Abstract
Objective:
To assess the efficacy of chincup therapy for mandibular growth retardation in early orthopedic treatment of Class III malocclusion.
Materials and Methods:
An electronic search for articles reporting randomized clinical trials, controlled clinical trials, and cohort studies testing the efficacy of chincup appliance for Class III malocclusion published up to the present was done through four databases: Cochrane Central Register of Controlled Trials (CENTRAL; to March 2010), MEDLINE (1950–March 2010), EMBASE (1980–March 2010), and CBM (1978–March 2010). Study quality assessment and data extraction were done by two reviewers independently. Meta-analysis was done with the assistance of Revman 5.01.
Results:
The search resulted in 50 articles. After selection following the established criteria, four cohort studies qualified for the final review analysis. The results showed that chincup therapy decreased SNB angle and increased ANB angle; the total pooled weighted mean difference values (95% confidence interval) were −1.18 (−1.69, −0.67; P < .00001) and 1.90 (0.60, 3.21; P = .004), respectively. Two studies showed a increase in Gonial angle (P < .05) but no significant change in the mandibular length (Cd-Gn; P = .059 and .39, respectively). One study indicated that chincup therapy exerted no effect on mandibular growth retardation, and mandibular growth continued after the treatment in a downward direction.
Conclusion:
There are insufficient data in these studies to make clear recommendations regarding the efficacy of chincup therapy in the retardation of mandibular growth.
Keywords: Systematic review, Class III malocclusion, Chincup therapy
INTRODUCTION
Skeletal Class III malocclusion can be present with maxillary retrusion, mandibular protrusion, or some combination of the two.1 The incidence of Angle Class III malocclusion in white populations has been reported below 5%.2–5 It is, however, a more common clinical problem in orthodontic patients of Asian or Mongoloid descent.5–9 Studies on the prevalence of Class III malocclusion in Asian patients have shown that a normal mandible with deficient maxilla occurred in 18% and an excessive mandible with normal maxilla occurred in 52%, concluding that overgrowth of the mandible is the main cause of Class III malocclusion.10–15 A major treatment strategy of skeletal Class III malocclusion with mandibular overgrowth in growing patients is retardation or redirection of mandibular growth and posterior positioning of the mandible.
The chincup has been used since the 19th century to control mandibular growth in patients with excessive and/or anteriorly positioned mandibles.16 Over the years, many studies have been conducted to investigate the effects of chincup force on dentofacial growth, but their results have varied a lot. Some studies indicated that the chincup had no effect on retarding mandibular growth but only produced a backward rotation of the mandible.5,17 Deguchi et al.18 reported that short-term chincup treatment showed a significant backward rotation of the mandible, while long-term application of the chincup force significantly inhibited growth of the ramus height and body length of the mandible and showed a significant closing of the gonial angle. Some investigators also reported that changes in the horizontal maxillary and mandibular relationship obtained with chincup therapy remained stable after fixed orthodontic treatment.10,15,18,19
Many studies have, however, reported a tendency of a return to the original skeletal morphology and growth pattern after chincup therapy was discontinued and uncertainties existed in the efficacy of chincup therapy in Class III malocclusion.4,11,13,15,20–24
The aim of this review is to analyze the efficacy of chincup treatment on the retardation of mandibular growth (measured by the SNB and ANB angles) in Class III malocclusion compared with an untreated control group, as derived from the existing literature according to the Cochrane systematic review principles.
MATERIALS AND METHODS
Search Strategy and Study Collection
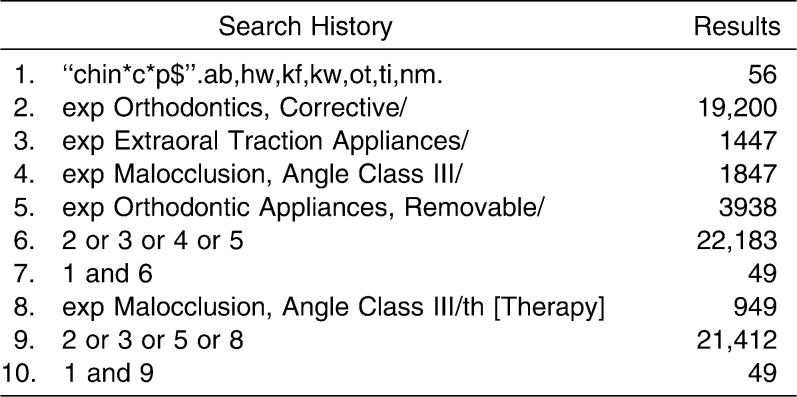
An electronic search for articles published up to the present was done through the Cochrane Central Register of Controlled Trials (CENTRAL; to March 2010), MEDLINE (1950–March 2010), EMBASE (1980–March 2010), and CBM (1978–March 2010), and there were no language restrictions. MeSh and free-text words that were used in the search as well as the search strategy is given in Table 1. Relevant Chinese journals were hand searched, and the World Health Organization International Clinical Trials Registry Platform were also searched for ongoing studies. Reference lists of identified articles and relevant review articles were checked for further possible studies. Abstracts of all studies identified by the searches were independently assessed by two reviewers. Full copies of all relevant and potentially relevant studies or those with insufficient data in the title and abstract to make a clear decision were obtained.
Table 1.
Ovid MEDLINE Search: 1950 to Present With Daily Updates
Selection Criteria
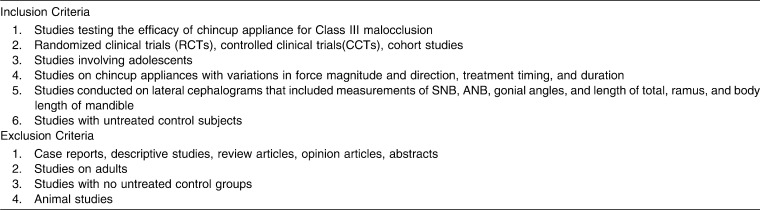
The inclusion and exclusion criteria are given in Table 2. Two reviewers assessed the full-text copies independently, and any disagreements on the eligibility of studies were resolved through discussion and, if not, by consultation of a third reviewer. Studies meeting the inclusion criteria underwent quality assessment and data extraction. Studies not meeting the inclusion criteria were excluded and eliminated from further review. Particulars of these studies and reasons for their exclusion are given in Figure 1.
Table 2.
Inclusion and Exclusion Criteria for the Retrieved Studies
Figure 1.
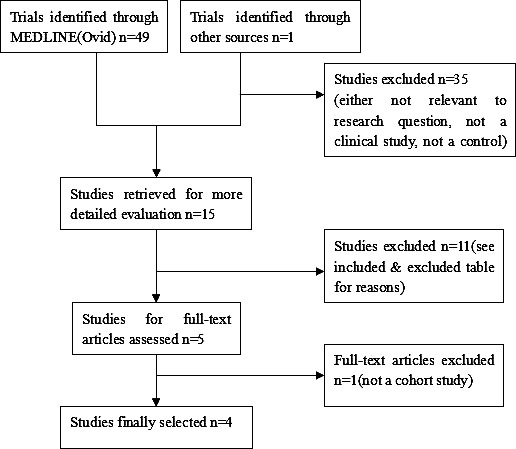
Flow diagram of study selected and meta-analysis.
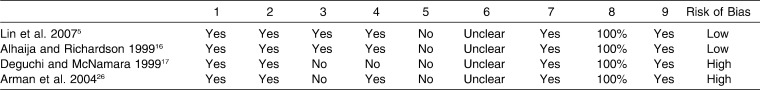
Reporting Quality and Risk of Bias Assessment
To ensure that variation was not caused by systematic errors in the design of the study, two reviewers independently graded selected studies, and every study was assessed following the criteria by Khan et al.25 with some modification. The evaluations were compared, and any inconsistencies between the review authors in the interpretation of the inclusion criteria and their significance to the selected trials were discussed and resolved.
The following criteria were used. Studies were judged as “yes,” “unclear,” and “no” to reflect on the quality of the studies. All criteria except the fifth criterion were used to reflect the risk of bias of all the studies. Studies getting 7 “yes” results or more than 7 “yes” results were considered as having a low risk of bias, studies with fewer than 7 “yes” results and not a “no” result were considered as having a moderate risk of bias, those receiving a “no” result were considered as at high risk of bias.
Was there sufficient description of the groups and the distribution of prognostic factors?
Were the groups assembled at a similar point in their disease progression?
Were the groups comparable on all important confounding factors?
Was there adequate adjustment for the effects of these confounding variables?
Was a dose-response relationship between intervention and outcome demonstrated?
Was outcome assessment blind to exposure status?
Was follow-up long enough for the outcomes to occur?
What proportion of the cohort was followed-up?
Were dropout rates and reasons for drop out similar across intervention and unexposed groups?
Data Extraction
Data extraction was carried out by two reviewers independently using a customized data extraction form. The following data were extracted: the study design, centers involved and location; the study's eligibility based on the inclusion and exclusion criteria; number, age range, mean age, and gender of the participants; the details of the intervention; losses to follow-up and the reasons, funding, and outcome details including the methods of assessment and time intervals at which the variables were recorded; and the baseline status.
Statistical Analysis
Data analysis was performed using Review Manager 5.01. All of the analysis was based on the data provided by the selected studies. Data synthesis was done if there was no significant clinical and methodological heterogeneity. If there was heterogeneity, subgroup analysis was considered, and if the subgroup analysis failed, only description of the intervention effects was used in the outcome part.
Statistical heterogeneity was made by Cochrane's test (I2) for heterogeneity. If there was substantial heterogeneity or considerable heterogeneity (I2 > 50%), the results were assessed using the random-effects model; if not, the fixed-effects model was used.
The meta-analysis was performed using dichotomous data and continuous data. For dichotomous data, risk ratios and 95% corresponding intervals were calculated. For continuous data, the weighted mean difference (WMD) and 95% confidence intervals (CIs) were calculated if the variable was assessed by the same method among the included studies; otherwise, the standard mean difference and 95% CIs were used. Special instructions suggested in the Cochrane Handbook for the continuous data combining were followed. We set the statistical significance for the hypothesis test (two-tailed z tests) for the meta-analysis at P < .05.
RESULTS
The search yielded 50 articles. After selection according to the inclusion and exclusion criteria, four articles qualified for the review analysis. Four eligible trials comprising 179 subjects met the inclusion criteria.5,16,17,26 The flow of the selection process is shown in Figure 1. The main reasons for exclusion were studies not relevant, animal studies, case reports, reviews, opinion articles, studies concerning chincup therapy in adult patients, or studies with no untreated control group.
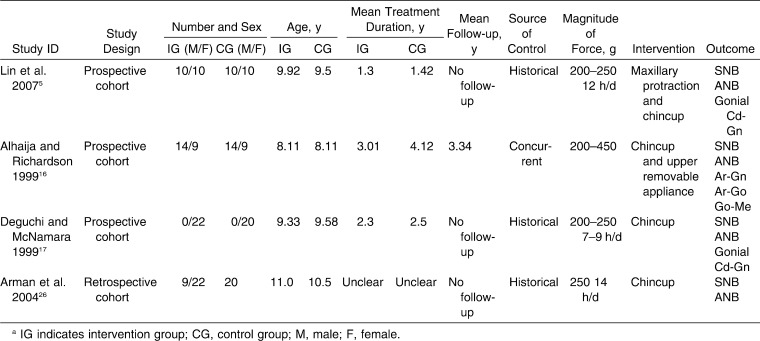
Of the studies included in the review analysis, one was done in Turkey, one in Japan, one in the United Kingdom, and one in China. Of the four studies included, one was a retrospective cohort study and three were prospective cohort studies. Table 3 shows the characteristics of the studies that were included in the review. All of the included studies exhibited high quality, except in item 3 to 6. Two studies showed a low risk of bias, and the other two showed a high risk of bias (Table 4).
Table 3.
Characteristics of Included Studiesa
Table 4.
Reporting Quality and Risk of Bias Assessment of Included Studies
Outcome Measures
SNB angle, ANB angle, gonial angle (Ar-Go-Me), total mandibular length (Cd-Gn), ramus height (Ar-Go), and mandibular body length (Go-Me), which were considered sensitive measures for correction of Class III malocclusion by retardation of mandibular growth, were adopted as primary outcome measures. Not all of these outcomes were, however, reported in all included studies. A meta-analysis of SNB and ANB angles was done, and forest plots are shown in Figures 2 and 3 for the effect of the chincup therapy.
Figure 2.
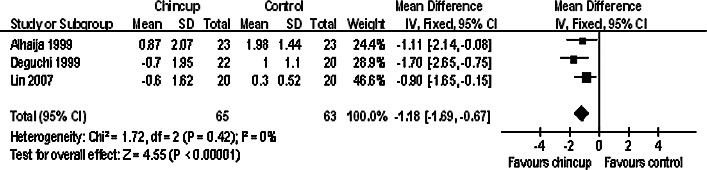
Chincup vs no-treatment control group for meta-analysis results in SNB angle.
Figure 3.
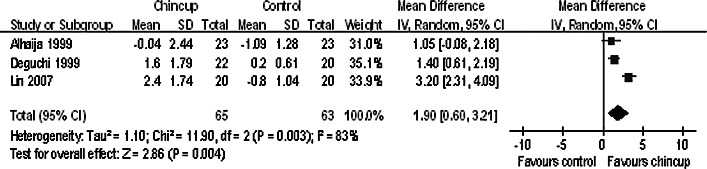
Chincup vs no treatment control group for meta-analysis results in ANB angle.
Chincup vs No-Treatment Control
SNB angle
Three studies reported this variable and were included in the meta-analysis.5,16,17 All of the studies reported a significantly better result in the chincup group compared with the control group. No heterogeneity was detected through the homogeneity test (I2 = 0%, P = .42), so the fixed-effect model was adopted. The total pooled WMD value (95% CI) of SNB was −1.18 (−1.69, −0.67; P < .00001), indicating the result favored the chincup group.
ANB angle
A meta-analysis of three studies was undertaken concerning the ANB angle.5,16,17 As significant heterogeneity existed, the random-effect model was adopted. The total pooled WMD value (95% CI) of ANB was 1.90 (0.60, 3.21), which favored the chincup group. Chincup therapy significantly increased the ANB angle, and there was an improvement of the maxillomandibular relationship.
Gonial angle (Ar-Go-Me)
Deguchi and McNamara17 showed that the gonial angle increased after chincup therapy in comparison to controls (P < .05). Lin et al.5 reported similar findings and concluded that the gonial angle changed more in the chincup group (P = .007).
Mandibular length (Cd-Gn), body length (Go-Me), and ramus height (Ar-Go)
Three studies included these variables. Deguchi and McNamara17 and Lin et al.5 reported that there was no significant change in the mandibular length (Cd-Gn), with P values .059 and .39, respectively (P > .05). Alhaija and Richardson16 found that there was no significant change in the mandibular length; however, the growth continued after the treatment, measured by Ar-Gn (considered the same as Cd-Gn) and Go-Me.
DISCUSSION
Randomized clinical trials (RCTs) have been seldom used in orthodontics due to ethical issues associated with blind allocation of patients to different treatment strategies. Long-term studies of Class III patients with an untreated control group are especially difficult to ethically conduct because some subjects may be designated to an untreated control group in which the treatment will be postponed after the study period, and these subjects may refuse to participate in the trial. In this systematic review, four studies were included. No RCTs were found for the outcomes of chincup therapy. All studies used in this review were cohort studies, with shortcomings such as no randomization and allocation concealment, no previous estimation of sample sizes, and no discussion on the possibility of type II error occurring. No blinding was reported in any of these studies, leading to higher possibilities of selection and measurement bias.
Clinical heterogeneity existed in all of the studies with regard to treatment modality and duration. Primary outcome measures were inadequately recorded in these studies, which made them impossible for meta-analysis and weak in evidence. Historical control groups were used in three of the included studies; although not as ideal as concurrent control groups, they are qualified in these studies as the untreated control groups are set to offset the impact of growth and development on treatment outcomes.
Although not included in the meta-analysis, the study by Arman et al.26 was in agreement with those three studies (P < .001) and came to a conclusion that chincup therapy significantly decreased the SNB and increased the ANB angle. These results were in agreement with many other clinical studies.23,27–29
A decrease in the SNB angle may due to backward and downward rotation of the mandible, as measured by the closure in the gonial angle. Backward and downward rotation of the mandible can also contribute to the increase in ANB angle. Whether changes of ANB angle resulted from change in the mandible only or in both the maxilla and mandible remained unclear.
There was no adequate evidence that chincup retarded growth of the mandible as measured by total, ramus, and body mandibular length in the studies included in this review. A later study by Deguchi et al.18 found that long-term treatment resulted in a retardation of mandibular total and body length growth.
The ultimate treatment goal of skeletal Class III patients should be not only the correction of the jaw relationship but also stabilization of intermaxillary skeletal and dental relationships obtained by the treatment. Thus, close observation and follow-up of excessive mandibular development during adolescence was essential.5 Only one article reported the cephalometric measurements 1 year posttreatment, which was far from adequate.16 No follow-up records were reported in the other studies included. Uner et al.23 reported a long-term follow-up study of chincup therapy and concluded that there was a relapse potential after 4 years of chincup treatment. In their long-term follow-up study, Sugawara et al.24 indicated that chincup therapy did not necessarily guarantee positive correction of skeletal profile after complete growth. However, these two studies were excluded from this systematic review because they lacked an untreated control group.
In a study on possible factors that contribute to the stability of chincup therapy, Ko et al.15 found that chincup therapy was applicable to skeletal Class III malocclusions with mandibular excess in growing patients, but the result depended on the facial skeletal pattern before chincup therapy and severity of the anteroposterior jaw discrepancy. This finding was supported by Ishikawa et al.30
Tahmina et al.19 found that the mandible of the unstable group had a significantly larger gonial angle than that of the stable group at the initial stage and that the mandible showed downward and backward rotation during early treatment and then rotated in an upward and forward direction after the correction of the anterior crossbite in the unstable group. It was concluded that the type of mandibular rotation and displacement and the degree of forward growth of the mandible were keys to the treatment outcomes in growing patients with Class III malocclusion after chincup therapy.
Deguchi et al.18 concluded that in the short term, chincup therapy resulted in backward rotation of the mandible, while the long-term treatment inhibited the growth of the mandible, leading to a decrease in total ramus and body length of the mandible (Ar-Go, Go-Me, Gn-Go) and a reduction in the gonial angle.
These suggested determinants of stability and differences between long-term and short-term effects of chincup were devoid of well-designed of controlled clinical trials and therefore were excluded from this systematic review. Because of the limited comparative evidence, there is a need for high-quality clinical trials to further investigate the efficacy of chincup therapy for retardation of mandibular growth. Further well-controlled studies with long-term follow-up should be done before concrete conclusions on the efficacy of chincup therapy in retardation of mandibular growth in Class III malocclusions can be made.
CONCLUSIONS
A meta-analysis showed that chincup therapy decreased the SNB angle and increased the ANB angle, leading to an improvement of the maxillomandibular relationship. Whether these results can be maintained after puberty is not clear because there was no long-term follow-up in the studies reported.
There are insufficient data in these studies to make clear recommendations regarding the efficacy of chincup therapy in retardation of mandibular growth.
Acknowledgments
This study was supported by a grant from the Science and Technology Bureau of Sichuan Province (No. 2008ZR0160). We acknowledge Professor Zongdao Shi for his guidance in conducting this systematic review.
REFERENCES
- 1.McNamara J. A., Jr An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21:598–608. [PubMed] [Google Scholar]
- 2.Thilander B, Myberg N. The prevalence of malocclusion in Swedish school children. Scand J Dent Res. 1973;81:12–20. doi: 10.1111/j.1600-0722.1973.tb01489.x. [DOI] [PubMed] [Google Scholar]
- 3.Jacobson A, Evans W. G, Preston C. B. Mandibular prognathism. Am J Orthod. 1974;66:140–171. doi: 10.1016/0002-9416(74)90233-4. [DOI] [PubMed] [Google Scholar]
- 4.Graber L. W. Chincup therapy for mandibular prognathism. Am J Orthod. 1977;72:23–41. doi: 10.1016/0002-9416(77)90122-1. [DOI] [PubMed] [Google Scholar]
- 5.Lin H. C, Chang H. P, Chang H. F. Treatment effects of occipitomental anchorage appliance of maxillary protraction combined with chincup traction in children with Class III malocclusion. J Formos Med Assoc. 2007;106:380–391. doi: 10.1016/S0929-6646(09)60323-5. [DOI] [PubMed] [Google Scholar]
- 6.Kameda A. The Begg technique in Japan. Am J Orthod. 1982;81:209–227. doi: 10.1016/0002-9416(82)90054-9. [DOI] [PubMed] [Google Scholar]
- 7.Yang W. S. The study on the orthodontic patients who visited Department of Orthodontics, Seoul National University Hospital. J Korean Dent Assoc. 1990;28:811–821. [PubMed] [Google Scholar]
- 8.Tang E. L. The prevalence of malocclusion amongst Hong Kong male dental students. Br J Orthod. 1994;21:57–63. doi: 10.1179/bjo.21.1.57. [DOI] [PubMed] [Google Scholar]
- 9.Nartallo-Turley P, Turley P. K. Cephalometric effects of combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod. 1998;68:217–224. doi: 10.1043/0003-3219(1998)068<0217:CEOCPE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Deguchi T, Kitsugi A. Stability of changes associated with chin-cup treatment. Angle Orthod. 1996;66:139–145. doi: 10.1043/0003-3219(1996)066<0139:SOCAWC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Mitani H. Early application of chincup therapy to skeletal Class III malocclusion. Am J Orthod Dentofacial Orthop. 2002;121:584–585. doi: 10.1067/mod.2002.124170. [DOI] [PubMed] [Google Scholar]
- 12.Yoo Y. K, Kim N. I, Lee H. K. A study on the prevalence of malocclusion in 2378 Yonsei University students. Korean J Orthod. 1971;2:35–40. [Google Scholar]
- 13.Mitani H, Sato K, Sugawara J. Growth of mandibular prognathism after pubertal growth peak. Am J Orthod Dentofacial Orthop. 1993;104:330–336. doi: 10.1016/S0889-5406(05)81329-0. [DOI] [PubMed] [Google Scholar]
- 14.Lee S. J, Kim T. W, Suhr C. H. Study of recognition of malocclusion and orthodontic treatments. Korean J Orthod. 1994;24:367–394. [Google Scholar]
- 15.Ko Y, Baek S, Mah J, Yang W. S. Determinants of successful chincup therapy in skeletal Class III malocclusion. Am J Orthod Dentofacial Orthop. 2004;126:33–41. doi: 10.1016/j.ajodo.2002.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Alhaija Abu E. S, Richardson A. Long-term effect of the chincap on hard and soft tissues. Eur J Orthod. 1999;21:291–298. doi: 10.1093/ejo/21.3.291. [DOI] [PubMed] [Google Scholar]
- 17.Deguchi T, McNamara J. A., Jr Craniofacial adaptations induced by chincup therapy in Class III patients. Am J Orthod Dentofacial Orthop. 1999;115:175–182. doi: 10.1016/s0889-5406(99)70346-x. [DOI] [PubMed] [Google Scholar]
- 18.Deguchi T, Kuroda T, Minoshima Y, Graber T. M. Craniofacial features of patients with Class III abnormalities: growth-related changes and effects of short-term and long-term chincup therapy. Am J Orthod Dentofacial Orthop. 2002;121:84–92. doi: 10.1067/mod.2002.120359. [DOI] [PubMed] [Google Scholar]
- 19.Tahmina K, Tanaka E, Tanne K. Craniofacial morphology in orthodontically treated patients of Class III malocclusion with stable and unstable treatment outcomes. Am J Orthod Dentofacial Orthop. 2000;117:681–690. [PubMed] [Google Scholar]
- 20.Sakamoto T, Iwase I, Uka A, Nakamura S. A roentgenocephalometric study of skeletal changes during and after chin-cup treatment. Am J Orthod. 1984;85:341–350. doi: 10.1016/0002-9416(84)90191-x. [DOI] [PubMed] [Google Scholar]
- 21.Mitani H, Sakamoto T. Chin-cup force to a growing mandible: long-term clinical reports. Angle Orthod. 1984;54:93–122. doi: 10.1043/0003-3219(1984)054<0093:CCFTAG>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Mitani H, Fukazawa H. Effects of chincap force on the timing and amount of mandibular growth associated with anterior reversed occlusion (Class III malocclusion) during puberty. Am J Orthod Dentofacial Orthop. 1986;90:454–463. doi: 10.1016/0889-5406(86)90105-8. [DOI] [PubMed] [Google Scholar]
- 23.Uner O, Yuksel S, Ucuncu N. Long-term evaluation after chincap treatment. Eur J Orthod. 1995;17:135–141. doi: 10.1093/ejo/17.2.135. [DOI] [PubMed] [Google Scholar]
- 24.Sugawara J, Asano T, Endo N, Mitani H. Long-term effects of chincap therapy on skeletal profile in mandibular prognathism. Am J Orthod Dentofacial Orthop. 1990;98:127–133. doi: 10.1016/0889-5406(90)70006-X. [DOI] [PubMed] [Google Scholar]
- 25.Khalid S. K, Riet G. T, Glanville J, Sowden A. J, Kleijnen J, editors. Undertaking Systematic Reviews of Research on Effectiveness CRD's Guidance for Those Carrying out or Commissioning Reviews. York, UK: York Publishing Services Ltd; 2001. [Google Scholar]
- 26.Arman A, Toygar T. U, Abuhijleh E. Profile changes associated with different orthopedic treatment approaches in Class III malocclusions. Angle Orthod. 2004;74:733–740. doi: 10.1043/0003-3219(2004)074<0733:PCAWDO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Irie M, Nakamura S. Orthopedic approach to severe skeletal Class III malocclusion. Am J Orthod. 1975;67:377–392. doi: 10.1016/0002-9416(75)90020-2. [DOI] [PubMed] [Google Scholar]
- 28.Chong Y. H, Ive J. C, Årtun J. Changes following the use of protraction headgear for early correction of Class III malocclusion. Angle Orthod. 1996;66:351–362. doi: 10.1043/0003-3219(1996)066<0351:CFTUOP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Üçüncü N, Üçem T. T, Yüksel S. A comparison of chincup and maxillary protraction appliances in the treatment of skeletal Class III malocclusions. Eur J Orthod. 2000;22:43–51. doi: 10.1093/ejo/22.1.43. [DOI] [PubMed] [Google Scholar]
- 30.Ishikawa H, Nakamura S, Kim C, Iwasaki H, Satoh Y, Yoshida S. Individual growth in Class III malocclusions and its relationship to the chin-cup effects. Am J Orthod Dentofacial Orthop. 1998;114:337–346. doi: 10.1016/s0889-5406(98)70217-3. [DOI] [PubMed] [Google Scholar]