Abstract
In this systematic review and meta-analysis, we sought to evaluate the prevalence of cardiac involvement in patients with COVID-19 using cardiac magnetic resonance imaging. A literature review was performed to investigate the left ventricular (LV) and right ventricular (RV) ejection fraction (EF), the prevalence of LV late gadolinium enhancement (LGE), pericardial enhancement, abnormality on T1 mapping, and T2 mapping/T2-weighted imaging (T2WI), and myocarditis (defined by modified Lake Louis criteria). Pooled mean differences (MD) between COVID-19 patients and controls for LVEF and RVEF were estimated using random-effects models. We included data from 10.462 patients with COVID-19, comprising 1.010 non-athletes and 9.452 athletes from 29 eligible studies. The meta-analysis showed a significant difference between COVID-19 patients and controls in terms of LVEF [MD = − 2.84, 95% confidence interval (CI) − 5.11 to − 0.56, p < 0.001] and RVEF (MD = − 2.69%, 95% CI − 4.41 to − 1.27, p < 0.001). However, in athletes, no significant difference was identified in LVEF (MD = − 0.74%, 95% CI − 2.41 to − 0.93, p = 0.39) or RVEF (MD = − 1.88%, 95% CI − 5.21 to 1.46, p = 0.27). In non-athletes, the prevalence of LV LGE abnormalities, pericardial enhancement, T1 mapping, T2 mapping/T2WI, myocarditis were 27.5% (95%CI 17.4–37.6%), 11.9% (95%CI 4.1–19.6%), 39.5% (95%CI 16.2–62.8%), 38.1% (95%CI 19.0–57.1%) and 17.6% (95%CI 6.3–28.9%), respectively. In athletes, these values were 10.8% (95%CI 2.3–19.4%), 35.4% (95%CI − 3.2 to 73.9%), 5.7% (95%CI − 2.9 to 14.2%), 1.9% (95%CI 1.1–2.7%), 0.9% (0.3–1.6%), respectively. Both LVEF and RVEF were significantly impaired in COVID-19 patients compared to controls, but not in athletes. In addition, the prevalence of myocardial involvement is not negligible in patients with COVID-19.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00380-022-02055-6.
Keywords: COVID-19, Cardiac involvement, Meta-analysis
Introduction
Coronavirus disease-2019 (COVID-19), caused by the novel severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), has become a global pandemic [1]. Cardiac involvement is a serious complication in patients with COVID-19 and elevated serum troponin levels are observed in 17–36% of the COVID-19 patients [2]. Cardiac involvement includes a variety of clinical manifestations, such as acute myocardial injury, heart failure, pulmonary embolism, myocarditis/pericarditis, and ventricular arrhythmias [3]. The mechanism of cardiac involvement is uncertain, but it may be related to endothelial dysfunction, systemic cytokine-mediated injury, or stress-related cardiomyopathy [4, 5]. Importantly, COVID-19 patients with cardiac involvement have worse clinical outcomes than those without cardiac involvement [6]. Therefore, elucidation of the imaging characteristics indicative of cardiac involvement may contribute to effective risk stratification for patients with COVID-19.
Cardiac magnetic resonance (CMR) imaging has emerged as a non-invasive imaging modality to accurately assess ventricular function, myocardial edema, and myocardial injury. Recently, several studies have demonstrated the utility of CMR imaging in detecting cardiac involvement in COVID-19 [7–11]. However, heterogeneity of data exists among these studies regarding the severity and prevalence of cardiac involvement detected by CMR imaging. Therefore, this study aimed to determine the prevalence of cardiac abnormalities detected by CMR imaging in patients with COVID-19.
Materials and methods
Literature search
The electronic database search formulas for PubMed, Web of Science Core Collection, Cochrane Advanced Search, and EMBASE are listed in the appendix (Supplemental material). Databases from the end of 2021 were searched on January 20, 2022. In addition, two review authors (SK and MA) independently performed additional manual searches. Potential research articles were screened and subjected to full-test scrutiny (KS, MA). When two authors could not resolve a disagreement, a third author participated in the discussion. The protocol for this systematic review, which complies with the Meta-analyses of Observational Studies in Epidemiology guidelines, has been registered on the website of the University Medical Informatics Network (UMIN000044237UMIN).
Eligibility criteria and outcomes
Publications including the CMR data of patients recovered from COVID-19 were screened. All study design types were used, including prospective studies, retrospective studies, and case series. However, we did not include case reports or case series with fewer than five cases because they are not suitable for estimating the frequency of adverse events. Eligible papers were written in English and both full articles and conference abstracts were accepted. Key study characteristics, such as author name, publication year, country of origin, and the number of COVID-19 patients, were extracted by two review authors (SK, MA). In addition, the outcome data were read by the authors. The main outcomes were mean averages of LVEF and RVEF, the prevalence of LV LGE, pericardial enhancement, abnormal T1 (native T1 time) mapping, abnormal T2 mapping/ T2 weighted image (T2WI), and myocarditis (defined by the modified Lake Louise criteria) [12]. LVEF and RVEF were compared between COVID-19 patients and controls. If one study had two cohorts (e.g., symptomatic vs. asymptomatic; LGE (+) vs. LGE (-)), we used patient data with abnormal findings and compared them to those of the controls (e.g., Brito 2021 symptomatic; Altay 2021 LGE (+); Chen 2021 troponin (+)). As the prevalence of cardiac involvement may differ between non-athletes and athletes, we analyzed these populations separately. In addition, the multisystem inflammatory syndrome is a different pathophysiologic response to SARS-CoV-2 exposure and is different (with a much different time course) from the convalescent phase post-acute COVID-19. We did not include multisystem inflammatory syndromes in our analysis [13].
Statistical analysis
The frequency of each cardiac abnormality was pooled using a random-model meta-analysis using the generic inverse variance method (RevMan ver 5.4. Cochrane Collaboration, London, UK). The standard error was calculated using the Agrestia method [14]. Random model meta-analysis was performed using RevMan 5.41 (Cochrane Collaboration, London, UK). LVEF and RVEF were expressed as median (range) in both COVID-19 patients and controls. Heterogeneity was indicated by I2, with 0% indicating no heterogeneity and 100% indicating the strongest heterogeneity.
Results
Study characteristics
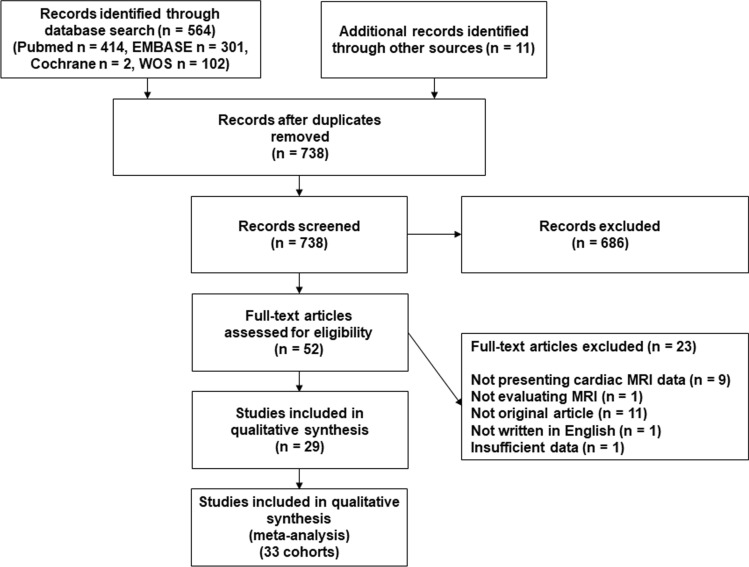
Of the 738 candidate studies, we finally selected 29 eligible reports [7–11, 15–38] (Fig. 1). Four of the studies presented two cohorts [8, 10, 21, 31]; therefore, we included a total of 33 independent cohorts. Among the 29 included studies, nine were from the USA [8, 15, 20, 22, 24, 32, 36–38], six were from China [10, 11, 16, 18, 21, 30], three each from the UK [19, 22, 26] and Germany [7, 23, 28, 35], two each from Italy [9, 27] and Turkey [29, 31], and one each from Poland [17], Norway [34], Hungary [33] and Spain [25]. The publication year was 2020 or 2021 (Table 1). Ten studies enrolled athletes recovered from COVID-19 [8, 15, 17, 20, 24, 32, 33, 36–38] and one study enrolled suspected myocarditis with COVID-19 [9]. Finally, 10.462 patients with COVID-19, including 1010 non-athletes and 9.452 athletes, and 746 controls were included in our analysis. A 1.5 T MR scanner was used in 15 studies [8, 9, 11, 15, 17, 22–26, 28, 29, 33–35] and a 3.0 T MR scanner was used in six studies [7, 10, 16, 18, 21, 30], Both 1.5 T and 3.0 T scanners were used in one study [20] and data regarding MR scanners were not provided in seven studies [19, 27, 31, 32, 36–38]. As the myocardial native T1 time substantially differs between different magnetic field strengths and sequences [39], we investigated the number patients with abnormal T1 time, rather than those with absolute value of native T1 time, among the nine studies presenting the prevalence of patients with abnormal native T1 times [7–9, 11, 17, 22, 26, 27, 32].
Fig. 1.
PRISMA flow diagram
Table 1.
Characteristics of 29 eligible studies
| Cohort | Country | MRI machine | Number of patients | Patient characteristics | Time from diagnosis (symptom) to MRI | LVEF, % | RVEF, % | LGE of LV, N (%) | Abnormal T1 map, N (%) | Abnormal T2 map/T2WI, N (%) | Pericardial enhancement, N (%) | Myocarditis, N (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brito 2021 | USA | 1.5 T | 37 asymptomatic; 11 symptomatic | Student athlete recovered from COVID-19 | 27 days | 59.09 (54.79–61.64) % in asymptomatic; 60.32 (56.66–63.33) % in symptomatic | 54.60% (47.55–59.77) in asymptomatic; 51.32% (50.82–57.22) in symptomatic | 0 (0%) in asymptomatic; 1 (3%) in symptomatic | 1 (9%) in asymptomatic; 8 (22%) in symptomatic | 0 (0%) in asymptomatic; 0 (0%) in symptomatic | 9 (82%) in asymptomatic; 10 (27%) in symptomatic | 0 (0%) |
| Clark 2021 | USA | 1.5 T | 59 | COVID-19–positive athletes | 21.5 days | 60 (56–63) % | 53 (50–56) % | 1 (2%) | N/A | N/A | 1 (2%) | 4 (15%) |
| Huang 2020 | China | 3.0 T | 26 CMR abnormal; 11 CMR normal | Patients recovered from COVID-19 (abnormal findings on CMR) | 48 days in CMR abnormal; 50 days in CMR normal | 60.7 ± 6.4% in CMR abnormal; 64.3 ± 5.8% in CMR normal | 36. 5 ± 6.1% in CMR abnormal; 41.1 ± 8.6% in CMR normal | 8 (26%) in CMR abnormal; N/A in CMR normal | N/A | N/A | N/A | N/A |
| Li 2021 | China | 3.0 T | 40 | Patients recovered from COVID-19 | 158 days | 62.6 ± 5.2% | 54.7 ± 5.8% | 1 (3%) | N/A | N/A | N/A | N/A |
| Pan 2021 | China | 3.0 T | 21 | Patients recovered from COVID-19 | N/A | 61.6 ± 6.5% | 54.7 ± 7.1% | N/A | N/A | N/A | N/A | N/A |
| Puntmann 2020 | Germany | 3.0 T | 100 | Patients recovered from COVID-19 | 71 days | 57 ± 6% | 54 ± 7% | 32 (32%) | 73 (73%) | 60 (60%) | 22 (22%) | N/A |
| Raisi-Estabragh 2021 | UK | N/A | 70 | UK Biobank participants with positive COVID-19 PCR | N/A | 59.6 ± 6.5% | 61.1 ± 6.2% | N/A | N/A | N/A | N/A | N/A |
| Wang 2021 | China | 3.0 T | 44 | Patients recovered from COVID-19 | 100.8 days in LGE positive; 103.3 days in LGE negative | 64.3 ± 5.9% in LGE positive; 62.2 ± 4.4% in LGE negative | 59.5 ± 8.6% in LGE positive; 56.6 ± 8.3% in LGE negative | 13 (29.5%) | N/A | N/A | N/A | N/A |
| Esposito 2020 | Italy | 1.5 T | 10 | COVID-19 patients suspected for myocarditis | N/A | N/A | N/A | 3 (30%) | 8 (100%) | 8 (100%) | N/A | 8 (80%) |
| Malek 2021 | Poland | 1.5 T | 26 | Elite athletes positive for COVID-19 PCR | 32 days | 61 (60–62) % | 59 (57–60) % | 1 (4%) | 0 (0%) | 4 (15%)a | N/A | 0 (0%) |
| Ng 2020 | China | 1.5 T | 16 | Patients recovered from COVID-19 | 56 days | 59 (56–65) % | 53 (48–57) % | 3 (19%) | 4 (25%) | 1 (5%) | N/A | N/A |
| Starekova 2021 | USA | 1.5 T or 3.0 T | 145 | Competitive student athletes recovered from COVID-19 | 16 days | 58 ± 5% | 54 ± 6% | 42 (29%) | N/A | N/A | N/A | 2 (1.4%) |
| Altay 2021 | Turkey | N/A | 15 | Symptomatic patients with COVID-19 | 81 days | 51 ± 16% | 45 ± 12% | 7 (46%) | N/A | N/A | N/A | N/A |
| Breitbart 2021 | Germany | 1.5 T | 56 | Post COVID-19 patients without previous heart diseases | 71 days | 62.3 ± 5.0% | N/A | 7 (12.5%) | N/A | N/A | N/A | 1 (2%) |
| Çakmak 2021 | Turkey | 1.5 T | 64 | Patients with cardiac symptoms after recovering from COVID-19 | 71 days | 67 (58–76) % in cardiac involvement (-); 62 (30–72) % in cardiac involvement ( +) | N/A | 46 (69%) | N/A | N/A | 11 (17%) | 0 (0%) |
| Chen 2021 | China | 3.0 T | 25 | Confirmed COVID-19 and at least one marker of cardiac involvement | 6.7 ± 5.7 days | 64.6 ± 4.6% | N/A | N/A | N/A | N/A | N/A | N/A |
| Daniels 2021 | USA | N/A | 1597 | Athletes with COVID-19 | N/A | N/A | N/A | 36 (2.3%) | 5 (0.3%) | N/A | N/A | 37 (2.3%) |
| Galea 2021 | Italy | N/A | 27 | Active COVID-19 and suspected cardiac involvement | 20 (13.5–31.5) days | 50.3 ± 7.2% | 48.8 ± 8.2% | 12 (44.4%) | 11 (40.7%) | 14 (51.9%) | 2 (7.4%) | 9 (33%) |
| Joy 2021 | UK, USA | 1.5 T | 149 |
Patients from COVID consortium |
N/A | 67.1 ± 4.9% | N/A | 13 (8.7%) | 6 (4%) | 9 (6%) | N/A | N/A |
| Kotecha 2021 | UK | 1.5 T | 148 | All patients admitted with a diagnosis of COVID-19 | 68 (39–103) days | 67 ± 11% | 61 ± 9% | 70 (47.3%) | 19 (12.8%) | 4 (2.7%) | N/A | 40 (27%) |
| Kravchenko 2021 | Germany | 1.5 T | 41 | SARS-CoV-2 infection who had persistent CCS symptoms | 103 (88–158) days | 62 ± 5% | N/A | 3 (7.3%) | N/A | N/A | N/A | 0 (0%) |
| Myhre 2021 | Norway | 1.5 T | 58 | Survivors from the prospective COVID MECH study | 175 (105–217) days | 58.7 ± 7.4% | 57.3 ± 6.3% | N/A | N/A | N/A | N/A | N/A |
| Rajpal 2021 | USA | 1.5 T | 26 | Competitive athletes referred to the sports medicine clinic after testing positive for COVID-19 | 11–53 days | N/A | N/A | 12 (46.2%) | N/A | N/A | N/A | 4 (15%) |
| Szabó 2021 | Hungary | 1.5 T | 147 | Athletes after SARS-CoV-2 infection | Median of 32 days | 57 (54–60)% | 56 (53–59)% | N/A | N/A | N/A | N/A | 1 (0.6%) |
| Tanacli 2021 | Germany | 1.5 T | 32 | Persistent cardiac symptoms after a COVID-19 infection | 95 ± 59 days | 62 ± 10% | 54 ± 8% | 6 (18.8%) | N/A | N/A | 3 (9.4%) | 3 (9%) |
| Urmeneta 2021 | Spain | 1.5 T | 57 | Post-COVID-19 patients | 81 ± 27 days, | 61 ± 10% | 60 ± 9% | 13 (22.8%) | N/A | N/A | 2 (3.5%) | N/A |
| Martinez 2021 | USA | N/A | 789 (30 MRI performed) | Professional athletes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 5 (0.6%) |
| Moulson 2021 | USA | N/A | 3018 (317 MRI performed) | Collegiate athletes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 21 (0.7%) |
| Petek 2021 | USA | N/A | 3597 (44 MRI performed) | Young competitive athletes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 5 (0.1%) |
LVEF and RVEF were presented as mean ± standard deviation or median (interquartile range). Myocarditis was diagnosed by modified Lake Louise Criteria
COVID-19 coronavirus diease-2019, CMR cardiac magnetic resonance, IQR interquartile range, LGE late gadolinium enhancement, LVEF left ventricular ejection fraction, MRI magnetic resonance imaging, RVEF right ventricular ejection fraction, T2WI T2 weighted image
aThree patients had abnormality in T2WI and one patient had abnormality in T2 mapping
Meta-analysis of CMR imaging findings in patients with COVID-19
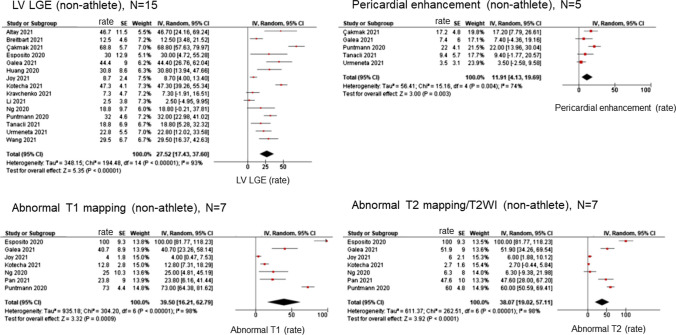
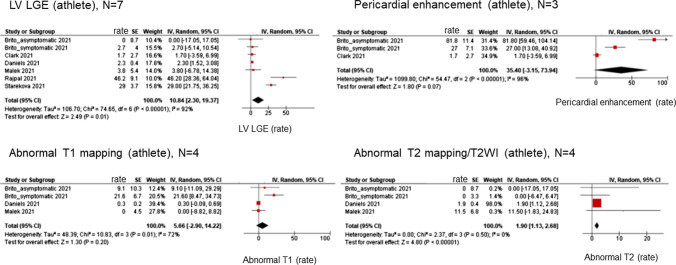
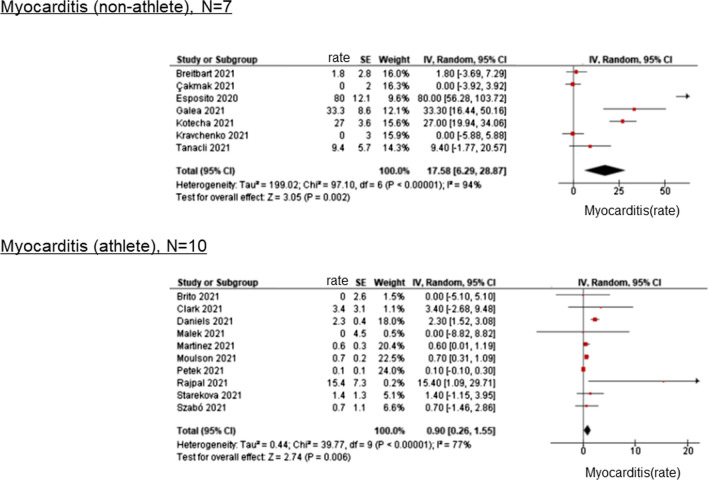
LVEF and RVEF were measured in 27 cohorts of 1414 COVID-19 patients. In COVID-19 patients, the median LVEF was 60.3% (range: 50.3–67.1%), and the median RVEF was 54.3% (range: 36.5–61.1%). In non-athlete, the median LVEF was 60.8% (range: 50.3–67.0%), and the median RVEF was 54.7% (range: 36.5–61.1%). In athlete, the median LVEF was 60.0% (range: 57.0–60.3%), and the median RVEF was 54.6% (range: 53.0–56.0%). In the controls, the median LVEF and RVEF were 61.3% (range: 57.0–67.0%) and 57.7% (range: 45.0–64.0%), respectively. The meta-analysis showed a significant difference between COVID-19 patients and controls in terms of LVEF [mean difference (MD) = − 2.84, 95% confidence interval (CI) − 5.11 to − 0.56, p < 0.001] and RVEF (MD = − 2.69%, 95% CI − 4.41, − 1.27, p < 0.001) (Fig. 2). However, in athletes, no significant differences were identified in LVEF (MD = − 0.74%, 95% CI − 2.41 to − 0.93, p = 0.39) and RVEF (MD = − 1.88%, 95% CI − 5.21 to 1.46, p = 0.27) (Fig. 3). Figure 4 illustrates the results of the meta-analysis of LGE of LV myocardium, pericardial enhancement, abnormal T1 mapping, and T2 mapping/T2WI in non-athletes. The prevalence of abnormalities of LV LGE, pericardial enhancement, T1 mapping, T2 mapping/T2WI were 27.5% (95%CI 17.4–37.6%), 11.9% (95%CI 4.1–19.6%), 39.5% (95%CI 16.2–62.8%), 38.1% (95%CI 19.0–57.1%), respectively (Fig. 4). In athletes, these values were 10.8% (95%CI 2.3–19.4%), 35.4% (95%CI − 3.2 to 73.9%), 5.7% (95%CI − 2.9 to 14.2%), 1.9% (95%CI 1.1–2.7%), respectively (Fig. 5). Figure 6 illustrates the prevalence of myocarditis, as defined by the modified Lake Louise criteria. The prevalence was 17.6% (95%CI 6.3–28.9%) for non-athletes and 0.9% (0.3–1.6%) for athletes.
Fig. 2.
Forest plot of comparison of LVEF and RVEF between non-athletes with COVID-19 and controls. The meta-analysis showed a significant difference between COVID-19 patients and controls in terms of LVEF (MD = − 2.84, 95%CI − 5.11 to − 0.56, p < 0.001) and RVEF (MD = − 2.69%, 95% CI − 4.41 to − 1.27, p < 0.001). CI confidence interval; CMR cardiac magnetic resonance; COVID-19 coronavirus disease-2019, LVEF left ventricular ejection fraction; MD mean difference; RVEF right ventricular ejection fraction
Fig. 3.
Forest plot of comparison of LVEF and RVEF between athletes with COVID-19 and controls. No significant difference was identified in LVEF (MD = − 0.74%, 95% CI − 2.41 to − 0.93, p = 0.39) and RVEF (MD = − 1.88%, 95% CI − 5.21 to 1.46, p = 0.27). CI confidence interval; COVID-19 coronavirus disease-2019, LVEF left ventricular ejection fraction; MD mean difference; RVEF right ventricular ejection fraction
Fig. 4.
Prevalence of cardiac abnormalities on CMR imaging in non-athletes with COVID-19. The prevalence of abnormalities such as LV LGE, pericardial enhancement, T1 mapping, T2 mapping/T2WI, and myocarditis were 27.5% (95%CI 17.4–37.6%), 11.9% (95%CI 4.1–19.6%), 39.5% (95%CI 16.2–62.8%), 38.1% (95%CI 19.0–57.1%). CI confidence interval; CMR cardiac magnetic resonance; COVID-19 coronavirus disease-2019, LGE late gadolinium enhancement; LV left ventricle
Fig. 5.
Prevalence of cardiac abnormalities on CMR imaging in athlete COVID-19. The prevalence of abnormalities of LV LGE, pericardial enhancement, T1 mapping, and T2 mapping/T2WI were 10.8% (95%CI 2.3–19.4%), 35.4% (95%CI − 3.2 to 73.9%), 5.7% (95%CI − 2.9 to 14.2%), 1.9% (95%CI 1.1–2.7%). CI confidence interval; CMR cardiac magnetic resonance; COVID-19 coronavirus disease-2019, LGE late gadolinium enhancement; LV left ventricle
Fig. 6.
Prevalence of myocarditis diagnosed by the modified Lake Louise criteria. The prevalence of myocarditis was 17.6% (95%CI 6.3–28.9%) for non-athletes and 0.9% (0.3–1.6%) for athletes
Discussion
The main findings of this study are as follows: both LVEF and RVEF were significantly reduced in non-athlete patients with COVID-19 compared with controls, whereas both parameters were not significantly reduced in athletes with COVID-19. There was a moderate prevalence of LV LGE, pericardial enhancement, abnormal T1 mapping, T2 mapping/T2WI, and myocarditis (defined by modified Lake Louise criteria) in patients with COVID-19. The prevalence of cardiac involvement was substantially higher in non-athletes than in athletes. These results indicate that cardiac involvement is not negligible in patients with COVID-19, and CMR imaging is useful for the non-invasive detection of cardiac abnormalities in patients with COVID-19.
The incidence of myocardial injury assessed by serum troponin was reported as 17–36% and is associated with poor clinical outcomes in patients with COVID-19 [6, 40–43]. For example, a report from New York including 2736 COVID-19 patients demonstrated that 36% of patients showed elevation of serum troponin T (defined as > 0.03 ng/dL), and even slight elevation of troponin I (> 0.03–0.09 ng/dL) was a significant predictor of mortality in COVID-19 patients [42]. A report from Wuhan revealed that serum creatinine kinase myocardial band (CK-MB), myoglobin, troponin I, and NT-proBNP were significantly elevated in deceased COVID-19 patients compared with survivors of COVID-19 [6]. In addition, higher CK-MB, myoglobin, and troponin I levels were associated with higher mortality, especially in older patients [6]. Therefore, an accurate assessment of cardiac involvement is crucial in patients with COVID-19.
Several echocardiographic studies have described the characteristics of cardiac abnormalities in patients with COVID-19. Szekely et al. investigated the echocardiographic spectrum of cardiac disease in hospitalized patients with COVID-19 and reported that the prevalence of RV dilatation/dysfunction was 39%, LV systolic dysfunction was 10%, and LV diastolic dysfunction was 16% [44]. Another echocardiographic study showed that the prevalence of right ventricular dilatation (basal diastolic RV diameter > 41 mm) was 31% and a significant predictive factor for worse clinical outcomes in COVID-19 patients [45]. Giustino et al. reported that the prevalence of RV dysfunction, LV wall motion abnormality, LV diastolic dysfunction, and LV global dysfunction were 26.3%, 23.7%, 13.2%, and 18.4%, respectively [5]. As shown in these studies, RV dysfunction is prevalent and clinically important in patients with COVID-19; however, an important limitation of echocardiographic assessment of RV function is that the accuracy is substantially dependent on the operator’s skill. Furthermore, the reproducibility of measurement of RV function is limited owing to the complexity of the anatomy of the RV.
CMR imaging is an accurate and highly reproducible technique for assessing RV function [46]. Previous studies have demonstrated the clinical relevance of CMR-derived RV function. A study including 250 patients with dilated cardiomyopathy showed that impaired RVEF (defined as RVEF ≤ 45%) is a significant predictor of transplant-free survival and adverse heart failure outcomes [47]. RV volume by cine CMR imaging after correction for age, sex, and body surface area strongly predicted mortality in patients with idiopathic pulmonary hypertension [48]. CMR-derived RVEF is a powerful prognostic marker, even in patients with non-cardiac diseases, such as interstitial lung disease [49]. In our study, RVEF by cine MRI was significantly lower in patients with COVID-19 than in controls, suggesting that RV dysfunction is an important spectrum of cardiac disease in patients with COVID-19 (Fig. 2).
In our analysis, several pathological changes in the LV which cannot be evaluated using echocardiology were observed, such as decreased LVEF, LGE, abnormal native T1 time, and T2 time/T2WI. These findings may be related to myocardial edema, necrosis, and fibrosis caused by SARS-CoV-2 infection [2]. Recently, an update of the CMR imaging diagnostic criteria for myocardial inflammation in patients with suspected acute myocardial inflammation has been published (modified Lake Louise criteria) [12]. These criteria include T2-based criteria (global or regional increase in myocardial T2 relaxation time or an increased signal intensity in T2WI) and T1-based criteria (increased myocardial T1, extracellular volume, or LGE), and maybe useful for evaluating myocarditis caused by COVID-19. Furthermore, the presence of LGE is associated with poor clinical outcomes in patients with acute myocarditis [50], indicating that the presence of LV LGE has the potential to effectively risk-stratify patients with COVID-19 suspected myocarditis. Further studies are necessary to clarify whether this is the case.
The precise mechanisms underlying cardiac disease in COVID-19 patients remain unclear. Direct viral infection, oxygen supply–demand imbalance (type 2 myocardial infarction), inflammation-related injury, coronary plaque rupture (type 1 myocardial infarction), microvascular dysfunction/thrombosis, and stress cardiomyopathy are possible pathophysiologies [2]. The angiotensin-converting enzyme 2 (ACE2) receptor may play an important role in COVID-19. SARS-CoV-2 is a single-stranded ribonucleic acid virus whose outer membrane spike protein binds with high affinity to the ACE2 receptor. Because ACE2 is primarily related to the conversion of angiotensin II to angiotensin 1–7, decreased ACE2 receptor density and impairment of ACE2 activity leads to an accumulation of angiotensin II, which results in vasoconstriction, inflammation, and fibrosis [2]. In another study, endothelial cell infection and endotheliitis of the kidney, small bowel, and lung tissue were demonstrated histopathologically [4]. For RV dysfunction, increased afterload following lung injury or hypoxemia, and RV ischemia due to hypoperfusion may be important pathophysiologies [51]. Further studies are required to confirm these points.
This meta-analysis had some limitations. First, the number of studies analyzed was small, and a multicenter study has not been published in this field. Second, we could not compare absolute T1 and T2 times between COVID-19 patients and controls, as these values substantially differ between different magnetic field strengths and sequences. Third, the inclusion criteria of each study were substantially variable; therefore, selection bias was not negligible. A large-scale prospective multicenter study will be required to address these limitations. Fourth, it should be noted that RVEF assessment is often less robust even with CMR imaging and more subjective with LVEF assessment due to problems with delineation of RV contours.
In conclusion, the meta-analysis showed that both LVEF and RVEF were significantly reduced in non-athletic patients with COVID-19 compared with the controls; however, these parameters were not significantly reduced in athletes with COVID-19. Furthermore, various abnormalities, such as LV LGE, pericardial enhancement, and abnormalities in T1 mapping and T2 mapping/T2WI were prevalent, and the occurrence of myocarditis was substantially higher in non-athletes than in athletes.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- ACE 2
Angiotensin converting enzyme 2
- COVID-19
Coronavirus disease 2019
- CI
Confidence interval
- CK-MB
Creatinine kinase myocardial band
- CMR
Cardiac magnetic resonance
- SARS-CoV-2
Severe acute respiratory syndrome-coronavirus-2
- LGE
Late gadolinium enhancement
- LV
Left ventricular
- MD
Mean difference
- MRI
Magnetic resonance imaging
- RV
Right ventricular
- T2WI
T2 weighted image
Funding
Research Grant, Japan Society for the Promotion of Science: Grant-in-Aid for Young Scientists.
Declarations
Conflict of interest
Nothing to declare.
Ethical approval
The present study is a meta-analysis of published articles. Accordingly, there is no need for IRB approval to conduct this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fauci AS, Lane HC, Redfield RR. Covid-19: navigating the uncharted. N Engl J Med. 2020;382(13):1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giustino G, Pinney SP, Lala A, Reddy VY, Johnston-Cox HA, Mechanick JI, Halperin JL, Fuster V. Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC focus seminar. J Am Coll Cardiol. 2020;76(17):2011–2023. doi: 10.1016/j.jacc.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hendren NS, Drazner MH, Bozkurt B, Cooper LT., Jr Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141(23):1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, Danilov T, Kukar N, Shaban N, Kini A, Camaj A, Bienstock SW, Rashed ER, Rahman K, Oates CP, Buckley S, Elbaum LS, Arkonac D, Fiter R, Singh R, Li E, Razuk V, Robinson SE, Miller M, Bier B, Donghi V, Pisaniello M, Mantovani R, Pinto G, Rota I, Baggio S, Chiarito M, Fazzari F, Cusmano I, Curzi M, Ro R, Malick W, Kamran M, Kohli-Seth R, Bassily-Marcus AM, Neibart E, Serrao G, Perk G, Mancini D, Reddy VY, Pinney SP, Dangas G, Blasi F, Sharma SK, Mehran R, Condorelli G, Stone GW, Fuster V, Lerakis S, Goldman ME. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2043–2055. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi S, Qin M, Cai Y, Liu T, Shen B, Yang F, Cao S, Liu X, Xiang Y, Zhao Q, Huang H, Yang B, Huang C. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(11):1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brito D, Meester S, Yanamala N, Patel HB, Balcik BJ, Casaclang-Verzosa G, Seetharam K, Riveros D, Beto RJ, 2nd, Balla S, Monseau AJ, Sengupta PP. High prevalence of pericardial involvement in college student athletes recovering from COVID-19. JACC Cardiovasc Imaging. 2021;14(3):541–555. doi: 10.1016/j.jcmg.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esposito A, Palmisano A, Natale L, Ligabue G, Peretto G, Lovato L, Vignale D, Fiocchi F, Marano R, Russo V. Cardiac magnetic resonance characterization of myocarditis-like acute cardiac syndrome in COVID-19. JACC Cardiovasc Imaging. 2020;13(11):2462–2465. doi: 10.1016/j.jcmg.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, Zeng H, Tao Q, Xia L. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC. 2020;13(11):2330–2339. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng MY, Ferreira VM, Leung ST, Yin Lee JC, Ho-Tung Fong A, To Liu RW, Man Chan JW, Wu AKL, Lung KC, Crean AM, Fan-Ngai Hung I, Siu CW. Patients recovered from COVID-19 show ongoing subclinical myocarditis as revealed by cardiac magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13(11):2476–2478. doi: 10.1016/j.jcmg.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, Kindermann I, Gutberlet M, Cooper LT, Liu P, Friedrich MG. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72(24):3158–3176. doi: 10.1016/j.jacc.2018.09.072. [DOI] [PubMed] [Google Scholar]
- 13.Theocharis P, Wong J, Pushparajah K, Mathur SK, Simpson JM, Pascall E, Cleary A, Stewart K, Adhvaryu K, Savis A, Kabir SR, Uy MP, Heard H, Peacock K, Miller O. Multimodality cardiac evaluation in children and young adults with multisystem inflammation associated with COVID-19. Eur Heart J Cardiovasc Imaging. 2021;22(8):896–903. doi: 10.1093/ehjci/jeaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coull AABA. Approximate is better than "exact" for interval estimation of binomial proportions. Am Stat. 1998;52:119–126. [Google Scholar]
- 15.Clark DE, Parikh A, Dendy JM, Diamond AB, George-Durrett K, Fish FA, Slaughter JC, Fitch W, Hughes SG, Soslow JH. COVID-19 myocardial pathology evaluation in athletes with cardiac magnetic resonance (COMPETE CMR) Circulation. 2021;143(6):609–612. doi: 10.1161/CIRCULATIONAHA.120.052573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li X, Wang H, Zhao R, Wang T, Zhu Y, Qian Y, Liu B, Yu Y, Han Y. Elevated extracellular volume fraction and reduced global longitudinal strains in participants recovered from COVID-19 without clinical cardiac findings. Radiology. 2021;299(2):E230–E240. doi: 10.1148/radiol.2021203998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Małek ŁA, Marczak M, Miłosz-Wieczorek B, Konopka M, Braksator W, Drygas W, Krzywański J. Cardiac involvement in consecutive elite athletes recovered from Covid-19: A magnetic resonance study. J Magn Reson Imaging. 2021;53(6):1723–1729. doi: 10.1002/jmri.27513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan C, Zhang Z, Luo L, Wu W, Jia T, Lu L, Liu WV, Qin Y, Hu F, Ding X, Qin P, Qian L, Chen J, Li S. Cardiac T1 and T2 mapping showed myocardial involvement in recovered COVID-19 patients initially considered devoid of cardiac damage. J Magn Reson Imaging. 2021;54(2):421–428. doi: 10.1002/jmri.27534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raisi-Estabragh Z, McCracken C, Cooper J, Fung K, Paiva JM, Khanji MY, Rauseo E, Biasiolli L, Raman B, Piechnik SK, Neubauer S, Munroe PB, Harvey NC, Petersen SE. Adverse cardiovascular magnetic resonance phenotypes are associated with greater likelihood of incident coronavirus disease 2019: findings from the UK Biobank. Aging Clin Exp Res. 2021;33(4):1133–1144. doi: 10.1007/s40520-021-01808-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Starekova J, Bluemke DA, Bradham WS, Eckhardt LL, Grist TM, Kusmirek JE, Purtell CS, Schiebler ML, Reeder SB. Evaluation for myocarditis in competitive student athletes recovering from coronavirus disease 2019 with cardiac magnetic resonance imaging. JAMA Cardiol. 2021;6(8):945–950. doi: 10.1001/jamacardio.2020.7444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang H, Li R, Zhou Z, Jiang H, Yan Z, Tao X, Li H, Xu L. Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2021;23(1):14. doi: 10.1186/s12968-021-00710-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joy G, Artico J, Kurdi H, Seraphim A, Lau C, Thornton GD, Oliveira MF, Adam RD, Aziminia N, Menacho K, Chacko L, Brown JT, Patel RK, Shiwani H, Bhuva A, Augusto JB, Andiapen M, McKnight A, Noursadeghi M, Pierce I, Evain T, Captur G, Davies RH, Greenwood JP, Fontana M, Kellman P, Schelbert EB, Treibel TA, Manisty C, Moon JC. Prospective case-control study of cardiovascular abnormalities 6 months following mild COVID-19 in healthcare workers. JACC Cardiovasc Imaging. 2021;14(11):2155–2166. doi: 10.1016/j.jcmg.2021.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanacli R, Doeblin P, Götze C, Zieschang V, Faragli A, Stehning C, Korosoglou G, Erley J, Weiss J, Berger A, Pröpper F, Steinbeis F, Kühne T, Seidel F, Geisel D, Cannon Walter-Rittel T, Stawowy P, Witzenrath M, Klingel K, Van Linthout S, Pieske B, Tschöpe C, Kelle S. COVID-19 vs. classical myocarditis associated myocardial injury evaluated by cardiac magnetic resonance and endomyocardial biopsy. Front Cardiovasc Med. 2021;8:737257. doi: 10.3389/fcvm.2021.737257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, Daniels CJ. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2021;6(1):116–118. doi: 10.1001/jamacardio.2020.4916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Urmeneta Ulloa J, Martínez de Vega V, Salvador Montañés O, Álvarez Vázquez A, Sánchez-Enrique C, Hernández Jiménez S, Sancho García FD, López Ruiz L, Recio Rodríguez M, Pizarro G, Carnevali Ruiz D, Ángel Cabrera J. Cardiac magnetic resonance in recovering COVID-19 patients. Feature tracking and mapping analysis to detect persistent myocardial involvement. Int J Cardiol Heart Vasc. 2021;36:1054. doi: 10.1016/j.ijcha.2021.100854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, Patel R, Chacko L, Brown JT, Coyle C, Leith D, Shetye A, Ariff B, Bell R, Captur G, Coleman M, Goldring J, Gopalan D, Heightman M, Hillman T, Howard L, Jacobs M, Jeetley PS, Kanagaratnam P, Kon OM, Lamb LE, Manisty CH, Mathurdas P, Mayet J, Negus R, Patel N, Pierce I, Russell G, Wolff A, Xue H, Kellman P, Moon JC, Treibel TA, Cole GD, Fontana M. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42(19):1866–1878. doi: 10.1093/eurheartj/ehab075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galea N, Marchitelli L, Pambianchi G, Catapano F, Cundari G, Birtolo LI, Maestrini V, Mancone M, Fedele F, Catalano C, Francone M. T2-mapping increase is the prevalent imaging biomarker of myocardial involvement in active COVID-19: a Cardiovascular Magnetic Resonance study. J Cardiovasc Magn Reson. 2021;23(1):68. doi: 10.1186/s12968-021-00764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kravchenko D, Isaak A, Zimmer S, Mesropyan N, Reinert M, Faron A, Pieper CC, Heine A, Velten M, Nattermann J, Kuetting D, Duerr GD, Attenberger UI, Luetkens JA. Cardiac MRI in patients with prolonged cardiorespiratory symptoms after mild to moderate COVID-19. Radiology. 2021;301(3):E419–e425. doi: 10.1148/radiol.2021211162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Çakmak Karaaslan Ö, Özilhan MO, Maden O, Tüfekçioğlu O. Prevalence of cardiac involvement in home-based recovered coronavirus disease 2019 (COVID-19) patients: a retrospective observational study. Irish J Med Sci. 2021 doi: 10.1007/s11845-021-02824-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen BH, Shi NN, Wu CW, An DA, Shi YX, Wesemann LD, Hu J, Xu JR, Shan F, Wu LM. Early cardiac involvement in patients with acute COVID-19 infection identified by multiparametric cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging. 2021;22(8):844–851. doi: 10.1093/ehjci/jeab042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Altay S. COVID-19 myocarditis cardiac magnetic resonance findings in symptomatic patients. Acta Radiol (Stockh, Swed) 2021 doi: 10.1177/02841851211046502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daniels CJ, Rajpal S, Greenshields JT, Rosenthal GL, Chung EH, Terrin M, Jeudy J, Mattson SE, Law IH, Borchers J, Kovacs R, Kovan J, Rifat SF, Albrecht J, Bento AI, Albers L, Bernhardt D, Day C, Hecht S, Hipskind A, Mjaanes J, Olson D, Rooks YL, Somers EC, Tong MS, Wisinski J, Womack J, Esopenko C, Kratochvil CJ, Rink LD. Prevalence of clinical and subclinical myocarditis in competitive athletes with recent SARS-CoV-2 infection: results from the big ten COVID-19 cardiac registry. JAMA Cardiol. 2021;6(9):1078–1087. doi: 10.1001/jamacardio.2021.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Szabó L, Juhász V, Dohy Z, Fogarasi C, Kovács A, Lakatos BK, Kiss O, Sydó N, Csulak E, Suhai FI, Hirschberg K, Becker D, Merkely B, Vágó H. Is cardiac involvement prevalent in highly trained athletes after SARS-CoV-2 infection? A cardiac magnetic resonance study using sex-matched and age-matched controls. Br J Sports Med. 2021 doi: 10.1136/bjsports-2021-104576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Myhre PL, Heck SL, Skranes JB, Prebensen C, Jonassen CM, Berge T, Mecinaj A, Melles W, Einvik G, Ingul CB, Tveit A, Berdal JE, Røsjø H, Lyngbakken MN, Omland T. Cardiac pathology 6 months after hospitalization for COVID-19 and association with the acute disease severity. Am Heart J. 2021;242:61–70. doi: 10.1016/j.ahj.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breitbart P, Koch A, Schmidt M, Magedanz A, Lindhoff-Last E, Voigtländer T, Schmermund A, Mehta RH, Eggebrecht H. Clinical and cardiac magnetic resonance findings in post-COVID patients referred for suspected myocarditis. Clin Res Cardiol. 2021;110(11):1832–1840. doi: 10.1007/s00392-021-01929-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martinez MW, Tucker AM, Bloom OJ, Green G, DiFiori JP, Solomon G, Phelan D, Kim JH, Meeuwisse W, Sills AK, Rowe D, Bogoch II, Smith PT, Baggish AL, Putukian M, Engel DJ. Prevalence of inflammatory heart disease among professional athletes with prior COVID-19 infection who received systematic return-to-play cardiac screening. JAMA Cardiol. 2021;6(7):745–752. doi: 10.1001/jamacardio.2021.0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moulson N, Petek BJ, Drezner JA, Harmon KG, Kliethermes SA, Patel MR, Baggish AL. SARS-CoV-2 cardiac involvement in young competitive athletes. Circulation. 2021;144(4):256–266. doi: 10.1161/CIRCULATIONAHA.121.054824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petek BJ, Moulson N, Baggish AL, Kliethermes SA, Patel MR, Churchill TW, Harmon KG, Drezner JA. Prevalence and clinical implications of persistent or exertional cardiopulmonary symptoms following SARS-CoV-2 infection in 3597 collegiate athletes: a study from the Outcomes Registry for Cardiac Conditions in Athletes (ORCCA) Br J Sports Med. 2021 doi: 10.1136/bjsports-2021-104644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haaf P, Garg P, Messroghli DR, Broadbent DA, Greenwood JP, Plein S. Cardiac T1 mapping and extracellular volume (ECV) in clinical practice: a comprehensive review. J Cardiovasc Magn Reson. 2016;18(1):89. doi: 10.1186/s12968-016-0308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, Zhao S, Somani S, Van Vleck T, Vaid A, Chaudhry F, De Freitas JK, Fayad ZA, Pinney SP, Levin M, Charney A, Bagiella E, Narula J, Glicksberg BS, Nadkarni G, Mancini DM, Fuster V. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76(5):533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan. China JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Szekely Y, Lichter Y, Taieb P, Banai A, Hochstadt A, Merdler I, Gal Oz A, Rothschild E, Baruch G, Peri Y, Arbel Y, Topilsky Y. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation. 2020;142(4):342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Argulian E, Sud K, Vogel B, Bohra C, Garg VP, Talebi S, Lerakis S, Narula J. Right Ventricular dilation in hospitalized patients with COVID-19 infection. JACC Cardiovasc Imaging. 2020;13(11):2459–2461. doi: 10.1016/j.jcmg.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J. 2006;27(23):2879–2888. doi: 10.1093/eurheartj/ehl336. [DOI] [PubMed] [Google Scholar]
- 47.Gulati A, Ismail TF, Jabbour A, Alpendurada F, Guha K, Ismail NA, Raza S, Khwaja J, Brown TD, Morarji K, Liodakis E, Roughton M, Wage R, Pakrashi TC, Sharma R, Carpenter JP, Cook SA, Cowie MR, Assomull RG, Pennell DJ, Prasad SK. The prevalence and prognostic significance of right ventricular systolic dysfunction in nonischemic dilated cardiomyopathy. Circulation. 2013;128(15):1623–1633. doi: 10.1161/CIRCULATIONAHA.113.002518. [DOI] [PubMed] [Google Scholar]
- 48.Swift AJ, Rajaram S, Campbell MJ, Hurdman J, Thomas S, Capener D, Elliot C, Condliffe R, Wild JM, Kiely DG. Prognostic value of cardiovascular magnetic resonance imaging measurements corrected for age and sex in idiopathic pulmonary arterial hypertension. Circ Cardiovasc Imaging. 2014;7(1):100–106. doi: 10.1161/CIRCIMAGING.113.000338. [DOI] [PubMed] [Google Scholar]
- 49.Kato S, Sekine A, Kusakawa Y, Ogura T, Futaki M, Iwasawa T, Kirigaya H, Gyotoku D, Iinuma N, Iguchi K, Nakachi T, Fukui K, Kimura K, Umemura S. Prognostic value of cardiovascular magnetic resonance derived right ventricular function in patients with interstitial lung disease. J Cardiovasc Magn Reson. 2015;17(1):10. doi: 10.1186/s12968-015-0113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Georgiopoulos G, Figliozzi S, Sanguineti F, Aquaro GD, di Bella G, Stamatelopoulos K, Chiribiri A, Garot J, Masci PG, Ismail TF. Prognostic impact of late gadolinium enhancement by cardiovascular magnetic resonance in myocarditis: a systematic review and meta-analysis. Circ Cardiovasc Imaging. 2021;14(1):e011492. doi: 10.1161/CIRCIMAGING.120.011492. [DOI] [PubMed] [Google Scholar]
- 51.Fayssoil A, Mustafic H, Mansencal N. The right ventricle in COVID-19 patients. Am J Cardiol. 2020;130:166–167. doi: 10.1016/j.amjcard.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.