract infection: a retrospective cohort study. BMC Geriatr. 2008;8:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fultz N, Girts T, Kinchen K, Nygaard I, Pohl G, Sternfeld B. Prevalence, management and impact of urinary incontinence in the workplace. Occup Med. 2005;55(7):552–557. [DOI] [PubMed] [Google Scholar]
- 75.United States Department of Labor Occupational Safety and Health Administration. 1915.88 - Sanitation. Occup Safety and Health Standards for Shipyard Employment. Accessed 3/16/21. https://www.osha.gov/laws-regs/regulations/standardnumber/1915/1915.88,
- 76.Pierce HM, Perry L, Gallagher R, Chiarelli P. Delaying voiding, limiting fluids, urinary symptoms, and work productivity: A survey of female nurses and midwives. J Adv Nurs. 2019;75(11):2579–2590. [DOI] [PubMed] [Google Scholar]
- 77.Shoham DA, Wang Z, Lindberg S, et al. School toileting environment, bullying, and lower urinary tract symptoms in a population of adolescent and young adult girls: Preventing lower urinary tract symptoms consortium analysis of Avon longitudinal study of parents and children. Urology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lundblad B, Hellström AL. Perceptions of school toilets as a cause for irregular toilet habits among schoolchildren aged 6 to 16 years. J Sch Health. 2005;75(4):125–128. [DOI] [PubMed] [Google Scholar]
- 79.Camenga DR, Brady SS, Hardacker CT, et al. U.S. Adolescent and adult women’s experiences accessing and using toilets in schools, workplaces, and public spaces: A multi-site focus group study to inform future research in bladder health. Int J Environ Res Public Health. 2019;16(18). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Peake S, Manderson L. The constraints of a normal life: the management of urinary incontinence by middle aged women. Women Health. 2003;37(3):37–51. [DOI] [PubMed] [Google Scholar]
- 81.Schneider B The dirty truth about San Francisco’s sidewalks. Is the city really drowning in filth? In: Lab BC, ed2018. Accessed 3/16/21. https://www.bloomberg.com/news/articles/2018-08-02/san-francisco-s-sidewalk-poop-crisis-explained. [Google Scholar]
- 82.Fultz NH, Fisher GG, Jenkins KR. Does urinary incontinence affect middle-aged and older women’s time use and activity patterns? Obstet Gynecol. 2004;104(6):1327–1334. [DOI] [PubMed] [Google Scholar]
- 83.Morin JP, King AB, Goetz LL, Wolfe LG, Klausner AP. Racial disparities in bladder management in veterans with spinal cord injury and disorders. Neurourol Urodyn. 2019;38(3):968–974. [DOI] [PubMed] [Google Scholar]
- 84.Sosland R, Kowalik CA, Cohn JA, et al. Nonclinical barriers to care for neurogenic patients undergoing complex urologic reconstruction. Urology. 2019;124:271–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Luppa M, Luck T, Weyerer S, König HH, Brähler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39(1):31–38. [DOI] [PubMed] [Google Scholar]
- 86.Wagner THMK, Subak LL, de Wachter S, Dudding T. Incontinence. Paper presented at: 6th International Consultation on Incontinence; 2017, 2017; Tokyo. [Google Scholar]
- 87.Subak LL, Brown JS, Kraus SR, et al. The “costs” of urinary incontinence for women. Obstet Gynecol. 2006;107(4):908–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Diokno AC, Sand PK, Macdiarmid S, Shah R, Armstrong RB. Perceptions and behaviours of women with bladder control problems. Fam Pract. 2006;23(5):568–577. [DOI] [PubMed] [Google Scholar]
- 89.Coyne KS, Wein A, Nicholson S, Kvasz M, Chen CI, Milsom I. Economic burden of urgency urinary incontinence in the United States: a systematic review. J Manag Care Pharm. 2014;20(2):130–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Antonelli JA, Maalouf NM, Pearle MS, Lotan Y. Use of the National Health and Nutrition Examination Survey to calculate the impact of obesity and diabetes on cost and prevalence of urolithiasis in 2030. Eur Urol. 2014;66(4):724–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.United States Environmental Protection Agency. Facts and Figures About Materials, Waste and Recycling. Guide to the Facts and Figures About Materials, Waste and Recycling. Accessed: 3/22/2021. https://www.epa.gov/facts-and-figures-about-materials-waste-and-recycling/guide-facts-and-figures-report-about-materials [Google Scholar]
- 92.Itsubo N, Wada M, Imai S, Myoga A, Makino N, Shobatake K. Life cycle assessment of the closed-loop recycling of used disposable diapers. Resources. 2020;9(3). [Google Scholar]
- 93.Willskytt STA-M. Resource efficiency of consumables - Life cycle assessment of incontinence products. Resour Conserv Recy. 2019;144:13–23. [Google Scholar]
- 94.Younes L The future: Energy-producing diapers. The EPA Blog blog. Vol 2021. https://blog.epa.gov/tag/disposalbe-diapers/ [Google Scholar]
- 95.Feldstein CA. Nocturia in arterial hypertension: a prevalent, underreported, and sometimes underestimated association. J Am Soc Hypertens. 2013;7(1):75–84. [DOI] [PubMed] [Google Scholar]
- 96.Tabara Y, Matsumoto T, Murase K, et al. Frequent nocturnal urination in older men is associated with arterial stiffness: The Nagahama study. Hypertens Res. 2019;42(12):1996–2001. [DOI] [PubMed] [Google Scholar]
- 97.Khan SA, Rahman EU, Chobufo MD, et al. Nocturia is an independent predictor of abdominal aortic calcification in women: Results from the National Health and Nutrition Examination Survey. J Community Health. 2020;45(6):1111–1115. [DOI] [PubMed] [Google Scholar]
- 98.Pressman MR, Figueroa WG, Kendrick-Mohamed J, Greenspon LW, Peterson DD. Nocturia. A rarely recognized symptom of sleep apnea and other occult sleep disorders. Arch Intern Med. 1996;156(5):545–550. [DOI] [PubMed] [Google Scholar]
- 99.Tsai M, Khayat R. Sleep apnea in heart failure. Curr Treat Options Cardiovasc Med. 2018;20(4):33. [DOI] [PubMed] [Google Scholar]
- 100.Victor RG, Li N, Blyler CA, et al. Nocturia as an unrecognized symptom of uncontrolled hypertension in black men aged 35 to 49 years. J Am Heart Assoc. 2019;8(5):e010794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Montorsi P, Ravagnani PM, Galli S, et al. The artery size hypothesis: a macrovascular link between erectile dysfunction and coronary artery disease. Am J Cardiol. 2005;96(12b):19m–23m. [DOI] [PubMed] [Google Scholar]
- 102.Zhao B, Hong Z, Wei Y, Yu D, Xu J, Zhang W. Erectile dysfunction predicts cardiovascular events as an independent risk factor: A systematic review and meta-analysis. J Sex Med. 2019;16(7):1005–1017. [DOI] [PubMed] [Google Scholar]
- 103.Panicker JN, Fowler CJ, Kessler TM. Lower urinary tract dysfunction in the neurological patient: clinical assessment and management. Lancet: Neurol. 2015;14(7):720–732. [DOI] [PubMed] [Google Scholar]
- 104.Roy HA, Nettleton J, Blain C, et al. Assessment of patients with lower urinary tract symptoms where an undiagnosed neurological disease is suspected: A report from an International Continence Society consensus working group. Neurourol Urodyn. 2020;39(8):2535–2543. [DOI] [PubMed] [Google Scholar]
- 105.Daneshgari F, Liu G, Birder L, Hanna-Mitchell AT, Chacko S. Diabetic bladder dysfunction: current translational knowledge. J Urol. 2009;182(6 Suppl):S18–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hardacker CT, Baccellieri A, Mueller ER, et al. Bladder health experiences, perceptions and knowledge of sexual and gender minorities. Int J Environ Res Public Health. 2019;16(17). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. Am J Public Health. 2015;105(12):e60–76. [DOI] [PMC free article] [PubMed] [Google Scholar]


