ABSTRACT
There has been significant progress in detection of bloodstream pathogens in recent decades with the development of more sensitive automated blood culture detection systems and the availability of rapid molecular tests for faster organism identification and detection of resistance genes. However, most blood cultures in clinical practice do not grow organisms, suggesting that suboptimal blood culture collection practices (e.g., suboptimal blood volume) or suboptimal selection of patients to culture (i.e., blood cultures ordered for patients with low likelihood of bacteremia) may be occurring. A national blood culture utilization benchmark does not exist, nor do specific guidelines on when blood cultures are appropriate or when blood cultures are of low value and waste resources. Studies evaluating the potential harm associated with excessive blood cultures have focused on blood culture contamination, which has been associated with significant increases in health care costs and negative consequences for patients related to exposure to unnecessary antibiotics and additional testing. Optimizing blood culture performance is important to ensure bloodstream infections (BSIs) are diagnosed while minimizing adverse events from overuse. In this review, we discuss key factors that influence blood culture performance, with a focus on the preanalytical phase, including technical aspects of the blood culture collection process and blood culture indications. We highlight areas for improvement and make recommendations to improve current blood culture practices among hospitalized patients.
KEYWORDS: benchmark, blood culture, healthcare resources, indications, utilization
INTRODUCTION
Blood cultures are the “gold standard” to diagnose bloodstream infections (BSIs), a major cause of death worldwide (1). Bacteremia refers to the presence of bacteria in the bloodstream; the resulting clinical manifestations can range from asymptomatic or minimally symptomatic transient bacteremia to bacteremia causing severe sepsis and death. Transient bacteremia is usually triggered by manipulations of the mucous membranes, such as dental, urinary, and biliary tract procedures, or simple daily activities, like toothbrushing or bowel movements. In the middle of the spectrum are bacteremias associated with localized infections (e.g., pyelonephritis or community-acquired pneumonia [CAP]) without causing severe sepsis. In many of these cases, detecting bacteremia does not change management (e.g., the treatment of CAP is still 5 to 7 days independent of blood culture results). Blood cultures are therefore of high value for patients when there is concern for sepsis or endovascular infection, whereas their value outside these conditions depends on the likelihood that the infection will cause bacteremia and the implications for the host. In the United States, the Centers for Medicare & Medicaid Services (CMS) Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) measure, adopted in 2015 to improve sepsis management, includes requirements for prompt blood culture collection and antibiotics for patients who meet criteria. However, due to the lack of specificity of the sepsis definition, adherence to the core measure may result in overuse of blood cultures and antibiotics (2).
A large portion of blood cultures ordered in the hospital are to evaluate fever or leukocytosis, both of which have been found to correlate poorly with bacteremia (3–6). Furthermore, national guidelines recommend careful evaluation and examination of patients with fever in the intensive care unit (ICU) rather than a “pan-culture” approach (7). However, expert guidelines specifying when to draw blood cultures for the initial workup of a patient or to document clearance of bacteremia are lacking, representing an important barrier to improving blood culture use among hospitalized patients (8). Optimizing blood culture use is important both to ensure true bacteremia is identified, particularly in patients with sepsis, and to reduce harms associated with unnecessary blood cultures, such as treatment of false-positive results with antibiotics, delays in hospital discharge, and increased health care costs (4, 9, 10). Interventions to reduce unnecessary blood cultures have been described in critically ill children, with scarce data from the adult population, especially among immunocompromised hosts.
In addition to careful selection of patients for blood culture testing, specimen management is critical to detect bacteremia and to obtain accurate blood culture results. Blood volume, including both volume per blood culture bottle and overall blood volume, has been recognized as a major determinant of blood culture sensitivity (11). The few studies that exist have shown that a substantial number of blood cultures both in children and in adults do not meet the recommended standards. Up to 40% of blood cultures drawn in adults are single blood cultures (i.e., one set instead of the recommended two to three blood culture sets), and up to 80% of blood cultures collected from adults and children are inappropriately filled (via under- or overfilling) (12, 13). These data show the need for better understanding of current blood culture practices at the national level. Efforts to improve both the blood culture collection process and blood culture indications are essential to ensure detection of true bacteremia and optimal management of patients while minimizing the impact on health care resources.
This minireview will discuss targets for and benefits of improving blood culture practices and describe interventions that have successfully reduced unnecessary blood cultures and improved blood culture collection.
THE NEED TO OPTIMIZE HOSPITAL BLOOD CULTURE USE
Sepsis is a major cause of mortality in hospitalized patients in the United States (14). Blood cultures are the test of choice to diagnose bacteremia; however, 90% or more of blood cultures in routine clinical practice do not grow any organisms, suggesting that many are likely not indicated (3–6, 8). One study showed that only 2% of blood cultures ordered for fever in adults in medicine wards resulted in bacteremia detection (3). Furthermore, 30 to 50% of blood cultures that grow organisms recover contaminants that are associated with several undesirable sequelae, including unnecessary antibiotics, especially vancomycin, which causes nephrotoxicity in up to 25% of exposed patients, additional testing (e.g., additional blood cultures, echocardiography, or joint imaging), unnecessary removal of vascular catheters, longer hospital stay, and increased health care costs (4, 9, 10, 15, 16). Of note, recent data on blood culture contamination rates are lacking, and there is a need for newer and more frequent information on blood culture contamination rates at the national level (15). Blood cultures yielding contaminants may also lead to patients meeting the National Healthcare Safety Network surveillance definition for central line-associated bloodstream infection (CLABSI) without actually having a CLABSI and can be associated with reimbursement penalties (17). One study indicated that 30% of CLABSIs were due to blood culture contaminants (18). These data underscore the need to improve blood culture ordering practices; however, promoting a practice change (reducing unnecessary blood cultures) may be challenging as signs and symptoms of bacteremia are nonspecific (e.g., fever) and can be present in localized infections (e.g., cellulitis) or processes (e.g., postoperative fever) that are not usually associated with bacteremia. Furthermore, fever is absent in up to a third of patients with bacteremia (3, 19).
A study reported that repeat blood cultures (defined as blood cultures obtained after a 24-h period of initial blood cultures) represented 30% of all blood cultures processed by the microbiology lab, and in only 2% of repeat blood cultures was a new pathogen detected (6). According to a French study, 10% of bacterial blood cultures ordered at a university hospital did not have an appropriate indication based on chart review by infectious disease physicians, although the specific criteria for inappropriateness were not described (20). We evaluated the indications for initial and repeat blood cultures for ICU and non-ICU patients (21). We found that 24% and ∼40% of initial blood cultures (those ordered to work up a new clinical event) in the ICU and medicine wards, respectively, were inappropriate, due to, most commonly, the presence of an alternative noninfectious process. Approximately 40% of repeat blood cultures (those ordered after initial blood cultures regardless of the initial blood culture result) in this study were inappropriate based on previous negative blood cultures in patients without additional signs of infection (e.g., ordered for persistent fever) (21). These data highlight the critical need to standardize recommendations regarding blood culture indications. Some published guidelines for certain syndromes (e.g., CAP, skin and soft tissue infections, and fever in critically ill patients) (7, 22–24) recommend obtaining blood cultures; however, these recommendations were not necessarily developed with a diagnostic stewardship perspective, and specific guidance on when blood cultures may be unnecessary is lacking.
Although blood cultures are among the most common microbiologic tests processed by hospital laboratories, few studies have described the rationale for ordering blood cultures or interventions to reduce unnecessary blood cultures. In a survey, clinicians from a large U.S. academic center stated that blood cultures are ordered reflexively in response to fever and identified fear of missing an infection and lack of specific guidelines on when to order blood cultures as barriers to improving blood culture ordering practices for hospitalized adult patients (25). Another potential concern of not ordering blood cultures is missing the opportunity of having susceptibility data to guide antibiotic therapy. However, several studies have shown that lacking blood culture data does not impact management of common infectious processes, such as community-acquired pneumonia, cellulitis, and urinary tract infections (8), either because antibiotic recommendations are based on the clinical syndrome without need for susceptibility data, or susceptibility data are available from the primary source of infection (e.g., urine culture) (8). Another potential concern is that negative blood cultures trigger stopping antibiotics that are not needed, and without these data, broad-spectrum antibiotics may be continued unnecessarily. This was investigated by Sick-Samuels and colleagues among children in a pediatric ICU, where despite a 46% reduction in blood culture use with implementation of a blood culture practice guideline for febrile patients, broad-spectrum antibiotic use remained unchanged (26).
A review of local protocols or policies containing blood culture recommendations should be undertaken regularly. For example, the practice of routine blood cultures before dedicating a central venous catheter (CVC) for parenteral nutrition was stopped at our institution when a patient without suspicion for a BSI met criteria for CLABSI as a consequence of a contaminated blood culture obtained for this purpose. Similarly, guidelines for routine blood cultures prior to insertion of peripherally inserted central catheters (PICCs) were modified to include only patients with risk factors for persistent bacteremia or concern for endovascular infection.
In addition to defining when blood cultures are appropriate, improvement efforts would benefit from a standardized blood culture utilization rate for different hospital settings. The American Society for Microbiology has suggested a blood culture utilization rate of 103 to 188 blood cultures/1,000 patient days, although this recommendation is not evidence based and does not take into account the patient population (27). Published blood culture rates in intensive care units (ICUs) are variable. For example, a study of bacteremia in German ICUs found that blood culture detection increased below a range of 80 to 90 blood cultures/1,000 patient days but not above it, suggesting such a range was a reasonable target in those units (28). At our institution, the blood culture utilization rate in the medical ICU was 220 to 270/1,000 patient days (although it was estimated that ∼30% of these were inappropriate based on retrospective chart review) (21). Blood culture utilization rates outside the ICU also have a wide range. The average blood culture rate in medicine wards in an Israeli hospital was twice the rate observed in medicine wards at a U.S. hospital (125 to 229 versus 80 to 110 blood cultures/1,000 patient days, respectively) (21, 29). These differences in blood culture rates may reflect different patient populations, different medical practices, or more likely, a combination of both and emphasize the importance of hospital-, unit-, and/or patient-level adjustments to benchmarks for fairer comparisons.
INTERVENTIONS THAT HAVE REDUCED UNNECESSARY BLOOD CULTURES
Most blood culture improvement initiatives have focused either on the blood culture collection process (i.e., optimal number of blood cultures, optimal filling volume, blood culture contamination-reducing strategies) or on development of bacteremia prediction tools to better select patients that would benefit the most from blood cultures, with very few studies evaluating interventions to reduce blood culture utilization and improving blood culture positivity. Woods-Hill and colleagues showed that provider education and implementation of blood culture clinical decision tools resulted in fewer blood cultures, including fewer central line blood cultures in a pediatric ICU without affecting patient outcomes, such as in-hospital mortality and readmissions (30). The clinical decision tools included an algorithm for rapid decision on the need for blood cultures based on clinical status and underlying comorbidities of the child and a fever/sepsis screening checklist with common scenarios that warrant or do not warrant consideration of blood cultures in critically ill children.
In 1988, Gross et al. reported a significant reduction on blood culture orders in an adult medical ICU after educating providers on the optimal number of blood cultures needed for endocarditis and sepsis and implementing a protocol that included not drawing blood cultures for persistent fever if initial blood cultures were negative in patients without additional clinical changes (31).
Pawlowicz and colleagues showed a 33% reduction in blood cultures utilization in the emergency department with implementation of a clinical decision tool to standardize blood culture ordering practices (32). The criteria for drawing blood cultures in their clinical decision tool included immunocompromised status, hemodynamic instability, one major Shapiro criterion (suspected endocarditis, temperature of ≥39.4°C, or presence of indwelling vascular catheter) or two minor Shapiro criteria (temperature of 38.3 to 39.3°C, age of >64 years, chills/rigors, vomiting, systolic blood pressure of <90 mm Hg, peripheral white cell count of >18,000/mm3, bands of >5%, platelet count of <150,000/μL, and/or creatinine of >2.0 mg/dL) (33), and CAP patients with severe disease (based on 2007 CAP guidelines) (32).
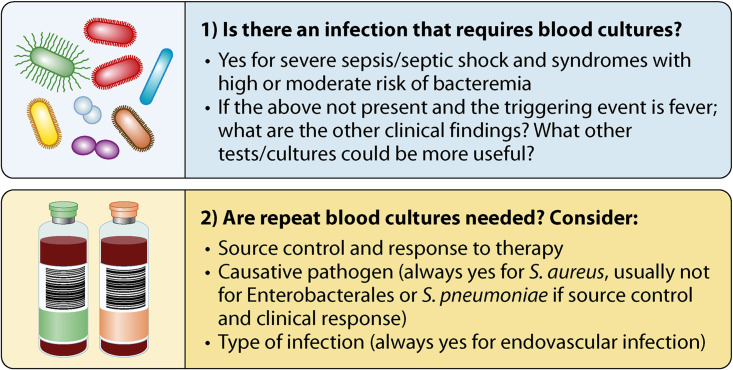
We implemented an evidence-based algorithm informing initial (those ordered upon a new clinical event) and repeat (those ordered after positive blood cultures) blood culture indications for nonneutropenic adults, along with provider feedback regarding inappropriate blood culture orders and education on blood culture indications (21). The intervention led to a significant reduction in blood cultures ordered in both the medical ICU and medicine wards without affecting compliance with the blood culture component of the CMS SEP-1 core measure or patient outcomes, including readmissions and mortality, and also led to a significant increase in blood culture positivity for true pathogens in the ICU. As shown in Fig. 1, the algorithm (8) was designed to answer two questions: (i) is there an infection that requires blood cultures, and (ii) are repeat blood cultures needed? In this algorithm, consideration for initial blood cultures is based on the pretest probability of bacteremia (high or moderate) and host characteristics (e.g., risk of endovascular infection) so that blood cultures are indicated for syndromes with high likelihood of bacteremia, such as meningitis or infective endocarditis, for syndromes with moderate likelihood of bacteremia when cultures from the primary source of infection are not available or will be delayed (e.g., cholangitis), when the patient is at high risk of endovascular infection (e.g., patients with prosthetic heart valves, vascular grafts, implantable defibrillator/pacemaker, valvular heart disease, or injection drug use), or when the results will impact patient management (e.g., severe nonpurulent cellulitis in an immunocompromised patient). Consideration for repeat blood cultures is based on the organism growing in blood (e.g., always for Staphylococcus aureus, given the frequency of persistent bacteremia and the clinical implication of this finding), source of infection (e.g., always for endovascular infection), and clinical response and source control (e.g., not indicated in Enterobacterales bacteremia of urinary or abdominal source or in Streptococcus pneumoniae bacteremia in the setting of pneumonia with adequate clinical response and source control). Examples of low and high diagnostic utility of blood cultures are summarized in Tables 1 and 2.
FIG 1.
Facilitator questions to guide blood culture decisions.
TABLE 1.
Examples of common scenarios when initial blood cultures have high and low diagnostic utility for immunocompetent hostsa
| Diagnostic value of initial blood cultures | Exception |
|---|---|
| High diagnostic value | |
| Severe sepsis/septic shock | NA |
| Infections associated with high or intermediate risk of bacteremia | NA |
| Low diagnostic value | |
| Fever ± leukocytosis in stable patients without suspicion for endovascular infection | Patients with splenectomy |
| Postoperative fever within 48 h | Presence of severe sepsis/septic shock |
| Infections with low risk of bacteremia (e.g., cystitis, prostatitis, cellulitis, non-severe pneumonia, prosthetic joint infection) | Endovascular infection suspected |
| Presence of severe sepsis/septic shock | |
| Persistent febrile neutropenia in hemodynamically stable patients with 2 negative sets | NA |
TABLE 2.
Examples of common scenarios when repeat blood cultures have high and low diagnostic utilitya
| Diagnostic value of repeat blood cultures | Exception |
|---|---|
| High diagnostic value | |
| To document clearance of S. aureus bacteremia | NA |
| To document clearance of S. lugdunensis bacteremia | NA |
| Any organism suspected to be causing infective endocarditis/endovascular infection | NA |
| Concern for persistent bacteremia | NA |
| To distinguish contamination from true bacteremia | NA |
| Low diagnostic value | |
| S. pneumoniae or β-hemolytic streptococcus bacteremia from pulmonary source | Infective endocarditis/endovascular infection suspected |
| Gram-negative organisms from urinary/abdominal source | Infective endocarditis/endovascular infection suspected |
| Enterococcus bacteremia from urinary or biliary source | Inadequate clinical response |
| Cases likely to represent contaminationb | Absence of source control |
For example, single blood culture with diphtheroids, Cutibacterium spp., coagulase-negative staphylococci (CoNS), and micrococci in immunocompetent hosts and those without prosthetic material. Careful interpretation of clinical context is needed (e.g., a single positive blood culture for CoNS in a patient with a prosthetic hip without any clinical changes may not need repeating blood cultures).
BLOOD CULTURE COLLECTION PRACTICES
Although there has been substantial progress in development and implementation of rapid diagnostic tests for BSIs in clinical practice, most still depend on the growth of organisms in blood cultures (34). Blood culture performance depends on several factors, including the preanalytical (e.g., number of blood cultures and volume per blood culture bottle), analytical (e.g., accurate detection of pathogens), and postanalytical (e.g., timely communication of results to patient providers and communication of blood culture contaminants) phases of blood culture testing (35). Microbiology laboratories periodically monitor several blood culture quality indicators, such as blood culture contamination rates, blood culture positivity, and single blood cultures; however, most bedside clinicians who order and/or draw blood cultures are unaware of these metrics (e.g., what they mean, what the goals are, or how they trend over time for their units). Therefore, efforts to educate non-laboratory personnel involved in blood draws on variables that influence blood culture sensitivity are essential to improve diagnosis of BSIs in hospitalized patients. Although all three aforementioned phases of blood culture testing must be considered to ensure the highest quality of blood cultures, we will focus discussion on the preanalytical phase. This phase requires a greater need for improvement and collaboration between the clinical microbiology laboratory and front-line providers, including nurses, physicians, and midlevel practitioners, all of whom are involved in either the collection of blood for cultures, the decision of ordering blood cultures, or both.
The following preanalytical parameters should be considered: (i) the number of blood cultures collected, volume per blood culture bottle, and need for both aerobic and anaerobic bottles; (ii) the time interval between blood cultures and timing of blood culture collection in relation to body temperature; and (iii) the blood culture sampling strategies. We recommend to readers a recent comprehensive review by Doern and colleagues on blood culture contamination, including diversion of the first portion of blood and blood draws from central vascular catheters and skin antisepsis (15).
Optimal number of blood culture sets, volume of blood per blood culture bottle, and blood culture medium for bacteremia/fungemia detection.
Both the number of blood cultures collected and the volume of blood per bottle (usually determined by weighting blood culture bottles) impact bacteremia detection.
The adequate number of blood cultures for optimal bacteremia/fungemia detection has been evaluated in several studies, and data consistently show that single blood cultures are inadequate to detect bacteria or yeast in blood. Single sets miss 10 to 40% of bacteremias, depending on the organism, with the lowest detection rates for Pseudomonas aeruginosa, Candida albicans, and Enterococcus spp. (36). When blood cultures were ordered to document clearance of S. aureus bacteremia, two sets had a higher negative predictive value for resolution of bacteremia than one set when ordered within the first 72 h from positive blood cultures (91 to 95% versus 87 to 93%, respectively), but rates were similar after day 3 (37). Another disadvantage of obtaining a single blood culture set is the inability to distinguish blood culture contamination from true bacteremia. Although a recommended threshold of ≤5% for single blood cultures exists (7), up to 40% of blood cultures drawn in the hospital may be single blood cultures, especially in the ICU setting, where peripheral venous access may be more challenging (5). The reasons behind high numbers of single blood cultures have not been well studied. In a survey, clinicians responded that single blood cultures were acceptable to detect bacteremia, highlighting the need to enhance education of bedside providers on preanalytical parameters (25). Anecdotally, bedside providers have also cited patient comfort and the perception that single sets are optimal for bacteremia detection to justify obtaining solitary blood cultures (V. Fabre’s personal communications).
Current guidelines recommend collection of at least two sets of blood cultures, with each set typically consisting of 10 mL of blood inoculated into each aerobic and anaerobic bottle to identify blood pathogens in adult patients (23). In children, the optimal blood volume can be calculated based on age (1-mL minimum, with the addition of 1 mL per year of age, up to a maximum of 10 mL) or weight (volumes per bottle of 1 to 1.5 mL for children weighing <11 kg and 7.5 mL for a patient weight of 11 to 17 kg). Despite the existing recommendations, 40 to 85% of blood cultures contain an inadequate blood volume (12, 13, 38). Female gender and older age have been associated with increased likelihood of lower volumes of blood collected (38). Another study identified older age and higher APACHE II score as risk factors for lower blood volumes collected for culture and found that bacteremia detection increased by 3% for each extra milliliter of blood cultured (odds ratio [OR], 1.03; 95% confidence interval [CI], 1.002 to 1.07) in patients with an APACHE II score of >18 (39). A study identified technical details like inability to see the target filling mark on the bottle or lack of a tray to place the bottles upright as barriers to adequate filling of the bottles (13). The authors showed that correction of these deficiencies along with staff education regarding the importance of blood volume in detection of blood pathogens resulted in significant improvement in bacteremia detection (20% increase in blood culture positivity) (13). The best approach to assess adequate filling of bottles has not been established; however, substantial weight variability of blood cultures bottles prior to filling can be observed, suggesting that premarking of bottles to the recommended 10 mL may be the best strategy to ensure adequate filling among adult patients.
Whether two blood cultures sets are sufficient or more than 2 sets are optimum deserves further evaluation. Studies evaluating this issue with automated blood culture detection methods (Bactec 9240 instrument; Becton, Dickinson Diagnostic Instrument Systems) found that three cumulative blood cultures over a 24-h period are needed to achieve >95% bacteremia detection (36, 40). This was not the case for patients with infective endocarditis, in whom the first blood culture in any blood culture series was frequently positive (likely due to more continuous or higher bacterial burden in infective endocarditis cases). Neither study described antimicrobial use or stratified BSI cases by indication or illness severity. It is worth highlighting that although improved blood culture performance (less blood culture contamination and fewer single blood cultures) has been associated with draws by phlebotomy personnel, most hospitals are unable to fulfill all blood culture collection requests through phlebotomy (5, 41). Hence, education on blood culture best practices must be included in nursing and medical training.
With respect to routine use of anaerobic bottles, a recent study showed that among 1,081 episodes of bacteremia in adult patients, 16% were detected only in anaerobic bottles (42). Most of these organisms were facultative anaerobes, such as coagulase-negative Staphylococcus, S. aureus, and Escherichia coli. Patients with bacteremia due to obligate anaerobic pathogens (only 13/83 were obligate anaerobic pathogens) were a mix of surgical, oncology, and critically ill patients, highlighting the challenge of using a “population-based” strategy to guide the use of anaerobic bottles. Therefore, it seems prudent to continue routine use of aerobic and anaerobic bottles in all patients, even when nonanaerobic infections are suspected. Similarly, a study in children (median age of the cohort, 24 months) reported that 18% (132/741) of bacteremias were detected by anaerobic cultures only, including 19% of S. aureus and 30% of common Enterobacterales bacteremias (43). Another study reported that only 13% of pediatric bacteremias were detected with anaerobic bottles only, with Bacteroides spp. and Peptostreptococcus being the two organisms only detected with anaerobic bottles in this cohort (44).
Optimal time to draw blood for culture: periodicity and time in relation to fever.
Bedside clinical providers’ blood culture education has focused on expeditious collection of blood cultures prior to antibiotic administration to maximize the yield of blood cultures (45), especially in patients with septic shock, when early antibiotic administration is critical for improved patient outcomes. The yield of blood cultures in these patients was recently evaluated among 325 adults presenting to the emergency department with severe sepsis/septic shock. The authors found that blood culture positivities were 31% for patients whose blood cultures were obtained before antibiotics and 19% for patients whose blood cultures were obtained up to 4 h post-antibiotic administration (45). Among 139 non-severely ill patients who had two sets of blood cultures before and after antibiotic administration within the first 72 h of hospitalization for fever or a community-acquired infection, <1% (1/139) had a positive blood culture with a different result in blood cultures obtained after antibiotic administration (46). Only the presence of endocarditis and isolation of S. aureus were independent predictors of positive blood cultures after antibiotic administration (46).
The optimal time interval between obtaining blood culture sets to maximize the yield of blood cultures is controversial. Historically, clinicians were taught that serial blood cultures may be a better strategy than simultaneous blood cultures to detect intermittent bacteremia. National guidelines recommend simultaneous blood draws in patients with septic shock to avoid delays in antibiotic administration, with a suggestion to space blood culture draws over several hours in nonurgent situations (23). Furthermore, an arbitrary 30- to 60-minute interval was proposed in the 1980s for non-critically ill patients. However, a study of blood cultures in the 1990s using the Bactec system found no difference in blood culture positivity if blood cultures were obtained simultaneously or at spaced intervals within a 24-h period (47). Further research with modern detection systems may be needed to validate the findings by Li and colleagues, especially for patients without endocarditis. Repeating blood cultures at ≥24 h of initial blood cultures is of value when trying to assess persistence of bacteremia: for example, during endovascular infections or in S. aureus bacteremia.
Riedel and colleagues evaluated the timing of blood culture collection in 1,436 febrile adult patients admitted with bacteremia and found that bacteremia detection was not enhanced by obtaining blood cultures closer to the time of the temperature spike, regardless of patient age and the pathogen causing bacteremia. This has not been evaluated in children or in adults with nosocomial bacteremia (48).
Optimal approach for obtaining blood culture: single versus multiple venipunctures.
Obtaining an adequate volume of blood for culture can be achieved through multiple venipunctures or by collecting an adequate large volume through a single venipuncture. In the United States, the multisampling strategy has been the preferred approach, and its advantages include a better chance to discriminate between blood culture contamination and true bacteremia and a hypothetical advantage of improving bacteremia detection (which, as noted earlier, the evidence does not seem to support), its major disadvantage being a higher rate of solitary blood cultures. In the single-sample strategy, the total recommended volume of blood is collected on a single draw and blood aliquots are equally distributed in the two aerobic bottles and two anaerobic bottles (36). Major advantages of this strategy include ensuring collection of enough blood volume and avoidance of multiple venipunctures to improve patient comfort. As noted, a single venipuncture performed with poor aseptic technique could lead to the appearance of a true bacteremia, with multiple bottles growing a skin commensal; thus, adherence to excellent antiseptic technique would be a prerequisite to adopting thus approach. In a prospective multicenter study, the single and multisite approaches were compared among 2,314 adults undergoing blood cultures for fever, hypothermia, or shock (49). Alcoholic povidone-iodine was used to clean the venipuncture site, and all patients underwent a 40-mL blood collection through a single venipuncture followed by additional blood culture collection (20 to 60 mL) within 24 h, so that for each patient both strategies were assessed. Rates of blood culture contamination were similar for both approaches (∼2%); however, blood culture positivity was higher for the single-site approach than the multisite approach when only 2 sets were obtained. (There was no difference in blood culture positivity with the multisite approach if >2 blood culture sets were obtained.) These data invite reconsideration of practice, especially in units for which longitudinal data are available and blood culture contamination rates are consistently low.
PARTNERSHIPS TO ENHANCE BLOOD CULTURE PERFORMANCE AND UTILIZATION
As mentioned earlier there is a critical need to improve blood culture practices for patient safety and health care resources reasons. We highlighted throughout this review several areas that need improvement and areas that require additional study from the moment a clinician is considering ordering blood cultures to how blood cultures are collected. Changing practices requires a multidisciplinary team, including representatives from the microbiology laboratory, antimicrobial stewardship, hospital epidemiology and infection control, nursing, medicine, surgery, the vascular access team, and phlebotomy. It is important that the blood culture quality metrics monitored by the microbiology laboratory reach the bedside providers so they can improve their practices. Identification of partners and venues to train and educate hospital staff about blood cultures is key to improve blood culture practices. Whenever possible, educators should include vascular access experts, microbiologists, and infectious disease specialists. Education can be multimodal and include “blood culture rounds” to discuss recent blood culture orders in the unit to help bedside providers recognize areas for improvement, workshops to improve blood culture draw technique, and passive education. Infection preventionists, clinical pharmacists, and other members of the medical team can identify additional aspects of blood cultures that require investigation, and they should be included in improvement efforts. We summarize considerations for implementing a blood culture improvement program in Table 3.
TABLE 3.
Consideration for a blood culture improvement program
| Consideration | Example of activity |
|---|---|
| Activities focused on the decision to order blood cultures | |
| Do baseline assessment of blood culture practices. | Audit 15–30 blood cultures in the ICU and non-ICU to characterize most common inappropriate indications locally. |
| Educate bedside staff on appropriate blood culture indications. | This can use already developed clinical decision tools. |
| This can use examples from audits of real cases. | |
| Develop/implement clinical guidance regarding appropriate blood cultures. | Consider starting with the “low hanging fruit” (limiting repeat blood cultures to document clearance of bacteremia and limiting repeat blood cultures for persistent fever/leukocytosis if there are previous negative blood cultures). |
| Implement blood culture ordering recommendations at the point of care and consider building these recommendations in the electronic medical record (EMR). | |
| Use a quality improvement framework. | The Plan-Do-Study-Act is a simple approach to improve practices, which includes evaluating the impact of a new intervention (e.g., new recommendations for blood culture indications on blood culture positivity) and collecting and providing feedback. |
| Make the blood culture improvement program a hospital priority and engage multiple stakeholders. | Involve multiple groups, such as vascular access teams (nursing and interventional radiology), pharmacy, and nutrition. |
| Review policies and protocols that have recommendations for blood cultures. | |
| Activities focused on the blood culture collection process | |
| Do baseline assessment of blood culture quality indicators. | Review blood culture quality indicator(s) already collected by the microbiology laboratory. |
| Make comparisons with similar units (e.g., single blood culture for 2 medical ICUs). | |
| Educate phlebotomy and non-phlebotomy personnel on preanalytical parameters that affect blood culture sensitivity. | If data are available, provide feedback to both unit leadership and frontline staff regarding blood culture positivity, single blood cultures, central line blood cultures, and blood culture contamination rates. |
| Assess barriers to improve practices. | Interview staff involved in collecting blood cultures. |
| Target the survey based on blood culture quality indicator data. | |
| Consider observing how blood cultures are being performed to identify additional barriers to improving practices. | |
SUMMARY
Diagnostic stewardship is critical to deliver safe patient care and to prevent devastating consequences related to test overuse, especially in an environment of value-based payment and quality metrics. Despite the role of blood cultures in the management of bloodstream infections, there has been a lack of national data on blood culture performance. Improvements are needed in both the process of blood culture collection and in blood culture indications. Establishing a blood culture range that maximizes bacteremia detection and minimizes potential harm and wasting of resources is critical to reduce unnecessary blood cultures. Equally important is the need to define clinical situations where blood cultures are not necessary or likely to be unhelpful to better guide clinicians in their decisions to order blood cultures. Benchmarks facilitate practice improvements and encourage collaborations among stakeholders; however, benchmarks for blood culture rates and blood culture positivity should be developed specific to hospital and unit characteristics.
ACKNOWLEDGMENT
We declare no conflict of interest.
Contributor Information
Valeria Fabre, Email: mfabre1@jhmi.edu.
Romney M. Humphries, Vanderbilt University Medical Center
REFERENCES
- 1.Goto M, Al-Hasan MN. 2013. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect 19:501–509. 10.1111/1469-0691.12195. [DOI] [PubMed] [Google Scholar]
- 2.Rhee C, Chiotos K, Cosgrove SE, Heil EL, Kadri SS, Kalil AC, Gilbert DN, Masur H, Septimus EJ, Sweeney DA, Strich JR, Winslow DL, Klompas M. 2021. Infectious Diseases Society of America position paper: recommended revisions to the National Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) sepsis quality measure. Clin Infect Dis 72:541–552. 10.1093/cid/ciaa059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linsenmeyer K, Gupta K, Strymish JM, Dhanani M, Brecher SM, Breu AC. 2016. Culture if spikes? Indications and yield of blood cultures in hospitalized medical patients. J Hosp Med 11:336–340. 10.1002/jhm.2541. [DOI] [PubMed] [Google Scholar]
- 4.Bates DW, Goldman L, Lee TH. 1991. Contaminant blood cultures and resource utilization. The true consequences of false-positive results. JAMA 265:365–369. 10.1001/jama.1991.03460030071031. [DOI] [PubMed] [Google Scholar]
- 5.Novis DA, Dale JC, Schifman RB, Ruby SG, Walsh MK. 2001. Solitary blood cultures: a College of American Pathologists Q-Probes study of 132,778 blood culture sets in 333 small hospitals. Arch Pathol Lab Med 125:1290–1294. 10.5858/2001-125-1290-SBC. [DOI] [PubMed] [Google Scholar]
- 6.Tabriz MS, Riederer K, Baran J, Jr, Khatib R. 2004. Repeating blood cultures during hospital stay: practice pattern at a teaching hospital and a proposal for guidelines. Clin Microbiol Infect 10:624–627. 10.1111/j.1469-0691.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 7.O'Grady NP, Barie PS, Bartlett JG, Bleck T, Carroll K, Kalil AC, Linden P, Maki DG, Nierman D, Pasculle W, Masur H, American College of Critical Care Medicine, Infectious Diseases Society of America. 2008. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med 36:1330–1349. 10.1097/CCM.0b013e318169eda9. [DOI] [PubMed] [Google Scholar]
- 8.Fabre V, Sharara SL, Salinas AB, Carroll KC, Desai S, Cosgrove SE. 2020. Does this patient need blood cultures? A scoping review of indications for blood cultures in adult non-neutropenic inpatients. Clin Infect Dis 71:1339–1347. 10.1093/cid/ciaa039. [DOI] [PubMed] [Google Scholar]
- 9.Zwang O, Albert RK. 2006. Analysis of strategies to improve cost effectiveness of blood cultures. J Hosp Med 1:272–276. 10.1002/jhm.115. [DOI] [PubMed] [Google Scholar]
- 10.Dunagan WC, Woodward RS, Medoff G, Gray JL, III, Casabar E, Smith MD, Lawrenz CA, Spitznagel E. 1989. Antimicrobial misuse in patients with positive blood cultures. Am J Med 87:253–259. 10.1016/S0002-9343(89)80146-9. [DOI] [PubMed] [Google Scholar]
- 11.Lamy B, Dargere S, Arendrup MC, Parienti JJ, Tattevin P. 2016. How to optimize the use of blood cultures for the diagnosis of bloodstream infections? A state-of-the art. Front Microbiol 7:697. 10.3389/fmicb.2016.00697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonsalves WI, Cornish N, Moore M, Chen A, Varman M. 2009. Effects of volume and site of blood draw on blood culture results. J Clin Microbiol 47:3482–3485. 10.1128/JCM.02107-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khare R, Kothari T, Castagnaro J, Hemmings B, Tso M, Juretschko S. 2020. Active monitoring and feedback to improve blood culture fill volumes and positivity across a large integrated health system. Clin Infect Dis 70:262–268. 10.1093/cid/ciz198. [DOI] [PubMed] [Google Scholar]
- 14.Buchman TG, Simpson SQ, Sciarretta KL, Finne KP, Sowers N, Collier M, Chavan S, Oke I, Pennini ME, Santhosh A, Wax M, Woodbury R, Chu S, Merkeley TG, Disbrow GL, Bright RA, MaCurdy TE, Kelman JA. 2020. Sepsis among medicare beneficiaries. 1. The burdens of sepsis, 2012–2018. Crit Care Med 48:276–288. 10.1097/CCM.0000000000004224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doern GV, Carroll KC, Diekema DJ, Garey KW, Rupp ME, Weinstein MP, Sexton DJ. 2019. A comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev 33:e00009-19. 10.1128/CMR.00009-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barber KE, Bell AM, Stover KR, Wagner JL. 2016. Intravenous vancomycin dosing in the elderly: a focus on clinical issues and practical application. Drugs Aging 33:845–854. 10.1007/s40266-016-0420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madden GR, Weinstein RA, Sifri CD. 2018. Diagnostic stewardship for healthcare-associated infections: opportunities and challenges to safely reduce test use. Infect Control Hosp Epidemiol 39:214–218. 10.1017/ice.2017.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyce JM, Nadeau J, Dumigan D, Miller D, Dubowsky C, Reilly L, Hannon CV. 2013. Obtaining blood cultures by venipuncture versus from central lines: impact on blood culture contamination rates and potential effect on central line-associated bloodstream infection reporting. Infect Control Hosp Epidemiol 34:1042–1047. 10.1086/673142. [DOI] [PubMed] [Google Scholar]
- 19.Seigel TA, Cocchi MN, Salciccioli J, Shapiro NI, Howell M, Tang A, Donnino MW. 2012. Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J Emerg Med 42:254–259. 10.1016/j.jemermed.2010.05.038. [DOI] [PubMed] [Google Scholar]
- 20.Vitrat-Hincky V, Francois P, Labarere J, Recule C, Stahl JP, Pavese P. 2011. Appropriateness of blood culture testing parameters in routine practice. Results from a cross-sectional study. Eur J Clin Microbiol Infect Dis 30:533–539. 10.1007/s10096-010-1115-8. [DOI] [PubMed] [Google Scholar]
- 21.Fabre V, Klein E, Salinas AB, Jones G, Carroll KC, Milstone AM, Amoah J, Hsu YJ, Gadala A, Desai S, Goyal A, Furfaro D, Zimmerman J, Lin S, Cosgrove SE. 2020. A diagnostic stewardship intervention to improve blood culture use among adult nonneutropenic inpatients: the DISTRIBUTE Study. J Clin Microbiol 58:e01053-20. 10.1128/JCM.01053-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, Griffin MR, Metersky ML, Musher DM, Restrepo MI, Whitney CG. 2019. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med 200:e45–e67. 10.1164/rccm.201908-1581ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gilligan PH, Gonzalez MD, Jerris RC, Kehl SC, Patel R, Pritt BS, Richter SS, Robinson-Dunn B, Schwartzman JD, Snyder JW, Telford S, III, Theel ES, Thomson RB, Jr, Weinstein MP, Yao JD. 2018. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update by the Infectious Diseases Society of America and the American Society for Microbiology. Clin Infect Dis 67:e1–e94. 10.1093/cid/ciy381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJC, Gorbach SL, Hirschmann JV, Kaplan SL, Montoya JG, Wade JC. 2014. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 59:e10–e52. 10.1093/cid/ciu296. [DOI] [PubMed] [Google Scholar]
- 25.Fabre V, Milstone AM, Keller SC, Carroll KC, Cosgrove SE. 2018. Prescribers’ knowledge, attitudes and perceptions about blood culturing practices for adult hospitalized patients: a call for action. Infect Control Hosp Epidemiol 39:1394–1396. 10.1017/ice.2018.224. [DOI] [PubMed] [Google Scholar]
- 26.Sick-Samuels AC, Woods-Hill CZ, Fackler JC, Tamma PD, Klaus SA, Colantuoni EE, Milstone AM. 2019. Association of a blood culture utilization intervention on antibiotic use in a pediatric intensive care unit. Infect Control Hosp Epidemiol 40:482–484. 10.1017/ice.2019.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baron EJ, Weinstein MP, Dunne WM, Jr, Yagupsky P, Welch DF, Wilson DM. 2005. Cumitech 1C, Blood cultures IV. Coordinating ed, Wilson DM. ASM Press, Washington, DC. [Google Scholar]
- 28.Karch A, Castell S, Schwab F, Geffers C, Bongartz H, Brunkhorst FM, Gastmeier P, Mikolajczyk RT. 2015. Proposing an empirically justified reference threshold for blood culture sampling rates in intensive care units. J Clin Microbiol 53:648–652. 10.1128/JCM.02944-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedman ND, Braun T, Fallach N, Carmeli Y. 2017. Blood culture sampling practices among internal medicine inpatients. Clin Microbiol Infect Dis 2:1–6. 10.15761/CMID.1000120. [DOI] [Google Scholar]
- 30.Woods-Hill CZ, Fackler J, Nelson McMillan K, Ascenzi J, Martinez DA, Toerper MF, Voskertchian A, Colantuoni E, Klaus SA, Levin S, Milstone AM. 2017. Association of a clinical practice guideline with blood culture use in critically ill children. JAMA Pediatr 171:157–164. 10.1001/jamapediatrics.2016.3153. [DOI] [PubMed] [Google Scholar]
- 31.Gross PA, Van Antwerpen CL, Hess WA, Reilly KA. 1988. Use and abuse of blood cultures: program to limit use. Am J Infect Control 16:114–117. 10.1016/0196-6553(88)90048-x. [DOI] [PubMed] [Google Scholar]
- 32.Pawlowicz A, Holland C, Zou B, Payton T, Tyndall JA, Allen B. 2016. Implementation of an evidence- based algorithm reduces blood culture overuse in an adult emergency department. Gen Int Med Clin Innov 1. 10.15761/GIMCI.1000108. [DOI] [Google Scholar]
- 33.Shapiro NI, Wolfe RE, Wright SB, Moore R, Bates DW. 2008. Who needs a blood culture? A prospectively derived and validated prediction rule. J Emerg Med 35:255–264. 10.1016/j.jemermed.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 34.She RC, Bender JM. 2019. Advances in rapid molecular blood culture diagnostics: healthcare impact, laboratory implications, and multiplex technologies. J Appl Lab Med 3:617–630. 10.1373/jalm.2018.027409. [DOI] [PubMed] [Google Scholar]
- 35.Morgan DJ, Malani P, Diekema DJ. 2017. Diagnostic stewardship—leveraging the laboratory to improve antimicrobial use. JAMA 318:607–608. 10.1001/jama.2017.8531. [DOI] [PubMed] [Google Scholar]
- 36.Lee A, Mirrett S, Reller LB, Weinstein MP. 2007. Detection of bloodstream infections in adults: how many blood cultures are needed? J Clin Microbiol 45:3546–3548. 10.1128/JCM.01555-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stewart JD, Graham M, Kotsanas D, Woolley I, Korman TM. 2019. Intermittent negative blood cultures in Staphylococcus aureus bacteremia; a retrospective study of 1071 episodes. Open Forum Infect Dis 6:ofz494. 10.1093/ofid/ofz494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Henning C, Aygul N, Dinnetz P, Wallgren K, Ozenci V. 2019. Detailed analysis of the characteristics of sample volume in blood culture bottles. J Clin Microbiol 57:e00268-19. 10.1128/JCM.00268-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bouza E, Sousa D, Rodríguez-Créixems M, Lechuz JG, Muñoz P, 2007. Is the volume of blood cultured still a significant factor in the diagnosis of bloodstream infections? J Clin Microbiol 45:2765–2769. 10.1128/JCM.00140-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cockerill FR, III, Wilson JW, Vetter EA, Goodman KM, Torgerson CA, Harmsen WS, Schleck CD, Ilstrup DM, Washington JA, II, Wilson WR. 2004. Optimal testing parameters for blood cultures. Clin Infect Dis 38:1724–1730. 10.1086/421087. [DOI] [PubMed] [Google Scholar]
- 41.Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J. 2009. Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. J Clin Microbiol 47:1021–1024. 10.1128/JCM.02162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lafaurie M, d'Anglejan E, Donay JL, Glotz D, Sarfati E, Mimoun M, Legrand M, Oksenhendler E, Bagot M, Valade S, Bercot B, Molina JM. 2020. Utility of anaerobic bottles for the diagnosis of bloodstream infections. BMC Infect Dis 20:142. 10.1186/s12879-020-4854-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shoji K, Komuro H, Watanabe Y, Miyairi I. 2013. The utility of anaerobic blood culture in detecting facultative anaerobic bacteremia in children. Diagn Microbiol Infect Dis 76:409–412. 10.1016/j.diagmicrobio.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 44.Gené A, Palacín E, García-García JJ, Muñoz-Almagro C. 2005. Value of anaerobic blood cultures in pediatrics. Eur J Clin Microbiol Infect Dis 24:47–50. 10.1007/s10096-004-1255-9. [DOI] [PubMed] [Google Scholar]
- 45.Cheng MP, Stenstrom R, Paquette K, Stabler SN, Akhter M, Davidson AC, Gavric M, Lawandi A, Jinah R, Saeed Z, Demir K, Huang K, Mahpour A, Shamatutu C, Caya C, Troquet JM, Clark G, Yansouni CP, Sweet D, FABLED Investigators. 2019. Blood culture results before and after antimicrobial administration in patients with severe manifestations of sepsis: a diagnostic study. Ann Intern Med 171:547. 10.7326/M19-1696. [DOI] [PubMed] [Google Scholar]
- 46.Grace CJ, Lieberman J, Pierce K, Littenberg B. 2001. Usefulness of blood culture for hospitalized patients who are receiving antibiotic therapy. Clin Infect Dis 32:1651–1655. 10.1086/320527. [DOI] [PubMed] [Google Scholar]
- 47.Li J, Plorde JJ, Carlson LG. 1994. Effects of volume and periodicity on blood cultures. J Clin Microbiol 32:2829–2831. 10.1128/jcm.32.11.2829-2831.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Riedel S, Bourbeau P, Swartz B, Brecher S, Carroll KC, Stamper PD, Dunne WM, McCardle T, Walk N, Fiebelkorn K, Sewell D, Richter SS, Beekmann S, Doern GV. 2008. Timing of specimen collection for blood cultures from febrile patients with bacteremia. J Clin Microbiol 46:1381–1385. 10.1128/JCM.02033-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dargere S, Parienti JJ, Roupie E, Gancel PE, Wiel E, Smaiti N, Loiez C, Joly LM, Lemee L, Pestel-Caron M, Du Cheyron D, Verdon R, Leclercq R, Cattoir V, UBC Study Group. 2014. Unique blood culture for diagnosis of bloodstream infections in emergency departments: a prospective multicentre study. Clin Microbiol Infect 20:O920–O927. 10.1111/1469-0691.12656. [DOI] [PubMed] [Google Scholar]
- 50.Berge A, Krantz A, Ostlund H, Naucler P, Rasmussen M. 2019. The DENOVA score efficiently identifies patients with monomicrobial Enterococcus faecalis bacteremia where echocardiography is not necessary. Infection 47:45–50. 10.1007/s15010-018-1208-3. [DOI] [PubMed] [Google Scholar]
- 51.Jafri F, Knoll BM. 2021. Low diagnostic yield of repeat blood cultures in adult haematologic malignancy patients with persistent neutropenic fever. J Intern Med 289:584–587. 10.1111/joim.13174. [DOI] [PubMed] [Google Scholar]
- 52.Kimura SI, Gomyo A, Hayakawa J, Tamaki M, Akahoshi Y, Harada N, Ugai T, Kusuda M, Kameda K, Wada H, Ishihara Y, Kawamura K, Sakamoto K, Sato M, Terasako-Saito K, Kikuchi M, Nakasone H, Kako S, Tanihara A, Kanda Y. 2017. Clinical significance of repeat blood cultures during febrile neutropenia in adult acute myeloid leukaemia patients undergoing intensive chemotherapy. Infect Dis (Lond) 49:748–757. 10.1080/23744235.2017.1340665. [DOI] [PubMed] [Google Scholar]