Abstract
Objective:
To determine the prevalence of white spot lesions (WSLs) in orthodontic patients at 6 and 12 months into treatment using the visual examination method.
Materials and Methods:
Patients 6 and 12 months into treatment were examined for the presence of WSLs. The control group consisted of patients who were examined for WSLs immediately after bonding. Upon clinical evaluation, teeth were given a visual score based on the extent of demineralization.
Results:
The percentages of individuals having at least one WSL were 38%, 46%, and 11% for the 6-month, 12-month, and control groups, respectively. The 6-month (P = .021) and 12-month groups (P = .005) were significantly different from the control group but were not significantly different from each other (P = .50). Of subjects in the study who had at least one visible WSL, 76% were males and 24% were females (P = .009).
Conclusions:
This clinical study showed a sharp increase in the number of WSLs during the first 6 months of treatment that continued to rise at a slower rate to 12 months. Clinicians should evaluate the oral hygiene status of patients during the initial months of treatment and, if necessary, should implement extra measures to prevent demineralization.
Keywords: White spot lesions, Prevalence, Demineralization, Dental plaque
INTRODUCTION
Enamel demineralization is a significant risk associated with orthodontic treatment when oral hygiene is poor. Prevention of demineralization during orthodontic treatment is one of the greatest challenges faced by clinicians despite modern advances in caries prevention. The development of white spot lesions (WSLs) is attributed to prolonged plaque accumulation around the brackets.1–5 Not only do fixed orthodontic appliances make conventional oral hygiene procedures more difficult, they also increase the number of plaque retention sites on the surfaces of the teeth that are normally less susceptible to caries development.6
After the introduction of orthodontic fixed appliances into the oral cavity, a rapid shift in the bacterial flora of plaque occurs. Higher levels of acidogenic bacteria are present in the plaque, most notably Streptococcus mutans and Lactobacilli.7 High levels of bacteria are capable of decreasing the pH of plaque in orthodontic patients to a greater extent than in nonorthodontic patients.8 Therefore, the progression of caries is faster in patients with full orthodontic appliances. WSLs can become noticeable around the brackets within 1 month of bracket placement, although the formation of regular caries usually takes at least 6 months.9 These lesions are commonly seen on the buccal surfaces of teeth around the brackets, especially in the gingival region.1,5,10
A review of available literature on the prevalence of WSLs revealed that most relevant studies reported the presence of these lesions at the completion of orthodontic treatment. Depending on the examination technique used, the prevalence of WSLs varies. Gorelick et al.,1 in their study using the visual examination technique, reported that 50% of patients had one or more WSLs at the end of treatment. Boersma et al.,11 using quantitative light fluoroscopy, investigated the prevalence of WSLs at the end of orthodontic treatment and reported that 97% of subjects had one or more lesions. In light of these studies, one may conclude that demineralization is a significant clinical problem resulting in an unacceptable esthetic presentation that, in some severe cases, may require restorative treatment.
Even though it was reported previously that WSLs can develop within 1 month, the formation of these lesions and their prevalence at different time points during orthodontic treatment have not been investigated. Early detection of WSLs during orthodontic treatment is of great importance, as it would allow clinicians to implement preventive measures to control the demineralization process before lesions progress. Therefore, the objective of this study was to determine the prevalence of white spot lesions using the visual examination method in orthodontic patients before orthodontic treatment and at 6 and 12 months into treatment.
MATERIALS AND METHODS
Before the start of this cross-sectional clinical study, approval was obtained from the Institutional Review Board of the Virginia Commonwealth University (VCU) Office of Research. Subjects 12 years and older with complete initial records who agreed to participate in the study were recruited among patients who were being treated with fixed orthodontic appliances at the VCU Orthodontic Clinic. Patients on a daily supplemental fluoride regimen were excluded from the study.
A research assistant searched the schedule at the VCU Department of Orthodontics at the start of each week for patients who met the requirements. Previously identified subjects were then asked if they would participate in the study, and informed consent was obtained. Measurements were performed on all patients enrolled in the study by the same clinician who was blind as to the patient's time frame for orthodontic therapy. The clinician evaluated subjects only after wires and auxiliary attachments had been removed by the orthodontic assistant, thus minimizing the availability of information that would otherwise indicate the duration of previous treatment. Following these measurements, the name of the group to which the patient belonged was added to the examination form by the research assistant.
The patient's date of birth, race, and gender, along with visual examination findings, were recorded on a clinical form with the treatment group section left blank. Before measurements were taken, maxillary teeth from the right second premolar to the left second premolar were isolated with cotton rolls and air-dried for 5 seconds. Only tooth surfaces gingival to the archwire were examined for the presence of WSLs, as this is the area most prone to enamel demineralization during orthodontic treatment. The following scale was used for the visual examination:
Score 0 = No visible white spots or surface disruption (no demineralization)
Score 1 = Visible white spot without surface disruption (mild demineralization)
Score 2 = Visible white spot lesion having a roughened surface but not requiring a restoration (moderate demineralization)
Score 3 = Visible white spot lesion requiring restoration (severe demineralization)
Statistical Analysis
The three groups (6-month, 12-month, and control) were evaluated for differences in the prevalence of having at least one white spot lesion by chi square analysis and were followed by Fisher's exact test. To evaluate the multiple effects of group (time in therapy) and gender, and to determine interactions between groups and gender, logistic regression was used. Differences in the mean number of white spots between groups were analyzed using analysis of variance. The prevalence of white spots by tooth type was evaluated with logistic regression. The significance level was set at P < .05.
RESULTS
The study consisted of three groups of patients who were examined for the presence of enamel demineralization. The 6-month group consisted of 37 subjects (16 females, 21 males) with a mean age of 17.4 ± 1.3 years who were 6 months (±3 weeks) into orthodontic treatment. The 12-month group consisted of 35 patients (18 females, 17 males) with a mean age of 17.5 ± 1.4 years who were 12 months (±4 weeks) into orthodontic treatment. The control group consisted of 28 patients (13 females, 15 males) with a mean age of 15.1 ± 1.5 years who were examined for WSLs immediately after braces were placed on their teeth.
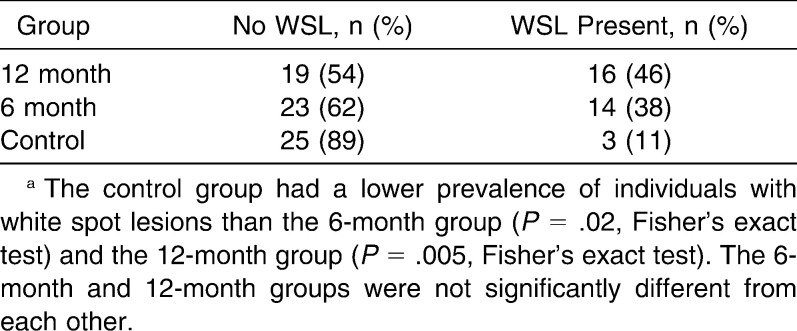
The frequency of individuals having a WSL upon visual examination is presented in Table 1. In the 6- and 12-month groups, the percentages of individuals having at least one visible WSL were 38% and 46%, respectively. In the control group, only 11% of the sample had at least one WSL. The 6-month (P = .021) and 12-month groups (P = .005) were significantly different from the control group but were not significantly different from each other (P = .50).
Table 1.
Frequency of Individuals With WSLsa
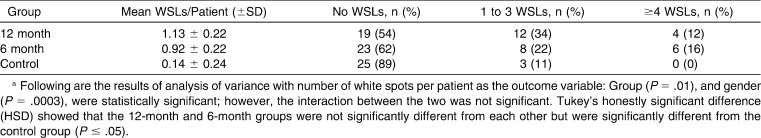
Table 2 presents the distribution of the white spots in greater detail. In the 6-month group, 23 patients had no detectable WSLs (62%), 8 patients had between 1 and 3 WSLs with visual scores of 1 and 2 (22%), and 6 patients had greater than or equal to 4 WSLs with visual scores of 1 and 2 (16%). In some cases, all six of the maxillary anterior teeth presented with WSLs. The 12-month group was similar with 19 patients unaffected (54%), 12 patients with one to three white spot lesions with visual scores of 1 (34%), and 4 patients with greater than or equal to four lesions per individual with visual scores of 2 and 3 (12%). In both groups, a great amount of individual variability was noted among patients, with some displaying no demineralization and others having WSLs almost on each tooth. However, almost 90% of the control group did not have any WSLs on the day of their bonding, and all of the remaining 10% had between one and three WSLs per patient.
Table 2.
Distribution of WSLs per Individuala
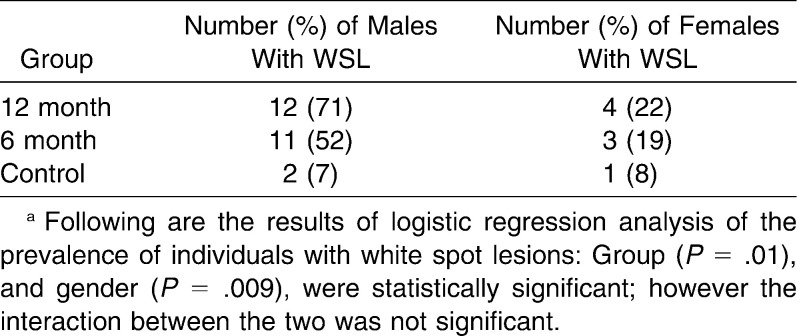
When the gender effect on WSL development was evaluated, a statistically significant difference (P = .009) was noted in the prevalence of WSLs between males and females (Table 3). In the 6-month group, 11 of 21 males (52%) had at least one WSL, as opposed to only 3 of 16 females (19%) within this group. In the 12-month group, 12 of 17 males (71%) developed at least one WSL. In the same group, the number of females who had at least one lesion was only 4 of 18 (22%). Overall, 76% of subjects in the study who had at least one visible white spot were males and 24% were females.
Table 3.
Gender Effect on White Spot Lesion Formationa
No statistically significant differences were noted in the distribution of WSLs among different types of teeth (maxillary central incisors, maxillary lateral incisors, and maxillary canines), indicating that all types of teeth were equally subjected to demineralization.
DISCUSSION
Results of the present study indicate that WSLs remain a considerable problem during orthodontic treatment. Fixed appliances serve as plaque retention sites, and, in the absence of good oral hygiene, plaque accumulates and acidogenic bacteria cause marked demineralization. In this study, 38% of subjects had a visual WSL 6 months into treatment; this number increased to 46% for the 12-month group. Only 11% of the control group presented with at least one white spot lesion. Gorelick et al.1 reported a prevalence of about 50% in their study, which examined the presence of WSLs at the end of orthodontic treatment. A higher prevalence in that study may be attributed to the inclusion of both maxillary and mandibular teeth, and to the length of the orthodontic treatment (about 24 months), as opposed to the examination of the maxillary teeth from canine to canine at 6 and 12 months into orthodontic treatment.
Detecting WSLs during active treatment can be challenging for the clinician. The clinical crown must be free from plaque and debris, and the presence of excess gingival tissue can make visualization of WSLs difficult. Furthermore, to detect incipient WSLs, the tooth must be air-dried. If these steps are not followed, a WSL could easily be overlooked. Therefore, a thorough examination of each patient should be done at each appointment, and each patient should receive a customized oral hygiene treatment regimen to halt the progression of any demineralization.
In this study, it was possible to examine only the maxillary anterior teeth because the premolar tooth surfaces gingival to the archwire were generally covered by inflamed gingiva. This was probably due to more frequent gingival bracket placement on the premolars, as well as to gingival hyperplasia and inflammation that resulted from poor oral hygiene. To create cleansable and accessible tooth surfaces that would be less prone to inflammation and demineralization, laser gingivectomy has been recommended for teeth with inadequate space between the gingival margin and the bracket.12
In the literature, conflicting reports have described the distribution of WSLs. Gorelick et al.1 reported that the tooth most commonly affected was the maxillary lateral incisor. On the other hand, Mizrahi13 concluded that the maxillary and mandibular first molars were the teeth most commonly affected. In a later study, Øgaard5 agreed with Mizrahi's conclusions. In contrast, Geiger et al.4 reported that lesions occurred most frequently on maxillary lateral incisors and canines. The present study, however, found no significant differences among teeth in the distribution of WSLs at 6 months, at 12 months, or on the day of bonding (control).
The high prevalence of WSLs at 6 months into active orthodontic treatment suggests that demineralization can quickly become a concern in the presence of fixed appliances when oral hygiene is poor. According to Øgaard et al.,9 these lesions can become noticeable around the brackets within 1 month of bonding. Therefore, it is important for the clinician to recognize inadequate oral hygiene early, so that preventive measures can be implemented before the development of WSLs occurs.
In this study, the 6- and 12-month groups had an average of 1.03 and 1.11 white spots per individual, respectively, but these averages may be deceiving, as many patients had a much larger problem with demineralization. For instance, of subjects in the 6-month group with WSLs, 43% had four or more lesions in the maxillary anterior segment. However, not all subjects had such a severe problem, and individual results reflected a great amount of variability.
Another interesting finding of the study was the overwhelming difference between the prevalence of white spot lesions in males and females. Of subjects who had at least one white spot lesion, 76% were male. These findings differ from Gorelick's findings.1 In that study, the incidence was 44% for boys and 54% for girls. However, a more recent study by Boersma11 found that 40% of the buccal surfaces in males had demineralization compared with 22% in females. One possible explanation for these results is that females are generally more compliant orthodontic patients.14,15
CONCLUSIONS
Most of the patients undergoing orthodontic treatment had at least one white spot lesion in a mild form, but a few patients presented with moderate or severe demineralization. The prevalence of white spot lesions was 38% in the 6-month group, whereas it was 46% in the 12-month group.
Given the high number of lesions found at 6 months, it is therefore of great importance to evaluate the oral hygiene status of patients during the initial months of orthodontic treatment and, if necessary, to implement preventive measures immediately to prevent demineralization.
Acknowledgments
This research was supported by a grant from Johnson & Johnson Healthcare Products Division of McNeil-PPC, Inc, and the VCU School of Dentistry Alexander Fellowship Fund.
REFERENCES
- 1.Gorelick L, Geiger A. M, Gwinnet A. J. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 2.Artun J, Brobakken B. O. Prevalence of carious white spots after orthodontic treatment with multibonded appliances. Eur J Orthod. 1986;8:229–234. doi: 10.1093/ejo/8.4.229. [DOI] [PubMed] [Google Scholar]
- 3.O'Reilly M. M, Featherstone J. D. B. Demineralization and remineralization around orthodontic appliances: an in vivo study. Am J Orthod Dentofacial Orthop. 1987;92:33–40. doi: 10.1016/0889-5406(87)90293-9. [DOI] [PubMed] [Google Scholar]
- 4.Geiger A. M, Gorelick L, Gwinnett A. J, Griswold P. G. The effect of a fluoride program on white spot formation during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1988;94:123–128. doi: 10.1016/0889-5406(88)90190-4. [DOI] [PubMed] [Google Scholar]
- 5.Øgaard B. Prevalence of white spot lesions in 19-year-olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–427. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 6.Øgaard B. White spot lesions during orthodontic treatment: mechanisms and fluoride preventive aspects. Semin Orthod. 2008;14:183–193. [Google Scholar]
- 7.Lundstrom F, Krasse B. Streptococcus mutans and lactobacilli frequency in orthodontic patients: the effect of chlorhexidine treatments. Eur J Orthod. 1987;9:109–116. doi: 10.1093/ejo/9.2.109. [DOI] [PubMed] [Google Scholar]
- 8.Chatterjee R, Kleinberg I. Effect of orthodontic band placement on the chemical composition of human incisor plaque. Arch Oral Biol. 1979;24:97–100. doi: 10.1016/0003-9969(79)90056-6. [DOI] [PubMed] [Google Scholar]
- 9.Øgaard B, Rolla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell L. Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod. 1992;19:199–205. doi: 10.1179/bjo.19.3.199. [DOI] [PubMed] [Google Scholar]
- 11.Boersma J. G, van der Veen M. H, Lagerweij M. D, Bokhout B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res. 2005;39:41–47. doi: 10.1159/000081655. [DOI] [PubMed] [Google Scholar]
- 12.Sarver D. M. Principles of cosmetic dentistry in orthodontics: Part 3. Laser treatments for tooth eruption and soft tissue problems. Am J Orthod Dentofacial Orthop. 2005;127:262–264. doi: 10.1016/j.ajodo.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 13.Mizrahi E. Surface distribution of enamel opacities following orthodontic treatment. Am J Orthod. 1983;84:323–331. doi: 10.1016/s0002-9416(83)90348-2. [DOI] [PubMed] [Google Scholar]
- 14.Bartsch A, Witt E, Sahm G, Schneider S. Correlates of objective patient compliance with removable appliance wear. Am J Orthod Dentofacial Orthop. 1993;104:378–386. doi: 10.1016/S0889-5406(05)81337-X. [DOI] [PubMed] [Google Scholar]
- 15.Nanda R. S, Kierl M. J. Prediction of cooperation in orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102:15–21. doi: 10.1016/0889-5406(92)70010-8. [DOI] [PubMed] [Google Scholar]