Key Points
Question
Is the risk of posttraumatic stress disorder (PTSD) symptoms in family members of intensive care unit (ICU) patients with acute respiratory distress syndrome (ARDS) due to COVID-19 different from that of family members of patients with non–COVID-19 ARDS?
Findings
In a prospective cohort study of 517 family members of ICU patients, PTSD-related symptoms at 90 days after ICU discharge were significantly more common in family members of patients with COVID-19 ARDS compared with non–COVID-19 ARDS (35% vs 19%). In a multivariable analysis adjusting for age, sex, and level of social support, COVID-19 ARDS was independently associated with PTSD-related symptoms in family members (odds ratio, 2.05).
Meaning
ARDS due to COVID-19 was associated with a greater risk-adjusted rate of PTSD symptoms among family members compared with ARDS from other causes.
Abstract
Importance
Persistent physical and mental disorders are frequent in survivors of COVID-19–related acute respiratory distress syndrome (ARDS). However, data on these disorders among family members are scarce.
Objective
To determine the association between patient hospitalization for COVID-19 ARDS vs ARDS from other causes and the risk of posttraumatic stress disorder (PTSD)–related symptoms in family members.
Design, Setting, and Participants
Prospective cohort study in 23 intensive care units (ICUs) in France (January 2020 to June 2020 with final follow-up ending in October 2020). ARDS survivors and family members (1 family member per patient) were enrolled.
Exposures
Family members of patients hospitalized for ARDS due to COVID-19 vs ARDS due to other causes.
Main Outcomes and Measures
The primary outcome was family member symptoms of PTSD at 90 days after ICU discharge, measured by the Impact of Events Scale-Revised (score range, 0 [best] to 88 [worst]; presence of PTSD symptoms defined by score >22). Secondary outcomes were family member symptoms of anxiety and depression at 90 days assessed by the Hospital Anxiety and Depression Scale (score range, 0 [best] to 42 [worst]; presence of anxiety or depression symptoms defined by subscale scores ≥7). Multivariable logistic regression models were used to determine the association between COVID-19 status and outcomes.
Results
Among 602 family members and 307 patients prospectively enrolled, 517 (86%) family members (median [IQR] age, 51 [40-63] years; 72% women; 48% spouses; 26% bereaved because of the study patient’s death; 303 [50%] family members of COVID-19 patients) and 273 (89%) patients (median [IQR] age, 61 [50-69] years; 34% women; 181 [59%] with COVID-19) completed the day-90 assessment. Compared with non–COVID-19 ARDS, family members of patients with COVID-19 ARDS had a significantly higher prevalence of symptoms of PTSD (35% [103/293] vs 19% [40/211]; difference, 16% [95% CI, 8%-24%]; P < .001), symptoms of anxiety (41% [121/294] vs 34% [70/207]; difference, 8% [95% CI, 0%-16%]; P= .05), and symptoms of depression (31% [91/291] vs 18% [37/209]; difference, 13% [95% CI, 6%-21%]; P< .001). In multivariable models adjusting for age, sex, and level of social support, COVID-19 ARDS was significantly associated with increased risk of PTSD-related symptoms in family members (odds ratio, 2.05 [95% CI, 1.30 to 3.23]).
Conclusions and Relevance
Among family members of patients hospitalized in the ICU with ARDS, COVID-19 disease, as compared with other causes of ARDS, was significantly associated with increased risk of symptoms of PTSD at 90 days after ICU discharge.
Trial Registration
ClinicalTrials.gov Identifier: NCT04341519
This prospective cohort study compares the risk of posttraumatic stress disorder among family members of patients with COVID-19-related acute respiratory distress syndrome (ARDS) vs ARDS from other causes.
Introduction
Among hospitalized patients with COVID-19, 1 in 5 require intensive care, often leading to physical, cognitive, and psychiatric symptoms among survivors.1,2,3 Family members of patients with acute respiratory distress syndrome (ARDS) also experience an increased psychological burden,4,5 including posttraumatic stress disorder (PTSD), anxiety, and depression. Yet, little is known about the specific experience of COVID-19 on family members’ mental health.6,7
There are multiple mechanisms by which the intensive care experience during the pandemic could exacerbate the psychological outcomes of family members of patients with COVID-19. First, restricted or forbidden family visitation may have created new disruptions in the lives of patients and family members. Second, when visitation is possible, personal protective equipment may create barriers to effective communication between family members and their loved ones. Third, family members may experience fewer contacts with physicians, potentially affecting communication and trust. Fourth, survivors of COVID-19 intensive care may have a substantial care burden on families, compounded by pandemic-related societal factors such as financial insecurity, social distancing, or risk of job loss.5,8
To address this knowledge gap, a prospective multicenter study was conducted in 23 intensive care units (ICUs) in France to determine the risk-adjusted association between hospitalization with COVID-19 ARDS and symptoms of PTSD in family members compared with hospitalization for ARDS of other causes.
Methods
Participants
This study was conducted in 23 ICUs in France between January 2020 and October 2020. All of the ICUs are members of the FAMIREA study group—a multidisciplinary research network focused on understanding and improving the experience of family members of ICU patients.9 Each participating ICU included 1 family member per adult patient admitted between January 2020 and June 2020 for ARDS requiring noninvasive ventilation, high-flow nasal oxygen, or endotracheal mechanical ventilation. All patients had a history of acute hypoxemic respiratory failure within 1 week of a known illness onset (ie, COVID-19, community-acquired pneumonia, or influenza), with a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen (Pao2/Fio2) of less than 300 and bilateral opacities on chest radiograph not fully explained by cardiac failure or fluid overload. The family member included for each patient was the adult family member most involved in the patient’s ICU stay. Family members of patients who died in the ICU were also invited to participate. When competent, patients were also included. The CPP Sud Méditerranée ethics committee approved this study in March 2020 (#2020-A00809-30; CNRIPH: 20.03.27.73019). Oral informed consent was obtained from all family members and patients.
Study Procedures
Prior to the COVID-19 pandemic, the participating ICUs generally had a policy of unrestricted family visits, a routine family conference in a dedicated room soon after patient admission, and a routine end-of-life family conference for patients expected to die. Due to concern about SARS-CoV-2 transmission and staff shortages due to patient surge, these measures were altered based on institutional request to prohibit any family visit to the ICU unless the patient was dying.
Eligible family members and patients were contacted by post and telephone by 2 psychologists to obtain consent to participate in a telephone interview aimed at assessing their physical, mental, and emotional well-being and the potential burden generated by the ICU experience. Contact with participants occurred at least 1 month after ICU discharge. During this discussion and when respondents provided consent, a date was fixed for the research call, calculated at 90 (±) days after ICU discharge. Patients and family members who did not answer the first research call at day 90 were called again on different days and at different times. After 10 unsuccessful attempts, the person was considered lost to follow-up.
All interviews were conducted by 2 trained clinical psychologists supervised by a research nurse with extensive interviewing experience. During the telephone interviews, the patients and family members completed the Impact of Event Scale Revised (IES-R) to assess PTSD-related symptoms,10 the Hospital Anxiety and Depression Scale (HADS),11 and a questionnaire describing their experience during the patient’s ICU hospitalization. The patients completed the IES-R and the HADS, as well as the 36-Item Short Form Health Survey (SF-36) to assess health-related quality of life.12 The IES-R is not a tool for diagnosing PTSD but instead detects symptoms indicating a risk of PTSD (score range, 0-88 [>22 indicates the presence of PTSD-related symptoms that are of clinical concern]; minimal clinically important difference, 0.2). The HADS has a 7-item subscale for anxiety and a separate one for depression, with a score of 7 or greater on a 21-point scale indicating symptoms of anxiety or depression.13 The SF-36 is a well-documented tool12 that produces a Physical Component Summary (PCS) and Mental Component Summary (MCS) (score range, 0-100 with higher scores indicating better quality of life).
Each family member’s characteristics and their experience in the ICU were also collected during the day 90 telephone interview, including their perception of the quality of the information provided and symptoms control and their feelings of loneliness, distress, and about how much they could contribute to the patient’s well-being and comfort. In addition, visual analog scales (range, 0-10) were used to assess the intensity of unidimensional measures such as quality of the information provided, clinicians’ behaviors, symptom control, feelings of loneliness or distress, and contribution to patient’s well-being.
The patients were divided into 2 groups depending on whether the cause of ARDS was COVID-19–related or not (eFigure 1 and eFigure 2 in the Supplement). All the patients with COVID-19 ARDS had a positive reverse transcriptase-polymerase chain reaction for SARS-CoV-2 from upper or lower respiratory tract samples. Patients’ characteristics were obtained from the medical files and entered into an electronic case-report form.
Outcomes
The primary study population was the family members. The primary outcome was the prevalence of PTSD-related symptoms among family members assessed by the IES-R.
The 2 secondary outcomes in family members were the prevalence of symptoms of anxiety and depression measured using the HADS symptom score (HADS; score range, 0 [best] to 42 [worst]; minimal clinically important difference, 1.5). The presence of symptoms of anxiety and depression were defined by a HADS anxiety subscale of 7 or greater and/or a HADS depression subscale of 7 or greater.
In ARDS survivors, symptoms of PTSD, anxiety, and depression were also assessed. Quality of life was assessed using norm-based measurements of the SF-36 (mean [SD], 50 [10]), after standardization using reference values for the French population subscores. Physical and mental SF-36 aggregate components (ie, PCS and MCS) were computed as recommended14 and expressed on a normalized scale centered on 50 (representing the French population norm). Missing data in the individual SF-36 questions were imputed using the personal mean score approach.15
Statistical Analysis
Continuous variables are summarized as medians and IQRs and categorical variables as counts and percentages. Differences between COVID-19 and non–COVID-19 groups were assessed with the use of the Wilcoxon rank sum test for quantitative variables and the Fisher exact test for qualitative variables. The IES-R (cutoff 22),16 anxiety subscale of the HADS (cutoff 7), and depression subscale of the HADS (cutoff 7) were dichotomized at specific thresholds for the presence of symptoms of PTSD, anxiety, and depression.11 Correlations between PTSD, anxiety, and depression scores in the patients and family members were assessed using Pearson correlation coefficients with 95% CIs.
To determine the association between COVID-19 status and outcomes, multivariable logistic regression models were used along with a LASSO penalty.17 Variables included as confounders were as follows: (1) those known to be associated with the family experience; (2) those associated with an outcome with a P value less than .10; and (3) those with less than 20% missing data. For each outcome, the model selection involved the following steps: (1) 10-fold cross-validation to determine the λ value of the LASSO; (2) selection of the λ giving the most regularized model such that the cross-validated error is within 1 standard error of the minimum; and (3) application of the LASSO logistic regression model to obtain a set of variables associated with each outcome. COVID-19 status and all variables with a non-null coefficient in the latter model were included in the final model and calibration was measured using Hosmer-Lemeshow goodness-of-fit test.18 Coefficients and odds ratios (ORs) with their 95% CIs are presented.
Several sensitivity analyses were performed. First, a random-effects model was used to account for site. Second, to account for missing data,19 multiple imputation with chained equations was used to create 20 imputed data sets. Imputation models included all a priori potential confounders and the 3 outcomes of interest, and final model estimates were combined using Rubin rules.20 Third, a different IES-R cutoff (IES-R score >26) was used.
Statistical tests were not adjusted for multiple comparisons. Because of the potential for type I error due to multiple comparisons, the findings for analyses of secondary end points should be interpreted as exploratory. All reported P values are 2-sided; a P value of less than .05 was considered statistically significant. All analyses were performed using R version 4.0.4 (http://www.R-project.org/).
Results
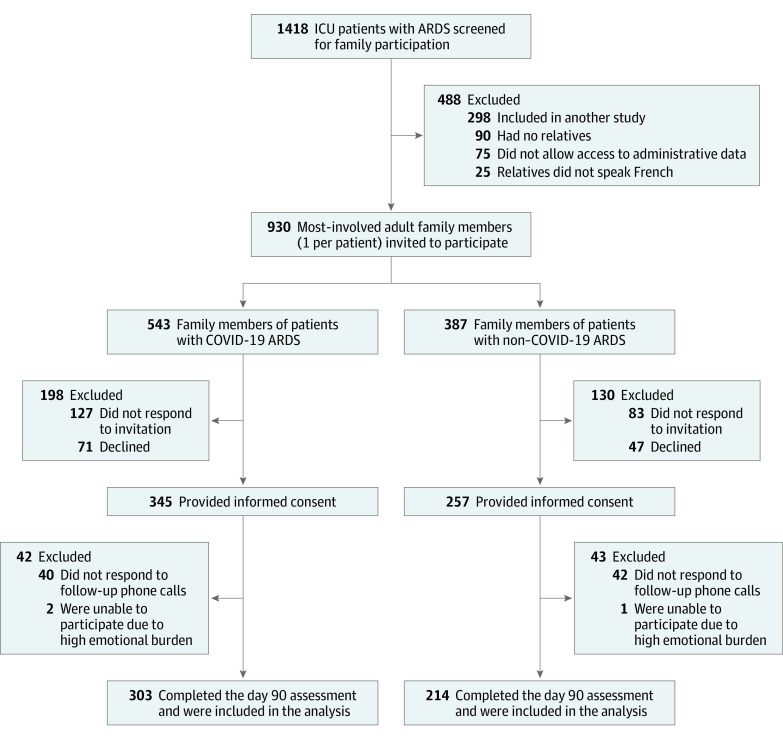
Among the 1418 patients with ARDS at 23 participating ICUs (eTable 1 in the Supplement), 930 patients and family members were screened for eligibility. Among them, 307 patients (33%) and 602 family members (65%) provided informed consent for study participation. The primary reasons for noninclusion were lack of family response to the invitation or follow-up phone call to participate in the study (n = 292 [31%]) and family declining study participation (n = 118 [13%]). Among ARDS survivors, 23% declined study participation (Figure 1; eFigure 2 in the Supplement).
Figure 1. Screening and Selection of Family Member Cohorts for the Study.
ARDS indicates acute respiratory distress syndrome; ICU, intensive care unit.
Family Members and Prevalence of Symptoms of PTSD, Anxiety, and Depression
Among the 602 participating family members, 517 (86%) completed the telephone interview (n = 303 in the COVID-19 group and n = 214 in the non–COVID-19 group) (Figure 1). Telephone assessments occurred at a median 112 days after ICU discharge (IQR, 90-147 days). On average, family members in the COVID-19 group were younger (median age, 50 vs 55 years), reportedly were less frequently allowed to visit the ICU (35% vs 88%), and more commonly received patient information by telephone call (84% vs 20%) compared with family members of non–COVID-19 ARDS patients (Table 1). Family members in the COVID-19 group self-rated (visual analog scale score range, 1 [no symptoms] to 10 [most intense symptoms]) more intense feelings of loneliness during the ICU stay (6 [1-10] vs 1 [1-6]) and distress (10 [8-10] vs 7 [5-10]) compared with family members of the non–COVID-19 group.
Table 1. Family Member and Intensive Care Unit Stay Characteristics in a Study Evaluating Posttraumatic Stress in Family Members of Critically Ill Hospitalized Patients With ARDSa.
| Demographics | COVID-19, No. (%)b | |
|---|---|---|
| Yes (n =303)c | No (n = 214)c | |
| Women | 224/300 (75) | 144/213 (68) |
| Men | 76/300 (25) | 69/213 (32) |
| Age, median (IQR) [No.], y | 50 (39-61) [294] | 55 (43-66) [204] |
| Spouses of ICU patients | 149/300 (50) | 99/210 (47) |
| Unemployed | 18/299 (6) | 28 (13) |
| Medication history, daily intaked | ||
| Medication | 90/299 (30) | 92/213 (43) |
| Anxiolytics | 28/298 (9) | 22/211 (10) |
| Characteristics of ICU stay | ||
| Date of ICU admission, median (IQR) | April 13, 2020 (February 11-March 24) | March 3, 2020 (January 30-April 4) |
| Were allowed to be present during ICU admission | 104/298 (35) | 176/199 (88) |
| Could visit patient in the ICU | 106/299 (35) | 190 (89) |
| Tools used to remotely interact with the patient | ||
| Telephone | 106/300 (35) | 85/203 (42) |
| Videoconferencing | 27/300 (9) | 2/203 (1) |
| Othere | 15/300 (5) | 6/203 (3) |
| None | 152/300 (51) | 110/203 (54) |
| Physicians and nurses wore personal protective equipmentf | 230/300 (77) | 115/213 (54) |
| Information was providedg | ||
| By incoming phone call | 254/300 (84) | 47/203 (20) |
| Family members called the ICU nurse | 154/300 (51) | 94/203 (46) |
| Family members called the ICU physician | 117/300 (39) | 48/203 (20) |
| During visits in the ICU | 61/300 (20) | 176/203 (87) |
| Family members’ assessments (self-ratings) at day 90, median (IQR) [No.]h | ||
| Felt shunned by ICU physicians and nurses | 1 (1-2) [205] | 1 (1-1) [152] |
| Quality of the information provided during the whole ICU stay | 8 (6-9) [299] | 8 (7-10) [210] |
| Social support during the ICU stay | 10 (8-10) [299] | 9 (8-10) [n = 214] |
| Clinician’s ability to deliver family-centered care during the ICU stay | 9 (7-10) [297] | 9 (8-10) [210] |
| Symptom control in patients during the ICU stay | 9 (8-10) [241] | 10 (9-10) [205] |
| Felt loneliness during the ICU stay | 6 (1-10) [299] | 1 (1-6) [212] |
| Felt distress during the ICU stay | 10 (8-10) [299] | 7 (5-10) [212] |
| Family member’s contribution to patient’s well-being and comfort during the ICU stay | 7 (2-9) [205] | 9 (7-10) [153] |
Abbreviations: ARDS, acute respiratory distress syndrome; ICU, intensive care unit.
Patients’ characteristics are shown in eTable 3, and ICU characteristics are shown in eTable 1 in the Supplement.
Values are reported as No. (%) unless otherwise indicated.
For each patient, 1 family member was included.
Indicates daily medication and anxiolytic intake at time of interview based on family member self-report. Any medication was included in daily medication. Anxiolytics were assessed by category (eg, “Do you take any medications for anxiety or nervousness?”).
Indicates various social media tools and apps.
Participating ICUs generally required personal protective equipment consisting of a bodysuit, gloves, safety glasses, hat, and masks; however, details for each situation were not available, and there may have been some differences based on site or patient.
Information could be provided by more than 1 method, and therefore, totals sum to more than 100%.
Visual analog scales were used by family members to assess the intensity of unidimensional measures (score range, 0 [no symptom/lowest rating] to 10 [the most intense symptom/highest rating]).
Among the 517 family members who completed interviews after ICU discharge, 143 (28%) exhibited symptoms of PTSD (Table 2; Figure 2). PTSD symptoms were significantly more common in family members of patients with COVID-19 than in those with non–COVID-19 ARDS (35% [103/293] vs 19% [40/211]; difference, 16% [95% CI, 8% to 24%]; P < .001). For anxiety, the occurrence of symptoms was significantly higher in the COVID-19 vs the non–COVID-19 group (41% [121/294] vs 34% [70/207]; difference, 8% [95% CI, 0% to 16%]; P = .05), and the occurrence of symptoms for depression were also higher in the COVID-19 group (31% [91/291] vs 18% [37/209]; difference, 13% [95% CI, 6% to 21%]; P < .001) (Table 2).
Table 2. 90-Day Outcomes in 517 Family Members of Patients With Respiratory Distress Hospitalized in the Intensive Care Unita.
| ARDS, No. (%) | Difference, mean or proportion (95% CI) | P value | ||
|---|---|---|---|---|
| COVID-19–associated | Non–COVID-19–associated | |||
| Family members, No. | 303 | 214 | ||
| Primary end point | ||||
| IES-R score, median (IQR)b | 15 [5-29] | 9 [3-19] | 6.4 (3.7-9.1) | <.001 |
| Family members with PTSD-related symptoms, No./total (%)b | 103/293 (35) | 40/211 (19) | 16% (8.0-24.0) | <.001 |
| Secondary end points | ||||
| HADS anxiety subscale score, median (IQR) | 5 [3-9] | 5 [2-8] | 0.9 (0.1-1.7) | .08 |
| Family members with symptoms of anxiety, No./total (%)c | 121/294 (41) | 70/207 (34) | 8% (0-16) | .05 |
| HADS depression subscale score, median (IQR) | 3 [1-8] | 2 [1-5] | 1.4 (0.6-2.2) | .02 |
| Family members with symptoms of depression, No./total (%)c | 91/291 (31) | 37/209 (18) | 13% (6-21) | <.001 |
Abbreviations: ARDS, acute respiratory distress syndrome; HADS, Hospital Anxiety and Depression Scale; IES-R, Impact of Event Scale Revised; PTSD, posttraumatic stress disorder.
A sensitivity analysis of the differences between family members of COVID-19 and non–COVID-19 groups that analyzed a set of data after imputation of missing variables is reported in eTable 7 in the Supplement.
The primary end point was the presence of PTSD-related symptoms as indicated by the proportion of family members with an IES-R score greater than 22. The IES-R assesses the subjective distress of a traumatic event using 22 self-reported items rated from 0 (not at all) to 4 (extremely), yielding a total score range of 0 to 88, with higher scores indicating greater distress.
Symptoms of anxiety and depression were measured using the HADS symptom score which uses 14 self-reported items (7 for depression and 7 for anxiety) to produce a total score ranging from 0 to 42 with the subscales for depression and anxiety ranging from 0 (least) to 21 (most). Anxiety or depression were each considered present at a score of 7 or greater on the respective subscale.
Figure 2. Symptoms of Posttraumatic Stress Disorder, Anxiety, and Depression in Family Members of Patients With COVID-19 ARDS vs Non–COVID-19 ARDS.
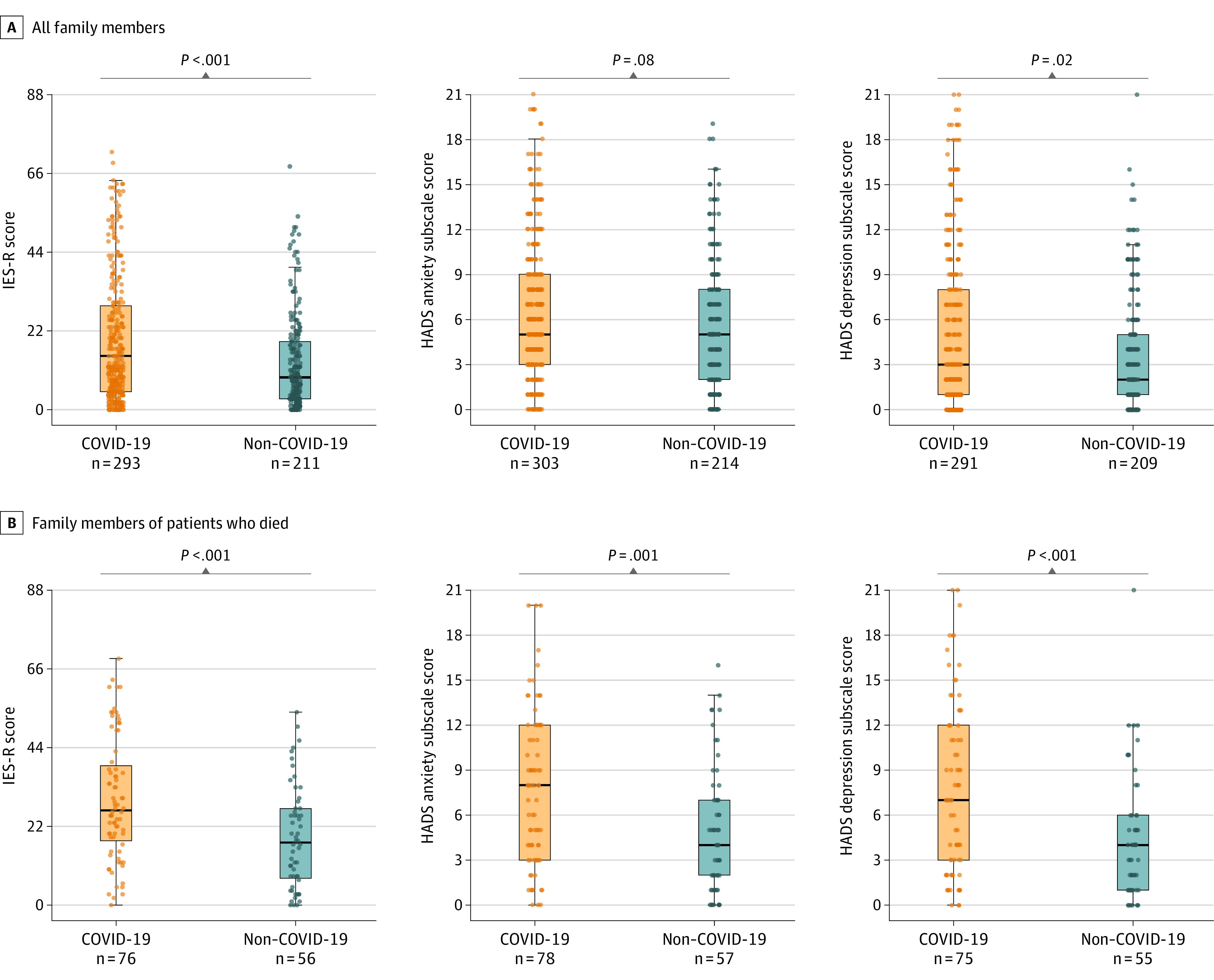
Posttraumatic stress disorder (PTSD) symptoms were measured using the Impact of Event Scale Revised (IES-R; score range, 0 [best] to 88 [worst]; minimal clinically important difference, 0.2; sample sizes, n = 271 for the COVID-19 group and 198 for the non–COVID-19 group). Symptoms of anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS) anxiety and depression subscales (score range for each, 0 [best] to 42 [worst]; minimal clinically important difference, 1.5; anxiety or depression considered present with a score of ≥7 [sample sizes for anxiety, n = 294 for the COVID-19 group and n = 207 for the non–COVID-19 group; sample sizes for depression, n = 291 for the COVID-19 group and n = 209 for the non–COVID-19 group]). Data are reported as median (solid horizontal lines) IQR (vertical height of boxes) scores, and the whiskers extend to the most extreme data point, which is no more than 1.5 times the IQR.
Among family members, 26% (135/517) of their relatives in this study died before the day-90 assessment (eTable 2 in the Supplement), and proportions were similar for patients with and without COVID-19 (difference, −1% [95% CI, −8% to 7%]; P = .92). The prevalence of symptoms of PTSD was significantly higher among the bereaved family members of patients who died from COVID-19 compared with non–COVID-19 ARDS (63% vs 39%; difference, 24% [95% CI, 7% to 40%]; P = .008) (Figure 2 and eTable 2 in the Supplement). In the COVID-19 group, significantly fewer family members reported having attended the funeral (77% vs 91%; difference, −14% [95% CI, −26% to −1%]; P = .04), and more family members reported that the funeral did not occur as they expected (57% vs 4%; difference, 53% [95% CI, 41% to 65%]; P < .001). Among bereaved family members, symptoms were also more common in family members of the COVID-19-group than in the non–COVID-19 group for anxiety (55% vs 32%; difference, 23% [95% CI, 7% to 39%]; P = .009) and for depression (55% vs 20%; difference, 35% [95% CI, 18% to 49%]; P < .001) (eTable 2 in the Supplement).
Factors Associated With PTSD Symptoms in Family Members of ARDS Patients
In multivariable models (Figure 3), COVID-19 ARDS was significantly associated with increased risk of PTSD-related symptoms in family members (OR, 2.05 [95% CI, 1.30 to 3.23]). Other factors independently associated with PTSD symptoms were male sex (OR, 0.39 [95% CI, 0.23 to 0.67]), age (OR, 0.83 per 10-year increase [95% CI, 0.72 to 0.96]), and level of social support (reported per additional point on a 10-point scale [0, extremely limited to 10, extremely effective] OR, 0.82 [95% CI, 0.74-0.90]).
Figure 3. Factors Independently Associated With the Presence of PTSD-Related Symptoms in Family Members of Patients With ARDS.
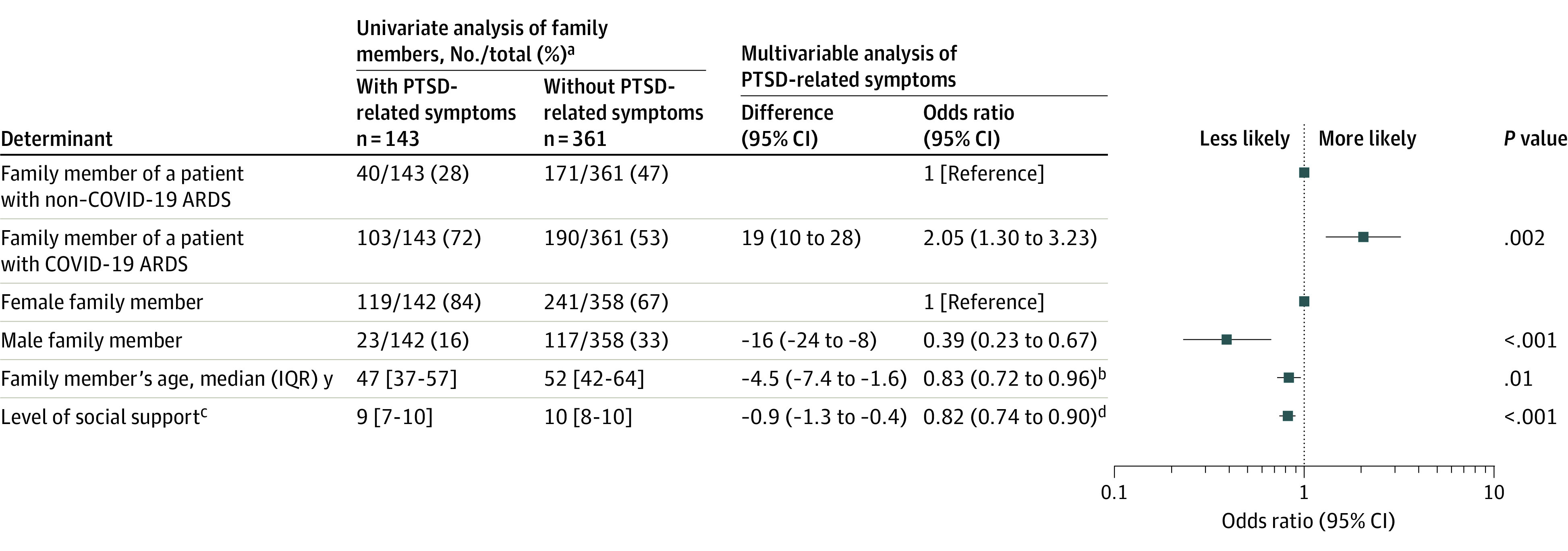
Variables considered for the LASSO step included sex, age, marital status, profession, and social support. For the Hosmer and Lemeshow goodness of fit test, P = .26. The sensitivity analyses took into account a center effect and another one that used a set of data after imputation of missing variables provided similar results and are reported in eTables 8 and 9 in the Supplement.
aValues are given according to posttraumatic stress disorder (PTSD) status, and values are reported as No./total (%) unless otherwise indicated.
bIndicates the odds ratio per 10-years increase.
cLevel of social support was evaluated on a scale ranging from 0 (extremely limited) to 10 (extremely effective).
dIndicates the odds ratio per additional point of the social support scale.
Factors associated with anxiety included COVID-19 ARDS, age, male sex, and level of social support, while COVID-19 ARDS and level of social support were independently associated with depression (P < .01 for all, eTable 6 in the Supplement).
Sensitivity Analyses
Multiple sensitivity analyses gave similar results (eTables 8-10 in the Supplement).The primary findings were not changed when accounting for site. When multiple imputation was used to account for missing data, COVID-19 ARDS remained significantly associated with greater odds of PTSD among family members (OR, 2.12 [95% CI, 1.37 to 3.27]) compared with non–COVID-19 ARDS. The primary findings were not changed in a model that used a cutoff of 26 for the IES-R.
Comparison Data Among ARDS Patients
Of the 307 surviving patients, 178 were admitted to the ICU for COVID-19 and 129 for non–COVID-19 ARDS (eTables 3 and 4 in the Supplement). Day 90 telephone interviews were completed by 273 (89%) patients (eFigure 2 in the Supplement). Compared with non–COVID-19 ARDS, ICU survivors of COVID-19 ARDS had rates of symptoms that were not significantly different for PTSD (20% vs 15%; P = .24), anxiety (25% vs 35%; P = .07), or depression (22% vs 24%; P = .65). Neither the PCS nor the MCS SF-36 subscores were significantly different across the 2 groups (eFigures 3 and 4 in the Supplement). Compared with family members, ICU survivors reported fewer PTSD symptoms (eTable 5 in the Supplement; difference, 10% [95% CI, 4% to 16%]; P = .001), which were only weakly correlated (coefficient, 0.27 [95% CI, 0.14 to 0.39]).
Discussion
In a prospective cohort study in 23 ICUs in France, family members of patients with COVID-19 ARDS had a significantly higher prevalence of symptoms of PTSD, anxiety, and depression at 90 days after patients’ discharge from the ICU than family members of patients with non–COVID-19 ARDS. In multivariable models adjusting for age, sex, and level of social support, COVID-19 ARDS was significantly associated with increased risk of PTSD-related symptoms in family members.
Prior research has demonstrated that hospitalization with ARDS is associated with a greater risk of patients and family members experiencing post-ICU psychological burden.4,5,21,22 This study extends prior findings to show that the level of social support was associated with PTSD symptoms. There are many potential explanations for these findings including the need to comply with strict isolation measures to prevent viral transmission and the strain put on ICU staff due to the surge in patient numbers caused by the pandemic. When ICUs are perceived as closed departments, visitors may feel unwelcome, and these closed ICUs can generate stress and symptoms of anxiety, depression, or PTSD in the family members.23
These findings are consistent with other research. In a 2019 cross-sectional study of families of patients who required mechanical ventilation for more than 3 days, 65% of family members were at risk for anxiety, 76% for depression, and 68% for PTSD.24 A survey study conducted in The Netherlands showed that individuals who had experienced a non–COVID-19-related loss within the past 5 months experienced more severe acute grief during the pandemic than before.25 In the present study, the 62% prevalence of PTSD in bereaved family members of patients who died from COVID-19 was nearly twice as high than the 35% found in family members of survivors. The disruption produced by the pandemic may have adversely affected the post-ICU outcomes. For instance, depending on the group, 27% to 40% of family members were unable to say goodbye to their dying relative, a ritual that plays a key role in promoting healthy grieving.8 Similarly, more bereaved family members in the COVID-19 group than in the non–COVID-19 group failed to attend the funeral, possibly due to concerns over transmitting the virus.
Perceived social support during the ICU stay was an important factor associated with family outcomes. Social support is the subjective perception of the extent to which family, friends, and other network members, as well as mental health specialists, are available and helpful. In a survey of 898 patients hospitalized with COVID-19 in China, poorer perceived social support was associated with anxiety, depression, and PTSD.26 Interventions to improve well-being after traumatic events are warranted.27
Limitations
This study has several limitations. First, the patients were admitted during early 2020 in France. The results may not apply to subsequent seasons or to the resilience of family members later in the pandemic.
Second, all participating ICUs belonged to a research network with extensive experience investigating and improving family care in the ICU. These results may not apply to ICUs that do not place a strong focus on family care.
Third, all the participating hospitals are in France; this may limit generalizability of participants and results to countries that have different ICU staffing, COVID-related census, and cultural approaches to critical illness and death. However, this is mitigated to some extent by the inclusion of both university-affiliated and non–university-affiliated hospitals and the high consent rate and follow-up participation by family members.8,28
Fourth, not all the patients may have met the strict consensus criteria for ARDS. However, all patients had acute hypoxemic respiratory failure within 7 days, a Pao2/Fio2 ratio of less than 300, and bilateral opacities on chest radiography not fully explained by cardiac failure or fluid overload. Intubation rates were also similar comparing COVID-19 with non–COVID-19 patients.
Fifth, ICU clinical staff did not participate in the study, and they may have contributed to differential experiences of patients and family members after intensive care.
Conclusions
Among family members of patients hospitalized in the ICU with ARDS, COVID-19 disease, as compared with other causes of ARDS, was significantly associated with increased risk of symptoms of PTSD at 90 days after ICU discharge.
Section Editor: Christopher Seymour, MD, Associate Editor, JAMA (christopher.seymour@jamanetwork.org).
eTable 1. Main Characteristics of the 23 Participating ICUs
eTable 2. Assessment of the 135 Bereaved Relatives on Day 90 After ICU Discharge
eTable 3. Characteristics of Patients Who Provided Informed Consent
eTable 4. Assessment of the Patients on Day 90 After ICU Discharge
eTable 5. Day 90 Outcomes in 307 Surviving Patients
eTable 6. Multivariable Analysis: Independent Determinants of Symptoms of Anxiety and Depression in the Family Members
eTable 7. Day 90 Outcomes in 517 Family Members of COVID-19 and Non–COVID-19 Patients After Multiple Imputation
eTable 8. Independent Determinants of PTSD-Related Symptoms in Family Members Including Center Effect
eTable 9. Independent Determinants of PTSD-Related Symptoms in Family Members After Multiple Imputation
eTable 10. Independent Determinants of PTSD-Related Symptoms Defined by Score Greater Than 26
eFigure 1. Study Design
eFigure 2. Patients’ Flow Diagram
eFigure 3. Health-Related Quality of Life in Patients Who Were Alive at 90 Days
eFigure 4. Mental (Left) and Physical (Right) Components Scores of the SF-36 in Patients With COVID-19 (Red) vs Non–COVID-19 (Blue) ARDS 90 Days After ICU Discharge
References
- 1.Piroth L, Cottenet J, Mariet A-S, et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. 2021;9(3):251-259. doi: 10.1016/S2213-2600(20)30527-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Writing Committee for the COMEBAC Study Group; Morin L, Savale L, Pham T, et al. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021; 325(15):1525-1534. doi: 10.1001/jama.2021.3331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Crit Care Med. 2012;40(2):618-624. doi: 10.1097/CCM.0b013e318236ebf9 [DOI] [PubMed] [Google Scholar]
- 4.Herridge MS, Cheung AM, Tansey CM, et al. ; Canadian Critical Care Trials Group . One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683-693. doi: 10.1056/NEJMoa022450 [DOI] [PubMed] [Google Scholar]
- 5.Cameron JI, Chu LM, Matte A, et al. ; RECOVER Program Investigators (Phase 1: towards RECOVER); Canadian Critical Care Trials Group . One-year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374(19):1831-1841. doi: 10.1056/NEJMoa1511160 [DOI] [PubMed] [Google Scholar]
- 6.Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228-229. doi: 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, Spudich S. Neuropathogenesis and neurologic manifestations of the coronaviruses in the age of coronavirus disease 2019: a review. JAMA Neurol. 2020;77(8):1018-1027. doi: 10.1001/jamaneurol.2020.2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robert R, Le Gouge A, Kentish-Barnes N, et al. Terminal weaning or immediate extubation for withdrawing mechanical ventilation in critically ill patients (the ARREVE observational study). Intensive Care Med. 2017;43(12):1793-1807. doi: 10.1007/s00134-017-4891-0 [DOI] [PubMed] [Google Scholar]
- 9.Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356(5):469-478. doi: 10.1056/NEJMoa063446 [DOI] [PubMed] [Google Scholar]
- 10.Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale-Revised. Behav Res Ther. 2003;41(12):1489-1496. doi: 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- 11.Pochard F, Azoulay E, Chevret S, et al. ; French FAMIREA Group . Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29(10):1893-1897. doi: 10.1097/00003246-200110000-00007 [DOI] [PubMed] [Google Scholar]
- 12.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. doi: 10.1177/2050312116671725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The Hospital Anxiety And Depression Scale. Acta Psychiatr Scand. 1983;67(6):361-370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 14.Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(4)(suppl):AS264-AS279. [PubMed] [Google Scholar]
- 15.Peyre H, Leplège A, Coste J. Missing data methods for dealing with missing items in quality of life questionnaires: a comparison by simulation of personal mean score, full information maximum likelihood, multiple imputation, and hot deck techniques applied to the SF-36 in the French 2003 decennial health survey. Qual Life Res. 2011;20(2):287-300. doi: 10.1007/s11136-010-9740-3 [DOI] [PubMed] [Google Scholar]
- 16.Carson SS, Cox CE, Wallenstein S, et al. Effect of palliative care-led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA. 2016;316(1):51-62. doi: 10.1001/jama.2016.8474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc B. 1996;58:267-288. doi: 10.1111/j.2517-6161.1996.tb02080.x [DOI] [Google Scholar]
- 18.Hosmer DW, Lemeshow S. Applied Logistic Regression. John Wiley and Sons; 2000. doi: 10.1002/0471722146 [DOI] [Google Scholar]
- 19.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377-399. doi: 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- 20.Barnard J, Rubin D. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86(4):948-955. doi: 10.1093/biomet/86.4.948 [DOI] [Google Scholar]
- 21.Dinglas VD, Chessare CM, Davis WE, et al. Perspectives of survivors, families and researchers on key outcomes for research in acute respiratory failure. Thorax. 2018;73(1):7-12. doi: 10.1136/thoraxjnl-2017-210234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herridge MS, Moss M, Hough CL, et al. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med. 2016;42(5):725-738. doi: 10.1007/s00134-016-4321-8 [DOI] [PubMed] [Google Scholar]
- 23.Rosa RG, Falavigna M, da Silva DB, et al. ; ICU Visits Study Group Investigators and the Brazilian Research in Intensive Care Network (BRICNet) . Effect of flexible family visitation on delirium among patients in the intensive care unit: the ICU Visits randomized clinical trial. JAMA. 2019;322(3):216-228. doi: 10.1001/jama.2019.8766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jo M, Song M-K, Knafl GJ, Beeber L, Yoo Y-S, Van Riper M. Family-clinician communication in the ICU and its relationship to psychological distress of family members: a cross-sectional study. Int J Nurs Stud. 2019;95:34-39. doi: 10.1016/j.ijnurstu.2019.03.020 [DOI] [PubMed] [Google Scholar]
- 25.Eisma MC, Tamminga A. Grief before and during the COVID-19 pandemic: multiple group comparisons. J Pain Symptom Manage. 2020;60(6):e1-e4. doi: 10.1016/j.jpainsymman.2020.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen Y, Huang X, Zhang C, et al. Prevalence and predictors of posttraumatic stress disorder, depression and anxiety among hospitalized patients with coronavirus disease 2019 in China. BMC Psychiatry. 2021;21(1):80. doi: 10.1186/s12888-021-03076-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peirce RS, Frone MR, Russell M, Cooper ML, Mudar P. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychol. 2000;19(1):28-38. doi: 10.1037/0278-6133.19.1.28 [DOI] [PubMed] [Google Scholar]
- 28.White DB, Angus DC, Shields A-M, et al. ; PARTNER Investigators . A randomized trial of a family-support intervention in intensive care units. N Engl J Med. 2018;378(25):2365-2375. doi: 10.1056/NEJMoa1802637 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Main Characteristics of the 23 Participating ICUs
eTable 2. Assessment of the 135 Bereaved Relatives on Day 90 After ICU Discharge
eTable 3. Characteristics of Patients Who Provided Informed Consent
eTable 4. Assessment of the Patients on Day 90 After ICU Discharge
eTable 5. Day 90 Outcomes in 307 Surviving Patients
eTable 6. Multivariable Analysis: Independent Determinants of Symptoms of Anxiety and Depression in the Family Members
eTable 7. Day 90 Outcomes in 517 Family Members of COVID-19 and Non–COVID-19 Patients After Multiple Imputation
eTable 8. Independent Determinants of PTSD-Related Symptoms in Family Members Including Center Effect
eTable 9. Independent Determinants of PTSD-Related Symptoms in Family Members After Multiple Imputation
eTable 10. Independent Determinants of PTSD-Related Symptoms Defined by Score Greater Than 26
eFigure 1. Study Design
eFigure 2. Patients’ Flow Diagram
eFigure 3. Health-Related Quality of Life in Patients Who Were Alive at 90 Days
eFigure 4. Mental (Left) and Physical (Right) Components Scores of the SF-36 in Patients With COVID-19 (Red) vs Non–COVID-19 (Blue) ARDS 90 Days After ICU Discharge