Abstract
Objectives
Our aim was to identify if working during hot days while wearing Covid-19 related personal protective equipment causes occupational heat stress for nurses and nursing assistants in Germany.
Design
Using an online survey, we assessed the impact of hot weather on nurses and nursing assistants working with personal protective equipment. Respondents were recruited by distributing the link to the survey via personal communication, email and various social media channels to nursing staff from hospitals, nursing homes and outpatient care.
Results
There were in total 428 participants (18.2% male, 82.5% female), mostly (30.5%) aged between 45 and 55 years. Half of respondents (48.3%) had more than 20 years of experience in nursing. Cardiac, pulmonary, or other pre-existing conditions were reported by 46.2%.
Nurses and nursing assistants working in personal protective equipment during hot days were exposed to occupational heat stress. Work was found exhaustive by 96.5% of the participants during those days. 93.0% reported breathing problems and 85.8% reported difficulties with focusing on their work. Many workplaces did not provide adequate heat protection, with distinct differences concerning the amount of prophylactic and heat mitigating measures across institutions. There were significant differences across institutions when it comes to the number of drinks served (p < 0.001), the availability of room thermometers (p < 0.001), the use of mobile cooling devices (p < 0.001) and fans (p < 0.05).
Conclusions
Results suggest employers must make more of an effort to provide adequate heat protection for their nursing staff. In order to ensure patient care, there is a need for action; in particular, attention must be paid to the pre-existing health conditions of the nursing staff.
Keywords: Climate change, Covid-19, Occupational heat stress, Nursing profession, Personal protective equipment
Abbreviations
- COPD
chronic obstructive pulmonary disease
- Covid-19
Corona virus disease
- FFP
filtering face piece
- HCW
healthcare worker
- LMU
Ludwig-Maximilians University
- PPE
personal protective equipment
- WHO
World Health Organization
1. Introduction
One of the greatest health threats in our century is climate change [1]. An increase in global temperature, with negative affects to human health, is occuring [2]. Average temperatures as well as the number of heat wave spikes will increase [3]. A recent study compared heat stress experiences of nurses in personal protective equipment (PPE) working in India and Singapore during the 2020 Covid-19 pandemic [4,5]. Healthcare workers (HCWs) from both countries reported a high degree of thirst, sweating, exhaustion and an increased desire to move into comfort zones. Singaporean nurses had more choices to mitigate thermal stress in form of air conditioning, available rest areas and the opportunity to take off PPE during breaks [5]. HCWs are often aware of their situation, but with few opportunities for relief due to work-based constraints [6]. Moreover if institutional environments do not provide dedicated measures to mitigate heat stress, nurses may not be able to do so themselves [5].
According to the World Health Organization (WHO), one lesson learned from the West-African Ebola disease outbreaks of the last decade was that "personal protective equipment is hot and cumbersome" [7,8]. However, in the case of Ebola, heat stress can be mitigated by including ventilation within the PPE, as Ebola is not an airborne disease [8]. Such an option, of course, is not available for handling SARS-CoV-2, as the latter can indeed be transmitted through droplets [9]. Daanen et al. (2020) suggest the implementation of strategic measures - adjusting work and rest times, wearing lighter clothing, and drinking cold water to precool and to reduce the increase in body core temperature [10].
In August 2020, many places across Germany experienced a three-week long heat wave. The double burden of infection protection measures due to the ongoing SARS-CoV-2 pandemic and exposure to heat may have led to added challenges for nurses, as it is known that on its own, wearing PPE can lead to headaches and other mental and physical symptoms [11]. Existing heat-health plans may include a clearly outlined response to heat emergencies, a timely alert system, and a reduction in exposure to indoor heat [10,12,13].
According to the Federal Statistical Office of Germany, there were 6% excess deaths during August 2020 because of the extreme heat wave in the country. During the week of August 10th alone, deaths reported were 20% above average as compared to the same week between 2016 and 2019 [14]. During such heat waves there is a need to protect workers in PPE from heat stress, even without the presence of a pandemic [15], [16], [17].
1.1. Objectives
The aim of this survey was to identify if working during hot days while wearing COVID-19 related PPE causes occupational heat stress for nurses and nursing assistants in Germany.
Central questions of this study were:
Are nurses and nursing assistants exposed to thermal stress by working in PPE on hot days?
What measures are being taken to better protect them from heat strain?
Are there differences in behavioural and condition-oriented prevention when comparing nursing staff in hospitals, nursing homes and outpatient care services?
What are the implications of wearing PPE and working on very hot days, for professional nurses and nursing assistants?
2. Material and methods
We collected data for this study via an online questionnaire using LimeSurvey as our tool.
2.1. Settings
The study was a standardized, descriptive cross-sectional survey. It collected structural data, such as participants' years of employment, area of work, their usage of PPE, their experiences and perspectives in relation to the workload and job satisfaction on hot days as well as their personal feelings of security. If there were more than two answer choices, a 4-point Likert scale was used. The options were 'yes', 'likely', 'unlikely', 'no'. The online questionnaire was open to study participants from the 1st to the 31st of August 2020. A pre-test was run to evaluate potential study results upon their practical relevance and to check whether the questions were easily understandable. Specifically, the first section of the survey contained questions about the participants' current work situation and general workload. To explore the answers in more detail, this was followed by a thematic block on working conditions in PPE, such as protective gowns, medical mouth and nose protection (FFP2 or FFP3 masks), surgical caps, protective gloves, goggles or visors, in normal temperature or heat. A perceived temperature of 32 °C or higher for at least two days in a row was considered as 'hot'. To elucidate whether employers took any steps to mitigate the workload under hot conditions, questions were asked about heat protection measures on the part of the employer when caregivers in PPE were working (relative prevention), and questions were asked about the way in which caregivers protected themselves from heat at work (behavioural prevention). Finally, socio-demographic information about each participant was collected. In total, the survey contained 66 questions that could be answered within 20 minutes.
2.2. Participants
Participants were professional nurses and nursing assistants from various healthcare homes, hospitals and ambulatory care associations in Germany. To recruit participants, invitations to participate were send out via personal communication, email and various social media channels. Thus, no information about the survey response rate were available. An information letter was used to further educate the participants about the nature of the study. In addition, participants were encouraged to notify colleagues about the study.
2.3. Ethical considerations
The data collection was based exclusively on prospectively anonymised questionnaires. No personally identifiable data was requested or recorded and participation was voluntary. Participants had to give informed consent before engaging. Their anonymity, their right to cancel participation and the protection of people from harm were guaranteed [18] following the “World Medical Association Declaration of Helsinki” ethical principles. The Ethics Commission of the Medical Faculty LMU has released a waiver for this project (21-0103 KB).
2.4. Statistical methods
Completely and incompletely answered questionnaires were analysed using both, Chi-square tests for independence and Fisher's exact tests (SPSS version 24). Graphics and diagrams were created using R 4.0.
3. Results
A total of 428 professional nurses and nursing assistants took part in the survey (see Table 1 ). 91.3% of respondents found their job strenuous and 80.2% suffered from physical complaints such as back pain, sleep disorders, exhaustion or headaches. Almost half (46.2%) of all participants had a previous illness including hypertension, mental illness, diabetes, asthma, COPD or skin diseases. 59.2% of those questioned who felt that their work was not appreciated. In outpatient care 91.7% of the employees had to perform their work without support of other nursing staff, for nursing homes the percntage was 40.6% and for hospitals 24.4%. Not having enough protective clothing at their workplace was reported by around one third of the staff in each institution.
Table 1.
Participants’ demographics and information about employment.
| Institution | ||||
|---|---|---|---|---|
| Characteristics | Hospital, N = 254a | Nursing home, N = 101a | Ambulatory care service, N = 73a | Total, N = 428a |
| Gender | ||||
| Male | 43 (20.1%) | 14 (20.0%) | 4 (6.5%) | 61 (17.6%) |
| Female | 171 (79.9%) | 56 (80.0%) | 58 (93.5%) | 285 (82.4%) |
| Age | ||||
| 16–25 years | 20 (9.3%) | 2 (2.9%) | 0 (0.0%) | 22 (6.3%) |
| 26–35 years | 57 (26.5%) | 10 (14.3%) | 12 (19.4%) | 79 (22.8%) |
| 36–45 years | 44 (20.5%) | 20 (28.6%) | 12 (19.4%) | 76 (21.9%) |
| 45–55 years | 63 (29.3%) | 24 (34.3%) | 19 (30.6%) | 106 (30.5%) |
| 56–65 years | 30 (14.0%) | 14 (20.0%) | 19 (30.6%) | 63 (18.2%) |
| 65+ | 1 (0.5%) | 0 (0.0%) | 0 (0.0%) | 1 (0.3%) |
| Working hours | ||||
| Full-time | 125 (58.7%) | 48 (69.6%) | 40 (64.5%) | 213 (61.9%) |
| Part-time | 86 (40.4%) | 20 (29.0%) | 22 (35.5%) | 128 (37.2%) |
| Mini job | 2 (0.9%) | 1 (1.4%) | 0 (0.0%) | 3 (0.9%) |
| Employment relationship | ||||
| Directly employed | 207 (96.3%) | 68 (98.6%) | 57 (91.9%) | 332 (96.0%) |
| Leasing | 6 (2.8%) | 1 (1.4%) | 1 (1.6%) | 8 (2.3%) |
| Self-employed | 2 (0.9%) | 0 (0.0%) | 4 (6.5%) | 6 (1.7%) |
| Duration of employment | ||||
| < 1 year | 7 (3.3%) | 2 (2.9%) | 2 (3.2%) | 11 (3.2%) |
| 1–2 years | 4 (1.9%) | 3 (4.3%) | 2 (3.2%) | 9 (2.6%) |
| 3–5 years | 20 (9.4%) | 9 (12.9%) | 2 (3.2%) | 31 (9.0%) |
| 6–10 years | 38 (17.9%) | 7 (10.0%) | 10 (16.1%) | 55 (16.0%) |
| 11–20 years | 41 (19.3%) | 20 (28.6%) | 11 (17.7%) | 72 (20.9%) |
| > 20 years | 102 (48.1%) | 29 (41.4%) | 35 (56.5%) | 166 (48.3%) |
| Previous illnesses | 111 (44.0%) | 49 (48.5%) | 36 (50.7%) | 196 (46.2%) |
| Working mostly alone | 61 (24.4%) | 41 (40.6%) | 66 (91.7%) | 168 (39.7%) |
| Enough protective clothing at workplace | 176 (69.8%) | 68 (67.3%) | 49 (67.1%) | 293 (68.8%) |
| Hygiene plan at workplace | 232 (98.3%) | 93 (96.9%) | 65 (97.0%) | 390 (97.7%) |
| Physically demanding work | 236 (93.7%) | 91 (91.0%) | 60 (83.3%) | 387 (91.3%) |
| Feeling valued | 78 (31.1%) | 53 (53.0%) | 41 (57.7%) | 172 (40.8%) |
| Frequently suffering from physical complaints | 206 (83.1%) | 77 (77.8%) | 53 (73.6%) | 336 (80.2%) |
Measures: n (%)
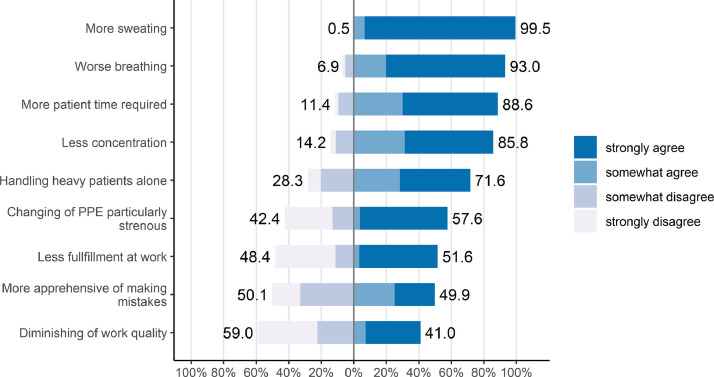
3.1. Consequences of working in PPE on hot days
When working in PPE on hot days nearly all (99.5%) respondents said that they were sweating more, and 93.0% had trouble breathing. 88.6% needed more time to work and 85.8% found it harder to concentrate (see Fig. 1 ). 71.6% were on their own when it came to moving patients, even those with a higher bodyweight. For 57.6%, the necessity of frequently changing PPE was particularly stressful, which was the case when there was not enough nursing staff to assist with the work in the isolation room, and when the nursing staff had to procure missing material outside the isolation room.
Fig. 1.
Restrictions due to working with protective clothing on hot days (perceived temperature is at least 32 degrees on two days in a row). “Do you perceive heat as a problem/ burden at your workplace?”. 4-point-likert scale used (1 = “strongly disagree”; 2 = “disagree”; 3 = “agree”, 4 = “strongly agree”).
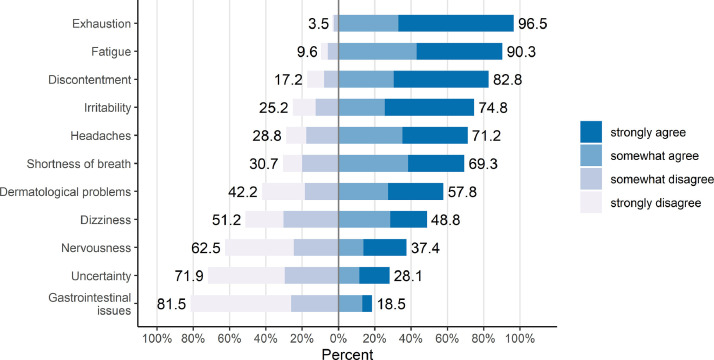
Heat exposure had an impact on emotional experience and physical well-being. A significant proportion of those questioned reported exhaustion and irritability. When working in protective clothing on hot days, most participants reported that they were exhausted, tired, dissatisfied and irritated (see Fig. 2 ). A majority of the participants suffered from headaches and shortness of breath (see Fig. 2).
Fig. 2.
Consequences of working in personal protective equipment on hot days (perceived temperature is at least 32 degrees on two days in a row). 4-point-likert scale used (1 = “strongly disagree”; 2 = “disagree”; 3 = “agree”, 4 = “strongly agree”).
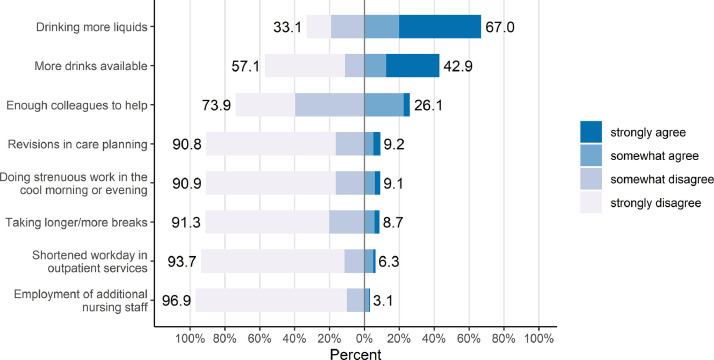
3.2. Short-term countermeasures to prevent heat problems when working in PPE (Behavioural Prevention)
To avoid adverse effects the nursing staff took certain countermeasures when working in PPE on hot days (see Fig. 3 ). Most commonly reported was an increase in liquid uptake (67.0%), likely to compensate for the loss of fluid due to sweating. There was little support from employers: no additional drinks were available and a significant number did not have enough colleagues to help. Almost all individuals surveyed (96.9%), mentioned that no additional nursing staff was available to support the regular nursing staff
Fig. 3.
Question regarding occupational safety and health: countermeasures by healthcare workers against excessive heat. 4-point-likert scale used (1 = “strongly disagree”; 2 = “disagree”; 3 = “agree”, 4 = “strongly agree”).
(see Fig. 3). Only 8.7% of employees were able to take more and/or longer breaks to better allocate their efforts or to regenerate more quickly. Only 9.2% were able to make changes to their care planning and were able to do strenuous work at cooler times of the day. Shorter workdays were only possible in 6.3% of the workers in outpatient care (see Fig. 3, Table S1, Table S1).
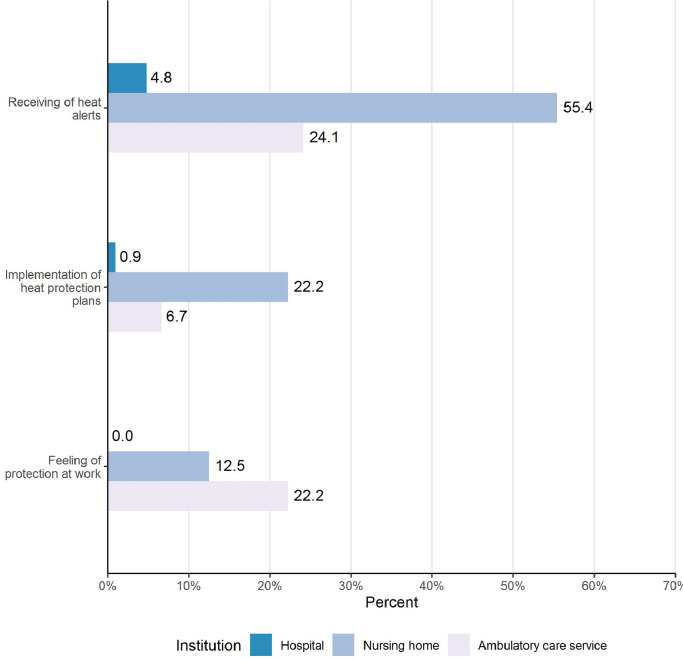
3.3. Heat warnings and heat protection action plans and facility comparisons
One way to protect nurses and nursing assistants from heat strain are heat warnings and heat protection action plans. Fig. 4 shows the current situation across the three institutions. Regarding heat warnings and heat action plans, 12.5% of the nursing staff felt well protected in the nursing homes. In outpatient care, 24.1% received heat warnings and 6.7% received heat protection action plans (see Fig. 4, Table S2,). 22.2% of the nursing staff felt that they were well protected at work. In the clinics, 4.8% of the nursing staff received heat warnings and 0.9% were aware of heat protection action plans. As a result, the nursing staff in the hospitals did not feel well protected at all (see Fig. 4).
Fig. 4.
Heat alerts, heat action plans and related feeling of protection at work across institutions.
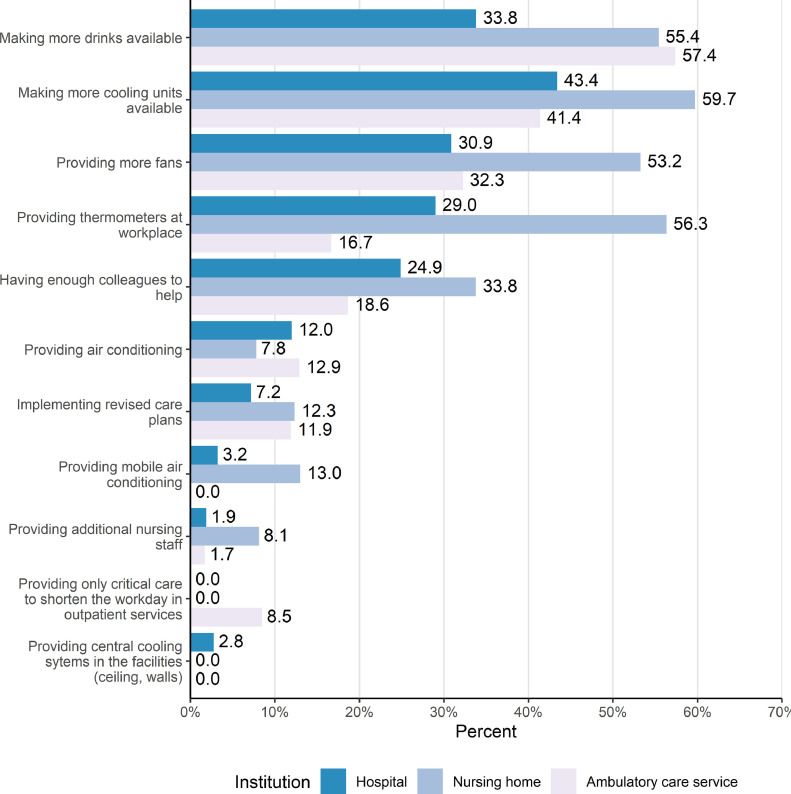
3.4. Condition-oriented prevention when working in PPE on hot days and facility comparisons
Fig. 5 shows that in nursing homes (55.4%) and in ambulatory care services (57.4%), more drinks were served than in hospitals (33.8%), (p < 0.001). In 56.3% of nursing homes, room thermometers were available. This was significantly more than in clinics (29.0%) or ambulatory care sites (16.7%), (p < 0.001). In 59.7% of the nursing homes, refrigerators were available (43.4% clinic, 41.4% outpatient care service; p = 0.5). The personnel situation was similarly poor in all areas, e. g. 75.1% in the clinic, 66.2% in the home and 81.4% in outpatient care said that there was insufficient staff (p = 0.13). Changes in care planning were not made in any of the settings (87.7–92.8%) (p = 0.3) (see also Fig. 1).
Fig. 5.
Question regarding occupational safety and health: Condition-oriented preventative measures by employer against excessive heat shown across institutions.
Permanently installed air conditioning systems were available in hospitals, as reported by 12% of nursing staff; in nursing homes, it was 7.8%, and 12.9% in ambulatory care (p = 0.5). Of all participants, 13.0% mentioned the use of mobile cooling devices in nursing care facilities (3.2% clinic, 0.0% outpatient care; p < 0.001). In nursing homes, 53.2% used fans, 30.9% in clinics and 32.3% in outpatient care (p = 0.002). There were no more fixed air conditioning systems in the hospitals than in other settings (see Fig. 5).
4. Discussion
The majority of nurses and nursing assistants in our survey were female, over 45 years of age and had more than 10 years of experience, some even 20 years. This is in line with the public understanding of the nursing field being dominated by women, however the shortage of younger nurses could be due to a perceived absence of appreciation and low pay [19]. Two thirds of participants (59%) felt that their work was not appreciated, which may have contributed to feelings of being overwhelmed and psychological or even physical hardship. 91%, the vast majority of individuals taking part in the survey, suffered from various complaints like back pain, headaches, exhaustion, sleep deprivation and so forth. Moreover, 46% of participants already suffered from pre-existing conditions such as hypertension, depression, diabetes and others. These problems could become enhanced when being subjected to mentally and physically taxing work with uncomfortable clothing in hot temperatures. Working in PPE during hot days resulted in discomfort; almost everyone complained from more sweating and shortness of breath, and half of the participants were afraid to make mistakes and became stressed when changing PPE during shifts. This corroborates with previously published results [20] and suggests that the anguish and discomfort felt when wearing PPE was both due to wearing the clothing and the elevated temperatures. Recent studies have pointed out that discomfort and stress levels increased with the duration of wearing PPE. This suggests that the stress felt while wearing PPE is not just a psychological effect but linked to actually wearing the clothing [21]. Irrespective of the reason, our survey results suggest that healthcare organizations should provide opportunities for nurses and nursing assistants to alleviate the thermal stress they experience, including institutional policies outlining a maximum duration for which PPE could be worn, at least during peak temperatures [21].
Offering opportunities and implementing the right policies is also important because the overwhelming majority of nurses and nursing assistants were not able to effectively deploy countermeasures against occupational heat stress on their own. As two thirds of study participants (67%) reported drinking more water, healthcare centres may need to offer extra water or ice slurries, as has been recommended recently [9]. Offering cold water has both a cooling effect and increases the likelihood that nurses will drink more fluid during their shifts. Moreover, training staff to frequently drink water will not only help during heat waves but will in general work against another common danger in the workplace - dehydration [9,15]. One possibility to incorporate this into the nursing shifts would be for the employer or hospital to inform nurses of this option and offering boxes filled with ice for everyone to use. Another way to mitigate occupational heat stress would be to offer longer breaks to nurses, so they have more time to recuperate [22]. Still, longer breaks may be difficult to implement, as as staff may feel obligated to treat patients throughout their shifts, especially if the hospital is understaffed and this is consistent with previously published research [23]. Introducing more rest breaks may not only help provide heat relief, but also mitigate workplace stress. Therefore, having mandatory break times may help reduce with nursing staff turnover, which would be a distinct advantage especially during pandemics like SARS-CoV-2 [24]. A large number of care facilities in which the questioned participants worked did not have a clear heat action plan, and even simple devices like room thermometers and additional refrigerators were absent. In cases where it is difficult to implement air conditioning, mobile cooling devices can help; less than a fifth of hospitals, nursing homes and ambulatory care settings had those available at the time of our survey. Foster et al. recommend a combination of ingestion of water and ice slurries, air conditioning – if financially possible for the corresponding institution – and shading in areas that are strongly impacted by heat [9].
In summary, there is a distinct need for stronger institutional policies that acknowledge the existence of occupational heat stress and the need of cooling for nurses and nursing assistants. Climate change will not only increase overall average temperatures but will also result in a rising number of annual heat waves [3]. Thus, our study suggests adequate heat mitigation steps should be taken by hospitals, care homes and even in ambulatory care, to protect nursing staff from occupational heat stress in combination with, or exacerbating, the wearing of PPE. Moreover, it may be necessary to add heat protection measures for nursing staff to occupational health and safety laws and these need to be stringently enforced. It should be noted that Germany – has occupational safety laws in place, whereby air temperatures indoor cannot be higher than 26 °C, however nursing staff still suffer from occupational heat stress. [25]. The expected increase in future demand for nursing personnel suggests that there are good reasons to improve working conditions for nursing staff. In a future with higher temperatures heat protection measures for nurses that have to wear PPE [26] will be important .
4.1. Limitations
Our survey was not designed to address whether temperature and/or uncomfortable, too warm clothing applied independently of one another, or whether the elevated temperature exacerbated existing discomfort from wearing PPE. The year 2020 was an unprecedented time and the pandemic itself might have caused some of the distress for the staff. Other limitations of this study are imbalances in the sample (distribution of registered nurses, nursing assistants, geriatric nurses) and the possibility of a selection bias in favour of the participation of dissatisfied older employees. Moreover, the survey was done exclusively with nurses and nursing assistants in Germany. Selection bias is also possible due to the participation of nursing professionals associated with professional associations and online publishers; we did not assess from which geographic region the participants came. Thus, our group of participants may epitomize employees with special characteristics that are therefore not representative of nurses and nursing assistants in general.
5. Conclusions
The results from the survey show that nurses and nursing assistants report discomfort during hot days whilst working with PPE. As we are all living in a world of rapid climate change it is important that nurses are knowledgeable about climate change and its impact on people-this includes their patients and themselves. It is important that employers have a strong strategy in place to mitigate negative effects from heat, especially since increased nursing personnel will be necessary in the future. Training nurses to inform them of the necessity of protecting themselves from heat and available ways to do so is important. Moreover, hospitals, nursing homes and outpatient services should offer several tools to reduce heat and associated stress, such as air conditioning or cooling devices, ice-water baths for consumption, and an updated break schedule that allows nurses to properly regain their mental and physical strength during their respective shift. Further investigation is needed to ascertain whether occupational heat stress reported by nursing personnel in this study led to an increased desire to change professions, a desire to move to a different healthcare region, or an intention to decrease working hours. A recent paper concluded a paradoxical relation in the German nursing context between job loyalty and job satisfaction [27]. Future studies should assess the impact of heat protection measures and the wearing of PPE during hot ambient temperatures on job satisfaction and turnover.
Funding sources
This work was supported by the Federal Ministry for the Environment, Nature Conservation and Nuclear Safety (BMU) on the basis of a resolution of the German Bundestag (grant number 67DAS213).
CRediT author statement
Yvette Jegodka: Conceptualization, Methodology, Formal analysis, Investigation, Writing – Original Draft Lena Lagally: Conceptualization, Investigation, Software, Formal analysis, Data curation, Visualization Hanna Mertes: Conceptualization, Methodology, Resources, Writing – Review & Editing Katharina Deering: Conceptualization, Methodology, Resources, Writing – Review & Editing Julia Schoierer: Conceptualization, Methodology, Resources, Writing – Original Draft, Project administration, Funding acquisition Barbara Buchberger: Conceptualization, Methodology, Writing – Review & Editing, Supervision Stephan Bose-O'Reilly: Conceptualization, Methodology, Resources, Writing – Original Draft, Supervision
Data sharing statement
The data can be shared upon reasonable request, by sending an email to the corresponding author.
Declaration of Competing Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The authors want to thank Nicole O'Reilly for editing the text and cross checking our English language.
Footnotes
Tweetable abstract: On hot days it is strenuous for nursing professionals to work, even more if personal protective equipment due to Covid-19 needs to be used.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.joclim.2021.100031.
Appendix. Supplementary materials
References
- 1.Watts N, Amann M, Arnell N, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.IPCC. Masson-Delmotte V, Zhai P, et al. 2018. Global warming of 1.5°C an IPCC special report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of clima.; 2019. [Google Scholar]
- 3.Pachauri R.K., Meyer L.A., editors. Climate Change 2014: synthesis report. Contribution of working groups I, II and III to the fifth assessment report of the intergovernmental panel on climate change. 2014. eds. Geneva. [Google Scholar]
- 4.Golechha M, Panigrahy RK. COVID-19 and heatwaves: a double whammy for Indian cities. Lancet Planet Health. 2020;4(8):e315–e316. doi: 10.1016/S2542-5196(20)30170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee J, Venugopal V, Latha PK, et al. Heat stress and thermal perception amongst healthcare workers during the covid-19 pandemic in India and Singapore. Int J Environ Res Public Health. 2020;17(21):1–12. doi: 10.3390/ijerph17218100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park SH. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infect Chemother. 2020;52(2):165–182. doi: 10.3947/ic.2020.52.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuklane K, Lundgren K, Gao C, et al. Ebola: improving the design of protective clothing for emergency workers allows them to better cope with heat stress and help to contain the epidemic. Ann Occup Hyg. 2015;59(2):258–261. doi: 10.1093/annhyg/mev003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . 2014. Unprecedented number of medical staff infected with Ebola.https://www.who.int/mediacentre/news/ebola/25-august-2014/en/ [accessed 12/15/2020] [Google Scholar]
- 9.Foster J, Hodder SG, Goodwin J, Havenith G. Occupational heat stress and practical cooling solutions for healthcare and industry workers during the COVID-19 pandemic. Ann Work Expos Health. 2020;64(9):915–922. doi: 10.1093/annweh/wxaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daanen H, Bose-O’Reilly S, Brearley M, et al. COVID-19 and thermoregulation-related problems: practical recommendations. Temperature. 2020;8(1):1–11. doi: 10.1080/23328940.2020.1790971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ong JJY, Bharatendu C, Goh Y, et al. Headaches associated with personal protective equipment – a cross-sectional study among frontline healthcare workers during COVID-19. Headache. 2020;60(5):864–877. doi: 10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- 12.Barouki R, Kogevinas M, Audouze K, et al. The COVID-19 pandemic and global environmental change: emerging research needs. Environ Int. 2021;146 doi: 10.1016/j.envint.2020.106272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matthies F, Bickler G, Cardenosa Marin N, Hales S. 2008. World Health Organization (WHO). Heat - health action plans. Copenhagen. [Google Scholar]
- 14.Statistisches Bundesamt (Destatis) 2021. Deaths and life expectancy – special evaluation of death figures for 2020.https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Sterbefaelle-Lebenserwartung/sterbefallzahlen.html [Accessed 01/08/2021] [Google Scholar]
- 15.Bose-O’Reilly S, Daanen H, Deering K, et al. COVID-19 and heat waves: new challenges for healthcare systems. Environ Resiron Res. 2021 doi: 10.1016/j.envres.2021.111153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kandic S. Master Thesis series in environmental studies and sustainability science. 2020. Heat – an invisible hazard.https://lup.lub.lu.se/student-papers/search/publication/9011508 [Accessed 01/08/2021] [Google Scholar]
- 17.Global Heat Health Information Network. Extreme heat and COVID-19: FAQs. 2020.www.ghhin.org/heat-and-covid-19. [accessed 12/12/2020].
- 18.Redmiles EM, Acar Y, Fahl S, Mazurek ML. Proceedings - 2017 IEEE cybersecurity development conference, SecDev 2017. 2017. A summary of survey methodology best practices for security and privacy researchers; pp. 22–26. [Google Scholar]
- 19.Marć M, Bartosiewicz A, Burzyńska J, Chmiel Z, Januszewicz P. A nursing shortage – a prospect of global and local policies. Int Nurs Rev. 2019;66(1):9–16. doi: 10.1111/inr.12473. [DOI] [PubMed] [Google Scholar]
- 20.Davey SL, Lee BJ, Robbins T, Randeva H, Thake CD. Heat Stress and PPE during COVID-19: impact on health care workers’ performance, safety and well-being in NHS settings. J Hosp Infect. 2020;108:185–188. doi: 10.1016/j.jhin.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoedl M, Eglseer D, Bauer S. Associations between personal protective equipment and nursing staff stress during the COVID-19 pandemic. medRxiv 2020:2020.08.06.20164129.https://doi.org/10.1101/2020.08.06.20164129Accessed. [DOI] [PMC free article] [PubMed]
- 22.Morabito M, Messeri A, Crisci A, Pratali L, Bonafede M, Marinaccio A. Heat warning and public and workers’ health at the time of COVID-19 pandemic. Sci Total Environ. 2020;738(January) doi: 10.1016/j.scitotenv.2020.140347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lasater KB, Aiken LH, Sloane DM, et al. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf. 2020:1–9. doi: 10.1136/bmjqs-2020-011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wendsche J, Hacker W, Wegge J. Understaffing and registered nurses’ turnover: the moderating role of regular rest breaks. German J Hum Resour Manag. 2017;31(3):238–259. doi: 10.1177/2397002216683880. [DOI] [Google Scholar]
- 25.Mücke HG, Litvinovitch JM. Heat extremes, public health impacts, and adaptation policy in Germany. Int J Environ Res Public Health. 2020;17(21):1–14. doi: 10.3390/ijerph17217862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rafferty AM, Busse R, Zander-Jentsch B, Sermeus W, Bruyneel L, World Health Organization . 2019. Strengthening health systems through nursing: evidence from 14 European countries. [PubMed] [Google Scholar]
- 27.Alameddine M, Bauer JM, Richter M, Sousa-Poza A. The paradox of falling job satisfaction with rising job stickiness in the German nursing workforce between 1990 and 2013. Hum Resour Health. 2017;15(1):1–11. doi: 10.1186/s12960-017-0228-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.