Abstract
Nabothian cysts (NCs) are benign cervical mucous retention cysts, which are usually considered insignificant. A 45 years para 2, presented with lower abdominal heaviness, abnormal uterine bleeding and severe dysmenorrhea for 1 year. On examination, only a part of the anterior cervical lip was visible, and a tense bulging cyst was replacing the posterior lip. The cyst extended supravaginally and filled the posterior fornix. Magnetic resonance imaging suggested a 15 cm × 10 cm huge NC. Laparoscopic hysterectomy was done. There were difficulties in bladder dissection, ureteric identification, and vault delineation. The cyst contained 800 ml of clear fluid with a few milliliters of yellowish mucinous fluid. To our knowledge, NC of this size has not been reported in the literature. NCs are benign lesions, but they have to be differentiated from other cervical cysts - particularly malignant or premalignant lesions. NC can very well be managed laparoscopically, provided the skills of precise dissection are possessed by the surgeon
Keywords: Cervical cysts, hysterectomy, laparoscopy, nabothian cyst
INTRODUCTION
Nabothian cysts (NCs) are benign cervical cysts, which result from blockage of an endocervical gland. It is a mucous retention cyst. They are caused due to a chronic inflammatory process, which occurs due to any minor trauma or due to childbirth. NCs are generally considered clinically insignificant. These cysts rarely exceed 1 cm. Usually, these are asymptomatic; they usually rupture after a certain size. We present a case of huge NC with severe dysmenorrhea, for whom a laparoscopic hysterectomy was performed.
CASE REPORT
A 45-year-old para 2, previous two cesarean sections, with no other medical comorbidity, presented with lower abdominal heaviness, abnormal uterine bleeding (AUB) and severe dysmenorrhea for the past 1 year. On per speculum examination, only a small portion of the anterior lip of the cervix was visible and was looking normal. On per vaginal examination, a bulging tense cystic lesion was palpable in the posterior cervical lip, which was extending supravaginally and filling the posterior fornix. It mimicked the feel of bulging membranes with full cervical dilatation in a term fetus. The extent resembled that of a cervical fibroid, except for the tense cystic consistency. Ultrasonography (USG) suggested a right ovarian cyst; magnetic resonance imaging (MRI) was done to look for any cervical lesion as there was a mismatch between the clinical findings and the USG. MRI showed a huge NC of size 15 cm × 10 cm. Her cancer antigen-125 levels were normal. Cervical cytology was negative for malignancy. Endometrial scraping showed proliferative phase endometrium.
Laparoscopic hysterectomy was done by an experienced endogynecologist. The uterus was bulky and pushed cranially and to the left by a huge cervical cyst of 15 cm × 10 cm, which was tense, glistening, and stretching the surrounding visceral peritoneum [Figure 1].
Figure 1.
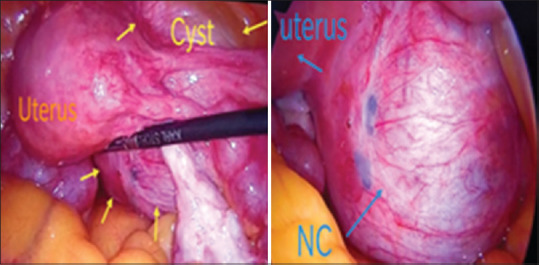
Intraoperative picture of nabothian cyst
Challenging aspects of the surgery
Bladder was drawn up and was densely adherent to the previous Lower Segment Cesarean Section (LSCS)scar. Unlike a cervical fibroid, wherein there is a distinct difference in consistency between the bladder and the cervix, separating the cyst from the bladder was not an easy task, because both the structures had the same consistency and the cyst was yielding to the dissection forces. The cesarean scar adhesion added to the difficulty at this level. Retrograde filling of the bladder was done, to aid the dissection
Identification of the ureteric course was important, as the ureters were pushed laterally and stretched on the lateral surface of the cyst. Prophylactic ureteric stenting was not done, as it would make the ureter nonpliable and more prone to injury
Identification of the vaginal fornix for vault incision was difficult as the cyst was stretching the planes. Hence, at this point, the cyst was decompressed with a laparoscopic needle, without any peritoneal contamination. Around 800 ml of clear serous fluid was aspirated along with a few milliliters of yellowish mucinous fluid. The rent was sutured with 2-0 vicryl.
Hysterectomy was completed uneventfully; the specimen was examined, which showed that except for the distal 1 cm of the anterior cervical lip, the entire cervix was replaced by a huge unilocular cyst. The inner walls of the cyst were smooth, with no septations or solid areas. HPE suggested a benign NC.
DISCUSSION
NC is usually asymptomatic, but with this huge size, it is practical that there was lower abdominal heaviness for our patient associated with an obstructive dysmenorrhea. As with any huge pelvic mass, congestion would have led to the heavy menstrual bleeding. Case reports from across the globe have shown NC with chronic urinary retention,[1] presenting as genitourinary fistula,[2] uterine obstruction,[3] AS chronic pelvic pain,[4] rectal pressure,[5] nulliparous prolapse,[6] obstructed labor,[7] and heavy sudden bleeding episodes.[8] Our case is the first with such a huge size of NC, with abdominal heaviness, AUB, and dysmenorrhea. Our report will be of great aid for surgeons in managing these cases laparoscopically.
It is important to rule out NC from other malignant or premalignant lesions. Ando et al.[9] have studied 94 cases with multicystic appearance of the cervix, and of them, 10.6% had minimal deviation adenocarcinoma (MDA), 62.7% showed lobular endocervical glandular hyperplasia (LEGH), and only 26.5% had benign NC. On MRI, MDA showed a solid or invasive pattern, LEGH showed cosmos pattern (microcystic glands surrounded by medium to large cysts) or microcystic pattern (aggregation of small cysts without peripheral large cysts - which may also be malignant), and NCs showed coarse cystic pattern, with irregular medium to large cysts, without solid or invasion pattern. All of the cases presented with excessive watery discharge. MDA usually has a normal cytology, hence it is better to do a colposcopy in patients with suspicious cervical cysts. It would be wise to go with an MRI to be more precise with our diagnosis. The differentiation is crucial because NC is benign, whereas LEGH, though benign, may be a precursor of MDA. Furthermore, 5%–10% of LEGH cases already had progressed to malignancy in their study.
An increase in the size of the cysts and appearance of malignant cells in the pap smear are early signs of progression from LEGH to MDA. In a poor-resource setting, follow-up with an ultrasound is important. If surgery is planned, the modality ranges from conization, simple hysterectomy, or radical hysterectomy.
The other differential diagnosis includes cystic degeneration of leiomyoma and cervical ectopic and requires management accordingly.
CONCLUSION
NCs can also grow to huge sizes and should always be considered while handling pelvic cysts. MRI is the mainstay of preoperative diagnosis. Laparoscopic management is feasible, provided there is no suspicion of malignancy. Laparoscopic hysterectomy is safe in expert hands. The surgeon should be aware of the possible injury to the ureter and bladder.
Ethical approval
This study was approved by the Research Ethics Committee of GEM Hospital & Research Center (approved number: GEMREC 21012020).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wu Z, Zou B, Zhang X, Peng X. A large nabothian cyst causing chronic urinary retention: A case report. Medicine (Baltimore) 2020;99:e19035. doi: 10.1097/MD.0000000000019035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yelikar K, Deshpande S, Deshmukh S, Pagare S. An unusual presentation of nabothian cyst: A case report. Int J Reprod Contracept Obstet Gynecol. 2015:1589–92. [Google Scholar]
- 3.Harou K, Elfarji A, Bassir A, Boukhanni L, Asmouki H, Soummani A. Multiple nabothian cysts: A cause of cervical obstruction. OALib. 2019;06:1–5. [Google Scholar]
- 4.Kim HK, Park SH, Kim CJ, Kwon JY, Namkung J. Large nabothian cyst with chronic pelvic pain: case report and literature review. Clinical and Experimental Obstetrics & Gynecology. 2020;47:1–3. [Google Scholar]
- 5.Temur I, Ulker K, Sulu B, Karaca M, Aydin A, Gurcu B. A giant cervical nabothian cyst compressing the rectum, differential diagnosis and literature review. Clin Exp Obstet Gynecol. 2011;38:276–9. [PubMed] [Google Scholar]
- 6.Nigam A, Choudhary D, Raghunandan C. Large nabothian cyst: A rare cause of nulliparous prolapse. Case Rep Obstet Gynecol. 2012;2012:192526. doi: 10.1155/2012/192526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vural F, Sanverdi I, Coskun AD, Kusgöz A, Temel O. Large nabothian cyst obstructing labour passage. J Clin Diagn Res. 2015;9:QD06–7. doi: 10.7860/JCDR/2015/15191.6630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen F, Duan H, Zhang Y, Liu Y, Wang X, Guo Y. A giant nabothian cyst with massive abnormal uterine bleeding: A case report. Clin Exp Obstet Gynecol. 2017;44:326–8. [PubMed] [Google Scholar]
- 9.Ando H, Miyamoto T, Kashima H, Takatsu A, Ishii K, Fujinaga Y, et al. Usefulness of a management protocol for patients with cervical multicystic lesions: A retrospective analysis of 94 cases and the significance of GNAS mutation. J Obstet Gynaecol Res. 2016;42:1588–98. doi: 10.1111/jog.13083. [DOI] [PMC free article] [PubMed] [Google Scholar]


