Abstract
The limited number of effective antituberculosis drugs available necessitates optimizing current treatments. We show that melatonin, which is synthesized in the pineal gland, can cause at least a threefold increase in the efficacy of isoniazid. This suggests that tuberculosis chemotherapy can be improved by innate molecules such as melatonin.
Free radicals are usually regarded as harmful, but they can be utilized in the destruction of tumors and can protect against infection, such as nitric oxide and reactive oxygen intermediates in macrophages (4). Melatonin, a natural substance produced by the pineal gland in animals (9), has no known toxicity and has been shown to protect against harmful reactive free radical species in animals (15–17). Melatonin protects against infection and is thought to do so via its pro-oxidative properties (2, 3, 7, 10). However, there are no reports concerning the effect melatonin has on the viability of pathogenic bacteria, such as Mycobacterium tuberculosis. Other agents, such as isoniazid (INH), may depend on the generation of free radicals for their effects (8). INH is a frontline drug of tuberculosis therapy but problems associated with it include the rapid development of drug resistance and potential adverse reactions in many patients. Therefore, agents which potentiate existing concentrations of INH (without adverse side-effects) or allow the use of a lower INH concentration may be extremely important.
Mycobacterium bovis BCG and strains of drug sensitive and resistant M. tuberculosis were cultured in Middlebrook’s 7H9 (13) medium enriched with albumin-dextrose-catalase. Continuous stirring at 37°C kept all cultures uniformly aerated, and they grew reproducibly (<1.0% difference) (12) to log phase (0.4 to 0.6 at A600). Mycobacterial strains included M. tuberculosis H37Rv reference strain and two clinical multidrug-resistant strains (TBRI 40 and TBRI 204; INH resistance occurred at >40 μg/ml, and catalase activities were 0 mm by the method of Kent and Kubica [9a]). From a 1-McFarland BACTEC culture (18), 0.1 ml was inoculated into a BACTEC vial with INH, melatonin, and streptozotocin alone and in different combinations. Controls with no drugs were included. Table 1 shows marginal or no inhibition of growth at melatonin concentrations between 0.26 nM and 0.01 mM. Higher concentrations of melatonin (0.1 to 10 mM) resulted in a dose-dependent inhibition of mycobacterial growth measured in BCG, H37Rv, and clinical strains that was maintained over five doublings (results not shown).
TABLE 1.
M. tuberculosis H37Rv treated with melatonin and INH
| Concn of melatonina | % Growth inhibition of H37Rv with INH at a concn (μg/ml) of:
|
||||||
|---|---|---|---|---|---|---|---|
| 0.00 | 0.005 | 0.010 | 0.02 | 0.025 | 0.05 | 0.1 | |
| 0 nM | 0.0 | 8.5 | 10.2 | 19.2 | 73.6 | 100.0 | 100.0 |
| 0.26 nM | 0.0 | 46.0 | 52.0 | 60.0 | |||
| 1.4 nM | 0.0 | 55.0 | 53.0 | 59.0 | |||
| 26.0 nM | 1.0 | 58.0 | 60.0 | 56.0 | |||
| 2.6 μM | 0.0 | 57.0 | 58.0 | 58.0 | |||
| 0.01 mM | 9.3 | 60.3 | 62.4 | 62.4 | 79.9 | 100.0 | 100.0 |
| 0.1 mM | 14.9 | 65.7 | 69.6 | 67.5 | 81.0 | 100.0 | 100.0 |
| 0.2 mM | 20.9 | 64.3 | 67.9 | 74.7 | 79.3 | 100.0 | 100.0 |
| 0.4 mM | 32.4 | 75.0 | 71.7 | 88.5 | 100.0 | 100.0 | |
| 0.8 mM | 39.7 | 78.4 | 77.9 | 81.1 | 90.3 | 100.0 | 100.0 |
| 1.6 mM | 56.9 | 95.0 | 100.0 | 100.0 | |||
| 2.0 mM | 54.0 | ||||||
| 4.0 mM | 79.0 | ||||||
| 8.0 mM | 94.0 | ||||||
| 10.0 mM | 100.0 | ||||||
Melatonin tested covered physiological concentrations up to 1.4 nM and pharmacological concentrations up to 10 mM.
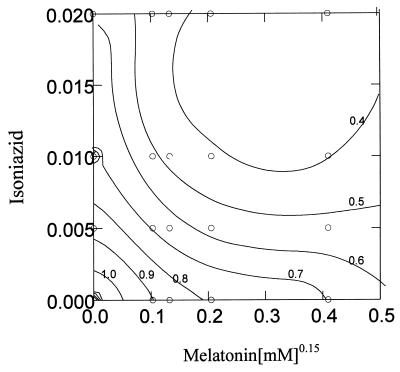
Slight inhibition of H37Rv growth was seen at INH concentrations of 0.005 to 0.01 μg/ml (below the MIC of 0.03 μg/ml) and melatonin concentrations of 0.26 nM to 0.1 mM. At an INH concentration of 0.005 μg/ml and a melatonin concentration of 0.01 mM, bacterial growth was inhibited 3.4-fold more than the sum of the inhibition obtained for the compounds alone (Table 1). A similar effect was observed for M. bovis BCG (Table 2). The MIC for INH in M. bovis BCG was 0.1 μg/ml, and at 0.05 μg/ml INH, BCG growth was slightly inhibited (2%) compared to that of the control. With 0.006 mM melatonin and 0.05 μg of INH/ml, 77% growth inhibition was observed. This is approximately 10-fold higher than the compounds acting alone. Little or no effect on mycobacterial growth relative to the control was observed at any of the following concentrations (Table 1): 0.26 nM melatonin, the average nocturnal plasma concentration in humans; 1.4 nM melatonin, the highest nocturnal level recorded in young adults; 26.0 nM melatonin, the average serum level of humans taking melatonin regularly; and 2.6 μM melatonin, the upper plasma level recorded in humans taking melatonin daily as an antioxidant (5). However, combining these melatonin concentrations with below-MICs of INH resulted in an increased inhibition of H37Rv growth. This effect was analyzed statistically by using a Kriging model in accordance with the method of Cressie (6). The response model was the ratio of the BACTEC growth under a specific treatment combination over the growth in the control. The data of 19 treatment combinations of INH and melatonin were used in the model, and the resulting contour plot showed a bucket-shaped response curve (Fig. 1), which indicates a synergistic interaction between INH and melatonin in M. tuberculosis H37Rv and M. bovis BCG. Combinations of INH and melatonin gave smaller ratios (more inhibition) than those achieved on their own.
TABLE 2.
M. bovis BCG treated with melatonin and INHa
| Concn of melatonin (mM) | % Growth inhibition of BCG with INH at a concn (μg/ml) of:
|
||||
|---|---|---|---|---|---|
| 0.00 | 0.025 | 0.05 | 0.1 | 0.2 | |
| 0.00 | 0.0 | 0.0 | 2.0 | 95.0 | 99.5 |
| 0.006 | 0.0 | 4.6 | 77.0 | ||
| 0.06 | 0.0 | 24.5 | 84.1 | ||
| 0.13 | 20.0 | 54.0 | 79.0 | ||
| 0.25 | 35.0 | 54.3 | 80.7 | ||
| 0.5 | 53.0 | 73.5 | 93.3 | ||
| 10.0 | 100.0 | ||||
The MIC of INH for M. bovis BCG is 0.1 μg/ml.
FIG. 1.
M. tuberculosis H37Rv treated with low concentrations of melatonin (0.26 to 2,600 nM) and INH (0.005 to 0.02 μg/ml) (see Table 1). The contour plot is the result of Kriging analysis of growth index data. The melatonin scale has been transformed to facilitate the response surface modeling by making a power transformation of 0.15. The bucket shape of the response surface indicates a synergistic interaction between INH and melatonin on mycobacterial killing.
Table 3 shows that the growth rates of the multidrug-resistant strains are negatively affected at 10.0-μg/ml concentrations of INH, with maximum growth inhibition at 40.0 μg/ml. Melatonin alone also inhibits bacterial growth in a dose-dependent manner, as it does for H37Rv and M. bovis BCG. No significant cumulative effect was observed with a combination of melatonin and INH, and Kriging analysis showed the effect to be additive for the multidrug-resistant strains.
TABLE 3.
Multidrug-resistant isolates of M. tuberculosis treated with melatonin and INHa
| Concn of melatonin (mM) | % Growth inhibition of multidrug-resistant isolates with INH at a concn (μg/ml) of:
|
||||||
|---|---|---|---|---|---|---|---|
| 0.0 | 0.025 | 0.05 | 0.5 | 10.0 | 20.0 | 40.0 | |
| 0 | 0.0 | 0.0 | 0.0 | 0.0 | 20.0 | 47.5 | 100.0 |
| 0.01 | 13.0 | 0.0 | 0.0 | 7.5 | 49.5 | 57.0 | |
| 0.1 | 17.0 | 11.0 | 15.0 | 8.0 | 41.0 | 67.5 | |
| 0.2 | 24.8 | 23.0 | 33.0 | 33.0 | 52.0 | 70.5 | |
| 0.4 | 37.5 | 40.5 | 41.0 | 40.0 | 57.0 | 79.5 | |
| 0.8 | 57.8 | 60.0 | 53.5 | 60.5 | 72.0 | 94.0 | |
| 1.0 | 54.0 | 67.0 | |||||
| 2.0 | 70.5 | 70.5 | |||||
| 4.0 | 85.0 | 79.5 | |||||
| 8.0 | 98.2 | 94.0 | |||||
| 10.0 | 99.2 | ||||||
Two multidrug-resistant M. tuberculosis patient isolates were treated with melatonin and INH, and the results were averaged. Both strains were resistant to INH (20 and 40 μg/ml) and rifampin and were classified catalase negative (19 and 0 mm).
Intracellular bacterial growth in human monocyte-derived macrophages was studied. These were infected with M. tuberculosis H37Rv, and INH and melatonin were added 16 h later. The concentrations used had no effect on macrophage morphology or viability (results not shown). The growth rate of M. tuberculosis was monitored by the BACTEC system (18). After 5 days of growth in control or drug-treated human macrophages, both 1.6 mM melatonin and a 0.08-μg/ml concentration of INH alone had no significant effect on mycobacterial growth. However, their combination gave a marked reduction in bacterial load, implying potentiation of INH killing of the mycobacteria by melatonin in macrophages.
To demonstrate that oxidative stress may also play a role in the observed effect of melatonin, M. bovis BCG and M. tuberculosis H37Rv were cultured in the presence of streptozotocin, a known free radical donor via nitric oxide (11). At sublethal doses (2 to 20 μM), little growth inhibition of BCG was observed (results not shown). However, in the presence of 2.0 μM streptozotocin, the bactericidal activity of INH was increased such that 0.05 μg/ml approximated the activity seen with INH (alone) at the MIC.
The results show that melatonin enhances the activity of INH. Melatonin, at concentrations in excess of those achieved physiologically, can itself inhibit mycobacterial growth, as can INH. However, at dosages where neither compound exerts significant inhibition of mycobacterial growth, the combined effect was higher than the sum of the individual compounds. This synergistic effect was confirmed by statistical modelling and was also observed with the intramacrophage killing of H37Rv by the combination of melatonin and INH at concentrations which individually have no effect. It is possible that this effect is mediated via formation of radicals, since a similar effect of enhanced bactericidal activity of INH may be seen using other (but toxic) radical donor compounds, such as streptozotocin. Melatonin cytotoxicity through radical generation has been shown in monocytes (14). It is possible that the ability of melatonin to form stable radicals can modify the activation of INH in some way and that the addition of INH to a melatonin radical species may initiate INH activation. Alternatively, melatonin, being substantially hydrophobic, may locate itself in the mycobacterial cell wall, causing destabilization and enhanced permeability for molecules such as INH, as has been shown with other antibacterial drugs (1). For the multidrug-resistant strains, it would appear that melatonin could not reverse resistance. This may be because melatonin does not affect the mechanisms responsible for drug resistance in M. tuberculosis.
Following melatonin administration, there is a 90-min window during which the plasma levels stay elevated before gradually declining to normal. The therapeutic significance of this window is not known, but because melatonin has ready access to all cells (15), it can be postulated that this is a period during which antituberculosis therapy could be enhanced. Therefore, simultaneous dosing with melatonin and INH may be effective. This regimen may be particularly effective for fast acetylators or those experiencing INH-induced hepatotoxicity.
Acknowledgments
We thank GlaxoWellcome Action TB initiative for financial assistance.
We thank Paul Smith (GlaxoWellcome) for helpful discussions and the TB Research Programme of the MRC (South Africa) for the clinical strains used.
REFERENCES
- 1.Barrett B K, Newbolt L, Edwards S. The membrane destabilising action of the antibacterial agent chlorohexidine. FEMS Microbiol Lett. 1994;119:249–253. doi: 10.1111/j.1574-6968.1994.tb06896.x. [DOI] [PubMed] [Google Scholar]
- 2.Ben-Nathan D, Maestroni G J M, Conti A. The protective effect of melatonin in viral and bacterial infections. In: Maestroni G J M, Conti A, Reiter R J, editors. Therapeutic potential of melatonin. Basel, Switzerland: Karger; 1997. pp. 71–80. [Google Scholar]
- 3.Ben-Nathan D, Maestroni G J M, Lustig S, Conti A. Protective effect of melatonin in mice infected with encephalitis virus. Arch Virol. 1995;140:223–230. doi: 10.1007/BF01309858. [DOI] [PubMed] [Google Scholar]
- 4.Bredt D S, Snyder S H. Nitric oxide: a physiologic messenger molecule. Annu Rev Biochem. 1994;63:175–195. doi: 10.1146/annurev.bi.63.070194.001135. [DOI] [PubMed] [Google Scholar]
- 5.Brezezinski A. Melatonin in humans. N Engl J Med. 1997;336:186–195. doi: 10.1056/NEJM199701163360306. [DOI] [PubMed] [Google Scholar]
- 6.Cressie N A C. Statistics for spatial data. New York, N.Y: John Wiley & Sons, Inc.; 1991. [Google Scholar]
- 7.Ellis L C. Melatonin reduces mortality from aleutian disease in mink (Mustela vison) J Pineal Res. 1996;21:214–217. doi: 10.1111/j.1600-079x.1996.tb00288.x. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin D C, Aust S D, Grover T A. Free radicals produced during the oxidation of hydraxines by hypochlorous acid. Chem Res Toxicol. 1996;9:1333–1339. doi: 10.1021/tx960108l. [DOI] [PubMed] [Google Scholar]
- 9.Guerrero J M, Reiter R J. A brief survey of pineal gland-immune system interrelationships. Endocr Res. 1992;18:91–113. doi: 10.1080/07435809209035401. [DOI] [PubMed] [Google Scholar]
- 9a.Kent P T, Kubica G P. A guide for the level III laboratory. Atlanta, Ga: Centers for Disease Control; 1985. pp. 81–82. [Google Scholar]
- 10.Lin J Y, Chadee K. Macrophage cytotoxicity against Entamoeba histolytica trophozoites is mediated by nitric oxide from l-arginine. J Immunol. 1992;141:3999–4004. [PubMed] [Google Scholar]
- 11.Melchiorri D, Reiter R J, Attia A M, Hara M, Burgos M, Nistico G. Potent protective effect of melatonin on in vivo paraquat-induced oxidative damage in rats. Life Sci. 1995;56:83–89. doi: 10.1016/0024-3205(94)00417-q. [DOI] [PubMed] [Google Scholar]
- 12.Meyers P R, Bourn W R, Steyn L M, van Helden P D, Beyers A D, Brown G D. Novel method for rapid measurement of growth of mycobacteria in detergent-free media. J Clin Microbiol. 1998;36:2752–2754. doi: 10.1128/jcm.36.9.2752-2754.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Middlebrook G. Automatable radiometric detection in growth of Mycobacterium tuberculosis in selective media. Annu Rev Respir Dis. 1977;115:1066–1069. doi: 10.1164/arrd.1977.115.6.1066. [DOI] [PubMed] [Google Scholar]
- 14.Morrey K M, McLachlan J M, Serkin C D, Bakouche O. Activation of human monocytes by the pineal hormone melatonin. J Immunol. 1994;153:2671–2680. [PubMed] [Google Scholar]
- 15.Reiter R J. Antioxidant action of melatonin. Adv Pharmacol. 1997;38:103–117. doi: 10.1016/s1054-3589(08)60981-3. [DOI] [PubMed] [Google Scholar]
- 16.Reiter R J, Tang L, Garcia J J, Munoz-Hoyos A. Pharmacological actions of melatonin in oxygen radical pathophysiology. Life Sci. 1997;60:2255–2271. doi: 10.1016/s0024-3205(97)00030-1. [DOI] [PubMed] [Google Scholar]
- 17.Reiter R J, Carneiro R C, Oh C S. Melatonin in relation to cellular antioxidative defense mechanisms. Horm Metab Res. 1997;29:363–372. doi: 10.1055/s-2007-979057. [DOI] [PubMed] [Google Scholar]
- 18.Siddiqui S H. BACTEC 460 TB system. Product and procedure manual. Sparks, Md: Becton Dickinson and Co.; 1995. [Google Scholar]