Myocarditis is a rare complication of COVID-19 mRNA vaccines.1 Although the short-term prognosis is usually favorable, little is known about the longitudinal follow-up and/or midterm prognosis of patients with COVID-19 vaccine–associated myocarditis (COV19VAM). In non–vaccine-related myocarditis, the persistency of nonischemic myocardial injury on cardiac magnetic resonance (CMR) imaging is associated with an increased risk of adverse cardiovascular events.2 However it is unknown whether the same occurs in COV19VAM. We present CMR imaging findings, as well as clinical characteristics (Table 1 ), of 5 adult patients previously affected by COV19VAM (Figures 1, 2, 3, 4, and 5 ). To our knowledge, this is the first systematic longitudinal evaluation of both clinical and imaging data up to 3-month follow-up (median follow-up time from first CMR in this study was 106 days; IQR: 75.5-107.5 days) for patients with previous COV19VAM.
Table 1.
Clinical Characteristics of Patients With Previous COVID-19 Vaccine–Associated Myocarditis
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | |
|---|---|---|---|---|---|
| Age, y | 34 | 32 | 24 | 19 | 18 |
| Sex | Male | Female | Male | Female | Male |
| Peak troponin, ng/mL | 5.9 | 10.9 | 6.3 | 10.7 | 4.4 |
| Vaccination type | Pfizer | Moderna | Pfizer | Moderna | Pfizer |
| Time between 1st and 2nd vaccination, d | 21 | No second dose | 17 | No second dose | 24 |
| Time between most recent vaccine and symptom onset, d | 4 | 19 | 5 | 1 | 2 |
| Previous COVID-19 infection (laboratory confirmed) | No | Yes | No | No | No |
| Comorbid conditions | None | None | None | Anxiety, depression | ADHD, anxiety |
| COVID-19 testing on admission | Negative | Negative | Negative | Negative | Negative |
| Time between initial CMR and follow-up CMR, d | 109 | 106 | 106 | 57 | 94 |
| LVEF on Initial CMR, % | 49 | 57 | 56 | 47 | 59 |
| LVEF on follow-up CMR, % | 59 | 57 | 60.0 | 58 | 63 |
| Symptoms at follow-up | Asymptomatic | Asymptomatic | Rare inspiratory chest pain | Exertional shortness of breath and chest pain | Asymptomatic |
| Extended Holter monitoring | No significant arrhythmia | Did not complete | No significant arrhythmia | No significant arrhythmia | No significant arrhythmia |
ADHD = attention-deficit/hyperactivity disorder; CMR = cardiac magnetic resonance; LVEF = left ventricular ejection fraction.
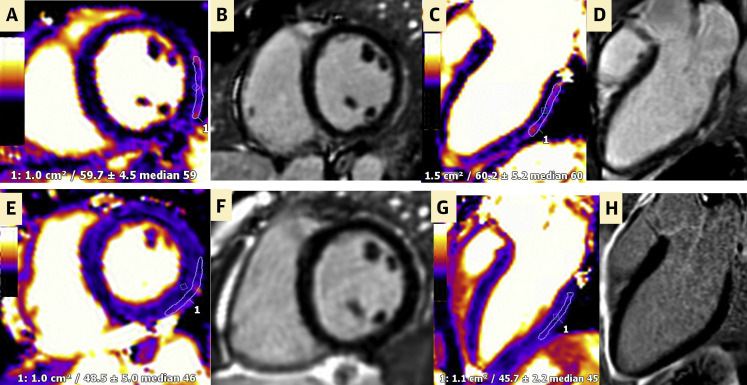
Figure 1.
Initial and Follow-Up CMR of Patient 1
(A to D) Initial cardiac magnetic resonance (CMR) of patient 1 that demonstrates (A and C) inferior and inferolateral epicardial edema on T2 mapping (region of interest #1 >55 ms, which is supportive of regional edema) and (B and D) corresponding nonischemic myocardial injury on imaging with late gadolinium enhancement (LGE) in a skip pattern, consistent with acute myocarditis according to the 2018 updated Lake Louise criteria. (E to H) Follow-up CMR demonstrating resolution of myocarditis without myocardial edema, scarring, or fibrosis.
Figure 2.
Initial and Follow-Up CMR of Patient 2
(A to D) Initial CMR of patient 2 demonstrating (A and C) myocardial edema and (B and D) epicardial to midmyocardial gadolinium uptake in a skip pattern consistent with acute myocarditis. (E to H) Follow-up CMR demonstrating (E and G) complete resolution of myocardial edema, with (F and H) discrete epicardial nonischemic fibrosis in the basilar inferior and inferolateral wall. 1 and 2 = regions of interest. Abbreviation as in Figure 1.
Figure 3.
Initial and Follow-Up CMR of Patient 3
(A to D) Initial CMR of patient 3 demonstrating (A and C) prominent myocardial edema and (B and D) LGE of the basal inferior and inferolateral walls consistent with acute myocarditis. (E to H) Follow-up CMR demonstrating (E and G) resolution of myocardial edema and (F and H) decrease in nonischemic LGE, consistent with the transition from injury or inflammation to replacement fibrosis. 1 and 2 = regions of interest. Abbreviations as in Figure 1.
Figure 4.
Initial and Follow-Up CMR of Patient 4
(A to D) Initial CMR of patient 4 demonstrating (A and C) epicardial edema on basal inferior, lateral, and middle anterolateral segments and (B and D) nonischemic myocardial injury involving the basal lateral and middle anterolateral segments in skip lesions on LGE imaging consistent with acute myocarditis. (E to H) Follow-up CMR demonstrating (E and G) resolution in myocardial edema and (F and H) improvement of nonischemic fibrosis along the basal lateral wall. 1 and 2 = regions of interest. Abbreviations as in Figure 1.
Figure 5.
Initial and Follow-Up CMR of Patient 5
(A to D) Initial CMR of patient 5 demonstrating (A and C) discrete myocardial edema in the mid anterolateral and (B and D) the corresponding nonischemic myocardial injury consistent with acute myocarditis. (E to H) Follow-up CMR demonstrating (E and G) resolved myocardial edema and (F) nearly resolved areas of gadolinium uptake but (H) still present in the epicardium of the midlateral to apical lateral wall. 1 and 2 = regions of interest. Abbreviation as in Figure 1.
Given the novelty of COV19VAM, data on midterm and long-term risks for these patients are lacking. Our study is the first to show a side-by-side systematic comparison of dedicated CMR imaging between the initial diagnosis of acute myocarditis and the approximately 3-month follow-up. This study demonstrated normalization of left ventricular ejection fraction in all patients and resolution of myocardial edema in all patients. There was interval improvement of nonischemic fibrosis seen on late gadolinium enhancement (LGE), albeit fibrosis was still present in 80% of patients. Although this finding could represent vulnerability for adverse cardiovascular long-term events, there were no unfavorable atrial or ventricular arrhythmias seen on a 2-week event monitor placed at 3-month follow-up from the initial diagnosis. Studies of non–vaccine-related myocarditis have demonstrated that persistence of LGE at a median follow-up of 4.7 years is a predictor of all-cause mortality and cardiac mortality.3 Although there is no current consensus on a timeline for repeat CMR imaging for patients affected by COV19VAM, our study highlights the need for ongoing longitudinal clinical evaluation in those patients with persistent LGE, to understand the long-term risks and prognosis of these patients more clearly.
Funding Support and Author Disclosures
Dr Cavalcante has reported research support from Circle Cardiovascular Imaging and Siemens Healthineers. Dr Gössl has reported consulting for Abbott Vascular. Dr Shaw has reported that she has no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Bozkurt B., Kamat I., Hotez P.J. Myocarditis with COVID-19 mRNA vaccines. Circulation. 2021;144(6):471–484. doi: 10.1161/CIRCULATIONAHA.121.056135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aquaro G.D., Perfetti M., Camastra G., et al. Cardiac Magnetic Resonance Working Group of the Italian Society of Cardiology. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function. J Am Coll Cardiol. 2017;70(16):1977–1987. doi: 10.1016/j.jacc.2017.08.044. [DOI] [PubMed] [Google Scholar]
- 3.Grün S., Schumm J., Greulich S., et al. Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol. 2012;59(18):1604–1615. doi: 10.1016/j.jacc.2012.01.007. [DOI] [PubMed] [Google Scholar]