Abstract
Objective:
Self-compassion is a positive psychological construct characterized by extending compassion towards oneself, often during periods of suffering. Whereas self-compassion has been associated with psychological outcomes, research linking self-compassion to physical health is limited. We tested the hypothesis that greater self-compassion would be associated with less subclinical cardiovascular disease (CVD) as assessed by carotid intima media thickness (IMT). We adjusted for demographics, CVD risk factors and additionally depressive symptoms in these associations.
Methods:
One hundred and ninety-five women (mean age=59 years) without CVD were recruited. Women completed questionnaires (Neff Self-Compassion Scale, Center for Epidemiology Studies of Depression Scale); physical measures [body mass index (BMI), blood pressure (BP)]; phlebotomy (lipids, insulin resistance); and ultrasound assessments of the carotid artery (mean, maximal IMT). Cross-sectional associations between self-compassion and IMT were assessed in linear regression models covarying for age, race/ethnicity, education, and CVD risk factors (BMI, BP, insulin resistance, lipids, medications), and additionally depressive symptoms.
Results:
Higher self-compassion was associated with lower mean IMT [B(SE)=−.03 (.01), p=.02], adjusting for demographic factors and CVD risk factors. Associations persisted adjusting for depressive symptoms. When considering self-compassion subscale bifactors, the positive self-compassion bifactor (self-compassion), but not negative self-compassion bifactor (self-coldness), was related to lower IMT.
Conclusions:
Self-compassion is associated with lower subclinical CVD. Associations were not explained by standard CVD risk factors nor by depressive symptoms. Future research should consider whether enhancing self-compassion improves women’s vascular health.
Keywords: Self-compassion, cardiovascular disease, intima media thickness, women, positive psychology
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the United States (Kochanek, Xu, & Arias, 2020; Virani et al., 2020). A large literature links negative psychosocial factors, such as depression or anxiety, to CVD risk (Penninx, 2017; Thurston, Rewak, & Kubzansky, 2013). An emerging body of research also links positive psychological factors, such as optimism, life satisfaction, or emotional vitality to reduced CVD risk (Kubzansky & Thurston, 2007; Matthews, Owens, Edmundowicz, Lee, & Kuller, 2006; Shahabi et al., 2016), associations which often persist after adjustment for negative psychological factors. One positive psychological trait of growing empirical interest is self-compassion. Self-compassion is a positive psychological construct characterized by extending compassion towards oneself, often during periods of suffering (Neff, 2003). Self-compassion is a multi-dimensional cognitive-affective construct whose core components include self-kindness, or relating to oneself with warmth and kindness; mindfulness, or a non-judgmental mind state towards one’s internal thoughts and feelings; and common humanity, or the awareness that difficulties are a universal human experience (Neff, 2003). Notably, a range of interventions have been developed to enhance self-compassion, and thereby it is modifiable and can be increased to promote health (Kirby, 2017).
Although self-compassion has been associated with a wide range of desirable psychological outcomes (Neff, Rude, & Kirkpatrick, 2007; Trompetter, de Kleine, & Bohlmeijer, 2017), the relation of self-compassion to CVD risk has received limited empirical attention. Emerging data are suggestive of a link between self-compassion and a variety of behavioral and biological CVD risk factors. For example, self-compassion is linked to health-promoting behaviors, including increased physical activity (Biber & Ellis, 2019; Dunne, Sheffield, & Chilcot, 2018; Holden, Rollins, & Gonzalez, 2020; Sirois, Kitner, & Hirsch, 2015), improved medical adherence in clinical patient populations (Sirois & Hirsch, 2019), and adaptive responding to CVD risk information (Semenchuk et al., 2020). Self-compassion has also been linked to select CVD risk factors such as lower insulin resistance, improved stress management, and better sleep quality (Butz & Stahlberg, 2018; Ferrari, Dal Cin, & Steele, 2017; Friis, Johnson, Cutfield, & Consedine, 2016; Morrison et al., 2019; Ventura et al., 2019). Finally, self-compassion has been associated with more adaptive physiological responses to acute stressors (e.g., inflammation, heart rate variability, systolic blood pressure) (Arch et al., 2014; Bluth et al., 2016; Breines et al., 2014; Luo, Qiao, & Che, 2018). Taken together, this research suggests that self-compassion may be associated with reduced risk for the development of CVD. However, no studies have examined self-compassion in relation to clinical or subclinical CVD.
Subclinical CVD indicators provide an important understanding of cardiovascular health before frank clinical disease is present. One well-established subclinical CVD indicator is carotid intima media thickness (IMT). Carotid IMT, assessed via ultrasound, is the thickness of the intimal and medial layers of the carotid artery, with higher IMT associated with greater risk for subsequent CVD (Peters, den Ruijter, Bots, & Moons, 2012; Stein et al., 2008). IMT predicts future CVD even among low risk populations (Peters et al., 2012; Stein et al., 2008). Thus, leveraging subclinical indicators of cardiovascular health to understand the relations of self-compassion to cardiovascular health can shed important light into the development of CVD risk before clinical disease is present.
Investigating self-compassion and cardiovascular health is particularly important among midlife women. For women, midlife and the menopause transition are times of vulnerability to negative mood (Bromberger & Epperson, 2018) and accelerated atherosclerosis accumulation (El Khoudary et al., 2013). As midlife occurs directly before the typical onset of clinical CVD in women, it is an important time for prevention. Identifying modifiable psychological factors or skills, such as self-compassion, that may protect mental and cardiovascular health is of critical clinical importance in this population.
Among a well-characterized cohort of CVD-free midlife women, we tested the hypothesis that greater self-compassion would be associated with lower carotid IMT. We hypothesized that associations between self-compassion and IMT would persist with adjustment for demographics and for standard CVD risk factors. Finally, given links between self - compassion and depression (Krieger, Berger, & Holtforth, 2016) and between depression and CVD risk (Penninx, 2017), we also considered the role of depressive symptoms in any self-compassion-IMT associations.
Methods
Sample
Midlife women (N=197) aged 45-67 participated in the MsBrain Study, a study of menopause and cardiovascular and brain health. MsBrain participants were recruited between 2017 and 2020 from the Pittsburgh, PA community and from the MsHeart study, a study of non-smoking women free of clinical CVD who were studied for menopause and cardiovascular health (Thurston et al., 2016). MsBrain exclusion criteria included a reported history of stroke or cerebrovascular accident; dementia; current chemotherapy; active substance use; pregnancy; and current use of select medications, including hormone therapy (oral or transdermal estrogen and/or progesterone), selective estrogen receptor modulators, aromatase inhibitors, selective serotonin reuptake inhibitors, or serotonin norepinephrine reuptake inhibitors. Of the 197 participants, two women were excluded due to missing data on carotid IMT (N=1) or self-compassion (N=1), yielding a sample of 195 women for primary models. Four additional women were missing data on key blood-based biomarkers [homeostatic model assessment (HOMA) and triglycerides], yielding a sample of 191 women for multivariable models that included CVD risk factors.
Design and Procedures
Participants completed screening procedures, physical measurements, a medical history interview, questionnaires, and a carotid ultrasound. Procedures were approved by the University of Pittsburgh Institutional Review Board. Participants provided written informed consent.
Measures
Self-compassion
Self-compassion was assessed via the Self Compassion Scale-Short form (Neff, 2016). This scale consists of 12 items rated from 1 (almost never) to 5 (almost always) and scored to yield a total self-compassion score. This scale has established reliability and validity (Neff, 2016; Raes, Pommier, Neff, & Van Gucht, 2011) and showed strong internal consistency in this investigation (α=.83). This scale includes six subscales which, consistent with other work (Brenner, Heath, Vogel, & Crede, 2017), we combined into self-compassion (self-kindness, mindfulness, common humanity) and self-coldness (self-judgement, isolation, over-identification) bifactors, which showed high internal consistency in the present study (self-compassion: α=.77; self-coldness: α=.80).
Carotid atherosclerosis
Trained and certified sonographers at the University of Pittsburgh’s Ultrasound Research Laboratory obtained bilateral carotid images via B-mode ultrasound using a Acuson Antares (Model# 10032747; Siemens, Malvern, Pennsylvania) high-resolution duplex scanner equipped with a VF10-5 transducer according to a standardized protocol (Sutton-Tyrrell et al., 1992). Digitized images were obtained at end-diastole from eight locations (four locations each from the left and right carotid arteries): the near and far walls of the distal common carotid artery, the far walls of the carotid bulb, and the internal carotid artery. Images were read using semi-automated reading software (Wendelhag, Gustavsson, Suurkula, Berglund, & Wikstrand, 1991). Values were obtained by electronically tracing the lumen-intima interface and the media-adventitia interface across a 1-cm segment for each of these eight segments. Average and maximal values were recorded for each of the eight locations; mean and maximal IMT was the mean of the mean and maximal readings across these eight locations, respectively. Reproducibility of IMT measures was excellent [intraclass correlation coefficient between sonographers ≥0.87, between readers=0.92].
Additional measures
Additional measures included demographic factors, CVD risk factors, and additional psychological characteristics. Demographics; medical and psychiatric history; medication use; and health behaviors were assessed by questionnaires and an interview. Race/ethnicity was self-reported. Educational attainment was assessed as years of completed education (classified as high school/vocational, college graduate, >college). Height was measured via fixed stadiometer, weight via a balance beam scale, and BMI was calculated [weight (kg)/height2 (m)]. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) was the average of three seated measurements taken via a Dinamap v100. Physical activity was assessed via the International Physical Activity Questionnaire (IPAQ) (Craig et al., 2003). Glucose, total cholesterol, high density lipoprotein cholesterol (HDL), and triglycerides were determined using enzymatic assays; insulin was determined by immunoturbidimetric assay in serum (ACE Axcel, Alfa Wasserman; West Caldwell, NJ). LDL was calculated using the Friedewald equation (Friedewald, Levy, & Fredrickson, 1972). HOMA, an index reflecting insulin resistance, was calculated [(fasting insulin*fasting glucose)/22.5] (Matthews, Hosker, Rudenski, Naylor, Treacher, et al., 1985). Depressive symptoms were assessed via the Center for Epidemiologic Studies Depression Survey (CESD) (Radloff, 1977). Anxiety was assessed via the State-Trait Anxiety Inventory (Spielberger, 1983).
Statistical analysis
Variables were examined for distributions, outliers, and cell sizes. BMI, HOMA, triglycerides, and IMT were log transformed to conform to model assumptions of normality. Bivariate relations between study variables and study outcomes were examined via Pearson and Spearman correlation coefficients. We tested the relation of self-compassion (total scale score) to mean IMT in linear regression models. Each outcome was considered separately. Covariates were a priori selected for inclusion in models, and included demographic factors age, race, and education, as well as standard CVD risk factors (BMI, blood pressure, lipids, insulin resistance, medications to treat hypertension, diabetes, and dyslipidemia). For multiple highly correlated risk factors (e.g., systolic and diastolic blood pressure, lipids), those most strongly related to the outcome was considered in models. Depressive symptoms (considered as both as a continuous variable and categorized according to the clinical cutpoint: CESD score ≥16) (Radloff, 1977) were considered in a separate step as a covariate. In additional models, subscale bifactors (self-compassion, self-coldness) were considered separately in relation to IMT; interactions between self-compassion and depressive symptoms in relation to IMT were tested with cross product terms; and anxiety and health behaviors were considered as additional covariates in self-compassion-IMT relationships. Maximal IMT was considered as a secondary outcome. All tests were two tailed with an alpha set to 0.05. Analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC).
Results
Participants were on average 59 years old, overweight, and normotensive (Table 1). Self-compassion scores were consistent with other studies of midlife women (Brown, Bryant, Brown, Bei, & Judd, 2014). Participant characteristics did not vary as function of self-compassion with the exception of age, physical activity, and depressive symptoms, with more self-compassionate women being older (r=.17, p=.02) and more physically active (r=.15, p=.04), and having lower depressive symptoms (r=−.56, p<.0001).
Table 1.
Participant characteristics
| N | 195 |
| Age, M (SD) | 58.81 (4.20) |
| Race/ethnicity, N (%) | |
| White | 146 (74.87) |
| Black / Other | 49 (25.13) |
| Education, N (%) | |
| High school/some college/vocational | 75 (38.46) |
| College graduate | 59 (30.26) |
| >College | 61 (31.28) |
| BMI, Median (IQR) | 28.02 (24.53, 33.60) |
| SBP, mmHg, M (SD) | 117.93 (14.19) |
| DBP, mmHg, M (SD) | 68.16 (8.87) |
| LDL, mg/dL, M (SD) | 118.85 (33.92) |
| HDL, mg/dL, M (SD) | 64.29 (16.93) |
| Triglycerides, mg/dL, Median (IQR) | 95.00 (71.00, 123.00) |
| HOMA, Median (IQR) | 3.42 (2.10, 4.95) |
| Physical activity, Median (IQR)† | 396.00 (0.00, 1399.00) |
| Smoking, N (%) | 5 (2.56) |
| Medications, N (%) | |
| Anti-hypertensive | 46 (23.59) |
| Anti-diabetic | 13 (6.67) |
| Lipid-lowering | 32 (16.41) |
| Depressive symptoms, high, N (%)‡ | 31 (15.90) |
| Self-compassion, M (SD)¶ | 3.60 (0.74) |
| Mean IMT, mm, Median (IQR) | 0.69 (0.62, 0.77) |
| Maximal IMT, mm, Median (IQR) | 0.86 (0.77, 0.95) |
IPAQ leisure time physical activity scores,
CESD score ≥16,
Total self-compassion scale score
We tested the relation of self-compassion to IMT. We found that women with higher self-compassion had lower mean IMT (Table 2, Figure 1). These associations persisted when controlling for covariates, including demographic factors and standard CVD risk factors. Findings were similar when considering the outcome of maximal IMT (Supplemental Table, Supplemental Figure).
Table 2.
Association between self-compassion and IMT
| Mean IMT | ||
|---|---|---|
|
| ||
| Model 1 B(SE) |
Model 2 B(SE) |
|
| Self-compassion | −.04 (.02)** | −.03 (.01)* |
| Age | .01 (.003)*** | .01 (.003)*** |
| Race (White vs. Non-white) | −.02 (.03) | −.003 (.03) |
| Education (≥College) | −.05 (.02) | −.04 (.02) |
| SBP | .002 (.001)** | |
| BMI | .04 (.06) | |
| HOMA | .02 (.02) | |
| Triglycerides | .04 (.03) | |
| Hypertension medication | .03 (.03) | |
| Lipid-lowering medication | .03 (.03) | |
| Diabetes medication | −.04 (.05) | |
IMT = intima media thickness; SBP = systolic blood pressure; BMI = body mass index; HOMA = homeostatic model assessment. IMT, BMI, HOMA, triglycerides, values log transformed for analysis.
p<.05,
p<.01,
p<.001
Figure 1. Mean IMT by self-compassion score.
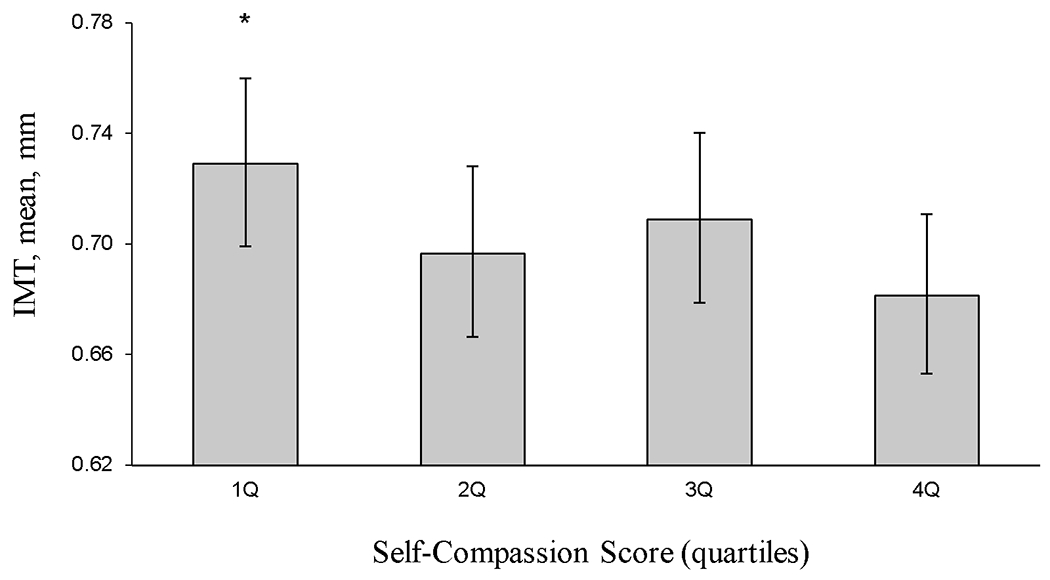
Means adjusted for age, race, and education. IMT = intima-media thickness. * p<.05 (first versus fourth quartile comparison).
We next considered the role of depressive symptoms in these relationships. Depressive symptoms were not significantly related to mean IMT [e.g., b(SE)=.001(.001), p=.52, multivariable, controlling for demographic factors and CVD risk factors] and associations of self-compassion to IMT persisted controlling for depressive symptoms [e.g., self-compassion in relation to mean IMT: b(SE)=−.04 (.02), p=.02, controlling for demographic factors, CVD risk factors, and depressive symptoms].
We explored the relationship between self-compassion and self-coldness bifactors in relation to mean IMT. Results indicated that the self-compassion bifactor was related to lower mean IMT [B(SE)=−.02 (.005), p=.002], whereas self-coldness was not [B(SE)=.007 (.005), p=.12] in models adjusted for age, race, education, BMI, HOMA, triglycerides, SBP, and medications for blood pressure, lipids, and diabetes.
Further, given potential interest in self-compassion as a resilience factor that may protect the cardiovascular health among women with negative mood, we explored an interaction between self-compassion (total scale score) and high depressive symptoms (CESD score ≥16); a significant interaction was observed (p=.04, adjusted for age, race, education), suggesting that associations between self-compassion and IMT may be most pronounced among women with high depressive symptoms [high depressive symptoms: b(SE)= −0.12 (.06), p=.05; low depressive symptoms: b(SE)=−.03 (.02), p=.09, adjusted for age, race, education]; however, these analyses should be regarded with caution given the relatively few women with high depressive symptoms (N=31). Finally, we explored other possible mechanisms linking self-compassion to health, including anxiety and health behaviors (physical activity, smoking); but these factors were not significantly related to IMT, nor did they alter associations between self-compassion and IMT when included in multivariable models (data not shown).
Discussion
In this study of midlife women, women with greater self-compassion had lower IMT than those with lower self-compassion. These associations were not explained by demographic factors or by traditional CVD risk factors such as blood pressure, insulin resistance, or lipids, nor by depressed mood. When further considering self-compassion and self-coldness subscale bifactors, associations with IMT were most apparent for self-compassion. Collectively, these data indicate the importance of self-compassion to women’s cardiovascular health.
This study is the first to show self-compassion associated with lower subclinical CVD. Use of subclinical CVD indicators are particularly important here as they provide a direct measure of the vasculature and thus represent a more proximal indicator of disease development. Notably, we demonstrated a consistency of associations of self-compassion to IMT measured as mean IMT, which represents the mean thickness of the intimal and medial layers of the carotid artery across eight locations, as well as maximal IMT, which represents the maximal thickness across these locations (Stein et al., 2008). The consistency of associations between self-compassion and IMT across IMT measures supports the reliability of findings. In fact, the magnitude of difference in IMT associated with low versus high self-compassion was similar to IMT differences associated with standard CVD risk factors (e.g., obesity, elevated triglycerides) or five years of aging among these midlife women (El Khoudary et al., 2013; Herder, Johnsen, Arntzen, & Mathiesen, 2012).
Multiple potential mechanisms may link self-compassion to cardiovascular outcomes, several of which we considered here. Specifically, less self-compassionate women may have more adverse traditional CVD risk factors, including lower physical activity and higher insulin resistance (Biber & Ellis, 2019; Dunne et al., 2018; Holden et al., 2020; Matthews, Hosker, Rudenski, Naylor, Teacher, et al., 1985; Morrison et al., 2019; Sirois et al., 2015). However, we assessed CVD risk factors here; none of these CVD risk factors varied as a function of self-compassion, nor did they explain associations between self-compassion and IMT. Some prior work has shown self-compassion to be associated with health-promoting behaviors (Biber & Ellis, 2019; Sirois et al., 2015), and self-compassion was related to more leisure time physical activity here. However, we considered both physical activity and smoking as covariates in additional analyses; neither of these factors were related to IMT, nor did they explain associations between self-compassion and IMT. Notably, an extensive prior literature links depression to subclinical and clinical CVD risk (Penninx, 2017), and higher self-compassion is typically associated with lower depressive symptoms (Krieger et al., 2016). However, depression did not explain relationships of self-compassion to IMT. We also considered anxiety, as anxiety has been linked to CVD risk (Thurston et al., 2013); however, anxiety did not relate to IMT nor did it explain self-compassion-IMT associations. Future work should examine the role of other potential physiologic systems, such as alterations in the autonomic nervous system (Arch et al., 2014; Luo et al., 2018; Svendsen et al., 2016), the hypothalamic pituitary adrenal axis (Herriot, Wrosch, & Gouin, 2018), inflammatory pathways (Breines et al., 2014), or epigenetic changes in these associations.
In exploratory analyses, to further understand what aspects of self-compassion were related to IMT, we considered self-compassion subscales in the context of two bifactors: self-compassion and self-coldness, consistent with prior work (Brenner et al., 2017). Findings showed self-compassion, rather than self-coldness, related to IMT. Prior work has pointed to the potential importance of mindfulness to cardiovascular health (Loucks et al., 2015); here we expand this examination to consider self-compassion, of which mindfulness is a component, yet is a relatively novel psychological factor to consider in relation to CVD risk. Positive and negative psychological functioning are often moderately inversely correlated and many aspects of negative psychological functioning have emerged as CVD risk factors; yet research has emphasized the importance of positive psychological functioning beyond simply the absence of negative psychological functioning for cardiovascular health (Kubzansky et al., 2018). Our findings further underscore the importance of positive psychological functioning broadly, and self-compassion in particular, to women’s cardiovascular health.
We considered self-compassion as a potential resilience factor buffering women from the potential negative cardiovascular sequelae of depression. A significant interaction between depressive symptoms and self-compassion in relation to IMT indicated that the lower IMT observed among those with higher self-compassion may be most apparent among women with elevated depressive symptoms. These patterns of findings are consistent with prior findings that relationships between self-compassion and CVD risk factors are most apparent under conditions of stress or distress (Bluth et al., 2016; Friis, Johnson, Cutfield, & Consedine, 2015; Herriot et al., 2018). This interaction must be interpreted with caution given the exploratory nature of analyses and the few women with elevated depressive symptoms. However, they do point to potential future areas of investigation and intervention, including targeting more distressed women with self-compassion interventions to protect their cardiovascular health.
This work has limitations. This study is a cross-sectional, observational study. Thus, the directionality or temporality of associations cannot be inferred from this study. Future work should consider whether self-compassion is associated with changes in cardiovascular health over time and whether intervening to enhance self-compassion improves cardiovascular health. Several analyses, such as bifactor analyses and interactions by depressive symptoms, were exploratory in nature and should be regarded as hypothesis generating. This study included key exclusions, such as select antidepressant use, hormone therapy use, and oophorectomy that may have resulted in a lower psychosocial and biological risk sample than the general population. Finally, this sample largely included non-Hispanic White and Black women; these associations require replication in women from a wider range of racial/ethnic groups and in men.
This work had key strengths. This study represents a novel investigation of self-compassion with cardiovascular health. We addressed this question using direct measurements of the vasculature, a more proximal measurement of underlying vascular disease than self-reported indicators or more nonspecific biomarkers. We assessed these associations in midlife women, a key population often experiencing challenges to both their psychological and physical health and who may benefit from preventive intervention. A wide range of measurements of CVD risk factors and of psychological functioning were included, allowing for investigation of a range of potential confounders or mechanisms in these associations.
In conclusion, we found that higher self-compassion was associated with lower carotid IMT among a well-characterized sample of midlife women. Findings were not explained by standard CVD risk factors, demographic factors, nor by negative mood. These findings point to the importance of self-compassion to women’s cardiovascular health. As self-compassion is modifiable (Kirby, 2017), our findings point to potential promising areas for future intervention, including whether self-compassion may be leveraged to enhance women’s cardiovascular health as they age.
Supplementary Material
Acknowledgments
This research was supported by the National Institutes of Health (NIH), National Institute on Aging (RF1AG053504 to Thurston & Maki) and the NIH Heart Lung and Blood Institute (2K24HL123565 to Thurston). This work was also supported by the University of Pittsburgh Clinical and Translational Science Institute (NIH Grant UL1TR000005). This project used the University of Pittsburgh Small Molecule Biomarker Core (NIH Grant S10RR023461-01).
Dr. Thurston receives consultant fees from Astellas Pharma, Vira Health and Happify Health. Dr. Maki receives consultant fees from Abbvie, Astellas, Pfizer Inc., and Balchem Corporation. Drs. Fritz, Chang, and Barinas-Mitchell have no conflicts.
REFERENCES
- Arch JJ, Brown KW, Dean DJ, Landy LN, Brown KD, & Laudenslager ML (2014). Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology, 42, 49–58. doi: 10.1016/j.psyneuen.2013.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biber DD, & Ellis R (2019). The effect of self-compassion on the self-regulation of health behaviors: A systematic review. Journal of Health Psychology, 24(14), 2060–2071. doi: 10.1177/1359105317713361 [DOI] [PubMed] [Google Scholar]
- Bluth K, Roberson PN, Gaylord SA, Faurot KR, Grewen KM, Arzon S, & Girdler SS (2016). Does Self-compassion Protect Adolescents from Stress? J Child Fam Stud, 25(4), 1098–1109. doi: 10.1007/s10826-015-0307-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breines JG, Thoma MV, Gianferante D, Hanlin L, Chen X, & Rohleder N (2014). Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain Behav Immun, 37, 109–114. doi: 10.1016/j.bbi.2013.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner RE, Heath PJ, Vogel DL, & Crede M (2017). Two is more valid than one: Examining the factor structure of the Self-Compassion Scale (SCS). Journal of Counseling Psychology, 64(6), 696–707. doi: 10.1037/cou0000211 [DOI] [PubMed] [Google Scholar]
- Bromberger JT, & Epperson CN (2018). Depression During and After the Perimenopause: Impact of Hormones, Genetics, and Environmental Determinants of Disease. Obstetrics and Gynecology Clinics of North America, 45(4), 663–678. doi: 10.1016/j.ogc.2018.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown L, Bryant C, Brown VM, Bei B, & Judd FK (2014). Self-compassion weakens the association between hot flushes and night sweats and daily life functioning and depression. Maturitas, 78(4), 298–303. doi: 10.1016/j.maturitas.2014.05.012 [DOI] [PubMed] [Google Scholar]
- Butz S, & Stahlberg D (2018). Can self-compassion improve sleep quality via reduced rumination? Self and Identity, 17(6), 666–686. doi: 10.1080/15298868.2018.1456482 [DOI] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, … Oja P (2003). International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc, 35(8), 1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- Dunne S, Sheffield D, & Chilcot J (2018). Brief report: Self-compassion, physical health and the mediating role of health-promoting behaviours. Journal of Health Psychology, 23(7), 993–999. doi: 10.1177/1359105316643377 [DOI] [PubMed] [Google Scholar]
- El Khoudary SR, Wildman RP, Matthews K, Thurston RC, Bromberger JT, & Sutton-Tyrrell K (2013). Progression rates of carotid intima-media thickness and adventitial diameter during the menopausal transition. Menopause, 20(1), 8–14. doi: 10.1097/gme.0b013e3182611787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari M, Dal Cin M, & Steele M (2017). Self-compassion is associated with optimum self-care behaviour, medical outcomes and psychological well-being in a cross-sectional sample of adults with diabetes. Diabet Med, 34(11), 1546–1553. doi: 10.1111/dme.13451 [DOI] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, & Fredrickson DS (1972). Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem, 18(6), 499–502. [PubMed] [Google Scholar]
- Friis AM, Johnson MH, Cutfield RG, & Consedine NS (2015). Does kindness matter? Self-compassion buffers the negative impact of diabetes-distress on HbA1c. Diabet Med, 32(12), 1634–1640. doi: 10.1111/dme.12774 [DOI] [PubMed] [Google Scholar]
- Friis AM, Johnson MH, Cutfield RG, & Consedine NS (2016). Kindness Matters: A Randomized Controlled Trial of a Mindful Self-Compassion Intervention Improves Depression, Distress, and HbA1c Among Patients With Diabetes. Diabetes Care, 39(11), 1963–1971. doi: 10.2337/dc16-0416 [DOI] [PubMed] [Google Scholar]
- Herder M, Johnsen SH, Arntzen KA, & Mathiesen EB (2012). Risk factors for progression of carotid intima-media thickness and total plaque area: a 13-year follow-up study: the Tromso Study. Stroke, 43(7), 1818–1823. doi: 10.1161/STROKEAHA.111.646596 [DOI] [PubMed] [Google Scholar]
- Herriot H, Wrosch C, & Gouin JP (2018). Self-compassion, chronic age-related stressors, and diurnal cortisol secretion in older adulthood. J Behav Med, 41(6), 850–862. doi: 10.1007/s10865-018-9943-6 [DOI] [PubMed] [Google Scholar]
- Holden CL, Rollins P, & Gonzalez M (2020). Does how you treat yourself affect your health? The relationship between health-promoting behaviors and self-compassion among a community sample. Journal of Health Psychology, 1359105320912448. doi: 10.1177/1359105320912448 [DOI] [PubMed] [Google Scholar]
- Kirby JN (2017). Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychology and Psychotherapy, 90(3), 432–455. doi: 10.1111/papt.12104 [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Xu J, & Arias E (2020). Mortality in the United States, 2019. NCHS Data Brief(395), 1–8. [PubMed] [Google Scholar]
- Krieger T, Berger T, & Holtforth MG (2016). The relationship of self-compassion and depression: Cross-lagged panel analyses in depressed patients after outpatient therapy. Journal of Affective Disorders, 202, 39–45. doi: 10.1016/j.jad.2016.05.032 [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, … Labarthe DR (2018). Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. Journal of the American College of Cardiology, 72(12), 1382–1396. doi: 10.1016/j.jacc.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky LD, & Thurston RC (2007). Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry, 64(12), 1393–1401. doi: 10.1001/archpsyc.64.12.1393 [DOI] [PubMed] [Google Scholar]
- Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, & Fulwiler C (2015). Mindfulness and Cardiovascular Disease Risk: State of the Evidence, Plausible Mechanisms, and Theoretical Framework. Curr Cardiol Rep, 17(12), 112. doi: 10.1007/s11886-015-0668-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X, Qiao L, & Che X (2018). Self-compassion modulates heart rate variability and negative affect to experimentally induced stress. Mindfulness, 9(5), 1522–1528. [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, & Turner RC (1985). Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia, 28(7), 412–419. doi: 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- Matthews KA, Owens JF, Edmundowicz D, Lee L, & Kuller LH (2006). Positive and negative attributes and risk for coronary and aortic calcification in healthy women. Psychosom Med, 68(3), 355–361. doi: 10.1097/01.psy.0000221274.21709.d0 [DOI] [PubMed] [Google Scholar]
- Morrison AE, Zaccardi F, Chatterjee S, Brady E, Doherty Y, Robertson N, … Davies MJ (2019). Self-Compassion, Metabolic Control and Health Status in Individuals with Type 2 Diabetes: A UK Observational Study. Exp Clin Endocrinol Diabetes. doi: 10.1055/a-0897-3772 [DOI] [PubMed] [Google Scholar]
- Neff KD (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–101. doi:doi: 10.1080/15298860390129863 [DOI] [Google Scholar]
- Neff KD (2016). The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7(1), 264–274. [Google Scholar]
- Neff KD, Rude SS, & Kirkpatrick KL (2007). An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality, 41, 908–916. doi:doi: 10.1016/j.jrp.2006.08.002 [DOI] [Google Scholar]
- Penninx BW (2017). Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neuroscience and Biobehavioral Reviews, 74(Pt B), 277–286. doi: 10.1016/j.neubiorev.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Peters SA, den Ruijter HM, Bots ML, & Moons KG (2012). Improvements in risk stratification for the occurrence of cardiovascular disease by imaging subclinical atherosclerosis: a systematic review. Heart, 98(3), 177–184. doi: 10.1136/heartjnl-2011-300747 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Raes F, Pommier E, Neff KD, & Van Gucht D (2011). Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother, 18(3), 250–255. doi: 10.1002/cpp.702 [DOI] [PubMed] [Google Scholar]
- Semenchuk BN, Boreskie KF, Hay JL, Miller C, Duhamel TA, & Strachan SM (2020). Self-compassion and responses to health information in middle-aged and older women: An observational cohort study. Journal of Health Psychology, 1359105320909860. doi: 10.1177/1359105320909860 [DOI] [PubMed] [Google Scholar]
- Shahabi L, Karavolos K, Everson-Rose SA, Lewis TT, Matthews KA, Sutton-Tyrrell K, & Powell LH (2016). Associations of Psychological Well-Being With Carotid Intima Media Thickness in African American and White Middle-Aged Women. Psychosom Med, 78(4), 511–519. doi: 10.1097/PSY.0000000000000293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirois FM, & Hirsch JK (2019). Self-Compassion and Adherence in Five Medical Samples: the Role of Stress. Mindfulness (N Y), 10(1), 46–54. doi: 10.1007/s12671-018-0945-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirois FM, Kitner R, & Hirsch JK (2015). Self-compassion, affect, and health-promoting behaviors. Health Psychology, 34(6), 661–669. doi: 10.1037/hea0000158 [DOI] [PubMed] [Google Scholar]
- Spielberger CD (1983). Manual for the State-Trait Anxiety Inventory (STAI). PaloAlto, CA: Consulting Psychologists Press. [Google Scholar]
- Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, … American Society of Echocardiography Carotid Intima-Media Thickness Task, F. (2008). Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr, 21(2), 93–111; quiz 189-190. doi: 10.1016/j.echo.2007.11.011 [DOI] [PubMed] [Google Scholar]
- Sutton-Tyrrell K, Wolfson SK Jr., Thompson T, & Kelsey SF (1992). Measurement variability in duplex scan assessment of carotid atherosclerosis. Stroke, 23(2), 215–220. [DOI] [PubMed] [Google Scholar]
- Svendsen JL, Osnes B, Binder PE, Dundas I, Visted E, Nordby H, … Sorensen L (2016). Trait Self-Compassion Reflects Emotional Flexibility Through an Association with High Vagally Mediated Heart Rate Variability. Mindfulness (N Y), 7(5), 1103–1113. doi: 10.1007/s12671-016-0549-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurston RC, Chang Y, Barinas-Mitchell E, Jennings JR, Landsittel DP, Santoro N, … Matthews KA (2016). Menopausal hot flashes and carotid intima media thickness among midlife women. Stroke, 47(12), 2910–2915. doi: 10.1161/strokeaha.116.014674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurston RC, Rewak M, & Kubzansky LD (2013). An anxious heart: anxiety and the onset of cardiovascular diseases. Prog Cardiovasc Dis, 55(6), 524–537. doi: 10.1016/j.pcad.2013.03.007 [DOI] [PubMed] [Google Scholar]
- Trompetter HR, de Kleine E, & Bohlmeijer ET (2017). Why Does Positive Mental Health Buffer Against Psychopathology? An Exploratory Study on Self-Compassion as a Resilience Mechanism and Adaptive Emotion Regulation Strategy. Cognit Ther Res, 41(3), 459–468. doi: 10.1007/s10608-016-9774-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura AD, Nefs G, Browne JL, Friis AM, Pouwer F, & Speight J (2019). Is self-compassion related to behavioural, clinical and emotional outcomes in adults with diabetes? Results from the Second Diabetes MILES—Australia (MILES-2) study. Mindfulness, 10(7), 1222–1231. doi: 10.1007/s12671-018-1067-0 [DOI] [Google Scholar]
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, … Stroke Statistics, S. (2020). Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation, 141(9), e139–e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- Wendelhag I, Gustavsson T, Suurkula M, Berglund G, & Wikstrand J (1991). Ultrasound measurement of wall thickness in the carotid artery: fundamental principles and description of a computerized analysing system. Clin Physiol, 11(6), 565–577. doi: 10.1111/j.1475-097x.1991.tb00676.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


