Abstract
Purpose
Hook plate (HP) is a popular implant of choice in the management of highgrade acute acromioclavicular joint (ACJ) dislocations. Recently, suspensory loop systems have drawn significant interest with comparable results and additionally does not warrant implant removal. However, no studies have compared the outcomes of HP vis-a-vis Dog Bone TM Button with dual FiberTape® (DB).
Methods
38 patients who underwent HP or Arthroscopic assisted single tunnel DB fixation to stabilize high-grade ACJ dislocations were retrospectively included in study for clinically and radiological evaluation at a minimum follow up of one year. American Shoulder and Elbow Society and Constant Murley scores were used for clinical assessment. The radiological evaluation was done by assessing quality of reduction, measuring coracoclavicular distance (CCD), and extent of subacromial erosion.
Results
For final follow up evaluation, both HP and DB group had 16 patients each. The mean follow-up was 55.38 ± 10.9 and 32.88 ± 14.0 months in HP and DB group, respectively. No significant difference in mean ASES (p=0.71) and CM score (p=0.62) was found between the two groups. The DB group revealed higher CCD at the final follow-up compared to the HP group (p=0.01). Although statistically insignificant, there were more subluxations and dislocations in the DB group (37.5%) compared to the HP group (25%). The subacromial erosion was noted in all cases of the HP group at time of implant removal.
Conclusion
Both groups revealed satisfactory functional and radiological outcome. However, the DB group showed a higher tendency of loss of reduction.
Keywords: Shoulder, Acromioclavicular joint, Dislocation, Hook plate, DogBone Button
Highlights
-
•
Formulation of cinnamon essential oil in emulsion ensures the encapsulation and retention of bioactive compounds for slow release into food products.
-
•
Cinnamon oil emulsion-based films improved the functionality and shelf-life extension and storage stabilities of wax apples (Syzygium samarangense L.)
-
•
Encapsulation of bioactive compounds of cinnamon oil caused a significant increase in the antioxidant activity of active films and preserved the wax apples (Syzygium samarangense L.).
1. Introduction
There are several surgical options are available for the management of acute high-grade ACJ injuries, but none is considered as the gold standard. Currently, two techniques are commonly used to stabilize an unstable AC joint- Hook plate and Suspensory system. Hook plate (HP) is a popular implant used for managing the high-grade ACJ dislocations with good results reported in various series.1,2 However, its application is marred by many complications such as subacromial impingement, subacromial bony erosion, rotator cuff injury, fractures of the clavicle and acromion.3, 4, 5 To avoid these complications from the retained hardware, most authors routinely recommend the plate removal between three to four months postoperatively after the likely healing of coracoclavicular ligament (CCL) and ACJ capsule by fibrosis.6
The mandatory HP removal and other complications of HP led to the development of suspensory loop systems (SLS) wherein the ACJ is kept reduced with the help of strong non-absorbable suture materials between coracoid and clavicle supported by single, dual or triple button systems passed via single or double tunnels, and thus allowing the CCL and ACJ capsule heal with fibrosis. Most SLS are effective in the treatment of ACJ dislocation with satisfactory functional and radiological outcome.7, 8, 9, 10, 11 The latest addition to the SLS is Dog Bone™ Button (Arthrex, Naples, FL) with dual 2-mm FiberTape® rather than dual loop of Fibrewire® of Tight rope®. The design of this device is improvised over the previous generation (TightRope®) with claimed advantages of better distribution of tensile forces due to wider and flatter buttons, a higher ultimate load to failure (as FiberTape® have a larger cross-sectional area) and the need for drilling (3 mm) smaller tunnels to avoid coracoid fracture.12 Recently, it was noted that ACJ dislocation stabilised with ‘dynamic’ Dog Bone™ Button system (Arthrex) either by arthroscopy or miniopen technique provided excellent to good functional outcomes with a stable joint at long term follow-up.13
Several publications have compared the functional and radiological outcomes of Hook plate and suspensory fixation for the ACJ injuries.14 However, no studies have compared the outcomes between HP vis-à-vis DB. The present study was conducted to assess the functional and radiological outcomes, along with complications associated with both techniques. The hypothesis was that the DB group patients would result in superior functional and radiological outcomes with minimal complications.
2. Material and methods
This study was a retrospective, cohort analysis conducted at a single tertiary care center after obtaining Institutional Ethical Committee approval. Between 2014 and early 2016, 18 consecutive patients with acute high-grade ACJ injuries (Rockwood type III and V) underwent HP fixation. Following the evolving modern trends and interests in the application of suspensory fixation devices, between late 2016 and 2018, twenty consecutive acute high-grade ACJ injuries were managed with Arthroscopic assisted single tunnel Dog Bone™ Button dual FiberTape® construct (Arthrex, Naples, US). The inclusion criteria were adult patients (>18 years), high-grade ACJ dislocations (Rockwood type IV,V and VI), Type III in manual laborers, acute injuries (<3 weeks of injury), and a minimum one year follow up after the index surgery. Incomplete follow up/records, revision surgery, and cases with associated fractures of the ipsilateral shoulder or clavicle were excluded from the study.
All patients underwent standard clinical and radiological examinations. The radiological assessment included a bilateral shoulder standing anteroposterior (AP) stress view with 10 pounds around the wrist, and axillary view of the injured side. The type of AC joint dislocation was classified based upon radiological classification suggested by Rockwood. The coracoclavicular distance (CCD) was measured in the AP view by measuring the shortest vertical distance between the superior surface of the coracoid and the inferior surface of the clavicle on both normal and index side [Fig. 1]. The vertical displacement of less than 100% of the contralateral normal side and more than 100% vertical displacement compared to the contralateral normal side was classified as type 3 and 5, respectively. In no case, Alexander view to assess horizontal instability was taken.
Fig. 1.
Plain AP radiograph (stress view) of both shoulders shows increased CCD (>100%) on left side indicating Type 5 ACJ dislocation. AP, anteroposterior; CCD, coracoclavicular distance; ACJ, Acromioclavicular joint.
2.1. Surgical technique
Hook plate: After general anaesthesia, the patient was positioned in a beach-chair position. After sterile preparation and draping, a horizontal incision of about 6–8 cms was made over the lateral end of the clavicle. After raising full-thickness skin flaps, the lateral end of the clavicle and AC joint was exposed. In almost all cases, deltotrapezoid fascia (DTF) and the AC joint capsule was found to be torn. The displaced clavicle was held with a bone clamp and reduced to the corresponding acromial border, both in the horizontal and vertical plane. The ACJ reduction was temporarily held with a transfixing 2 mm K-wire, passed percutaneously from the lateral end of acromion under fluoroscopic control. An interval in the Trapezius muscle fibers overlying the posterior aspect of the AC joint adjacent to the medial border of the acromion and anterior to the spine of the scapula was opened with a curved Hemostat to facilitate placement of hook of the HP. A 3.5 mm (3 or 4 holed) locking Clavicle Hook Plate with a 15 mm long curve was used in all cases. The accuracy of hook position under the acromion was confirmed under fluoroscopic control. The medial end of the plate was seated on to the clavicle with a bone clamp and fixed with a 3.5 mm cortical and two-three locking screws. The transfixing K-wire was removed. The accuracy of ACJ reduction and HP placement was confirmed under fluoroscopic control. In most cases, the remnant ACJ capsule and DTF were repaired with No. 1 Vicryl (Johnson & Johnson, USA). However, in some cases, the repair of DTF was not satisfactory due to poor quality of DTF tissue, and presence of the HP over clavicle hindered the repair. No supplemental coracoclavicular procedure (repair, reconstruction, or suture augmentation) was performed. The wound was closed in layers. All patients were counselled for HP removal at six months after the surgery. We believe that three months are essential for the ligaments and capsule to heal, and an additional three months are required for the consolidation of the healing, without seriously risking the associated complications such as impingement, significant subacromial erosion or rotator cuff tear. However, in the index series, due to various personal reasons, the patients returning for the HP removal varied between six and twelve months.
Dog Button: After general anaesthesia, the patient was positioned in a beach chair position. After standard part preparation and draping, diagnostic shoulder arthroscopy was performed from the standard posterior portal. All intraarticular findings were noted and treated as per standard principles. An anterosuperolateral (ASL) portal was made which opened in rotator interval parallel and anterior to anteromedial biceps pulley. The tissues of the rotator interval were cleared using a radiofrequency device until the undersurface of the coracoid process was visualized till the base. In all cases, ACJ reduction was temporarily held with a transfixing 2 mm K-wire, passed percutaneously from the lateral end of acromion under fluoroscopic control. A 2 cm long incision, perpendicular to the long axis of the clavicle, was made over the clavicle 3 cm medial to the AC joint. Next, Arthrex AC joint guide was placed under the coracoid base and its tip over the clavicle at the site of incision. Under fluoroscopic and arthroscopic control, a guidepin was inserted from the superior surface of the clavicle to the inferior surface of the coracoid base. Then, guidepin was over drilled with a 2.4 mm cannulated drill. The guidepin was removed while cannulated drill was left in situ. A suture lasso was inserted from the top of the cannulated drill and was retrieved from the base of coracoid via the cannula in the ASL portal. The cannulated drill was removed, leaving only the suture lasso passing via the coracoclavicular tunnel. Next, tails of two tapes (FibreTape® and TigerTape®) were passed via the slot of Dog Bone™ Button, and then tails were passed inside the loop of suture lasso. The Dog button was gently held with a broad tissue grasper, and the suture lasso was slowly pulled out from the superior clavicular cortex dragging the dual tapes in the coracoclavicular tunnel till the concave surface of Dogbutton got seated on the base of the coracoid process.
The adequate seating of the Dogbutton over the undersurface of coracoid was facilitated by the tissue grasper and confirmed arthroscopically as well as under fluoroscopic control. Next, four tails of suture tapes were loaded on another Dog-button, and Dogbutton was pushed down over the superior cortex of the clavicle hole till the concave surface of Dogbutton was seated correctly over the superior clavicle cortex. The fixation was secured by knotting two tapes sequentially, and suture limbs were cut. Once again, the reduction was confirmed under the image intensifier, and K-wire was removed. In none of the cases of DB fixation, no attempts were made to repair capsule of AC joint, DTF, or coracoclavicular ligament. The wounds were closed in layers, and sutures applied. Postoperative AP and axillary radiographs were taken to confirm the accurate reduction and implant position.
2.2. Post-op rehabilitation protocol (HP and DB group)
HP Group: The patients were given arm sling for three weeks, and they were advised to initiate gentle passive forward flexion up to 90°, 45° abduction and 30° of external rotation in the supine position from the very next day. From the fourth week onwards, they could actively move the shoulder in all directions in gradual fashion along with the simultaneous strengthening of cuff and scapular muscle. Return to routine activities was permitted at the end of 3 months, and sports was allowed only after implant removal. The HP was removed between 6 and 12 months after the index surgery. Post HP removal, patients were not allowed to lift heavy weight (more than 5 kg) or participate in sports for three months to let the screw holes heal and avoid stress fractures in the clavicle. Three months after the HP, patients were permitted to participate in sports and all heavy activities.
DB group: The patients were given arm sling for four weeks, and they were advised to initiate gentle passive 45° forward flexion, 45° abduction and 30° of external rotation to be performed in supine from the very next day. At 5th week, they were permitted to actively move the shoulder in all directions in gradual fashion along with the simultaneous strengthening of cuff and scapular muscle. Return to routine activities was allowed at the end of 3 months. Return to active sports or heavy lifting activities was permitted after six months.
Follow up: The patients in both groups came for clinical and radiological follow up at one, three, and six months regularly. AP and axillary radiographs of index shoulder were taken on each visit to check the quality of reduction in the superior-inferior and horizontal plane and note complications, if any. However, after six months, only patients of the HP group came for implant removal, whereas patients of the DB group were reviewed as and when required. After IEC clearance for the study, all patients were requested to return for one last follow up for clinical and radiological assessment. The patients in the DB group were followed up to a minimum of one-year postoperative, whereas patients from the HP group were followed up to a minimum of six months after the HP removal. The final clinical follow up involved American shoulder and elbow (ASES) and Constant Murley (CM) scoring, plain radiograph of the shoulder, and to note any complications of surgery. The radiological assessment involved Anteroposterior (AP) and axillary radiograph for assessment of the quality of reduction (intact, subluxation or dislocation), evidence of AC joint arthritis, lateral end clavicle osteolysis or any complications (subacromial osteolysis, fractures of acromion or clavicle, HP breakage, screw loosening or breakage and dog button migration). In the AP view of immediate postoperative and final follow-up x rays, the quality of ACJ reduction was noted. It was categorized as ‘intact’ (reduction remained the same as postoperative accurate reduction wherein inferior cortex of clavicle and acromion were at the same level), ‘subluxed’ (partial loss of contact of lateral end of clavicle with the medial end of acromion), ‘dislocated’ (complete loss of contact of lateral end of clavicle with the medial end of acromion), and ‘over-reduction’ wherein the inferior cortex of lateral end of the clavicle was inferior to the inferior cortex of the acromion. The CCD was measured in the AP view, and was compared with CCD of the normal side. CCD was further classified into two categories of loss of reduction; CCD <3 mm and CCD ≥ 3 mm. Similar categorization of CCD was performed by Çarkçı et al. to assess differences in clinical scores in patients with higher loss (>3 mm) in reduction compared to lesser loss (<3 mm).15
The subacromial osteolytic zone, if present, was measured in AP view of shoulder immediately after the HP removal and again, at last, follow up to assess its continuation or resolution. The axillary view was utilized to assess the quality of reduction in the horizontal plane.
Statistical analysis: It was performed using SPSS version 22 (IBM, Armonk, NY, USA). For all the tests, the level of significance was defined as P < 0.05. A paired t-test was performed for the analysis of pre-operative and postoperative coracoclavicular distances (CCD) for the same group. An independent t-test was performed for comparing remaining parametric data between the HP and DB groups. One way ANOVA test was performed to assess the ASES and CM scores in patients of two groups with an intact, subluxated, or dislocated shoulder. Chi-square test was performed to assess the difference in rates of postoperative normal, subluxated, and dislocated in two groups. Pearson Correlation Coefficient (R-value) was calculated to determine the relationship between the duration of the HP implant in situ versus extent (area) of subacromial erosion.
3. Results
A total of 18 patients of HP group and 20 patients from the DB group were included in the study. At the final follow up evaluation at a minimum of one year postoperative of DB group and six months after the plate removal in the HP group, both DB and HP group had 16 patients each. However, only 13 out of 16 patients from the HP group underwent plate removal, while three of them refused to undergo plate removal as they were asymptomatic along with other personal reasons. A total of six patients (four from the DB group and two from the HP group) could not be included in the study due to refusal to participate or change of address. The baseline characteristics of the patients in the two groups are mentioned in Table 1 and were comparable in all the parameters (P > 0.05). 75% of all the cases were due to road traffic accident, and 87.5% cases were Rockwood type V ACJ dislocation.
Table 1.
Baseline characteristics of two groups. RTA, Road traffic accident; SD, standard deviation; CCD, coracoclavicular distance; Preop, preoperative.
| Parameter | Hook plate group (n = 16) | Dog Bone™ Button Fibretape® group (n = 16) | P value |
|---|---|---|---|
| Mean age (in years) ± SD | 44.25±12.82 | 42.1±11.85 | 0.61 |
| Male: Female | 16:0 | 13:3 | 0.42 |
| Side of injury; Right:Left | 8:8 | 5:11 | 0.28 |
| RTA: Fall injury | 13:3 | 11:5 | 0.42 |
| Rockwood Type III: V | 2:14 | 2:14 | 1 |
| Mean Injury to surgery interval (in days) ± SD [range] | 3.82 ± 2.46 [1–8] | 3.93 ± 2.67 [1–10] | 0.37 |
| Preop Mean Index side CCD (in mm) ± SD | 14.93 ± 4.08 | 17.85 ± 3.23 | 0.03 |
| Preop Mean Normal side CCD (in mm) ± SD | 6.03 ± 1.95 | 7.40 ± 2.48 | 0.06 |
| Intra-articular lesion | Not assessed | Two patients: Type II SLAP tear One patient: Partial articular side supraspinatus fraying |
|
| Mean ± SD follow-up (in months) | 55.38 ± 10.9 | 32.88 ± 14.0 | 0.001 |
Clinical outcome: There was no significant difference in final postoperative ASES and CM score between either group (p = 0.02) [Table 2].
Table 2.
Summary of postoperative results. ASES, American Shoulder and Elbow score; CC, Coracoclavicular; SD, CCDL, Final Coracoclavicular distance difference with immediate post-op; Standard deviation∗ means statistically significant.
| Assessment Parameter | Hook plate group (n = 16) | Dog Bone™ Button Fibretape® group (n = 16) | P value | ||||
|---|---|---|---|---|---|---|---|
| CCD immediate post-op [Mean (mm) ± SD] | 5.16 ± 2.24 | 7.35 ± 1.83 | 0.005∗ | ||||
| CCD final follow-up [Mean (mm) ± SD] | 7.02 ± 2.36 (Range: 4.6–10.6) | 10.08 ± 4.08 (Range: 4.6–16.9) | 0.01∗ | ||||
| ASES score (mean ± SD) | 94.73 ± 8.07 | 95.58±4.35 | 0.71 | ||||
| CM score (mean ± SD) | 92.38 ± 6.64 | 94.65 ± 2.38 | 0.62 | ||||
| FCCDD | <3 mm (n = 12) | ≥3 mm (n = 4) | <3 mm (n = 10) | ≥3 mm (n = 6) | 0.86 | 0.23 | |
| ASES score (Mean ± SD) | 94.95 ± 7.87 | 94.15 ± 8.69 | 96.48 ± 4.2 | 93.62 ± 4.4 | |||
| CM score (Mean ± SD) | 94.23 ± 1.31 | 93.65 ± 3.26 | 94.89 ± 5.42 | 92.76 ± 4.56 | 0.75 | 0.65 | |
| Radiological outcome | Normal | 12 | 10 | 0.37 | |||
| Subluxed | 4 | 3 | |||||
| Dislocated | 0 | 3 | |||||
Radiological outcome: In both groups, the postoperative CCD was restored within normal limits (comparable to CCD of the normal side of index case) with no significant difference [P value: 0.225 and 0.914] [Table 1, Table 2]. However, mean reduction in CCD in the HP group was significantly lesser compared to the DB group (P = 0.005) [Table 2]. Furthermore, no case in the DB group had an ‘over-reduction’ of CCD compared to the normal side, whereas five cases of HP group had over the reduction of CCD (mean 4.14 mm; range: 3.0–5.4 mm) in immediate postoperative AP radiograph [Table 3; Fig. 2A & B]. Except in one patient whose CCD remained the same till the final follow up (with plate retained), CCD of the other four became comparable to the index side at the last follow-up with or without HP removal [Table 3].
Table 3.
Summary of five cases with overreduction of CCD (in mm) after hook plate application. CCD, coracoclavicular distance.
| Patient | CCD Normal side (mm) | CCD immediate post-op Index side (mm) | CCD final follow up Index side (mm) | Plate removed |
|---|---|---|---|---|
| AS | 10.4 | 7.4 | 7.4 | No |
| SB | 7.5 | 2.9 | 4.6 | Yes |
| SS | 6.7 | 2.0 | 7 | No |
| PR | 5.1 | 2.1 | 6.5 | No |
| RV | 8.8 | 3.4 | 9.2 | Yes |
Fig. 2.
A, B: Plain AP radiograph (2A) reveals over reduction of right-side AC joint after hook plate fixation while Fig. 2B reveals gradual correction of over reduction along with subacromial osteolysis (yellow arrow).
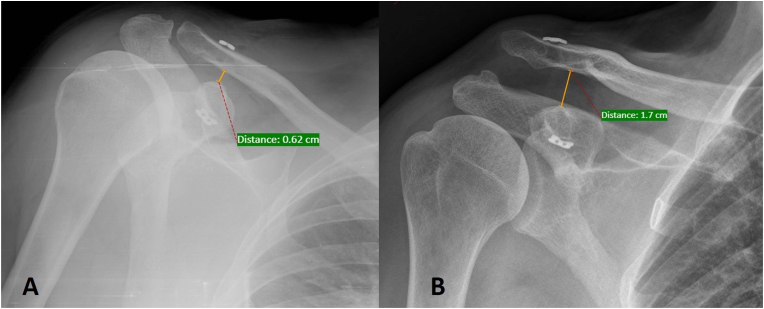
25% (n = 4) patients of HP group had subluxation after plate removal while 37.5% (n = 6) of DB group had subluxation (n = 3) and dislocation (n = 3) [Table 2, Fig. 3A &3B]. Although there were more patients in the DB group with either subluxation or dislocation, the difference was not significant (p = 0.37) [Table 2]. None of the patients with subluxation or dislocation in either group had any specific complaints, and all returned to their previous level of activity. There was no significant difference in clinical scores (ASES and CM) between the patients with normal CCD and loss of reduction (>3 mm) in final CCD compared to immediate post-operative CCD [Table 2].
Fig. 3.
A, B: Plain AP radiograph (3A) reveals accurate reduction of right-side AC joint with DogBone TM Button. Fig. 3B reveals loss of AC joint reduction (re-dislocation) at one year follow up.
Subacromial erosion: Subacromial erosion was evident in 6/13 patients (46.15%) as early as one month postoperative, and it was present in all cases at the time of the plate removal (mean: 8.46 months). The area of subacromial bony erosion varied from 44.52 mm2 to 216 mm2 at the time of HP removal [Fig. 4A & B]. Further, the subacromial erosion resolved in all cases at the final follow up in the HP group except one case wherein it persisted even after 20 months of post-implant removal. There was a weak correlation (r = 0.418) between the duration of the HP in situ and the extent (area) of subacromial erosion.
Fig. 4.
A, B: Plain AP radiograph of left AC joint with hook plate (in situ) reveals subacromial osteolysis (blue circle) at one year postoperative. Fig. 4B reveals huge subacromial osteolytic area after the plate removal.
Impingement: Four cases (25%) in the HP group had clinical signs of impingement, which resolved after implant removal. Three patients who opted to retain the plate did not complain of impingement like symptoms or any other discomfort.
AC joint arthritis, distal clavicle osteolysis: Three patients in the HP group and one in the DB group revealed radiological evidence of ACJ arthritis. However, none had any clinical feature (tenderness over the ACJ or positive cross-chest adduction test) of ACJ arthritis. One patient in the HP group revealed distal clavicle osteolysis.
Other complications: No patient in either group had any ‘clinical’ evidence of rotator cuff injury at the time of final follow up. No implant breakage or fractures of either acromion or clavicle were observed in HP or DB group. One case in the DB group revealed slight medial migration of DB without an increase in coracoclavicular distance and another patient had migration of inferior button (loose) lateral to the coracoid, but not in the joint, without loss of reduction. One patient complaint of irritation by prominent knots of tapes under the skin overlying the clavicle, which subsided in due course of time. Additionally, during arthroscopy in DB group, two cases had type II SLAP tear and one patient had partial articular side supraspinatus fraying. These concomitant lesions were debrided using radiofrequency device.
4. Discussion
The principal finding of our study is that both HP and DB via single coracoclavicular tunnel are acceptable alternatives to manage type III and V ACJ dislocation with similar good to excellent clinical outcomes without any significant unacceptable complications in either group. However, the DB group carries a ‘higher trend’ of loss of reduction than the HP group without affecting the final clinical outcome.
Clinical or functional outcomes: The clinical results in both groups of our study are similar without any significant differences with high ASES and CM scores, indicating overall good to excellent outcome with either method of stabilizing a high-grade unstable AC joint. However, a systematic review of 16 studies confirmed that CM score in HP fixation is lower than suspensory fixation (by 2.13 points), but the difference is not significant.14 Our research, too, revealed that the overall CM score of HP was lower than the DB group by 2.17 points, but the difference was not significant. Many reasons such as altered scapula-clavicular biomechanics, subacromial impingement, and rotator cuff lesion due to hook may contribute to slightly inferior clinical results in the HP group, and which is why many patients report improved pain and CM score after the plate removal.14,16 In the index series, four cases of HP group had clinical symptoms of impingement and pain while HP was in situ, which resolved after the HP removal.
Radiological outcomes: While comparing radiological outcomes, the DB group revealed significantly higher final postoperative CCD as compared to the HP group. Though statistically insignificant, a higher trend of subluxation and dislocation (loss of reduction) was observed in the DB group (37.5%) compared to the HP group (25%). In a recently published systematic review by Gowd et al., the overall pooled failure rate of all devices was 20.8%.17 They also concluded that there was no difference in failure rates of open vs. arthroscopic techniques.17 However, data of loss of reduction in the HP group of our study could be under- or over-estimated as three patients refused HP removal. In our series too, there was no functional difference between the groups with CCD difference less or more than 3 mm (between immediate post-operative and final follow up) implying that loss of reduction might not affect the functional outcome. Even though FibreTape® used in DogBone™ Button construct is theoretically stronger compared to FibreWire® of TightRope®, the FibreTape does not seem to be offering any advantage in terms of superior vertical stability in comparison to FibreWire® loop of original TightRope® system.
Possible reasons behind relatively better vertical stability of ACJ in the HP group of our series could be attributed to several facts. Firstly, HP application in high-grade ACJ dislocation is an open procedure wherein torn DTF, and ACJ capsule18 is often repaired after the HP application, which may further contribute to additional vertical and horizontal stability19 other than the constant mechanical support by HP itself. In contrast, SLS is performed in closed ‘arthroscopic fashion’ wherein no attempt is made to repair torn DTF and ACJ capsule, possibly rendering the suspensory construct’ lesser vertically and horizontally stable’ compared to the HP group. Pastor et al. emphasized the synergistic role of DTF in the stability of ACJ.19 Hence, no repair of either structure (ACJ capsule and DTF) in arthroscopically performed SLS might result in increased stress over the suspensory fixation during cyclical loading causing gradual loss of reduction. Secondly, button movement, knot slippage, and suture breakage might also contribute to the higher loss of reduction in SLS (DB) group. Thirdly, some reports suggest that a single coracoclavicular tunnel is not enough to restore the biomechanical stability provided by conoid and trapezoid ligaments. It may require having dual coracoclavicular (CC) tunnels to mimic the biomechanics of CC ligaments20,21 and separate stabilization of AC joint to restore stability in both vertical and horizontal plane of the entire construct to minimize loss of reduction.22,23 However, pooled data comparing clinical outcomes and loss of reduction between single vs. dual CC tunnel finds no significant difference between the two groups.14
Five patients of the HP group had over-reduction of ACJ in an immediate postoperative AP radiograph, which has also been reported by other authors.1,24 It possibly happened as a standard 15 mm hook was used in all patients, which might be too tight for few individuals causing hook size-acromion mismatch. However, in due course of time, the over reduction normalized in four patients due to subacromial erosion resulting in gradual superior migration of the HP (Table 3).
Subacromial osteolysis: Although several studies reported varying degrees of subacromial osteolysis4,24,25 our study is perhaps first series to report subacromial erosion in all the cases of HP fixation. One argument for this outcome could be longer than usual (>3 months) retention of the plate as our patients underwent delayed implant removal between 6 and 12 months (mean: 8.46 months). According to one of the manufacturer's guidelines (Synthes, USA), it is recommended to remove the implant ‘three months after implantation to prevent potential irritation of the acromion or impingement on the rotator cuff.’ Although most authors advocate HP removal as soon as ligamentous healing is completed, there is no consensus regarding the ‘exact’ timing of this implant removal. A recent recommendation, based on the patient's symptoms, is to consider hardware removal before three months, only if there is persistent pain after the surgery.14 If there are mere functional limitations and no pain, the plate must be retained for a minimum of three months as early implant removal poses an inherent risk of loss of reduction or re-displacement. In a series of 61 patients with Neer's type II lateral third clavicle fracture fixed by HP, Zhang et al. observed that the timing of implant removal was crucial in terms of functional outcomes and complications (impingement, subacromial osteolysis). They noted that the Constant scores were better with early removal, and complications rates were 10%, 22.9%, and 50% in the early (<3 months), delayed removal (3–6 months), and retained plate groups, respectively.4 Although Zhang et al. stated that subacromial osteolysis would occur if the plate is retained for a longer time,4 68.75% of patients in our series of HP group showed radiological evidence of subacromial erosion seen as early as one month after the implantation. Contrary to our findings, a few case series noted lesser subacromial osteolysis (4–8.3%) if HP was retained for more than six months.25,26 Regardless of the presence and size of subacromial erosion, it does not appear to be a factor affecting the clinical outcome in our series.
Many technical factors seem to affect the development of subacromial erosion, and one such factor is the size of the hook. If the Hook selected is too short, it leads to over reduction of the clavicle and results in excessive pressure at the undersurface of the acromion. By trial-and-error method or using sizing templates supplied by the manufacturer, the most appropriate hook size (12,15 and 18 mm) is selected to ensure a proper reduction of the clavicle. It has also been suggested that to adapt the plate to the patient's anatomy; it may be necessary to bend the plate or Hook as various hook angles cast different pressure on the undersurface of acromion.4 However, intra-operatively, it is difficult to effectively determine the degree of the plate or hook bending required to match the given acromial morphology and its impact on the contact pressure exerted under the acromion. It has been observed that the gender differences in the thickness of acromion, anatomical variations of the distal clavicle, distal clavicle–acromion angle, and distal clavicle–coronal angle results in an imperfect fit between HP and the bone and promote the occurrence of subacromial erosion.27,28 To overcome this limitation, Wu et al. recommend pre-operative 3D templating to decide the appropriate countering of the implant.29 Furthermore, the contact pressure would dynamically vary with the position of the shoulder joint in the postoperative phase.
Limitations to the study: First is the retrospective nature of the study design with 84% follow up rate. There is a risk of selection and recall bias in a retrospective design along with random lack of desirable data. However, in the literature, most of the published papers are retrospective case series, which have enabled reliable insight into the nature of these injuries and the outcomes expected from diverse interventions. The second limitation is the small sample size. A larger sample size in each category and longer follow-up (particularly to observe for the development of further loss of reduction and arthritic changes in the ACJ) would be more meaningful in analysing the functional and radiological outcomes of two popular methods of ACJ fixation. Third, we did look at injury involving dominant or non-dominant side. This could have influenced the overall clinical outcome scores. Lastly, the residual horizontal instability was assessed by performing only the axillary view. Postoperative cross chest adduction or Alexander view was not performed in any of the case and thus compromising our ability to analyse the residual instability in the horizontal plane.
5. Conclusions
Our study suggests that both fixation modalities result in comparable and satisfactory functional and radiological outcomes. However, it is not possible to conclude the superiority of one method over the other as both the implants have specific types of complications that still needs to be taken into consideration while planning the surgery.
Funding
None.
Ethical approval
Institutional Ethical Committee approval obtained (IEC:407/2020).
Informed consent
Obtained.
Authors’ contribution
SaM: Design of work, Drafting Manuscript, Data collection, Revision, final approval.
VP: Design of work, Drafting Manuscript, Data analysis, Revision, final approval.
SuM: Design of work, Drafting Manuscript, Data collection, final approval.
KA: Design of work, Drafting Manuscript, Data analysis, final approval.
All authors read and approved the final manuscript.
Declaration of competing interest
None.
Acknowledgements
None.
Contributor Information
Sandesh Madi, Email: sandesh.madi@gmail.com.
Vivek Pandey, Email: vivekortho@gmail.com.
Sujayendra Murali, Email: sujayendra16@gmail.com.
Kiran Acharya, Email: kirankatte@gmail.com.
References
- 1.Hemmann P., Koch M., Gühring M., Bahrs C., Ziegler P. Acromioclavicular joint separation treated with clavicular hook plate: a study of radiological and functional outcomes. Arch Orthop Trauma Surg. 2021;141(4):603–610. doi: 10.1007/s00402-020-03521-4. [DOI] [PubMed] [Google Scholar]
- 2.Steinbacher G., Sallent A., Seijas R., Boffa J.M., Espinosa W., Cugat R. Clavicular hook plate for grade-III acromioclavicular dislocation. J Orthop Surg. 2014;22(3):329–332. doi: 10.1177/230949901402200312. [DOI] [PubMed] [Google Scholar]
- 3.Chiang C.L., Yang S.W., Tsai M.Y., Kuen-Huang Chen C. Acromion osteolysis and fracture after hook plate fixation for acromioclavicular joint dislocation: a case report. J Shoulder Elbow Surg. 2010;19(4):e13–e15. doi: 10.1016/j.jse.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Zhang L., Xiao H., Gao Y., Zhang H., Zhang L., Tang P. Late function and complications of hook plate implantation for distal-third clavicle fractures : a retrospective study. Acta Orthop Belg. 2018;84(4):485–490. [PubMed] [Google Scholar]
- 5.Lin H.Y., Wong P.K., Ho W.P., Chuang T.Y., Liao Y.S., Wong C.C. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion - dynamic sonographic evaluation. J Orthop Surg Res. 2014;9(1):6. doi: 10.1186/1749-799X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modi C.S., Beazley J., Zywiel M.G., Lawrence T.M., Veillette C.J.H. Controversies relating to the management of acromioclavicular joint dislocations. Bone Joint Lett J. 2013;95-B(12):1595–1602. doi: 10.1302/0301-620X.95B12.31802. [DOI] [PubMed] [Google Scholar]
- 7.Lee P.Y., Brock J. A radiological and clinical evaluation of acromioclavicular joint reconstruction using dog bone double endobutton technique. J Arthritis. 2016;5(4) doi: 10.4172/2167-7921.1000207. [DOI] [Google Scholar]
- 8.Walz L., Salzmann G.M., Fabbro T., Eichhorn S., Imhoff A.B. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices. Am J Sports Med. 2008;36(12):2398–2406. doi: 10.1177/0363546508322524. [DOI] [PubMed] [Google Scholar]
- 9.Clavert P., Meyer A., Boyer P., Gastaud O., Barth J., Duparc F. Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation. Prospective multicenter study of 116 cases. Orthop Traumatol Surg Res. 2015;101(8):S313–S316. doi: 10.1016/j.otsr.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 10.Olivos-Meza A., Almazán-Diaz A., Calvo J.A., et al. Radiographic displacement of acute acromioclavicular joint dislocations fixed with AC TightRope. JSES Int. 2020;4(1):49–54. doi: 10.1016/j.jseint.2019.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shin S.J., Kim N.K. Complications after arthroscopic coracoclavicular reconstruction using a single adjustable–loop-length suspensory fixation device in acute acromioclavicular joint dislocation. Arthroscopy. 2015;31(5):816–824. doi: 10.1016/j.arthro.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 12.Vulliet P., le Hanneur M., Cladiere V., Loriaut P., Boyer P. A comparison between two double-button endoscopically assisted surgical techniques for the treatment acute acromioclavicular dislocations. Musculoskelet Surg. 2017 doi: 10.1007/s12306-017-0501-0. Published online August 31. [DOI] [PubMed] [Google Scholar]
- 13.Ryazantsev M.S., Il’in D.O., Rybin K.E., et al. Stabilization of acromioclavicular joint using DogBone dynamic system (Arthrex): a literature review and long-term follow-up. Genij Ortopedii. 2018;24(4):530–537. doi: 10.18019/1028-4427-2018-24-4-530-537. [DOI] [Google Scholar]
- 14.Arirachakaran A., Boonard M., Piyapittayanun P., et al. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: a systematic review and meta-analysis. J Orthop Traumatol. 2017;18(4):293–304. doi: 10.1007/s10195-017-0451-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Çarkçı E., Polat A.E., Gürpınar T. The frequency of reduction loss after arthroscopic fixation of acute acromioclavicular dislocations using a double-button device, and its effect on clinical and radiological results. J Orthop Surg Res. 2020;15(1):136. doi: 10.1186/s13018-020-01674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Athar M., Ashwood N., Arealis G., Hamlet M., Salt E. Acromioclavicular joint disruptions: a comparison of two surgical approaches ‘hook’ and ‘rope. J Orthop Surg. 2018;26(1) doi: 10.1177/2309499017749984. 230949901774998. [DOI] [PubMed] [Google Scholar]
- 17.Gowd A.K., Liu J.N., Cabarcas B.C., et al. Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med. 2019;47(11):2745–2758. doi: 10.1177/0363546518795147. [DOI] [PubMed] [Google Scholar]
- 18.Rockwood C., Young D. In: The Shoulder. third ed. Rockwood C., Matsen F., editors. WB Saunders; 1990. Disorders of the acromioclavicular joint; pp. 413–476. [Google Scholar]
- 19.Pastor M.F., Averbeck A.K., Welke B., Smith T., Claassen L., Wellmann M. The biomechanical influence of the deltotrapezoid fascia on horizontal and vertical acromioclavicular joint stability. Arch Orthop Trauma Surg. 2016;136(4):513–519. doi: 10.1007/s00402-015-2389-1. [DOI] [PubMed] [Google Scholar]
- 20.Patzer T., Clauss C., Kühne C.A., et al. Arthroscopically assisted reduction of acute acromioclavicular joint separations: comparison of clinical and radiological results of single versus double TightRopeTM technique. Unfallchirurg. 2013;116(5):442–450. doi: 10.1007/s00113-011-2135-2. [DOI] [PubMed] [Google Scholar]
- 21.Venjakob A.J., Salzmann G.M., Gabel F., et al. Arthroscopically assisted 2-bundle anatomic reduction of acute acromioclavicular joint separations. Am J Sports Med. 2013;41(3):615–621. doi: 10.1177/0363546512473438. [DOI] [PubMed] [Google Scholar]
- 22.Saier T., Venjakob A.J., Minzlaff P., et al. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1498–1505. doi: 10.1007/s00167-014-2895-7. [DOI] [PubMed] [Google Scholar]
- 23.Dyrna F., Imhoff F.B., Haller B., et al. Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med. 2018;46(14):3471–3479. doi: 10.1177/0363546518807908. [DOI] [PubMed] [Google Scholar]
- 24.Eschler A., Gradl G., Gierer P., Mittlmeier T., Beck M. Hook plate fixation for acromioclavicular joint separations restores coracoclavicular distance more accurately than PDS augmentation, however presents with a high rate of acromial osteolysis. Arch Orthop Trauma Surg. 2012;132(1):33–39. doi: 10.1007/s00402-011-1399-x. [DOI] [PubMed] [Google Scholar]
- 25.Jafary D., Keihan Shokouh H., Najd Mazhar F., Shariat Zadeh H., Mochtary T. Clinical and radiological results of fixation of acromioclavicular joint dislocation by hook plates retained for more than five months. Trauma Mon. 2014;19(2) doi: 10.5812/traumamon.13728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campbell N., Hujazi I., Viner J., Marynissen H. Delayed removal of clavicular hook plates; the effect on complications and functional outcome. Int J Orthod. 2018;5(5):968–971. doi: 10.17554/j.issn.2311-5106.2018.05.287. [DOI] [Google Scholar]
- 27.Yoon J.P., Lee Y.S., Song G.S., Oh J.H. Morphological analysis of acromion and hook plate for the fixation of acromioclavicular joint dislocation. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):980–986. doi: 10.1007/s00167-016-3987-3. [DOI] [PubMed] [Google Scholar]
- 28.Shen P Cheng, Zhu Y., Zhang H., et al. Three-dimensional morphological analysis of acromioclavicular joint in patients with and without subacromial erosion after hook plate fixation. J Int Med Res. 2018;46(1):511–521. doi: 10.1177/0300060517725973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu X., Wang G., Xia Q., et al. Digital technology combined with 3D printing to evaluate the matching performance of AO clavicular hook plates. Indian J Orthop. 2020;54(2):141–147. doi: 10.1007/s43465-019-00034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]