Abstract
Objective:
To compare the treatment outcomes of rapid maxillary expansion (RME) plus face mask (FM) and LeFort 1 osteotomy + FM during maxillary protraction.
Materials and Methods:
This study was carried on 34 patients all having maxillary retrognathic, anterior cross-bite, Class III skeletal and dental malocclusion characteristics and a concave profile. Eighteen patients with milder maxillary retrognathism were treated with RME + FM. Sixteen other patients with moderate to severe maxillary retrognathism were treated with an incomplete LeFort 1 osteotomy + FM therapy. Cephalometric data were evaluated statistically.
Results:
Significantly higher values of maxillary advancement and reduced treatment time were achieved with surgically assisted FM therapy.
Conclusions:
The surgically assisted FM treatment was more rapid and effective in maxillary protraction compared to the RME + FM treatment.
Keywords: Maxillary protraction, Face mask, Surgery
INTRODUCTION
Treatment of Class III malocclusion is still demanding in orthodontics. However, etiological studies have shown that 40% to 60% of Class III skeletal malocclusions are due to maxillary deficiency or retrusion, which is possible to treat if the patient is still growing and cooperative.1–4 Face mask (FM) therapy has been proposed and is the most frequently used treatment protocol for this anomaly.
Animal and human studies5–11 show that it is possible to advance a maxilla in a growing subject over a certain period of time. Clinical studies show that rapid palatal expansion has often been performed as part of the treatment protocol. This approach proposes to stimulate sutural activity of the neighboring sutures of the maxilla and increase the amount of advancement. Treatment results with a FM actually comprise a combination of forward movement of the maxilla, clockwise rotation of mandible, and forward movement of the upper incisors with retrusion of the lower incisors.12,13
The main target of treatment is forward movement of the maxilla, but the values reported in the literature11–14 are not more than 2 mm in 6 to 12 months of treatment time. On the other hand, it is not possible to achieve any advancement following growth completion, and it is also very difficult to mobilize the maxilla via FM therapy in cleft cases as a result of scarring from previous surgeries. In such situations we can either use distraction or wait for the completion of growth and then perform surgery.
Distraction is a biologic process of new bone formation between the surfaces of bone segments that are gradually separated by incremental traction.15 Animal and human studies16–18 have shown that it is possible to elongate the membranous bone of the maxilla using a distraction protocol. There are many sophisticated distractors on the market, but with the exception of the FM, they are all expensive.
Rachmiel and others19–25 reported that the values related to the treatment effects of surgically assisted protraction of the maxilla using a FM range from 3 to 12 mm in the very short term, compared to conventional FM therapy. In this study we aimed to compare the treatment results of surgically assisted protraction of the maxilla with FM therapy and the results of RME-assisted FM therapy.
MATERIALS AND METHODS
The study was conducted with 34 patients (15 males, 19 females), all of whom had maxillary retrognathic, anterior cross-bite, Class III skeletal and dental malocclusion characteristics and concave profiles. Eighteen patients (10 males, 8 females; mean age 12.9 ± 1.1 years; Table 1) with comparatively mild maxillary retrognathism (FH-NA: 86.75 ± 3.21, Nper-A: −3.83 ± 2.97; Table 2) were treated with rapid maxillary expansion (RME) + FM.
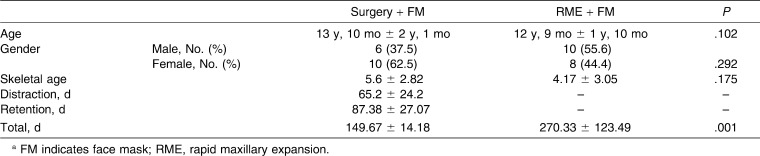
Table 1.
Mean Ages in Groupsa
Table 2.
Dental and Skeletal Changes in Sagittal Direction. Mean and Standard Deviation (SD) Values Before and After Treatment in Each Groupa
The other 16 patients (10 females, 6 males; mean age 13.1 ± 2.1 years; Table 1) with moderate to severe maxillary retrognathism (FH-NA: 83.25 ± 6, Nper-A: −6.84 ± 5.2; Table 2) were treated with surgery + FM. In this latter group, four of the patients had cleft lip and palate, and all had undergone lip and palate repair in infancy or early childhood.
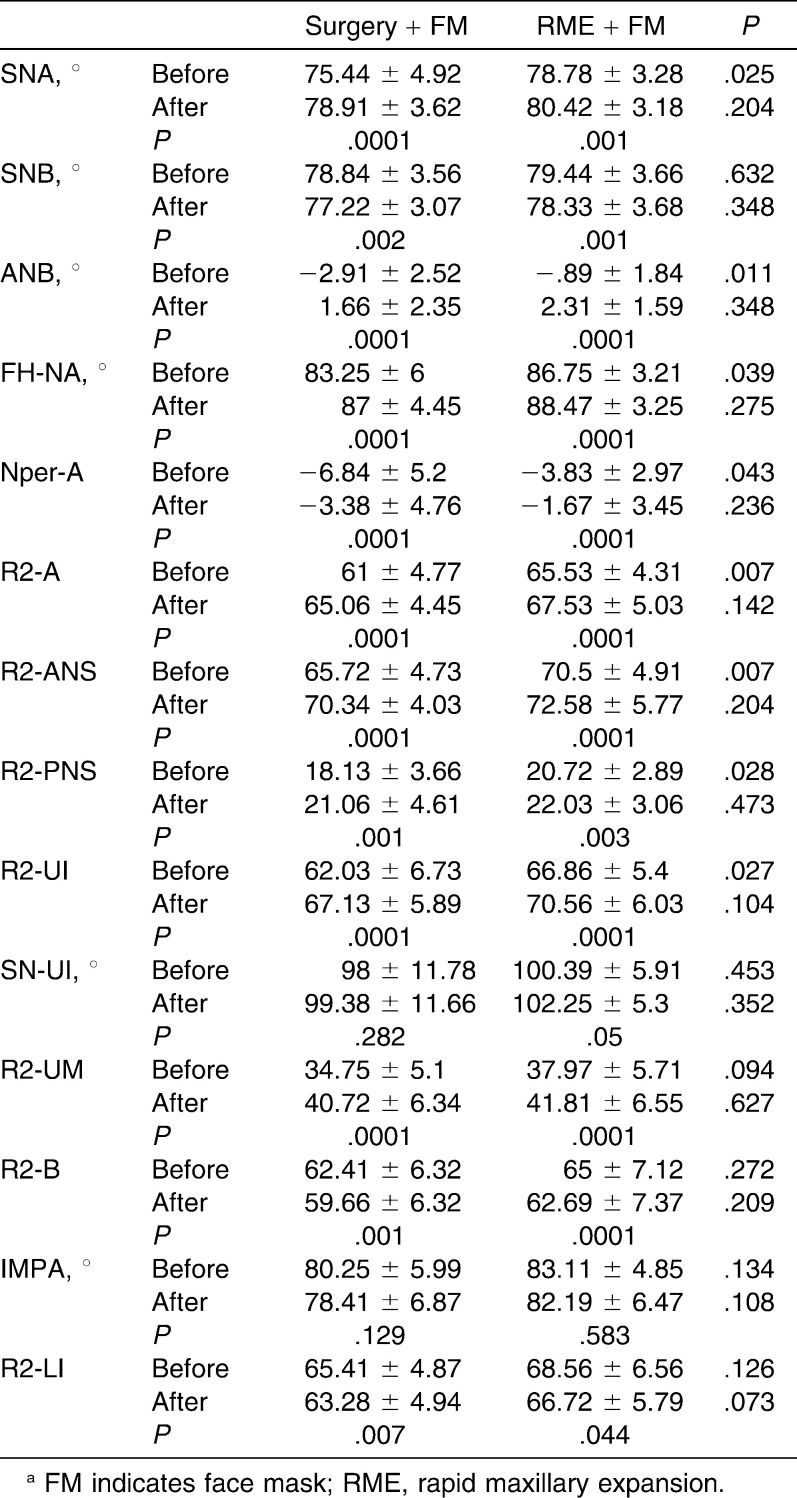
Treatment Protocol in RME-Assisted FM Group
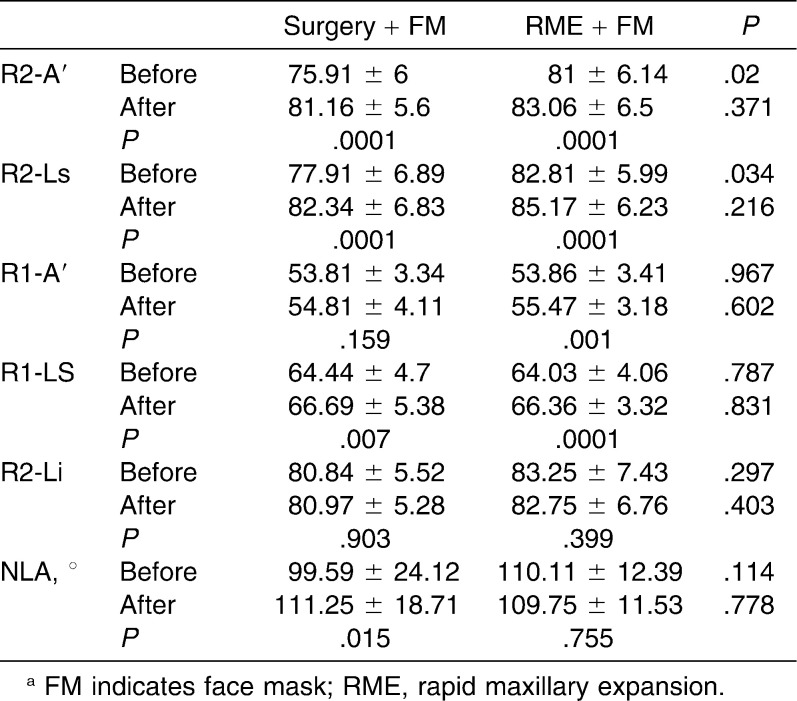
In the RME + FM group all patients underwent RME with acrylic-covered hyrax appliance, regardless of whether or not they exhibited posterior cross-bite (Figure 1). The expander was specially designed to have hooks in the canine area for the attachments of the elastics. There was also a lingual wire (0.9 mm) welded to the anterior arms of the hyrax to support the upper incisors during protraction. A FM was applied with 1000 g of total force following the occurrence of a median diastema. In order to decrease the counterclockwise rotation of the upper occlusal plane, elastics were oriented with a 30° angle to the occlusal plane. Patients wore the FM nearly 16 hours a day until a Class II relationship was achieved.
Figure 1.
Intraoral appliance design in the rapid maxillary expansion (RME)–assisted group.
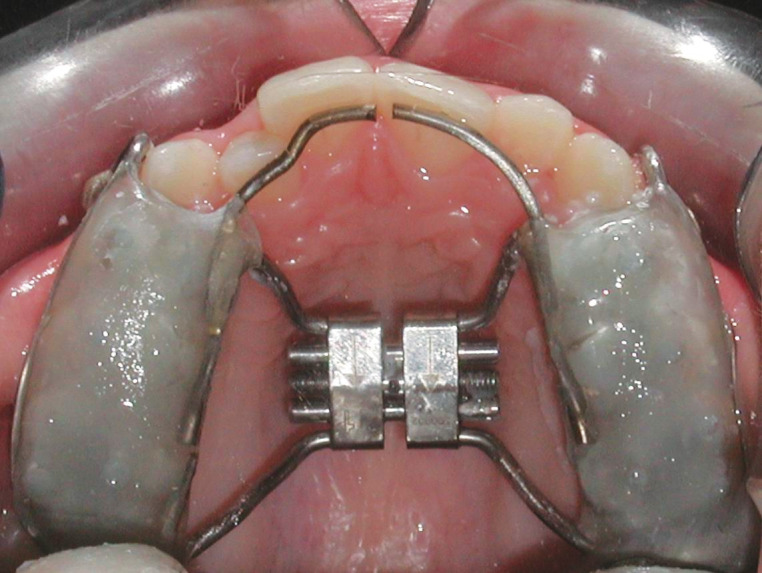
Treatment Protocol in Surgery-Assisted FM Group
A continuous 1.1-mm SS wire framework was bent, starting from the buccal side of the upper canines and touching the buccal and palatal surfaces of the posterior teeth and lingual surfaces of the anterior teeth. The wire was sandblasted and covered with acrylic on the posterior segments. RME was not performed for any of the patients in this group (Figure 2a,b). The same plastic surgeon performed an incomplete LeFort 1 osteotomy for each patient. The osteotomy involved the lateral walls of the maxilla, starting from the apertura piriformis and extending to the tuberosity, without separation of the pterygomaxillary suture (Figure 2c). The FM was applied on the fifth to seventh day postsurgery, with a total force value ranging from 1700 g to 2000 g. The elastics were oriented with a 30° angle to the occlusal plane, as in the previous study group (Figure 2d). Patients wore the FM 24 hours a day (except during meals) until a Class II dental relationship was achieved; then patients switched to nighttime wear for 3 months for retention purposes. The treatment progress of one patient from this group is shown in Figure 3.
Figure 2.
(a, b) Intraoral appliance design in the surgery group. (c) LeFort I osteotomy performed in the surgery group. (d) Face mask (FM) application after osteotomy.
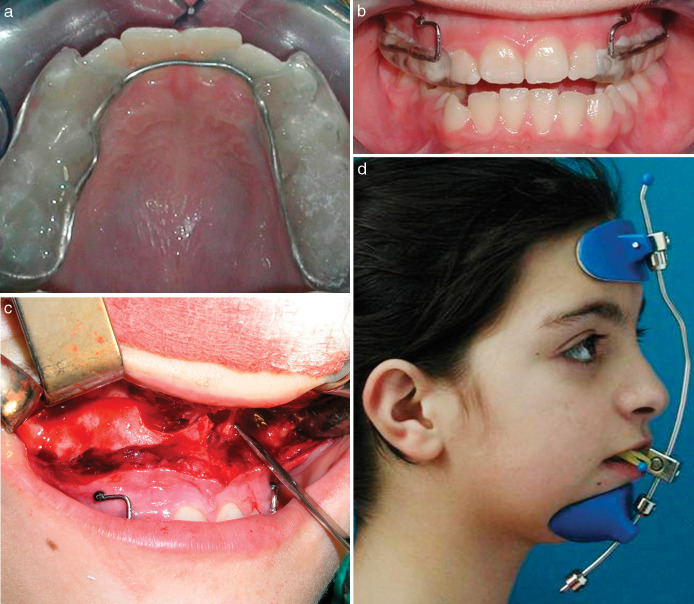
Figure 3.
(a–d) Progress of a case from surgery-assisted face mask (FM) group. (e) Superimposition of pretreatment and posttreatment cephalometric films of the patient following debonding of the intraoral device.
In both groups maxillary splints were debonded following retention periods. Lateral cephalometric films were taken before treatment and immediately after debonding of the maxillary devices. Treatment continued with a multibracket system in both groups.
Cephalometric Method
Horizontal reference plane (R1) was drawn with a 7° angle below the SN plane at point S, and a perpendicular line was drown through the S point to this horizontal reference plane (R2). Perpendicular lines were drawn to these reference planes from various anatomical points to determine vertical and sagittal changes. Twenty-one linear and 11 angular parameters were traced and measured on the lateral cephalograms. Statistical analysis was conducted using the Graph Pad Prisma V.3 package program, and the data were evaluated by Student's t-test.
RESULTS
Table 2 shows that the Class III occlusion and maxillary retrognathism were more severe in the surgery-assisted group. In the surgery group the duration of distraction was 65.2 ± 24.2 days, and retention was 87.38 ± 27.07 days. The total treatment time for this group was 149.67 ± 14.18 days (5 months). On the other hand, the total treatment time for the RME group was 270.33 ± 123.49 days (9 months). The difference between total treatment times for the two groups was statistically significantly different (Table 1).
The anterior cross-bites were eliminated in all patients, changing their profiles from a concave to a straight or almost convex profile. Tables 2–4 show the mean values before and after the skeletal, dental, and soft tissue changes in both groups and the statistical significance of the treatment outcomes. On the other hand, Table 5 shows the differences resulting from treatment and offers a statistical comparison of the two groups.
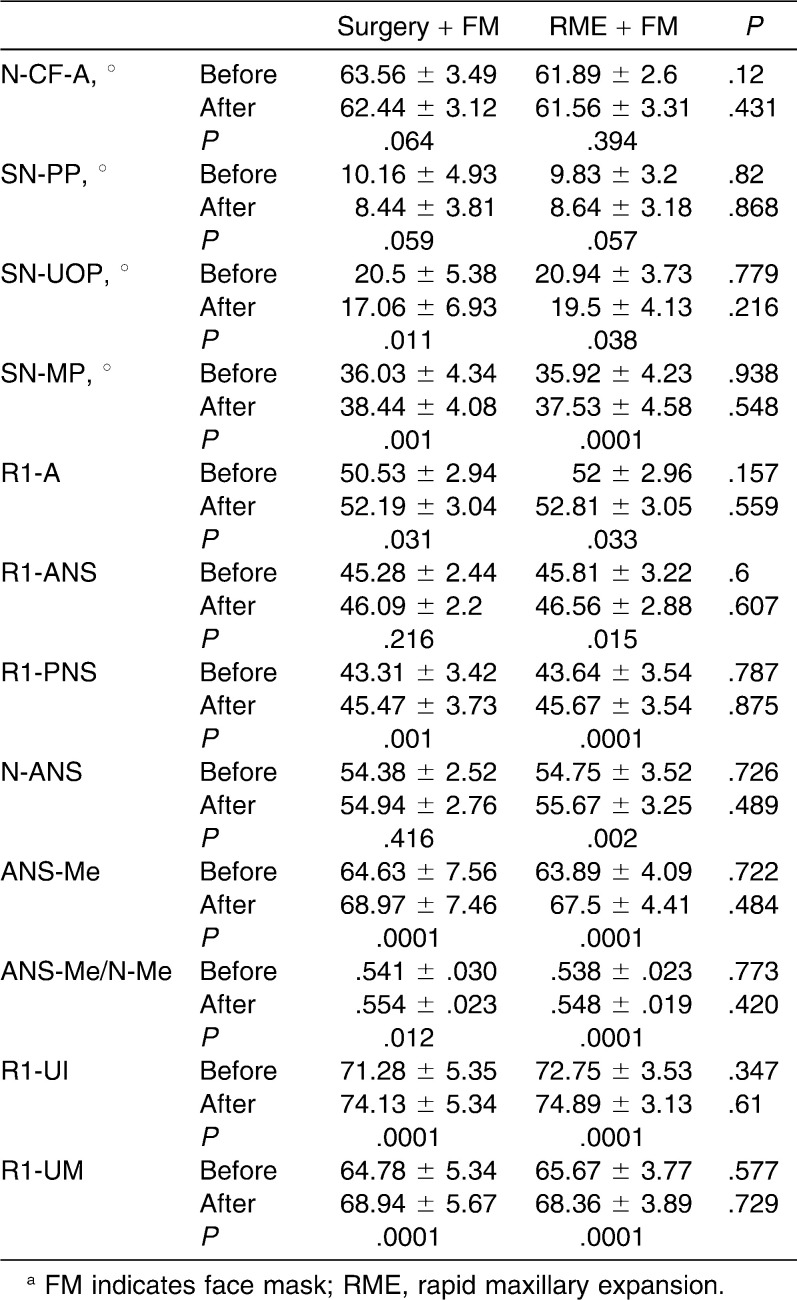
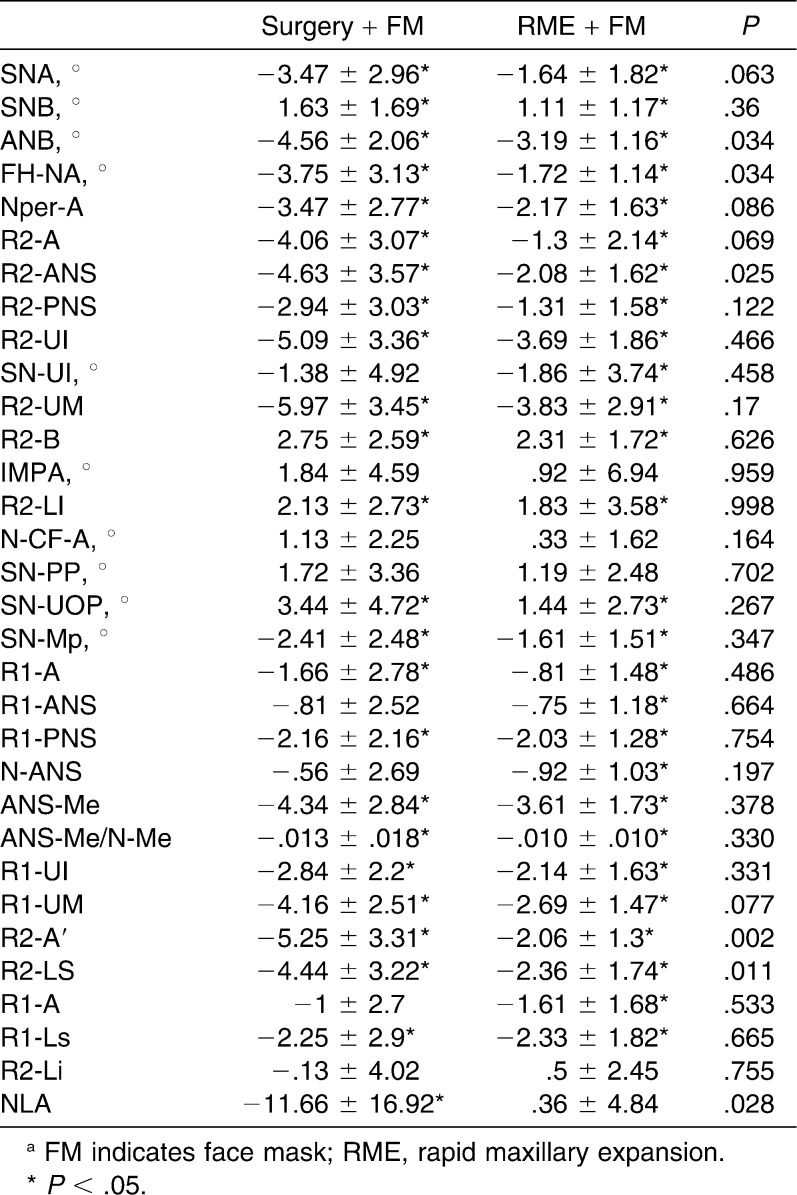
Table 3.
Dental and Skeletal Changes in Vertical Direction. Mean and Standard Deviation (SD) Values Before and After Treatment in Each Groupa
Table 4.
Soft Tissue Changes. Mean and Standard Deviation (SD) Values Before and After Treatment in Each Groupa
Table 5.
Mean and Standard Deviation (SD) Values of Differences for Each Group and the Comparison of Treatment Groupsa
SNA and ANB angles increased and SNB angle decreased significantly (P < .05; Table 2) in both groups, and the sagittal maxillo-mandibular relationships were normalized.
Increasing values of maxillary depth angle (P < .001) and Nper-A, R2-ANS, R2-PNS, and R2-A parameters also demonstrated significant maxillary advancement in both groups (Table 2). However, there was a significant difference between treatment groups in terms of maxillary advancement, demonstrated by higher values of ANB, maximum depth angles, and R2-ANS parameters in the surgery group (P < .03; Table 5) However, the other sagittal parameters measured did not present any significant differences between the treatment groups.
The increase in the values of linear parameters (R2-UI, R2-UM) showed that the upper incisors and upper molars also moved forward a similar amount, showing that dental arches followed the advancement of the maxilla. SN-UI values showed that upper incisors proclined forward significantly (1.86°; P < .05; Table 2) in the RME group, while in the surgery group the proclination of the incisors was 1.38°, which was not significant (SN-UI: P > .05; Table 2). However, a comparison of the treatment groups revealed no statistically significant differences between groups (Table 5).
Soft tissue results revealed that the upper lip and upper lip sulcus moved significantly forward in both groups during treatment. However, the values were significantly higher in the surgery group (P < .05; Table 5). The nasolabial angle also increased dramatically in the surgery group (NLA: 11.66 ± 16.92; Table 5), while this parameter was not significantly changed in the RME + FM group.
DISCUSSION
Maxillary retrognathism is usually present with midface retrusion, so the most favorable approach is to advance the maxilla, either with a FM or with surgery, depending on the patient's age. However, surgery cannot be performed before growth is completed, which means that young adolescents must live with their Class III profiles as well as the potential psychological problems and lack of self esteem that sometimes occur in these adolescents. On the other hand, the cost of orthognathic surgery is high, and some patients need grafting after down-fracture, which means an extra donor site surgery. Considering that the FM has to be applied at an early age and for an extended duration, this treatment option can be discouraging for some patients. The literature11–14 reports that the FM achieves approximately 1.5 mm to 2 mm of maxillary advancement with 6 months to 12 months of FM wear, but this treatment protocol requires patient compliance and is not indicated in adult patients, in whom growth is complete.
On the other hand, surgery-assisted maxillary protraction is effective at any age, and the improvement is achieved in a relatively short period of time, which motivates patients. In the literature this procedure is termed distraction, which is defined as a biologic process of new bone formation between surfaces of bone segments that are gradually separated by incremental traction. It has been reported25 that the advantage of this method is not only its rapidity but also the soft tissue lengthening that occurs during new bone formation, which causes significant changes with less risk of relapse. Distraction osteogenesis has become an important technique in the treatment of maxillary and midfacial hypoplasia. Both external and internal devices have been successfully used for this purpose.
Although application of the rigid external distraction device is technically easy to perform, patient discomfort makes this treatment choice unpleasant. Intraoral distraction devices allow three-dimensional control and a quantifiable amount of movement of the bone segments during maxillary advancement.26 Roser et al.27 reported 7.5 mm of advancement, achieved within a 3-month period with a rigid external distractor (RED). However, it is more difficult to place an intraoral distraction device parallel to the distraction vector of the maxilla, and removal requires a second surgical intervention.
In 2008 Kırçelli and Pektaş28 reported a 4.8-mm movement of the A point in 10.8 months using skeletal anchorage in conjunction with FM therapy in the late mixed dentition period. In 1998 Polley and Figueroa29 performed maxillary protraction using a FM following LeFort 1 osteotomy on four patients and achieved 5.2 mm of maxillary advancement in 3 months. Researchers performed a distraction procedure for the rest of the patients in the same group (14 patients) and reported 11.7 mm in advancement in the same time period using RED. With regard to the results obtained with RED and similar rigid appliances, it is possible to obtain more significant maxillary advancement, but these appliances are expensive and more complicated to apply. There are additional studies based on surgery-assisted FM therapy, and in most of them the appliances are applied to cleft lip and palate patients. Molina et al.25 reported 43 cases, all of which involved treatment with this method; these patients were corrected from a Class III skeletal relationship to a Class I relationship, and the maxilla was advanced 5 to 9 mm. Moline et al. reported that there was new bone formation at the pterygomaxillary suture and that pretreatment apnea was decreased.
We believe that 5 to 9 mm of maxillary advancement is enough for the correction of many Class III cases. This approach could be an effective and rapid solution and also an alternative to some surgery treatments, which led us to design this study and to compare this technique with the conventional RME + FM therapy. We found 4 mm of maxillary advancement with the surgically assisted approach in 5 months, compared to 1.3 mm with RME + FM therapy in 9 months, which supports the findings of Molina et al. Therefore, our findings show that maxillary protraction is significantly more rapid and that the amount of improvement was significantly larger compared to treatment with RME-assisted FM. The skeletal Class III relationship was changed to a Class I relationship in both groups, but considering that the surgical group had more severe pretreatment discrepancies, the results were more dramatic in this group. The amount of movement of the ANS point was 4.63 mm for the surgery group and 2.08 mm for the RME group, and these values were significantly different (Table 5). The upper lip and lip sulcus also moved forward more dramatically and significantly in the surgical group compared to the RME group. Hence, forward movement of the upper lip sulcus and nasolabial angle presented large increases (11°) in the surgical group, which shows that the nose tip was elevated in a fashion similar to that associated with maxillary advancement surgery.
The upper incisors moved forward significantly in the surgery group, while there was no significant change in the RME group. This may be explained by the more rapid movement (5 months) in the surgery group, while the mesial force vector on the upper incisors lasted for a longer time (9 months) in the RME group. However, this difference was not statistically significant, which is probably due to the small sample size. Surgically assisted maxillary protraction seems more rapid and effective compared to the conventional method, but considering long-term mandibular growth, selection of the patients should be done carefully to avoid relapse. The LeFort 1 osteotomy will be safer if it is accomplished after full eruption of the permanent teeth, which means we should wait until the patient is 12 or 13 years of age. It may be safer to exclude the hereditary factor by diagnosing patients carefully and waiting longer in suspicious cases to be certain that growth has been completed. We support using the RME-assisted approach in growing patients, preferably those who are less than 10 years of age.
CONCLUSIONS
Significant skeletal and soft tissue changes were obtained by both RME and surgically assisted FM therapy.
Surgery-assisted treatment was more rapid and effective compared to the RME + FM approach.
REFERENCES
- 1.Jacobson A, Evans W. G, Preston L. B, Sadowsky P. W. Mandibular prognathism. Am J Orthod. 1974;66:140–171. doi: 10.1016/0002-9416(74)90233-4. [DOI] [PubMed] [Google Scholar]
- 2.Kapust A. J, Sinclair M, Turley P. Cephalometric effects of face mask/expansion therapy in Class III children. A comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212. doi: 10.1016/s0889-5406(98)70141-6. [DOI] [PubMed] [Google Scholar]
- 3.Sue G, Chanoca S. J, Turley P. K, Itoh J. Indicators of skeletal Class III growth. J Dent Res. 1987;66:343. [Google Scholar]
- 4.Dietrich U. C. Morphological variability of skeletal Class III relationships as revealed by cephalometric analysis. Rep Congr Eur Orthod Soc. 1970:131–143. [PubMed] [Google Scholar]
- 5.Nanda R. Protraction of maxilla in rhesus monkeys by controlled extraoral forces. Am J Orthod. 1978;74:121–141. doi: 10.1016/0002-9416(78)90080-5. [DOI] [PubMed] [Google Scholar]
- 6.Jackson G. W, Kokich V. G, Shapiro P. A. Experimental and post experimental response to anteriorly directed extraoral force in young Macaca nemestrina. Am J Orthod. 1979;75:318–333. doi: 10.1016/0002-9416(79)90278-1. [DOI] [PubMed] [Google Scholar]
- 7.Smalley W. M, Shapiro P. A, Hohl T. H, Kokich V. G, Bränemark P. I. Osseo integrated titanium implants for maxillofacial protraction in monkeys. Am J Orthod Dentofacial Orthop. 1988;94:285–295. doi: 10.1016/0889-5406(88)90053-4. [DOI] [PubMed] [Google Scholar]
- 8.McNamara J. A., Jr An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21:598–608. [PubMed] [Google Scholar]
- 9.Turley P. K. Early management of the developing Class III malocclusion. Aust Orthod J. 1993;13:19–22. [PubMed] [Google Scholar]
- 10.Mermigos J, Full C. A, Andreasen G. Protraction of the maxillofacial complex. Am J Orthod Dentofacial Orthop. 1990;98:47–55. doi: 10.1016/0889-5406(90)70031-7. [DOI] [PubMed] [Google Scholar]
- 11.Baik H. S. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 12.Filho O. G. S, Magro A. C, Filho L. C. Early treatment of the Class III malocclusion with rapid maxillary expansion and maxillary protraction. Am J Orthod Dentofacial Orthop. 1998;113:196–203. doi: 10.1016/s0889-5406(98)70292-6. [DOI] [PubMed] [Google Scholar]
- 13.Bacetti T, McGill J. S, Franchi L, McNamara J. A, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 14.Alcan T, Keles A, Erverdi N. The effect of a modified protraction headgear on maxilla. Am J Orthod Dentofacial Orthop. 2000;117:27–38. doi: 10.1016/s0889-5406(00)70245-9. [DOI] [PubMed] [Google Scholar]
- 15.Swennen G, Schliephake H, Dempf R, Schierle H, Malevez C. Craniofacial distraction osteogenesis: a review of the literature. Part 1: clinical studies. Int J Oral Maxillofac Surg. 2001;30:89–103. doi: 10.1054/ijom.2000.0033. [DOI] [PubMed] [Google Scholar]
- 16.Hierl T, Klöpper R, Hemprich A. Midfacial distraction osteogenesis without major osteotomies: a report on the first clinical application. Plast Reconstr Surg. 2001;108:1667–1672. doi: 10.1097/00006534-200111000-00035. [DOI] [PubMed] [Google Scholar]
- 17.Cohen S. R, Burstein F. D, Stewart M. B, Rathburn M. A. Maxillary-midface distraction in children with cleft lip and palate: a preliminary report. Plast Reconstr Surg. 1997;99:1421–1428. doi: 10.1097/00006534-199704001-00036. [DOI] [PubMed] [Google Scholar]
- 18.Altuna G, Walker D. A, Freeman E. Surgically assisted rapid orthodontic lengthening of the maxilla in primates—a pilot study. Am J Orthod Dentofacial Orthop. 1995;107:531–536. doi: 10.1016/s0889-5406(95)70120-6. [DOI] [PubMed] [Google Scholar]
- 19.Rachmiel A, Potparic Z, Jackson I. T, Sugihara T, Clayman L, Topf J. S, Forté R. A. Midface advancement by gradual distraction. Br J Plast Surg. 1993;46:201–207. doi: 10.1016/0007-1226(93)90169-c. [DOI] [PubMed] [Google Scholar]
- 20.Rachmiel A, Jackson I. T, Potparic Z, Laufer D. Midface advancement in sheep by gradual distraction: a 1-year follow-up study. J Oral Maxillofac Surg. 1995;53:525–529. doi: 10.1016/0278-2391(95)90064-0. [DOI] [PubMed] [Google Scholar]
- 21.Rachmiel A, Levy M, Laufer D, Clayman L, Jackson I. T. Multiple segmental gradual distraction of facial skeleton: an experimental study. Ann Plast Surg. 1996;36:52–59. doi: 10.1097/00000637-199601000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Rachmiel A, Lewinson D, Eizenbud D, Rosen D, Laufer D. Distraction osteogenesis for hypoplastic facial bones. Harefuah. 1997;132:833–836. [PubMed] [Google Scholar]
- 23.Rachmiel A, Aizenbud D, Ardekian L, Peled M, Laufer D. Surgically-assisted orthopedic protraction of the maxilla in cleft lip and palate patients. Int J Oral Maxillofac Surg. 1999;28:9–14. [PubMed] [Google Scholar]
- 24.Rachmiel A, Aizenbud D, Peled M. Application of Ilizarov method in maxillofacial treatment. Harefuah. 2003;142:359–363. [PubMed] [Google Scholar]
- 25.Molina F, Ortiz Monasterio F, de la Paz Aguilar M, Barrera J. Maxillary distraction: aesthetic and functional benefits in cleft lip-palate and prognathic patients during mixed dentition. Plast Reconstr Surg. 1998;101:951–963. doi: 10.1097/00006534-199804040-00010. [DOI] [PubMed] [Google Scholar]
- 26.Polley J. W, Figueroa A. A. Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg. 1997;8:181. doi: 10.1097/00001665-199705000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Roser M, Cornelius C. P, Bacher M, Reinert S, Krimmel M. Callus distraction of the maxilla. Supplement or alternative to advancement osteotomy. Mund Kiefer Gesichtschir. 2000;4:438–441. doi: 10.1007/PL00014569. [DOI] [PubMed] [Google Scholar]
- 28.Kırçelli B. H, Pektaş ZÖ. Midfacial protractions with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 29.Polley J. W, Figueroa A. A. Rigid external distraction: its application in cleft maxillary deformities. Plast Reconstr Surg. 1998;102:1360–1372. [PubMed] [Google Scholar]