Abstract
Background
Virtual reality (VR) balance training is increasingly being pursued in biomedical research, specifically with respect to investigating balance ability with VR. However, existing systematic reviews have found inconsistent conclusions about the efficacy of VR in improving balance in Parkinson disease (PD) patients.
Objective
The goal of the research was to evaluate the impact of VR balance training on the balance ability of patients with PD.
Methods
All major databases, including Web of Science, PubMed, Scopus, China National Knowledge Infrastructure, and Wanfang, were searched to identify all relevant studies published in English or Chinese since September 15, 2010. Two researchers independently conducted document retrieval, study selection, data extraction, and methodological quality evaluation.
Results
A total of 16 randomized controlled trials were analyzed (n=583 patients with PD), with the methodological quality evaluation score ranging from 5 to 8 points. A random effects model was selected to combine effect sizes. Meta-analysis showed that the balance ability of PD was significantly improved after VR training compared with the control group (standardized mean difference [SMD] 2.127, 95% CI 1.202 to 3.052, P<.001, I2=95.1, df=15). It is worth noting that the intervention platform may be the main reason for heterogeneity. Meta regression analysis showed that no training program could predict the impact of VR training (P=.57 to .94) on PD balance ability. Subgroup result showed that a single training time of 0 to 20 minutes (SMD 6.446), 4 to 6 times per week (SMD 4.067), training for 3 to 5 weeks (SMD 62.478), training course reached more than 30 times (SMD 4.405), and 201 to 300 minutes per week (SMD 4.059) maybe have more benefit.
Conclusions
A systematic review and meta-analysis confirmed that VR balance training is a highly effective means to improve balance performance with large effects in PD. In addition, we preliminarily extracted dose-effect relationships for training volume, informing clinicians and practitioners to design effective VR balance training for balance ability. Further research is needed to reveal optimal dose-response relationships following VR balance training.
Keywords: virtual reality, Parkinson disease, balance, systematic review, meta-analysis, meta-regression, serious games, VR, rehabilitation, VR training
Introduction
Background
Parkinson disease (PD) is the most common neurodegenerative movement disorder and is the result of impaired dopamine-producing nerve cells in the ventral midbrain accompanied by progressive neuronal loss [1,2]. These impairments lead to the maladjustment of motor performance and symptoms such as tremors, stiffness, and reduced limb coordination [3]. Such symptoms can reduce the ability to balance, which often further increases the risk of falling, limits mobility, and reduces the quality of daily life [4-6]. PD has a higher incidence rate among people older than 50 years, with a prevalence rate as high as 4% [4-6]. It is also the fastest growing neurodegenerative condition, impacting 17.5 million individuals globally by 2040. [7,8]. At present, PD is mainly treated by slowing down the course of the disease and improving its core symptoms. The most common clinical scheme for the current treatment of PD is dopamine and deep brain electrical stimulation; however, these have limited and unstable effects in improving posture control and balance [9,10]. In addition, rehabilitation therapy is crucial in the treatment of PD. Exercise has been used as a common rehabilitation therapy, including stretching exercises, strength training, and aerobic exercises to help restore motor function in PD patients [11]. Overall, research shows that rehabilitation therapy based on exercise and cognitive reeducation can effectively improve balance and motor function of PD patients in daily life [12].
As a relatively new intervention measure, virtual reality (VR) technology has become an important auxiliary means in the treatment of various diseases. VR technology involves human-computer interaction technology based on perception (visual, tactile, kinesthetic) and can provide patients with multisensory stimulation and rich virtual scenes, increase the sense of immersion, and realize real-time feedback on physical actions. The main potential mechanisms of VR therapy include the repeatability of virtual tasks, positive feedback from virtual devices, and concrete simulation of a virtual environment. Studies have found that task-oriented repetitive training can enhance the synaptic strength in the brain, continuously affect nerve transmission, and maintain the enhanced functional circuit, thereby accelerating neuroplasticity in patients with neurodegenerative diseases [13]. Therefore, VR technology may be an effective means of treating neurodegenerative diseases such as PD. Under VR conditions, individuals experience multiple sources of sensory stimulation and complete multiple forms of repetitive tasks in a comfortable, safe, and immersive virtual environment, thereby promoting individual functional learning and the transfer of learning function. The potential advantage of VR is that training in VR environments can realize the maintenance and transfer of individual motor skills, which is an important feature of motor skill learning and the basis of real-world behavior [14]. Therefore, VR therapy is considered a supplement to traditional rehabilitation therapy and has been proven to be feasible and effective for treating a variety of neurological diseases [15,16].
At present, optimizing and strengthening the brain compensation mechanism is an important treatment method for PD and other movement disorders [17]. The virtual environment created by VR technology can promote the illusion of bodily movement, increase immersion to enhance the activation of motor brain regions, mobilize the changes of brain neural plasticity, reconstruct the synapses of nervous system cells, and directly train the central nervous system [18,19], resulting in significant benefits to the reorganization and recovery of nerve structure in PD and other neurodegenerative diseases [20]. Existing systematic reviews have found inconsistent conclusions about the efficacy of VR in improving balance in PD patients. One such review found that VR training can effectively improve balance in PD patients compared to other positive interventions [20,21]; however, other studies did not find these effects [22], a discrepancy that may be due to publication bias and diversity of interventions [20]. In addition, sample sizes of randomized controlled trials (RCTs) are currently insufficient to explore the dose effect of VR technology training on improving PD balance [20].
Objectives
In view of the current state of research consensus, the primary objective of this study was to review and analyze the existing RCT studies to verify whether VR training can improve balance in PD patients. Positive findings would prompt further investigation of an optimal dose of VR training to improve the balance of PD patients with the eventual goal of providing clinical workers with stronger theoretical support for VR training in the treatment of PD.
Methods
This study was conducted in accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-analyses [20].
Research Retrieval
We searched 5 databases: Web of Science, PubMed, Scopus, China National Knowledge Infrastructure, and Wanfang. The last retrieval date was September 15, 2020. We conducted a literature retrieval using three sets of keywords: (1) virtual reality, VR, Kinect, Wii, Xbox; (2) Parkinson, parkinsonian disorders, Parkinson, parkinsonism, Parkinson disease, PD; and (3) balance, equilibrium, dynamic postural control; the three groups of keywords were retrieved using the AND combination in the database. The Chinese database used the Chinese translation of the above keywords. Finally, the references of all included studies and relevant systematic reviews [20,21,23-27] were manually searched to further identify relevant studies.
Inclusion Criteria
Research Type
The studies were either RCTs or nonrandomized controlled trials, where nonrandomized trials generated by pseudorandom or nonrandom sequences were defined as nonrandomized controlled trials. Those that did not involve a comparison group or did not report intergroup comparisons were excluded. In the case of cross-sectional designs, a set of postmortem and qualitative analyses were also excluded. We further excluded reviews, conference summaries, and book chapters and restricted our research to articles written in the English or Chinese language.
Participant Type
The subjects of the study were PD patients aged 18 years or older who had been formally diagnosed by the hospital or by internationally recognized diagnostic criteria. There were no restrictions on sex, course of disease, or severity of the disease.
Intervention Type
The VR training immersion included a variety of modes, such as nonimmersive, semi-immersive, and fully immersive. The control group consisted of a wait group, routine physical therapy, or other types of treatment such as drug therapy.
Types of Outcome Indicators
In order to improve the quality of research, it was necessary to use effective and reliable tools to measure balance ability. Due to the high task specificity of balance ability, we selected the Berg Balance Scale (BBS), which is widely used to assess overall balance ability of patients with movement disorders [28]. The full assessment includes 14 balance-related activities, in which higher scores indicate better balance ability. The maximum possible score is 56 points, and a score below 40 indicates a risk of declining balance ability.
Study Selection and Data Extraction
We conducted independent screening of studies based on the title, abstract, and full text, and two researchers discussed the results before reaching a consensus. In the event of no consensus, a third researcher made the final decision.
Descriptive data were extracted after reading the full text. The extracted content comprised 3 categories: literature characteristics, participant characteristics, and intervention plan. Literature characteristics included first author, number of years of publication, country, and language. Participant characteristics included diagnostic criteria (diagnostic tools), number of participants (number and sex ratio of the experimental group and control group), and age. In order to determine the dose-response relationship of VR training to improve balance in PD patients, the balance training scheme was coded as follows: training group (experimental group and control group), single training duration, training frequency, total number of training sessions, weekly training duration and total training duration, and VR training platform [27,29]. We extracted the quantitative balance data in the experimental and control group in each eligible RCT study (ie, BBS scores before and after intervention were extracted), and the results must be quantitative data that can be used for effect size calculation. If there were multiple control groups in the study, only the control group with active intervention measures was extracted.
Quality Assessment
We used the Physiotherapy Evidence Database (PEDro) Scale to assess the methodological quality of clinical trials in physiotherapy and rehabilitation [30]. The quality evaluation was carried out using the PEDro quality assessment sheet to evaluate the treatment included in the study. The evaluation criteria were as follows: eligibility criteria, randomization, concealed allocation, baseline equivalence, blinding of participants, blinding of instructors, blinding of assessors, retention rate of 85%, missing data management (intent-to-treat analysis), between-group analysis, and measures of variability. One point was awarded if the information was explicitly presented, with a maximum of 9 points per study. If the above information was clear in the study, 1 point was awarded; if not, 0 points were awarded, while the maximum score for each study was 11 points. According to the scores, the quality of these studies can be divided into 4 grades: excellent (>9 points), good (6 to 8 points), fair (4 to 5 points), and poor (<4 points) quality. For studies that did not provide enough information to complete the assessment, the authors requested relevant information via email; a lack of author response resulted in a designation of ambiguous information.
Data Analysis
In order to explore the benefits of VR training on PD balance, we combined extracted BBS scale data with effect size using the statistical software STATA (version 15.1, StataCorp LLC), resulting in a random effect model for further analysis calculation. The standardized mean difference (SMD) was selected as the index of effect scale for statistics. The effect size indicated the degree of impact of VR training on PD balance ability, where SMD <0.20 indicated a negligible effect, 0.20 to <0.50 indicated a small effect, 0.50 to <0.80 indicated a large effect, and an SMD >0.80 indicated a larger effect [31].
We used the statistic I2 to evaluate the heterogeneity of the selected studies, in which a larger I2 statistic indicates greater heterogeneity [31]. In addition, we used funnel plots and Egger tests to evaluate publication bias [32]. Subgroup analyses were used to estimate the impact of publication bias on the interpretation of results [33]. We further used meta-regression models to analyze the effect of the VR training program according to length and frequency of training courses, total time of weekly training courses, total number, and time of training courses. Therefore, this meta-regression part was not analyzed in this study due to its failure in quantifying the intensity of treatment. For studies that did not provide the above data, the author was contacted by email to obtain the data, so as to improve the quality of this research.
Results
Study Selection
We retrieved a total of 491 records through electronic databases: 200 records were retrieved by Web of Science, 84 records were retrieved by PubMed, 144 records were retrieved by Scopus, 53 records were retrieved by China National Knowledge Infrastructure, and 10 records were retrieved by Wanfang. In addition, 10 records were added manually.
We then excluded 105 duplicate records. The remaining 393 records were further screened by titles and abstracts, and 373 records that did not meet the study criteria were deleted. We then evaluated 23 studies for full-text qualification, and 7 studies were found not to meet the predetermined inclusion criteria. Finally, a total of 16 studies were identified for meta-analysis. The flow chart of literature retrieval and study selection is shown in Figure 1.
Figure 1.
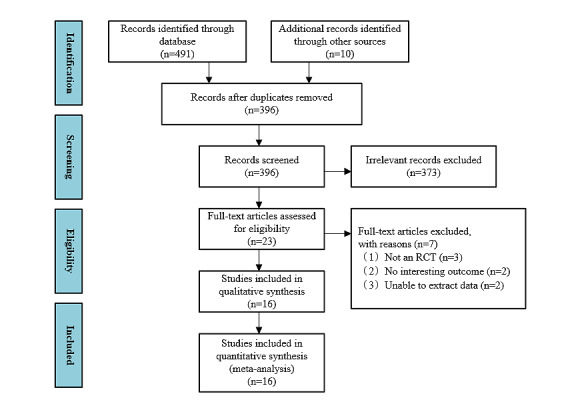
The flow of literature search and study selection. RCT: randomized controlled trial.
Research Characteristics
Table 1 lists the characteristics and descriptions of the 16 studies published from 2012 to 2020, involving 583 PD (experimental group: 291; control group: 292) participants aged 55 to 75 years in the included study. All the included PDs were tested using diagnostic tools such as the Movement Disorder Society Clinical Diagnostic Criteria for Parkinson disease (MDS-PD), the United Kingdom Parkinson Disease Society Brain Bank criteria (UK-PDSBB), and the Chinese Parkinson Diagnostic Criteria, or patients who had been clinically diagnosed as PD by doctors, of which six [33] studies were conducted in China, two [34,35] studies were conducted in the United Kingdom, two [34,35] studies were conducted in Brazil, and two [36,37] studies were conducted in Taiwan, including one study each in South Korea [38], Italy [39], the United States [40], and Istanbul [41]. All of the included studies were comparative studies between the VR group and conventional rehabilitation.
Table 1.
Study characteristics.
| Reference | Participant characteristics | Intervention protocol | ||||||||
| Authors | Country, Language | Diagnostic criteria | Hoehn-Yahr classification | N, male/female | Age | Method | Session duration/frequency/period/# sessions/duration of VRa treatment per week | Platform | ||
| Chen et al [33] | China, Chinese | Chinese Parkinson Diagnostic Criteria | EGb: 2.52 (SD 0.51); CGc: 2.57 (SD 0.50) | EG: 23, 14/9; CG: 23, 12/11 | EG: 62.09 (SD 6.11); CG: 64.65 (SD 5.06) | EG: VR training; CG: routine rehabilitation training | 50 min/5 times per wk/6 wk/30/250 min | BioFlex-FP posture control evaluation and training system | ||
| Cheng et al [47] | China, Chinese | MDS-PDd | EG: 3.1 (SD 0.6); CG: 3.0 (SD 0.6) | EG: 20, 9/11; CG: 20, 8/12 | EG: 59.2 (SD 7.3); CG: 58.6 (SD 7.5) | EG: VR training+ routine rehabilitation training (40 min); CG: routine rehabilitation training | 20 min/2 times per wk/8 wk/16/40 min | Silverfit 3D motion capture analysis system | ||
| Sun et al [46] | China, Chinese | Clinical diagnosis | Total: 1-4 | EG: 30, 19/11; CG: 30, 21/9 | EG: 61.43 (SD 7.34); CG: 62.54 (SD 6.98) | EG: VR training + strengthen muscle strength training (20 min); CG: routine rehabilitation training + medication | 20 min/5 times per wk/4 wk/20/100 min | Silverfit 3D motion capture analysis system | ||
| Lin et al [48] | China, Chinese | Chinese Parkinson Diagnostic Criteria | Total: 2.5-4 | EG: 18, 12/6; CG: 15, 10/5 | EG: 61.4 (SD 8.2); CG: 62.1 (SD 6.3) | EG: VR training + medication; CG: routine rehabilitation training + medication | 30 min/5 times per wk/4 wk/20/150 min | Xbox (Microsoft Corp) | ||
| Liu et al [45] | China, Chinese | Chinese Parkinson diagnostic criteria | Total: 3 | EG: 21, 11/10; CG: 21, 12/9 | EG: 60.9 (SD 7.20); CG: 63.9 (SD 5.82) | EG: VR training; CG: routine rehabilitation training | 20 min/5 times per wk/4 wk/20/150 min | Computer-assisted rehabilitation environment (CAREN) | ||
| Pompeu et al [35] | Brazil, English | Clinical diagnosis | Total: 1-2 | Total: 32, 17/15 | Total: 67.4 (SD 8.1) | EG: VR training; CG: routine rehabilitation training | 30 min/2 times per wk/7 wk/14/60 min | Wii Fit (Nintendo Co Ltd) | ||
| Van et al [34] | UK, English | UK-PDSBBe | Total: 2-3 | EG: 17, 12/5; CG: 16, 8/8 | EG: 66.3 (SD 6.39); CG: 68.8 (SD 9.68) | EG: VR training; CG: routine rehabilitation training | 60 min/2 times per wk/5 wk/10/120 min | Workstations consisted of a flat-panel LCD monitor connected to a PC containing a total of 6 commercially available, interactive dynamic balance exercises (Motek Medical) | ||
| Lee et al [37] | Korea, English | Clinical diagnosis | NRf | EG: 10, 5/5; CG: 10, 5/5 | EG: 68.4 (SD 2.9); CG: 70.1 (SD 3.3) | EG: VR training + neurodevelopmental therapy (NR) + functional electrical stimulation therapy (NR); CG: routine rehabilitation training | 30 min/5 times per wk/6 wk/30/150 min | k-pop dance festival (Nintendo Inc) game for the Wii (Nintendo Inc) video game system | ||
| Shih et al [41] | Taiwan, English | UK-PDSBB | EG: 1.6 (SD 0.84) ; CG: 1.4 (SD 0.52) | EG: 10, 9/1; CG: 10, 7/3 | EG: 67.5 (SD 9.96); CG: 68.8 (SD 9.67) | EG: VR training; CG: routine rehabilitation training | 50 min/2 times per wk/8 wk/16/100 min | Kinect sensor (Microsoft Corp) | ||
| Yang et al [36] | Taiwan, English | UK-PDSBB | Total: 2-3 | EG: 11, 7/4; CG: 12, 7/5 | EG: 75.4 (SD 6.3); CG: 72.5 (SD 8.4) | EG: VR training; CG: routine rehabilitation training | 50 min/2 times per wk/6 wk/12/100 min | VR balance training system included a 22-inch all-in-one touchscreen computer (Micro-Star International Co Ltd) and a wireless balance board | ||
| Ozgonenel et al [40] | Istanbul, English | Clinical diagnosis | Total: 1-3 | EG: 15, 10/5; CG: 18, 12/6 | EG: 64; CG: 65 | EG: VR training + routine rehabilitation training (NR); CG: balance rehabilitation training | 20 min/3 times per wk/5 wk/15/60 min | Xbox (Microsoft Corp) | ||
| Gandolfi et al [38] | Italy, English | UK-PDSBB | Total: 1-3 | EG: 38, 23/15; CG: 38, 28/10 | EG: 67.45 (SD 7.18); CG: 69.84 (SD 9.41) | EG: VR training + balance rehabilitation training (NR); CG: sensory integration balance rehabilitation training | 50 min/3 times per wk/7 wk/21/150 min | Wii Fit gaming system and balance board (Nintendo Co Ltd) | ||
| Ribas et al [43] | Brazil, English | UK-PDSBB | Total: 2-3 | EG: 10, 4/6; CG: 10, 4/6 | EG: 61.7. (SD 6.83); CG: 60.20 (SD 11.29) | EG: VR training; CG: routine rehabilitation training | 30 min/2 times per wk/12 wk/24/60 min | Wii Fit gaming system, and balance board (Nintendo Co Ltd) | ||
| Santos et al [39] | US, English | UK-PDSBB | EG: 1.4 (SD 0.6); CG: 1.3 (SD 0.3) | EG: 13; CG: 14 | EG: 61.7 (SD 7.3); CG: 64.5 (SD 9.8) | EG: VR training; CG: routine rehabilitation training | 50 min/2 times per wk/8 wk/16/100 min | Wii Fit gaming system and balance board (Nintendo Co Ltd) | ||
| Feng et al [42] | China, English | UK-PDSBB | EG: 3.03 (SD 0.55); CG: 2.97 (SD 2.66) | EG: 14, 8/7; CG: 14, 9/6 | EG: 67.47 (SD 4.79); CG: 66.93 (SD 4.64) | EG: VR training + medication; CG: routine rehabilitation training + medication | 45 min/5 times per wk/12 wk/60/225 min | NR | ||
| Tollár et al [49] | UK, English | UK-PDSBB | EG: 2.3 (SD 0.48); CG: 2.4 (SD 0.51) | EG: 25, 12/13; CG: 25, 11/14 | EG: 70.0 (SD 4.69); CG: 70.6 (SD 4.10) | EG: VR training + medication; CG: routine rehabilitation training + medication | 60 min/5 times per wk/5 wk/25/300 min | EXEg used the following 3 visual feedback modules of the Xbox 360 core system (Kinect Adventures, Microsoft Corp) | ||
aVR: virtual reality.
bEG: experiment group.
cCG: control group.
dMDS-PD: Movement Disorder Society clinical diagnostic criteria for Parkinson disease.
eUK-PDSBB: United Kingdom Parkinson Disease Society Brain Bank criteria.
fNR: no report.
gEXE: exergame.
The VR training program has a single duration between 30 and 60 minutes, with frequency varying from 2 to 5 times per week and duration ranging from 4 to 12 weeks. All of the 16 studies were nonimmersive VR devices, including Xbox (Microsoft) and Wii Fit (Nintendo Co Ltd). Among them, four studies [35,36,41,42] used Xbox Kinect equipment and five studies [38-40,43,44] used Wii Fit equipment. Additionally, two studies [45,46] used Silverfit 3D motion capture analysis system, three studies [37,47,48] were personalized development VR rehabilitation systems, and one study [34] only reported device components and game types, among which one study [49] did not report the name of VR device. The outcome indicators of interest in this study were all BBG scales, thereby having no separate description in the study characteristics.
Methodological Quality
The results of methodological assessment are shown in Table 2, with scores ranging from 5 to 8 and an average score of 6.56. Specifically, the most common methodological flaw in these studies was that there was no allocation concealment. Due to the difficulty in conducting blind training in VR training and routine rehabilitation training, most of the included studies did not implement subject blindness, therapist blindness, or evaluator blindness.
Table 2.
Study quality assessment of eligible studies.
| Author | Eligibility criteria | Randomization | Concealed allocation | Similar baseline | Blinding of participants | Blinding of instructors | Blinding of assessors | Retention >85% | Intent-to-treat analysis | Between-group comparison | Point measure and measures of variability | Sum score |
| Chen et al [33] | 1a | 1 | 0b | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Cheng et al [47] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5 |
| Sun et al [46] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Lin et al [48] | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Liu et al [45] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Pompeu et al [35] | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Van et al [34] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 7 |
| Lee et al [37] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 5 |
| Shih et al [41] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 8 |
| Yang et al [36] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Ozgonenel et al [40] | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 6 |
| Gandolfi et al [38] | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Ribas et al [43] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Santos et al [39] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 7 |
| Feng et al [42] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| Tollár et al [49] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 8 |
aExplicitly described and present in details.
bAbsent, inadequately described, or unclear.
Effect Of VR Training on Improving PD Balance Ability
A total of 16 studies investigated the effects of VR training on improving PD balance ability. These data were analyzed for random effects to combine the results. Figures 2 and 3 illustrate the effects of VR balance training on balance. The meta-analysis results showed that SMD 2.13, 95% CI 1.20 to 3.05, P<.001 (see Figure 2). This indicates the balance ability of PD was significantly improved after VR training compared with the control group. The Egger test results found no significant publication bias (Egger regression intercept 10.69691, P<.001, df=15). However, results of funnel plots showed that three studies [49] exhibited asymmetry. That is, the included studies may have publication bias (see Figure 3). It is worth noting that the interstudy heterogeneity was very high, the value of I2 with over 75% (I2=95.1, P<.001).
Figure 2.
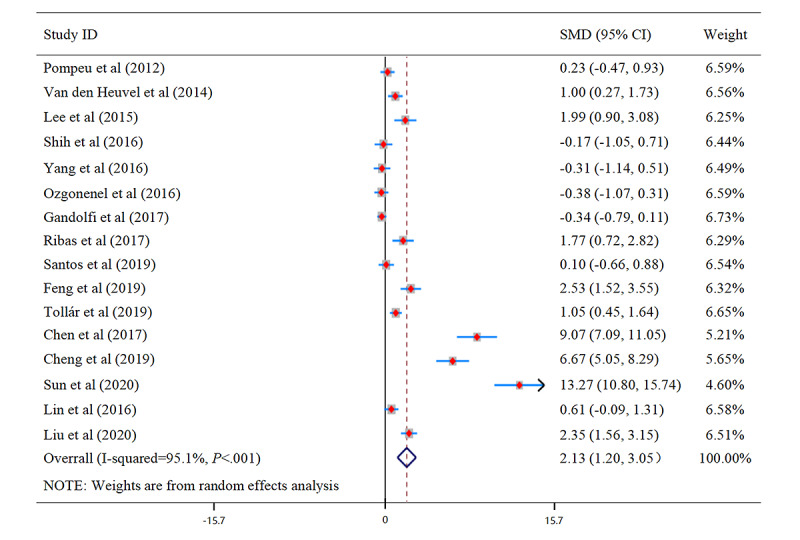
Forest plot for balance. SMD: standardized mean difference.
Figure 3.
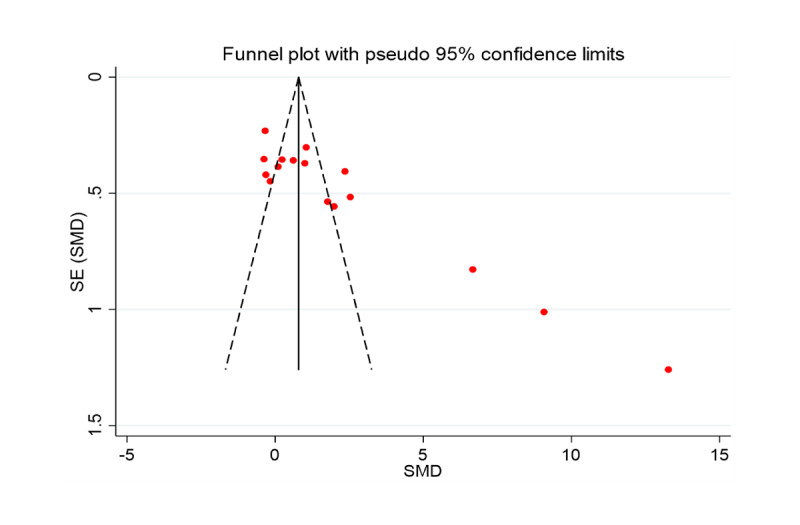
Funnel plot for balance. SMD: standardized mean difference.
Moderating Variable Analysis: Impact of Premode and Intervention Platform
We conducted subgroup analysis on intervention modes and intervention platforms (excluding one study [49] that did not report VR equipment) to clarify the regulatory effect of these 2 variables on PD balance ability. Subgroup analysis showed that training methods had great influence on balance ability. It is worth noting that intervention platform may be the main reason for heterogeneity, as subgroup analysis of the VR rehabilitation and commercial game VR platforms found that the heterogeneity of VR rehabilitation platforms (I2=96.8%) was very large, while that of commercial game VR reality platforms was relatively small; however, there was no significant difference in the improvement of PD balance ability of commercial game VR platforms (SMD 0.447, 95% CI 0.03 to 0.898), which may be the reason for the different conclusions in the previous review. Nevertheless, due to the lack of research on VR rehabilitation platforms, this result should be treated with caution (Table 3).
Table 3.
Results of the overall balance subgroup analyses on the influence of intervention method and intervention platform on virtual reality training in Parkinson disease.
| Independent training modality | SMDa | 95% CI | z value (P value) | I2b (%) | df | P value between groups | |
| Intervention method | |||||||
|
|
Virtual reality mixed physical rehabilitation methods | 2.64 | 0.699 to 4.588 | 2.66 | 96.8 | 5 | <.001 |
|
|
Virtual reality | 1.83 | 0.795 to 2.872 | 3.46 | 93.5 | 9 | <.001 |
| Intervention platform | |||||||
|
|
Virtual rehabilitation platform | 7.75 | 3.134 to 12.365 | 3.29 | 97.1 | 3 | <.001 |
|
|
Commercial gaming virtual reality platform | 0.45 | –0.0.3 to 0.898 | 1.95 | 76.2 | 10 | <.001 |
aSMD: standardized mean difference.
bI2: heterogeneity between studies.
Impact of VR Balance Training and the Dose-Effect Relationship
In order to explore the optimal training variables, this study first conducted a meta-regression to explore the effect of a training program on the effectiveness of PD balance. In addition to meta-regression (Table 3), subgroup analysis was conducted to preliminarily analyze the effect size of each training program subgroup and presented for the preliminary analysis of dose response relationships (Table 4).
Table 4.
Results for the subgroup analyses on the effects of different categories of respective training volume on balance ability.
| Training volume | Coefficient | SE | 95% CI | z value | 2-sided P value |
| Training period | –0.0558 | 0.2075 | –0.4626 to 0.3509 | –0.27 | .79 |
| Training frequency | 1.9711 | 3.4458 | –4.7826 to 8.7248 | 0.57 | .57 |
| Number of sessions | 0.4613 | 1.3035 | –2.0935 to 3.0162 | 0.35 | .72 |
| Single session duration | –0.1145 | 0.3182 | –0.7381 to 0.5091 | 0.36 | .72 |
| Total duration per week | –2.1933 | 0.0572 | –0.1167 to 0.1077 | –0.08 | .94 |
Meta-Regression Analysis of Volume of VR Balance Training
Due to the low number of studies, we performed meta-regression only for the subcategory training volume. The regression analysis revealed that no variable within the training volume subcategory (single training duration, training frequency, total number of training sessions, weekly training duration, total training duration) produced significant effects (P=.57 to .94) on the ability of improving balance level. That is, in the included studies, we could not use time or number of training sessions to predict the ability of improving balance level (see Table 4).
Dose-Effect Relationship of VR Balance Ability
Single Training Time
A total of 13 studies were included in this subanalysis, and the time range of single training from 0 to 20 minutes produced large effects on balance, with SMD of 6.446 (95% CI –1.098 to 13.990; z=1.67; I2=98%; df=2; see Table 5).
Table 5.
Results for the subgroup analyses on the effects of different categories of respective training volume on overall balance.
| Independent training modality | SMDa | 95% CI | z value (P value) | I2b (%) | df | P value between groups | |||||||
| Single training time | |||||||||||||
|
|
0-20 min | 6.446 | –1.098 to 13.990 | 1.67 (.094) | 98.7 | 2 | <.001 | ||||||
|
|
21-40 min | 1.050 | 0.122 to 1.979 | 2.22 (.027) | 89.4 | 5 | <.001 | ||||||
|
|
41-60 min | 1.644 | 0.378 to 2.910 | 2.54 (.011) | 93.6 | 6 | <.001 | ||||||
| Training frequency | |||||||||||||
|
|
1-3 sessions per week | 0.770 | –0.060 to 1.600 | 1.82 (.069) | 90.6 | 8 | <.001 | ||||||
|
|
4-6 sessions per week | 4.067 | 2.223 to 5.911 | 4.32 (<.001) | 96.1 | 6 | <.001 | ||||||
| Training period | |||||||||||||
|
|
3-5 weeks | 2.478 | 0.893 to 4.063 | 3.06 (.002) | 95.9 | 5 | <.001 | ||||||
|
|
6-8 weeks | 1.917 | 0.515 to 3.320 | 2.68 (.007) | 95.5 | 7 | <.001 | ||||||
|
|
9-12 weeks | 2.166 | 1.417 to 2.914 | 5.67 (.001) | 5.30 | 1 | <.001 | ||||||
| Total number of training sessions | |||||||||||||
|
|
10-20 sessions | 0.844 | –0.210 to 1.898 | 1.57 (.117) | 91.4 | 6 | <.001 | ||||||
|
|
21-30 sessions | 2.638 | 1.003 to 4.272 | 3.16 (.002) | 96.5 | 5 | <.001 | ||||||
|
|
>30 sessions | 4.405 | 1.102 to 7.707 | 2.61 (.009) | 95.0 | 2 | <.001 | ||||||
| Total duration of VRc training per week | |||||||||||||
|
|
0-100 min | 2.313 | 0.671 to 3.955 | 2.76 (.006) | 96.1 | 7 | <.001 | ||||||
|
|
101-200 min | 1.079 | 0.046 to 2.112 | 2.05 (.041) | 90.6 | 4 | <.001 | ||||||
|
|
201-300 min | 4.059 | 0.738 to 7.379 | 2.40 (.017) | 96.7 | 2 | <.001 | ||||||
aSMD: standardized mean difference.
bI2: heterogeneity between studies.
cVR: virtual reality.
Training Frequency
The training frequency was 1 to 6 sessions per week in the 14 studies, and the result showed the SMD for 4 to 6 sessions per week was 4.067 (95% CI 2.223 to 5.911; z=4.32 ; I2=96.1%; df=7), indicative of large effects (see Table 5).
Training Period
In 13 studies, during the training period, a time under training of 3 to 5 weeks with SMD of 2.478 appears most effective compared other training period (95% CI 0.893 to 4.063; z=3.03; I2=95.9%; df=5) in this subanalysis (see Table 5).
Total Number of Training Sessions
Based on data from 13 studies, we computed the effect of total number of training sessions (range: 10 to 20 sessions, 21 to 30 sessions, >30 sessions) of VR training for balance ability. Above 30 sessions in total, with SMD of 4.405 is the most effective for balance ability (95% CI 1.102 to 7.707; z=2.61; I2=95.0%; df=2; see Table 5).
Total Duration of VR Training per Week
In 14 studies, we also computed the effect of total duration of VR training per week (range 0 to 100 minutes, 101 to 200 minutes, 201 to 300 minutes). The largest effect was shown for 201 to 300 minutes of training per week (SMD 4.059; 95% CI 0.738 to 7.379; z=2.40; I2=96.7%; df=2; see Table 5).
Discussion
Summary
In this study, we examined the effect of VR technology on improving PD balance ability. Data analysis of 16 RCTs showed that (1) VR technology has a significant impact on the improvement of PD balance ability, (2) different VR platforms may have different effects on PD balance and the effect of rehabilitation platforms is superior to commercial platforms, and (3) variability in training methods cannot predict the effect of VR training on PD balance ability.
Impact of VR on PD Balance Ability
VR can provide visual and auditory feedback to PD patients, thereby minimizing the lack of movement caused by internal prompts due to reduced dopamine consumption [49]. In addition, the real-time feedback provided by VR platforms may also facilitate the movement process [50]. PD, by contrast, shows insufficient interaction between vestibular and proprioceptive systems, leading to changes in human biomechanics that affect balance. The visual and auditory input provided by VR can therefore effectively integrate the feedback of vestibular receptors and proprioceptive receptors in PD patients, improving PD balance ability [51]. VR training has been shown to stimulate the integration of PD-related cognitive functions such as attention and executive ability, as well as stimulate the reward mechanism of the brain. Moreover, success in alleviating PD symptoms using VR training requires attention, sensory integration, and treatment of stimuli in VR environments and may be more effective than traditional rehabilitation programs [52,53]. A functional near-infrared spectroscopy study found that VR training increases the blood oxygen concentration in the prefrontal cortex of the brain, indicating that prefrontal cortex is involved in VR balance task and degree of activation is modulated by VR task difficulty [54].
Long-term physical therapy is also beneficial for PD. Due to the incentive stimulation of VR technology, it can maintain motivation during the long-term rehabilitation process and improve compliance so as to reduce the negative impacts during the rehabilitation process [55]. In addition, studies have indicated that VR balance training and traditional interventions can increase the muscle strength and balance ability of patients with anterior cruciate ligament injury [56], as well as improve coordination and reflex conduction [57]. However, due to the fact that the measurement methods are not often very precise, it is difficult to find optimal balance points between the two.
Moderating Effect
Our subgroup analyses of intervention methods and intervention platforms found no statistically significant difference between intervention methods, nor did heterogeneity decrease significantly. However, we found VR rehabilitation platforms to be significantly heterogeneous, and the commercial game VR platform’s I2 reduced to 71.2%, which may be the main source of heterogeneity in this study. It should also be noted that we found no statistically significant effect of VR platform training of commercial games; that is, the effects of VR training and traditional rehabilitation training on PD balance ability were similar, which is consistent with previous research results [22]. We therefore conclude that the VR platform itself may be one of the reasons for the inconsistency of previous results, although a small sample size means that this result should also be treated with caution.
Although commercial systems such as Wii are now included in the neurorehabilitation program [58], such commercial games are not personalized and do not allow precise interactions between individuals and VR environments [58]. Furthermore, the overall safety and clinical nature of sports-based computer games have not been fully confirmed [52]. In addition, VR device design may not be optimized for PD, which may damage the experience and safety of PD patients [52].
Impact of VR Training and the Dose-Effect Relationship
As discussed previously, VR balance training is of great benefit to PD patients. Our results showed that no particular training method could predict the effect of VR balance training on PD balance performance. With the exception of meta-regression, subgroup analysis was conducted for each training program to explore the magnitude of the effect of a specific subgroup.
In addition to meta-regression, subgroup analysis was conducted for each training program to explore the magnitude of the effect of a specific subgroup and explain the effect of the amount of certain subgroups. The most successful VR training program to enhance PD balance was a single training duration of 0 to 20 minutes, 4 to 6 times a week, training for 3 to 5 weeks, training course reached more than 30 times, 201 to 300 minutes per week. However, this study only provides a preliminary analysis of the dose-response relationship through subgroup analysis and should be more widely explored in future research.
Limitations
The biggest limitation of this study is that there was considerable heterogeneity across studies (ie, I2=95.1%). Even if subgroup analysis was performed to observe the underlying causes of heterogeneity, the results should be treated with caution. Another limitation is that due to the limited number of available studies, there were data from only 16 RCTs, and the intervention plans included in the study varied widely, making it difficult for subgroup analyses to provide a clear picture of the dose-response relationship. Moreover, due to the fact that the BBS scale is assessed manually, there may be a degree of error in the balance ability data.
Conclusion
The systematic review and meta-analysis confirmed that VR balance training is a highly effective means to improve balance performance with large effects in PD. In addition, we preliminarily extracted dose-effect relationships for training volume, informing clinicians and practitioners to design effective VR balance training for balance ability. Future studies should particularly focus on the detailed description of training variables, so as to further analyze the dose-effect relationship of VR balance training in PD.
Acknowledgments
This research was funded by grant 17QNFC59 from Humanities and Social Science, ShenZhen University, Young Teacher Award; grant QNJS0274 from the Research Foundation for Young Teachers of Shenzhen University; and grant RC00228 from the High-level Scientific Research Foundation for the Introduction of Talent of Shenzhen University.
Abbreviations
- BBS
Berg Balance Scale
- MDS-PD
Movement Disorder Society Clinical Diagnostic Criteria for Parkinson disease
- PD
Parkinson disease
- PEDro scale
Physiotherapy Evidence Database
- RCT
randomized controlled trial
- SMD
standardized mean difference
- UK-PDSBB
United Kingdom Parkinson Disease Society Brain Bank
- VR
virtual reality
Footnotes
Authors' Contributions: JW, H Zhang, and ZR contributed to the conception and design of the review. JW, RF, and HY applied the search strategy. JW, H Zhang, and ZC applied the selection criteria. JW and ZR completed assessment of risk of bias. JW and H Zhang analyzed and interpreted the data. JW wrote the manuscript. RF and H Zeng edited this manuscript. ZR is responsible for the overall project.
Conflicts of Interest: None declared.
References
- 1.Rocchi L, Chiari L, Horak F. Effects of deep brain stimulation and levodopa on postural sway in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2002 Sep;73(3):267–274. doi: 10.1136/jnnp.73.3.267. https://jnnp.bmj.com/lookup/pmidlookup?view=long&pmid=12185157 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan AU, Akram M, Daniyal M, Zainab R. Awareness and current knowledge of Parkinson's disease: a neurodegenerative disorder. Int J Neurosci. 2019 Jan 22;129(1):55–93. doi: 10.1080/00207454.2018.1486837. [DOI] [PubMed] [Google Scholar]
- 3.Lin MT, Beal MF. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006 Oct 19;443(7113):787–795. doi: 10.1038/nature05292.nature05292 [DOI] [PubMed] [Google Scholar]
- 4.Jankovic J. Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008 Apr 01;79(4):368–376. doi: 10.1136/jnnp.2007.131045.79/4/368 [DOI] [PubMed] [Google Scholar]
- 5.Wu J, Loprinzi PD, Ren Z. The rehabilitative effects of virtual reality games on balance performance among children with cerebral palsy: a meta-analysis of randomized controlled trials. Int J Environ Res Public Health. 2019 Oct 28;16(21):4161. doi: 10.3390/ijerph16214161. https://www.mdpi.com/resolver?pii=ijerph16214161 .ijerph16214161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sofuwa O, Nieuwboer A, Desloovere K, Willems A, Chavret F, Jonkers I. Quantitative gait analysis in Parkinson's disease: comparison with a healthy control group. Arch Phys Med Rehabil. 2005 May;86(5):1007–1013. doi: 10.1016/j.apmr.2004.08.012.S0003-9993(04)01395-4 [DOI] [PubMed] [Google Scholar]
- 7.Hayes MT. Parkinson's Disease and Parkinsonism. Am J Med. 2019 Jul;132(7):802–807. doi: 10.1016/j.amjmed.2019.03.001.S0002-9343(19)30235-9 [DOI] [PubMed] [Google Scholar]
- 8.Berg D, Deuschl G. Movement disorders: discoveries in pathophysiology and therapy. Lancet Neurol. 2015 Jan;14(1):9–11. doi: 10.1016/s1474-4422(14)70307-2. [DOI] [PubMed] [Google Scholar]
- 9.Bloem BR, de Vries NM, Ebersbach G. Nonpharmacological treatments for patients with Parkinson's disease. Mov Disord. 2015 Sep 15;30(11):1504–1520. doi: 10.1002/mds.26363. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong MJ, Okun MS. Choosing a Parkinson disease treatment. JAMA. 2020 Apr 14;323(14):1420. doi: 10.1001/jama.2020.1224.2764458 [DOI] [PubMed] [Google Scholar]
- 11.Maggio MG, Russo M, Cuzzola MF, Destro M, La Rosa G, Molonia F, Bramanti P, Lombardo G, De Luca R, Calabrò R. Virtual reality in multiple sclerosis rehabilitation: a review on cognitive and motor outcomes. J Clin Neurosci. 2019 Jul;65:106–111. doi: 10.1016/j.jocn.2019.03.017.S0967-5868(19)30185-7 [DOI] [PubMed] [Google Scholar]
- 12.Abbruzzese G, Marchese R, Avanzino L, Pelosin E. Rehabilitation for Parkinson's disease: current outlook and future challenges. Parkinsonism Relat Disord. 2016 Jan;22 Suppl 1:S60–4S6. doi: 10.1016/j.parkreldis.2015.09.005.S1353-8020(15)00380-6 [DOI] [PubMed] [Google Scholar]
- 13.Kim A, Schweighofer N, Finley JM. Locomotor skill acquisition in virtual reality shows sustained transfer to the real world. J Neuroeng Rehabil. 2019 Sep 14;16(1):113. doi: 10.1186/s12984-019-0584-y. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-019-0584-y .10.1186/s12984-019-0584-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pompeu JE, Mendes FADS, Silva KGD, Lobo AM, Oliveira TDP, Zomignani AP, Piemonte MEP. Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson's disease: a randomised clinical trial. Physiotherapy. 2012 Sep;98(3):196–204. doi: 10.1016/j.physio.2012.06.004.S0031-9406(12)00062-4 [DOI] [PubMed] [Google Scholar]
- 15.Lloréns R, Noé E, Colomer C, Alcañiz M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2015 Mar;96(3):418–425. doi: 10.1016/j.apmr.2014.10.019.S0003-9993(14)01220-9 [DOI] [PubMed] [Google Scholar]
- 16.Cai D, Zeng Q, He L, Huang G. Application and mechanism of virtual reality technology in post-stroke rehabilitation of the hemiplegic upper limb. Chin J Tissue Eng Res. 2020;24(32):5228–5235. doi: 10.3969/j.issn.2095-4344.2872. [DOI] [Google Scholar]
- 17.van Nimwegen M, Speelman AD, Hofman-van Rossum EJM, Overeem S, Deeg DJH, Borm GF, van der Horst MHL, Bloem BR, Munneke M. Physical inactivity in Parkinson's disease. J Neurol. 2011 Dec;258(12):2214–2221. doi: 10.1007/s00415-011-6097-7. http://europepmc.org/abstract/MED/21614433 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen Y, Gao Q, He C, Bian R. Effect of virtual reality on balance in individuals with Parkinson disease: a systematic review and meta-analysis of randomized controlled trials. Phys Ther. 2020 Jun 23;100(6):933–945. doi: 10.1093/ptj/pzaa042.5802008 [DOI] [PubMed] [Google Scholar]
- 19.Triegaardt J, Han TS, Sada C, Sharma S, Sharma P. The role of virtual reality on outcomes in rehabilitation of Parkinson's disease: meta-analysis and systematic review in 1031 participants. Neurol Sci. 2020 Mar 06;41(3):529–536. doi: 10.1007/s10072-019-04144-3. http://europepmc.org/abstract/MED/31808000 .10.1007/s10072-019-04144-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dockx K, Bekkers EM, Van den Bergh V, Ginis P, Rochester L, Hausdorff JM, Mirelman A, Nieuwboer A. Virtual reality for rehabilitation in Parkinson's disease. Cochrane Database Syst Rev. 2016 Dec 21;12:CD010760. doi: 10.1002/14651858.CD010760.pub2. http://europepmc.org/abstract/MED/28000926 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015 Jan 02;350:g7647. doi: 10.1136/bmj.g7647. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=25555855 . [DOI] [PubMed] [Google Scholar]
- 22.Casuso-Holgado MJ, Martín-Valero R, Carazo AF, Medrano-Sánchez E, Cortés-Vega M, Montero-Bancalero FJ. Effectiveness of virtual reality training for balance and gait rehabilitation in people with multiple sclerosis: a systematic review and meta-analysis. Clin Rehabil. 2018 Sep 13;32(9):1220–1234. doi: 10.1177/0269215518768084. [DOI] [PubMed] [Google Scholar]
- 23.Lei C, Sunzi K, Dai F, Liu X, Wang Y, Zhang B, He L, Ju M. Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson's disease: a systematic review. PLoS One. 2019 Nov 7;14(11):e0224819. doi: 10.1371/journal.pone.0224819. https://dx.plos.org/10.1371/journal.pone.0224819 .PONE-D-19-10618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maggio MG, Russo M, Cuzzola MF, Destro M, La Rosa G, Molonia F, Bramanti P, Lombardo G, De Luca R, Calabrò R. Virtual reality in multiple sclerosis rehabilitation: a review on cognitive and motor outcomes. J Clin Neurosci. 2019 Jul;65:106–111. doi: 10.1016/j.jocn.2019.03.017.S0967-5868(19)30185-7 [DOI] [PubMed] [Google Scholar]
- 25.Massetti T, Trevizan IL, Arab C, Favero FM, Ribeiro-Papa DC, de Mello Monteiro CB. Virtual reality in multiple sclerosis: a systematic review. Mult Scler Relat Disord. 2016 Jul;8:107–112. doi: 10.1016/j.msard.2016.05.014.S2211-0348(16)30075-X [DOI] [PubMed] [Google Scholar]
- 26.Pickenbrock HM, Diel A, Zapf A. A comparison between the Static Balance Test and the Berg Balance Scale: validity, reliability, and comparative resource use. Clin Rehabil. 2016 Mar 23;30(3):288–293. doi: 10.1177/0269215515578297.0269215515578297 [DOI] [PubMed] [Google Scholar]
- 27.Lesinski M, Hortobágyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of balance training on balance performance in healthy older adults: a systematic review and meta-analysis. Sports Med. 2015 Dec 1;45(12):1721–1738. doi: 10.1007/s40279-015-0375-y. http://europepmc.org/abstract/MED/26325622 .10.1007/s40279-015-0375-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Albanese E, Bütikofer L, Armijo-Olivo S, Ha C, Egger M. Construct validity of the Physiotherapy Evidence Database (PEDro) quality scale for randomized trials: item response theory and factor analyses. Res Synth Methods. 2020 Mar 05;11(2):227–236. doi: 10.1002/jrsm.1385. http://europepmc.org/abstract/MED/31733091 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muller K. Statistical Power Analysis for the Behavioral Sciences. Technometrics. 1989 Nov;31(4):499–500. doi: 10.1080/00401706.1989.10488618. [DOI] [Google Scholar]
- 30.Herbert R, Moseley A, Sherrington C. PEDro: a database of randomised controlled trials in physiotherapy. Health Inf Manag. 2016 Sep 09;28(4):186–188. doi: 10.1177/183335839902800410. [DOI] [PubMed] [Google Scholar]
- 31.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep 6;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. http://europepmc.org/abstract/MED/12958120 .327/7414/557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000 Jun;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 33.Chen S, Liu J, Li S. Effects of virtual reality technology on balance function in patients with Parkinson's disease. Theory Pract Rehab China. 2017;23:1091–1095. doi: 10.3969/j.issn.1006-9771.2017.09.021. [DOI] [Google Scholar]
- 34.van den Heuvel MR, Kwakkel G, Beek PJ, Berendse HW, Daffertshofer A, van Wegen EE. Effects of augmented visual feedback during balance training in Parkinson's disease: a pilot randomized clinical trial. Parkinsonism Relat Disord. 2014 Dec;20(12):1352–1358. doi: 10.1016/j.parkreldis.2014.09.022. https://linkinghub.elsevier.com/retrieve/pii/S1353-8020(14)00359-9 .S1353-8020(14)00359-9 [DOI] [PubMed] [Google Scholar]
- 35.Pompeu JE, Mendes FADS, Silva KGD, Lobo AM, Oliveira TDP, Zomignani AP, Piemonte MEP. Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson's disease: a randomised clinical trial. Physiotherapy. 2012 Sep;98(3):196–204. doi: 10.1016/j.physio.2012.06.004.S0031-9406(12)00062-4 [DOI] [PubMed] [Google Scholar]
- 36.Yang W, Wang H, Wu R, Lo C, Lin K. Home-based virtual reality balance training and conventional balance training in Parkinson's disease: a randomized controlled trial. J Formos Med Assoc. 2016 Sep;115(9):734–743. doi: 10.1016/j.jfma.2015.07.012. https://linkinghub.elsevier.com/retrieve/pii/S0929-6646(15)00249-1 .S0929-6646(15)00249-1 [DOI] [PubMed] [Google Scholar]
- 37.Lee N, Lee D, Song H. Effect of virtual reality dance exercise on the balance, activities of daily living, and depressive disorder status of Parkinson's disease patients. J Phys Ther Sci. 2015 Jan;27(1):145–147. doi: 10.1589/jpts.27.145. http://europepmc.org/abstract/MED/25642060 .jpts-2014-407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gandolfi M, Geroin C, Dimitrova E, Boldrini P, Waldner A, Bonadiman S, Picelli A, Regazzo S, Stirbu E, Primon D, Bosello C, Gravina AR, Peron L, Trevisan M, Garcia AC, Menel A, Bloccari L, Valè N, Saltuari L, Tinazzi M, Smania N. Virtual reality telerehabilitation for postural instability in Parkinson's disease: a multicenter, single-blind, randomized, controlled trial. Biomed Res Int. 2017:7962826. doi: 10.1155/2017/7962826. doi: 10.1155/2017/7962826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Santos P, Machado T, Santos L, Ribeiro N, Melo A. Efficacy of the Nintendo Wii combination with conventional exercises in the rehabilitation of individuals with Parkinson's disease: a randomized clinical trial. NeuroRehabilitation. 2019;45(2):255–263. doi: 10.3233/NRE-192771.NRE192771 [DOI] [PubMed] [Google Scholar]
- 40.Özgönenel L, Çağırıcı S, Çabalar M, Durmuşoğlu G. Use of game console for rehabilitation of Parkinson's Disease. Balkan Med J. 2016 Jul 01;33(4):396–400. doi: 10.5152/balkanmedj.2016.16842. doi: 10.5152/balkanmedj.2016.16842.bmj-33-4-396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shih M, Wang R, Cheng S, Yang Y. Effects of a balance-based exergaming intervention using the Kinect sensor on posture stability in individuals with Parkinson's disease: a single-blinded randomized controlled trial. J Neuroeng Rehabil. 2016 Aug 27;13(1):78. doi: 10.1186/s12984-016-0185-y. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-016-0185-y .10.1186/s12984-016-0185-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Feng H, Li C, Liu J, Wang L, Ma J, Li G, Gan L, Shang X, Wu Z. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: a randomized controlled trial. Med Sci Monit. 2019 Jun 05;25:4186–4192. doi: 10.12659/msm.916455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ribas CG, Alves da Silva L, Corrêa MR, Teive HG, Valderramas S. Effectiveness of exergaming in improving functional balance, fatigue and quality of life in Parkinson's disease: a pilot randomized controlled trial. Parkinsonism Relat Disord. 2017 May;38:13–18. doi: 10.1016/j.parkreldis.2017.02.006.S1353-8020(17)30039-1 [DOI] [PubMed] [Google Scholar]
- 44.Shen X, Mak MKY. Balance and gait training with augmented feedback improves balance confidence in people with Parkinson's disease: a randomized controlled trial. Neurorehabil Neural Repair. 2014 Jul 09;28(6):524–535. doi: 10.1177/1545968313517752.1545968313517752 [DOI] [PubMed] [Google Scholar]
- 45.Liu J, Yan Z. Effect of virtual reality technology on the rehabilitation of balance function in patients with Parkinson's disease. Chin J Rehab Med. 2020;35(6):682–687. doi: 10.3969/j.issn.1001-1242.2020.06.007. [DOI] [Google Scholar]
- 46.Sun L, Chen R. Effects of virtual reality balance games combined with muscle strength training on balance function and motor ability in patients with Parkinson's disease. J Hainan Med Univ. 2020;26(9):655–663. doi: 10.13210/j.cnki.jhmu.20200304.007. [DOI] [Google Scholar]
- 47.Cheng Y, Yu Y, Liang S. Effects of virtual reality combined with rehabilitation training on balance function in patients with Parkinson's disease. Med Rev. 2019;25:4325–4329. doi: 10.3969/j.issn.1006-2084.2019.21.032. [DOI] [Google Scholar]
- 48.Lin C, Chen A, Jiang Y. Effect of virtual reality balance game training on balance function in patients with Parkinson's disease. Theory Pract Rehab China. 2016;22:1059–1063. doi: 10.3390/electronics10091003. [DOI] [Google Scholar]
- 49.Tollár J, Nagy F, Hortobágyi T. Vastly different exercise programs similarly improve parkinsonian symptoms: a randomized clinical trial. Gerontology. 2019;65(2):120–127. doi: 10.1159/000493127.000493127 [DOI] [PubMed] [Google Scholar]
- 50.Griffin HJ, Greenlaw R, Limousin P, Bhatia K, Quinn NP, Jahanshahi M. The effect of real and virtual visual cues on walking in Parkinson's disease. J Neurol. 2011 Jun 9;258(6):991–1000. doi: 10.1007/s00415-010-5866-z. [DOI] [PubMed] [Google Scholar]
- 51.Praamstra P, Stegeman DF, Cools AR, Horstink MW. Reliance on external cues for movement initiation in Parkinson's disease. Evidence from movement-related potentials. Brain. 1998 Jan;121 (Pt 1):167–177. doi: 10.1093/brain/121.1.167. [DOI] [PubMed] [Google Scholar]
- 52.Barry G, Galna B, Rochester L. The role of exergaming in Parkinson's disease rehabilitation: a systematic review of the evidence. J Neuroeng Rehabil. 2014 Mar 07;11(1):33. doi: 10.1186/1743-0003-11-33. https://jneuroengrehab.biomedcentral.com/articles/10.1186/1743-0003-11-33 .1743-0003-11-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tinazzi M, Geroin C, Gandolfi M, Smania N, Tamburin S, Morgante F, Fasano A. Pisa syndrome in Parkinson's disease: an integrated approach from pathophysiology to management. Mov Disord. 2016 Dec 25;31(12):1785–1795. doi: 10.1002/mds.26829. [DOI] [PubMed] [Google Scholar]
- 54.Basso Moro S, Bisconti S, Muthalib M, Spezialetti M, Cutini S, Ferrari M, Placidi G, Quaresima V. A semi-immersive virtual reality incremental swing balance task activates prefrontal cortex: a functional near-infrared spectroscopy study. Neuroimage. 2014 Jan 15;85 Pt 1:451–460. doi: 10.1016/j.neuroimage.2013.05.031.S1053-8119(13)00525-9 [DOI] [PubMed] [Google Scholar]
- 55.Pompeu JE, Mendes FADS, Silva KGD, Lobo AM, Oliveira TDP, Zomignani AP, Piemonte MEP. Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson's disease: a randomised clinical trial. Physiotherapy. 2012 Sep;98(3):196–204. doi: 10.1016/j.physio.2012.06.004.S0031-9406(12)00062-4 [DOI] [PubMed] [Google Scholar]
- 56.Baltaci G, Harput G, Haksever B, Ulusoy B, Ozer H. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2013 Apr 29;21(4):880–887. doi: 10.1007/s00167-012-2034-2. [DOI] [PubMed] [Google Scholar]
- 57.Taube W, Gruber M, Beck S, Faist M, Gollhofer A, Schubert M. Cortical and spinal adaptations induced by balance training: correlation between stance stability and corticospinal activation. Acta Physiol (Oxf) 2007 Apr;189(4):347–358. doi: 10.1111/j.1748-1716.2007.01665.x.APS1665 [DOI] [PubMed] [Google Scholar]
- 58.Meldrum D, Glennon A, Herdman S, Murray D, McConn-Walsh R. Virtual reality rehabilitation of balance: assessment of the usability of the Nintendo Wii(®) Fit Plus. Disabil Rehabil Assist Technol. 2012 May 25;7(3):205–210. doi: 10.3109/17483107.2011.616922. [DOI] [PubMed] [Google Scholar]


