Abstract
Objective:
We evaluated the impact of the 2017 American Academy of Pediatrics hypertension Clinical Practice Guideline (CPG), compared with the previous guideline (“Fourth Report”), on the frequency of hypertensive blood pressure (BP) measurements in childhood and associations with hypertension in adulthood using data from the International Childhood Cardiovascular Cohort Consortium.
Study Design:
Childhood BPs were categorized in normal, pre-hypertensive/elevated, and hypertensive (stage 1 and 2) ranges using the Fourth Report and the CPG. Participants were contacted in adulthood to assess self-reported hypertension. The associations between childhood hypertensive range BPs and self-reported adult hypertension were evaluated.
Results:
Data were available for 34,014 youth (10.4±3.1 years, 50.6% female) with 92,751 BP assessments. Compared with the Fourth Report, the CPG increased hypertensive readings from 7.6 to 13.5% and from 1.3 to 2.5% for stage 1 and 2 hypertensive range, respectively (p <0.0001). Of 12,761 adults (48.8±7.9 years, 43% male), 3,839 (30.1%) had self-reported hypertension. The sensitivity for predicting adult hypertension among those with hypertensive range BPs at any point in childhood, as defined by the Fourth Report and the CPG, respectively, was 13.4% and 22.4% (specificity 92.3% and 85.9%, p <0.001), with no significant impact on positive and negative predictive values. Associations with self-reported adult hypertension were similar and weak (c-statistic range 0.61–0.68) for hypertensive range BPs as defined by the Fourth Report and CPG.
Conclusion:
The CPG significantly increased the prevalence of childhood BPs in hypertensive ranges and improved the sensitivity (without an overall strengthened association) of predicting self-reported adult hypertension.
Keywords: Pediatric, Hypertension, Sensitivity, Specificity, Guideline
Introduction
Beginning in the 1970s, BP screening became a regular component of the pediatric physical examination, with standards endorsed by the National Institutes of Health and Pediatric societies updated regularly. The most recent guideline, the American Academy of Pediatrics Clinical Practice Guideline (CPG) on the screening and management of high BP in children and adolescents, serves as an update with key changes to the “Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents” (Fourth Report),1 was published in 2017.2 The CPG includes a revised definition of pediatric hypertension; new standardized BP reference tables that, in contrast to the Fourth Report, exclude data from overweight and obese children; and new BP static cut-points for hypertension in adolescents (≥13 years old) (Table 1, online) that were introduced to provide consistency with the updated adult hypertension guidelines.3
Table 1 (Online).
Blood pressure definitions used by the Fourth Report and the Clinical Practice Guideline
| Fourth Report | Clinical Practice Guideline | ||
|---|---|---|---|
| 1-<13ya | ≥13y | ||
| Normal BP | <90th percentile | <90th percentileb | <120/<80 mmHg |
| Pre-hypertension/Elevated BP c | ≥90 to <95th% percentile ≥120/80 mmHg in adolescents |
≥90th to <95th percentile | 120/<80 to 129/<80 mmHg |
| Stage 1 HTN | ≥95th to <99th percentile + 5 mmHg | ≥95th to <95th percentile + 12 mmHg | 130/80 to 139/89 mmHg |
| Stage 2 HTN | ≥99th percentile + 5 mmHg | ≥95th percentile + 12 mmHg | ≥140/90 mmHg |
If BP percentile values exceed the static threshold cut-offs for ≥13 year old children, then those corresponding cutoffs are used.
Normative values for the CPG were generated using only data from normal weight youth (i.e., body mass index <85th percentile)
The BP category previously referred to as pre-hypertension in the Fourth Report is termed elevated BP in the CPG.
Several studies have demonstrated that the CPG BP definitions result in an increased prevalence of hypertension in youth compared with the Fourth Report, though studies evaluating prevalence changes across the pediatric age span are lacking.4 Moreover, the impact of these revised definitions on associations with BP tracking into adulthood have not been evaluated. Using longitudinal data from the International Childhood Cardiovascular Cohort (i3C), a consortium of seven cohorts recruited in childhood with follow-up assessments in adulthood, the present study was designed to evaluate the impact of the CPG pediatric hypertension definitions on the prevalence of BPs throughout childhood in hypertensive ranges and associations with self-reported hypertension in adulthood.
Methods
International Childhood Cardiovascular Cohort (i3C) Consortium
Data were obtained from the i3C, a consortium of seven longitudinal cohorts, five from the United States (Bogalusa Heart Study [BHS], Minneapolis Childhood Cohort Studies [MPLS], Muscatine Study [MUSC], National Heart Lung and Blood Institute Growth and Health Study [NGHS], and the Princeton Lipid Research Study [PLRS]), one from Finland (Cardiovascular Risk in Young Finns Study [YFS]), and one from Australia (Childhood Determinants of Adult Health [CDAH] Study), as previously described.5, 6. Participants in each cohort were enrolled between ages 3–19 years in the 1970s to 1990s and were examined periodically during childhood and into adulthood. Data from children with BP measurements between 6-<18 years of age were included in the present study. The study has been approved by the Institutional Review Boards at each of the seven cohort sites.5
Blood Pressure Measurement
BP was measured on one occasion during a study visit in a standardized manner according to the protocols of each of the seven studies, as previously reported.7 With the exception of the initial BP taken in the CDAH Study, measurements were taken in the right arm. All studies used a standard mercury sphygmomanometer, with the exception of MPLS, where a random zero sphygmomanometer was used.7–10 The mean of the BP measurements taken at each participant assessment (ranging from 2–6, depending on the cohort) was used for analysis.
Using the age-, sex-, and height-specific percentiles and definitions from the Fourth Report and the CPG (Table 1, online), BP measurement levels were categorized as normal, pre-hypertensive/elevated BP (the CPG changed the terminology from pre-hypertension to elevated BP), stage 1 hypertensive range, or stage 2 hypertensive range.1, 2 In all cohorts, height and weight were measured with a stadiometer and calibrated scale, respectively, and body mass index (BMI, kg/m2) was calculated. Height, weight, and BMI were then converted to age- and sex-specific percentiles using Centers for Disease Control and Prevention (CDC) growth charts.11
Self-reported hypertension in adulthood
Between 2014 and 2019 the i3C attempted to contact all the original cohort members in order to obtain information on adult-onset cardiovascular disease, using a Heart Health Survey (HHS), as previously described.5 Aside from the YFS, the HHS was completed by the participants either on paper forms, online, or by phone interviews with research coordinators. Self-reported hypertension was defined by answering “yes” to the question “has a doctor or other health professional ever told you that you have high blood pressure or hypertension”.5
Statistical analysis
Relevant demographic and clinical data were collected and displayed as means with standard deviations or frequencies with percentages, as appropriate. In addition to determining the prevalence of BPs in the pre-hypertensive/elevated BP and stage 1 and 2 hypertensive ranges as defined by the Fourth Report and the CPG, the re-classification rates to a new BP category as a result of the CPG were computed. Statistical agreement in BP categorization between the Fourth Report and the CPG was evaluated using Bowker’s test of symmetry. The study analysis was undertaken for the whole study population (ages 6-<18 years) and again for individual age groups categorized as: school-age children (6-<9 years), pre-adolescents (9-<13 years), young adolescents (13-<15 years), and older adolescents (15-<18 years). Given that the data were obtained from longitudinal studies, most participants had more than one data point. In these cases, for analysis involving the whole study population age range, a random data entry BP measurement for each participant was used for analysis. The same was done for analysis within specific individual age groups. However, if the multiple data collection points occurred in different age groupings as designated above, then one data point from each age group was included. Two-by-two tables were generated to evaluate the sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) of a pediatric BP reading in a hypertensive range (stage 1 and 2) as defined by the Fourth Report and the CPG at each age group and the occurrence of self-reported adult hypertension. Logistic regression analyses were performed and receiver operating characteristic (ROC) curves were generated to evaluate the association between self-reported hypertension in adulthood with pre-hypertensive/elevated and hypertensive BP ranges in youth, as defined by the Fourth Report and CPG. Statistical analysis was performed using SAS® version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Data were available from 34,014 children (10.4 ± 3.1 years, 50.6% female) with a total of 92,751 BP measurements. BP and anthropometric data in the study population are presented in Table 2. BP and descriptive data across BP categories are presented in Table 3 (online). Of the 34,014 children recruited in the original longitudinal cohort studies, 46.1% (15,667) completed the HHS, and self-reported adult BP status was available for 81.5% (12,761, mean age 48.8 ± 7.9 years) (Figure 1, online). A significantly higher proportion of participants with self-reported BP status in adulthood were female compared to those without self-reported BP status in adulthood (57.3% vs 46.5%, p<0.0001) (Table 2). Of the 12,761 with self-reported adult BP status, 3,839 (30.1%) had self-reported hypertension.
Table 2.
Descriptive characteristics of all childhood participants and children with self-reported blood pressure (BP) status in adulthood
| All Participants N = 34,014 |
Participants with self-reported BP status in adulthood N = 12,761 |
Participants without self-reported BP status in adulthood N = 21,253 |
p
Presence vs absence of self-reported BP status in adulthood |
|
|---|---|---|---|---|
| Age (yrs) | 10.4 (3.1) | 10.6 (3.1) | 10.3 (3.1) | <0.0001 |
| Sex (female) | 17,196 (50.6%) | 7,307 (57.3%) | 9,889 (46.5%) | <0.0001 |
| Race (white)* | 19,466 (74.6%) | 6,687 (74.9%) | 12,779 (74.5%) | 0.45 |
| Systolic BP (mmHg) | 104.7 (12.6) | 105.2 (12.8) | 104.4 (12.5) | <0.0001 |
| Systolic BP percentile | 50.5 (28.7) | 50.6 (28.6) | 50.4 (28.7) | 0.53 |
| Diastolic BP (mmHg) | 57.0 (14.7) | 58.4 (14.1) | 56.2 (15.0) | <0.0001 |
| Diastolic BP percentile | 41.5 (30.7) | 43.7 (30.2) | 40.2 (30.9) | <0.0001 |
| Height (cm) | 140.6 (17.9) | 142.0 (17.7) | 139.7 (18.0) | <0.0001 |
| Height percentile | 61.0 (28.3) | 62.3 (27.8) | 60.3 (28.5) | <0.0001 |
| Weight (kg)# | 37.7 (15.6) | 38.8 (15.8) | 37.0 (15.5) | <0.0001 |
| Weight percentile# | 61.3 (27.5) | 62.2 (27.0) | 60.5 (27.7) | <0.0001 |
| BMI (kg/m2)# | 18.2 (3.6) | 18.5 (3.7) | 18.1 (3.6) | <0.0001 |
| BMI percentile# | 57.9 (28.0) | 59.0 (27.7) | 57.3 (28.2) | <0.0001 |
All values displayed as means with standard deviations or frequencies with percentages as appropriate
N = 26,079 for all participants, 8,925 for participants with self-reported BP status in adulthood, and 17,154 for participants without self-reported BP status in adulthood
N = 33,984 for all participants, 12,754 for participants with self-reported BP status in adulthood, and 21,230 for participants without self-reported BP status in adulthood
Table 3 (Online).
Blood pressure and anthropometric data in childhood by single visit blood pressure measure categorization
| N = 34,014 | NT Range 4th | NT Range CPG | Pre-HTN Range 4th | Elevated BP Range CPG | HTN Range 4th | HTN Range CPG |
|---|---|---|---|---|---|---|
| Age (yrs) | 27,371 10.1 (2.9) |
25,079 10.2 (3.0) |
3,611 12.3 (3.4) |
3,498 11.2 (3.4) |
3,032 11.0 (3.2) |
5,437 10.8 (3.3) |
| Sex (male) | 13,543 (49%) | 12,224 (49%) | 1,950 (54%) | 1,857 (53%) | 1,325 (44%) | 2,737 (50%) |
| Race (white)* | 15,321 (72%) | 14,156 (71%) | 2,281 (87%) | 2,057 (83%) | 1,864 (88%) | 3,253 (87%) |
| Systolic BP (mmHg) | 100.6 (9.1) | 99.8 (8.9) | 118.3 (7.9) | 114.5 (8.9) | 125.8 (12.1) | 121.2 (11.6) |
| Systolic BP percentile | 41.8 (24.0) | 38.7 (22.0) | 80.3 (16.7) | 77.5 (15.9) | 92.9 (12.9) | 87.4 (16.7) |
| Diastolic BP (mmHg) | 53.8 (13.2) | 53.0 (13.0) | 68.4 (11.8) | 64.3 (11.1) | 73.0 (13.6) | 71.1 (13.5) |
| Diastolic BP percentile | 34.6 (27.1) | 32.3 (25.7) | 65.3 (28.3) | 58.5 (27.7) | 75.9 (26.9) | 73.4 (27.7) |
| Height (cm) | 138.7 (17.0) | 139.3 (17.3) | 151.8 (19.4) | 145.1 (19.8) | 144.2 (18.2) | 143.4 (18.5) |
| Height percentile | 60.4 (28.3) | 60.0 (28.4) | 64.2 (27.7) | 62.5 (28.1) | 62.6 (28.1) | 64.8 (27.4) |
| Weight (kg) | 35.6 (14.1) | 36.0 (14.4) | 48.3 (18.5) | 42.4 (17.9) | 43.7 (18.4) | 42.3 (17.9) |
| Weight percentile | 59.5 (27.5) | 58.8 (27.6) | 67.3 (26.2) | 65.5 (26.2) | 70.3 (26.0) | 70.1 (25.8) |
| BMI (kg/m2) | 17.8 (3.3) | 17.8 (3.3) | 20.1 (4.2) | 19.2 (4.0) | 20.1 (3.6) | 19.7 (4.4) |
| BMI percentile | 56.0 (28.0) | 55.2 (28.0) | 63.8 (26.7) | 62.5 (27.0) | 68.8 (26.5) | 67.5 (26.7) |
Race data available for 26,079 participants
All values displayed as means with standard deviations or frequencies with percentages as appropriate
NT: normotensive; 4th: Fourth Report; CPG: Clinical Practice Guideline; HTN: hypertension; BP: blood pressure; BMI: body mass index
Figure 1 (online).
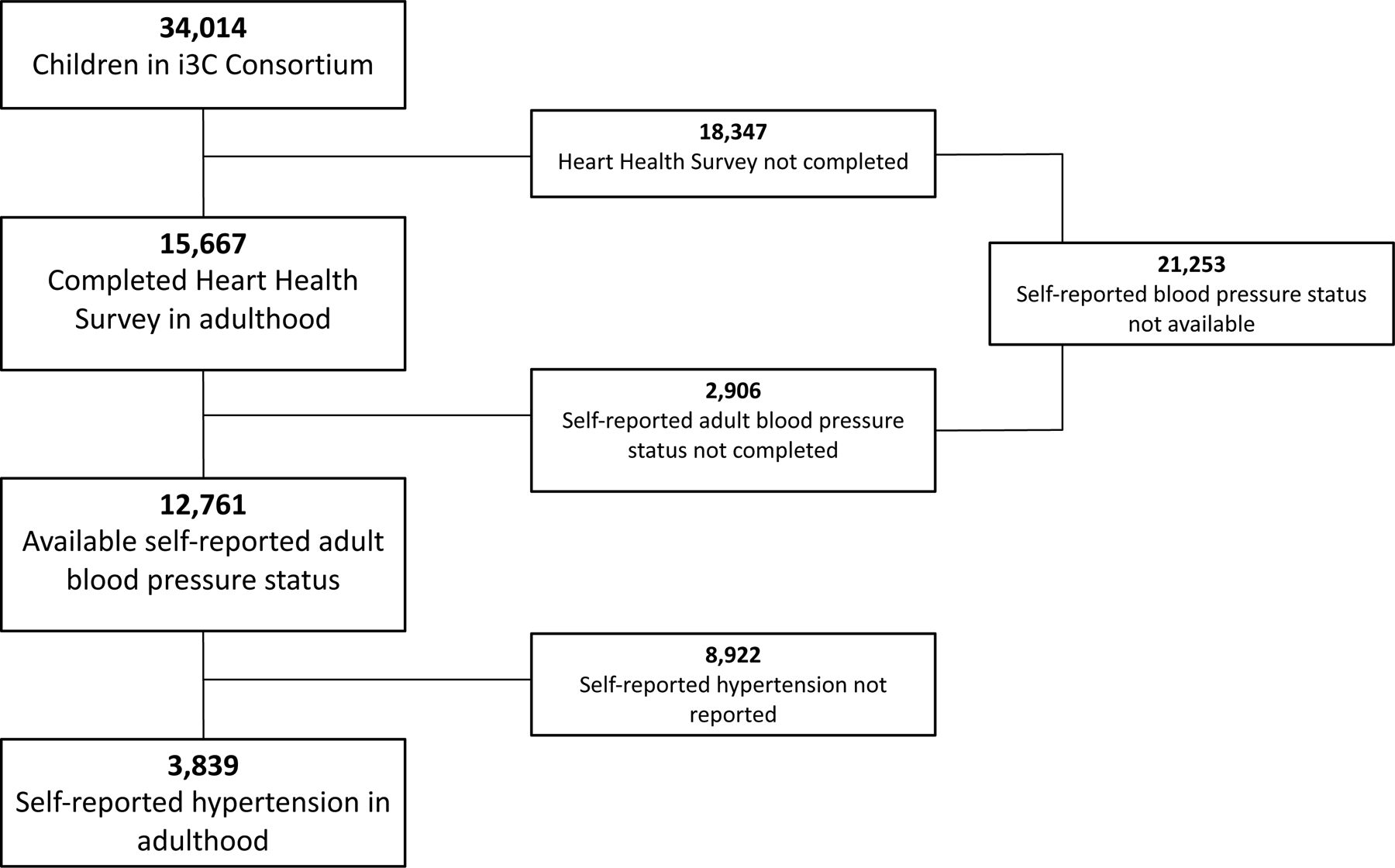
Flow diagram of participants involved in the International Childhood Cardiovascular Cohort (i3C) Consortium in childhood and follow-up in adulthood with self-reported BP status via the Heart Health Survey.
BP categorization using the CPG resulted in a significant increase in the prevalence of stage 1 (7.6% to 13.5%) and stage 2 (1.3% to 2.5%) hypertensive BP readings for the study population as a whole and across each age group (Table 4, online). The most marked increase in the prevalence of BPs in the stage 1 hypertensive range occurred in participants <13 years old, with a prevalence that nearly doubled for both the 6-<9 (6.9% to 12.9%) and 9-<13 (6.4% to 12.6%) year old cohorts.
Table 4 (online).
Prevalence of hypertensive measures as defined by the Fourth Report and the CPG*
| Pre-Hypertension/Elevated BP Range | Stage 1 Hypertension Range | Stage 2 Hypertension Range | ||||
|---|---|---|---|---|---|---|
| 4th | CPG | 4th | CPG | 4th | CPG | |
| Total (N = 34,014) | 2,611 (7.7%) | 3,498 (10.3%) | 2,580 (7.6%) | 4,583 (13.5%) | 452 (1.3%) | 854 (2.5%) |
| 6-<9y (N = 14,813) | 880 (5.9%) | 1,317 (8.9%) | 1,020 (6.9%) | 1,916 (12.9%) | 113 (0.8%) | 240 (1.6%) |
| 9-<13y (N = 21,916) | 1,814 (8.3%) | 1,893 (8.6%) | 1,398 (6.4%) | 2,755 (12.6%) | 222 (1.0%) | 420 (1.9%) |
| 13-<15y (N = 12,108) | 1,897 (15.7%) | 1,511 (12.5%) | 789 (6.5%) | 1,053 (8.7%) | 168 (1.4%) | 241 (2.0%) |
| 15-<18y (N = 13,337) | 3,278 (24.6%) | 2,211 (16.6%) | 940 (7.0%) | 1,698 (12.7%) | 197 (1.5%) | 500 (3.8%) |
p <0.0001 for classification asymmetry for the total study population and for each age group
BP: blood pressure; HTN: hypertension; 4th: Fourth Report; CPG: Clinical Practice Guideline
Re-classification to a higher BP category was more common than to a lower BP category, which occurred infrequently (Table 5, p<0.001 for re-classification in all age categories). The most significant re-classification occurred in participants <13 years old, with 91.5% (805/880) aged 6–9 years old and 72.7% (1,319/1,814) aged 9-<13 years old with pre-hypertensive BP ranges increasing to stage 1 hypertensive BP range using the CPG. Re-classification from stage 1 to stage 2 hypertensive BP range using the CPG was most marked for older adolescents (33.0% (294/891)). Clinical and demographic factors associated with BP category re-classification across the different age categories are found in Table 6 (online). Notably, adolescents that re-classified to a higher BP category had significantly higher diastolic BP readings. Conversely, systolic BPs were lower for 13-<15 year old adolescents that re-classified from pre-hypertensive range to the stage 1 hypertensive range and not significantly different for 15-<18 year olds.
Table 5.
Re-classification of single-visit blood pressure measures when using Clinical Practice Guideline thresholds (p <0.001 for re-classification in all age categories)
| Age (yr) |
Normal range by Fourth Report1 | Pre-HTN range by Fourth Report | Stage 1 HTN range by Fourth Report2 | Stage 2 HTN range by Fourth Report3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal range by CPG | Elevated range by CPG | Stage 1 HTN range by CPG | Normal range by CPG | Elevated range by CPG | Stage 1 HTN range by CPG | Stage 2 HTN range by CPG | Elevated range by CPG | Stage 1 HTN range by CPG | Stage 2 HTN range by CPG | Stage 1 HTN range by CPG | Stage 2 HTN range by CPG | |
| 6-<9 | 11,340 (89%) | 1,242 (10%) | 218 (2%) | 0 (0%) | 75 (8%) | 805 (91%) | 0 (0%) | 0 (0%) | 893 (88%) | 127 (12%) | 0 (0%) | 113 (100%) |
| 9-<13 | 16,848 (91%) | 1,398 (8%) | 236 (1%) | 0 (0%) | 495 (27%) | 1,319 (73%) | 0 (0%) | 0 (0%) | 1,200 (86%) | 198 (14%) | 0 (0%) | 222 (100%) |
| 13-<15 | 9,254 (100%) | 0 (0%) | 0 (0%) | 49 (3%) | 1,399 (74%) | 449 (24%) | 0 (0%) | 112 (14%) | 586 (74%) | 91 (12%) | 18 (11%) | 150 (89%) |
| 15-<18 | 8,922 (100%) | 0 (0%) | 0 (0%) | 6 (0%) | 2,162 (66%) | 1,099 (34%) | 11 (0%) | 49 (5%) | 597 (64%) | 294 (31%) | 2 (1%) | 195 (99%) |
HTN: hypertension; CPG: Clinical Practice Guideline
No patients re-classified to stage 2 hypertension range
No patients re-classified to normal blood pressure range
No patients re-classified to elevated or normal blood pressure ranges
Table 6 (online).
Demographic and clinical characteristics associated with re-classification to a higher blood pressure category as defined by the Clinical Practice Guideline (CPG)
| Pre-hypertension range by Fourth Report | Stage 1 hypertension range by Fourth Report | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Remained elevated BP range by CPG | Re-classified to Stage 1 HTN range by CPG | p | Remained Stage 1 HTN range by CPG | Re-classified to Stage 2 HTN range by CPG | p | |
| 6-<9 years old | N = 75 | N = 805 | N = 893 | N = 127 | ||
| Age (yr) ± SD | 7.1 ± 0.9 | 7.6 ± 0.9 | <0.0001 | 7.6 ± 0.9 | 7.6 ± 1.0 | 0.998 |
| Sex (male) | 14 (19%) | 421 (52%) | <0.0001 | 361 (40%) | 72 (57%) | <0.001 |
| Race (white)* | 31 (76%) | 371 (71%) | 0.9 | 483 (81%) | 88 (90%) | 0.03 |
| Height (cm) ± SD | 119.7 ± 7.7 | 126.0 ± 7.6 | <0.0001 | 126.1 ± 7.9 | 126.9 ± 6.7 | 0.2 |
| Height (percentile) ± SD | 42.7 ± 28.3 | 67.1 ± 27.7 | <0.0001 | 65.8 ± 27.7 | 72.3 ± 25.8 | 0.01 |
| BMI (kg/m2) ± SD | 16.1 ± 1.8 | 17.6 ± 3.1 | <0.0001 | 17.7 ± 3.2 | 18.4 ± 3.7 | 0.02 |
| BMI (percentile) ± SD | 56.8 ± 28.3 | 68.6 ± 26.7 | 0.0003 | 68.8 ± 26.5 | 74.1 ± 25.8 | 0.03 |
| SBP (mmHg) ± SD | 105.9 ± 5.8 | 111.9 ± 6.2 | <0.0001 | 116.8 ± 7.1 | 124.0 ± 5.9 | <0.0001 |
| DBP (mmHg) ± SD | 63.6 ± 10.2 | 64.5 ± 13.7 | 0.6 | 67.9 ± 13.7 | 69.9 ± 16.3 | 0.1 |
|
| ||||||
| 9-<13 years old | N = 495 | N = 1,319 | N = 1,200 | N = 198 | ||
| Age (yr) ± SD | 11.9 ± 1.0 | 11.1 ± 1.3 | <0.0001 | 11.0 ± 1.2 | 10.9 ±- 1.2 | 0.7 |
| Sex (male) | 214 (43%) | 658 (50%) | 0.013 | 482 (40%) | 104 (53%) | 0.0014 |
| Race (white)* | 299 (84%) | 7684 (85%) | 0.36 | 674 (86%) | 116 (89%) | 0.56 |
| Height (cm) ± SD | 154.1 ± 10.7 | 145.9 ± 9.9 | <0.0001 | 145.2 ± 10.1 | 145.5 ± 9.0 | 0.7 |
| Height (percentile) ± SD | 74.2 ± 27.8 | 65.6 ± 26.9 | <0.0001 | 63.7 ± 27.5 | 67.1 ± 25.8 | 0.1 |
| BMI (kg/m2) ± SD | 20.5 ± 4.4 | 19.7 ± 4.0 | 0.0003 | 19.9 ± 4.1 | 20.7 ± 4.8 | 0.01 |
| BMI (percentile) ± SD | 66.8 ± 27.0 | 66.9 ± 26.8 | 0.9 | 68.7 ± 26.7 | 71.3 ± 28.5 | 0.2 |
| SBP (mmHg) ± SD | 117.7 ± 7.4 | 116.7 ± 6.8 | 0.005 | 121.7 ± 8.7 | 128.9 ± 7.2 | <0.0001 |
| DBP (mmHg) ± SD | 66.6 ± 10.9 | 69.7 ± 12.0 | <0.0001 | 72.2 ± 12.5 | 76.6 ± 12.3 | <0.0001 |
| 13-<15 years old | N = 1,399 | N = 449 | N = 586 | N = 91 | ||
| Age (yr) ± SD | 14.1 ± 0.6 | 14.2 ± 0.6 | 0.01 | 14.0 ± 0.6 | 14.2 ±- 0.5 | 0.003 |
| Sex (male) | 772 (55%) | 237 (53%) | 0.38 | 278 (47%) | 48 (53%) | 0.37 |
| Race (white)* | 706 (75%) | 211(80%) | 0.13 | 301 (80%) | 44 (76%) | 0.63 |
| Height (cm) ± SD | 164.7 ± 7.6 | 166.8 ± 8.1 | <0.0001 | 162.9 ± 7.3 | 167.3 ± 7.8 | <0.0001 |
| Height (percentile) ± SD | 67.7 ± 25.6 | 73.6 ± 24.8 | <0.0001 | 62.7 ± 27.1 | 74.2 ± 25.8 | 0.0002 |
| BMI (kg/m2) ± SD | 22.1 ± 4.3 | 22.2 ± 4.8 | 0.8 | 23.1 ± 5.1 | 23.5 ± 4.7 | 0.4 |
| BMI (percentile) ± SD | 69.9 ± 23.4 | 68.8 ± 24.5 | 0.4 | 73.3 ± 23.4 | 77.5 ± 20.3 | 0.1 |
| SBP (mmHg) ± SD | 122.9 ± 2.6 | 118.5 ± 9.2 | <0.0001 | 129.7 ± 7.9 | 131.7 ± 11.1 | 0.03 |
| DBP (mmHg) ± SD | 63.3 ± 11.2 | 77.1 ± 8.7 | <0.0001 | 75.5 ± 13.3 | 80.1 ± 15.1 | <0.0001 |
|
| ||||||
| 15-<18 years old | N = 2,162 | N = 1,099 | N = 597 | N = 294 | ||
| Age (yr) ± SD | 16.2 ± 0.9 | 16.4 ± 0.9 | <0.0001 | 16.0 ± 0.8 | 16.4 ± 0.9 | <0.0001 |
| Sex ( male) | 1,306 (60%) | 719 (65%) | 0.015 | 238 (40%) | 216 (73%) | <0.0001 |
| Race (white)* | 1,391 (78%) | 703 (88%) | <0.0001 | 397 (87%) | 177 (87%) | 0.89 |
| Height (cm) ± SD | 170.3 ± 8.3 | 172.5 ± 8.4 | <0.0001 | 165.5 ± 7.5 | 173.6 ± 7.7 | <0.0001 |
| Height (percentile) ± SD | 58.7 ± 26.8 | 64.5 ± 25.8 | <0.0001 | 49.0 ± 26.8 | 65.3 ± 24.8 | <0.0001 |
| BMI (kg/m2) ± SD | 22.4 ± 4.3 | 22.5 ± 4.2 | 0.6 | 23.5 ± 5.1 | 24.7 ± 5.5 | 0.001 |
| BMI (percentile) ± SD | 61.4 ± 25.4 | 61.7 ± 25.8 | 0.7 | 67.4 ± 25.1 | 72.6 ± 24.2 | 0.003 |
| SBP (mmHg) ± SD | 123.5 ± 2.8 | 123.7 ± 9.0 | 0.3 | 129.6 ± 8.2 | 137.1 ± 9.1 | <0.0001 |
| DBP (mmHg) ± SD | 65.1 ± 10.3 | 75.9 ± 10.1 | <0.0001 | 76.4 ± 11.1 | 79.8 ± 13.6 | <0.0001 |
Race data available for 26,079 participants
HTN: hypertension; CPG: Clinical Practice Guideline; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure
The sensitivity of hypertensive range BPs at any point in childhood predicting adult hypertension was 13.3% (95% CI 12.2%, 14.4%) and 22.1% (95% CI 20.9%, 23.5%), as defined by the Fourth Report and the CPG, respectively, while the specificity was 92.6% (95% CI 92.1%, 93.1%) and 86.3% (95% CI 85.5%, 87.0%), respectively (p <0.0001). The increased sensitivity and reduced specificity of the CPG in detecting self-reported adult hypertension was noted across each age range (Table 7). The NPV and PPVs were not substantially different between the Fourth Report and CPG at various age ranges (Table 7).
Table 7.
Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV), with 95% confidence intervals, of a pediatric hypertensive measure at a single visit across various age ranges predicting self-reported adult hypertension.
| 6 - <9 yo | 9 - <13 yo | 13 - <15 yo | 15 - <18 yo | |||||
|---|---|---|---|---|---|---|---|---|
| 4th | CPG | 4th | CPG | 4th | CPG | 4th | CPG | |
| Sensitivity | 0.11 [0.10, 0.13] |
0.19 [0.17, 0.21] |
0.12 [0.10, 0.14] |
0.225 [0.20, 0.25] |
0.18 [0.15, 0.22] |
0.21 [0.18, 0.25] |
0.19 [0.16, 0.22] |
0.32 [0.28, 0.36] |
| Specificity | 0.95 [0.94, 0.95] |
0.89 [0.88, 0.90] |
0.92 [0.91, 0.93] |
0.85 [0.84, 0.86] |
0.90 [0.88, 0.92] |
0.88 [0.86, 0.90] |
0.90 [0.88, 0.92] |
0.79 [0.76, 0.82] |
| NPV | 0.73 [0.71, 0.74] |
0.73 [0.72, 0.75] |
0.72 [0.71, 0.73] |
0.73 [0.72, 0.74] |
0.67 [0.64, 0.69] |
0.67 [0.64, 0.70] |
0.68 [0.66, 0.71] |
0.69 [0.66, 0.72] |
| PPV | 0.45 [0.40, 0.50] |
0.41 [0.37, 0.45] |
0.37 [0.33, 0.42] |
0.38 [0.34, 0.41] |
0.50 [0.43, 0.58] |
0.49 [0.42, 0.56] |
0.50 [0.43, 0.57] |
0.44 [0.39, 0.49] |
4th: Fourth Report; CPG: Clinical Practice Guideline
In the logistic regression modeling, a significant difference with respect to hypertensive categorization status was noted across study sites. Thus, study site was included in all reported outcomes of the analysis. The ROC curves, both for the whole pediatric age range (6-<18 years old) and for adolescents (≥13 years old), demonstrated similar associations between hypertensive range BP categorization when defined by the Fourth Report and CPG and selfreported hypertension in adulthood, with c-statistics ranging from 0.61 – 0.68 (Figure 2). The association between childhood BP in the hypertensive range and self-reported hypertension was stronger when the analysis was restricted to youth ≥13 years old. For example, for the CPG, the c-statistic was 0.62 (95% CI 0.61 – 0.63) for all ages and 0.67 (95% CI 0.65 – 0.69) for adolescents ≥13 years old. Odds ratios for self-reported hypertension were similar between the Fourth Report and CPG for all ages and when restricted to adolescents (1.8 for pre-hypertension/EBP readings and ranging between 2.3–2.7 for hypertensive readings) (Table 8, online).
Figure 2.
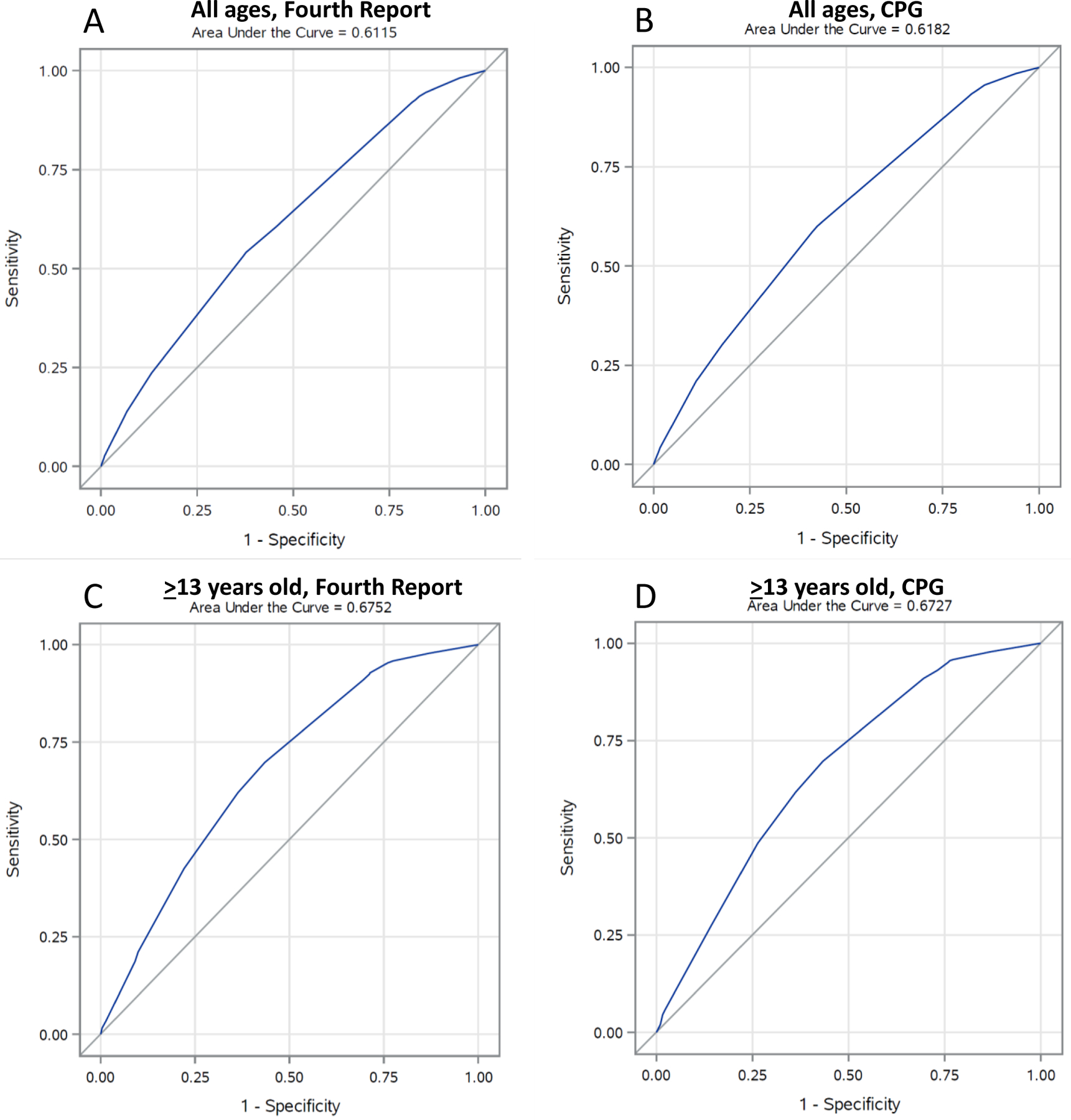
Receiver operating characteristic (ROC) curves evaluating prediction of self-reported hypertension in adulthood for a pediatric BP reading in the hypertensive range as defined by the Fourth Report or the CPG, for children at all ages or those ≥13 years old.
Table 8 (Online).
Odds ratios (OR) with 95% confidence intervals (CI) of self-reported hypertension in adulthood for youth with pre-hypertensive/elevated blood pressure (EBP) and hypertensive measures from a single visit, as defined by the Fourth Report and Clinical Practice Guideline (CPG)
| OR (95% CI) | ||
|---|---|---|
| Pre-hypertension/EBP Range | Hypertensive Range | |
| Fourth Report, all ages | 1.8 (1.6 – 2.0) | 2.4 (2.1 – 2.7) |
| Fourth Report, ≥13 years old | 1.8 (1.5 – 2.2) | 2.7 (2.1 – 3.5) |
| CPG, all ages | 1.8 (1.6 – 2.0) | 2.3 (2.1 – 2.5) |
| CPG, ≥13 years old | 1.8 (1.4 – 2.2) | 2.4 (1.9 – 2.9) |
Study site included in the logistic regression analysis model and for each OR reported in the table
Discussion
Using data from over 30,000 youth from the i3C Consortium cohorts, the prevalence of hypertensive BP readings determined from the more recently published CPG tables (13.5% for stage 1 and 2.5% for stage 2) was significantly greater than the prevalence determined from the Fourth Report tables (7.6% for stage 1 and 1.3% for stage 2, p<0.0001). However, this study expands on prior comparisons between CPG and the Fourth Report by showing that, despite the increased prevalence, the CPG did not significantly alter the PPV or NPV, nor did it improve overall associations between BP measurements in hypertensive ranges in youth with selfreported hypertension in adulthood.
The increased prevalence of hypertensive BP measurements as defined by the CPG in this study is consistent with the findings of most previous studies that have compared the CPG to the Fourth Report.4, 12–16 Similar to the findings in the present study, a study in 10-<18 year old youth reported that the CPG increased the prevalence of stage 1 hypertensive BP from 6% to 10% and stage 2 hypertensive BP from 2% to 3%, while the prevalence of pre-hypertensive/elevated BP measurement decreased from 21% to 16%.12 A particularly noteworthy finding in the present study was that the vast majority of children aged 6 - <9 and 9 - <13 years old (91% and 73%, respectively) were re-classified from pre-hypertensive to stage 1 hypertensive BP ranges using the CPG. Previous studies have shown a similar pattern of re-reclassification (70% in 10–12 year olds 14 and 53% in youth 3 – 18 years, with increased re-classification in those <13 years old13). As a result of generating normative values from non-overweight and obese individuals, percentile cut-points in the CPG are about 4 mmHg lower than in the Fourth Report. While this difference of 4 mmHg is small in absolute terms, 4 mmHg encompasses most of the range of BPs that would have previously fallen between pre-hypertension and stage 1 hypertension in the Fourth Report, as demonstrated in Figure 3 (online). Thus, as a result of the revised normative values, the majority of patients defined as having pre-hypertension by the Fourth Report now re-classify to stage 1 hypertension by the CPG. The lower re-classification rates observed for adolescents were similar to other previously reported findings.12, 15 As was demonstrated in a previous study by Khoury et al.,12 most of this re-classification in adolescents was due to the decrease in the CPG BP cut-point for diastolic stage 1 hypertension to 80 mmHg. Re-classification from stage 1 to stage 2 hypertensive ranges occurred to the greatest degree (31%) in the 15 - <18 year olds, due to the larger absolute difference between the CPG static cut-points and the Fourth Report percentile cut-points for stage 2 hypertension.
Figure 3 (online).
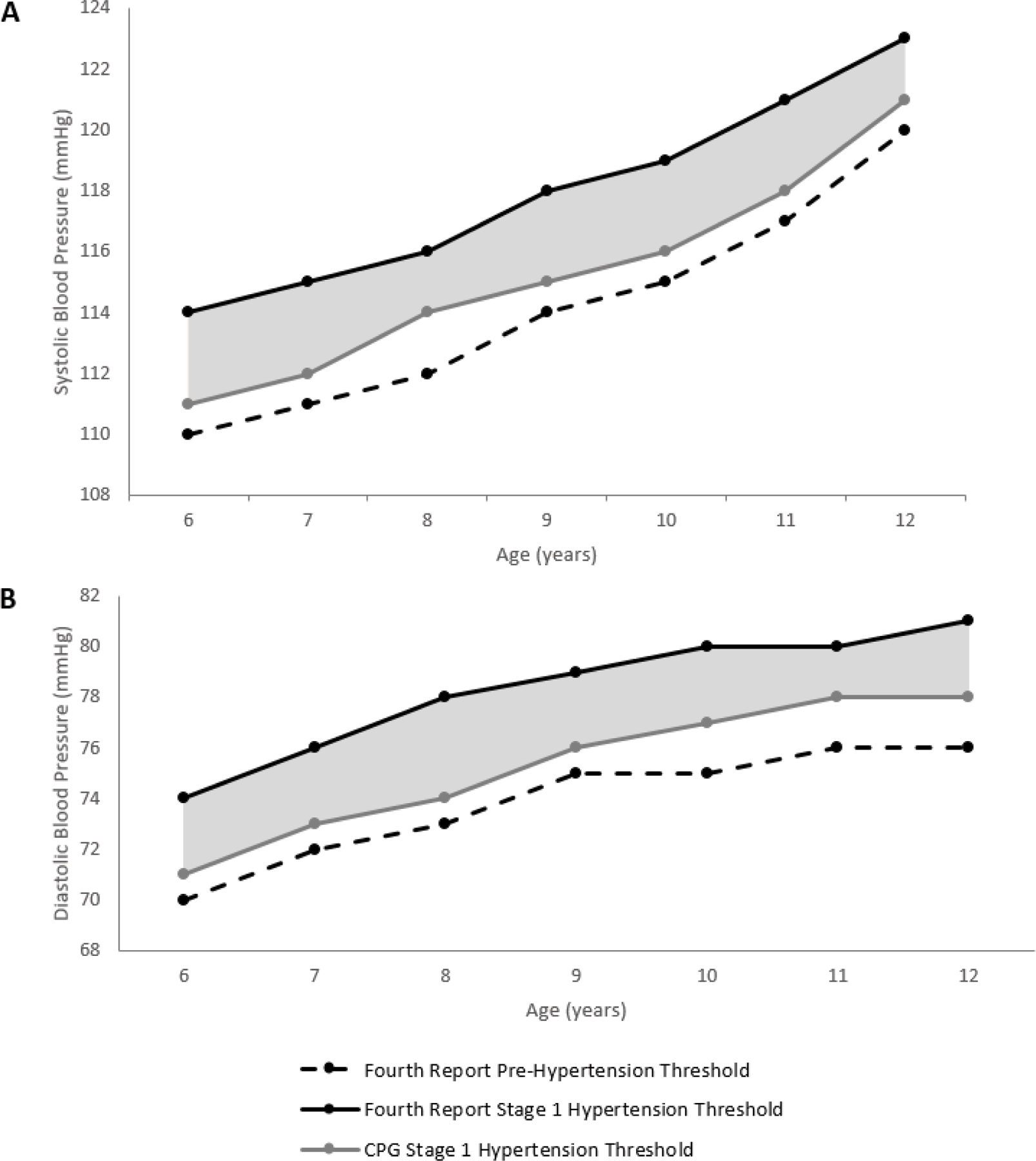
Threshold cut-points (A. systolic and B. diastolic) for 6–12 year old males (height 50th percentile), demonstrating the pre-hypertension blood pressure (BP) ranges and the stage 1 hypertension cut-point as defined by the Clinical Practice Guideline (CPG). The shaded area represents all BPs that would result in re-classification from pre-hypertension to stage 1, as defined by the CPG.
The present study found an increased sensitivity of predicting self-reported hypertension in adulthood for youth with hypertensive BP measurements when defined by the CPG compared with the Fourth Report. Similarly, a prior study demonstrated that re-classification as a result of the CPG improved the sensitivity of target organ damage detection in youth,12 including left ventricular mass, a key measure given its associations with manifest cardiovascular disease in adults.17 Data from the Bogalusa Heart Study has further demonstrated that the CPG improved the sensitivity of predicting left ventricular hypertrophy in adulthood.18 It is important to note, however, that with this improved sensitivity and increased prevalence comes a correspondingly reduced specificity, which may have important implications, including an increase in clinical evaluations, laboratory testing, and other diagnostic investigations (e.g., echocardiography, ultrasonography, and 24-hour ambulatory BP monitoring) in patients not at-risk of developing hypertension in adulthood or premature cardiovascular disease or target organ damage. While the CPG helps identify more cases of pediatric hypertension that will correspond with hypertension in adulthood, a higher false-positive rate indicates that more children will be diagnosed with hypertension that will be normotensive in adulthood. Moreover, the associations between isolated hypertensive readings in childhood with self-reported adult hypertension remained noticeably weak, regardless of the definition used (CPG or Fourth Report), and the PPV and NPV were not significantly impacted. Thus, regardless of the pediatric definition used, our ability to predict the risk for hypertension in adulthood on the basis of hypertensive BP readings at a single time point in youth is limited. This limitation of singular hypertensive measurements in childhood is supported by similar findings in a prior study from the i3C Consortium7 and systematic review and meta-analysis findings,19 among others. Rather, the trajectory of BP measurements throughout childhood demonstrates a stronger association with hypertension in adulthood. In an effort to help clinicians identify youth with hypertension who are at risk of future cardiovascular disease, evaluations of cardiac and vascular target organ damage and surrogate measures of atherosclerosis (such as carotid intima media thickness) should be considered, given their associations both with pediatric hypertension and manifest cardiovascular disease in adulthood.20, 21 Ultimately, defining the relation with adult cardiovascular events will determine the role of BP measurement in children.
Limitations
There are several limitations that should be considered when interpreting the results of the present study. First, of 34,014 participants involved in the longitudinal cohorts, 46% (15,667) were successfully recruited into the HHS follow-up in adulthood, of which 82% (12,761) had available data on self-reported hypertension. A higher proportion of participants with self-reported BP status in adulthood were female compared to those without self-reported BP status (57.3% vs. 46.5%). This sex difference may have implications in the associations observed between childhood hypertensive BP measurements and self-reported hypertension in adulthood, particularly as the prevalence of hypertension in middle-aged males has previously been demonstrated to be higher than in middle-aged females.3 Other differences were noted between those with and without self-reported hypertension status in adulthood, including age, systolic and diastolic BP, and height, weight, and BMI. While these observed differences were statistically significant, they were small in absolute terms (Table 2) and are less likely than the observed sex differences to represent important differences in the study population.
As the study participants were predominately white, the generalizability of the findings may be limited. Moreover, race as a variable for self-reported hypertension status was not consistently available across the study cohorts and thus was not included. The use of BP measurements from one time-point for classification (versus three time points required for a clinical diagnosis of hypertension at separate clinical encounters within a pre-specified timeframe21) may account for the relatively higher prevalence of BP readings in hypertensive ranges (7.6% and 1.3% for stage 1 and 2 hypertension categorization, respectively, as defined by the Fourth Report) compared to the <2–4% prevalence of hypertension that has typically been reported in clinical studies of children and adolescents.22–25 Despite this, the re-classification observed as a result of the CPG is a direct result of differing definitions of hypertension, and thus the relative degree of re-classification is similar to what would be observed within a clinical context. However, the use of single-visit BP readings may have negatively impacted observed associations with self-reported hypertension. Whether the association between a clinical diagnosis of hypertension and hypertension in adulthood is similarly weak to those observed for singular BP measurements in childhood requires further study.
Key biases must be considered when interpreting self-reported hypertension, including recall bias, selection bias, and survivorship bias. However, the validity of the self-reported hypertension is supported by a similar prevalence of hypertension in another self-reported large cohort study26 and true measured hypertension in the 2011–2014 NHANES.27 Moreover, for most of the time of self-report (2014–2019), hypertension was relatively uniformly defined as ≥140/90.28 Thus, newer, lower definitions of adult hypertension3 may not be as reflected in our self-reported data. We expect that lower cut-points for adult hypertension would have improved the specificity but reduced the sensitivity of pediatric hypertension (both as defined by the CPG and Fourth Report) in detecting adult hypertension.
Conclusion
This study confirms that changes made in the standardized BP tables from the Fourth Report to CPG result in a significant increase in the prevalence of childhood BP readings in hypertensive ranges, with increased sensitivity but reduced specificity of predicting self-reported adult hypertension. However, despite the increased sensitivity, BP measurement categorization via the CPG demonstrated similar and weak associations with self-reported adult hypertension when compared with the Fourth Report, and no significant impact on PPV and NPV was observed. Thus, clinicians should be cognizant of the limited utility of isolated hypertensive BP readings in childhood.
Acknowledgements:
We wish to express our gratitude for study participants in each of the longitudinal assessments, as their repeated involvement made this work possible.
Funding:
NHLBI R01 HL121230
Abbreviations
- BP
blood pressure
- CPG
Clinical Practice Guideline
- HHS
Heart Health Survey
- i3C
International Childhood Cardiovascular Cohort
- NPV
negative predictive value
- PPV
positive predictive value
- ROC
receiver operating characteristic
Footnotes
Conflicts of Interest: None
Prior presentation: Aspects of this work was presented as a poster at the 2019 AHA Epi/Lifestyle Scientific Sessions
References
- [1].The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555–76. [PubMed] [Google Scholar]
- [2].Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017. [DOI] [PubMed]
- [3].Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017. [DOI] [PubMed]
- [4].Blanchette E, Flynn JT. Implications of the 2017 AAP Clinical Practice Guidelines for Management of Hypertension in Children and Adolescents: a Review. Curr Hypertens Rep 2019;21:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sinaiko AR, Jacobs DR Jr., Woo JG, Bazzano L, Burns T, Hu T, et al. The International Childhood Cardiovascular Cohort (i3C) consortium outcomes study of childhood cardiovascular risk factors and adult cardiovascular morbidity and mortality: Design and recruitment. Contemp Clin Trials 2018;69:5564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Dwyer T, Sun C, Magnussen CG, Raitakari OT, Schork NJ, Venn A, et al. Cohort Profile: the international childhood cardiovascular cohort (i3C) consortium. Int J Epidemiol 2013;42:86–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Urbina EM, Khoury PR, Bazzano L, Burns TL, Daniels S, Dwyer T, et al. Relation of Blood Pressure in Childhood to Self-Reported Hypertension in Adulthood. Hypertension 2019;73:1224–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998;338:1650–6. [DOI] [PubMed] [Google Scholar]
- [9].Juhola J, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation 2013;128:217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics 2007;120:340–5. [DOI] [PubMed] [Google Scholar]
- [11].Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data 2000:1–27. [PubMed]
- [12].Khoury M, Khoury PR, Dolan LM, Kimball TR, Urbina EM. Clinical Implications of the Revised AAP Pediatric Hypertension Guidelines. Pediatrics 2018;142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Condren M, Carter J, Mushtaq N, Puckett S, Kezbers K, Sabet S, et al. The impact of new guidelines on the prevalence of hypertension in children: A cross-sectional evaluation. J Clin Hypertens (Greenwich) 2019. [DOI] [PMC free article] [PubMed]
- [14].Larkins NG, Teixeira-Pinto A, Kim S, Burgner DP, Craig JC. The population-based prevalence of hypertension and correlates of blood pressure among Australian children. Pediatr Nephrol 2019. [DOI] [PubMed]
- [15].Sharma AK, Metzger DL, Rodd CJ. Prevalence and Severity of High Blood Pressure Among Children Based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr 2018;172:557–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Al Kibria GM, Swasey K, Sharmeen A, Day B. Estimated Change in Prevalence and Trends of Childhood Blood Pressure Levels in the United States After Application of the 2017 AAP Guideline. Prev Chronic Dis 2019;16:E12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Verdecchia P, Carini G, Circo A, Dovellini E, Giovannini E, Lombardo M, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol 2001;38:1829–35. [DOI] [PubMed] [Google Scholar]
- [18].Du T, Fernandez C, Barshop R, Chen W, Urbina EM, Bazzano LA. 2017 Pediatric Hypertension Guidelines Improve Prediction of Adult Cardiovascular Outcomes. Hypertension 2019:HYPERTENSIONAHA11812469. [DOI] [PMC free article] [PubMed]
- [19].Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 2008;117:3171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Khoury M, Urbina EM. Cardiac and Vascular Target Organ Damage in Pediatric Hypertension. Front Pediatr 2018;6:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017;140. [DOI] [PubMed] [Google Scholar]
- [22].Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA 2007;298:874–9. [DOI] [PubMed] [Google Scholar]
- [23].McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr 2007;150:640–4, 4.e1. [DOI] [PubMed] [Google Scholar]
- [24].Chiolero A, Cachat F, Burnier M, Paccaud F, Bovet P. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight. J Hypertens 2007;25:2209–17. [DOI] [PubMed] [Google Scholar]
- [25].Lo JC, Sinaiko A, Chandra M, Daley MF, Greenspan LC, Parker ED, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics 2013;131:e415–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Fang J, Gillespie C, Ayala C, Loustalot F. Prevalence of Self-Reported Hypertension and Antihypertensive Medication Use Among Adults Aged >/=18 Years - United States, 2011–2015. MMWR Morbidity and mortality weekly report 2018;67:219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Yoon SS, Carroll MD, Fryar CD. Hypertension Prevalence and Control Among Adults: United States, 2011–2014. NCHS Data Brief 2015:1–8. [PubMed]
- [28].Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52. [DOI] [PubMed] [Google Scholar]


