Abstract
Background
There has been promising progress toward screening, testing, and retaining patients with HIV in care in Ethiopia. Concern exists that possible disruptions in HIV programs due to coronavirus disease 2019 (COVID-19) could result in a more HIV-related mortality and new HIV infections. This study aimed to investigate the real-time burden of COVID-19 on patients with HIV attending antiretroviral therapy.
Methods
We conducted a facility-based, multicenter, and cross-sectional study among patients with HIV attending antiretroviral therapy in 10 healthcare facilities in Addis Ababa, Ethiopia, in the COVID-19 pandemic period. Data were collected using adapted, interviewer-based questionnaires, and entered into EpiInfo version 7 and exported to SPSS version 26 for analysis.
Result
A total of 212 patients with HIV were included. The participants who missed visits for refill were 58 (27.4%). When the effects of other independent variables on appointments/visits for refill were controlled, the following characteristics were found to be the most important predictors of missed appointments (p< 0.05): age ≥ 55 [adjusted odds ratio (AOR) = 6.73, 95% CI (1.495–30.310)], fear of COVID-19 [AOR = 24.93, 95% CI (2.798–222.279)], transport disruption [AOR = 4.90, 95% CI (1.031–23.174)], reduced income for traveling to a health facility [AOR = 5.64, 95% CI (1.234-25.812)], limited access to masks [AOR = 7.67, 95% CI (1.303–45.174)], sanitizer [AOR = 0.07, 95% CI (0.007–0.729)], and non-medical support [AOR = 2.32, 95% CI (1.547–12.596)]. The participants were well aware of the COVID-19 preventive measures. The most costly COVID-19 preventive measures that cause financial burden to the patients were the costs for buying face masks (63.7%), disinfectants (55.2%), and soap for handwashing (22.2%). The participants who missed follow-up diagnostic tests were 56 (26.4%). Variables, which were found to be statistically significant, include the following: age ≥ 55 [AOR = 0.22, 95% CI (0.076–0.621)], partial lockdown [AOR = 0.10, 95% CI (0.011–0.833)], limited access to health services [AOR = 0.15, 95% CI (0.045–0.475)], reduced income for traveling to health facility [AOR = 0.18, 95% CI (0.039–0.784)], and unable to get masks [AOR = 0.12, 95% CI (0.026–0.543)]. The participants who missed counseling services were 55 (25.9%). In multivariate logistic regression, the following were statistically significant: age ≥ 55 [AOR = 0.21, 95% CI (0.078–0.570)], fear of COVID-19 [AOR = 0.11, 95% CI (0.013–0.912)], reduced income [AOR = 0.17, 95% CI (0.041–0.699)], unable to get face masks [AOR = 0.19, 95% CI (0.039–0.959)], and partial lockdown [AOR = 0.08, 95% CI (0.008–0.790)].
Conclusions
The COVID-19 had a significant burden on patients with HIV to attend their routine clinical care and treatment, which may lead to treatment failure and drug resistance. The impact was on their appointments for medication refills and clinical and laboratory follow-ups. Targeted initiatives are needed to sustain HIV clinical care and treatment services and improve the well-being of people living with HIV.
Keywords: coronavirus disease 2019 (COVID-19), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), HIV, clinical care, treatment, antiretroviral therapy, Ethiopia
Background
Coronavirus disease 2019 (COVID-19) could be the most catastrophic pandemic in modern history. It has infected over 173,674,509 people globally and resulted in more than 3,744,408 deaths as of June 9, 2021 (1). Countries have been taking strong preventive measures to reduce and curve the transmission (2–4). Many health care professionals shifted and health facilities were repurposed into targeted COVID-19 centers to manage patients (5–7). Evidence showed these measures have led to restrictions of health facilities to the management of emergency medical conditions and chronic diseases care and treatment services (8, 9). Ethiopia, a country in sub-Saharan Africa (SSA), is categorized under COVID-19 epidemic phase III (advancing outbreak) according to the Africa Centers for Disease Control and Prevention (Africa CDC) classification (10). On March 13, 2020, the first known case of COVID-19 in Ethiopia was reported in the capital city (11). As of December 17, 2021, people that have been diagnosed with the coronavirus were 374,402, of whom 6,855 (1.83%) died, 16,850 (4.50%) are still sick, and 350,697 (93.67%) have recovered (12). Addis Ababa became the first major city in Ethiopia to report cases and deaths from COVID-19. In Ethiopia, COVID-19 imposed a burden on physical infrastructure and exacerbated the preexisting weaknesses of health systems. As the country has limited numbers of hospitals and health centers, it presented a significant challenge to manage the pandemic and other diseases simultaneously (11–13).
By the end of 2020, it was estimated that 37.6 million people have HIV infection globally, and 1.5 million are newly infected. Only 27.4 million of them are on treatment with antiretroviral therapy (ART), which means 10.2 million (27%) people are still remains untreated with ART (14). The HIV remains highly prevalent in Africa, accounting for more than 67% of the people living with HIV/AIDS (PLWH) worldwide (15). The sub-Saharan region is the most affected place in the world with 25.6 million PLWH (16). Ethiopia is one of the majorly affected countries in sub-Saharan Africa with a national prevalence rate 0.9% (17). Concern exists that possible disruptions in HIV programs due to COVID-19 could result in more HIV-related mortality and new HIV infections.
The double burden of COVID-19 and HIV is one of the major health challenges, especially in developing countries with high HIV prevalence (18). The PLWH might be particularly at high risk for infection with poor clinical outcomes (19–22). Containment measures, disruptions to supply chains, and loss of income have the potential to exacerbate the impacts of the pandemic on patients with HIV (23). While these impacts will vary significantly across countries, some recommended providing ART for 3–6 months, and others began to offer home delivery services through volunteers to reduce the adverse health outcomes (24, 25). The extensive demand for physicians has led to the rescheduling of routine reviews and hospital visits of patients with HIV (26–28). Fear of COVID-19 exacerbated food insecurity, and COVID-19 protective behaviors hindered voluntary HIV testing and healthcare services.
Many countries warned that they are at risk of stock-outs of antiretroviral (ARV) medicines, and some have critically low stocks as a result of the pandemic (29). In addition, PLWH were doubtful about the availability of ART services and about which HIV clinic to attend in the pandemic period (30).
There are limited real-time patient-level pieces of research on how effective and useful country-level COVID-19 interventions were for patients with HIV. As well, the impact of the COVID-19 pandemic on HIV at a population level is not well-known. With the limited level of evidence in the world and as to our knowledge, no research was done on the impact of the pandemic on patients attending HIV care and treatment services in Ethiopia. There is an urgent need for adequately powered studies that investigate the impact of COVID-19 on HIV clinical care and treatment to augment the health of people living with HIV.
Thus, this study aimed to investigate the real-time burden of COVID-19 on people living with HIV who were attending antiretroviral therapy facilities in Addis Ababa, Ethiopia.
Methods
Design and Setting
A cross-sectional multi-center study was carried out at 10 primary health care centers in Addis Ababa, from March 15 to April 25, 2021. The city has 10 sub-cities and 116 woredas, and has different government health facilities, including six hospitals and 106 public health centers. In Ethiopia, the COVID-19 pandemic is higher in the capital Addis Ababa (31). Addis Ababa is the highest in HIV prevalence next to Gambella regional state (32). The study was conducted in 10 health facilities, one in each sub-city, which has high flow of patients with HIV.
Participants
In this study, the source population was all patients with HIV of age > 18 years attending care and treatment in the selected health centers. The study population were those who were attending care and treatment services during the data collection period. The participants were included if they were (I) the patients with HIV, as confirmed within the study facilities or result referred from another health facility; (II) a man or a woman aged ≥ 18 years; (III) volunteered to participate in the study. As this study was conducted during the high COVID-19 time in Ethiopia, we approached only 212 participants to minimize the exposure for the pandemic during the interview. All eligible participants who have been attending clinical care and treatment in those study sites during the data collection period were considered with strict precautions to prevent the transmission of the corona virus. The health facilities were selected purposively, one in each subcity, where routine HIV care and treatment services are given and provide services for large number of patients with HIV in comparison with other health centers in the subcities. Patients with HIV who attend clinical care and treatment services during the data collection period were taken from each health facility (Table 1).
Table 1.
Sampling procedure.
| Name of the health facility | Sub-city | No. of. HIV cases on ART |
|---|---|---|
| Addis raey HC | Addis ketema | 20 |
| Akaki HC | Akakikality | 50 |
| Kebena HC | Arada | 18 |
| Goro HC | Bole | 11 |
| Addisugebya HC | Gulele | 16 |
| Kazanchis HC | Kirkos | 30 |
| Alem bank | Kolfe | 10 |
| T/haymanot HC | Lideta | 36 |
| Woreda 02 HC | Nifas-silk lafto | 10 |
| Woreda 13 HC | Yeka | 11 |
Data Collection
The questionnaire was developed by reviewing relevant literature to ensure reliability. The questionnaire was adapted, pre-tested, and structured to collect primary data for the assessment of the overall impact of COVID-19. During data collection procedures, all the collected data were reviewed and checked daily for their completeness. The data collection instrument was developed in English and was translated to Amharic, and later back-translated to English to check for any inconsistencies or distortion in the meaning and concepts of the words by another person. Eligible participants who were attending the selected health centers were invited to participate. The participants were given information about the study through an information sheet and signed a consent form if they agreed to be part of the study. The data collectors and supervisors were trained before the actual data collection period regarding the approach, objective of the study, and ethical issues. The data collection was interviewer administered, and the questionnaire includes sections, such as sociodemographic characteristics, awareness about preventive measures, care, and treatment services.
Data Analysis and Interpretation
All questionnaires were checked for completeness every day by the principal investigator and supervisors. Data cleaning was conducted at the end of the data entry. The analysis was done using bivariate and multivariate logistic regression to observe the effects of independent variables on the outcome variable while simultaneously controlling for other potential confounding factors. The raw data entered into Epi Info version 7 to control entry errors and exported to SPSS 26 for analysis.
Results
Sociodemographic Characteristics
A total of 212 patients with HIV were enrolled in the study, with a response rate of 100%, and 133 (62.7%) were female. Of the total, 103 (48.6%) were in the age group 35–54 years. Most of them (41.5%) were married, and 59 (27.8%) had attended primary education. One hundred and forty-six (68.9%) were Orthodox Christian, and 24.1% were governmental employees (Table 2).
Table 2.
Sociodemographic characteristics of respondents, Addis Ababa, Ethiopia, May 2021.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Sex | Male | 79 | 37.3% |
| Female | 133 | 62.7% | |
| Age | 18–34 | 55 | 25.9% |
| 35–54 | 103 | 48.6% | |
| ≥55 | 54 | 25.5% | |
| Marital status | Single | 50 | 23.6% |
| Married | 88 | 41.5% | |
| Widowed | 40 | 18.9% | |
| Divorced | 26 | 12.3% | |
| Separated | 8 | 3.8% | |
| Level of education | No education | 46 | 21.7% |
| Can read and write | 30 | 14.2% | |
| Primary education | 59 | 27.8% | |
| Secondary education | 44 | 20.8% | |
| Diploma and above | 33 | 15.6% | |
| Religion | Orthodox | 146 | 68.9% |
| Muslim | 36 | 17.0% | |
| Protestant | 21 | 9.9% | |
| Catholic | 3 | 1.4% | |
| Others | 6 | 2.8% | |
| Occupation | Student | 3 | 1.4% |
| Daily laborer | 41 | 19.3% | |
| Merchant | 22 | 10.4% | |
| Governmental employee | 51 | 24.1% | |
| Private/NGO employee | 43 | 20.3% | |
| Farmer | 5 | 2.4% | |
| Housewife/unemployed | 47 | 22.2% |
Most Effective Preventive Measure of COVID-19
Most participants (86.8%) responded “Cover mouth nose with a face mask” is the most effective preventive measure of COVID-19. Responses of the study participants on preventive measures such as “stay at home” and “use disinfectant” were 77.4%, 76.4%, respectively (Table 3).
Table 3.
Awareness of respondents on COVID-19 preventive measure, Addis Ababa, Ethiopia, May 2021.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Stay at home | No | 48 | 22.6% |
| Yes | 164 | 77.4% | |
| Maintain physical distancing | No | 87 | 41.0% |
| Yes | 125 | 59.0% | |
| Avoid close contact | No | 85 | 40.1% |
| Yes | 127 | 59.9% | |
| Cover mouth nose with facemask | No | 28 | 13.2% |
| Yes | 184 | 86.8% | |
| Frequent handwashing with soap | No | 43 | 20.3% |
| Yes | 169 | 79.7% | |
| Avoid touching of eyes nose and mouth with unwashed hands | No | 68 | 32.1% |
| Yes | 144 | 67.9% | |
| Avoid mass gathering | No | 92 | 43.4% |
| Yes | 120 | 56.6% | |
| Restrict movement | No | 98 | 46.2% |
| Yes | 114 | 53.8% | |
| Use disinfectant | No | 50 | 23.6% |
| Yes | 162 | 76.4% |
The Financial Burden of COVID-19
The most costly COVID-19 preventive measures that cause financial burden to the patients were costs for buying face masks [135 (63.7%)], disinfectants [117 (55.2%)], and soap for handwashing [47 (22.2%)] (Table 4).
Table 4.
Financial burden of the respondents on the COVID-19 preventive measures, Addis Ababa, Ethiopia, May 2021.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Facemask | No | 77 | 36.3% |
| Yes | 135 | 63.7% | |
| Soap for frequent hand washing | No | 165 | 77.8% |
| Yes | 47 | 22.2% | |
| Disinfectant | No | 95 | 44.8% |
| Yes | 117 | 55.2% |
HIV Care and Treatment Services During COVID-19
The participants who obliged to change a health center were three (1.4%), and 27 (12.7%) denied health services. Almost all the participants said health care providers were polite and respectful (99.5%), willing to listen and answer their questions (99.5%), give attention to their individual needs (99.1%) (Table 5).
Table 5.
Response of study participants on health care facilities and service delivery, Addis Ababa, Ethiopia, May 2021.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Obliged to change the health center because of this pandemic? | Yes | 3 | 1.4% |
| No | 209 | 98.6% | |
| Denied health services? | Yes | 27 | 12.7% |
| No | 185 | 87.3% | |
| Politeness and respect of health professionals? | Yes | 211 | 99.5% |
| No | 1 | 0.5% | |
| Willingness of professionals to listen and answer your questions? |
Yes | 211 | 99.5% |
| No | 1 | 0.5% | |
| Attention of professionals to your individual needs? | Yes | 210 | 99.1% |
| No | 2 | 0.9% | |
| Staff seemed uncomfortable with you? | Yes | 23 | 10.8% |
| No | 189 | 89.2% | |
| Contact care provider when there is a health problem or comorbidities quickly? | Yes | 101 | 47.6% |
| No | 111 | 52.4% |
Main Barriers to Access Health Care During the Pandemic
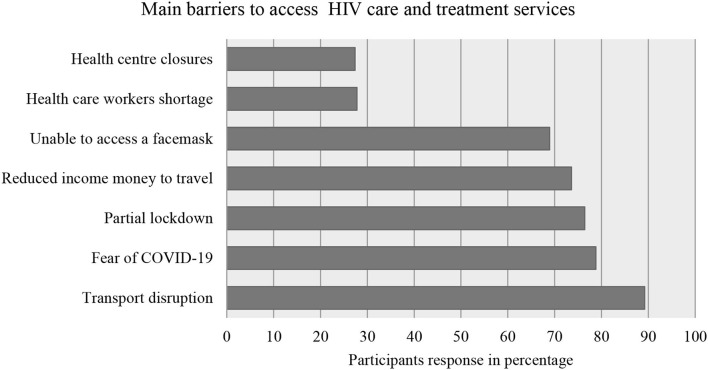
Among the study subjects, 189 (89.2%) said transport disruption was the main barrier to access health care. Fear of getting infected with COVID-19 (78.8%) was the second main barrier for the participants (Figure 1).
Figure 1.
Response of the study participants regarding barriers in accessing health care and treatment during the pandemic, Addis Ababa, Ethiopia, May 2021.
COVID-19 Precaution Measures in Healthcare Facilities
Among the participants, 143 (67.5%) responded that health centers provide screening services for COVID-19, and all health professionals wear masks. The participants responded that there were water (97.2%) and soap (95.8%) at the gate of the healthcare facilities, but not sanitizer (74.1%) (Table 6).
Table 6.
Response of the study participants to the precautions of health facilities for COVID-19 protection, Addis Ababa, Ethiopia, May 2021.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Health center provide screening service for COVID-19? | Yes | 143 | 67.5% |
| No | 69 | 32.5% | |
| Health professionals wear the gloves during caregiving? | Yes | 211 | 99.5% |
| No | 1 | 0.5% | |
| Health professionals wear the mask during caregiving? |
Yes | 212 | 100% |
| No | 0 | 0.0% | |
| Water available at the entrance of the health center for hand washing? | Yes | 206 | 97.2% |
| No | 6 | 2.8% | |
| Soap available at the entrance of the health center for hand washing? | Yes | 203 | 95.8% |
| No | 9 | 4.2% | |
| Sanitizer available at the entrance of the healthcentre for cleaning of hands? |
Yes | 55 | 25.9% |
| No | 157 | 74.1% |
Medications and Follow-Ups During COVID-19
Among the total participants, 125 (59.%) said that the ordered drugs were available. Two hundred (94.3%) were able to collect their multi-month drug supply. The participants who missed appointments, follow-up tests, and counseling services were 58 (27.4%), 56 (26.4%), and 55 (25.9%), respectively (Table 7).
Table 7.
Response of the study participants to medications and follow-up, Addis Ababa, Ethiopia May, 2021.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Availability of ordered drugs? | Yes | 125 | 59.0% |
| Some | 80 | 37.7% | |
| Not at all | 7 | 3.3% | |
| Non-medical support since COVID 19? | Same as before | 163 | 76.9% |
| Slightly harder | 15 | 7.1% | |
| Much harder | 23 | 10.8% | |
| Impossible | 11 | 5.2% | |
| Have you had multi-month drug supply | Yes | 200 | 94.3% |
| No | 12 | 5.7% | |
| For how many months | 3 months | 90 | 42.5% |
| 6 months | 110 | 51.9% | |
| Have you missed appointments (visits) | Yes | 58 | 27.4% |
| No | 154 | 72.6% | |
| Follow-up tests done | Yes | 156 | 73.6% |
| No | 56 | 26.4% | |
| Counseling done on your medication or healthstatus? | Yes | 157 | 74.1% |
| No | 55 | 25.9% |
Logistic Regression Analysis of Missing Appointments/Visits for Medication Refill Variable
Bivariate and Multivariate Logistic Regression analysis showed that the following variables are significantly associated with the likelihood of missing appointments and medication refill. Independent variables, such as older age, less education, fear of COVID-19, transport disruption, reduced income, inability to access mask, no sanitizer availability, and high cost of disinfectant, were related to more missed appointments (Table 8).
Table 8.
Bivariate and multivariate logistic regression analysis of missing appointments/visits for the medication refill variable, Addis Ababa, Ethiopia, 2021.
| Missed appointments | Odds ratio | |||||
|---|---|---|---|---|---|---|
| Variables | Category | No | Yes | COR (CI) | AOR (CI) | P-value |
| Age | 18–34 35–54 ≥55 |
43 (28.0%) 92 (59.7%) 19 (12.3%) |
12 (20.7%) 11 (19.0%) 35 (60.3%) | 1 0.43 (0.175–1.048) 6.60 (2.823–15.434) |
1 0.41 (0.091–1.875) 6.73 (1.495–30.310) | 0.252 0.013* |
| Education | No education Read + write Primary edu. Secondary edu. ≥ Diploma |
14 (9.1%) 19 (12.3%) 50 (32.5%) 38 (24.7%) 33 (21.4%) |
31 (53.5%) 11 (19.0%) 9 (15.5%) 6 (10.3%) 1 (1.7%) | 1 0.25 (0.096–0.670) 0.08 (0.031–0.203) 0.07 (0.024–0.201) 0.01 (0.0012–1.021) |
1 0.01 (0.001–0.165) 0.02 (0.002–0.229) 0.05 (0.003–1.022) 0.01 (0.001–1.002) | 0.001* 0.002* 0.052 0.997 |
| Fear of COVID-19 | No Yes |
44 (28.6%) 110 (71.4%) |
1 (1.7%) 57 (98.3%) | 1 22.80 (3.062–169.782) |
1 24.93 (2.798–222.279) | 0.004* |
| Transport disruption | No Yes |
22 (14.3%) 132 (85.7%) |
1 (1.7%) 57 (98.3%) | 1 9.50 (1.250–31.185) |
1 4.90 (1.031–23.174) | 0.038* |
| Reduced income | No Yes |
53 (34.4%) 101 (65.6%) |
3 (5.2%) 55 (94.8%) | 1 9.62 (2.873–32.219) |
1 5.64 (1.234–25.812) | 0.026* |
| Unable to access mask | No Yes |
64 (41.6%) 90 (58.4%) |
2 (3.4%) 56 (96.6%) | 1 19.91 (4.687–84.577) |
1 7.67 (1.303–45.174) | 0.024* |
| Sanitizer available | No Yes |
110 (71.4%) 44 (28.6%) |
47 (81.0%) 11 (19.0%) | 1 0.58 (0.278–1.231) |
1 0.07 (0.007–0.729) | 0.026* |
| For how many months | 3 months 6 months |
52 (35.9%) 93 (64.1%) |
38 (69.1%) 17 (30.9%) | 1 0.25 (0.129–0.486) |
1 0.33 (0.132–0.825) | 0.018* |
| Cost of disinfectant | No Yes |
85 (55.2%) 69 (44.8%) |
10 (17.2%) 48 (82.8%) | 1 5.91 (2.788–12.539) |
1 16.64 (1.462–189.569) | 0.023* |
| Non-medical support since COVID-19 | Same as before Slightly harder Much harder Impossible |
130 (84.4%) 12 (7.8%) 10 (6.5%) 2 (1.3%) |
33 (56.9%) 3 (5.2%) 13 (22.4%) 9 (15.5%) | 1 0.98 (0.263–3.693) 5.12 (2.064–12.705) 17.72 (3.655–85.987) |
1 3.68 (0.434–31.204) 3.78 0.774–18.421) 2.32 (1.547–12.596) | 0.233 0.100 0.044* |
Statistically significant at p < 0.05, COR, crude odds ratio at 95% confidence interval; AOR, adjusted odds ratio at 95% confidence interval.
Logistic Regression Analysis of the Follow-Up Tests Variable
In Bivariate and Multivariate Logistic Regression analysis of the follow-up tests variable, the following variables found to be significant: age, denied health services, reduced income/money to travel, partial lockdown, and inability to access face masks (Table 9).
Table 9.
Bivariate and multivariate logistic regression analysis of the follow-up tests variable, Addis Ababa, Ethiopia, 2021.
| Followup test | Odds ratio | |||||
|---|---|---|---|---|---|---|
| Variables | Category | No | Yes | COR (CI) | AOR (CI) | P-value |
| Age | 18–34 35–54 ≥55 |
12 (21.4%) 10 (17.9%) 34 (60.7%) |
43 (27.6%) 93 (59.6%) 20 (12.8%) | 1 2.59 (1.041–6.472) 0.16 (0.070–0.382) |
1 2.65 (0.913–7.670) 0.22 (0.076–0.621) | 0.073 0.004* |
| Partial lockdown | No Yes |
1 (1.8%) 55 (98.2%) |
49 (31.4%) 107 (68.6%) | 1 0.04 (0.005–0.295) |
1 0.10 (0.011–0.833) | 0.034* |
| Denied health services | No Yes |
35 (62.5%) 21 (37.5%) |
150 (96.2%) 6 (3.8%) | 1 0.07 (0.025–0.177) |
1 0.15 (0.045–0.475) | 0.001* |
| Reduced income | No Yes |
3 (5.4%) 53 (94.6%) |
53 (34.0%) 103 (66.0%) | 1 0.11 (0.033–0.369) |
1 0.18 (0.039–0.784) | 0.023* |
| Unable to get mask | No Yes |
2 (3.6%) 54 (96.4%) |
64 (41.0%) 92 (59.0%) | 1 0.05 (0.013–0.226) |
1 0.12 (0.026–0.543) | 0.006* |
Statistically significant at p < 0.05, COR, crude odds ratio at 95% confidence interval; AOR, adjusted odds ratio at 95% confidence interval.
Logistic Regression Analysis of the Counseling Variable
Bivariate and Multivariate Logistic Regression analysis of the counseling variable, factors such as age, education, fear of COVID-19, reduced income money to travel, inability to access face masks, and partial lockdown were significant (Table 10).
Table 10.
Bivariate and multivariate logistic regression analysis of the counseling variable, Addis Ababa, Ethiopia, 2021.
| Counslingdone | Odds ratio | |||||
|---|---|---|---|---|---|---|
| Variable | Category | No | Yes | COR (CI) | AOR (CI) | P-value |
| Age | 18–34 35–54 ≥55 |
12 (21.8%) 10 (18.2%) 33 (60.0%) |
43 (27.4%) 93 (59.2%) 21 (13.4%) | 1 2.59 (1.041–6.472) 0.18 (0.077–0.412) |
1 2.28 (0.842–6.170) 0.21 (0.078–0.570) | 0.105 0.002* |
| Education | No education Read + write Primary edu. Secondary edu. ≥Diploma |
29 (52.7%) 11 (20.0%) 8 (14.5%) 6 (10.9%) 1 (1.8%) |
16 (10.2%) 19 (12.1%) 51 (32.5%) 38 (24.2%) 33 (21.0%) | 1 3.24 (1.241–8.449) 11.95 (4.572–31.251) 11.87 (4.142–34.047) 4.60 (0.391–15.227) |
1 3.68 (1.230–11.022) 11.46 (3.906–33.615) 6.48 (1.921–21.876) 1.23 (0.238–6.412) | 0.020* 0.000* 0.003* 0.801 |
| Fear of COVID-19 | No Yes |
1 (1.8%) 54 (98.2%) |
44 (28.0%) 113 (72.0%) | 1 0.05 (0.006–0.354) |
1 0.11 (0.013–0.912) | 0.041* |
| Reduced income | No Yes |
3 (5.5%) 52 (94.5%) |
53 (33.8%) 104 (66.2%) | 1 0.11 (0.034–0.380) |
1 0.17 (0.041–0.699) | 0.014* |
| Unable get face mask | No Yes |
2 (3.6%) 53 (96.4%) |
64 (40.8%) 93 (59.2%) | 1 0.05 (0.013–0.233) |
1 0.19 (0.039–0.959) | 0.044* |
| Partial lockdown | No Yes |
1 (1.8%) 54 (98.2%) |
49 (31.2%) 108 (68.8%) | 1 0.04 (0.005–0.304) |
1 0.08 (0.008–0.790) | 0.031* |
Statistically significant at p < 0.05, COR, crude odds ratio at 95% confidence interval; AOR, adjusted odds ratio at 95% confidence interval.
Discussions
To the best of our knowledge, this study was the first of its kind to assess the impact of COVID-19 on HIV care and treatment services in Ethiopia. We studied the overlap between the two ongoing pandemics (HIV and COVID-19) in Ethiopia. The findings underscore several factors rendering HIV care and treatment services more difficult. A significant number of participants have missed appointments, follow-up tests, and counseling services due to COVID-19. The COVID-19 containment measures taken by the government, sociodemographic characteristics of the patients, and inconsistent access to personal protective equipment are the main factors that have hindered the retention and adherence of patients with HIV to their routine HIV care and treatment.
The patient living with HIV had great concerns about whether they are at high risk for the pandemic and the worse outcomes if they get infected with COVID-19. Research findings on these concerns have been in agreement with previous studies conducted elsewhere (12, 18, 19, 21, 22, 33, 34). Studies indicated that, although the pandemic affected the health care for all disease conditions, chronic patients such as people living with HIV are likely to be uniquely vulnerable (4, 17, 35). It has been reported that the elderly and the people with chronic conditions are more likely to be infected with COVID-19, and patients with HIV may miss appointments as a result. According to this study, older patients with HIV were more likely to miss the clinical care and treatment services given by the health centers. This finding is in agreement with the study done in Addis Ababa in Tikur Anbessa Specialized Hospital (TASH), Dessie town government, and private hospitals where older chronic patients were more likely to miss clinical appointments/visits (36, 37). The result of another study in Uganda was also consistent with this finding that older people were more likely to miss ART and related services (19, 38). In our findings, those who had formal education are more likely to have care and treatment services. This might be because the respondents who had formal education may have a deeper understanding of the negative consequence if they missed their follow-up visits and they could have more tendency to request and to access information about COVID-19 and its preventive measures.
Our results also indicated that patients with HIV, who had a fear of getting infected with COVID-19, were more likely to miss appointments for care and treatment. This is also consistent with other findings (39–41). Containment measures of COVID-19 taken in Ethiopia had a significant contribution to halting the spread of COVID-19 in Ethiopia; however, they had their own implications on HIV care and treatment services as the response from the patients with HIV as indicated. Transport disruption, partial lockdown that impaired mobility, and income reduction were significant factors in missing health care visits, which was in agreement with previous studies conducted in Ethiopia (13, 42), and elsewhere in the world (43–50) that the COVID-19 containment measure had a significant impact on patients' access to healthcare facilities.
Undue expenses related to protective equipment, including face masks and sanitizers, were a burden for the people living with HIV. This finding is in agreement with previous findings in Ethiopia (14) and elsewhere in Africa, wherein sufficient money to buy protective equipment was commonly reported effects of the COVID-19 on attending HIV clinical care and treatment services (51). The city of Addis Ababa introduced innovative measures providing ART medications for 3 to 6 months to mitigate these challenges. In our finding, those who collect medications for 6 months were less likely to miss appointments for medication refill compared to those who took for 3 months.
Indirect impacts arising from the pandemic, which reduced non-medical support, had economical burdens. The participants who said non-medical support was much harder and impossible were more likely to miss clinical visits. Similar observations were reported in other studies as well (52). Furthermore, WHO stated that the COVID-19 pandemic has affected the availability of medicines and non-medical supports in many countries as the world focused on the COVID-19 pandemic (53, 54). Indeed, health centers in Addis Ababa have had preeminent COVID-19 precaution procedures and measures to protect their clients from the pandemic. Availability of sanitizer, water, and soap at the health facilities' gates encouraged the patients with HIV to attend their routine care. These results are in line with a finding from North Shoa health care facilities, where patients who got sanitizer and other supports to protect themselves from the pandemic were more satisfied by health services and attended the clinical appointments/vests (14, 55).
Our study has some limitations. The study was limited to healthcare facilities in Addis Ababa, and, therefore, may not be representative of Ethiopia. As the study design was a cross-sectional study, it does not show a causal relationship and only provides a view of the impacts of COVID-19 in a specific period. Otherwise, the study was based on real-time, patient-level primary data, and it was conducted in a resource-constrained, high-HIV-burden country context.
Conclusion
The COVID-19 had a significant burden on patients with HIV to attend their routine clinical care and treatment, which may lead to treatment failure and drug resistance. The impact was on their appointments for medication refills and clinical and laboratory follow-ups. Targeted initiatives are needed to sustain HIV clinical care and treatment services and improve the well-being of people living with HIV. Stakeholders, such as the Addis Ababa health bureau, the ministry of health, and others, should work in partnership to reduce the impact of this pandemic on those patients to maintain their economic well-being.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Scientific and Ethics Review Committee of the Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), College of Health Sciences, Addis Ababa University. Ethical clearance and support letters were obtained from Addis Ababa public health research and emergency directorate, Addis Ababa City Government Health Bureau. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DC collected the primary data, conducted the analyses, and drafted the manuscript. TM and YW contributed to the data collection and analysis and reviewed the manuscript. All the authors have read and approved the manuscript.
Funding
This study was supported by the Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa). TM was supported in part by the Fogarty International Center and National Institute of Allergy and Infectious Diseases of the US National Institutes of Health (D43TW009127).
Author Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the CDT-Africa or the National Institutes of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors acknowledge the Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), College of Health Sciences, and Addis Ababa University for supporting the study. The authors acknowledge all health centers from where data were collected and study participants for their cooperation. The authors also forward their gratitude to Amarech Taye for her cooperation during the data collection.
Glossary
Abbreviations
- AAU
Addis Ababa University
- COVID-19
Coronavirus Disease 2019
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- HIV
human immunodeficiency virus
- PLWH
people living with HIV
- HC
health center
- ICU
intensive care unit
- PPE
personal protective equipment
- WHO
World Health Organization
- AOR
adjusted odds ratio
- CI
confidence interval.
References
- 1.World Health Organization . Coronavirus disease 2019 (COVID-19) dashboard. Geneva (2021). [Google Scholar]
- 2.Mirzaei H, McFarland W, Karamouzian M, Sharifi H. COVID-19 among people living with HIV: a systematic review. AIDS Behav. (2021) 25:85–92. 10.1007/s10461-020-02983-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lesko CR, Bengtson AM. HIV and COVID-19: intersecting epidemics with many unknowns. Am J Epidemiol. (2021) 190:10–6. 10.1093/aje/kwaa158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones DL, Morgan KE, Martinez PC, Rodriguez VJ, Vazquez A, Raccamarich PD, et al. COVID-19 burden and risk among people with HIV. J Acquir Immune Defic Syndr. (2021) 87:869–74. 10.1097/QAI.0000000000002656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zang X, Krebs E, Chen S, Piske M, Armstrong WS, Behrends CN, et al. Localized HIV modeling study. the potential epidemiological impact of coronavirus disease (2019) (COVID-19) on the human immunodeficiency virus (HIV) epidemic and the cost-effectiveness of linked. Opt-out HIV testing: a modeling study in 6 US Cities. Clin Infect Dis. (2021) 72:e828–34. 10.1093/cid/ciaa1547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gatechompol S, Avihingsanon A, Putcharoen O, Ruxrungtham K, Kuritzkes DR. COVID-19 and HIV infection co-pandemics and their impact: a review of the literature. AIDS Res Ther. (2021) 18:28. 10.1186/s12981-021-00335-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parmley LE, Hartsough K, Eleeza O, Bertin A, Sesay B, Njenga A, et al. COVID-19 preparedness at health facilities and community service points serving people living with HIV in Sierra Leone. PLoS ONE. (2021) 16:e0250236. 10.1371/journal.pone.0250236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budak JZ, Scott JD, Dhanireddy S, Wood BR. The impact of COVID-19 on HIV care provided via telemedicine-past, present, and future. Curr HIV/AIDS Rep. (2021) 18:98–104. 10.1007/s11904-021-00543-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tamuzi JL, Ayele BT, Shumba CS, Adetokunboh OO, Uwimana-Nicol J, Haile ZT, et al. Implications of COVID-19 in high burden countries for HIV/TB: a systematic review of evidence. BMC Infect Dis. (2020) 20:744. 10.1186/s12879-020-05450-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pearson CA Van Schalkwyk C Foss AM O'Reilly KM SACEMA Modelling and Analysis Response Team CMMID COVID-19 working group . Projected early spread of COVID-19 in Africa through 1 June 2020. Euro Surveill. (2020) 25:2000543. 10.2807/1560-7917.ES.2020.25.18.2000543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ethiopian Public Health Institute. COVID-19 Update. Addis Ababa: Ethiopian Public Health Institute (2020). Available online at: https://www.ephi.gov.et/index.php/2014-04-10-07-22-18/
- 12.Corona Scanner,. Realtime Coronavirus Statistics. Ethiopia: Global Corona Virus Statistics; (2021). Available online at: https://corona-scanner.com/country/ethiopia [Google Scholar]
- 13.Mohammed H, Oljira L, Roba KT, Yimer G, Fekadu A, Manyazewal T. Containment of COVID-19 in Ethiopia and implications for tuberculosis care and research. Infect Dis Poverty. (2020) 9:131. 10.1186/s40249-020-00753-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kassie BA, Adane A, Tilahun YT, Kassahun EA, Ayele AS, Belew AK. Knowledge and attitude towards COVID-19 and associated factors among health care providers in Northwest Ethiopia. PLoS ONE. (2020) 15:e0238415. 10.1371/journal.pone.0238415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tesfaye ZT, Yismaw MB, Negash Z, Ayele AG. COVID-19-Related Knowledge, Attitude and practice among hospital and community pharmacists in Addis Ababa, Ethiopia. Integr Pharm Res Pract. (2020) 9:105–12. 10.2147/IPRP.S261275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biressaw W, Tilaye H, Melese D. Clustering of HIV patients in Ethiopia. HIV AIDS. (2021) 13:581–92. 10.2147/HIV.S301510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kibret GD, Ferede A, Leshargie CT, Wagnew F, Ketema DB, Alebel A. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. (2019) 8:90. 10.1186/s40249-019-0594-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zikargae MH. COVID-19 in Ethiopia: assessment of how the Ethiopian government has executed administrative actions and managed risk communications and community engagement. Risk Manag Healthc Policy. (2020) 13:2803–10. 10.2147/RMHP.S278234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asnakew Z, Asrese K, Andualem M. Community risk perception and compliance with preventive measures for COVID-19 pandemic in Ethiopia. Risk Manag Healthc Policy. (2020) 13:2887–s2897. 10.2147/RMHP.S279907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.HIV.gov. Global statistics (2019). Available online at: https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics (accessed July 5, 2021).
- 21.World Health Organization. Summary of the Global HIV Epidemic. Geneva (2019). Available online at: https://www.who.int/gho/hiv/en/
- 22.World Health Organization . Summary of the Global HIV Epidemic. Geneva (2019). Available online at: https://www.who.int/gho/hiv/en/
- 23.Huang J, Xie N, Hu X, Yan H, Ding J, Liu P, et al. Epidemiological, virological and serological features of COVID-19 cases in people living with HIV in Wuhan City: a population-based cohort study. Clin Infect Dis. (2020) 73:e2086–94. 10.1093/cid/ciaa1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nagarakanti SR, Okoh AK, Grinberg S, Bishburg E. Clinical outcomes of patients with COVID-19 and HIV coinfection. J Med Virol. (2021) 93:1687–93. 10.1002/jmv.26533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mondi A, Cimini E, Colavita F, Cicalini S, Pinnetti C, Matusali G, et al. COVID-19 in people living with HIV: clinical implications of dynamics of the immune response to SARS-CoV-2. J Med Virol. (2021) 93:1796–804. 10.1002/jmv.26556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sachdev D, Mara E, Hsu L, Scheer S, Rutherford G, Enanoria W, et al. COVID-19 susceptibility and outcomes among people living with HIV in San Francisco. J Acquir Immune Defic Syndr. (2021) 86:19–21. 10.1097/QAI.0000000000002531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seddiki N, French M. COVID-19 and HIV-associated immune reconstitution inflammatory syndrome: emergence of pathogen-specific immune responses adding fuel to the fire. Front Immunol. (2021) 12:649567. 10.3389/fimmu.2021.649567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thekkur P, Tweya H, Phiri S, Mpunga J, Kalua T, Kumar AMV, et al. Assessing the impact of COVID-19 on TB and HIV programme services in selected health facilities in Lilongwe, Malawi: operational research in real time. Trop Med Infect Dis. (2021) 6:81. 10.3390/tropicalmed6020081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liang M, Luo N, Chen M, Chen C, Singh S, Singh S, et al. Prevalence and mortality due to COVID-19 in HIV co-infected population: a systematic review and meta-analysis. Infect Dis Ther. (2021) 3:1–9. 10.1007/s40121-021-00447-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Riley ED, Hickey MD, Imbert E, Clemenzi-Allen AA, Gandhi M. Coronavirus disease 2019 (COVID-19) and HIV spotlight the United States imperative for permanent affordable housing. Clin Infect Dis. (2021) 72:2042–3. 10.1093/cid/ciaa1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bartilotti Matos F, Davies P. Pearls and pitfalls: Two contrasting HIV diagnoses in the COVID-19 era and the case for screening. J Med Virol. (2021) 93:652–4. 10.1002/jmv.26428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Santos GM, Ackerman B, Rao A, Wallach S, Ayala G, Lamontage E, et al. Economic, mental health, HIV Prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of cisgender gay men and other men who have sex with men. AIDS Behav. (2021) 25:311–21. 10.1007/s10461-020-02969-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mukwenha S, Dzinamarira T, Mugurungi O, Musuka G. Maintaining robust HIV and tuberculosis services in the COVID-19 era: a public health dilemma in Zimbabwe. Int J Infect Dis. (2020) 100:394–5. 10.1016/j.ijid.2020.09.1425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ooms G. COVID-19 and It's Far-reaching Health Impacts in Sub-Saharan Africa. Health Action International (2020). [Google Scholar]
- 35.Swaminathan N, Moussa P, Mody N, Lo KB, Patarroyo-Aponte G. COVID-19 in HIV-infected patients: a case series and literature review. J Med Virol. (2021) 93:2557–63. 10.1002/jmv.26671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aklilu TM, Abebe W, Worku A, Tadele H, Haile T, Shimelis D, et al. The impact of COVID-19 on care seeking behavior of patients at tertiary care follow-up clinics: a cross-sectional telephone survey. Addis ababa, Ethiopia. medRxiv. (2020) 1. 10.1101/2020.11.25.20236224 [DOI] [Google Scholar]
- 37.Singh K, Kondal D, Mohan S, Jaganathan S, Deepa M, Venkateshmurthy NS, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. (2021) 21:685. 10.1186/s12889-021-10708-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muwanguzi PA, Kutyabami P, Osingada CP, Nasuuna EM, Kitutu FE, Ngabirano TD, et al. Conducting an ongoing HIV clinical trial during the COVID-19 pandemic in Uganda: a qualitative study of research team and participants' experiences and lessons learnt. BMJ Open. (2021) 11:e048825. 10.1136/bmjopen-2021-048825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kowalska JD, Kase K, Vassilenko A, Harxhi A, Lakatos B, Lukić GD, et al. The characteristics of HIV-positive patients with mild/asymptomatic and moderate/severe course of COVID-19 disease-A report from Central and Eastern Europe. Int J Infect Dis. (2021) 104:293–6. 10.1016/j.ijid.2020.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Calza L, Bon I, Tadolini M, Borderi M, Colangeli V, Badia L, et al. COVID-19 in patients with HIV-1 infection: a single-centre experience in Northern Italy. Infection. (2021) 49:333–7. 10.1007/s15010-020-01492-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang R, Gui X, Zhang Y, Xiong Y, Gao S, Ke H. Clinical characteristics of COVID-19 patients with HIV coinfection in Wuhan, China. Expert Rev Respir Med. (2021) 15:403–9. 10.1080/17476348.2021.1836965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ssentongo P, Heilbrunn ES, Ssentongo AE, Advani S, Chinchilli VM, Nunez JJ, et al. Epidemiology and outcomes of COVID-19 in HIV-infected individuals: a systematic review and meta-analysis. Sci Rep. (2021) 11:6283. 10.1038/s41598-021-85359-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anka AU, Tahir MI, Abubakar SD, Alsabbagh M, Zian Z, Hamedifar H, et al. Coronavirus disease (2019) (COVID-19): an overview of the immunopathology, serological diagnosis and management. Scand J Immunol. (2021) 93:e12998. 10.1111/sji.12998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pizzirusso M, Carrion-Park C, Clark US, Gonzalez J, Byrd D, Morgello S. Physical and mental health screening in a New York City HIV cohort during the COVID-19 pandemic: a preliminary report. J Acquir Immune Defic Syndr. (2021) 86:e54–60. 10.1097/QAI.0000000000002564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee KW, Yap SF, Ngeow YF, Lye MS. COVID-19 in people living with HIV: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:3554. 10.3390/ijerph18073554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mbithi I, Thekkur P, Chakaya JM, Onyango E, Owiti P, Njeri NC, et al. Assessing the real-time impact of COVID-19 on TB and HIV services: the experience and response from selected health facilities in Nairobi, Kenya. Trop Med Infect Dis. (2021) 6:74. 10.3390/tropicalmed6020074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abdela SG, Berhanu AB, Ferede LM, van Griensven J. Essential healthcare services in the face of COVID-19 prevention: experiences from a referral hospital in Ethiopia. Am J Trop Med Hyg. (2020) 103:1198–200. 10.4269/ajtmh.20-0464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Linnemayr S, Jennings Mayo-Wilson L, Saya U, Wagner Z, MacCarthy S, Walukaga S, et al. HIV care experiences during the COVID-19 pandemic: mixed-methods telephone interviews with clinic-enrolled HIV-infected adults in Uganda. AIDS Behav. (2021) 25:28–39. 10.1007/s10461-020-03032-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kalichman SC, Shkembi B, Kalichman MO, Eaton LA. Trust in health information sources and its associations with COVID-19 disruptions to social relationships and health services among people living with HIV. BMC Public Health. (2021) 21:817. 10.1186/s12889-021-10856-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jarolimova J, Yan J, Govere S, Ngobese N, Shazi ZM, Khumalo AR, et al. Medical mistrust and stigma associated with COVID-19 among people living with HIV in South Africa. AIDS Behav. (2021) 17:1–1. 10.1007/s10461-021-03307-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Celestin K, Allorant A, Virgin M, Marinho E, Francois K, Honoré JG, et al. Short-term effects of the COVID-19 pandemic on HIV care utilization, service delivery, and continuity of HIV antiretroviral treatment (ART) in Haiti. AIDS Behav. (2021) 25:1366–72. 10.1007/s10461-021-03218-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gwadz M, Campos S, Freeman R, Cleland CM, Wilton L, Sherpa D, et al. Black and Latino persons living with HIV evidence risk and resilience in the context of COVID-19: a mixed-methods study of the early phase of the pandemic. AIDS Behav. (2021) 25:1340–60. 10.1007/s10461-021-03177-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Muhula S, Opanga Y, Oramisi V, Ngugi C, Ngunu C, Carter J, et al. Impact of the first wave of the COVID-19 pandemic on HIV/AIDS programming in Kenya: evidence from kibera informal settlement and COVID-19 hotspot counties. Int J Environ Res Public Health. (2021) 18:6009. 10.3390/ijerph18116009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown LB, Spinelli MA, Gandhi M. The interplay between HIV and COVID-19: summary of the data and responses to date. Curr Opin HIV AIDS. (2021) 16:63–73. 10.1097/COH.0000000000000659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nachega JB, Kapata N, Sam-Agudu NA, Decloedt EH, Katoto PDMC, Nagu T, et al. Minimizing the impact of the triple burden of COVID-19, tuberculosis and HIV on health services in sub-Saharan Africa. Int J Infect Dis. (2021) 113 Suppl 1:S16–21. 10.1016/j.ijid.2021.03.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.