Abstract
Asthma is a common respiratory disease, and immune system dysregulation has direct relevance to asthma pathogenesis. Probiotics and prebiotics have immunomodulatory effects and can regulate immune responses and may attenuate allergic reactions. Therefore, in this study, we explored the role of probiotics and prebiotics in regulating acute airway inflammation and the TLR4/NF-kB pathway. Allergic asthma model of BALB/c mice was produced and treated with probiotics (LA-5, GG, and BB-12) and prebiotics (FOS and GOS). Then AHR, BALF cells count, EPO activity, IL-4, 5, 13, 17, 25, 33, as well as IFN-γ, total and OVA-specific IgE, IgG1, Cys-LT, LTB4, LTC4, and TSLP levels were measured. Also, the GTP/GOT assay was performed and gene expression of Akt, NLR3, NF-kB, PI3K, MyD88, TLR4, CCL11, CCL24, MUC5a, Eotaxin, IL-38, and IL-8 were determined. Finally, lung histopathological features were evaluated. Treatment with probiotics could control AHR, eosinophil infiltration to the BALF and reduce the levels of immunoglobulins, IL-17, GTP and also decrease mucus secretion, goblet cell hyperplasia, peribronchial and perivascular inflammation and also, EPO activity. It could reduce gene expression of TLR4 and CCL11. On the other hand, IL-38 gene expression was increased by both probiotic and prebiotic treatment. Treatment with probiotics and prebiotics could control levels of IL-4, 5, 13, 25, 33, leukotrienes, the gene expression of AKT, NLR3, NF-κB, MyD88, MUC5a. The prebiotic treatment could control peribronchial inflammation and PI3K gene expression. Both of the treatments had no significant effect on the GOT, TSLP and IL-8, eotaxin and CCL24 gene expression. Probiotics and prebiotics could induce tolerance in allegro-inflammatory reactions and alter immune responses in allergic conditions. Probiotics could also modulate cellular and humoral immune responses and prevent allergic disorders.
Keywords: Allergy, Microbe, Diet, Immunomodulation, Asthma
Main findings of the study
Probiotics controls AHR, eosinophil infiltration to the perivascular and BALF, levels of immunoglobulins, IL-17, GTP and also mucus secretion, goblet cell hyperplasia, EPO activity. It could reduce gene expression of TLR4 and CCL11,
Probiotics and prebiotics control levels of cytokines (IL-4, 5, 13, 25, and 33), leukotrienes, the gene expression of AKT, NLR3, NF-κB, MyD88, MUC5a, peribronchial inflammation and increase IL-38 gene expression.
Prebiotic controls and PI3K gene expression.
Introduction
Asthma, pneumonia, and lung injury are common acute respiratory problems in the clinic and allergic asthma is a relatively prevalent condition worldwide. Patients with asthma cannot be cured completely, and all available treatments generally aim to control the pathological condition. There is a huge economic burden on patients and governments [1, 2]. Allergic asthma is one of the most important health problems, especially in developed countries. Several pathways are involved in the pathophysiology of allergic asthma. Immune system dysregulation is directly related to health and is involved in the pathogenesis of a variety of immune disorders, including allergic diseases. On the other hand, the imbalance of inflammatory and anti-inflammatory factors and also dysregulation of the lung immune system through the TLR4/NF-kB signaling pathway can lead to pulmonary oxidative stress and injury [3, 4].
The therapeutic applications of probiotics and prebiotics in diseases such as asthma and pneumonia were not studied very well. Probiotics and prebiotics have been shown to possess immunomodulatory effects and be involved in the pathophysiology of various diseases. Short-chain (galacto-oligosaccharides) and long-chain (fructo-oligosaccharides or lcFOS) prebiotics along with probiotics (beneficial microbes) have also been noted to prevent allergic sensitization via regulating immune responses. Beneficial probiotic bacteria can modulate immune cells such as Th1, Th2, Th17, Treg, and also B cells [5, 6].
There are many microbial infections can active TLR4 signaling and probiotics as part of commensal gut microbiota, can have effect on the TLRs, especially TLR4 [7, 8]. LPS is structural material of bacteria and TLR4 activation by bacteria is initiated via LPS/TLR4/NF-kB pathway [9, 10]. On the other hand, LPS can induce acute lung injury and inflammation, which leads to accumulation of inflammatory cells in the lung and airway [11, 12]. OVA can induce allergic asthma model but, OVA-LPS can induce asthma and acute inflammation in airways. Also, it can involve with TLR4 and actives TLR4 signaling. Therefore, in this study, we explored the functional mechanisms of probiotics and prebiotics in regulating of the host’s defense against LPS-OVA-induced lung injury and airway inflammation and the TLR4/NF-kB pathway. Also, immuno-inflammatory responses and pulmonary pathological features were studied in the mice that were treated with probiotics and prebiotics. The effect of probiotics and prebiotics of on acute form of allegro-inflammatory airway asthma with TLRs involving was studied.
Material and methods
Reagents and chemicals
OVA and LPS were procured from Sigma-Aldrich. Probiotics and prebiotics were obtained from Caruso Natural Health (Sydney, NSW, Australia) and Sebogard Oral, Cantabria Labs Difa Cooper Caronn (Pertusella, Italy), respectively. ELISA kits for total IgE were purchased from BD Biosciences (USA); OVA-specific IgE was prepared from MyBiosource (USA); IgG1 from Abcam (USA); Cys-LT from Cayman Chemical Ann Arbor (USA); LTB4 and LTC4 from MyBiosource (USA); and TSLP from Rndsystems (USA); and cytokines ELISA kits BD Biosciences (USA). All the chemicals and solvents used in various analyses had analytical grades.
Experimental animals
Total of 90 male BALB/c mice (6–8 weeks) were initially acclimatized to standard animal laboratory conditions for one week prior to experiments. The experiments were strictly conducted in accordance with the protocols approved by the Institutional Animal Ethical Committee (IAEC).
OVA-LPS sensitization and challenge
For the sensitization, challenge, and treatment protocol, mice were randomly divided into six groups (n = 15/group, five for AHR, five for histopathology, and five for immune-biochemical analyses). Group I was the non-sensitized control group; group II was the OVA + LPS control group, and group III received OVA + LPS + probiotics. Each probiotic oral dose consisted of multi-strain probiotics N25 billion CFU [containing Lactobacillus acidophilus LA-5 (7.5 billion), L. rhamnosus GG (8.75 billion CFU), and Bifidobacterium animalis subspecies lactis BB-12 (8.75 billion CFU)] [13]. Group IV received OVA + LPS + prebiotics [FOS and GOS (10 mg/kg, BW, PO)] in PBS solution. Two treatments were diluted in PBS solution and administrated via oral gavage [14]. Group V was the OVA control group, and group VI was the LPS control group.
For creating asthma models, mice were sensitized on days 1, 7, and 14 by the IP injection of 100 μg OVA emulsified in 1 mg aluminum hydroxide gel in a total volume of 200 μL. On days 15, 17, and 19 after the initial sensitization, the animals of the groups II, III, and IV were challenged IN with OVA + LPS (50 μg of OVA combined with 1 μg of LPS in saline in a total volume of 50 μL) and on days 21, 23, and 25. The mice were challenged for 30 min with 3% OVA aerosol (w/v) in saline. Group V was received OVA and group VI was received LPS following the same protocol. Exposure to the aerosolized solution was done in a closed chamber (40 × 20 × 20 cm). The animals in the healthy control group were exposed to PBS following the same protocol. Treatments with probiotics and prebiotics were done once a day from the day 15 to 25 at four hours after OVA-aerosol inhalation. During the study, all animals received food and water ad libitum. On day 27th after the last OVA challenge, sampling was done.
Assessment of AHR in response to methacholine challenge
The effects of probiotics and prebiotics on AHR in asthmatic mice were assessed by whole-body plethysmograph and MCh challenge test via intubation. AHR was measured on day 27th after the last challenge by determining the enhanced pause (i.e., the Penh value). Tube of the ventilator was connected to the trachea after anesthesia and surgery. Mice were anesthetized with 1.5% pentobarbital sodium, then tracheotomized, and finally connected to a ventilator. Baseline parameters were determined after exposure to aerosolized PBS for 3 min, followed by exposure to the increasing concentrations of aerosolized MCh (1, 2, 4, 8, 16, and 32 mg/ml in PBS). Each dose was nebulized for 15 min, and airway responses were recorded for 5 min. Following each administration through the inlet of the main chamber, the Penh was recorded for 5 min. The mean Penh values were measured during each 5-min period and for each dose and plotted against changes from the baseline per dose of MCh. Differences in Penh values respective to the baseline at each concentration were used to compare airway reactivity between the experimental groups.
Collection of BALF and differential cell count
After anaesthetization, 24 h after the last challenge, the mice were euthanized by CO2; then tracheotomy was performed. Lungs were lavaged for three times with 1.0 ml aliquots of PBS via a cannulated tracheal tube (1.0 ml × 3). Afterward, BALF was pooled and cryocentrifuged (1500 rpm, 10 min, 4 °C). The supernatant was separated and stored at − 80 °C for immune-biochemical analyses while the cell sediment was used for cell/gene expression studies.
To perform a differential cell count, a total of 2–4 × 104 BALF cells were placed on a slide and centrifuged (750 rpm, 2 min) using a cytospin machine. The slides were dried, and cells were stained using Giemsa. The absolute number of Eos was determined by microscopical analysis.
EPO activity
EPO activity was determined in BALF. Briefly, 1 ml of a substrate solution containing 0.1 mM O-phenylenediamine dihydrochloride, 0.1%Triton X-100, and 1 mM hydrogen peroxide in 0.05 M Tris (hydroxymethyl) aminomethane hydrochloride was added to 1 ml BALF, and the mixture was incubated at 37 °C for 30 min. The reaction was stopped by adding 0.5 ml 4 M sulfuric acid, and the absorbance was read at 492 nm.
Analysis of cytokines in BALF
The concentrations of IL-4, -5, -13, -17, -25, -33 and IFN-γ in BALF were measured via specific ELISA kits according to the manufacturer’s instructions.
Serum immunoglobulins
IgG1, total and OVA-specific IgE levels in serum were measured by ELISA following the manufacturer’s protocol.
Eicosanoid assessment and biofactors’ levels
In BALF supernatant, Cys-LT, LTB4, LTC4, and TSLP levels were assayed using ELISA kits following the manufacturer’s protocol.
GTP/GOT assay
Oxidative stress in the lung was examined using a glutathione assay kit (Cayman Chemicals) according to the manufacturer’s instructions.
Quantitative real-time PCR
RNA from BALF cells was extracted using the RNAiso Plus kit following the manufacturer’s protocol. One µg RNA was reversed transcribed to cDNA in a total volume of 20 µl using the PrimeScript RT Reagent Kit. Target genes’ expressions (Akt, NLR3, NF-kB, PI3K, MyD88, TLR4, CCL11, CCL24, MUC5a, Eotaxin, IL38, and IL8) were studied using SYBR Green Master Mix and specific primers.
The specific primers’ sequences (5ʹ–3ʹ) for RNA amplification were as follows:
GAPDH Forward: TGTTCCTACCCCCAATGTGT, Reverse: GGTCCTCAGTGTAGCCCAAG as housekeeping gene; MUC5a Forward: CAGGACTCTCTGAAATCGTACCA, Reverse: AAGGCTCGTACCACAGGGA;
TLR4 Forward: AGTGGGTCAAGGAACAGAAGCA, Reverse: CTTTACCAGCTCATTTCTCACC; NLR3 Forward: ACCAGCCAGAGTGGAATGA, Reverse: GCGTGTAGCGACTGTTGAG; IL-8 Forward: ACTGAGAGTGATTGAGAGTGGAC, Reverse: AACCCTCTGCACCCAGTTTTC; IL-38 Forward: CCTGGCGTGTGTAAAGACAA, Reverse: CAGATCCCAAGCTTCTCTGG;
CCL24 Forward: AGGCAGTGAGAACCAAGT, Reverse: GCGTCAATACCTATGTCCAA; CCL11: Forward GGCTTCATGTAGTTCCAGAT, Reverse: CCATTGTGTTCCTCAATAATCC; PI3K Forward: CTCTCCTGTGCTGGCTACTGT, Reverse: GCTCTCGGTTGATTCCAAACT; Akt Forward: ATCCCCTCAACAACTTCTCAGT, Reverse: CTTCCGTCCACTCTTCTCTTTC; Eotaxin Forward: CTGCTCACGGTCACTTCCTT, Reverse: GGGGTCAGCACAGATCTCTT; NF-kB Forward: ACCTTTGCTGGAAACACACC, Reverse: ATGGCCTCGGAAGTTTCTTT; MyD88 Forward: TGGCATGCCTCCATCATAGTTAACC, Reverse: GTCAGAAACAACCACCACCATGC.
Lung histopathological study
Lung tissues were isolated and fixed in formalin; then histological slides were produced and stained with H&E and PAS stains. The slides were evaluated under the light microscopy for detecting eosinophilic infiltration around bronchi and vessels, goblet cell hyperplasia, and mucus hypersecretion. It was performed by two investigators as pathologist, blinded to the status of the animal. The mucus production ratio was determined by visually scoring the intensity of PAS stain (in 10 randomly selected microscopy fields). The score 0 was used for absence of any observable PAS stain and 0. 5 score was used for low level of PAS stain. The score 1 was used when approximately 25% of the space inside of the bronchi was filled with mucus, score 2 fore 50%, score 3 fore 75% and score 4 for 100%. Moreover, number of the goblet cells was quantified per 100 epithelial cells at several randomly microscopy fields on sections at 400 × magnification. The calculated number was GCI. The GCI was classified to 4 scores as follows; GCI < 5%: score 0, 5% ≤ GCI < 25%: score 1, 25% ≤ GCI < 50%: score 2: 50% ≤ GCI < 75%: score 3, 75% ≤ GCI ≤ 100%: score 4. Population of the eosinophils was examined at 1000 × magnification. Absence or presence few eosinophils was scored 0, score between 0.1–1 was used for incomplete layer, one complete layer of eosinophils in peribronchial/perivascular was scored 1, two complete layers was 2, three complete layers was 3, more than three complete layers was scored 4 [2].
Statistical analysis
One-way analysis of variance (ANOVA) was used to analyze statistical differences between the groups. All data were expressed as mean ± SEM. Statistical analyses were performed and graphs were drawn in GraphPad Prism 5.0 software (GraphPad Software Inc., San Diego, CA, USA). The level of statistical significance was set at p-value < 0.05.
Results
Effect of probiotic and prebiotic treatment on AHR
AHR is the most important pathological feature of asthma, which distinguishes it from other airway inflammatory diseases. AHR was assessed by measuring Penh value in OVA-LPS sensitized/challenged mice exposed to the increasing concentrations of inhaled MCh. In our study, AHR significantly increased in the OVA and OVA-LPS sensitized asthma groups compared to healthy control animals (p < 0.05). A higher level of Penh indicated a more severe bronchospasm/AHR to the allergen. However, the oral administration of probiotics and prebiotics to OVA-LPS sensitized/challenged mice improved AHR. The results revealed that from the two different prophylactic interventions, only probiotic administration significantly decreased AHR in asthmatic animals (3 ± 0.7 at the dose 4, and 6 ± 0.2 at the dose 32 mg/ml MCh) as compared to the OVA-LPS sensitized/challenged group (7.5 ± 0.4 at the dose 4, and 14 ± 0.7 at the dose 32 mg/ml MCh), (p < 0.05). Treatment of asthmatic animals with prebiotics also reduced AHR (7 ± 0.4 at the dose 4, and 13.5 ± 0.3 at the dose 32 mg/ml MCh), but the results had not significantly difference compared to the OVA-LPS sensitized/challenged group at the all doses of MCh (p > 0.05).
Effect of probiotic and prebiotic treatment on BALF cells and EPO activity
The recruitment of activated eosinophils to airways is a characteristic feature of asthma. Eosinophils from patients with allergic asthma have been reported to excessively produce ROS via multiple mechanisms that are known to contribute to airway inflammation and remodeling. In our study, a significant increase in the eosinophil count of the BALF (9 × 105 ± 6 × 104 cells/ml) was observed in OVA-LPS challenged mice (and also OVA challenged group) as compared to normal healthy animals (3 × 104 ± 1.5 × 104 cells/ml) (p < 0.05). We also found that treatment with probiotics markedly decreased the recruitment of eosinophils (6.4 × 105 ± 6 × 104 cells/ml) in the BALF of asthmatic animals (p < 0.05). Prebiotic treatment also decreased eosinophilic infiltration into BALF (7.6 × 105 ± 4.5 × 104 cells/ml), but the result was not statistically significant compared to the non-treated asthma control group. In this study, a significant increase in the neutrophils count of the BALF was observed in groups that were challenged with LPS [LPS (3.7 × 105 ± 3 × 104 cells/ml), OVA-LPS (3.6 × 105 ± 6 × 104 cells/ml), OVA-LPS probiotics (1.6 × 105 ± 3 × 104 cells/ml) and prebiotics (2.2 × 105 ± 4.5 × 104 cells/ml) treated groups] compared to PBS (4.5 × 104 ± 5 × 103 cells/ml) and OVA (6 × 104 ± 5 × 103 cells/ml) groups. Treatment with probiotics and prebiotics could significantly (p < 0.05) control neutrophils infiltration to the BALF.
EPO plays an important role in the pathogenesis of asthma by mediating oxidative events, leading to the production of ROS and RNS. A considerable reduction of EPO was observed in OVA-LPS sensitized mice after oral treatment with probiotics (0.21 ± 0.02) compared to the non-treated asthma group (0.34 ± 0.04). These results implicated that probiotics could have antioxidant properties by reducing EPO activity. Prebiotics (0.3 ± 0.02); however, had no significant (p > 0.05) effects on EPO activity.
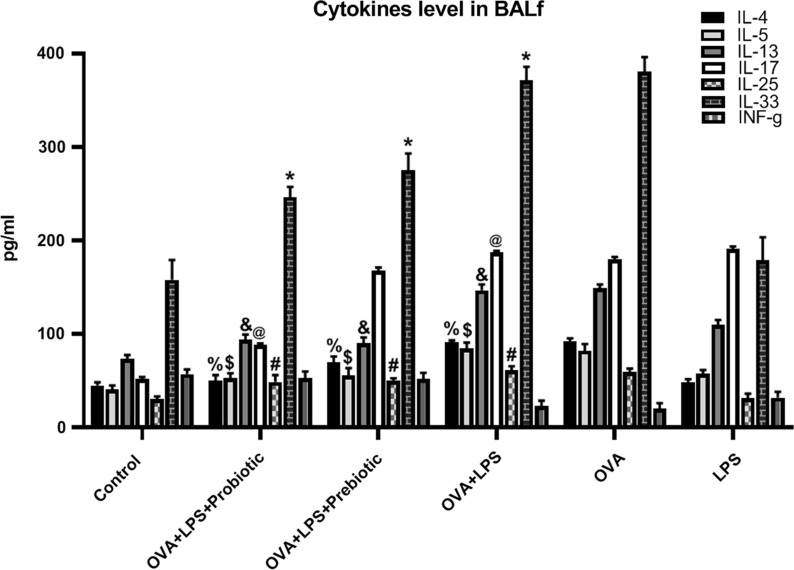
Effect of probiotic and prebiotic treatments on cytokines’ levels
The effects of probiotics and prebiotics on Th2-related inflammatory and pro-inflammatory cytokines (IL-4, IL-5, IL-13, IL-17, IL-25, and IL-33) in BALF were analyzed by ELISA. The levels of all the cytokines analyzed in our study increased significantly (p < 0.05) after sensitization/challenge with OVA and also OVA-LPS as compared to their levels in normal control animals. Substantial reductions (p < 0.05) were observed in the BALF of pro- and pre-biotic treated animals regarding the levels of IL-4 (50.4 ± 5.7 and 69.7 ± 6.4 pg/ml, respectively), IL-5 (53.2 ± 4.9 and 55.7 ± 7.8 pg/ml, respectively), IL-13 (94.25 ± 5.24 and 90.25 ± 6.12 pg/ml, respectively), IL-17 (88.14 ± 2.07 and 167.9 ± 3.24 pg/ml, respectively), IL-25 (48.95 ± 7.24 and 50.24 ± 2.52 pg/ml, respectively), and IL-33 (246.36 ± 10.98 and 274.85 ± 18.25 pg/ml, respectively) as compared to OVA-LPS induced asthmatic mice (IL-4: 91.19 ± 2.03, IL-5: 84.84 ± 6.11, IL-13: 146.78 ± 6.25, IL-17: 187.02 ± 1.89, IL-25: 61.36 ± 4.25, and IL-33: 371.36 ± 14.36 pg/ml) (Fig. 1). The level of IL-17 was significantly decreased only in probiotics treated group, and treatment with prebiotics had no significant (p > 0.05) effect on decreasing of IL-17 level. Besides the induction of Th2-type inflammatory cytokines, allergen sensitization and provocation also significantly decreased IFN-γ level, a Th1-type cytokine, in the BALF. The levels of IFN-γ considerably (p < 0.05) increased in the animals treated with either probiotics or prebiotics (52.90 ± 7.16 and 51.74 ± 6.70 pg/ml, respectively) compared to the non-treated asthma group (22.85 ± 5.90 pg/ml), demonstrating that both the prophylactic treatments had the ability to modulate immune reactions by balancing Th1/Th2 responses in lungs (Fig. 1).
Fig. 1.
Cytokines. The levels of cytokines (IL-4, 5, 13, 17, 25, 33, and IFN-γ) were measured in BALF in all groups. The levels of IL-4, 5, 13, 17, 25, and 33 were increased significantly (p < 0.05) after sensitization/challenge with OVA and also OVA-LPS as compared to their levels in non-sensitized animals and the level of INF-γ were decreased in sensitized/challenged group. The pro- and pre-biotic treated reduced the levels of IL-4, IL-5, IL-13, IL-25 and IL-33 as compared to non-treated OVA-LPS induced asthmatic mice. The level of IL-17 was significantly decreased only in probiotics treated group. The levels of IFN-γ considerably (p < 0.05) increased in the probiotics and prebiotics treated groups. The significant difference (p < 0.05) between treated groups and non-treated OVA-LPS group was shown with symbols that include: * for IL-33, # for IL-25, @ for IL-17, & for IL-13, $ for IL-5, and % for IL-4
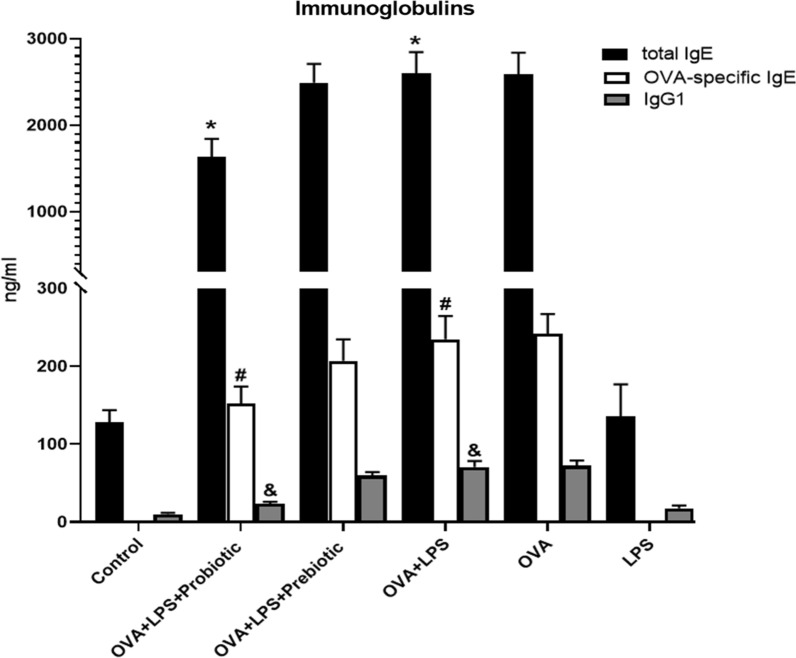
Effect of probiotic and prebiotic treatments on total IgE, OVA-specific IgE, and IgG1
We next investigated the effects of probiotic and prebiotic treatments on the production of total IgE, OVA-specific IgE, and IgG1, showing that these immunoglobulins significantly (p < 0.05) increased in the sensitization group compared to the control group (healthy mice). The oral administration of both probiotics and prebiotics decreased the production of these immunoglobulins in OVA-LPS-sensitized mice as compared to untreated asthmatic animals (Fig. 2). Probiotic treatment significantly decreased the production of total IgE (p < 0.05), OVA-specific IgE (p < 0.05), and IgG1 (p < 0.05) compared to asthma control animals (group II). Treatment with prebiotics could decrease the levels of these immunoglobulins (total IgE, OVA-specific IgE, and IgG1), but the results were not significantly (p > 0.05) different compared to that of the asthmatic group (Fig. 2).
Fig. 2.
Immunoglobulins. The levels of immunoglobulins (total IgE, OVA specific IgE, and IgG1) were measured in all groups. The total IgE, OVA-specific IgE, and IgG1, were significantly increased in the OVA-LPS-sensitized mice compared to the healthy mice (p < 0.05). The administration of probiotics and prebiotics decreased the production of these immunoglobulins, but only probiotic treatment significantly decreased the production of total IgE, OVA-specific IgE and IgG1 (p < 0.05) compared to non-treated asthma group. The significant difference (p < 0.05) between treated groups and non-treated OVA-LPS group was shown with symbols that include: * for total IgE, # for OVA-specific IgE and & for IgG1
Effect of probiotic and prebiotic treatments on leukotrienes’ levels
The levels of Cys-LTs, LTC4, and LTB4 were increased in OVA + LPS group (807.9 ± 37.3, 248.9 ± 20.1, 109.4 ± 9.3 pg/ml respectively) compared with control group (101.9 ± 4.7, 72.0 ± 28.0, 64.1 ± 7.1 pg/ml respectively). Assessing the effects of probiotics and prebiotics on the BALF levels of leukotrienes in asthmatic mice, we observed that the oral administration of probiotics significantly (p < 0.05) reduced the levels of Cys-LTs (374.9 ± 29.1 pg/ml), LTC4 (137.4 ± 24.8 pg/ml), and LTB4 (70.3 ± 9.1 pg/ml). Similarly, the levels of all the assessed leukotrienes decreased in the asthmatic animals treated by prebiotics (Cys-LTs: 429.7 ± 50.8, LTC4: 153.6 ± 37.9: and LTB4 (78.4 ± 7.8 pg/ml).
Effect of probiotic and prebiotic on TSLP
Exposure to airborne allergens including fungal and viral pathogens elevates TSLP level in the epithelial cells of asthmatic lungs. In our study, OVA-LPS challenge in mice increased TSLP (2.8 ± 0.3 ng/ml) level in the BALF as compared to the normal control (0.4 ± 0.1 ng/ml). However, treatment with probiotics (2.1 ± 0.5 ng/ml) and prebiotics (2.6 ± 0.2 ng/ml) reduced TSLP level in the BALF as compared to asthma control animals, but these were not statistically significant (p > 0.05).
Effect of probiotic and prebiotic treatments on GTP and GOT
Oxidative stress in the lung was examined using the glutathione assay. In our study, OVA-LPS challenge resulted in an increase in the levels of GTP (129.4 ± 21.4 IU/L) and GOT (419.7 ± 43.7 IU/L) as compared to the normal control group (GTP: 43.2 ± 10.3 and GOT: 119.4 ± 27.6 IU/L). Only, treatment with probiotics (64.5 ± 19.2 IU/L), but not prebiotics (101.6 ± 17.7 IU/L), significantly (p > 0.05) reduced GTP levels as compared to asthma control animals.
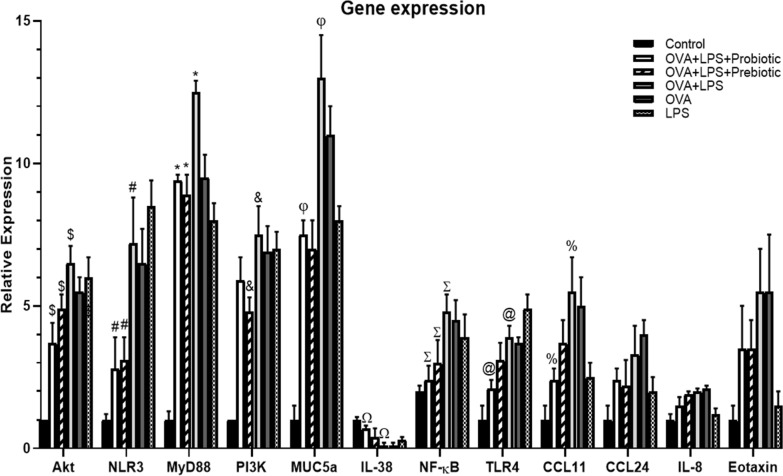
Effect of probiotic and prebiotic treatments on the genes expressions
To evaluate the potential mechanisms of probiotic and prebiotic treatments in reversing the symptoms of asthma and inflammation in allergen-sensitized and challenged animals, the expressions of the genes involved in the PI3K/Akt and TLR4/NF‐κB signaling pathways were examined. The PI3K/AKT signal pathway contributes to the epithelial-mesenchymal transition and airway structural changes and remodeling in chronically and acutely inflamed asthmatic lungs. In an induced asthma model, the gene expression of Th-related cytokines and signaling molecules were assessed. Consistent with previous records, we also observed that the expression levels of Akt, PI3K, NF-kB, and TLR4 significantly increased in the non-treated asthma group. The administration of probiotics and prebiotics dramatically attenuated the expression of Akt. The gene expression of TLR4 and NF‐κB were also found to be elevated in asthmatic mice. As expected, the oral administration of probiotics and prebiotics remarkably inhibited the gene expression of NF‐κB as compared to the non-treated asthma group (Fig. 3). Treatment with probiotics could control expression of TLR4 and treatment with prebiotics remarkably inhibited expressions of PI3K. Taken together, probiotics and prebiotics seemed to be involved in regulating PI3K/Akt- and TLR4/NF‐κB-mediated immune responses.
Fig. 3.
Gene expression. The gene expressions of Akt, PI3k, NLR3, MyD88, NF-κB, TLR4, CCL24, CCL11, Eotaxin, MUC5a, IL-8, and IL-38 were assessed in all groups. GAPDH was used as reference gene. It was observed that the expression levels of Akt, PI3K, NF-kB, and TLR4 significantly (p < 0.05) increased in the OVA-LPS group. The administration of probiotics and prebiotics dramatically attenuated the expression of Akt. Administration of probiotics and prebiotics remarkably inhibited the gene expressions of NF‐κB as compared to the asthma control group (p < 0.05). Treatment with probiotics could control TLR4 expression and prebiotics remarkably inhibited PI3K expressions. In our study, MyD88, MUC5a and NLR3 were up-regulated in the airways of OVA-LPS mice. However, MyD88, NLR3 and MUC5a expression significantly reduced (p < 0.05) in the animals treated with pro-/pre-biotics. The eotaxin gene expression increased in OVA-LPS sensitization/challenge animals. After treatment with probiotics and prebiotics; however, the level of eotaxin reduced (but it was not statistically significant; p > 0.05). On the other hand, the expressions of CCL11 and CCL24 were reduced in the pro- and pre-biotics treated mice, while there was a significant reduction in only CCL11 in the probiotics treated mice (p < 0.05). Also, the up-regulation of IL-8 gene was considerably inhibited following the treatment of OVA-LPS-sensitized mice with probiotics (but not statistically significant; p > 0.05). Allergen exposure significantly (p < 0.05) disturbed the expression of IL-38. Probiotics and prebiotics treatment increased IL-38 gene expression, but only probiotics treatment had significant effect (p < 0.05). The significant difference (p < 0.05) between treated groups and non-treated OVA-LPS group was shown with symbols that include: * for MyD88, # for NLR3, & for PI3k, @ for TLR4, $ for Akt, % for CCL11, Σ for NF-κB, Ω for IL-38 and φ for MUC5a
The sensitization and provocation of mice airways with OVA and LPS are mediated by the MyD88. In our study, MyD88 was up-regulated in the airways of OVA-LPS-treated mice. However, MyD88 expression significantly reduced in the animals treated with pro-/pre-biotics. Similar results were observed for NLR3 (Fig. 3). In the mice models of asthma, MyD88 expression was found to be a critical factor for eosinophilic inflammation in ECs. The reduced expression of MyD88 after treatment with pro-/pre-biotics implicated their role in preventing eosinophilic infiltration in asthma.
Eotaxin is a chemotactic cytokine/chemokine with potent effects on eosinophils. The expression of eotaxin gene increases in asthmatic lungs after allergen challenge, leading to the accumulation of eosinophils in airways and impaired pulmonary function. The results of our study showed an increased expression of eotaxin after OVA-LPS sensitization/challenge in the animals. After treatment with probiotics and prebiotics; however, the level of eotaxin reduced (but it was not statistically significant; p > 0.05), revealing the ability of the both compounds in normalizing the expression of eotaxin in asthmatic lungs. Due to their chemotactic properties for eosinophils, CCL11 and CCL24 chemokines have attracted a great attention in allergic inflammation. Eotaxin-1/CCL11 is important for early eosinophil recruitment to the airways of asthmatics. The number of the cells expressing eotaxin-1 mRNA significantly correlated with the number of eosinophils. In our study, the observed significant increases in the expressions of CCL11 and CCL24 were consistent with the literature. On the other hand, the expressions of CCL11 and CCL24 in the BALF reduced in the mice treated with probiotics and prebiotics while there was a significant reduction in only CCL11 in the OVA-LPS sensitized/challenged mice treated with probiotics (p < 0.05). The data showed that prophylactic probiotics and prebiotics could inhibit the infiltration of eosinophils into asthmatic lungs (Fig. 3).
IL-8 is produced by numerous cell types including monocytes, neutrophils, basophils, eosinophils, alveolar macrophages, bronchial epithelial cells, pulmonary microvascular endothelial cells, and airway smooth muscle cells. In our study, OVA + LPS sensitization and provocation increased IL-8 expression in the BALF samples of asthmatic mice compared to healthy animals. The up-regulation of IL-8 gene was considerably inhibited following the treatment of OVA-LPS-sensitized mice with probiotics as compared to asthma control animals (but not statistically significant; p > 0.05). On the other side, prebiotic treatment did not elicit any significant improvement in the expression of this cytokine (p > 0.05). IL-38, a newly discovered cytokine belonging to the IL-1 family, has been shown to be aberrantly expressed in allergic asthma and COPD in clinical and animal studies. The cytokine suppresses the asthma-induced production of CXCL8, suggesting an inhibitory role for IL-38 in regulating allergic inflammatory responses. Allergen exposure significantly disturbed the expression of IL-38 in mice. All the asthmatic mice treated with oral probiotics and prebiotics showed an increased expression of IL-38 gene in the BALf (Fig. 3). Probiotics and prebiotics treatment increased IL-38 gene expression, but only probiotics treatment had significant effect (p < 0.05).
Increased mucus production is associated with the increased expression of mucin subfamily genes. Mucins are large glycoproteins constituting the major components of the mucus layer. They are produced by goblet cells or submucosal glands in airway epithelia. Out of two principal mucus forming enzymes, MUC5a and MUC5b, the overproduction of MUC5a has a major contribution to airway obstruction. In our study, treating asthmatic mice with probiotics and prebiotics significantly (p < 0.05) reduced MUC5a gene expression when compared to non-treated asthmatic mice (OVA-LPS group) (Fig. 3).
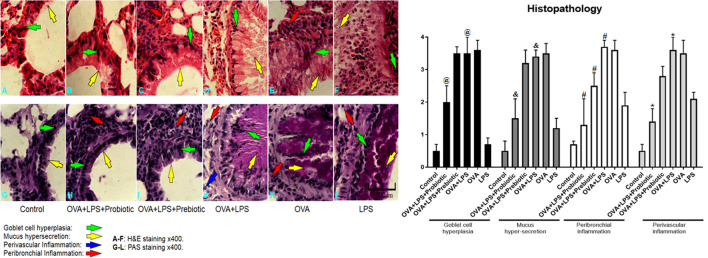
Effect of probiotic and prebiotic treatments on histopathological study
In order to assess the role of probiotics and prebiotics in reversing asthma symptoms in animal models, we examined the histopathological features of the lung tissue sections stained with H&E and PAS. In OVA-LPS-induced asthmatic mice, we observed marked pulmonary infiltration by inflammatory cells into the perivascular and peribronchial regions compared with the mice sensitized with PBS. A semi-quantitative analysis further revealed a significant reduction in inflammation in the probiotic-treated groups compared with the OVA-LPS group. The scores related to goblet cell hyperplasia and mucus production reduced significantly (p < 0.05) in the probiotic-treated group compared to OVA-LPS asthmatic animals. Treatment with prebiotics could control only peribronchial inflammation. On the other hand, we did not find any remarkable histological change in the animals treated with prebiotics (Fig. 4).
Fig. 4.
Lung histopathology. Lung sections were stained with H&E and PAS and the infiltration of inflammatory cells (eosinophils) into perivascular and peribronchial, along with goblet cell hyperplasia, and mucus hypersecretion were studied. The histopathological results showed that infiltration of inflammatory cells into the perivascular and peribronchial regions, goblet cell hyperplasia and mucus hyper-production were increased significantly (p < 0.05) in OVA-LPS-induced asthmatic mice compared with the PBS sensitized mice. A result analysis revealed a significant (p < 0.05) reduction in perivascular and peribronchial inflammation, goblet cell hyperplasia and mucus hyper-production in the probiotic-treated groups compared with the OVA-LPS group. Treatment with prebiotics could significantly (p < 0.05) control only peribronchial inflammation. The significant difference of the results (p < 0.05) between treated groups and non-treated OVA-LPS groups was shown with symbols that include: * for perivascular inflammation, # for peribronchial inflammation, & for mucus hypersecretion, and @ for goblet cell hyperplasia. In the histopathologic sections, hyperplasia of the goblet cells were shown by green arrow, hypersecretion of mucus was shown by yellow arrow, perivascular eosinophilc inflammation was shown by blue arrow and peribronchial eosinophilc inflammation was shown by red arrow
Discussion
Atopy and allergy affect more than 30% of the global population. The prevalence of allergic diseases has been increasing in developed countries during the past 20 years and probiotics, as live microorganisms, have been beneficial for managing allergic diseases [5]. Clinical evidence showed the therapeutic role of probiotics in allergic rhinitis and asthma, improving cure rates and alleviating allergic rhinitis symptoms and the need for drug use. In clinical trials, receiving probiotics has led to the successful control of the immunologic outcomes of allergy (total and allergen specific IgE, leukocyte counts, blood and nasal eosinophils, Th2/Th1 ratio, IL-4 level, thymus-and activation-regulated chemokines, and quality of life). Also, probiotics increased the number of Treg and TGF-β-producing cells; on the other hand, Treg activity could modulate the severity of allergic inflammation [5, 6]. In general, probiotics can decrease disease severity mainly via modulating the immune responses involved in the development of allergic inflammation [5, 15]. According to hygiene hypothesis, in early childhood, lack of exposure to pathogens increases the susceptibility to allergic diseases such as asthma. It leads to Th1-like pattern immunity shits to the Th2-immunoallergic response. Probiotics in adequate amounts confer a health benefit to the host and have ability to modulate mucosal immune responses, stimulatory effects on the innate and adaptive immune system and enhance mucosal barrier functions [16, 17]. Moreover, the innate immune stimulation by bacteria is essential for the establishment of mucosal immune tolerance and, it can be continued by TLR2, TLR4, and TLR9 recognizing microbial components via production of Th1 cytokines. Probiotics may have a strong action in allergic pathologies via TLRs pathways. In particular, the probiotics play a pivotal role in the Th1/Th2 balance. In the allergic asthma, probiotics attenuate the influx of eosinophils to the airway and reduce the levels of MCP-1, and IL-13 level [16, 17]. We observed that probiotic and prebiotic treatments attenuated the recruitment of activated eosinophil to the lung and decreased EPO activity in BALF. Probiotic treatment also decreased eosinophils’ infiltration into BALF. The increased neutrophils in BALF of the LPS challenged groups was controlled by probiotics and prebiotics. LPS acts as TLR4 activator that in this study, increased and recruited neutrophils to the BALF and treatment with probiotics and prebiotics could markedly decrease neutrophils infiltration to the BALF. Therefore, TLR4 was involved in this study by LPS and effect of probiotic and prebiotic treatments on inflammation via TLR4 was noted. Probiotic and prebiotic treatments diminished the production of TSLP, cyst-LTs, LTC4, LTB4, GTP, and GOT which lead to control of inflammation in airways and harnessing of immune-inflammatory responses in lung and could control bronchial inflammo-pathology. Also, Probiotic and prebiotic treatments decreased the elevated levels of total IgE, OVA-specific IgE, and IgG1 and had effect on humoral immunity. The B cell activation is mainly controlled by T cells and T cell releasing cytokines. When B cells are activated can produce and release specific immunoglobulins. Allergen-activated B cells produce IgG1, total and OVA-specific IgE (in mice) and produced Igs bind to the specific receptors on surface of the mast cells, lead to mast cells degranulation and releasing of allegro-inflammatory mediators [2, 4]. In this study, treatment by probiotic had effect on T cell's cytokines and T cell response (cellular immunity) and may have directly effect on B cell to decrease of allegro-inflammatory immunoglobulins. Between two used treatment (probiotic and prebiotic), probiotic had stronger effect on control of allegro-inflammatory factors than prebiotic and could significantly decrease asthma related immune-inflammatory biomarkers. These results implicated that probiotics might have anti-inflammatory properties. In asthmatic lung tissues, the infiltration of inflammatory cells into perivascular and peribronchial areas and increased scores of goblet cell hyperplasia and mucus secretion were observed. This inflammation significantly decreased in probiotic- and prebiotic-treated animals. The scores of goblet cell hyperplasia and mucus secretion reduced in probiotic-treated mice.
On the other hand, according to the ‘hygiene hypothesis’, the increasing prevalence of immune-mediated anti-microbial activity may be related to the decreased incidence of allergic diseases. The crosstalk between gut microflora (probiotics) and the immune system (gut-associated lymphoid tissues) enables balancing Th1/Th2 immune responses in healthy individuals and mediates tolerance and mucosal immunity [6, 15, 17]. The effects of probiotics and prebiotics on Th2-related pro-inflammatory cytokines (IL-4, IL-5, IL-13, IL-25, and IL-33), Th1-related pro-inflammatory cytokine (IFN-γ) and Th17-related cytokine (IL-17) were analyzed. Probiotic and prebiotic treatments reduced the levels of Th2 cytokines (IL-4, IL-5, IL-13, IL-17, IL-25, and IL-33) and increased IFN-γ level in the BALF of asthmatic mice as compared to the non-treated asthma group. Also, gene expression of IL-8 was decreased, and IL-38 was increased in the probiotic- and prebiotic-treated groups compared with the non-treated asthma group, indicating the regulatory effects of probiotics and prebiotics on the Th1/Th2 balance. In this study, probiotic had surprising effect on modulation of cytokines levels in treatment of asthma, but prebiotic treatment had weak effect especially on cytokines levels and genes expression. It was reported that bacterial probiotics (Bifidobacterium infantis) treatment decreased levels of OVA specific-IgE, and IgG in serum, reduced the release of IL-4, -5, -13 in splenocytes. Moreover, the protective effect of probiotics on allergic asthma was correlated with superoxide dismutase and antioxidative enzyme [19, 20]. Treg cells have important role in asthma, and less functional Treg cells lead to enhanced Th2-type immune responses, and eosinophilic airways inflammation. High-fibre prebiotics, via the acetate production, prime Treg cell to protect against asthma. Prebiotics such as soluble fibres and inulin should be fermented by beneficial bacteria and this is time-taking process. Therefore, these products cannot quickly act and present anti-inflammatory properties [13, 21].
Several studies showed that prebiotic supplementation improved airway hyperresponsiveness and decreased inflammatory cells’ counts in the sputum of asthmatic patients [13, 22–24]. Penh is a dimensionless index that generally evaluates changes in the shape of the airflow pattern entering and leaving a whole-body flow plethysmograph when an animal breathes and also by monitoring of AHR changes via connected tube to the ventilator. A higher level of Penh indicates a more severe bronchospasm/airway hyperreactivity to allergens. Interestingly, the oral administration of probiotics and prebiotics could improve AHR. Our results revealed that probiotic administration, but not prebiotic, significantly decreased AHR in asthmatic animals. Nevertheless, prebiotic treatment also reduced AHR, but the results were not significant that was similar to a study in 2020 [25].
LPS as part of the cell membrane of Gram-negative bacteria is one of TLR4 ligands. When LPS binds to TLR4, activates the MyD88 leading to the downstream production of kinases, which allow translocation of the NFκB-related proteins into the nucleus. The NF-κB complex triggers transcription of genes that are involved in the immune-inflammatory responses, and once activated begins a cascade of pro-inflammatory cytokine, specifically TNF-α, IL-1β and IL-6. Once activated NLRP3 inflammasome via microbial components cleaves pro-IL-1β, -IL-18, leukotrienes and prostaglandins [26–28]. In this study, LPS was used as TLR4 activating factor for airway inflammation. When TLR4 in involved, it can participate in asthma pathophysiology and treatment with probiotic has influence on the TLR4 and related signaling pathways. Therefore, the effect of probiotic on regulation of TLR4/ NF-kB Signalling Pathway will be notable. In this study, it was observed that probiotic therapy could decrease and control gene expression of TLR4, NLRP3 and NF-kB as main inflammatory molecules.
It has been demonstrated that many factors and signaling molecules contribute to the induction of allergic inflammation, including cytokines, chemokines, superoxide, ECP, TLRs, and intracellular kinases (NF-κB, ERK, Akt, p38, MAPK, etc.) [3, 29, 30]. AngII could increase ROS production and oxidative stress by activating NADPH oxidases, and promoting release of inflammatory cytokines. It was demonstrated that AngII exhibits pro-inflammatory responses via TLR4 upregulation and stimulating TLR4-dependent signaling pathways. Likewise, AngII upregulates TLR4 and MyD88 gene and AngII-TLR4 crosstalk promotes pro-inflammatory effects, and also, AngII-induced ROS production is dependent on the presence of a functional TLR4. AngII-induced TLR4 upregulation promotes functional consequences such as increase in NF-kB activation, which is dependent the presence of functional AP-1, ETS, and PU.1 transcriptional site. Moreover, molecular mechanisms of AngII-TLR4 activation may indicate an interaction between TLR4 and AT1r signaling downstream effector molecules. Also, TLR4-mediated NF-kB activation in response to LPS is dependent on EGFR signaling. These suggest a regulatory mechanism between AT1r, TLR4, and NF-kB indicating their role in pro-inflammatory effects [31, 32]. Moreover, AngII can directly activate the NF-κB that is critical for initiating the inflammatory cytokines responses during the inflammation. Also, during the inflammatory process, activation of the TLR4 could induce the pro-inflammatory cytokines production and activation of NF-κB via MAPK signaling pathway. On the other hand, TLR4 expression is modulated by local AngII and caused the activation of NF-κB signaling and induction of TNF-α, CD40, and IL-6 expression (33). In this regard, probiotics were used in this study to modulate these pathways. Probiotic and prebiotic treatments reduced the expression of asthma related genes involved in the PI3K/Akt and TLR4/NF‐κB signaling pathways in asthmatic lungs. As we observed, the expression levels of Akt, PI3K, NF-kB, and TLR4 raised in asthmatic mice, and the administration of probiotics dramatically attenuated the expression levels of these genes. The oral administration of probiotics and prebiotics remarkably inhibited the gene expressions of TLR4, NLR3, NF‐κB, and MyD88, but decreasing of TLR4 gene expression by prebiotics was not significant.
IL-4 induces GATA3 expression and in result Th2 cell differentiation. OX40 ligand is linked to the development of Th2-related allergic responses. The activity of probiotic (Lactobacillus murinus) against food allergy showed that oral administration attenuated allergen-induced diarrhoea, mast cell activation, serum IgE and IL-4 production by splenocytes. It enhanced IFN-γ and IL-12 production. Concordantly, it suppressed expression GATA3 and OX40 ligand expression by intestinal CD11c + cells and increased T-bet expression. These demonstrate that probiotic possesses anti-allergic activities via modulating CD11c + cell functionality and the Th1/Th2 immunobalance, which may be employed against food allergy [34, 35]. IL-38 acts as a partial antagonist receptor of IL-36 inflammatory cytokine, suppressing the asthma-induced production of CXCL8 and inhibiting allergic inflammatory responses [36–38]. IL-38 may regulate airway inflammation and can diminish the production of the inflammatory cytokines and chemokines that are regulated by the intracellular p38, ERK1/2, and NF-κB signaling pathways [39, 40]. Eotaxin, a chemotactic cytokine/chemokine with potent effects on eosinophils, increases in asthmatic lungs after exposure to allergens, causing the accumulation of eosinophils in airways. After treatment with both probiotics and prebiotics, the gene expression of eotaxin, CCL11, and CCL24 reduced in the lungs of asthmatic mice, but only CCL11 gene expression by probiotic was significant.
Bronchial inflammation is principal problem in asthma and free oxygen radicals have main role in airway inflammation and pathogenesis of allergic asthma. The oxidation and antioxidative defense modulation is new therapy in management of asthma. Mitochondrial abnormalities have collaboration with oxidative stress that can cause airways injury. Co-Q10 is one of the important antioxidant supplementations, which contributes in the regulation of mitochondrial function and pathology, and also, allergic inflammation. CO-Q10 can induce resistance against the asthma development, protect upper and lower airways against allergic response, and control inflammation [32, 41]. The effects of probiotics on the immune system are classified into two categories involving the activation of the innate immune cells and the inhibition of excessive abnormal immune responses [42, 43]. Oxidative stress is involved in the pathogenesis of several tissue damages and expression of striatal proteins contribute to oxidative stress and damage. ROS production and subsequent toxic events including; mitochondrial membrane potential collapse, lipid peroxidation, lysosomal membrane injury and enzymes dysfunction indicating that oxidative stress. Mitochondrial ROS formation is important mediator in tissue damage and antioxidants combat with free radicals to control oxidative stress. Also, angiotensin II is produced by ACE and can bind cell-surface receptors via AT1 and type 2. AT1 receptor is linked to ROS formation, and inflammation via activation of several downstream signals including, Ras/Rho, ERK, MAPK and JAK/STAT signaling pathway [44, 45]. Probiotics and prebiotics can shift immune reactions from Th2 to Th1 responses in allergic diseases, promoting tolerance in allegro-inflammatory conditions. Probiotics also modulate cellular (Th1, Th2,) and humoral (B cells) immune responses and improve general health by preventing allergies and immune disorders. Probiotic could reduce oxidative and inflammation markers and control airway inflammation and asthma pathophysiology, but prebiotic could not strongly control the inflammation and allergic asthma symptoms. Probiotics use major mechanisms to improve allergic asthma clinical symptoms and prevent them, with several known mechanisms: Th2 suppression and shift response to Th1, tolerance induction, increase of IL-10, Treg cells and their responses for control immune-inflammation, increase the IFN-γ/IL-4 ratio, decrease eosinophil, Th2 cytokines and IgE levels, reduce gene expression of allegro-immune response related, chemokines and cytokines signaling pathways, and also, control AHR. Finally, probiotics can be used as therapeutic approach to treatment of allergic asthma with priority of the tolerance and the lowest side effects.
The probiotics act through several mechanisms to maintain the homeostasis and perform beneficial functions, including pathogens elimination, vitamins and short-chain fatty acids production, as well as modulation of the systemic and mucosal immune system and also inflammation via controlling of NF-κB activation and pro-inflammatory cytokines. Probiotics are live organisms can act as delivery systems and proliferate in tissues for long time, but prebiotics have not these characters. Also, mechanisms action of probiotics in the host include; colonization, regulation of a dysbiotic microbiota, epithelial barrier protection by maintaining tight junction integrity, competitive exclusion of pathogens, production of anti-inflammatory properties, signaling molecules regulation of immunological pathways and inducing host autophagy to attenuate oxidative stress-induced injury. Prebiotics may be added as supplementary agent and stimulate probiotic action. Prebiotic fermentation can modulate the composition and function of probiotics. Prebiotics with regulatory ability, modify the commensal microbiota to a beneficial state. Prebiotics, when associated with a probiotic, are more efficient than when are used separately (13, 14, 46). Therefore, prebiotics may show lower effect than probiotics on control of eosinophilic airway inflammation, EPO activity, immune-allergic response, and allergic asthma.
In this study, there were some limitations. We did not study the effect of probiotic and prebiotic on control group and also on the OVA group and LPS group. We did not have data about protein of the signaling pathways, and phosphorylation of pathway proteins. We could not study to verify the pathway using genetic gain/loss of function models or pharmacologic treatments. We could not show that probiotics can inhibit asthma pathophysiology in absence of TLR4. Also, we did not study the effect of probiotic and prebiotic on chronic form of airway inflammation and asthma.
Acknowledgements
Not applicable.
Abbreviations
- ACE
Angiotensin converting enzyme
- AngII
Angiotensin II
- AHR
Airway hyperresponsiveness
- Akt
Protein kinase B
- AP-1
Activator protein 1
- AT1
Angiotensin II receptor type 1
- BALF
Bronchoalveolar lavage fluid
- BW
Body weight
- CCL
Chemokine (C–C motif) ligand
- CD
Cluster of differentiation
- CFU
Colony forming units
- COPD
Chronic obstructive pulmonary disease
- CXCL
C–X–C Motif chemokine ligand
- Cys-LT
Cysteinyl Leukotriene
- EGFR
Epidermal growth factor receptor
- ELISA
Enzyme-linked immunosorbent assay
- Eos
Eosinophil
- EPO
Eosinophil peroxidase
- ERK
Extracellular signal-regulated kinases
- ETS
Erythroblast Transformation Specific
- FOS
Fructo-oligosaccharides
- FOXP3
Forkhead box P3
- GCI
Goblet Cell Index
- GOS
Galacto-oligosaccharides
- GOT
Glutamic oxaloacetic transaminase
- GPR
G protein-coupled receptor
- GTP
Glutamic pyruvic transaminase
- HDAC
Histone deacetylase
- H&E
Haemotoxylin and eosin stain
- IFN
Interferon
- Ig
Immunoglobulin
- IL
Interleukin
- IN
Intranasally administration
- IP
Intraperitoneal injection
- JAK
Janus Kinase
- LPS
Lipopolysaccharide
- LT
Leukotriene
- MAMP
Microbe-associated molecular pattern
- MAPK
Mitogen-Activated Protein Kinases
- MCh
Methacholine
- MCP
Monocyte chemoattractant protein
- MUC5a
Mucin 5a
- MyD88
Myeloid differentiation primary response 88
- NF-kB
Nuclear factor kappa-light-chain-enhancer of activated B cells
- NK
Natural killer cells
- NLR
NLR Family Pyrin domain containing
- OVA
Ovalbumin
- OX40
Tumor necrosis factor receptor superfamily member 4 (TNFRSF4)/or CD134
- RNS
Reactive nitrogen species
- ROS
Reactive oxygen species
- PAMP
Pathogen-associated molecular pattern
- PAS
Periodic-acid-Schiff stain
- PBS
Phosphate-buffered saline
- PI3K
Phosphoinositide 3-kinase
- RLR
Retinoic acid-inducible gene-I (RIG-)-like receptor
- PO
Per oral
- PRR
Pattern recognition receptor
- STAT
Signal Transducer and Activator of Transcription
- TGF
Transforming growth factor
- Th
T helper
- TLR
Toll-like receptor
- TNF
Tumor necrosis factor
- Treg
Regulatory T cell
- TSLP
Thymic stromal lymphopoietin
Authors' contributions
ZW, EMN, PA, SSA participated in the design of the study, lab analysis and assisted in statistical analysis. ZW and SSA supervised the study and assisted in result analysis and drafting the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Animal study methods have been approved by ethical committee of animal house of ix.med.vet.dep, 2021 (No. IX.MED.VET.DEP.REC.2021.300114.2).
Consent for publication
Not applicable.
Competing interests
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Seyyed SA, Seyyed MA. The importance of eosinophil, platelet and dendritic cell in asthma. Asian Pac J Trop Dis. 2014;4(1):41–47. [Google Scholar]
- 2.MasoumeAthari S, MehrabiNasab E, Shamsadin AS. Study effect of Ocimum basilicum seeds on mucus production and cytokine gene expression in allergic asthma mice model. Rev franç d’allergolo. 2018;58(7):489–493. [Google Scholar]
- 3.Seyyed SA, Seyyede MA, Fateme B, Masoud M, Esmaeil M, Mehdi T. Critical role of Toll-like receptors in pathophysiology of allergic asthma. Europ J Pharmacol. 2017;808:21–27. doi: 10.1016/j.ejphar.2016.11.047. [DOI] [PubMed] [Google Scholar]
- 4.Seyyed Shamsadin Athari Targeting cell signaling in allergic asthma. Signal Transduc Target Therapy. 2019;4:45. doi: 10.1038/s41392-019-0079-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vliagoftis H, Kouranos VD, Betsi GI, Falagas ME. Probiotics for the treatment of allergic rhinitis and asthma: systematic review of randomized controlled trials. Anna Aller Asthma Immunol. 2008;101:570–579. doi: 10.1016/S1081-1206(10)60219-0. [DOI] [PubMed] [Google Scholar]
- 6.Dargahi N, Johnson J, Donkor O, Vasiljevic T, Apostolopoulos V. Immunomodulatory effects of probiotics: Can they be used to treat allergies and autoimmune diseases? Maturitas. 2019;119:25–38. doi: 10.1016/j.maturitas.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Safaa KM, Yosra MM, Dalia AA, Enas SN, Mohamed AH, Omnyah A. Modulation of hippocampal TLR4/BDNF signal pathway using probiotics is a step closer towards treating cognitive impairment in NASH model. Physiol Behavior. 2020;241:112762. doi: 10.1016/j.physbeh.2019.112762. [DOI] [PubMed] [Google Scholar]
- 8.Marco TS. Link between microbiota and hypertension: Focus on LPS/TLR4 pathway in endothelial dysfunction and vascular inflammation, and therapeutic implication of probiotics’. Biomedic Pharmacotherap. 2021;138:111432. doi: 10.1016/j.biopha.2021.111432. [DOI] [PubMed] [Google Scholar]
- 9.Jia T, Lingqi X, Yiwen Z, Fang G. Effect of gut microbiota on LPS-induced acute lung injury by regulating the TLR4/NF-kB signaling pathway. Int ImmunopharmacoL. 2021;91:107272. doi: 10.1016/j.intimp.2020.107272. [DOI] [PubMed] [Google Scholar]
- 10.Narendra VT, Anamika S, Robin J, Monika K, Vishal A. Vitex negundo Linn extract alleviates inflammatory aggravation and lung injury by modulating AMPK/PI3K/Akt/p38-NF-κB and TGF-β/Smad/Bcl2/caspase/LC3 cascade and macrophages activation in murine model of OVA-LPS induced allergic asthma. J Ethnopharmaco. 2021;271:113894. doi: 10.1016/j.jep.2021.113894. [DOI] [PubMed] [Google Scholar]
- 11.Sixuan G, Wanyan L, Feiyue C, Shuzhan Y, Yunmao H, Yunbo T, Danning X, Nan C. Polysaccharide of Atractylodes macrocephala Koidz regulates LPS-mediated mouse hepatitis through the TLR4-MyD88-NFκB signaling pathway. Int Immunopharmacol. 2021;98:107692. doi: 10.1016/j.intimp.2021.107692. [DOI] [PubMed] [Google Scholar]
- 12.Meng B, Juan W, Yu W, Anzheng N, Chunsheng Z, Zongxi S, Zheng Z, Bing Z. Chicory ameliorates hyperuricemia via modulating gut microbiota and alleviating LPS/TLR4 axis in quail. Biomed Pharmacother. 2020;131:110719. doi: 10.1016/j.biopha.2020.110719. [DOI] [PubMed] [Google Scholar]
- 13.Rebecca M, Bronwyn SB, Geraint BR, Katherine JB, Lex EXL, Peter GG, Evan JW, Lisa GW. Soluble fibre supplementation with and without a probiotic in adults with asthma: A 7-day randomised, double blind, three way cross-over trial. EBioMedicine. 2019;46:473–485. doi: 10.1016/j.ebiom.2019.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang X, Chen S, Duan F, Liu An, Li S, Zhong W, Sheng W, Chen J, Jiang Xu, Xiao S. Prebiotics enhance the biotransformation and bioavailability of ginsenosides in rats by modulating gut microbiota. J Ginseng Res. 2021;45(2):334–343. doi: 10.1016/j.jgr.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John S. Mechanisims of asthma and allergic disease-1075. Probiotics in infants for prevention of allergic disease and food hypersensitivity. Sinn World Allerg Organ J. 2013;6(1):72. [Google Scholar]
- 16.Kyung MK, Seo-Jin Y, Du SK, Chang-Wan L, Ha YK, Suyeon L, Ji-Whi C, Johann S, Song SS, Seunghun L. Probiotic properties and immune-stimulating effect of the Jeju lava seawater mineral-coated probiotics. LWT-Food Sci Technol. 2020;126:109299. [Google Scholar]
- 17.Drago L, Toscano M, Pigatto PD. Probiotics: Immunomodulatory Properties in Allergy and Eczema. G Ital Dermatol Venereol. 2013;148(5):505–514. [PubMed] [Google Scholar]
- 18.Hardy H, Harris J, Lyon E, Beal J, Foey AD. Probiotics, prebiotics and immunomodulation of gut mucosal defences: homeostasis and immunopathology. Nutrients. 2013;5:1869–1912. doi: 10.3390/nu5061869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang H-J, Kim G-C, Lee C-G, Park S, Sharma G, Verma R, Im S-H, Kwon H-K. Probiotics-derived metabolite ameliorates skin allergy by promoting differentiation of FOXP3+ regulatory T cells. J Allerg Clin Immunol. 2021;147(4):1517–1521. doi: 10.1016/j.jaci.2020.11.040. [DOI] [PubMed] [Google Scholar]
- 20.Yang Bo, Luo Y, Liu Z, Yang P, Gui Y. Probiotics SOD inhibited food allergy via downregulation of STAT6-TIM4 signaling on DCs. Molec Immunol. 2018;103:71–77. doi: 10.1016/j.molimm.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Ma J, Zhang J, Li Q, Shi Z, Huajie Wu, Zhang H, Liping Tang Ru, Yi HS, Sun X. Oral administration of a mixture of probiotics protects against food allergy via induction of CD103+ dendritic cells and modulates the intestinal microbiota. J Function Foods. 2019;55:65–75. [Google Scholar]
- 22.Alison N, Craig I, Sj S, Dragana S, Laurence M, Linda J, Laura K, Connie HYW, Raymond S, Remy R, Nina C, Jian K, Eliana M, Rob JM, Lee W, Malcolm JM, Dedreia LT, Lisa GW, Vanessa EM, Joerg M, Peter GG, Charles RM. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nature Communicat. 2015;73320:6. doi: 10.1038/ncomms8320. [DOI] [PubMed] [Google Scholar]
- 23.Roberfroid MB. Introducing inulin-type fructans. Br J Nutr. 2005;93(1):S13–S22. doi: 10.1079/bjn20041350. [DOI] [PubMed] [Google Scholar]
- 24.de Preter V, Vanhoutte T, Huys G, Swings J, Rutgeerts P, Verbeke K. Baseline microbiota activity and initial bifidobacteria counts influence responses to prebiotic dosing in healthy subjects. Aliment Pharmacol Ther. 2008;27(6):504–513. doi: 10.1111/j.1365-2036.2007.03588.x. [DOI] [PubMed] [Google Scholar]
- 25.Eslami M, Bahar A, Keikha M, Karbalaei M, Kobyliak NM, Yousefi B. Probiotics function and modulation of the immunesystem in allergic diseases. Allergol Immunopathol (Madr) 2020;48(6):771–788. doi: 10.1016/j.aller.2020.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Alex EM, Anthony JB, Melisa SC, Karen LS, Katie CC. Probiotic Supplementation Has a Limited Effect on Circulating Immune and Inflammatory Markers in Healthy Adults: A Systematic Review of Randomized Controlled Trials. J Academy Nut Die. 2020;120(4):548–564. doi: 10.1016/j.jand.2019.08.018. [DOI] [PubMed] [Google Scholar]
- 27.Zakie M, Najaf AF, Zarrin M, Nahid J. Package of anti-allergic probiotic Lactobacillus by focusing on the regulatory role of immunosuppressive motifs in allergy. Inform Medic Unlocked. 2020;18:100280. [Google Scholar]
- 28.Bermudez-Brito M, Plaza-Díaz J, Muñoz-Quezada S, Gómez-Llorente C, Gil A. Probiotic mechanisms of action. Ann Nutr Metab. 2012;61(2):160–174. doi: 10.1159/000342079. [DOI] [PubMed] [Google Scholar]
- 29.Xiaoyu S, Tianheng H, Edwin C, Tiffany NN, Victor W-HT, Ida M-T C, Sin-Man T, Kay-Sheung C, Christopher W-KL and Chun-Kwok W. Anti-inflammatory mechanisms of the novel cytokine interleukin-38 in allergic asthma. Cell Mol Immunol 2020; 17:631- 646 [DOI] [PMC free article] [PubMed]
- 30.Teal SH, Tillie LH, William AA, Gustavo M-B, Philip MH, Darryl AK. Airway epithelial regulation of pulmonary immune homeostasis and inflammation. Clin Immunol. 2014;151:1–15. doi: 10.1016/j.clim.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 31.Vinicia CB, Gisele FB, Wagner LR, Sarah A-G, Kenia PN. The interplay between Angiotensin II, TLR4 and hypertension. Pharmaco Res. 2017;120:88–96. doi: 10.1016/j.phrs.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 32.Qixue D, Wei M, Seyyed SA, Renzhong W. The effect of Co-Q10 on allergic rhinitis and allergic asthma. Allergy Asthma Clin Immunol. 2021;17(1):32. doi: 10.1186/s13223-021-00534-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qi F, Dongwei L, Yanfang L, Zhangsuo L. The interplay of renin-angiotensin system and toll-like receptor 4 in the inflammation of diabetic nephropathy. J Immunol Res. 2020;3:6193407. doi: 10.1155/2020/6193407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang C-H, Shen C-C, Liang Y-C, Jan T-R. The probiotic activity of Lactobacillus murinus against food allergy. J Func Foods. 2016;25:231–241. [Google Scholar]
- 35.Ashraf R, Vasiljevic T, Day SL, Smith SC, Donkor ON. Lactic acid bacteria and probiotic organisms induce different cytokine profile and regulatory T cells mechanisms. J Func Foods. 2014;6:395–409. [Google Scholar]
- 36.Man C, Ida MT, Edmund CMY, Christopher WKL, Ting FL, Gary WKW, Chun KW. Aberrant expression of novel cytokine IL-38 and regulatory T lymphocytes in childhood asthma. Molecules. 2016;21:933. doi: 10.3390/molecules21070933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frank L, Angela K, Gouping W, Aaron NB, Tania A, Mihai GN, Leo AB, Jos WM, Ruyi H, Vassili K, Charles AD. IL-38 binds to the IL-36 receptor and has biological effects on immune cells similar to IL-36 receptor antagonist. Proc Natl Acad Sci USA. 2012;109:3001–3005. doi: 10.1073/pnas.1121534109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mora J, Schlemmer A, Wittig I, Richter F, Putyrski M, Frank A-C, Han Y, Jung M, Ernst A, Weigert A, Brüne B. Interleukin-38 is released from apoptotic cells to limit inflammatory macrophage responses. J Mol Cell Biol. 2016;8:426–438. doi: 10.1093/jmcb/mjw006. [DOI] [PubMed] [Google Scholar]
- 39.Xu WD, Huang AF. Role of interleukin-38 in chronic inflammatory diseases: a comprehensive review. Front Immunol. 2018;9:1462. doi: 10.3389/fimmu.2018.01462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yingying H, Javier M, Arnaud H, Priscila S, Svenja W, Mateusz P, Christian S, Eiman E, Guangping L, Anica S, Tatjana S, Tobias S, de Natasja B, Pierre B, Carlo S, Harald B, Michael JS, Andreas E, Bernhard B, Andreas W. IL-38 ameliorates skin inflammation and limits IL-17 production from γδ T cells. Cell Rep. 2019;27:835–846. doi: 10.1016/j.celrep.2019.03.082. [DOI] [PubMed] [Google Scholar]
- 41.Aziz E, Elham A, Aida A, Mohammad J-A, Mohammad AE. Protective effects of coenzyme Q10 nanoparticles on dichlorvos-induced hepatotoxicity and mitochondrial/lysosomal injury. Environ Toxicol. 2018;33(2):167–177. doi: 10.1002/tox.22505. [DOI] [PubMed] [Google Scholar]
- 42.Leesa P, Thangapalam JA, Harresh A, Gadadhar D, Talagunda SN. Effects of dietary supplementation of vitamin-E and commercial probiotics on the innate immunity of Labeo rohita against Aeromonas hydrophila infection. Fish Shellfish Immunol Rep. 2021;2:100013. doi: 10.1016/j.fsirep.2021.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Julio P-D, Francisco JR-O, Mercedes G-C, Angel G. Mechanisms of Action of Probiotics. Adv Nutr. 2019;10(1):S49–S66. doi: 10.1093/advances/nmy063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aziz E, Elham A, Yadollah A, Alireza P, Hamed H, Mohammad AE. In vitro/vivo studies towards mechanisms of risperidone-induced oxidative stress and the protective role of coenzyme Q10 and N-acetylcysteine. Toxicol Mech Methods. 2016;26(7):520–528. doi: 10.1080/15376516.2016.1204641. [DOI] [PubMed] [Google Scholar]
- 45.Elham A, Peter SP, Aziz E, Reza H, Mohammad AE. Role of renin-angiotensin system in liver diseases: an outline on the potential therapeutic points of intervention. Expert Rev Gastroenterol Hepatol. 2016;10(11):1279–1288. doi: 10.1080/17474124.2016.1207523. [DOI] [PubMed] [Google Scholar]
- 46.Batista VL, da Silva TF, de Jesus LCL, Coelho-Rocha ND, Barroso FAL, Tavares LM, Azevedo V, Mancha-Agresti P, Drumond MM. Probiotics, Synbiotics, and Paraprobiotics as a Therapeutic Alternative for Intestinal Mucositis. Front Microbiol. 2020;11:544490. doi: 10.3389/fmicb.2020.544490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.