Abstract
Background
The distal tibial metaphysis is located in the lower (distal) part of the tibia (shin bone). Fractures of this part of the tibia are most commonly due to a high energy injury in young men and to osteoporosis in older women. The optimal methods of surgical intervention for a distal tibial metaphyseal fracture remain uncertain.
Objectives
To assess the effects (benefits and harms) of surgical interventions for distal tibial metaphyseal fractures in adults. We planned to compare surgical versus non‐surgical (conservative) treatment, and different methods of surgical intervention.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (9 December 2014), the Cochrane Central Register of Controlled Trials (2014, Issue 12), MEDLINE (1946 to November Week 3 2014), EMBASE (1980 to 2014 Week 48), the Airiti Library (1967 to 2014 Week 8), China Knowledge Resource Integrated Database (1915 to 2014 Week 8), ClinicalTrials.gov (February 2014) and reference lists of included studies.
Selection criteria
We included randomised and quasi‐randomised controlled clinical studies comparing surgical versus non‐surgical (conservative) treatment or different surgical interventions for treating distal tibial metaphyseal fractures in adults. Our primary outcomes were patient‐reported function and the need for secondary or revision surgery or substantive physiotherapy because of adverse outcomes.
Data collection and analysis
Two authors independently selected studies, assessed the risk of bias in each study and extracted data. We resolved disagreement by discussion and, where necessary, in consultation with a third author. Where appropriate we pooled data using the fixed‐effect model.
Main results
We included three randomised trials that evaluated intramedullary nailing versus plating in 213 participants, with useable data from 173 participants of whom 112 were male. The mean age of participants in individual studies ranged from 41 to 44 years. There were no trials comparing surgery with non‐surgical treatment. The three included trials were at high risk of performance bias, with one trial also being at high risk of selection, detection and attrition bias. Overall, the quality of available evidence was rated as very low for all outcomes, meaning that we are very unsure about the estimates for all outcomes.
Although the pooled results of three different measures of foot and ankle function indicated a small difference in favour of nailing (standard mean difference 0.28, 95% CI ‐0.02 to 0.59; 172 participants, 3 trials), the results of individual trials indicated that this was very unlikely to be a clinically important difference. Pooled data (173 participants, 3 trials) for the need for reoperation or substantive physiotherapy for adverse events favoured nailing (4/90 versus 10/83; RR 0.37, 95% CI 0.12 to 1.12), but included the possibility of a better outcome after plating. Based on an illustrative risk of 100 re‐operations for adverse outcomes within one year of plate fixation in 1000 people with these fractures, 63 fewer (95% CI 88 fewer to 12 more) people per 1000 would have re‐operations after nailing. Similarly pooled data (173 participants, 3 trials) for the symptomatic nonunion or malunion, wound complications and fracture union favoured nailing but the 95% confidence intervals crossed the line of no effect and thus included the possibility of a better outcome after plating. Evidence from one trial (85 participants) showed no clinically important difference in pain between the two groups.
Authors' conclusions
Overall, there is either no or insufficient evidence to draw definitive conclusions on the use of surgery or the best surgical intervention for distal tibial metaphyseal fractures in adults. The available evidence, which is of very low quality, found no clinically important differences in function or pain, and did not confirm a difference in the need for re‐operation or risk of complications between nailing and plating.
The addition of evidence from two ongoing trials of nailing versus plating should inform this question in future updates. Further randomised trials are warranted on other issues, but should be preceded by research to identify priority questions.
Keywords: Adult; Female; Humans; Male; Bone Plates; Epiphyses; Epiphyses/injuries; Epiphyses/surgery; Fracture Fixation, Intramedullary; Fracture Fixation, Intramedullary/adverse effects; Fracture Fixation, Intramedullary/methods; Randomized Controlled Trials as Topic; Reoperation; Reoperation/statistics & numerical data; Tibial Fractures; Tibial Fractures/surgery
Plain language summary
Surgical interventions for treating distal tibial fractures (breaks of the lower end of the shin bone) in adults
Background
Breaks in the lower (distal) end of the shin bone (or tibia) are mostly caused by high‐energy trauma, such as motor vehicle accidents. We set out to compare surgical treatment (such as putting the broken parts back into position and fixing these either by inserting a metal nail into the central cavity of the bone (nailing) or with a metal plate and securing it to the bone using screws (plating)) with non‐surgical treatment (plaster cast immobilisation). We also set out to compare different methods of surgery such as nailing versus plating.
Study characteristics
We searched medical databases and trials registries in December 2014. We wanted to include studies in which receiving one surgical treatment or another surgical treatment was decided by chance. This research method, termed a randomised controlled trial (RCT), is the best way to ensure that any measured improvement is caused by the treatment itself and no other factors. We found three RCTs involving 213 adults (with results available from 173) that compared nailing versus plating for treating distal tibial fractures. Overall the studies included around twice as many males as females and the average age of the study participants was just over 40 years. We found no trials comparing surgery with non‐surgical treatment.
Key results
We found no clear differences between the nailing and plating groups in terms of patient‐reported functional outcomes, re‐operations for adverse outcomes, troublesome non‐healing of the bone or deformity, pain, wound problems such as infection, or the numbers of individuals with healed fractures.
Quality of the evidence
Only three trials were identified and the sample sizes were small, so the results are imprecise. Moreover, the results of one trial were very likely to be biased due to flawed methodology. We therefore judged the overall quality of evidence to be very low, which means that we are very unsure of these results.
Conclusions
Overall, the evidence is of very low quality and is insufficient to draw definite conclusions about the best method of surgery, including nailing versus plating, for treating breaks of the lower end of the shin bone in adults. Future updates of this review are likely to include evidence from currently ongoing research comparing nailing versus plating. Although other RCTs are needed to address key clinical questions on surgical methods for treating these fractures, these studies should be preceded by research to determine which questions should be prioritised.
Summary of findings
Summary of findings for the main comparison. Summary of findings: Surgical interventions for treating distal tibial metaphyseal fractures in adults.
| Surgical interventions for treating distal tibial metaphyseal fractures in adults | ||||||
|
Population: individuals more than 18 years old with distal tibial metaphyseal fractures Settings: hospitals (all linked with a university) Intervention: intramedullary nailing Comparison: plating | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Plating | Intramedullary nailing | |||||
|
Patient‐reported functional outcomes (pooled data)1 1. AOFAS score at 1 year 2. OMAS percentage of normal side at 2 years 3. OMAS score at 1 year |
See comment | See comment | SMD 0.28 (‐0.02 to 0.59) |
172 (3 trials) |
⊕⊝⊝⊝ very low2 |
0.2 SD represents a small difference, 0.5 SD a moderate difference and 0.8 SD a large difference. However, this does not mean that the 95% CI includes a clinically important effect. The separate results of two trials (87% of the data) showed no clinically important differences. Only the point estimate and wide CI of the third trial included the possibility of a clinically important effect.3 |
|
Need for a secondary/revision operation or substantive physiotherapy for adverse outcomes (e.g. non‐union, malunion or infection) 1 year |
100 per 10004 | 37 per 1000 (12 to 112) |
RR 0.37 (0.12 to 1.12) |
173 (3 trials) | ⊕⊝⊝⊝ very low5 |
|
|
Symptomatic non‐union or malunion, including limping 1 year |
67 per 10004 | 49 per 1000 (12 to 188) | RR 0.72 (0.18 to 2.80) | 173 (3 trials) | ⊕⊝⊝⊝ very low6 |
|
|
Pain
(0 to 40: no pain) 1 year |
The mean pain score in the plating group was 31.5 points | The mean pain score in the nailing group was 1.00 higher (0.63 lower to 0.76 higher) | MD 1.00 (‐0.63 to 2.63) | 85 (1 trial) |
⊕⊝⊝⊝ very low7 |
The CI is unlikely to include a minimal clinically important difference. Higher scores were better |
|
Wound complications including superficial/deep wound infection and osteomyelitis 1 year |
147 per 1000 | 70 per 1000 (30 to 162) | RR 0.47 (0.20 to 1.10) | 173 (3 trials) | ⊕⊝⊝⊝ very low8 |
|
|
Fracture union 1 year |
934 per 1000 | 953 per 1000 (888 to 1000) |
RR 1.02 (0.95 to 1.09) |
173 (3 trials) | ⊕⊝⊝⊝ very low9 |
|
| *The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AOFAS: American Orthopaedic Foot and Ankle Surgery score; CI: confidence interval; MD: mean difference; OMAS: Olerud and Molander Ankle Functional Score; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
1. Functional data were presented as AOFAS data in one trial, and OMAS data in the other two trials but in different ways, as described.
2. The evidence was downgraded two levels for study limitations in design and implementation (all three trials were at high risk of bias, including performance bias) and one level for inconsistency (mainly reflecting pooling of disparate outcome measures and timing of measurement).
3. Individual trial results:
a. AOFAS score (0 (worst) to 100 (best)) at 12 months: MD 2.20 favouring nailing, 95% CI ‐0.97 to 5.37; 85 participants b. OMAS percentage of normal side at 24 months: MD 0.30, 95% CI ‐1.27 to 1.87; 64 participants c. OMAS score (0 (worst) to 100 (best)) at 12 months: MD 15.80, 95% CI 0.80 to 30.80; 23 participants.
4. The basis for the assumed risk was the median plating group risk across studies.
5. The evidence was downgraded one level for study limitations in design and implementation (all three trials were at high risk of bias, in particular performance bias), one level for inconsistency (Chi² = 2.17, df = 1 (P value = 0.14); I² = 54%), and one for imprecision (wide CIs and small numbers).
6. The evidence was downgraded one level for study limitations in design and implementation (all three trials were at high risk of bias, in particular performance bias) and two levels for serious imprecision (wide CIs and small numbers).
7. The evidence was downgraded two levels for study limitations in design and implementation (the trial was at high risk of selection, performance, detection and attrition biases) and one level for imprecision (wide CI and small numbers).
8. The evidence was downgraded two levels for study limitations in design and implementation (all three trials were at high risk of bias, in particular performance bias) and one level for inconsistency (Chi² = 4.55, df = 2 (P value = 0.10); I² = 56%).
7. The evidence was downgraded one level for study limitations in design and implementation (all three trials were at high risk of bias, in particular performance bias) and two levels for serious imprecision (there were few cases of non‐union; if these had been pooled instead the result would have been 3/90 versus 4/83; RR 0.72, 95% CI 0.18 to 2.80).
Background
Description of the condition
The lower (distal) end of the tibia (shin bone) of the lower leg articulates with the distal fibula (the other bone of the lower leg) and talus (the ankle bone) to form the ankle joint. An epidemiological study of fractures in adults showed that distal tibial fractures comprised 0.7% of all fractures with an annual incidence of 7.9 per 10,000 adults presenting to the Edinburgh Royal Infirmary in 2000 (Court‐Brown 2006). These fractures are more common in young adults, usually males, but are becoming more common in older females. Court‐Brown 2006 reported a male to female ratio of 57 to 43. In younger adults, the most common cause is high‐energy trauma such as a motor vehicle accident or sports injury (Court‐Brown 1995; Court‐Brown 2005). Fractures in older adults often result from low‐energy trauma, such as falls from standing height, which reflects underlying osteopenia and osteoporosis (Court‐Brown 2005; Court‐Brown 2006). The frequency of high‐energy trauma and the relatively thin muscle coverage of the tibia increases the risk of an open fracture. The sparse muscle cover also makes fracture management more difficult. As with tibial fractures in general, these fractures and related complications, including non‐union and infection, can lead to employment loss and other socioeconomic problems (Court‐Brown 2005).
The distal tibia metaphysis is located in the distal part of the tibia. It lies above the plafond, which is the part of the tibia that articulates with the fibula and talus to form the ankle joint. Müller 1990 defined the distal tibial metaphysis by constructing a square, with the sides of length defined by the widest portion of the tibial plafond. Extra‐articular fractures of the distal tibia correspond to type 43A according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification (AO/OTA 1996). The mechanism of injury and the prognosis of these fractures differ from those of pilon fractures, which are intra‐articular fractures involving the plafond (Mast 1988; Ovadia 1986). Additionally, the proximity of the fracture to the ankle joint makes it technically demanding to achieve acceptable alignment and stable fixation using intramedullary nails, the most commonly used surgical technique for tibial shaft or diaphyseal fractures (Robinson 1995). Further, the subcutaneous and relatively exposed position of the metaphysis means that fractures in the distal tibia metaphysis, even following low‐energy trauma, usually have more severe soft tissue injury than reported for fractures of the tibia diaphysis (Court‐Brown 1990). Thus, the distal metaphysis is distinct from the diaphysis and a separate review of surgical interventions for treating distal tibia metaphyseal fractures is warranted.
Description of the intervention
Generally, undisplaced fractures are treated non‐surgically, whereas most displaced or unstable fractures are treated surgically because of the risk of malunion or non‐union. Most surgeons regard displacement as angulation of more than 5 degrees, shortening greater than 1 cm and rotation greater than 10 degrees (Petrisor 2010). Non‐surgical or conservative treatment of displaced fractures generally comprises closed reduction (realignment of bone fragment without making an incision in the skin) and plaster cast immobilisation. Several surgical methods are available. Intramedullary nailing consists of a metal rod, inserted from the upper tibia into the inner cavity of the tibia, which is typically locked into place with screws. Plating is another treatment option. Traditionally, this required extensive exposure of the soft tissues to reduce (reposition) the fracture fragment(s) before fixation with plates. Minimally invasive percutaneous osteosynthesis (MIPO) is an alternative surgical method that causes less damage to tissue. Nowadays, precontoured locking plates are available, which are thinner, fit more closely to the bone and provide stronger support than traditional plates. External fixation is another alternative, especially for excessive soft tissue injury or comminuted fractures. Sometimes, two treatment methods may be used in combination; for example, nailing combined with plating.
How the intervention might work
Non‐operative treatments for distal tibial fractures can lead to unfavourable results such as unacceptable deformity, shortening, rotation malunion and ankle stiffness (Digby 1982; Haines 1984). However, all methods of surgical fixation carry the risk of additional complications, including general complications from the operation itself.
The advantages of intramedullary nailing include the preservation of the soft tissue sleeve around the fracture site and the potential for early mobilisation of the adjacent joints (Whittle 2008). While intramedullary nails have become the mainstay for tibial diaphyseal fractures, there is a potential risk of propagation of the fracture into the ankle joint when introducing implants, and greater difficulties in aligning the distal fragment, which could lead to malalignment and malunion (Mosheiff 1999; Robinson 1995). Knee pain is also sometimes noted after nailing (Court‐Brown 1997; Toivanen 2002).
Plating could provide improved alignment but has the disadvantages of wound complications, infection, implant prominence because of inadequate soft tissue coverage, and increased violation of soft tissue and blood supply during surgery (Borelli 2002; Im 2005; Obremskey 2004). With the evolution of implants, newly designed precontoured locking plates provide another treatment option for adult distal metaphyseal fractures. Combined with the MIPO technique, locking plates may provide greater biomechanical strength than conventional plates, and better reduction of the fracture with less violation of the soft tissue and periosteum (Ahmad 2010; Collinge 2010; Hasenboehler 2007; Redfern 2004). Because compression of the plate onto the bone is unnecessary, the periosteal blood supply and fracture hematoma are preserved, which enhances fracture healing (Wagner 2003).
External fixation is another treatment, often favoured for open fractures, excessive soft tissue injury or comminuted fractures (Court‐Brown 2005). However, problems such as insufficient reduction, malunion, joint motion restriction and pin tract infections are frequently encountered (Babis 1997; Blauth 2001; Court‐Brown 2005).
Why it is important to do this review
While relatively uncommon, distal tibial metaphyseal fractures are serious and clinically distinct injuries that may result in severe disability and are frequently treated surgically. A variety of surgical interventions are available but it is unclear which is the best method. A previous systematic review investigating the treatment of distal tibia fracture without articular involvement (Zelle 2006), which found no evidence from randomised controlled trials (RCTs), concluded that the optimal treatment for these fractures "remains controversial". Given this uncertainty and that RCTs have been conducted since the publication of this article, a review of the currently available best evidence is warranted in order to provide orthopaedic surgeons and individuals with such a fracture with a useful reference to inform their decision‐making about the treatment of distal tibial metaphyseal fractures in adults.
Objectives
To assess the effects (benefits and harms) of surgical interventions for distal tibial metaphyseal fractures in adults.
We planned to compare surgical versus non‐surgical (conservative) treatment, and different methods of surgical intervention.
Methods
Criteria for considering studies for this review
Types of studies
RCTs and quasi‐RCTs (in which the method of allocating participants to a treatment is not strictly random, e.g. by date of birth, hospital record number or alternation) evaluating surgical interventions or comparing surgical versus non‐surgical interventions for treating distal tibial metaphyseal fractures in adults.
Types of participants
We included trials of skeletally mature people undergoing primary surgical fixation (surgical fixation of an acute fracture or early fixation following failure of conservative treatments, nominally within two weeks of injury) of fractures of the distal tibial metaphysis. While we accepted the definition and associated classification of the fracture as provided in trial reports, ideally the fractures should be entirely extra‐articular and in the distal metaphysis of the tibia (thus the fracture will be within 4 cm of the tibia plafond (Bedi 2006) or be assigned as type 43A according to the AO/OTA classification (AO/OTA 1996)).
Since articular injuries behave so differently, we excluded trials with a primary focus on people with intra‐articular (pilon) fractures or people with other fractures, except fibular fracture, affecting the same limb. We also excluded trials for which the primary focus was skeletally immature people; notably rigid intramedullary nailing cannot be performed in this group. Unless separate data for extra‐articular fractures could be obtained, we excluded articles reporting mixed populations of intra‐articular and extra‐articular fractures if more than 25% of the fractures involved the plafond.
Types of interventions
We included trials comparing surgery with conservative treatment and trials comparing different surgical interventions: either different categories of surgical intervention (e.g. intramedullary nailing, plating or external fixation) or different methods of performing an intervention in the same category (e.g. different types or methods of plating).
Types of outcome measures
Primary outcomes
Patient‐reported functional outcome, such as the American Orthopaedic Foot and Ankle Surgery (AOFAS) score (Kitaoka 1994) and the Olerud and Molander Ankle Functional Score (OMAS) (Olerud 1984)
Need for a secondary/revision operation or substantive physiotherapy for adverse outcomes (e.g. non‐union, malunion and infection)
Timing of primary outcome measurement
Where available, we extracted outcome data for short‐term follow‐up (up to six weeks following treatment); intermediate follow‐up (more than six weeks and up to six months after the end of treatment) and long‐term follow‐up (greater than six months after the end of treatment).
Secondary outcomes
Symptomatic non‐union or malunion, including limping
Pain
Wound complications, including superficial wound infections, deep wound infections and osteomyelitis
Bone healing outcomes, including the proportion of fractures that united (fracture union) and healing time
Surgical details, including operation time, radiation time and any type of intraoperative complication such as fracture propagation
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (9 December 2014), the Cochrane Central Register of Controlled Trials (CENTRAL; 2014, Issue 12), MEDLINE (1946 to November Week 3 2014), MEDLINE In‐Process & Other Non‐Indexed Citations (4 December 2014), EMBASE (1980 to 2014 Week 48), the Airiti Library (1967 to 2014 Week 8) and the China Knowledge Resource Integrated Database (CNKI) (1915 to 2014 week 8). We did not apply any language restrictions.
In MEDLINE, we combined the subject‐specific search strategy with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2011). The search strategies for The Cochrane Library, MEDLINE, EMBASE, Airiti Library and CNKI are listed in Appendix 1.
We also searched ClinicalTrials.gov (February 2014) for ongoing studies.
Searching other resources
We scanned the reference lists of included studies and relevant reviews. We contacted experts in this field and companies that manufacture intramedullary nails or plates for information on unpublished and ongoing studies.
Data collection and analysis
Selection of studies
We removed duplicate records of the search results. Two review authors (LTK and CHC) independently checked titles, abstracts and keywords from the searches to identify potentially eligible studies. The review authors were not blinded to the names of original researchers, journals or institutions. Upon obtaining the full texts of potentially eligible trials, the same two review authors performed independent study selection. We resolved disagreements by discussion and, where necessary, in consultation with a third review author (CCC).
Data extraction and management
Two review authors (LTK and CHC) independently extracted data from each trial, including trial methods, participants, interventions, outcomes and results, using a data extraction form. We resolved disagreements by discussion and, where necessary, in consultation with a third review author (CCC). One review author (LTK) entered the data into Review Manager software (RevMan 5.3; RevMan 2014), and another review author (CCC) rechecked the entered data.
Assessment of risk of bias in included studies
Two review authors (LTK and CHC) independently assessed each included trial for risk of bias using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2011). We resolved disagreements by discussion and, where necessary, by recourse to a third review author (CCC). We assessed the following:
random sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment (subjective (patient‐reported) outcomes; re‐operation and other objective outcomes);
incomplete outcome data (short‐term follow‐up; longer‐term follow‐up);
selective reporting (assessment dependent on availability of trial protocol);
other sources of bias: any other possible concerns about bias, such as major imbalances in baseline characteristics (e.g. age, open fractures, concomitant fibular fractures) and performance bias resulting in major differences in care programmes, including the treatment of concomitant fibular fractures, or experience with the interventions under investigation by the operating surgeons. Upon recommendation from editorial feedback at the review stage, we also considered sponsorship bias.
We judged each of the above domains as being at low risk of bias, high risk of bias or unclear risk of bias (indicating either lack of information or uncertainty over the potential for bias).
Measures of treatment effect
We expressed the treatment effects for dichotomous outcomes as risk ratios (RRs) and 95% confidence intervals (CIs). We expressed the treatment effects for continuous outcomes as mean differences (MDs) and 95% CIs for single studies or for two or more studies with comparable outcome measures. We used standardised mean differences (SMDs) and 95% CIs for data from disparate outcome measures. Where appropriate, we planned to express the dichotomous results as number needed to treat for an additional beneficial outcome (NNTB) and number needed to treat for an additional harmful outcome (NNTH) for outcomes where the RR was statistically significant.
Unit of analysis issues
We used the individual participant as the unit of analysis. For trials including bilateral fractures, we planned to follow the analytic methods stated in section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). However, we found no trials including bilateral fractures.
Dealing with missing data
Where necessary, we contacted trial researchers to request missing data. We planned to conduct intention‐to‐treat analyses to include all participants randomised where possible. If participant dropout led to missing data for dichotomous outcomes, we planned to conduct a sensitivity analysis where participants with missing data would be viewed as treatment failures and included in the analysis. We planned not to impute data for continuous outcomes for either missing participants or results; however, we planned to derive missing standard deviations where standard errors, 95% CIs, or exact P values were reported instead (Higgins 2011).
Assessment of heterogeneity
We assessed statistical heterogeneity by visual inspection of the forest plot (analysis) and the I² statistic (Higgins 2003). We assessed clinical heterogeneity arising from the interventions, participants and outcome measures. We undertook meta‐analyses if the I² statistic was less than 75%, and there was acceptable clinical homogeneity.
Assessment of reporting biases
We planned to investigate publication bias by using a funnel plot (Egger 1997) if at least 10 studies were available for meta‐analysis of a primary outcome. Had there been pooled data from a mixture of one very large trial and several small trials, we planned to explore the presence of small study bias in the overall meta‐analysis by checking if the random‐effects estimate of the intervention effect varied significantly from the fixed‐effect estimate.
Data synthesis
Where pooling was considered clinically appropriate, we initially pooled data using the fixed‐effect model. We planned to use the random‐effects model, especially if there was unexplained and substantial heterogeneity. Where it was not appropriate to pool data, we summarised the data for each trial in the text and tables.
Subgroup analysis and investigation of heterogeneity
Where sufficient data are available in future updates, we plan to explore the following potential sources of heterogeneity using subgroup analyses (Higgins 2004).
Open fracture versus closed fracture (different soft tissue injury)
Combined injury versus isolated injury (concurrent tibial and fibular fractures versus tibial fracture only)
Delayed surgery after conservative treatment versus surgery started immediately
Müller's definition versus other definitions of the distal tibia metaphysis
Different methods of the same category of surgery (e.g. MIPO versus open surgery for plate fixation; locked versus conventional (non‐locking) plate fixation).
We will investigate whether the results of subgroups are significantly different by inspecting the overlap of CIs and performing the test for subgroup differences available in RevMan.
Sensitivity analysis
If sufficient data had been available, we would have conducted sensitivity analyses to examine the effects of various aspects of trial and review methodology, including study susceptibility to selection and performance biases, the effects of missing data and the use of different models (fixed‐effect versus random‐effects for pooling data where there was heterogeneity). In future updates, we plan also to examine the effects of including trials that include intra‐articular fractures.
'Summary of findings' tables
We summarised the results for the only comparison investigated by the trials included in this review in a 'Summary of findings' table. We used the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach to assess the quality of evidence related to each primary outcome and the first four secondary outcomes listed in the section Types of outcome measures (Higgins 2011; section 12.2).
Results
Description of studies
See the Characteristics of included studies, Characteristics of excluded studies and Characteristics of ongoing studies tables.
Results of the search
We completed the search in December 2014 (see Figure 1). We screened a total of 910 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (11 records); CENTRAL (45), MEDLINE (149), EMBASE (211), Airiti Library (90), CNKI (402), ClinicalTrials.gov (2). We obtained one potentially eligible trial from a referee of this review.
1.
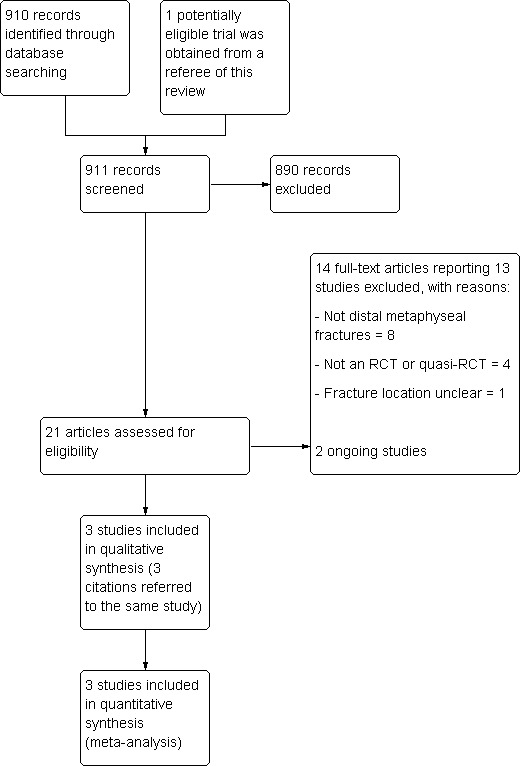
Study flow diagram
We identified 21 potentially eligible articles. Following study selection, we included three trials in the review: Guo 2010; Im 2005; and Mauffrey 2012 , which was reported in 3 articles. All three included studies were reported in English. We excluded 13 studies (Cheng 2011; Dai 2009; Hontzsch 2014 (2 articles); Li 2014; Liu 2014; Ristiniemi 2011; Shon 2012; Sun 2014; Vallier 2011; Vallier 2012; Yang 2006; Zou 2012; Zou 2013). We identified two ongoing studies (ISRCTN99771224; NCT01047826). No studies await classification.
Included studies
All three included studies compared two types of surgical devices for internal fixation. None compared surgical versus non‐surgical treatment. Details of the methods, participants, interventions and outcome measures of individual trials are provided in the Characteristics of included studies table.
Study design
All three studies were single‐centre RCTs with two parallel groups.
Setting
The included trials were conducted in single hospitals in China (Guo 2010), Korea (Im 2005) and the UK (Mauffrey 2012).
Participants
Guo 2010 randomised 111 participants and included 85 participants in the final analyses. Im 2005 randomised 78 participants and included 64 participants in the final analyses. Mauffrey 2012 randomised 24 participants and included all of them in the final analyses. In total, the three studies randomised 213 participants with 213 fractures, and 173 participants were included in the final analyses.
Of the 173 participants included in the final analyses, 112 were men and 61 were women. The mean age of participants in individual studies ranged from 41.1 (Im 2005) to 44.3 years (Guo 2010). The type of distal tibial metaphyseal fractures included was either closed fracture or Gustilo open type I fracture. Im 2005 included 51 closed fractures and 13 open fractures. The other two trials (Guo 2010; Mauffrey 2012) did not provide details of the number of open fractures. Two trials (Guo 2010; Im 2005) used the AO/OTA classification type 43 to define distal tibial metaphyseal fracture. Mauffrey 2012 defined distal tibial metaphysis as the area within two Müller squares of the ankle joint, in which the proximal and the distal segments of long bones were defined by a square whose sides had the same length as the widest part of the epiphysis (Müller 1990). Im 2005 additionally used the Tscherne classification (Oestern 1984) to assess the extent of the soft tissue injuries in closed fractures.
Interventions
One trial (Im 2005) compared intramedullary nailing versus plating with non‐locking screws, while the other two (Guo 2010; Mauffrey 2012) compared intramedullary nailing versus plating with fixed‐angle locking screws. Guo 2010 used the MIPO technique in all cases, whereas Mauffrey 2012 used MIPO only in some cases (the exact number was not reported).
Outcomes
The length of follow‐up ranged from one year in two trials (Guo 2010; Mauffrey 2012) to two years in Im 2005. All three trials recorded patient‐reported functional outcome. In terms of foot and ankle function scores, Guo 2010 reported the AOFAS score at 12 months after surgery, and Im 2005 and Mauffrey 2012 reported OMAS results. However, Im 2005 reported OMAS for the injured side as a percentage of the OMAS for the normal side at 24 months after surgery. Mauffrey 2012 reported OMAS at 3, 6 and 12 months after surgery. Mauffrey 2012 also recorded Disability Rating Index (DRI) scores and EuroQol EQ‐5D questionnaire and scale results at the same follow‐up times. All three trials provided details of secondary/revision operations, symptomatic non‐union/malunion, wound complications and fracture union; Guo 2010 and Im 2005 reported time to fracture union using the same criteria to determine union. Only Guo 2010 reported pain level at one year after surgery, using the pain component of the AOFAS score. Guo 2010 and Im 2005 provided data on operation time; Guo 2010 provided details of radiation time; and Im 2005 reported an intra‐operative complication.
Excluded studies
Thirteen studies were excluded for reasons stated in the Characteristics of excluded studies table. Four studies (Dai 2009; Ristiniemi 2011; Shon 2012; Yang 2006) were neither RCTs nor quasi‐RCTs. The other nine trials included either no or insufficient numbers of participants with distal tibial metaphyseal fractures: eight trials (Cheng 2011; Hontzsch 2014; Li 2014; Liu 2014; Sun 2014; Vallier 2012; Zou 2012; Zou 2013) primarily included individuals with distal diaphyseal fractures of the tibia, and one trial (Vallier 2011) included individuals with fractures 4 cm to 11 cm from the tibia plafond.
Ongoing studies
We found two ongoing studies on distal tibial metaphyseal fractures: ISRCTN99771224, which is comparing nailing with locking plate fixation, aims to recruit a minimum of 320 participants; and NCT01047826, which is comparing intramedullary nailing with plate fixation, aims to recruit 180 participants.
Risk of bias in included studies
We present 'Risk of bias' assessments for individual studies in 'Risk of bias' tables in the Characteristics of included studies and have summarised these assessments in Figure 2 and Figure 3.
2.
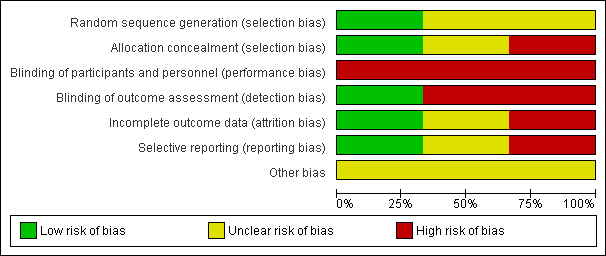
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
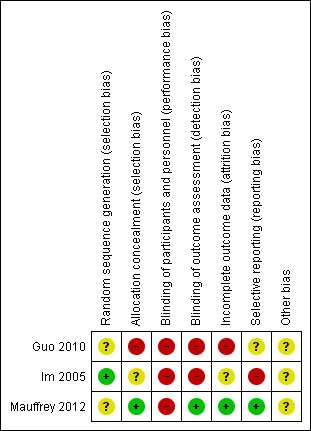
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study
Allocation
We judged Guo 2010, which described neither the method of random sequence generation nor allocation concealment, as being at unclear risk of bias relating to sequence generation and at high risk of bias relating to lack of allocation concealment. We judged Im 2005, which described drawing envelopes from a box, at low risk of bias relating to random sequence generation but at unclear risk of bias relating to lack of allocation concealment as there was no mention of safeguards. We judged Mauffrey 2012, which described a "pseudo‐random number sequence" as being at unclear risk of bias relating to random sequence generation but at low risk of bias relating to allocation concealment, reflecting the remote and independent administration of allocation.
Blinding
None of the three trials reported any details about blinding of participants and personnel. However, blinding of surgeons and participants in this condition is not possible since the surgical incisions in nailing and plating are very different and the metalwork is easily palpable. Thus, we judged the three trials to be at high risk of performance bias.
Guo 2010, where outcomes were assessed by doctors who were also involved in the treatment, we judged to be at high risk of detection bias. Im 2005 described outcome assessment at two years by "an independent physician". However, as this and other assessments (e.g. of complications) were not blinded, we judged this trial to be at high risk of detection bias. We judged Mauffrey 2012 to be at low risk of detection bias, reflecting the use of an outcome assessor who was blinded to treatment allocation.
Incomplete outcome data
In judging the risk of bias for this item, we considered a less than 80% completion rate in the treatment group to indicate a high risk of bias. We also assessed whether missing data were balanced between the two groups and whether an intention‐to‐treat analysis had been reported for the primary outcome. All three trials (Guo 2010; Im 2005; Mauffrey 2012) provided data on dropouts/loss to follow‐up and 23.4%, 15.3% and 8.3% participants, respectively, were excluded from the outcome analyses of these trials. We also judged Guo 2010 to be at high risk of attrition bias, reflecting contradictory statements in the report in terms of the post‐randomisation exclusion of participants whose fibular fracture had been fixed. We judged Im 2005 to be at unclear risk of attrition bias. Since the trialists of Mauffrey 2012 provided us with raw data, we judged the study to be at low risk of attrition bias.
Selective reporting
Neither trial registration documents nor protocols were available for any of the three trials. We obtained raw data from trialists of one study (Mauffrey 2012), which we thus judged as being at low risk of bias. We judged Guo 2010 as being at unclear risk of reporting bias and Im 2005 at high risk given the disparity between the methods and results in how OMAS data were reported.
Other potential sources of bias
While we considered Guo 2010 and Im 2005 to be at low risk of performance bias relating to surgeon experience and comparability of care programmes, there was an unclear risk of bias relating to a lack of data on baseline characteristics for all trial participants. The comparability of care programmes was not established in Mauffrey 2012, which we also judged to be at unclear risk of other bias because the mean age of the nailing group was older than that of the plating group. While the trial authors performed a linear regression analysis to adjust for the effects of age, only the adjusted data for DRI at six months of follow‐up were reported. In addition, while similar numbers in Im 2005 and Mauffrey 2012 underwent fixation of fibula fractures, we considered that any differences between groups in the decision to fix these fractures were a potential source of other bias. We found no evident sponsorship from manufacturers of intramedullary nails or plates.
Effects of interventions
See: Table 1
All three included trials compared intramedullary nailing versus plating (Guo 2010; Im 2005; Mauffrey 2012). There were no trials comparing surgery with non‐surgical treatment.
Intramedullary nailing versus plating
The three trials recruited a total of 213 participants and reported data for 173 participants at follow‐up. Due to the clinical heterogeneity across available trials and the lack of relevant data, we were unable to perform prespecified subgroup analyses, including of different methods of the same category of surgery.
Primary outcomes
Patient‐reported functional outcome
All three trials reported patient‐reported functional outcome relating to the ankle, but used different measures (Guo 2010: AOFAS scores at one year; Im 2005: OMAS, percentage of normal side at two years; Mauffrey 2012: OMAS scores at one year). Standard deviations were calculated from exact P values presented in Guo 2010 and Im 2005, and from individual participant data provided for Mauffrey 2012. Pooled data from these three trials were in favour of the nailing group (SMD 0.28, 95% CI ‐0.02 to 0.59; 172 participants; Analysis 1.1). Separate data for these outcomes and for DRI data (direction reversed in the Analysis to present a direction of benefit consistent with the other scores) reported for Mauffrey 2012 are shown in Analysis 1.2. It is notable that all results favour the nailing group, although all CIs cross the line of no effect, with the exception of those for OMAS at 12 months in Mauffrey 2012. Mauffrey 2012 reported that the minimal clinically important difference for the DRI is 8 points. Hence, although the effect size is less than 8 points, the wide CIs at all three time points for this outcome include the potential for a clinically important effect both in favour of nailing and, to a lesser extent, of plating (e.g. at 12 months, the MD was 3.90 in favour of nailing (95% CI ‐19.22 to 27.02)). Mauffrey 2012 also found no significant differences in the EQ‐5D scores between the two groups at all follow‐up times (data not presented).
1.1. Analysis.
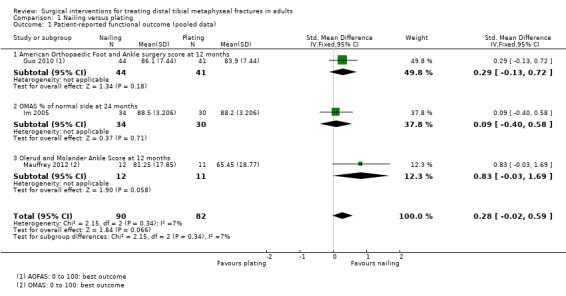
Comparison 1 Nailing versus plating, Outcome 1 Patient‐reported functional outcome (pooled data).
1.2. Analysis.
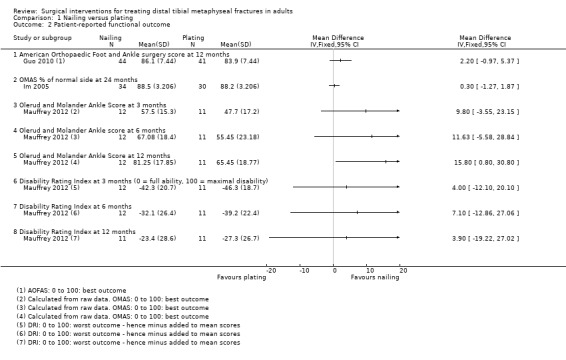
Comparison 1 Nailing versus plating, Outcome 2 Patient‐reported functional outcome.
Need for a secondary/revision operation or substantive physiotherapy for adverse outcomes (e.g. non‐union, malunion and infection)
Pooled data from the three trials showed a lower incidence in the nailing group than in the plating group of participants undergoing or waiting for a secondary operation for adverse outcomes (4/90 versus 10/83; RR 0.37 favouring nailing, 95% CI 0.12 to 1.12; 173 participants; Analysis 1.3). These data were moderately heterogeneous (Chi² = 2.17, df = 1 (P value = 0.14); I² = 54%). The details of the revision operations for each trial are listed in Table 2. Not included in Analysis 1.3 are fasciotomies performed for compartment syndrome in one participant in each group included in Mauffrey 2012; this is because it is unclear whether these participants had a subsequent complication. Notably, no secondary surgeries were performed in Guo 2010 during the 12‐month follow‐up period. However, similar numbers (23 in the nailing group versus 24 in the plating group) of participants had their implants removed after the end of follow‐up (mean 15.5 months). The main factors contributing to the decision for implant removal were prominence of the plate and pain. Guo 2010 observed that all nails were removed without difficulty, but that difficulties were encountered with the removal of locking screws in nine participants in the plating group.
1.3. Analysis.
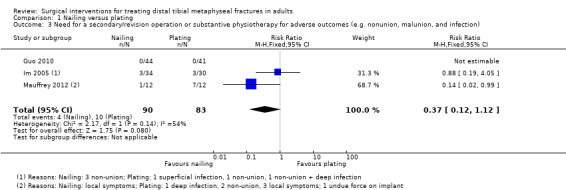
Comparison 1 Nailing versus plating, Outcome 3 Need for a secondary/revision operation or substantive physiotherapy for adverse outcomes (e.g. nonunion, malunion, and infection).
1. Details of secondary/revision surgery for complications.
| Trial ID | Group | Reasons for revision operation | Secondary procedures |
| Guo 2010 | None1 | None | |
| Im 2005 | Nailing | 3 non‐union | 2 exchange nailing and autogenous bone grafting; 1 bone grafting |
| Plating | 1 non‐union | 1 autogenous bone grafting | |
| 1 non‐union with deep infection | 1 plate removal and debridement, then change to external fixator, revision plate osteosynthesis after infection control |
||
| 1 superficial wound infection | 1 skin grafting | ||
| Mauffrey 2012 | Nailing | 1 hardware impingement | 1 removal of hardware |
| 1 compartment syndrome | 1 fasciectomy | ||
| Plating | 2 non‐union | 1 exchange nailing, 1 awaiting surgery | |
| 3 hardware impingement | 3 removal of hardware | ||
| 1 compartment syndrome | 1 fasciectomy | ||
| 1 deep infection | 1 debridement, antibiotics and plate removal upon fracture union |
1. 47 implants were removed (23 in the nail group versus 24 in the plate group) after end of follow‐up (mean 15.5 months). The main factors contributing to the decision for implant removal were prominence of the plate and pain.
Secondary outcomes
Symptomatic non‐union or malunion, including limping
Pooled data from the three trials (Guo 2010; Im 2005; Mauffrey 2012) showed no significant differences in symptomatic non‐union or malunion between the nailing and plating groups (3/90 versus 4/83; RR 0.72 favouring nailing, 95% CI 0.18 to 2.80; Analysis 1.4). Mauffrey 2012 reported that one participant in the nailing group had a malunion (10 degrees valgus) but did not mention whether this was symptomatic.
1.4. Analysis.
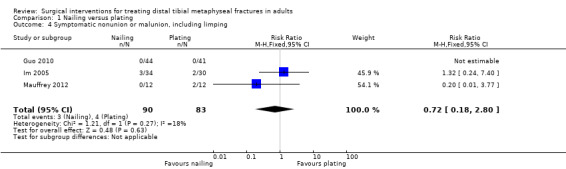
Comparison 1 Nailing versus plating, Outcome 4 Symptomatic nonunion or malunion, including limping.
Pain
Only Guo 2010 reported on pain (scale 0 to 40: highest score = no pain); however, this measure was part of the AOFAS score. Guo 2010 found little difference in pain between the nailing and plating groups at one year after operation (MD 1.00 favouring nailing, 95% CI ‐0.63 to 2.63; 85 participants; Analysis 1.5).
1.5. Analysis.
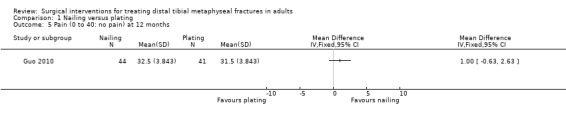
Comparison 1 Nailing versus plating, Outcome 5 Pain (0 to 40: no pain) at 12 months.
Wound complications including superficial wound infections, deep wound infections and osteomyelitis
Pooled data from the three trials (Guo 2010; Im 2005; Mauffrey 2012) showed a lower incidence of wound complications in the nailing group than in the plating group (7/90 versus 14/83; RR 0.47 favouring nailing, 95% CI 0.20 to 1.10; 173 participants; Analysis 1.6). Overall, 19 participants had a superficial wound infection, one of whom required a skin graft (Table 2), and two participants, both of whom had plating, had a deep infection requiring debridement and other treatment (Table 2). These data were moderately heterogeneous (Chi² = 4.55, df = 2 (P value = 0.10); I² = 56%) but no data on risk factors for wound complications such as open fractures and delayed surgery were available for subgroup analyses to explore this.
1.6. Analysis.
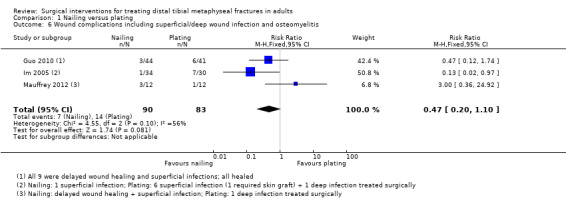
Comparison 1 Nailing versus plating, Outcome 6 Wound complications including superficial/deep wound infection and osteomyelitis.
Bone healing outcomes including fracture union and healing time
Pooled data from the three trials (Guo 2010; Im 2005; Mauffrey 2012) found no significant differences between the two intervention groups in the proportion of fractures that united (87/90 versus 79/83; RR 1.02 favouring nailing, 95% CI 0.95 to 1.09; Analysis 1.7). Pooled data from the two trials reporting on time to fracture union showed no significant differences between the two groups (MD 0.09 weeks, 95% ‐1.46 to 1.44 weeks; 149 participants; Analysis 1.8).
1.7. Analysis.
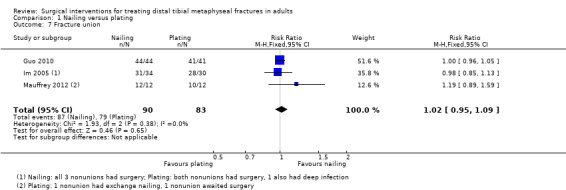
Comparison 1 Nailing versus plating, Outcome 7 Fracture union.
1.8. Analysis.
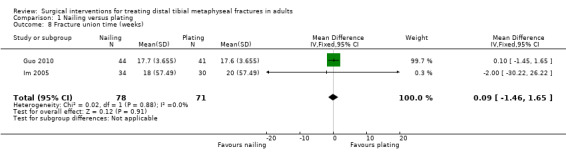
Comparison 1 Nailing versus plating, Outcome 8 Fracture union time (weeks).
Surgical details, including operation time, radiation time and any type of intraoperative complications
Pooled data from two trials (Guo 2010; Im 2005) showed a shorter mean operation time in the nailing group than in the plating group (81.23 minutes versus 97.90 minutes; MD ‐16.78 minutes favouring nailing, 95% CI ‐24.67 to ‐8.88 minutes; 149 participants; Analysis 1.9). Guo 2010 reported a shorter total radiation exposure time in the nailing group than in the plating group (2.2 minutes versus 3.0 minutes; MD ‐0.80 minutes, 95% CI ‐1.31 to ‐0.29 minutes; Analysis 1.10). Im 2005 also reported a case of intraoperative fracture comminution in the nailing group that needed further screw fixation.
1.9. Analysis.
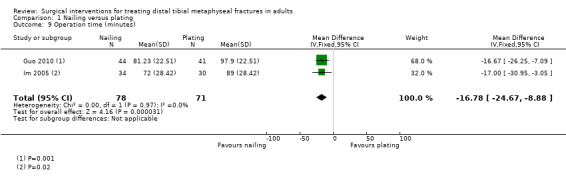
Comparison 1 Nailing versus plating, Outcome 9 Operation time (minutes).
1.10. Analysis.
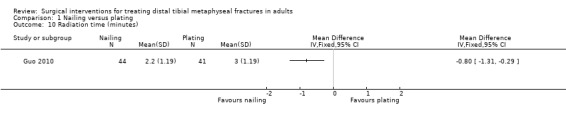
Comparison 1 Nailing versus plating, Outcome 10 Radiation time (minutes).
Discussion
Summary of main results
In this review, we included three RCTs that compared the effects of nailing versus plating in treating distal tibial metaphyseal fractures in adults. These trials provided outcome data for a maximum of 173 participants with 173 mainly closed fractures. We found no trials comparing surgery with non‐surgical treatment, or trials comparing other surgical methods. Overall, the quality of available evidence was rated as very low for all outcomes; this means that we are very uncertain about the estimates and that further research is very likely to have an important impact on the estimates of effect. A summary of the results of the comparison of nailing versus plating is presented in Table 1.
Although the pooled SMD results (172 participants, 3 trials), which crossed the line of no effect, from three different measures of foot and ankle function indicated a small difference in favour of nailing, the results of individual trials indicated that this was very unlikely to be a clinically important difference. Pooled data (173 participants, 3 trials) for the need for re‐operation, symptomatic non‐union or malunion, wound complications and fracture union all favoured nailing, but the 95% CIs crossed the line of no effect and thus included the possibility of a better outcome after plating. For example, based on an illustrative risk of 100 re‐operations for adverse outcomes within one year of plate fixation in 1000 people with these fractures, 63 fewer (95% CI 88 fewer to 12 more) people per 1000 would have had re‐operations after nailing. Evidence from one trial (85 participants) showed no clinically important difference in pain between the two groups.
Overall completeness and applicability of evidence
There is evidence available from a total of only 173 adults with distal tibial metaphyseal fractures for one surgical comparison only. Although the three trials compared nailing with plating, the two types of intervention differed between trials. In particular, one trial (Im 2005) used conventional plating with non‐locking screws, whereas the other two (Guo 2010; Mauffrey 2012) involved plating with locking screws. Open surgery was used in Im 2005, whereas the MIPO technique was used in all cases in Guo 2010 and in at least some cases in Mauffrey 2012. The age and sex distributions of participants in the three trials were comparable and similar to that reported in Court‐Brown 2006. The fracture populations also appeared comparable; however, there were insufficient data to determine how many of the fractures in Guo 2010 and Mauffrey 2012 were open. As all three trials excluded open fractures other than Gustilo type 1 fractures, our findings may not apply to more severe open fractures. In such fractures, especially Gustilo types 2 and 3, debridement is important, and a temporary external fixator is usually used for stabilisation. Additional concerns about infection extending to the intramedullary canal during procedures mean that plating may be used in preference to nailing.
Developments in plating could also affect the findings of this review. The technique and experience of individual surgeons can affect outcomes, and surgeons often choose what they are familiar with. Nonetheless, there is a trend towards the increased use of locking plate fixation. In addition, the MIPO technique should cause less tissue damage and, hence, could theoretically achieve better outcomes. This may also be influenced by the use of precontoured locking plates. Both of the ongoing trials we have identified use locking plates and one specifically uses the MIPO technique. The planned enrolment of the ongoing trial (ISRCTN99771224) for which recruitment is confirmed as ongoing is over 320 participants. This highlights the limitations of the currently available evidence in terms of sample size and current practice.
Quality of the evidence
A summary of the 'Risk of bias' judgements for each domain across the included studies shows a mixed picture but one in which at least one trial was at high risk of bias for five of seven domains (see Figure 2).
Overall, the quality of the evidence assessed using GRADE was very low, which means that we are very uncertain about the estimates for all six outcomes presented in our 'Summary of findings' table (Table 1). Although, our main reasons for downgrading the evidence varied, we usually downgraded one or two levels for study limitations that reflected the high risk of bias of the included studies. We further downgraded for imprecision (wide CIs and small sample size) and for inconsistency where there was clear heterogeneity.
Potential biases in the review process
With the exception of a few items (detailed in the section Differences between protocol and review) we conducted the review following the prespecified protocol. A comprehensive database search was performed but it is possible that we have missed unpublished studies and study findings. We tried to contact authors of all included trials for detailed data, but only the authors of Mauffrey 2012 responded; they provided us with their original data. We calculated missing standard deviations from P values for both Guo 2010 and Im 2005, and calculated means and standard deviations from individual patient data provided for Mauffrey 2012. Especially for Mauffrey 2012, we assumed a normal distribution for all outcomes. This assumption may be less appropriate where the sample sizes are small.
Agreements and disagreements with other studies or reviews
We have identified two recently published systematic reviews, both of which include a broader range of study designs that include retrospective studies. One review (Xue 2014), including 14 studies of mixed design that compared nailing with plating for distal tibial metaphyseal fractures, found nailing to be associated with better functional scores (reported P value = 0.01), a lower risk of infection (P value = 0.02) and comparable pain scores (P value = 0.33), total complication rates (P value = 0.53) and times to union (P value = 0.86) than plating. Conversely, the malunion rate was lower in the plating group (P value < 0.0001). The second review (Kwok 2014) included eight studies testing the same comparison of nailing versus plating for distal tibial fractures. This also found the malunion rate to be lower in the plating group than in the nailing group (reported P value = 0.001). Kwok 2014 found no difference in the fracture union rate and in wound complications between the two groups. As well as differences in the inclusion criteria, both reviews included studies with fractures (generally AO/OTA type 42) other than those included in our review.
Authors' conclusions
Implications for practice.
Overall, there is either no or insufficient evidence to draw definitive conclusions on the best surgical treatment for distal tibial metaphyseal fractures in adults. The current available evidence, which is of very low quality, suggests there are no clinically important differences in functional or pain outcomes, and does not confirm a difference in the need for major re‐operations or risk of complications between nailing and plating. There is no evidence available from RCTs to inform on the use of surgery for less serious fractures or on the relative effects of other surgical interventions.
Implications for research.
In future updates of this review, the addition of evidence from the two ongoing trials identified will help to inform the selection of optimal treatments in managing distal tibial metaphyseal fractures. Further RCTs are needed but, in order to optimise research efforts, these should be preceded by research that aims to identify priority questions that can then be tested in large multicentre trials. Key clinical questions include the use of different plating techniques such as the minimally invasive percutaneous osteosynthesis technique, the fixation or not of fibula fractures, locking bolts and other techniques of nailing, and the use of the external fixation. In such trials, full data on functional outcomes, pain, complications, re‐operations and cost outcomes should be reported.
What's new
| Date | Event | Description |
|---|---|---|
| 3 April 2015 | Amended | Missing paragraph reinserted into Abstract: Main results |
Acknowledgements
We are grateful for helpful comments from Matthew Costa, Helen Handoll and Mario Lenza on drafts of the protocol for this review. The authors would also like to acknowledge the help of Catherine Deering, Joanne Elliott and Lindsey Elstub in the development of the protocol. We are grateful for helpful comments from Xavier Griffin, Matthew Costa, Helen Handoll, Joanne Elliott and Laura MacDonald on drafts of this review.
This project was supported by the National Institute for Health Research (NIHR) via Cochrane Infrastructure funding to the Cochrane Bone, Joint and Muscle Trauma Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR or the UK National Health Service or Department of Health.
Appendices
Appendix 1. Search strategies
CENTRAL (Wiley Online Library)
#1 MeSH descriptor: [Tibial Fractures] explode all trees and with qualifier(s): [Surgery ‐ SU] (157) #2 MeSH descriptor: [Fracture Fixation] this term only (346) #3 MeSH descriptor: [Fractures, Bone] this term only (1209) #4 #2 or #3 (1508) #5 MeSH descriptor: [Tibia] this term only (394 #6 #4 and #5 (8) #7 tibia*:ti (865) #8 (fracture*):ti,ab,kw (10116) #9 (metaphyseal or metaphysis or distal*):ti,ab,kw (5665) #10 #7 and #8 and #9 (62) #11 #1 or #6 (163) #12 #11 and #9 (27) #13 #10 or #12 (67) #14 MeSH descriptor: [Internal Fixators] this term only (151) #15 MeSH descriptor: [Bone Screws] this term only (578) #16 MeSH descriptor: [Fracture Fixation, Internal] this term only (730) #17 MeSH descriptor: [Bone Plates] this term only (372) #18 MeSH descriptor: [Bone Nails] this term only (357) #19 (pin* or nail* or screw* or plate* or fix* or prosthes* or ream* or unreamed):ti,ab,kw (40579) #20 MeSH descriptor: [External Fixators] this term only (136) #21 MeSH descriptor: [Orthopedic Fixation Devices] this term only (70) #22 MeSH descriptor: [Ilizarov Technique] this term only (12) #23 (minimally invasive plate osteosynthesis):ti,ab,kw (23) #24 (Mipo near/1 technique):ti,ab,kw (3) #25 #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 (40583) #26 #25 and #13 (45) [Trials]
MEDLINE (Ovid Online)
1 exp Tibial Fractures/su [Surgery] (7561) 2 Fracture Fixation/ (16836) 3 Fractures, Bone/ (49111) 4 2 or 3 (61539) 5 Tibia/ (27992) 6 4 and 5 (1015) 7 tibia$.ti. (19699) 8 fracture$.tw. (182445) 9 (metaphyseal or metaphysis or distal$).tw. (193452) 10 7 and 8 and 9 (1366) 11 (1 or 6) and 9 (1509) 12 10 or 11 (2027) 13 Internal Fixators/ or Bone Screws/ or Fracture Fixation, Internal/ or Bone Plates/ or Bone Nails/ (51151) 14 (pin$1 or nail$ or screw$1 or plate$1 or fix$ or prosthes$ or ream$ or unreamed).tw. (515370) 15 External Fixators/ or Orthopedic Fixation Devices/ or Ilizarov Technique/ (10663) 16 ((Mipo adj1 technique) or (minimally adj invasive adj plate adj osteosynthesis)).tw. (159) 17 13 or 14 or 15 or 16 (534345) 18 12 and 17 (1434) 19 Randomized controlled trial.pt. (401553) 20 Controlled clinical trial.pt. (90822) 21 randomized.ab. (321810) 22 placebo.ab. (164757) 23 Drug therapy.fs. (1789870) 24 randomly.ab. (230217) 25 trial.ab. (335714) 26 groups.ab. (1446586) 27 or/19‐26 (3545656) 28 exp Animals/ not Humans/ (4099183) 29 27 not 28 (3046502) 30 18 and 29 (149)
EMBASE (Ovid Online)
1 Tibia Fracture/ or Distal Tibia Fracture/ (11859) 2 exp Fracture Fixation/ (64556) 3 Fracture/ (64075) 4 2 or 3 (120598) 5 Tibia/ (28724) 6 4 and 5 (3014) 7 tibia$.ti. (19998) 8 fracture$.tw. (201566) 9 (metaphyseal or metaphysis or distal$).tw. (218297) 10 Metaphysis/ (4182) 11 9 or 10 (219269) 12 7 and 8 and 11 (1500) 13 (1 or 6) and 11 (2469) 14 12 or 13 (2804) 15 exp Fixation Device/ (44587) 16 exp Surgical Equipment/ (277456) 17 (pin$1 or nail$ or screw$1 or plate$1 or fix$ or prosthes$ or ream$ or unreamed).tw. (558152) 18 ((Mipo adj1 technique) or (minimally adj invasive adj plate adj osteosynthesis)).tw. (175) 19 or/15‐18 (830183) 20 14 and 19 (1691) 21 Randomized controlled trial/ (353243) 22 Clinical trial/ (834048) 23 Controlled clinical trial/ (388219) 24 Randomization/ (63897) 25 Single blind procedure/ (19033) 26 Double blind procedure/ (116034) 27 Crossover procedure/ (40609) 28 Placebo/ (247319) 29 Prospective study/ (266630) 30 ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. (776337) 31 (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. (191602) 32 ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. (164277) 33 (cross?over$ or (cross adj1 over$)).tw. (70703) 34 ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. (251970) 35 RCT.tw. (15276) 36 or/21‐35 (1936765) 37 Case Study/ or Abstract Report/ or Letter/ (933293) 38 36 not 37 (1897787) 39 Animal/ or Animal Experiment/ or Nonhuman/ (6197012) 40 Human/ (15089379) 41 39 and 40 (1298730) 42 39 not 41 (4898282) 43 38 not 42 (1745667) 44 20 and 43 (211)
Airiti Library
1 tibia* (2955) 2 fracture* (22544) 3 1 and 2 (1358) 4 distal* (4540) 5 3 and 4 (229) 6 proximal* (3621) 7 5 not 6 (90)
CNKI
1 tibia or tibial (9245) 2 fracture or fractures (38782) 3 1 and 2 (4162) 4 metaphyseal or metaphysis or distal (15683) 5 3 and 4(724) 6 plate or nail (21986) 7 5 and 6 (402)
Data and analyses
Comparison 1. Nailing versus plating.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Patient‐reported functional outcome (pooled data) | 3 | 172 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.02, 0.59] |
| 1.1 American Orthopaedic Foot and Ankle surgery score at 12 months | 1 | 85 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.29 [‐0.13, 0.72] |
| 1.2 OMAS % of normal side at 24 months | 1 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.40, 0.58] |
| 1.3 Olerud and Molander Ankle Score at 12 months | 1 | 23 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.83 [‐0.03, 1.69] |
| 2 Patient‐reported functional outcome | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 American Orthopaedic Foot and Ankle surgery score at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 OMAS % of normal side at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Olerud and Molander Ankle Score at 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Olerud and Molander Ankle score at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Olerud and Molander Ankle Score at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Disability Rating Index at 3 months (0 = full ability, 100 = maximal disability) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Disability Rating Index at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.8 Disability Rating Index at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Need for a secondary/revision operation or substantive physiotherapy for adverse outcomes (e.g. nonunion, malunion, and infection) | 3 | 173 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.12, 1.12] |
| 4 Symptomatic nonunion or malunion, including limping | 3 | 173 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.18, 2.80] |
| 5 Pain (0 to 40: no pain) at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Wound complications including superficial/deep wound infection and osteomyelitis | 3 | 173 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.20, 1.10] |
| 7 Fracture union | 3 | 173 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.95, 1.09] |
| 8 Fracture union time (weeks) | 2 | 149 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐1.46, 1.65] |
| 9 Operation time (minutes) | 2 | 149 | Mean Difference (IV, Fixed, 95% CI) | ‐16.78 [‐24.67, ‐8.88] |
| 10 Radiation time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Guo 2010.
| Methods | Randomisation: participants were allocated a sequential study number but there was no mention of method otherwise
Assessor blinding: there was no assessor blinding Length of follow‐up: 12 months |
|
| Participants | First Affiliated Hospital of Soochow University, Suzhou, China
Period of study: July 2005 to January 2008
111 participants each with distal metaphyseal fracture of the tibia. There were 26 participants "who had not reached one year by the time of the study."
Sex (of 85): 35 female, 50 male
Age: mean 44.3 years, range 23 to 70
Fracture type: AO/OTA 43‐A1:26, 43‐A2: 28, 43‐A3: 31 Unknown number of open fractures (Gustilo type I). Most participants had a fractured fibula (19 that were surgically fixed were excluded) Inclusion criteria 1. Distal metaphyseal fracture of tibia 2. Presence of a distal fragment of at least 3 cm in length with no articular incongruity (OTA type 43‐A fracture) Exclusion criteria 1. Individuals with pathological fractures, non‐osteoporotic osteopathies such as endocrine disorders, rheumatologic disorders, diabetes mellitus, renal disease, immunodeficiency states, mental impairment or difficulty in communication 2. Those with open fractures according to Gustilo and Anderson type II or type III or fractures with a displaced intra‐articular fragment Assigned: 57/54 participants (intramedullary nail/plate) Analysed: 44/41 (12 months) |
|
| Interventions | 1. Closed reduction and intramedullary nailing (IMN) (S2 nailing system; Stryker, Schönkirchen, Germany). Nails were inserted after reaming. Static locking applied in all cases. 2. Closed reduction and locking compression plate (LCP) (LCP; Synthes, Bettlach, Switzerland) applied with minimally percutaneous plate osteosynthesis (MIPO) technique. Operation was usually performed on day of injury. However, operations were delayed 5 to 10 days in 5 plate group participants because of excessive swelling or bruising. Other care: All received prophylactic antibiotics. Same postoperative care for both groups. Sutures removed after 14 or 15 days. Ankle was immobilised on a short‐leg cast or splint for 3 weeks. Range of motion ankle exercises were encouraged. Timing of partial and full weight‐bearing was on an individual basis. |
|
| Outcomes |
|
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were allocated a sequential study number. There was no mention how this was done. |
| Allocation concealment (selection bias) | High risk | Participants were allocated a sequential study number. Thus it appears that the sequence was predictable and allocation was not concealed. It was stated there were "no exclusions after randomisation" but then stated that "If the associated fibular fracture was fixed, the patient was excluded from the study". This applied to "ten patients in the IMN group and nine in the LCP group". reported that 19 participants whose associated fibular fracture was fixed surgically were excluded. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The difference between the two methods means that blinding is not possible for the surgeon and unlikely for the participants. There was no statement on blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were assessed by the two of the three operating surgeons involved in the treatment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "The remaining 26 patients had not reached one year by the time of the study." "Ten patients in the IMN group and nine in the LCP group were excluded due to fixation of fibular fracture." Contradictory statements mean that it is unclear how many were excluded from the trial. |
| Selective reporting (reporting bias) | Unclear risk | Protocol unavailable and results reported in a different way between abstract and text. Subsequent correction published. |
| Other bias | Unclear risk | Since the baseline characteristics of 26 participants (23% of 111) were not provided, we cannot tell if the baseline characteristics were balanced. Similar numbers in the 2 groups who had surgically fixed fibular fractures (10 in nail group and 9 in plate group) but these people were excluded; it is unclear whether these were counted in the 111 participants. All operations were carried out by the three senior surgeons. Postoperative care was reported to be comparable. |
Im 2005.
| Methods | Randomised trial, allocation by drawing from a box of envelopes Assessor blinding: one physician who had not been involved in the treatment performed an independent evaluation of all trial participants at 24 months Length of follow‐up: 24 months | |
| Participants | Dongguk University Hospital, Goyang, Korea
Period of study: July 1998 to June 2001
78 participants, each with a distal metaphyseal fracture of the tibia. Two died and 12 did not complete the study at 2 years follow‐up; these were excluded from the trial analyses and baseline characteristics
Sex (of 64): 18 female, 46 male
Age: mean 41.1 years, range 17 to 65
Fracture type: AO/OTA 43‐A1: 26, 43‐A2: 19, 43‐A3: 9, 43‐C1: 10 13 open fractures (Gustilo type I) and 51 closed fractures; 35 also had fibula fractures Inclusion criteria 1. Distal metaphyseal fractures of tibia 2. In all of the included cases, the centre of the fracture was in the distal metaphysis of tibia and either entirely extra‐articular (A1, A2, and A3) or with minimally displaced extension into the ankle joint (C1) Exclusion criteria 1. Open fractures of Gustilo‐Anderson type II or III 2. Fractures with displaced intra‐articular fragments 3. Based on the preoperative roentgenograph examination, two distal screw fixations were found to be not feasible (this applied to one case) Assigned: ?/? participants (intramedullary nail/plate) Analysed: 34/30 (24 months) |
|
| Interventions | 1. Closed reduction and intramedullary nailing (ACE tibial nails (ACE Depuy, El Segundo, California) used in 16 cases; or cannulated tibial nails (Mathys, Bettlach, Switzerland) used in 18 cases). Nails were inserted after reaming. Static locking applied in all cases. 2. Open reduction and fixation with anatomic plates (Waldermar‐Link, Hamburg, Germany) and screws. Eleven of the 35 fibular fractures were fixed with small dynamic compression plates (6 in the nail group versus 5 in the plate group). Other care: A long leg plaster cast was applied. After wound swelling had subsided, ankle joint mobilisation was encouraged under physiotherapist supervision. Timing of weight‐bearing was on an individual basis. A short leg cast was applied for participants with minimally displaced intra‐articular fractures. |
|
| Outcomes |
|
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The treatment method was chosen at random by drawing from the box containing an equal number of envelopes with either of the methods" |
| Allocation concealment (selection bias) | Unclear risk | "The treatment method was chosen at random by drawing from the box containing an equal number of envelopes with either of the methods". Adequate safeguards not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The difference between the two methods means that blinding is not possible for the surgeon and unlikely for the participants. There was no statement on blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "To limit the bias inherent in all clinical examinations and manual tests, the final follow‐up examination, 2 years after the operation, was performed by an independent physician who had not been involved in the actual treatment of any of the patient." However, this was not blinded and blinding of outcome assessment was not reported for other time points prior to 2 years after the operation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Treatment allocation and outcome were not provided for 14 participants (18% of 78), 2 of whom had died and 12 who were lost to follow‐up. |
| Selective reporting (reporting bias) | High risk | No protocol provided and the OMAS results only reported in the abstract and not in a way described in the methods. |
| Other bias | Unclear risk | Since the baseline characteristics of 14 participants were not provided, we cannot tell if the baseline characteristics were balanced. Although similar numbers in the 2 groups had surgically fixed fibular fractures (6 in nail group and 5 in plate group), we cannot be sure that the decision to operate was comparable in the 2 groups. Experience with both methods was stated; all operations were carried out or supervised by one senior surgeon. |
Mauffrey 2012.
| Methods | Randomised trial, allocation using computer‐generated random number sequence Assessor blinding: one physician blinded to treatment allocation performed evaluation of all participants Length of follow‐up: 12 months | |
| Participants | Warwick Orthopaedics, University of Warwick, Warwick, United Kingdom
Period of study: March 2008 to August 2009
24 participants with 24 distal metaphyseal fracture of the tibia
Sex: 8 female, 16 male
Age: mean 41.5 years
Fracture type: All fractures were closed or Gustilo type 1 fracture Inclusion criteria 1. Adults aged 18 years or over with a closed or Gustilo I extra‐articular fracture of the distal tibia 2. The distal tibia was defined as the area within two Müller squares of the ankle joint, in which the proximal and the distal segments of long bones are defined by a square whose sides have the same length as the widest part of the epiphysis Exclusion criteria 1. Open fractures of Gustilo‐Anderson type II or III 2. Fractures with displaced intra‐articular fragments 3. Individuals were excluded if they had other injuries that could affect the primary outcome measure, such as polytrauma or vascular or neurological injuries, if the fracture was too distal to achieve fixation of four cortices with distal interlocking screws, if the individual had a history of peripheral vascular disease or had a contraindication to anaesthesia Assigned: 12/12 participants (intramedullary nail/plate) Analysed: 12/11 (12 months) |
|
| Interventions | 1. Intramedullary nails were secured using a minimum of two distal non‐locking screws
2. Plate with a fixed‐angle screws (locking plate) was applied using indirect reduction techniques and bridge‐plating However, the surgeons were given the freedom to adapt these techniques as required by the configuration of the fracture and in accordance with their preferred technique and surgical approach. |
|
| Outcomes | Patient‐reported outcome (Disability Rating Index: DRI), Olerud and Molander Ankle Functional Score (OMAS), EuroQol (EQ‐5D), non‐union, delayed union, tibia malalignment, wound complications including superficial and deep infections, reoperation, need for hardware removal, broken hardware, compartment syndrome | |
| Notes | One participant in the intramedullary nail group receiving conservative treatment was included in the intention‐to‐treat analysis Individual participant data, characteristics and outcomes received from trialists (20 May 2013) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Treatment allocation was determined using a computer‐generated pseudo‐random number sequence" We are not sure why a pseudo‐random rather than random number sequence was used. |
| Allocation concealment (selection bias) | Low risk | Treatment allocation was administered by an independent trial co‐ordinator (KMG) who was contacted by telephone" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The difference between the two methods means that blinding is not possible for the surgeon and unlikely for the participants. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome data were collected by an experienced research physiotherapist (KMG) blinded to treatment allocation, at 6 weeks, 3 months, 6 months and 12 months postoperatively |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data reported, and the trialists provided us with the raw data. |
| Selective reporting (reporting bias) | Low risk | No protocol but no selective reporting was found, and the trialists provided us with the raw data. |
| Other bias | Unclear risk | Participants in the plate group were younger than those in the nail group (mean age 33 versus 50 years) Two fibulae were fixed in the nail group, whereas none was fixed in the plate group. No mention of the reason why fibulae were fixed. Although surgery was carried out by experienced surgeons, this was a pragmatic trial and the small numbers mean that variation in the postoperative rehabilitation regimens may have resulted in some important lack of comparability in the care programmes. |
AOFAS: American Orthopaedic Foot and Ankle Surgery AO/OTA: Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cheng 2011 | Fracture location is on the distal third of the tibia diaphysis, which is outside of the scope of review |
| Dai 2009 | The study design was not explicitly stated with no description of allocation method. It seems to be a retrospective study. Also, the fracture location was not clearly defined: the study included AO/OTA type A, B and C fractures, without mentioning whether type 42 or type 43 fracture was included. If type 42 fractures were included, they are outside the scope of this review. If type 43 fractures were included, a high proportion of intra‐articular fractures (type B+C, 21/25 versus 15/20) were present, which are also outside the scope of this review |
| Hontzsch 2014 | This RCT of two types of locking systems for intramedullary nailing included 75 participants in the experimental group and 67 participants in the control group. However, only 3/75 versus 0/67 were classified as AO/OTA 43 fractures; the rest being AO/OTA 42 fractures, which are outside the scope of this review |
| Li 2014 | The study focused on distal tibial shaft (AO 42) fractures, which was beyond the scope of review |
| Liu 2014 | The fracture location of the study was not clearly defined: the study included AO/OTA type A, B and C fractures, without mentioning whether type 42 or type 43 fracture was included. If type 42 fractures were included, they are beyond the scope of this review. If type 43 fractures were included, a high proportion (> 25%) of intra‐articular fractures (type B+C/total: 26/68) was present; which also is a reason for exclusion |
| Ristiniemi 2011 | Retrospective study design. The study design is outside the scope of review |
| Shon 2012 | Retrospective cohort study design. The study design is outside the scope of review |
| Sun 2014 | The study focused on distal tibial shaft (AO 42) fractures, which are outside the scope of review |
| Vallier 2011 | This was an RCT but the fracture location was 4 cm to 11 cm from the distal tibia plafond; which is outside the scope of this review |
| Vallier 2012 | The study focused on extra‐articular distal tibia shaft fractures (OTA 42), which was beyond the scope of review |
| Yang 2006 | Retrospective study design. The study design is outside the scope of this review |
| Zou 2012 | RCT but the trial included distal tibial shaft fractures (AO/OTA types 42 A, 42B, and 42C fractures), which are outside the scope of this review |
| Zou 2013 | RCT but the trial included distal tibial shaft fractures (AO/OTA types 42 A, 42B, and 42C fractures), which are outside the scope of this review |
AO/OTA: Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
ISRCTN99771224.
| Trial name or title | 'UK FixDT ‐ A Randomised Controlled Trial for patients with a displaced fracture of the distal tibia, is there a clinical and cost‐effectiveness difference between ‘locking’ plate fixation and intramedullary nail fixation' |
| Methods | Multicentre randomised clinical trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | 1. Intramedullary nailing The intramedullary nail is inserted at the proximal end of the tibia and passed down the centre of the bone in order to hold the fracture in the correct (anatomical) position. The reduction technique, the surgical approach, the type and size of the nail, the configuration of the proximal and distal interlocking screws and any supplementary device or technique will be left entirely to the discretion of the surgeon as per standard clinical practice. 2. Locking plate fixation The locking plate is inserted at the distal end of the tibia and passed under the skin on the surface of the bone. Again, the details of the reduction technique, the surgical approach, the type and position of the plate, the number and configuration of fixed‐angle screws and any supplementary device or technique will be left to the discretion of the surgeon. The only stipulation is that fixed‐angle screws must be used in at least some of the distal screw holes – this is standard practice with all distal tibia locking plates. |
| Outcomes | Primary outcome Disability Rating Index at 6 months after injury Secondary outcomes
|
| Starting date | Recruitment start date: 01/03/2013 Recruitment end date: 28/02/2017 |
| Contact information | Prof Matthew Costa, +44 (0)24 7615 1721 (UK) matthew.costa@warwick.ac.uk |
| Notes | Enrolment target: minimum 320 Ongoing |
NCT01047826.
| Trial name or title | Intramedullary nailing vs. M.I.P.O. in fractures of the tibia; a randomised controlled trial |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | 1. Minimally invasive percutaneous osteosynthesis (MIPO) using locked plates 2. Intramedullary nail group using the Expert Tibial Nail |
| Outcomes | Primary outcome measures: 1. Rate of malunion (time frame: 6 months) 2. Any healing that occurs with any one of the following: more than 5 degree angulation in the anterior‐posterior or lateral view or rotation of more than 10 degrees or shortening of more than 1 cm Secondary outcome measures: 1. Short Form (12) Health Score (SF‐12v2®) (time frame: every 3 months until healing or 24 months) 2. Blood loss (time frame: during the time of surgery) 3. Radiation exposure (time frame: during the time of surgery) 4. Duration of surgery 5. Infection rate (time frame: every 3 months until healing or 24 months) 6. Hospital stay (time frame: after surgery) 7. Time of fracture healing (time frame: 6 months) 8. Clinical criteria: no pain or tenderness while weight bearing or palpating the fracture site. 9. Radiological criteria: bridging of the fracture site in anterior‐posterior and lateral views. Trialists will use these two criteria to measure healing time |
| Starting date | Start date: December 2010 Estimated completion date: December 2014 |
| Contact information | Principal Investigator: Husam A AL‐Rumaih, MD (Saudi Arabia) +96612520088 ext 14119 rumaih@me.com |
| Notes | Estimated enrolment: 180 Status unknown (2/12/2014) |
Differences between protocol and review
We have made minor edits to the Background section, to improve clarity.
In the protocol, under 'Types of interventions', we said that we would make the more traditional method the 'control' group in any comparison; however, the final three included trials all compared the effect of intramedullary nailing and plating. Since, neither intervention was more traditional than the other, we made plating the control group.
We have clarified, under 'Types of studies', that we were interested in studies comparing surgical with non‐surgical interventions as well as studies comparing different interventions.
We have included sponsorship bias in the section 'Other potential sources of bias'.
We have added 'Different methods of the same category of surgery (e.g. MIPO versus open surgery for plate fixation; locked versus conventional (non‐locking) plate fixation)' to subgroup analyses.
Contributions of authors
Conceiving the review: LTK
Link with the editorial base and co‐ordinating the review: CCC
Drafting the protocol: LTK and CCC
Identifying relevant titles and abstracts from the searches: LTK and CHC
Obtaining copies of the trials: LTK
Selecting the trials: LTK and CHC
Extracting the data: LTK, CHC and CCC
Writing to authors of papers for additional information: LTK
Entering data into RevMan: LTK
Rechecking the data entered into RevMan: CCC
Analysis of data: LTK and CCC
Interpreting the data: LTK and CCC
Drafting the final review: LTK with contributions from CCC
Sources of support
Internal sources
Chang Gung Memorial Hospital, Chiayi, Taiwan.
External sources
No sources of support supplied
Declarations of interest
Liang Tseng Kuo: none known Ching‐Chi Chi: none known Ching‐Hui Chuang: none known
Edited (no change to conclusions)
References
References to studies included in this review
Guo 2010 {published data only}
- Guo JJ, Tang N, Yang HL, Tang TS. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia [Erratum appears in Journal of Bone and Joint Surgery. British Volume 2010;92(12):1717]. Journal of Bone and Joint Surgery. British Volume 2010;92(7):984‐8. [DOI] [PubMed] [Google Scholar]
Im 2005 {published data only}
- Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. Journal of Trauma 2005;59(5):1219‐23. [PUBMED: 16385303] [DOI] [PubMed] [Google Scholar]
Mauffrey 2012 {published data only}
- Mauffrey C. Raw data enquiry [personal communication]. Email to: LT Kuo 20 May 2013.
- Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML. A randomised pilot trial of "locking plate" fixation versus intramedullary nailing for extra‐articular fractures of the distal tibia. Journal of Bone and Joint Surgery. British volume 2012;94(5):704‐8. [DOI] [PubMed] [Google Scholar]
- Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML. A randomised pilot trial of intramedullary nailing versus 'locking‐plate' fixation for extra‐articular fractures of the distal tibia (abstract). Injury 2011;42(10):974. [DOI] [PubMed] [Google Scholar]
- Mauffrey C, McGuinness KR, Parsons N, Achten J, Costa ML. A randomised pilot trial of intramedullary nailing versus 'locking‐plate' fixation for extra‐articular fractures of the distal tibia (abstract). American Academy of Orthopaedic Surgeons Annual Meeting; 2012 Mar 7‐11; San Francisco (CA). 2012.
References to studies excluded from this review
Cheng 2011 {published data only}
- Cheng W, Li Y, Manyi W. Comparison study of two surgical options for distal tibia fracture‐minimally invasive plate osteosynthesis vs. open reduction and internal fixation. International Orthopaedics 2011;35(5):737‐42. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dai 2009 {published data only}
- Dai JP, Yan YQ, Yu YF, Zhou X. Curative effect comparison of two methods of treatment for distal tibial fractures [Chinese] [脛骨遠端骨折兩種治療方法的療效比較]. Zhongguo gu shang [China Journal of Orthopaedics and Traumatology] 2009;22(5):361‐3. [MEDLINE: ] [PubMed] [Google Scholar]
Hontzsch 2014 {published data only}
- Hoentzsch D. Trial to evaluate the effectiveness of angular stable locking system (ASLS) in patients with distal tibial fractures. clinicaltrials.gov/show/NCT00875992 (accessed 19 March 2015).
- Hontzsch D, Schaser KD, Hofmann GO, Pohlemann T, Hem ES, Rothenbach E, et al. Evaluation of the effectiveness of the angular stable locking system in patients with distal tibial fractures treated with intramedullary nailing: a multicenter randomized controlled trial. Journal of Bone and Joint Surgery. American Volume 2014;96(22):1889‐97. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Li 2014 {published data only}
- Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by three different surgical methods: a randomized, prospective study. International Orthopaedics 2014;38(6):1261‐7. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2014 {published data only}
- Liu CH, Wang ZC, Lu H, Yu SM, Mao YL, Zhou Q. Percutaneous locking plate versus traditional anatomical plate fixation for distal tibial fracture. Zhongguo Zuzhi Gongcheng Yanjiu 2014;18(17):2703‐8. [Google Scholar]
Ristiniemi 2011 {published data only}
- Ristiniemi J, Luukinen P, Ohtonen P. Surgical treatment of extra‐articular or simple intra‐articular distal tibial fractures: external fixation versus intramedullary nailing. Journal of Orthopaedic Trauma 2011;25(2):101‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Shon 2012 {published data only}
- Shon OJ, Park CH. Minimally invasive plate osteosynthesis of distal tibial fractures: a comparison of medial and lateral plating. Journal of Orthopaedic Science 2012;17(5):562‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sun 2014 {published data only}
- Sun LJ, Wu ZP, Guo XS, Chen H. Management of distal third tibial fractures: comparison of combined internal and external fixation with minimally invasive percutaneous plate osteosynthesis. International Orthopaedics 2014;38(11):2349‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vallier 2011 {published data only}
- Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. Journal of Orthopaedic Trauma 2011;25(12):736‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vallier 2012 {published data only}
- Vallier HA, Cureton BA, Patterson BM. Factors influencing functional outcomes after distal tibia shaft fractures. Journal of Orthopaedic Trauma 2012;26:178‐83. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Yang 2006 {published data only}
- Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: plating versus shortened intramedullary nailing. Injury 2006;37(6):531‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zou 2012 {published data only}
- Zou J, Shi ZM, Zhang W, Zhang CQ. Open reduction and internal fixation better than percutaneous plate osteosynthesis in distal tibial fractures. Journal of Investigative Surgery 2012;25(5):326‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zou 2013 {published data only}
- Zou J, Zhang W, Zhang CQ. Comparison of minimally invasive percutaneous plate osteosynthesis with open reduction and internal fixation for treatment of extra‐articular distal tibia fractures. Injury 2013;44(8):1102‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN99771224 {unpublished data only}
- Costa M. UK FixDT: Fixation of distal tibia fractures. www.isrctn.com/ISRCTN99771224 (accessed 6 March 2015).
NCT01047826 {unpublished data only}
- AL‐Rumaih HA, Taha WS. M.I.P.O. vs intramedullary nailing in tibia fractures (MINT). http://clinicaltrials.gov/ct2/show/NCT01047826?term=NCT01047826&rank=1 (accessed 19 March 2015).
Additional references
Ahmad 2010
AO/OTA 1996
- No authors listed. Fracture and dislocation compendium: Orthopaedic Trauma Association Committee for Coding and Classification. Journal of Orthopaedic Trauma 1996;10(Suppl 1):1‐154. [PubMed] [Google Scholar]
Babis 1997
- Babis GC, Vayanos ED, Papaioannou N, Pantazopoulos T. Results of surgical treatment of tibial plafond fractures. Clinical Orthopaedics and Related Research 1997;(341):99‐105. [PubMed] [Google Scholar]
Bedi 2006
- Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. Journal of the American Academy of Orthopaedic Surgeons 2006;14(7):406‐16. [DOI] [PubMed] [Google Scholar]
Blauth 2001
- Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. Journal of Orthopaedic Trauma 2001;15(3):153‐60. [DOI] [PubMed] [Google Scholar]
Borelli 2002
- Borrelli J, Prickett W, Song E, Becker D, Ricci W. Extra osseous blood supply of the distal tibia and the effects of different plating techniques: human cadaveric study. Journal of Orthopaedic Trauma 2002;16(10):691‐5. [DOI] [PubMed] [Google Scholar]
Collinge 2010
- Collinge C, Protzman R. Outcome of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. Journal of Orthopaedic Trauma 2010;24(1):24‐9. [DOI] [PubMed] [Google Scholar]
Court‐Brown 1990
- Court‐Brown CM, Christie J, McQueen MM. Closed intramedullary tibial nailing. Its use in closed and type I open fractures. Journal of Bone and Joint Surgery. British Volume 1990;72(4):605‐11. [DOI] [PubMed] [Google Scholar]
Court‐Brown 1995
- Court‐Brown CM, McBirnie J. The epidemiology of tibial fractures. Journal of Bone and Joint Surgery. British Volume 1995;77(3):417‐21. [PubMed] [Google Scholar]
Court‐Brown 1997
- Court‐Brown CM, Gustilo T, Shaw AD. Knee pain after intramedullary tibial nailing: its incidence, etiology, and outcome. Journal of Orthopaedic Trauma 1997;11(2):103‐5. [DOI] [PubMed] [Google Scholar]
Court‐Brown 2005
- Court‐Brown CM. Fractures of the tibia and fibula. In: Bucholz R, Heckman J, Court‐Brown C, et al. editor(s). Rockwood and Green's fractures in adults. 6th Edition. Vol. 2, Philadelphia: Lippincott Wiliams & Wilkins, 2005:2079‐146. [Google Scholar]
Court‐Brown 2006
- Court‐Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37(8):691‐7. [DOI] [PubMed] [Google Scholar]
Digby 1982
- Digby JM, Holloway GMN, Webb JK. A study of function after tibial cast bracing. Injury 1982;14(5):432‐9. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haines 1984
- Haines JF, Williams EA, Hargadon ES, Davies DR. Is conservative treatment of displaced tibial shaft fractures justified?. Journal of Bone and Joint Surgery. British Volume 1984;66(1):84‐8. [DOI] [PubMed] [Google Scholar]
Hasenboehler 2007
- Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury 2007;38(3):365‐70. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2004
- Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta‐regression. Statistics in Medicine 2004;23(11):1663‐82. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kitaoka 1994
- Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle, hindfoot, midfoot, hallux, and lesser toes. Foot and Ankle International 1994;15(7):349‐53. [DOI] [PubMed] [Google Scholar]
Kwok 2014
- Kwok CS, Crossman PT, Loizou CL. Plate versus nail for distal tibial fractures: a systematic review and meta‐analysis. Journal of Orthopaedic Trauma 2014;28(9):542‐8. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Mast 1988
- Mast JW, Spiegel PG, Pappas JN. Fractures of the tibial pilon. Clinical Orthopaedics and Related Research 1988;(230):68‐82. [PubMed] [Google Scholar]
Mosheiff 1999
- Mosheiff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury 1999;30(2):83‐90. [DOI] [PubMed] [Google Scholar]
Müller 1990
- Müller ME, Nezarian S, Koch P, Schatzker J. The Comprehensive Classification of Fractures of Long Bones. Berlin, Germany: Springer‐Verlag, 1990. [Google Scholar]
Obremskey 2004
- Obremskey WT, Medina M. Comparison of intramedullary nailing of distal third tibial shaft fractures: before and after traumatologists. Orthopedics 2004;27(11):1180‐4. [DOI] [PubMed] [Google Scholar]
Oestern 1984
- Oestern H‐J, Tscherne H. Pathophysiology and classification of soft tissue injuries associated with fractures. In: Tscherne H, Gotzen L editor(s). Fractures with Soft Tissue Injuries. Springer‐Verlag, 1984:1‐9. [Google Scholar]
Olerud 1984
- Olerud C, Molander H. A scoring scale for symptomatic evaluation after ankle fracture. Archives of Orthopaedic and Trauma Surgery 1984;103(3):190–4. [DOI] [PubMed] [Google Scholar]
Ovadia 1986
- Ovadia DN, Beals RK. Fractures of the tibial plafond. Journal of Bone and Joint Surgery. American Volume 1986;68:543‐51. [PubMed] [Google Scholar]
Petrisor 2010
- Petrisor BA, Bhandari M, Schemitsch E. Tibia and fibula fractures. Rockwood And Green's Fractures In Adults. 7th Edition. Vol. 2, Philadelphia: Lippincott Williams & Wilkins, 2010. [Google Scholar]
Redfern 2004
- Redfern DJ, Syed SU, Davies SJM. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury 2004;35(6):615‐20. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager (RevMan) Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robinson 1995
- Robinson CM, McLauchlan GJ, McLean IP, Court‐Brown CM. Distal metaphyseal fractures of the tibia with minimal involvement of the ankle: classification and treatment by locked intramedullary nailing. Journal of Bone and Joint Surgery. British Volume 1995;77(5):781‐7. [PubMed] [Google Scholar]
Toivanen 2002
- Toivanen JA, Väistö O, Kannus P, Latvala K, Honkonen SE, Järvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft: a prospective, randomized study comparing two different nail‐insertion techniques. Journal of Bone and Joint Surgery. American Volume 2002;84(4):580‐5. [DOI] [PubMed] [Google Scholar]
Wagner 2003
- Wagner M. General principles for the clinical use of the LCP. Injury 2003;34(Suppl 2):B31‐42. [DOI] [PubMed] [Google Scholar]
Whittle 2008
- Whittle AP. Fractures of the lower extremity. In: Canale ST, Beatty JH editor(s). Campbell's Operative Orthopaedics. 11th Edition. Vol. 3, Philadelphia: Mosby, Elsevier, 2008. [ISBN: 9780323033299] [Google Scholar]
Xue 2014
- Xue XH, Yan SG, Cai XZ, Shi MM, Lin T. Intramedullary nailing versus plating for extra‐articular distal tibial metaphyseal fracture: a systematic review and meta‐analysis. Injury 2014;45(4):667‐76. [DOI] [PubMed] [Google Scholar]
Zelle 2006
- Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M. Evidence‐Based Orthopaedic Trauma Working Group. Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. Journal of Orthopaedic Trauma 2006;20(1):76‐9. [DOI] [PubMed] [Google Scholar]


