Abstract
Objectives:
This study aimed to develop models that can automatically detect anterior disc displacement (ADD) of the temporomandibular joint (TMJ) on MRIs before orthodontic treatment to reduce the risk of developing serious complications after treatment.
Methods:
We used 9009 sagittal MRI of the TMJ as input and constructed three sets of deep learning models to detect ADD automatically. Deep learning models were developed using a convolutional neural network (CNN) based on the ResNet architecture and the “Imagenet” database. Five-fold cross-validation, oversampling, and data augmentation techniques were applied to reduce the risk of overfitting the model. The accuracy and area under the curve (AUC) of the three models were compared.
Results:
The performance of the maximum open mouth position model was excellent with accuracy and AUC of 0.970 (±0.007) and 0.990 (±0.005), respectively. For closed mouth position models, the accuracy and AUC of diagnostic Criteria 1 were 0.863 (±0.008) and 0.922 (±0.009), respectively significantly higher than that of diagnostic Criteria 2 with 0.839 (±0.013) (p = 0.009) and AUC of 0.885 (±0.018) (p = 0.003). The classification activation heat map also improved our understanding of the models and visually displayed the areas that play a key role in the model recognition process.
Conclusion:
Our CNN model resulted in high accuracy and AUC in detecting ADD and can therefore potentially be used by clinicians to assess ADD before orthodontic treatment, and hence improve treatment outcomes.
Keywords: Deep Learning, Magnetic Resonance Imaging, Temporomandibular Joint Disc
Introduction
Temporomandibular joint disorder (TMD) is considered as a collective term for different symptoms, including pain in the temporomandibular joint (TMJ), impaired mouth opening, headache, clicking, teeth clenching, grinding, crepitus in the TMJ, and tenderness of masticatory muscles.1,2 Its prevalence rate in the population reached 5–12%, which is the main cause of non-odontogenic oral and facial pain.3–5 The common causes of the disease are occlusal dysfunction, trauma, mental tension and anxiety, sleep disorders, malnutrition, dysplasia, systemic and local diseases.6 However, malocclusion is one of the most common risk factors.7 For TMD patients, occlusal splint and other conservative treatment combined with orthodontics can be used to improve the symptoms.8 However, for patients with TMD, inappropriate intermaxillary traction will lead to further displacement of articular disc, which will increase the burden of condyle and lead to condylar absorption and other adverse consequences.9 Therefore, it is very important to make a clear diagnosis of the joint condition of TMD patients before orthodontic treatment.
MRI is a non-invasive imaging technique widely used to assess TMJ.10 ADD is easily diagnosed by comparing the relative position between the TMJ disc and the condylar head (CH) using an oblique sagittal MRIs acquired with the patient in the closed mouth position and the maximum open mouth position. Patients diagnosed with anterior disc displacement without reduction (ADDWoR) are more likely to suffer from absorption of the condyle after orthodontic treatment. These patients would require additional treatment such as occlusal splints, physiotherapy, intra-articular injection prior to standard orthodontic treatment in order to obtain the best cosmetic result.11,12 However, clinicians experienced in evaluating ADD are not widely available, making it difficult to access this service before orthodontic treatment.
Deep learning using convolution neural networks (CNNs) is the most advanced artificial intelligence technology, and it is increasingly being used to detect pathological features on medical images automatically. This technique involves training the CNN algorithm using large amounts of annotated imaging data to develop prediction models that can, later on, be used to detect specific pathological images automatically.13 Deep learning has many applications in dentistry. Yu et al14 in 2020 made use of a CNN framework to classify facial bones automatically. Lee et al15 constructed models for the automatic detection of osteoarthrosis in the TMJ in CT in 2020, achieving an accuracy of 86%. However, to our knowledge, there is currently no model available that can be used to detect ADD automatically. Therefore, this study aims to develop a model to assist clinicians in evaluating ADD before orthodontics treatment.
Methods and materials
Data description and preprocessing
All patients diagnosed with ADD on either or both joints, aged over 16 years, with no history of blood or nervous system disease, oral inflammation or connective tissue disease, TMJ trauma, oral cancer, or craniomaxillofacial surgery and who had a bilateral MRI scan acquired between July 2019 and January 2021 at the Affiliated Stomatological Hospital of China Medical University were included in the study. MRIs with motion and/or other imaging artifacts were excluded from the study. For patients who had multiple MRIs acquired for this condition, only the first scan was included.
Image acquisition
All MRIs were acquired on a 1.5 Tesla scanner with a TMJ surface coil. The images were acquired with the patients in the supine position. The mid-sagittal plane of the face was positioned perpendicular to the couch, and the orbital ear plane was positioned parallel to the couch. Images were first acquired with the mouth closed and then at the maximum mouth open position. Two imaging sequences were acquired for each mouth position, including the fast spin-echo sequence T1 weighted imaging (T1WI, repetition time = 550.0, echo time = 12.0) and T2 weighted imaging (T2WI, repetition time = 2120.0, echo time = 23.0), with a layer thickness of 2 mm and a layer spacing of 0.2 mm and a resolution of 320*320 pixels. A minimum of five slices for each joint were obtained in the sagittal and axially corrected coronal views.
Since the sagittal view provided a better view of the disc, the coronal views were excluded. We manually selected the images in which condyle was visible and located within 1/3 of the center of the image. A total of 14–20 images were obtained from each patient. The outer edge of the image contained a lot of useless information such as shooting parameters. In order to prevent it from impacting the model recognition, we reduced the size of the image to improve the efficiency of training. We took (160,160) pixel coordinate as the central point, intercept the 200*200 pixels image, and saved them in JPEG format.
Diagnostic criteria
TMJ disc displacement can be divided into anterior displacement, medial displacement and lateral displacement. The clinical significance of simple medial and lateral displacement is not as good as that of anterior displacement. This study only deals with the sagittal MRI images, so it can only directly show the anterior displacement of disc.
The classification and label of the images were performed by two physicians with three to six years of experience on both T2- and T1 weighted MRI images. Any disagreements were resolved through consultation with a third expert with 30 years of clinical experience. Since there was no difference in the classification between the two imaging sequences, the data were merged to increase the sample size and hence improve the generalizability of the model.
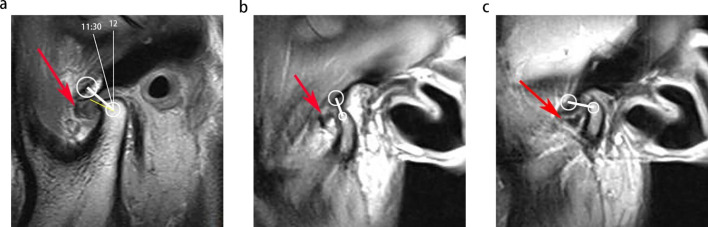
In both T1 and T2 weighted MRI images, the cortical outline of the condylar bone, disc, and articular eminence have a low signal intensity.16,17 The intensity of nearby tissue is relatively higher. There are two diagnostic criteria commonly used to evaluate MRI of anterior disc displacement of TMJ. They are the same in the maximum open position, but different in the closed position.18–20 The details were shown in Table 1 and Figure 1. The ADD is classified as ADDWoR if the TMJ disc is displaced anteriorly in both the closed and maximum open mouth position, and anterior disc displacement with reduction(ADDWR) if the disc is only displaced anteriorly in the maximum open mouth position.21
Table 1.
Diagnostic criteria of ADD
| Diagnostic criteria 1 (RDC/TMD) |
Closed-mouth position | ADD | In the sagittal plane, relative to the superior aspect of the condyle, the low signal of the disc and the high signal of the retrodiscal tissue is located anterior to the 11:30 clock position; and the intermediate zone of the disc is located anterior to the line connecting the condyle head and the center of the articular eminence. |
| Indeterminate | In the sagittal plane, relative to the superior aspect of the condyle, the low signal of the disc and the high signal of the retrodiscal tissue is located anterior to the 11:30 position, but the condyle contacts the intermediate zone located between the anterior-superior aspect of the condyle and the posterior-inferior aspect of the articular eminence; or relative to the superior aspect of the condyle, the low signal of the disc and the high signal of the retrodiscal tissue is located between the 11:30 and 12:30 clock positions, but the intermediate zone of the disc is located anterior to the condyle. | ||
| Normal Disc Position | In the sagittal plane, relative to the superior aspect of the condyle, the border between the low signal of the disc and the high signal of the retrodiscal tissue is located between the 11:30 and 12:30 clock positions; and the intermediate zone is located between the anterior-superior aspect of the condyle and the posterior-inferior aspect of the articular eminence. | ||
| Disc Not Visible | Neither signal intensity nor outlines make it possible to define a structure as the disc. | ||
| Open-mouth position | ADD | The intermediate zone of the disc is located anterior to the line connecting the condyle head and the center of the articular eminence. | |
| Normal Disc Position | The intermediate zone is located between the anterior-superior aspect of the condyle and the posterior-inferior aspect of the articular eminence. | ||
| Disc Not Visible | Neither signal intensity nor outlines make it possible to define a structure as the disc. | ||
| Diagnostic criteria 2 | Closed-mouth position | ADD | The intermediate zone of the disc is located anterior to the line connecting the condyle head and the center of the articular eminence. |
| Normal Disc Position | The intermediate zone is located between the anterior-superior aspect of the condyle and the posterior-inferior aspect of the articular eminence. | ||
| Disc Not Visible | Neither signal intensity nor outlines make it possible to define a structure as the disc. |
ADD, anterior disc displacement.
Figure 1.
Diagnostic criteria of ADD. Red arrows indicate the disc. White circles show the approximate outline of the articular eminence and the condyle head. Image a, image b and image c illustrate the ADD in diagnostic Criteria 1 close mouth, diagnostic Criteria 1 maximum open mouth and diagnostic Criteria 2 close mouth, respectively. ADD, anterior disc displacement.
According to the diagnostic criteria, the diagnosis of images can be divided into many groups such as ADD, indeterminate, normal disc position and disc not visible. ADD of TMJ is our most important diagnostic target, and the number of other diagnostic images is relatively small. We merge the images other than that of ADD group, which is called non-ADD (N-ADD) group.
In order to further compare the predictive accuracy of the two diagnostic criteria for the closed mouth position, the physicians classified these images twice using both diagnostic criteria. Two separate training models for each diagnostic criteria were then constructed for the closed mouth position, and one model was constructed for the open mouth position.
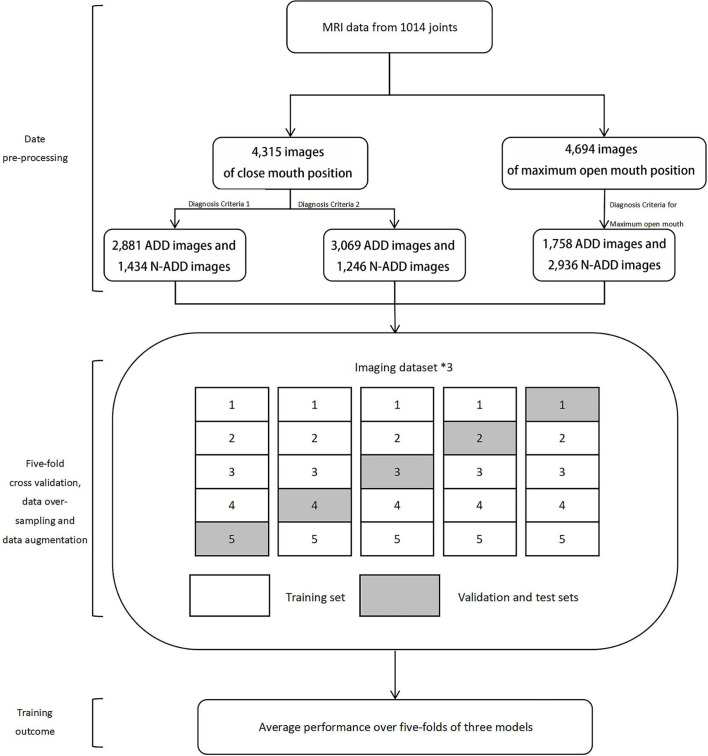
Five-fold cross-validation
Five-fold cross-validation was used to test the model’s ability to predict new data and to minimize the risk of overfitting the model due to the small sample size.22 The training, validation, and testing subset were split into 80%, 10% and 10% within each fold, respectively.
Since there was a large gap in the number between the classes, and we regarded our data set as imbalanced. This means that If the model was trained according to the existing proportions of data, the model might learn to do the easy task, i.e. to learn to classify all examples as the more frequent class and ignore the minority class.23 Therefore, we oversampled the original data in proportion to balance the number of data in each class. In order to make oversampling more efficient, the oversampled data were slightly augmented. Conventional image augmentation techniques could not be used, as these may generate increased variations over unnecessary parts of the data or result in biased learning by simulated variations. In this study, the ADD classification was mainly based on the relative positional relationship between the articular disc, condyle, and articular eminence. Therefore, the data augmentation methods only include horizontal flipping, a maximum of 10% zooming, and up to 10% left and right shifting for each image.24
Model building
The ResNet34 architecture was used to construct the basic model. This architecture uses the concept of residual connections between convolutional layers, allowing the model to be trained to deeper layers while maintaining low complexity.25 The “Imagenet” database was used for the pre-training of the model to increase its convergence speed. Initially, the neural network for trained using 20 rounds with a learning rate of 0.01. The learning rate was subsequently adjusted to 0.001 for 20 rounds of training. Finally, the Fast-AI’s learning rate search tool was used to identify the most suitable learning rate of the model, which was found to be 50 rounds of training. In this process, we set the accuracy of the validation group as the model performance indicator. All models were developed using a 64-bit Ubuntu 16.04.5 LTS operating system, with 31.4 GB of memory and NVIDIA GeForce GTX TITAN X graphics processing unit. The Fast-AI (v. 1.4) library and PyTorch backend engine were used to construct both the training and validation deep learning models. Overview of the study is shown in Figure 2
Figure 2.
Overview of the study. ADD, anterior disc displacement.
The CNN model was visually evaluated to understand the operating principle of the model. The class activation map was used to highlight the most relevant anatomical areas used by the model when classifying images into ADD and N-ADD. The class activation map is a heat gradient map, whereby hotter colors represent the most important areas for classification.26
Statistical analysis
The predictive performance of the models based on the mouth position and diagnostic criteria was measured using a confusion matrix. The sensitivity, specificity, and accuracy of the models were calculated. A receiver operator characteristic (ROC) curve was also plotted, AUC was also calculated for each model. We also calculated the mean and standard deviation of each five-fold evaluation indices. The paired t-test was used to identify any statistically significant difference between diagnostic Criteria 1 and diagnostic Criteria 2 for the closed mouth position. All statistical calculations were performed using the MedCalc19.0.4 software, and a p-value below 0.05 was considered statistically significant for all tests.
Ethical considerations
This study was conducted in accordance with the declaration of Helsinki and was approved by the Ethics Committee of Stomatological Hospital affiliated to China Medical University (20210001). There was no need to obtain written informed consent as the study adopted a non-intrusive retrospective research design, and all data used in this study were anonymized.
Results
Patient characteristics
A total of 507 patients (426 female patients and 81 male patients) with bilateral TMJ MRI were included in the study. The patient characteristics are summarized in Table 2. Out of the 1014 TMJ joints evaluated, 31% (n = 318) were classified as normal, 31% (n = 311) as ADDWR, and 38% (n = 385) as ADDWoR.
Table 2.
Basic characteristics of participating cases
| Normal | ADDWR | ADDWoR | Total | |
|---|---|---|---|---|
| Male | 67 | 72 | 23 | 162 |
| Female | 251 | 239 | 362 | 852 |
| Total | 318 | 311 | 385 | 1014 |
ADD, anterior disc displacement.
Image classification
After evaluating each T1 and T2 sagittal view from each patient, a total of 9009 sagittal images were selected. The images were then subsequently divided into four groups: close mouth position T1 (n = 2051), close mouth position T2 (n = 2264), open mouth position T1 (n = 2177), and open mouth position T2 (n = 2517). Based on the diagnostic criteria one for the closed mouth position, 67% (n = 2881) of the images were classified as ADD, and 33% (n = 1434) were classified as N-ADD, while for the maximum open mouth position, 37% (n = 1758) of the images were classified as ADD, and 63% (n = 2936) of the images were classified as N-ADD. According to diagnosis criteria two for the closed mouth position, 71% (n = 3069) of the images were classified as ADD, and 29% (n = 1246) of the images were classified as N-ADD. Details of training, verification and test datasets in each model are shown in Table 3.
Table 3.
Details of each data sets
| Diagnose Criteria 1 Close mouth position | Diagnose Criteria 1 Maximum open mouth position | Diagnose Criteria 2 Close mouth position | |
|---|---|---|---|
| Train (80%) | 3452 | 3756 | 3452 |
| Valid (10%) | 431 | 469 | 431 |
| Test (10%) | 432 | 469 | 432 |
| Total | 4315 | 4694 | 4315 |
Accuracy, sensitivity, and specificity
Table 4 summarizes the five-fold performance of the three models over the test subset. The overall performance of the maximum open mouth position model was exceptionally high, with accuracy, sensitivity, and specificity of 0.970 (±0.007), 0.975 (±0.007), and 0.961 (±0.025). The performance of diagnostic criteria one in the close mouth position model was generally better than that of diagnostic criteria two with an accuracy, sensivity, specificity of 0.863 (±0.008), 0.735 (±0.061), 0.926 (±0.029), respectively.
Table 4.
Performance measures of three models over five-fold test subsets
| Fold | Diagnose Criteria 1 Close mouth position |
Diagnose Criteria 1 Maximum open mouth position |
Diagnose Criteria 2 Close mouth position |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Accuracy (%) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Sensitivity (%) | Specificity (%) | |
| 1 | 0.861 | 0.639 | 0.972 | 0.983 | 0.976 | 0.994 | 0.850 | 0.608 | 0.948 |
| 2 | 0.852 | 0.764 | 0.896 | 0.962 | 0.986 | 0.920 | 0.821 | 0.677 | 0.879 |
| 3 | 0.859 | 0.722 | 0.927 | 0.966 | 0.976 | 0.949 | 0.858 | 0.661 | 0.938 |
| 4 | 0.870 | 0.727 | 0.941 | 0.966 | 0.966 | 0.966 | 0.838 | 0.573 | 0.945 |
| 5 | 0.873 | 0.825 | 0.896 | 0.972 | 0.969 | 0.977 | 0.829 | 0.808 | 0.837 |
| Mean | 0.863 | 0.735 | 0.926 | 0.970 | 0.975 | 0.961 | 0.839 | 0.665 | 0.909 |
| Standard deviation | 0.008 | 0.061 | 0.029 | 0.007 | 0.007 | 0.025 | 0.013 | 0.081 | 0.044 |
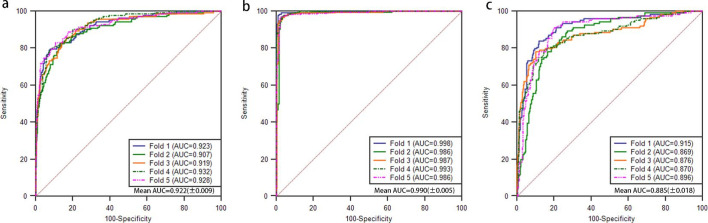
ROC and AUC
The ROCs and the AUCs with standard deviations for each five-folds of three models are provided in Figure 3. The AUCs exceeded 90% was all three models. The model based on the maximum open mouth position performed the best with an AUC of 0.990 (±0.005), followed by the model based on diagnostic criterion one in the closed mouth position with an AUC of 0.922 (±0.009) and ultimately the closed mouth position model for diagnostic criterion two with an AUC of 0.885 (±0.018).
Figure 3.
Receiver operating characteristic curves of three models. Image a, b and c for diagnostic criteria one close mouth, diagnostic criteria one maximum open mouth and diagnostic criteria two close mouth, respectively.
Comparison of diagnostic criteria one and two in close mouth position model
Table 5 compares the five-fold average performance of the classifier model when applied on Diagnostic 1 and 2 separately. Although there is no difference in sensitivity and specificity(p > 0.05), the accuracy and AUC of diagnostic Criterion 1 were significantly higher than those of based on diagnostic criterion two in the closed mouth position(p < 0.05).
Table 5.
Comparison of the five-fold average performance of two diagnostic criteria models in the close mouth position
| Index | Diagnose Criteria 1 | Diagnose Criteria 2 | p-value |
|---|---|---|---|
| Accuracy | 0.863 (0.008) | 0.839 (0.013) | 0.009 |
| Sensitivity | 0.735 (0.061) | 0.665 (0.081) | 0.159 |
| Specificity | 0.926 (0.029) | 0.909 (0.044) | 0.490 |
| AUC | 0.922 (0.009) | 0.885 (0.018) | 0.003 |
AUC, area under the curve.
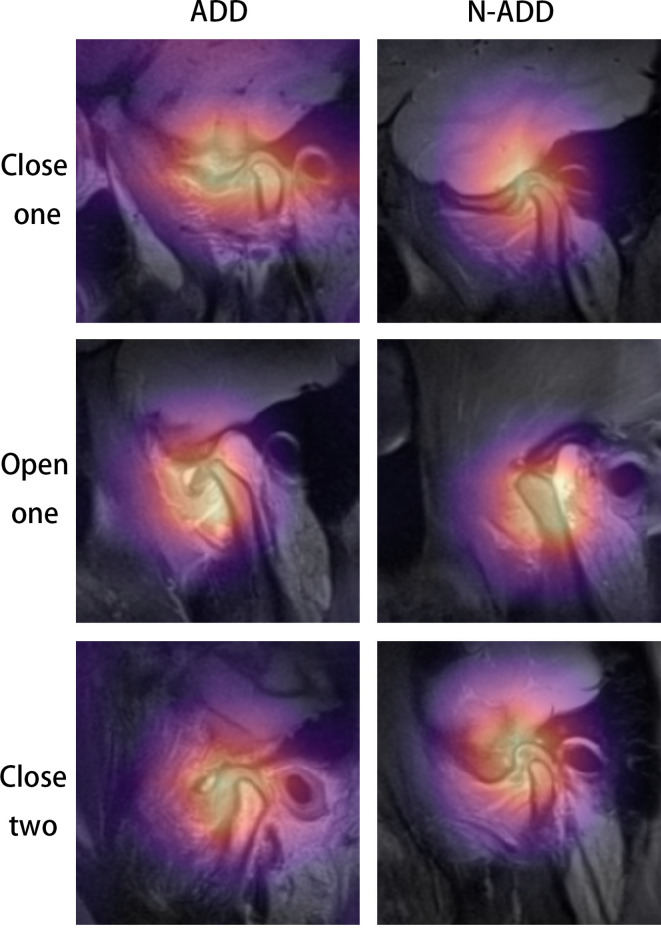
Classification activation heat map
Figure 4 illustrates the class activation maps for a correct ADD and N-ADD classification for the three models. The yellow color on the heat gradient map shows the most influential area, and the purple color indicates the least influential area in the decision-making process. The heat map for all three models in the ADD group was concentrated in the joint disc, the CH, and the posterior disc tissue, while the heat map in the N-ADD group in the open mouth position was concentrated on the condyle area.
Figure 4.
Class activation maps. Rows: model of close mouth position diagnostic Criteria 1, model of maximum open mouth position diagnostic Criteria 1 and model of close mouth position diagnostic Criteria 2. Columns: classification (ADD, N-ADD). ADD, anterior disc displacement.
Discussion
Orthodontic treatment in cases whereby there is ADD will increase the burden on the joints, causing microdamage. This damage causes the release of free radicals, cytokines, metabolites, and matrix-degrading enzymes, leading to absorption of the condyles while compromising the success of orthodontic treatment. MRI can effectively detect ADD disc, but the uneven distribution of experienced clinicians makes it difficult to evaluate MRI before orthodontic treatment. Therefore, we developed deep learning models using CNN to automatically diagnose ADD using MRI before orthodontic treatment and hence facilitate the decision-making process for clinicians.
Based on the MRI images of 507 patients, we constructed 3 models to automatically detect ADD. Two models were designed based on two different diagnostic criteria in the closed mouth position, while the third model was based on the open mouth position. All three models had an excellent performance with an average AUC above 90% and an average accuracy above 85%.
Studies have shown that the risk of osteoarthrosis with ADDWR and ADDWoR increases by 2.73 times and up to 8.25 times, respectively.11 According to the diagnostic criteria of ADDWoR, the disc needs to be located in front of the line connecting the CH and the center of the articular eminence in both the closed and open mouth positions.19 Therefore, the MRI classification of the open mouth position is particularly important. In this study, the performance of the open mouth position model was excellent, with accuracy, sensitivity, specifity, and AUC of 0.970 (±0.007), 0.975 (±0.007), 0.961 (±0.025), and 0.990 (±0.005), respectively. It also had good stability in identifying both ADD and N-ADD.
In the closed mouth position, the performance of the model constructed according to the first diagnostic criterion was better than that of the model based on the second criterion in accuracy and AUC. The improved performance was attributed to narrowing the definition of ADD, which simplified the classification process, increased the number of weak categories, and further balanced the quantitative differences between groups within the training data set. Furthermore, it also optimized the generalization ability of the model under the same amount of data, thereby improving the overall performance of the model.
Class activation maps showed that our model relied on the characteristics of several specific anatomical regions when classifying images. The most consistent area in the images of closed mouth position and ADD group for the maximum open mouth position was the disc area, suggesting that the model was classifying images by evaluating the shape of the articular disc relative to the position of the surrounding structures such as the CH and the articular eminence. This region coincides with the diagnostic criteria used by the physicians to classify the images in the study, indicating that the model has achieved the expected results. Studies have shown that the surface morphology, horizontal, and sagittal inclination of the condyle, are all related to the position of the TMJ disc.27 The model recognized this during the training process. The posterior disc area was also used for classification by the model. ADD causes a long-term forward traction force that deforms the posterior disc area, eventually leading to fibrotic degeneration leading to the formation of a pseudoarticular disc-like structure.28
On the other hand, the CH was consistently identified in the N-ADD group in the open mouth model. The use of this structure was not in line with the manual classification diagnostic criteria used in our study for the N-ADD classification. It indicates that the model ignores the state of the articular disc and uses the image characteristics of the condyle as the classification basis for identifying the ADD. Studies have shown that the deep learning process may summarize features that have not been recognized in previous studies.29 Due to the relatively small amount of data in our research, we cannot rule out whether this is caused by errors in the training process, highlighting the need for further studies with larger sample size.
Limitation
Despite the high level of accuracy obtained by the developed models, our study still has some limitations that have to be acknowledged. First of all, this system can only be used to identify ADD and cannot be used to identify the relatively more rare clinical posterior and mediolateral displacement. Moreover, this system can only evaluate a single sagittal image plane at a time. However, an accurate diagnosis requires a comprehensive interpretation of all sagittal and coronal multilayer image planes. Finally, the image data used to train the images were small and were obtained from a single center, potentially limiting the generalizability of the model. Therefore, further larger multicenter studies are recommended to improve and validate the performance of the model.
Conclusion
Our research illustrates the potential of deep learning models to detect ADD on MRIs for both the closed mouth and maximum open mouth positions. These models could be used to assist clinicians in assessing the state of the TMJ disc before orthodontic treatment, and hence reduce the occurrence of serious treatment complications.
Footnotes
Acknowledgments: Bolun Lin, contributed to conception, design, acquisition, analysis, interpretation, drafted and critically revised the manuscript; Mosha Cheng, contributed to design,analysis, interpretation and critically revised the manuscript; Shuze Wang, contributed to acquisition, analysis and critically revised the manuscript; Fulong Li, contributed to acquisition, analysis and critically revised the manuscript; Qing Zhou, contributed to conception, design and critically revised the manuscript. All
authors gave final approval and agree to be accountable for all aspects of the work.
Funding: This research was supported by a grant from the Natural Science Foundation of Liaoning Province (2019-ZD-0775; Liaoning, China).
Contributor Information
Bolun Lin, Email: 1209416035@qq.com.
Mosha Cheng, Email: 18640198343@163.com.
Shuze Wang, Email: 2623959569@qq.com.
Fulong Li, Email: 1905350149@qq.com.
Qing Zhou, Email: zqforstudent@163.com.
REFERENCES
- 1.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 112: 453–62. doi: 10.1016/j.tripleo.2011.04.021 [DOI] [PubMed] [Google Scholar]
- 2.Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am 2013; 57: 465–79. doi: 10.1016/j.cden.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 3.Tegnander T, Chladek G, Hovland A, Żmudzki J, Wojtek P. Relationship between clinical symptoms and magnetic resonance imaging in temporomandibular disorder (TMD) patients utilizing the Piper MRI diagnostic system. J Clin Med 2021; 10: 4698. doi: 10.3390/jcm10204698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu Y-K, Yang C, Cai X-Y, Xie Q-Y. Does condylar height decrease more in temporomandibular joint nonreducing disc displacement than reducing disc displacement?: a magnetic resonance imaging retrospective study. Medicine 2016; 95: e4715. doi: 10.1097/MD.0000000000004715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sena MFde, Mesquita KSFde, Santos FRR, Silva FWGP, Serrano KVD. Prevalence of temporomandibular dysfunction in children and adolescents. Rev Paul Pediatr 2013; 31: 538–45. doi: 10.1590/S0103-05822013000400018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohlin B, Axelsson S, Paulin G, Pietilä T, Bondemark L, Brattström V, et al. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod 2007; 77: 542–8. doi: 10.2319/0003-3219(2007)077[0542:TIRTMA]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 7.Khayat N, Winocur E, Kedem R, Winocur Arias O, Zaghal A, Shpack N. The prevalence of temporomandibular disorders and dental attrition levels in patients with posterior Crossbite and/or deep bite: a preliminary prospective study. Pain Res Manag 2021; 2021: 1–8. doi: 10.1155/2021/8827895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergmann A, Edelhoff D, Schubert O, Erdelt K-J, Pho Duc J-M, Pho DJ. Effect of treatment with a full-occlusion biofeedback splint on sleep bruxism and TMD pain: a randomized controlled clinical trial. Clin Oral Investig 2020; 24: 4005–18. doi: 10.1007/s00784-020-03270-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurbanov V, Bas B, Öz AA. Evaluation of stresses on temporomandibular joint in the use of class II and III orthodontic elastics: a three-dimensional finite element study. J Oral Maxillofac Surg 2020; 78: 705–16. doi: 10.1016/j.joms.2019.11.022 [DOI] [PubMed] [Google Scholar]
- 10.Helms CA, Richardson ML, Moon KL, Ware WH. Nuclear magnetic resonance imaging of the temporomandibular joint: preliminary observations. J Craniomandibular Pract 1984; 2: 219–24. doi: 10.1080/07345410.1984.11677866 [DOI] [PubMed] [Google Scholar]
- 11.Dias IM, Cordeiro PCdeF, Devito KL, Tavares MLF, Leite ICG, Tesch RdeS. Evaluation of temporomandibular joint disc displacement as a risk factor for osteoarthrosis. Int J Oral Maxillofac Surg 2016; 45: 313–7. doi: 10.1016/j.ijom.2015.09.016 [DOI] [PubMed] [Google Scholar]
- 12.Iwasaki H. Bayesian belief network analysis applied to determine the progression of temporomandibular disorders using MRI. Dentomaxillofac Radiol 2015; 44: 20140279. doi: 10.1259/dmfr.20140279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sultan AS, Elgharib MA, Tavares T, Jessri M, Basile JR. The use of artificial intelligence, machine learning and deep learning in oncologic histopathology. J Oral Pathol Med 2020; 49: 849–56. doi: 10.1111/jop.13042 [DOI] [PubMed] [Google Scholar]
- 14.Yu HJ, Cho SR, Kim MJ, Kim WH, Kim JW, Choi J. Automated skeletal classification with lateral cephalometry based on artificial intelligence. J Dent Res 2020; 99: 249–56. doi: 10.1177/0022034520901715 [DOI] [PubMed] [Google Scholar]
- 15.Lee KS, Kwak HJ, Oh JM, Jha N, Kim YJ, Kim W, et al. Automated detection of TMJ osteoarthritis based on artificial intelligence. J Dent Res 2020; 99: 1363–7. doi: 10.1177/0022034520936950 [DOI] [PubMed] [Google Scholar]
- 16.Tomura N, Otani T, Narita K, Sakuma I, Takahashi S, Watarai J, et al. Visualization of anterior disc displacement in temporomandibular disorders on contrast-enhanced magnetic resonance imaging: comparison with T2-weighted, proton density-weighted, and precontrast T1-weighted imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 260–6. doi: 10.1016/j.tripleo.2006.02.003 [DOI] [PubMed] [Google Scholar]
- 17.Vogl TJ, Lauer H-C, Lehnert T, Naguib NNN, Ottl P, Filmann N, et al. The value of MRI in patients with temporomandibular joint dysfunction: correlation of MRI and clinical findings. Eur J Radiol 2016; 85: 714–9. doi: 10.1016/j.ejrad.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 18.Provenzano MdeM, Chilvarquer I, Fenyo-Pereira M. How should the articular disk position be analyzed? J Oral Maxillofac Surg 2012; 70: 1534–9. doi: 10.1016/j.joms.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 19.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6: 301–55. [PubMed] [Google Scholar]
- 20.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 844–60. doi: 10.1016/j.tripleo.2009.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naeije M, Kalaykova S, Visscher CM, Lobbezoo F. Evaluation of the research diagnostic criteria for temporomandibular disorders for the recognition of an anterior disc displacement with reduction. J Orofac Pain 2009; 23: 303–11. [PubMed] [Google Scholar]
- 22.Jung Y, Hu J. A K-fold Averaging Cross-validation Procedure. J Nonparametr Stat 2015; 27: 167–79. doi: 10.1080/10485252.2015.1010532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao L, Zhang L, Liu C, Wu S. Handling imbalanced medical image data: a deep-learning-based one-class classification approach. Artif Intell Med 2020; 108: 101935. doi: 10.1016/j.artmed.2020.101935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bloice MD, Roth PM, Holzinger A. Biomedical image augmentation using augmentor. Bioinformatics 2019; 35: 4522–4. doi: 10.1093/bioinformatics/btz259 [DOI] [PubMed] [Google Scholar]
- 25.He F, Liu T, Tao D. Why ResNet works? residuals generalize. IEEE Trans Neural Netw Learn Syst 2020; 31: 5349–62. doi: 10.1109/TNNLS.2020.2966319 [DOI] [PubMed] [Google Scholar]
- 26.Stib MT, Vasquez J, Dong MP, Kim YH, Subzwari SS, Triedman HJ, et al. Detecting large vessel occlusion at multiphase CT angiography by using a deep Convolutional neural network. Radiology 2020; 297: 640–9. doi: 10.1148/radiol.2020200334 [DOI] [PubMed] [Google Scholar]
- 27.De Stefano AA, Guercio-Monaco E, Hernández-Andara A, Galluccio G. Association between temporomandibular joint disc position evaluated by magnetic resonance imaging and mandibular condyle inclination evaluated by computed tomography. J Oral Rehabil 2020; 47: 743–9. doi: 10.1111/joor.12962 [DOI] [PubMed] [Google Scholar]
- 28.Whyte A, Boeddinghaus R, Bartley A, Vijeyaendra R. Imaging of the temporomandibular joint. Clin Radiol 2021; 76: 76.e21–76.e35. doi: 10.1016/j.crad.2020.06.020 [DOI] [PubMed] [Google Scholar]
- 29.Van Craenendonck T, Elen B, Gerrits N, De Boever P. Systematic comparison of Heatmapping techniques in deep learning in the context of diabetic retinopathy lesion detection. Transl Vis Sci Technol 2020; 9: 64. doi: 10.1167/tvst.9.2.64 [DOI] [PMC free article] [PubMed] [Google Scholar]