Summary
Cerclage wiring is used to reinforce the stability of fractures and optimize plate fixations for femoral fractures such as periprosthetic fractures. However, cerclage wiring requires attention to neurovascular structures to prevent injuries. We have presented a case of iatrogenic sciatic nerve injury after osteosynthesis with cerclage wiring. A 71-year-old woman underwent osteosynthesis with cerclage wiring for a proximal periprosthetic femoral fracture. Immediately after the operation, the patient developed motor and sensory disorders, particularly in the sciatic nerve area, leading to a suspicion of nerve injury. Consequently, reoperation showed that the right sciatic nerve was strangulated by the cerclage wire, but the nerve was functional. Since the sciatic nerve was partially continuous and retained sensation to some extent, strangulation release was performed. Subsequently, both sensory and motor disorders improved. This case suggests that attention should be given to not only the blood vessels in the anterior region but also the sciatic nerve in the posterior region when performing cerclage wiring for femoral fractures.
Keywords: Iatrogenic sciatic nerve injury, Cerclage wiring, Proximal periprosthetic femoral fracture, Functional recovery of the peroneal and tibial nerve branch
Introduction
Cerclage wiring, which is used to reinforce the stability of fractures and optimize plate fixations for femoral fractures such as subtrochanteric and periprosthetic fractures, requires attention to soft tissues to prevent injuries. Among soft tissue injuries, vascular injuries have been encountered more frequent,1, 2, 3, 4 while nerve injuries have been encountered occasionally. Here, we have reported a case of iatrogenic sciatic nerve injury after osteosynthesis with cerclage wiring for a proximal periprosthetic femoral fracture.
Case report
A 71-year-old woman underwent total hip arthroplasty with a cemented femoral stem for osteoarthritis of the right hip joint at the age of 68 years. However, the patient sustained a fall and developed right hip pain, prompting her to consult a local hospital. The initial assessment did not reveal any motor or sensory disturbances in the right lower extremity. Radiographs showed a proximal periprosthetic femoral fracture from the greater trochanter to the shaft of the femur (Figure 1). There was no apparent stem loosening, but the fracture line was found in the femur and cemented area around the stem, which was classified as Vancouver type B2 and Baba type 2A. It was a minimally displaced fracture with no stem loosening. Hence, cerclage wiring and plate osteosynthesis were performed (Figure 2). All cerclage wires were passed using a wire passer from the lateral side of the femur to the anterior side. However, immediately after the operation, the patient showed motor deficits in the distal lower extremities. Manual muscle testing (MMT: right/left) results were 5/5 in the iliopsoas, 5/5 in the quadriceps, 5/5 in the biceps femoris, 0/5 in the tibialis anterior, 0/5 in the gastrocnemius, 0/5 in the flexor digitorum longus, and 0/5 in the extensor digitorum longus. In addition, the patient experienced hypoesthesia and numbness in the right lateral lower leg and dorsum of the foot, and anesthesia of the sole of the foot. Right sciatic nerve injury was suspected since the sciatic nerve area is responsible for motor and sensory function. Consequently, the patient was referred to our department, and revision surgery was planned on the fifth postoperative day. During reoperation, the patient was placed in the prone position, and a portion of the gluteus maximus just above the sciatic nerve was dissected. The right sciatic nerve was strangulated by the proximal cerclage wire at the lesser trochanter (Figure 3A). On the release of the nerve, the medial branch of the sciatic nerve, the tibial nerve branch, was severely damaged, while the lateral branch, the peroneal nerve branch, showed some continuity (Figure 3B). Neurolysis was performed after the release of nerve strangulation.
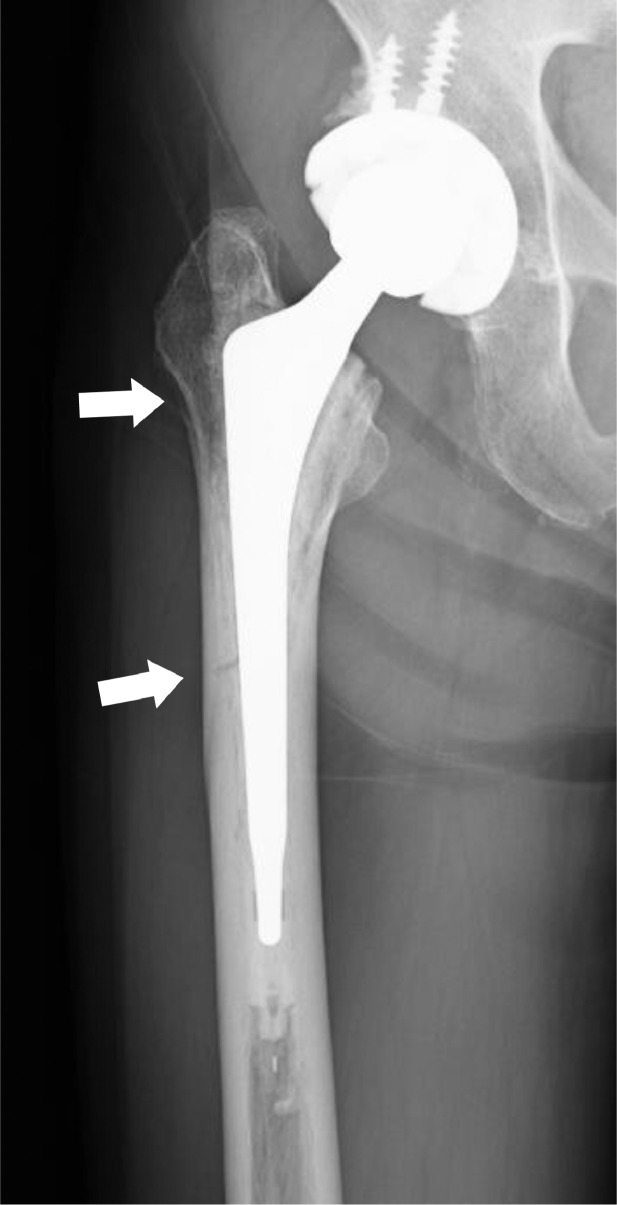
Figure 1.
Preoperative radiographs. There is no apparent stem loosening. However, a fracture line is present from the greater trochanter to the diaphysis (white arrow).
Figure 2.
Postoperative radiographs. Osteosynthesis using a plate with cerclage wiring is performed.
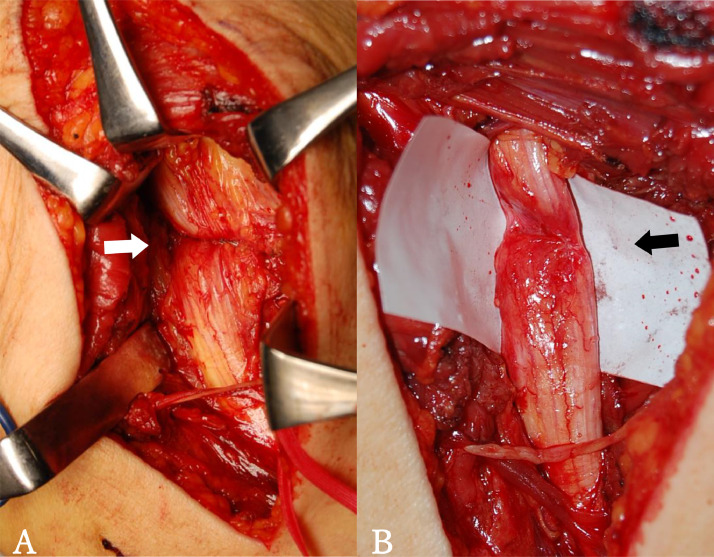
Figure 3.
Intraoperative photographs. (A) The sciatic nerve is strangulated by the cerclage wire (white arrow). (B) After removal of the cerclage wire, the sciatic nerve is mainly injured on the medial branch, while it is partially continuous on the lateral branch (black arrow).
Three months post-surgery, radiographs showed bone union without stem loosening. Twelve months post-surgery, numbness of the lower limbs recovered to approximately 20% of that before reoperation. Moreover, since MMT results revealed 2/5 in the tibialis anterior, 5/5 in the gastrocnemius, 1/5 in the flexor digitorum longus, and 1/5 in the extensor digitorum longus, motor function in the tibial nerve branch recovered better than that in the peroneal nerve branch.
Discussion
Treatment for proximal periprosthetic femoral fractures includes conservative treatment, osteosynthesis, and femoral revision hip arthroplasty. Cerclage wiring with plate osteosynthesis can enhance the stability of the fracture site and provide strong fixation, especially for rotation, compared to plate osteosynthesis alone. 5 Cerclage wiring is also frequently used in various femoral fractures, such as subtrochanteric fractures, as it effectively improving their stability.
However, cerclage wiring is associated with the entrapment of soft tissues, such as nerves and blood vessels. Vascular disruptions resulting iatrogenically from cerclage wiring in the femur occur in 1.6%–7.1% cases. 6 These disruptions can cause lower limb ischemia, which may eventually lead to below-knee amputation, or multiple organ failure, if untreated, which may ultimately lead to death. However, to date, only one case of sciatic nerve injury resulting iatrogenically from cerclage wiring has been reported, and the long-term results are unknown at that time. 7 This is the first report on the long-term results of sciatic nerve injury due to cerclage wiring.
Iatrogenic sciatic nerve injury occurs in acetabular fracture surgeries and total hip arthroplasties, but nerve recovery often occurs spontaneously. However, the treatment plan for sciatic nerve injury caused by cerclage wiring is controversial. Comparing the efficacy of neurolysis, nerve repair, and nerve grafting in sciatic nerve injuries of the buttocks, Kim et al. 8 reported that the recovery of the tibial and peroneal nerve branches was 87% and 71% for neurolysis, 73% and 30% for nerve repair, and 62% and 24% for nerve grafting. Similarly, Gousheh et al. 9 reported that the recovery of the tibial and peroneal nerve branches was 80% and 20% for neurolysis, 90% and 17% for nerve repair, and 80% and 21% for nerve grafting. In summary, all techniques resulted in effective tibial nerve branch recovery; however, peroneal nerve branch recovery was evidently inferior. In our case, there was no apparent rupture of the sciatic nerve. The peroneal nerve branch showed continuity, but there was critical nerve damage in the tibial nerve branch. Considering that there was no significant difference in treatment methods for the tibial nerve branch, there was continuity of the peroneal nerve with some residual sensation, and the patient's age, cerclage wire removal, and neurolysis were chosen to maximize the current function of the nerve. One year after reoperation, the nerve function of the tibial nerve branch showed greater recovery than that of the peroneal nerve branch, substantiating previous reports.
Modification in the usage of cerclage wire passers is imperative to prevent vascular and nerve injury. In our case, in the initial surgery, the cerclage passer was passed from the lateral side of the femur to the anterior side. If the wire passer is passed from the anterior side of the femur, it will not be possible to pass the apparatus along the posterior femoral cortex, prohibiting retraction of the sciatic nerve. Therefore, it is important to pass the wire passer from the posterior side of the femur to the anteromedial side along the bone cortex in the proximal part of the femur (Figure 4). Moreover, as reported by Apivatthakakul et al. 10, prior to using the wire passer, it is important to have sufficient knowledge of the neurovascular anatomy and the danger zones surrounding the fracture site to effectively reduce the fracture while making an appropriate incision for the wire passer to be handled securely. An appropriate wire passer with correct curvature and size must be used to allow sufficient space for cerclage wiring to completely encircle the bone while avoiding soft tissue entrapment.
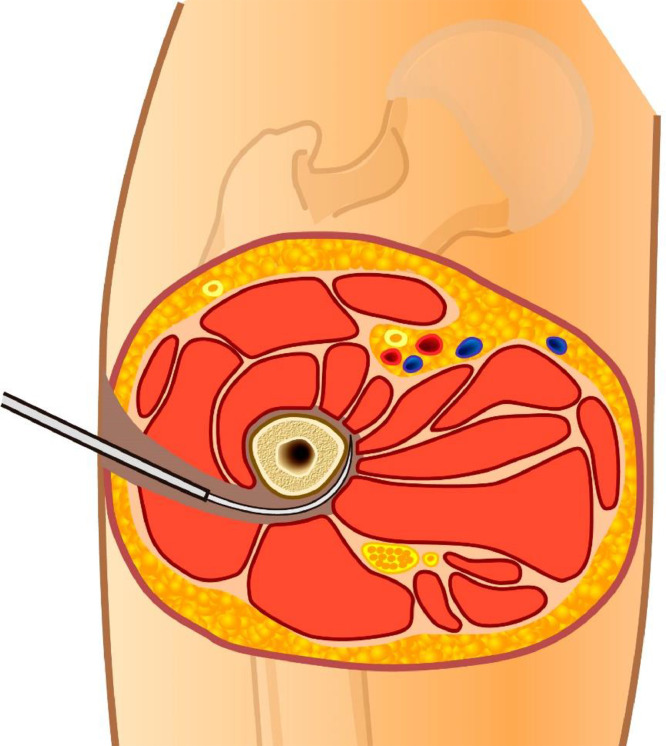
Figure 4.
Visualization on the proper use of the wire passer at the proximal femur. Sufficient space must be created between the bone and the soft tissue prior to the insertion of the wire passer. The wire passer is then inserted posteriorly, passing it alongside the bone cortex to the anterior medial femur.
Conclusion
A case of iatrogenic sciatic nerve injury due to cerclage wiring for a proximal periprosthetic femoral fracture was encountered. Although carefully monitoring of future progress is necessary, the outcomes 1 year after the sciatic nerve injury repair showed good functional recovery of the tibial nerve branch, while poor functional recovery of the peroneal nerve branch. This case suggests that attention should be paid to not only the anterior blood vessels but also the posterior nerves when performing cerclage wiring for femoral fractures.
Acknowledgments
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding statement
No funding was used in this study.
Conflict of Interest
There are no conflicts of interest to declare.
Guidelines
This report was written in line with the STROBE guidelines.
Ethical approval statement
This study was conducted in accordance with the Standards of the Committee on Human
Experimentation of the institution and was approved by the review board (approval No.1786).
References
- 1.Mehta V, Finn HA. Femoral artery and vein injury after cerclage wiring of the femur: a case report. J Arthroplasty. 2005 Sep;20(6):811–814. doi: 10.1016/j.arth.2004.12.050. [DOI] [PubMed] [Google Scholar]
- 2.Aleto T, Ritter MA, Berend ME. Case report: superficial femoral artery injury resulting from cerclage wiring during revision THA. Clin Orthop Relat Res. 2008 Mar;466(3):749–753. doi: 10.1007/s11999-007-0109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Won Y, Yang KH, Kim KK, Weaver MJ, Allen EM. Amputated limb by cerclage wire of femoral diaphyseal fracture: a case report. Arch Orthop Trauma Surg. 2016 Dec;136(12):1691–1694. doi: 10.1007/s00402-016-2580-z. [DOI] [PubMed] [Google Scholar]
- 4.Ehlinger M, Niglis L, Favreau H, Kuntz S, Bierry G, Adam P, et al. Vascular complication after percutaneous femoral cerclage wire. Orthop Traumatol Surg Res. 2018 May;104(3):377–381. doi: 10.1016/j.otsr.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE. Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty. 2000 Jun;15(4):523–528. doi: 10.1054/arth.2000.4339. [DOI] [PubMed] [Google Scholar]
- 6.Devendra A, Avinash M, Chidambaram D, Dheenadhayalan J, Rajasekaran S. Vascular injuries due to cerclage passer: Relevant anatomy and note of caution. J Orthop Surg (Hong Kong) 2018 Jan-Apr;26(1) doi: 10.1177/2309499018762616. [DOI] [PubMed] [Google Scholar]
- 7.Mallory TH. Sciatic nerve entrapment secondary to trochanteric wiring following total hip arthroplasty. A case report. Clin Orthop Relat Res. 1983 Nov;(180):198–200. [PubMed] [Google Scholar]
- 8.Kim DH, Murovic JA, Tiel R, Kline DG. Management and outcomes in 353 surgically treated sciatic nerve lesions. J Neurosurg. 2004 Jul;101(1):8–17. doi: 10.3171/jns.2004.101.1.0008. [DOI] [PubMed] [Google Scholar]
- 9.Gousheh J, Arasteh E, Beikpour H. Therapeutic results of sciatic nerve repair in Iran-Iraq war casualties. Plast Reconstr Surg. 2008 Mar;121(3):878–886. doi: 10.1097/01.prs.0000299286.67932.88. [DOI] [PubMed] [Google Scholar]
- 10.Apivatthakakul T, Siripipattanamongkol P, Oh CW, Sananpanich K, Phornphutkul C. Safe zones and a technical guide for cerclage wiring of the femur: a computed topographic angiogram (CTA) study. Arch Orthop Trauma Surg. 2018 Jan;138(1):43–50. doi: 10.1007/s00402-017-2804-x. [DOI] [PubMed] [Google Scholar]