LETTER
The first case of the new SARS-CoV-2 Omicron Variant of Concern (VOC) from South Africa was reported to WHO on November 24, 2021. The genomic analysis demonstrated that this Omicron VOC is classified into the Pangolin lineage B.1.1.529 and the Nextstrain clade 21K (https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/scientific-brief-omicron-variant.html). The spike gene of Omicron is characterized by the large number of mutations (at least 30 amino acid substitutions), three small deletions, and one small insertion; this small insertion, known as the 214 EPE insertion, is unique to Omicron and provides for targeted detection of Omicron. Of note, half of amino acid substitutions are found in the receptor binding domain, which can play an important role in ACE2 binding and antibody recognition. Importantly for the control and treatment of COVID-19, this is the same region that most vaccines present for immunity, and that therapeutic monoclonal antibodies target. Thus, these changes in Omicron raise significant concerns about vaccines' effectiveness and reduced efficacy of some monoclonal antibody treatments. In the United States, Omicron was first detected on December 1, 2021 in a traveler who returned from South Africa, and it is becoming a serious public health challenge (1). To rapidly detect Omicron in clinical specimens to direct therapies, we developed and evaluated the analytical and clinical performance characteristics of a SARS-CoV-2 Omicron variant RT-PCR assay for the qualitative detection of Omicron in the upper respiratory tract.
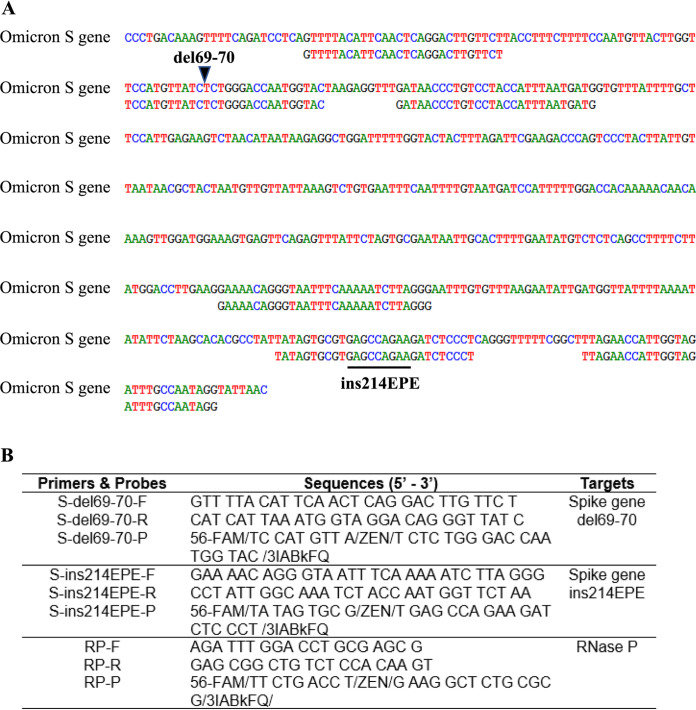
A total of 84 nasopharyngeal and nasal swabs in viral transport medium were used for the validation study. The specimens were previously SARS-CoV-2 tested by the Cepheid Xpert Xpress SARS-CoV-2/Flu/RSV test (Cepheid, Sunnyvale, CA, USA) or the Hologic Aptima SARS-CoV-2 test (Hologic, Bedford, MA, USA). The specimens were extracted using the EasyMag (bioMérieux, Marcy-l'Etoile, France). The specimen input and elution output volumes were 200 μL and 70 μL, respectively. The SARS-CoV-2 Omicron variant RT-PCR assay included three separate RT-PCRs. Two primer/probe sets were designed based on the small deletion del69-70 and the small insertion ins214EPE seen in the Omicron spike gene (Fig. 1a). An additional primer/probe set to detect human RNase P gene (RP) in human specimens was also included in the assay (Fig. 1b). Primers and probes were purchased from Integrated DNA Technologies (Coralville, IA, USA). Two primers and one probe in each set were pooled to generate a combined primer/probe mix in which the final concentration of primer and probe is 6.67 μM and 1.67 μM, respectively. For the RT-PCR setup, 5 μL of extracted viral genome was added to 15 μL of a reagent mixture consisting of 5 μL of TaqPath 1-Step RT-qPCR Master Mix (ThermoFisher, Waltham, MA, USA), 1.5 μL of combined primer/probe mix, and 8.5 μL nuclease-free water. The total RT-PCR volume was 20 μL. The RT step was performed at 25°C for 2 min and 50°C for 15 min, followed by incubation at 95°C for 2 min. The PCR step included 45 cycles of denaturation at 95°C for 3 sec, followed by annealing, extension, and data acquisition at 60°C for 30 sec on the Applied Biosystems 7500 Fast Dx real-time PCR system (ThermoFisher, Waltham, MA, USA).
FIG 1.
(A) Alignment of the SARS-CoV-2 Omicron variant RT-PCR assay’s primers and probes to the spike gene sequence of SARS-CoV-2 Omicron (B.1.1.529) Variant of Concern. The small deletion del69-70 and the small insertion ins214EPE are shown. (B) Names and sequences of the primers and probes used in the SARS-CoV-2 Omicron variant RT-PCR assay.
Since the quantitated Omicron variant is not available, we used the IDT gBlocks Omicron spike gene fragment dsDNA to determine the limit of detection (LOD) of the SARS-CoV-2 Omicron variant RT-PCR assay. The LOD was assessed by analyzing the IDT gBlocks Omicron spike gene fragment dsDNA simulated nasopharyngeal specimens with known titers ranging from 15 to 4,000 copies/mL. All specimen dilutions were prepared using a clinical negative nasopharyngeal matrix. The LOD titer is defined as the lowest concentration at which ≥95% of specimens tested generated positive calls. A minimum of 20 replicates were tested for the LOD verification. Table 1 showed that the positivity rate of 20 replicates observed was ≥95% at 1,000 copies/mL for del69-70 (19/20, 95%) and at 2,000 copies/mL for ins214EPE (20/20, 100%) targets. Since the FDA requires claimed LOD based on the least sensitive target, the LOD of the SARS-CoV-2 Omicron variant RT-PCR assay was determined as 2,000 copies/mL (or 2 copies/μL).
TABLE 1.
Limit of detection of the SARS-CoV-2 Omicron variant RT-PCR assay
| Copies/mL | del69-70 target | Copies/mL | ins214EPE target |
|---|---|---|---|
| positive calls | positive calls | ||
| 4000 | 12/12 (100%) | 4000 | 12/12 (100%) |
| 2000 | 12/12 (100%) | 2000 | 20/20 (100%) |
| 1000 | 19/20 (95%) | 1000 | 13/16 (81%) |
| 500 | 5/8 (62%) | 500 | 7/8 (87%) |
| 250 | 3/4 (75%) | 250 | 2/4 (50%) |
| 125 | 0/4 (0%) | 125 | 2/4 (50%) |
| 62 | 4/4 (100%) | 62 | 2/4 (50%) |
| 31 | 3/4 (75%) | 31 | 1/4 (25%) |
| 15 | 0/4 (0%) | 15 | 2/4 (50%) |
To assess clinical performance characteristics of the SARS-CoV-2 Omicron variant RT-PCR assay, a total of 80 nasopharyngeal and nasal swab specimens (20 residual nasopharyngeal negatives, 20 residual nasal negatives, 20 simulated nasopharyngeal positives, and 20 simulated nasal positives) were tested. The simulated specimens were made by spiking the IDT gBlocks Omicron spike gene fragment dsDNA in a clinical negative nasopharyngeal or nasal matrix to generate 10 different levels from 2X LOD to 1024X LOD. We did not see any false positives or false negatives when we tested the negative or positive specimens, respectively. The clinical sensitivity was 100%, the clinical specificity was 100%, and the agreement was 100%.
The SARS-CoV-2 Omicron variant RT-PCR assay’s cross-reactivity was evaluated by testing the ability of the assay to exclusively identify Omicron with no cross-reactivity to organisms that are closely related or cause similar clinical symptoms or may be present in nasopharyngeal or nasal specimens. AccuPlex SARS-CoV-2 Variant Panels were purchased from SeraCare (Life Sciences, Inc., Milford, MA, USA) and tested by the SARS-CoV-2 Omicron variant RT-PCR assay. The assay did not amplify the Wuhan wild type and other variants including B.1.351 (Beta), B.1.617.1 (Kappa), P.1 (Gamma), B.1.617.2 (Delta) and AY.1 (Delta Plus). While the del69-70 target was detected in the variant B.1.1.7 (Alpha) by the SARS-CoV-2 Omicron variant RT-PCR assay, the ins214EPE target was undetected. This observation is expected because del69-70 is seen in both B.1.1.7 (Alpha) and Omicron. No cross-reactivity with other respiratory viruses including influenza A(H3) virus, influenza B virus, respiratory syncytial virus A & B, common coronaviruses (OC43, NL63, and 229E), and bacteria including Klebsiella pneumoniae and Streptococcus pneumoniae (ZeptoMetrix, Buffalo, NY, USA) was seen.
The Omicron variant has turned out to be more contagious than any earlier coronavirus strains. The early research suggested that Omicron mutations enhance infectivity and reduce the neutralization of antibodies formed by prior infection or vaccination (2). Thus, rapid identification would help those patients at high risk of succumbing to COVID 19. While there are a variety of platforms currently being used to identify SARS-CoV-2, commercial assays specific for Omicron detection are not available. While the S-gene target failure (SGTF)-based method is widely used to flag potential Omicron cases, it is not accurate since SGTF is not unique to Omicron. The 69–70 deletion that reduces S-gene target amplification in some molecular assays is also found in the Alpha variant along with some other variants (3). Furthermore, negative identification is not as reliable a technique as positive identification.
At present, NGS is the best option to genotype SARS-CoV-2 (4); however, this approach is not fast enough and lacks adequate throughput for the current surge in cases. In addition, only a few clinical laboratories can perform NGS. Therefore, developing a rapid and accurate molecular test that effectively differentiates Omicron from other SARS-CoV-2 variants in clinical specimens is very important. Here, we successfully developed the new one-step qualitative RT-PCR assay to detect Omicron in respiratory specimens. While our assay was evaluated on the Applied Biosystems 7500 Fast Dx real-time PCR system (ThermoFisher, Waltham, MA, USA), clinical laboratories can validate it on other available Real-Time PCR systems. Our assay was designed to target the small deletion del69-70 and the small insertion ins214EPE seen in the Omicron spike gene, and human RNase P gene as an internal control. A specimen is considered positive only if two targets (del69-70 and ins214EPE) are detected. During the validation, precision analysis was also performed by testing two negative and two positive specimens, which were run by three different technologists, and all of them (100%) yielded expected results. In the carry-over contamination study, we ran the negative nasopharyngeal specimens next to the positive nasopharyngeal specimens with a high titer (106 copies/mL). All the negative specimens remained negative, suggesting that the carry-over contamination did not happen.
A total of 44 randomly selected SARS-CoV-2 positive clinical specimens (22 collected in mid-December 2021 and 22 collected in the first week of January 2022) were tested by the SARS-CoV-2 Omicron variant RT-PCR assay. The Omicron positive rate was 50% (11/22) in mid-December 2021 and 95% (21/22) in the first week of January 2022. Three Omicron positive specimens underwent NGS to ensure correct assignment and were confirmed as Omicron by the genomic analysis. The data supported that the SARS-CoV-2 Omicron variant RT-PCR assay correctly detects Omicron in SARS-CoV-2 positive clinical specimens.
ACKNOWLEDGMENTS
We thank the UPMC Clinical Microbiology Laboratory for testing the specimens and performing the evaluation. We thank the Microbial Genome Sequencing Center (MiGS) for expert SARS-CoV-2 whole genome sequencing.
The study was internally funded by the UPMC Clinical Laboratories as part of a Quality Improvement initiative. No funding was obtained from any commercial sources. The funders did not have input into study design, analysis, or generation of this communication.
T.P. and A.W. designed the study and wrote the manuscript; S.B., J.G., and M.M. performed and managed the PCR-specific testing; and J.M. and L.H.H. performed and managed the NGS sequence validation. All read and approved the final manuscript.
We declare no competing financial interests.
All testing was performed as apart routine clinical care and performed according to CLIA ’88 regulations by appropriate personnel. The entire study was deemed to be a Quality Improvement initiative by the UPMC IRB and approved by the UPMC QI Review Board.
Contributor Information
Tung Phan, Email: phantg@upmc.edu.
Yi-Wei Tang, Cepheid.
REFERENCES
- 1.CDC COVID-19 Response Team. 2021. SARS-CoV-2 B.1.1.529 (Omicron) Variant—United States, December 1–8, 2021. MMWR Morb Mortal Wkly Rep 70:1731–1734. 10.15585/mmwr.mm7050e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Syed AM, Ciling A, Khalid MM, Sreekumar B, Chen PY, Kumar GR, Silva I, Milbes B, Kojima N, Hess V, Shacreaw M, Lopez L, Brobeck M, Turner F, Spraggon L, Taha TY, Tabata T, Chen IP, Ott M, Doudna JA. 2022. Omicron mutations enhance infectivity and reduce antibody neutralization of SARS-CoV-2 virus-like particles. medRxiv 10.1101/2021.12.20.21268048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas E, Delabat S, Carattini YL, Andrews DM. 2021. SARS-CoV-2 and variant diagnostic testing approaches in the United States. Viruses 13:2492. 10.3390/v13122492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greninger AL, Dien Bard J, Colgrove RC, Graf EH, Hanson KE, Hayden MK, Humphries RM, Lowe CF, Miller MB, Pillai DR, Rhoads DD, Yao JD, Lee FM. 2021. Clinical and infection prevention applications of SARS-CoV-2 genotyping: an IDSA/ASM consensus review document. Clin Infect Dis 10.1093/cid/ciab761. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]