Sir,
Patients with COVID-19 infection, especially those with severe disease and those who have been treated with immunosuppressants, are prone to a number of rare and exotic infections. Histoplasmosis is a mycotic infection rarely described from the Indian subcontinent. Here, we describe a patient with acute localized pulmonary histoplasmosis, secondary to severe COVID infection with respiratory failure.
A 65-year-old female, known case of nonalcoholic steatohepatitis-associated stable chronic liver disease, developed severe COVID-19 infection with respiratory failure in April 2021. She required hospitalization and was treated with oxygen and intravenous methylprednisolone (40 mg twice daily), which was tapered over the next 7 days and eventually tapered in the oral form over the next 2 weeks. The patient was discharged from the hospital on supplemental oxygen, after 2 weeks of hospitalization. Two weeks postdischarge, the patient developed fever with cough. The fever was gradually progressive and at the end of 1 week was peaking at 102°F, with 2–3 peaks daily. There was associated mild cough. Apart from the occasional cough, no other discernable localizing signs were present with the fever. For evaluation of the fever, she was readmitted to the hospital. On hospitalization, repeat high-resolution computed tomography (HRCT) chest was done which showed variable post-COVID changes in the both the lungs along with a soft-tissue density (3.2 cm × 3 cm) in the lingular segment of the left lung. The patient was unable to bring out any sputum for evaluation, and in view of the frail status of the patient and peripheral location of the lesion, bronchoscopy was deferred. In view of the solitary mass like lesion on HRCT chest, suspicion of neoplastic etiology was raised and a whole-body positron emission tomography (PET) CT was done which revealed a highly metabolically active soft tissue density in the left lingular segment of the lung. No other metabolically active lesion was reported in the PET CT [Figure 1]. In view of the PET CT findings, CT-guided biopsy was done from the PET avid lesion. Histopathological examination of the lesion revealed diffuse sheets of histiocytes with numerous budding yeasts and epitheloid granulomas with lymphoplasmacytic infiltrates. Findings were suggestive of pulmonary histoplasmosis.
Figure 1.
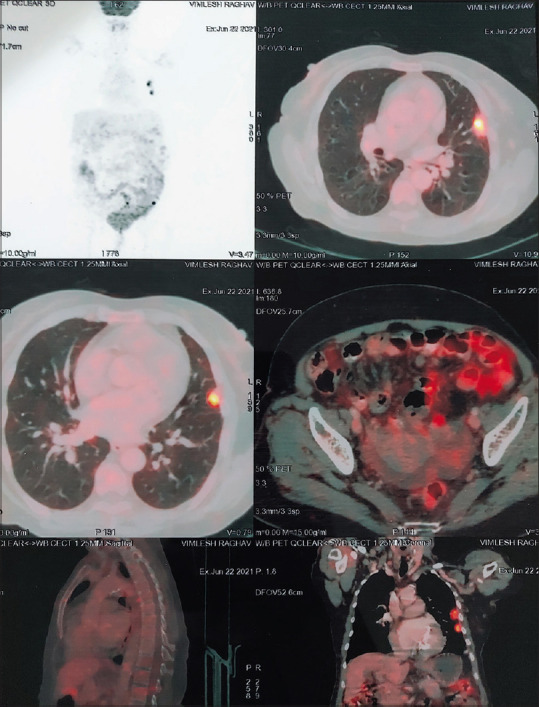
PET - CT Whole body, demonstrating a single PET avid nodular lesion in the left lingula.
In view of the histopathology findings, she was started on oral itraconazole, loading dose of 200 mg twice a day for 3 days followed by 200 mg once a day for 3 weeks. Therapy was stopped after 3 weeks as there was complete clinical and radiological resolution. Repeat HRCT chest, done after a month, revealed that the solitary mass like lesion had resolved completely. The patient is under follow-up and is currently doing well.
A number of fungal infections have been reported in patients who had severe COVID-19 infection and especially those who have been treated with high dose of steroids and other potent immunosuppressants. Most commonly reported fungal infections in these patients include Mucor and Aspergillus. Histoplasmosis is commonly reported in the Mid-Western USA but is hardly encountered in the Indian subcontinent. The pulmonary manifestations of histoplasmosis range from pneumonia, hilar/mediastinal lymphadenopathy/mass, cavitatory lung disease, and superior vena cava/other mediastinal organ obstruction.[1] Most common differential diagnosis includes tuberculosis, malignancy, and sarcoidosis.
Acute diffuse pulmonary syndrome is seen in patients with exposure to a high inoculum of conidia, especially in patients who have severe immunodeficiency (e.g., AIDS).[2] Acute localized pulmonary disease is less commonly reported, and the fungal burden is generally lower in these patients.[1] Our patient also presented with a localized pulmonary lesion. The yield of antigen detection for Histoplasma in the urine and serum is usually very poor in these patients. Serological test is fare better in these patients.[3] However, none of these tests, either antigen detection or serology, are available easily in India. To establish the diagnosis in our patient, we had to resort to lung biopsy, which clinched the diagnosis.
Most commonly used antifungal agents in the treatment of histoplasmosis include itraconazole, fluconazole, and amphotericin B. Amphotericin B is used in patients with severe lung disease. In most patients who do not require hospitalization, itraconazole is mainly the drug of choice.[4] Many patients, especially those with underlying immunosuppression, may require prolonged periods of treatment.
Histoplasma is another bug which has come out of the COVID’s Pandora box. Physicians treating post-COVID cases, who have persistent fever/radiological lesions which are not resolving, should be evaluated for common and rare mycosis, including histoplasmosis, as is highlighted by this case report.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wheat LJ, Conces D, Allen SD, Blue-Hnidy D, Loyd J. Pulmonary histoplasmosis syndromes: Recognition, diagnosis, and management. Semin Respir Crit Care Med. 2004;25:129–44. doi: 10.1055/s-2004-824898. [DOI] [PubMed] [Google Scholar]
- 2.Chu JH, Feudtner C, Heydon K, Walsh TJ, Zaoutis TE. Hospitalizations for endemic mycoses: A population-based national study. Clin Infect Dis. 2006;42:822–5. doi: 10.1086/500405. [DOI] [PubMed] [Google Scholar]
- 3.Hage CA, Ribes JA, Wengenack NL, Baddour LM, Assi M, McKinsey DS, et al. Amulticenter evaluation of tests for diagnosis of histoplasmosis. Clin Infect Dis. 2011;53:448–54. doi: 10.1093/cid/cir435. [DOI] [PubMed] [Google Scholar]
- 4.Freifeld AG, Iwen PC, Lesiak BL, Gilroy RK, Stevens RB, Kalil AC. Histoplasmosis in solid organ transplant recipients at a large Midwestern University Transplant Center. Transpl Infect Dis. 2005;7:109–15. doi: 10.1111/j.1467-8365.2005.00105.x. [DOI] [PubMed] [Google Scholar]


