Abstract
Objective
To determine whether surge conditions were associated with increased mortality.
Design
Multicenter cohort study.
Setting
U.S. ICUs participating in STOP-COVID.
Patients
Consecutive adults with COVID-19 admitted to participating ICUs between March 4 and July 1, 2020.
Interventions
None
Measurements and Main Results
The main outcome was 28-day in-hospital mortality. To assess the association between admission to an ICU during a surge period and mortality, we used two different strategies: (1) an inverse probability weighted difference-in-differences model limited to appropriately matched surge and non-surge patients and (2) a meta-regression of 50 multivariable difference-in-differences models (each based on sets of randomly matched surge- and non-surge hospitals). In the first analysis, we considered a single surge period for the cohort (March 23 – May 6). In the second, each surge hospital had its own surge period (which was compared to the same time periods in matched non-surge hospitals).
Our cohort consisted of 4342 ICU patients (average age 60.8 [sd 14.8], 63.5% men) in 53 U.S. hospitals. Of these, 13 hospitals encountered surge conditions. In analysis 1, the increase in mortality seen during surge was not statistically significant (odds ratio [95% CI]: 1.30 [0.47-3.58], p = .6). In analysis 2, surge was associated with an increased odds of death (odds ratio 1.39 [95% CI, 1.34-1.43], p < .001).
Conclusions
Admission to an ICU with COVID-19 in a hospital that is experiencing surge conditions may be associated with an increased odds of death. Given the high incidence of COVID-19, such increases would translate into substantial excess mortality.
Keywords: COVID-19, intensive care unit, mortality, surge, occupancy
Introduction
When reports first surfaced from Wuhan, China of a novel coronavirus (SARS-CoV-2) with both asymptomatic person-to-person transmissibility and a high incidence of acute respiratory distress syndrome (ARDS) and death, the world reacted with understandable alarm.1–3 In the United States, particular concern was expressed regarding mechanical ventilator capacity. Although the U.S. maintains a national strategic reserve of ventilators, it was estimated that supply would be far less than potential demand.4,5 In the spring of 2020—particularly in densely populated urban areas on the U.S. East Coast—outbreaks of COVID-19 tore through communities, overwhelming many hospitals.6 Somewhat surprisingly, patient morbidity due to the lack of mechanical ventilators was not extensively reported. This was likely due to a number of strategies including utilization of ventilators from the national stockpile, repurposing non-invasive ventilatory devices as invasive mechanical ventilators, and use of alternative non-invasive ventilation strategies (eg, bi-level positive airway pressure and high-flow nasal cannula).7
Although ventilator shortfalls were not widely reported, providers expressed concern that other factors such as inadequate staffing, lack of ICU beds, and shortages of other essential equipment may have led to increased mortality in critically ill COVID-19 patients in the hardest hit areas.7,8 Increasing this concern were reports of high mortality rates in COVID-19 patients with respiratory failure who were cared for under surge conditions.9–11 Although these reports may have painted an overly bleak picture biased by incomplete follow-up, this mortality rate is far higher than the 26.5 to 46.3% mortality rate reported for patients with non-COVID-19 ARDS in the modern era and the 31 to 35% mortality rate for COVID-19 patients with ARDS cared for in non-surge settings.12–17 Finally, Bravata et al. found, in a large cohort study of COVID-19 admissions to Veteran's Administration (VA) hospitals, that high ICU caseload was associated with increased mortality; however, this study was not focused on critically ill patients and its generalizability to non-VA hospitals is unknown.18
We sought to determine whether the surge conditions during the spring of 2020 were associated with an increased mortality rate in ICU patients with COVID-19 across a diverse cohort of U.S. hospitals. We hypothesized that admission to an ICU during a period of surge would be associated with worse outcomes.
Materials and Methods
We conducted a multicenter cohort study of consecutive adults (≥18 years-old) admitted to U.S. ICUs with COVID-19 using the Study of the Treatment and Outcomes in Critically Ill Patients (STOP-COVID) database to evaluate the association between admission to a hospital experiencing a surge in COVID-19 ICU cases and 28-day in-hospital mortality.19 Data collection for STOP-COVID included ICU admissions from March 4 through July 1, 2020. We excluded hospitals that submitted data on fewer than 30 patients during the study period.
Data Elements
From the STOP-COVID dataset, we abstracted patient-level data on demographics (age; sex; race), chronic health information (body mass index; comorbidities—diabetes, hypertension, coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, cancer; smoking history), and acute illness information (date of ICU admission; duration of symptoms prior to ICU admission; and respiratory failure [ratio of arterial partial pressure of oxygen to inspired oxygen fraction and use of mechanical ventilation], vasopressor use, and renal, coagulation, and liver dysfunction [assessed by sequential organ failure assessment score20] on ICU admission). Hospital-level data included the number of ICU beds at baseline (prior to COVID-19 admissions) and American Hospital Association region.21
Exposure
Surge status at a given hospital was defined on each calendar day as having a COVID-19 ICU census that was greater than or equal to the number of ICU beds at baseline. The study period was divided into 3 time periods—pre-surge (before any hospital surged), surge (while at least one hospital was surging), and post-surge (after all hospitals were no longer surging).
Outcome
Our primary outcome was in-hospital 28-day mortality. Patients discharged alive prior to day 28 were considered alive at 28 days.
Statistical Analysis
We described the cohort using standard summary statistics. Characteristics of patients admitted on surge or non-surge days were compared using Chi-square and t-testing as appropriate.
To evaluate the association of admission during surge and 28-day in-hospital mortality, we employed three analytic approaches. Our initial approach was a difference-in-differences (DiD) analysis including patients admitted to any study hospital. Patients admitted to hospitals that experienced surge during the surge epoch were considered “exposed”; patients admitted to hospitals that never surged served as temporal controls (e Figure 1a). Post-surge patients were excluded and, to limit misclassification, we also excluded patients who were admitted during the surge epoch to hospitals that experienced surge conditions, but whose hospital was not surging on their day of admission. All aforementioned covariates (other than ICU bed number) were included in the model and standard errors were clustered by hospital. However, the parallel trends assumption was not met. Thus, we could not conduct this analysis and moved on to two alternate approaches.
To identify a more comparable control group for our DiD analysis, we next excluded patients admitted to ICUs in U.S. states where no participating hospital ever surged. Among this group, we conducted an inverse probability weighted (IPW) DiD analysis.22 Weights were based on each patient's propensity to be in a given exposure group (1: surge hospital, pre-surge; 2: surge hospital, during surge; 3: non-surge hospital, pre-surge; 4: non-surge hospital, during surge; eFigure 1b). The parallel trends assumption was tested and met using this approach (e Figure 2).
In a final approach that sought to minimize patient and hospital exclusions (eFigure 1c), we re-defined surge periods at the hospital level, rather than across the entire cohort. Each of the 40 non-surge hospitals was then randomly matched to one of the 13 surge hospitals, 3 to 4 non-surge hospitals per surge hospital. The surge period for each non-surge hospital was defined as that of the surge hospital to which it was matched. This process of random matching was repeated to create 50 sets of matched surge and non-surge hospitals for which the parallel trends assumption was met (e Figure 3 and e Table 1). We then constructed a multivariable DiD model to assess the association of surge with mortality for each of the 50 matched sets. Finally, we combined effect estimates across these sets using meta-regression with robust variance estimation to account for the repeated use of observations.23 In all models, all cohort hospitals were included; the number of patients included varied (as “post-surge” exclusions for non-surge hospitals differed across matched sets).
We additionally performed two pre-planned sensitivity analyzes using the simple exposures of (1) “admitted on a surge day” or (2) “admitted during a hospital's surge period”. To accomplish this, we constructed a pair of multivariable mixed-effects models inclusive of all aforementioned covariates; hospital of admission was included as a random effect. Both analyses were performed on the full cohort and, separately, on only patients admitted to surge hospitals. Post-hoc, we conducted three additional sensitivity analyses to evaluate the robustness of our results to our definition of surge: (1) the IPW DiD approach with different values of percent of baseline ICU capacity used to define surge; (2) the simple exposure (non-DiD) model with surge included as a continuous variable (modeled linearly); and (3) the simple exposure model with surge included as a categorical variable (by 25% of baseline ICU capacity increments).
All statistical analyses were performed using StataMP 16 (StataCorp, College Station, Texas), R (www.R-project.org), and Microsoft Excel (Microsoft, Redmond, Washington). Institutional Review Board approval was obtained from the University of Miami (#20200750) and from each participating site.
Results
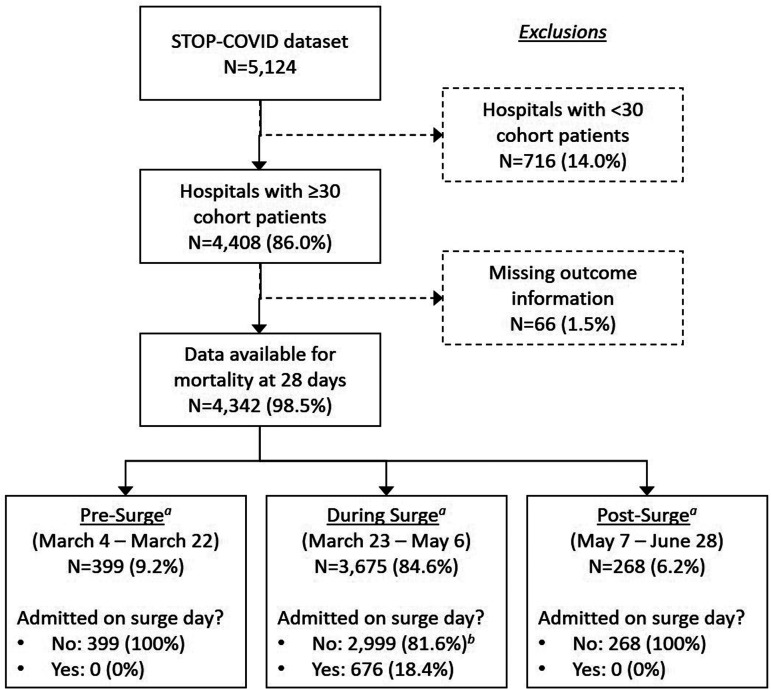
Our primary cohort consisted of 4342 critically ill adult patients admitted to 53 U.S. hospitals (Figure 1). Thirteen hospitals across Louisiana, Massachusetts, New Jersey, New York, Ohio, and Pennsylvania experienced at least 1 day of surge and all surge days occurred between March 23 and May 6 (Figure 2). A total of 676 of the 4342 patients (15.6%) were admitted to the ICU on a surge day (Table 1). Patients admitted on surge days tended to be older (64.0% vs. 55.5% were ≥60 years-old), less commonly of Black race (18.8% vs. 33.0%), and more commonly received invasive mechanical ventilation (75.5% vs. 59.4%) and vasopressor support (49.4% vs. 39.8%) on ICU day 1 (e Table 2). In-hospital 28-day mortality was higher in patients admitted on surge (58.9%) versus non-surge (33.8%) days (p < .001).
Figure 1.
Cohort creation.
a surge period includes first day any hospital experienced surge through the last day any hospital experienced surge
b 408 (13.6% of 2999) admissions were to surge hospitals during the surge period but on days in which their hospital did not experience surge; these are excluded from first primary analysis.
Figure 2.
Distribution of surge and non-surge days for each Cohort hospital.a
aEach row represents a unique cohort hospital (grouped by US State), each column a unique calendar day from March 4 to June 28. Blank squares represent days in which no new ICU admission was recorded in the cohort. Of days with ICU admissions, green squares represent non-surge days (COVID-19 ICU occupancy <100% of baseline ICU capacity) and red squares represent surge days (COVID-19 ICU occupancy ≥100% of baseline ICU capacity).
Table 1.
Cohort Baseline Characteristics and Outcomes.
| Not admitted on surge day, N(%) | Admitted on surge day, N(%) | p-valuea | |
|---|---|---|---|
| # of patients, N(row %) | 3666 (84.4) | 676 (15.6) | |
| Admission period | <.001 | ||
| Pre-surge (March 4 - March 22) | 399 (10.9) | 0 (.0) | |
| During surge (March 23 - May 6) | 2999 (81.8)b | 676 (100.0) | |
| Post-surge (May 7 - June 28) | 268 (7.3) | 0 (.0) | |
| Hospital ever experienced surge | 589 (16.1) | 676 (100.0) | <.001 |
| Age (years) | <.001 | ||
| ≤39 | 377 (10.3) | 40 (5.9) | |
| 40 to 49 | 460 (12.5) | 66 (9.8) | |
| 50 to 59 | 793 (21.6) | 137 (20.3) | |
| 60 to 69 | 1007 (27.5) | 207 (30.6) | |
| 70 to 79 | 680 (18.5) | 159 (23.5) | |
| 80 + | 349 (9.5) | 67 (9.9) | |
| Male gender | 2321 (63.3) | 436 (64.5) | .56 |
| Race | <.001 | ||
| White | 1365 (37.2) | 267 (39.5) | |
| Black | 1209 (33.0) | 127 (18.8) | |
| Other | 291 (7.9) | 49 (7.2) | |
| Unknown | 801 (21.8) | 233 (34.5) | |
| Body mass index | .004 | ||
| <25 | 664 (18.1) | 101 (14.9) | |
| 25-<30 | 1028 (28.0) | 224 (33.1) | |
| 30-<35 | 861 (23.5) | 159 (23.5) | |
| 35-<40 | 464 (12.7) | 72 (10.7) | |
| 40 + | 525 (14.3) | 84 (12.4) | |
| Unknown | 124 (3.4) | 36 (5.3) | |
| Comorbidities | |||
| Diabetes | 1546 (42.2) | 297 (43.9) | .39 |
| Hypertension | 2234 (60.9) | 418 (61.8) | .66 |
| Coronary artery disease | 494 (13.5) | 94 (13.9) | .76 |
| Congestive heart failure | 378 (10.3) | 55 (8.1) | .08 |
| Chronic obstructive pulmonary disease | 311 (8.5) | 55 (8.1) | .77 |
| Cancer | 154 (4.2) | 38 (5.6) | .10 |
| Current smoker | 198 (5.4) | 27 (4.0) | .13 |
| Symptoms started ≤3d pre-ICU admission | 829 (22.6) | 127 (18.8) | .027 |
| Week of studyc, mean(sd) | 5.31 (2.44) | 5.37 (1.35) | .53 |
| 28-day in-hospital mortality | 1238 (33.8) | 398 (58.9) | <.001 |
d: days; ICU: intensive care unit; sd: standard deviation.
Chi-square testing for categorical and t-testing for continuous variable comparisons.
2,999 patients were admitted during the surge period (March 23 to May 6), yet on days where their individual hospital did not experience surge (ie, total COVID-19 ICU census was <100% baseline ICU capacity).
The study period was divided into weeks, week 1 (March 4 through March 11) to week 17 (June 25 to June 28, a partial week).
Association of Surge and 28-Day In-Hospital Mortality
Inverse probability weighted DiD modeling
The restricted cohort used for IPW DiD modeling consisted of 2052 ICU admissions across 30 hospitals (13 that surged on at least one day, 17 that did not; eTable 3). The adjusted odds of death associated with being admitted during surge was not statistically significantly different than being admitted pre-surge after adjusting for temporal trends (odds-ratio, OR [95% confidence interval, CI] for interaction term of hospital surge status and time period: 1.30 [0.47-3.58]; Table 2). These results were robust to varying the ICU occupancy used to define surge (eTable 4).
Table 2.
Adjusted Association of Admission During Surge with 28-Day In-Hospital Mortality.a.
| Difference-in-Differences Models | ||||
|---|---|---|---|---|
| N (%) | OR (95% CI)a | p-valueb | ||
| Primary Analysis 1: IPW Model | 2052 | 1.30 (.47,3.58) | .61 | |
| Primary Analysis 2: Meta-Analysis | 3041 - 3,422c | 1.39 (1.34,1.43) | <.001 | |
| Simple Surge/Not Surge Models | ||||
| Not exposed, N (%) | Exposed, N (%) | OR (95% CI)d | p-valued | |
| Primary Surge Definition | ||||
| All Hospitals (N = 4342) | ||||
| Individual patient experienced surge | 3666 (84.4) | 676 (15.6) | 1.49 (1.10,2.02) | .009 |
| Admitted during hospital Surge | 3655 (84.2) | 687 (15.8) | 1.46 (1.08,1.96) | .014 |
| Only Surge Hospitals (N = 1265) | ||||
| Individual patient experienced surge | 589 (46.6) | 676 (53.4) | 1.23 (.88,1.73) | .23 |
| Admitted during hospital Surge | 578 (45.7) | 687 (54.3) | 1.21 (.87,1.69) | .26 |
| Alternative Surge Definitions | ||||
| All Hospitals (N = 4342); Individual patients experienced surge | ||||
| Model 1: surge as a patient-level continuous exposure (per 1% increase in ICU occupancy) | 3666 (84.4) | 676 (15.6) | 1.003 (1.001,1.005) | .008 |
| Model 2: surge as a patient-level categorical exposure | 3666 (84.4) | 676 (15.6) | ||
| <25% | Reference | |||
| 25 to 49% | 1.02 (.81,1.29) | .87 | ||
| 50 to 74% | 1.07 (.81,1.42) | .62 | ||
| 75 to 99% | 1.29 (.90,1.84) | .17 | ||
| 100 to 124% | 1.44 (.95,2.18) | .09 | ||
| 125 to 149% | 1.89 (1.01,3.53) | .046 | ||
| 150 to 174% | 2.46 (1.27,4.77) | .008 | ||
| 175 to 199% | 1.85 (.76,4.48) | .17 | ||
| 200 to 224% | .79 (.24,2.62) | .70 | ||
| 225 to 249% | 2.26 (.87,5.90) | .10 | ||
| 250 to 274% | 2.36 (1.12,4.97) | .024 | ||
| 275 to 299% | 2.90 (1.01,8.34) | .049 | ||
| 300 to 324% | 1.83 (.88,3.83) | .11 | ||
| 325 to 349% | 1.78 (.68,4.69) | .24 | ||
CI: confidence interval; IPW: inverse probability weighted; OR: odds-ratio.
All multivariable models included adjustment by the following covariables: age (grouped as <40, 40-49, 50-59, 60-69, 70-79, and 80 + ); male gender; race (categorized as White, Black, other, or unknown); body mass index (grouped as <25, 25-29, 30-34, 35-39, 40 + , and unknown); presence of diabetes mellitus; presence of hypertension; presence of coronary artery disease; presence of congestive heart failure; presence of chronic obstructive pulmonary disease; presence of cancer; current smoker; symptoms starting ≤3 days prior to intensive care unit admission; respiratory status at intensive care unit admission (not mechanically ventilated [MV]; MV with paO2/FiO2 ≥300; MV with paO2/FiO2 200-299; MV with paO2/FiO2 100-199; MV with paO2/FiO2 <100; and MV with unknown paO2/FiO2); use of vasopressors on intensive care unit day 1; renal sequential organ failure assessment (SOFA) score (grouped as 0/unknown, 1, 2, 3, or 4); coagulation SOFA score (grouped as 0/unknown, 1, 2, 3, or 4); liver SOFA score (grouped as 0, 1, 2, 3, 4, or unknown); and week of the study period for intensive care unit admission date. For the IPW model to create the propensity score, we also included adjustment for American Hospital Association geographic region (grouped as region 1 [Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont], 2 [New Jersey, New York, Pennsylvania], and 3-9 [all other states]).
for the interaction term of time period (pre-surge vs surge) and hospital surge status.
varies across 50 matched surge/non-surge hospital sets.
for the surge (vs not-surge) term in the model.
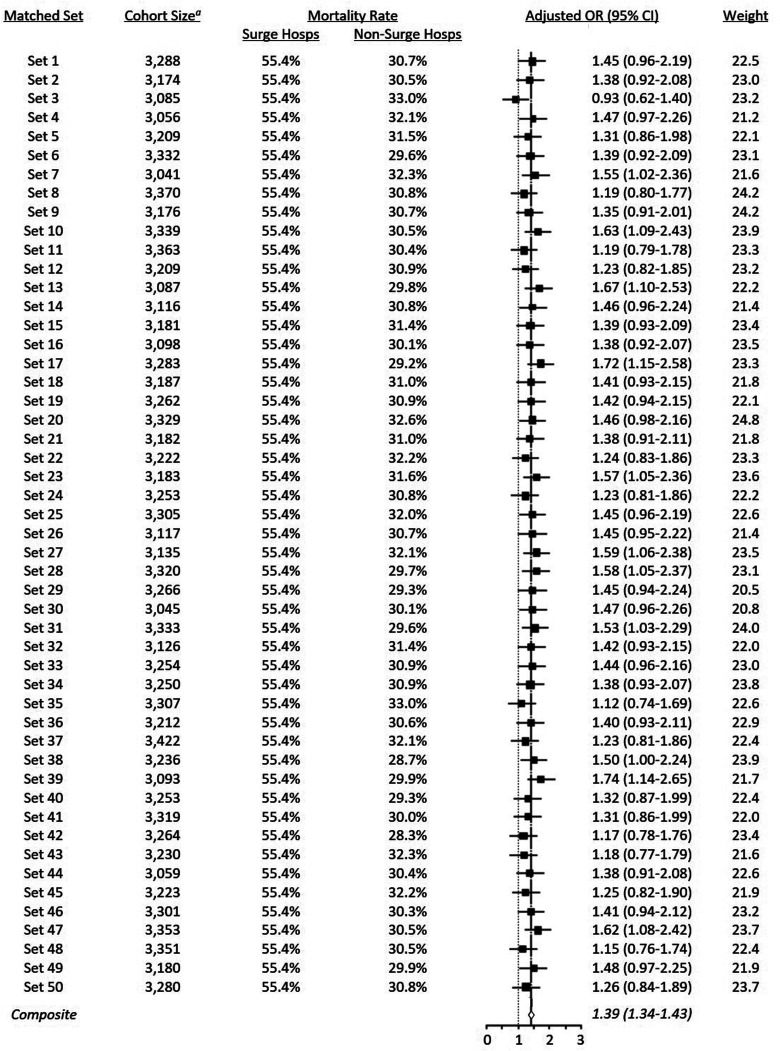
Meta-regression of DiD modeling of 50 matched hospital sets
The 50 matched surge/non-surge hospital sets each included 1185 patients admitted to 13 hospitals which ever surged; the number of patients included in the 40 non-surge hospitals ranged from 3041 to 3422 (Figure 3). After meta-regression with robust variance estimation, we found a significant association with being admitted during surge and 28-day in-hospital death (meta-analysis OR for interaction term of hospital surge status and time period: 1.39 [95% CI, 1.34-1.43], p < .001).
Figure 3.
Meta-analysis of difference-in-differences models on 50 randomly matched surge/non-surge hospital sets.
CI: confidence interval; hosps: hospitals; OR: odds-ratio
A each cohort includes 13 surge hospitals (with 1185 patients) and 40 non-surge hospitals.
Sensitivity Analyses
In our simplified models, we found that admission on a surge day (OR 1.49 [95% CI, 1.10-2.02], p = .009) and admission during a given hospital's surge period (OR 1.46 [95% CI, 1.08-1.96], p = .014) were each associated with increased 28-day in-hospital mortality. These results were robust to modeling surge as a continuous variable (OR 1.003 [95% CI, 1.001-1.005] for each 1% increase in ICU occupancy, p = .008). When the cohort was limited to only hospitals that experienced at least one surge day, the effect size was smaller and not statistically significant (Table 2).
Discussion
Using several approaches to assess the association between being admitted to an ICU at a hospital that was concomitantly experiencing a surge in ICU COVID-19 cases and mortality, we found that admission during times of surge may be associated with higher odds of in-hospital mortality by 28 days. Specifically, across analytic strategies, there was a 21 to 49% increased odds of death. In our more conservative approach, however, we could not exclude the possibility that this difference was due to chance.
Limitations in resources (eg, ICU nurses,24–27 intensivist staffing,28–30 overall staffing,31–34 and ICU beds35,36) have been shown to have variable but generally negative effects on the care and outcomes of critically ill patients without COVID-19. The COVID-19 surge in certain U.S. regions in spring, 2020 represented a “perfect storm” of resource limitations; profound deficiencies in ICU beds, clinicians, and vital equipment were reported simultaneously.6,7,37 To our knowledge, our study is the first to quantify the magnitude of the association of surge with critically ill COVID-19 patients’ outcomes across a diverse set of U.S. civilian hospitals.
Analyzing the effects of surge required sophisticated statistical techniques. Our analysis needed to address two issues: (1) hospitals surged at variable times and (2) treatment paradigms and patient case-mix varied over our study period. Our a priori plan was to use a DiD strategy with a single surge period for the full cohort (from the first through the last day any hospital surged). This approach would mitigate against both concerns aforementioned. However, it was limited in that all hospitals were assumed to surge simultaneously (even though each surge hospital truly did so only on certain days). To address this issue, we planned to exclude patients admitted to surge hospitals on non-surge days during the surge period. Unfortunately, this cohort did not meet assumptions necessary for our planned analysis.
Therefore, we used alternative analytic strategies decided upon post hoc. Our first alternative analysis was a replication of the a priori planned analysis using a smaller cohort which found a non-significant association of surge status with mortality. Our second alternative analysis excluded fewer patients and, perhaps as a result, showed a statistically significant negative association of ICU admission during surge with mortality. To complement these more complicated analyses, we performed several a priori planned simplified sensitivity analyses which showed similar increases in mortality for patients admitted during surge. Again, those with smaller sample sizes were not statistically significant.
The strengths of our study stem from our large, diverse cohort inclusive of many sites of COVID-19 infection as well as the robustness of our results across multiple statistical modeling techniques. Our results may be limited by confounding. However, we adjusted for several potential patient- and hospital-level confounders, selected a priori, and attempted to address unmeasured confounding through our DiD study design. Still, we cannot test whether other unmeasured differences exist between patients exposed to surge conditions – or the care they received – and those not exposed. Additionally, the non-statistical significance of several of our analytic results likely stems from their sample size, but may actually represent true null results. Furthermore, our cohort included only patients admitted early in the pandemic; it is unknown if our findings would differ if we had included patients hospitalized later in the pandemic (eg, with different treatment approaches, vaccinations, etc). Also, we defined our exposure, surge, based on the caseload of COVID-19 patients on the day of each patient's ICU admission rather than a larger portion of the ICU stay. We also were unable to include non-COVID-19 ICU patients in our calculations of ICU occupancy. Finally, our study was not able to identify what specific aspects of surge conditions drive the association with worse outcomes.
Our findings are consistent with those from two other retrospective studies. The first, a cohort of COVID-19 ICU admissions to VA hospitals, found higher ICU caseload during a patient's hospitalization was associated with increased death (hazard ratio [95% CI] of COVID-19 ICU caseload >100% vs. ≤25% of baseline ICU capacity: 2.35 [1.25-4.39]).17 The second, using administrative data from a 558 U.S. hospitals’ admissions (not focused specifically on ICU patients) found a dose-response in the increased odds of death associated with degrees of surge.38 Both studies were limited, however, by non-adjustment for temporal changes in casemix or practice patterns as the difference-in-differences approach we employed does.
Conclusion
As the COVID-19 pandemic has proven, novel infections pose an existential threat to the health of the nation. Having shown the potential impact on survival of allowing health systems to operate in suboptimal conditions, our work highlights that pandemic preparedness extends far beyond ventilator stockpiling. Readiness for the next pandemic will require investments that are commensurate with the threat.
Supplemental Material
Supplemental material, sj-docx-1-jicm-10.1177_08850666211067509 for Association of Surge Conditions with Mortality Among Critically Ill Patients with COVID-19 by Adam B. Keene, Andrew J. Admon, Samantha K. Brenner, Shruti Gupta, Deepa Lazarous, David E. Leaf, Hayley B. Gershengorn and in Journal of Intensive Care Medicine
Acknowledgments
AJA is an employee of the VA Ann Arbor Healthcare System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Participants in Study Group
The STOP-COVID Investigators include (* Site Principal Investigator):
Baylor College of Medicine: Carl P. Walther*, Samaya J. Anumudu; Baylor University Medical Center: Justin Arunthamakun*, Kathleen F. Kopecky, Gregory P. Milligan, Peter A. McCullough, Thuy-Duyen Nguyen; Beth Israel Deaconess Medical Center: Shahzad Shaefi,* Brian P. O’Gara, Megan L. Krajewski, Sean M. Baskin, Sidharth Shankar, Juan D. Valencia, Ameeka Pannu, Margaret M. Hayes, E. Wilson Grandin; Boston Medical Center: Sushrut S. Waikar*, Zoe A. Kibbelaar; Cook County Health: Ambarish M. Athavale*, Peter Hart, Shristi Upadhyay, Ishaan Vohra, Ajiboye Oyintayo; Cooper University Health Care: Adam Green*, Jean-Sebastien Rachoin, Christa A. Schorr, Lisa Shea; Duke University Medical Center: Daniel L. Edmonston*, Christopher L. Mosher; Hackensack Meridian Health Mountainside Medical Center: Alexandre M. Shehata*, Zaza Cohen, Valerie Allusson, Gabriela Bambrick-Santoyo, Noor ul aain Bhatti, Bijal Mehta, Aquino Williams; Hackensack Meridian Health Hackensack University Medical Center: Samantha K. Brenner*, Patricia Walters, Ronaldo C. Go, Keith M. Rose; Harvard T.H. Chan School of Public Health: Miguel A. Hernán; Harvard University: Rebecca Lisk; Icahn School of Medicine at Mount Sinai: Lili Chan*, Kusum S. Mathews*, Steven G. Coca, Deena R. Altman, Aparna Saha, Howard Soh, Huei Hsun Wen, Sonali Bose, Emily A. Leven, Jing G. Wang, Gohar Mosoyan, Girish N. Nadkarni, Pattharawin Pattharanitima, Emily J. Gallagher; Indiana University School of Medicine/Indiana University Health: Allon N. Friedman*, John Guirguis, Rajat Kapoor, Christopher Meshberger, Katherine J. Kelly; Johns Hopkins Hospital: Chirag R. Parikh*, Brian T. Garibaldi, Celia P. Corona-Villalobos, Yumeng Wen, Steven Menez, Rubab F. Malik, Carmen Elena Cervantes, Samir C. Gautam; Kings County Hospital Center: Mary C. Mallappallil*, Jie Ouyang, Sabu John, Ernie Yap, Yohannes Melaku, Ibrahim Mohamed, Siddhartha Bajracharya, Isha Puri, Mariah Thaxton, Jyotsna Bhattacharya, John Wagner, Leon Boudourakis; Loma Linda University: H. Bryant Nguyen*, Afshin Ahoubim; Mayo Clinic, Arizona: Leslie F. Thomas*, Dheeraj Reddy Sirganagari; Mayo Clinic, Florida: Pramod K. Guru*; Mayo Clinic, Rochester: Kianoush Kashani*, Shahrzad Tehranian; Medical College of Wisconsin: Yan Zhou,* Paul A. Bergl, Jesus Rodriguez, Jatan A. Shah, Mrigank S. Gupta; MedStar Georgetown University Hospital: Princy N. Kumar*, Deepa G. Lazarous, Seble G. Kassaye; Montefiore Medical Center/Albert Einstein College of Medicine: Michal L. Melamed*, Tanya S. Johns. Ryan Mocerino, Kalyan Prudhvi, Denzel Zhu, Rebecca V. Levy, Yorg Azzi, Molly Fisher, Milagros Yunes, Kaltrina Sedaliu, Ladan Golestaneh, Maureen Brogan, Neelja Kumar, Michael Chang, Jyotsana Thakkar; New York-Presbyterian Queens Hospital: Ritesh Raichoudhury*, Akshay Athreya, Mohamed Farag; New York-Presbyterian/Weill Cornell Medical Center: Edward J. Schenck*, Soo Jung Cho, Maria Plataki, Sergio L. Alvarez-Mulett, Luis G. Gomez-Escobar, Di Pan, Stefi Lee, Jamuna Krishnan, William Whalen; New York University Langone Hospital: David Charytan*, Ashley Macina, Sobaata Chaudhry, Benjamin Wu, Frank Modersitzki; Northwestern Memorial Hospital: Northwestern University Feinberg School of Medicine - Anand Srivastava*, Alexander S. Leidner, Carlos Martinez, Jacqueline M. Kruser, Richard G. Wunderink, Alexander J. Hodakowski; Ochsner Medical Center: Juan Carlos Q. Velez*, Eboni G. Price-Haywood, Luis A. Matute-Trochez, Anna E. Hasty, Muner MB. Mohamed; Oregon Health and Science University Hospital: Rupali S. Avasare*, David Zonies*; Partners Healthcare: Brigham and Women's Hospital, Brigham and Women's Faulkner Hospital, Massachusetts General Hospital, and Newton Wellesley Hospital - David E. Leaf*, Shruti Gupta*, Meghan E. Sise, Erik T. Newman, Samah Abu Omar, Kapil K. Pokharel, Shreyak Sharma, Harkarandeep Singh, Simon Correa, Tanveer Shaukat, Omer Kamal, Wei Wang, Heather Yang, Jeffery O. Boateng, Meghan Lee, Ian A. Strohbehn, Jiahua Li, Ariel L. Mueller; ProMedica Health System: Roberta E. Redfern,* Nicholas S. Cairl, Gabriel Naimy, Abeer Abu-Saif, Danyell Hall, Laura Bickley; Renown Health: Chris Rowan*, Farah Madhani-Lovely*; Rush University Medical Center: Vasil Peev*, Jochen Reiser, John J. Byun, Andrew Vissing, Esha M. Kapania, Zoe Post, Nilam P. Patel, Joy-Marie Hermes; Rutgers/New Jersey Medical School: Anne K. Sutherland*, Amee Patrawalla, Diana G. Finkel, Barbara A. Danek, Sowminya Arikapudi, Jeffrey M. Paer, Peter Cangialosi, Mark Liotta; Rutgers/Robert Wood Johnson Medical School: Jared Radbel*, Sonika Puri, Jag Sunderram, Matthew T. Scharf, Ayesha Ahmed, Ilya Berim, Jayanth S. Vatson; Stanford Healthcare: Stanford University School of Medicine – Shuchi Anand*, Joseph E. Levitt, Pablo Garcia; Temple University Hospital: Suzanne M. Boyle*, Rui Song, Ali Arif; Thomas Jefferson Health: Jingjing Zhang*, Sang Hoon Woo, Xiaoying Deng, Goni Katz-Greenberg, Katharine Senter; Tulane Medical Center: Moh’d A. Sharshir*, Vadym V. Rusnak; United Health Services Hospitals: Muhammad Imran Ali, Terri Peters, Kathy Hughes; University of Colorado Anschutz Medical Campus: Anip Bansal*, Amber S. Podoll, Michel Chonchol, Sunita Sharma, Ellen L. Burnham; University Hospitals Cleveland Medical Center: Arash Rashidi*, Rana Hejal; University of Alabama-Birmingham Hospital: Eric Judd*, Laura Latta, Ashita Tolwani; University of California-Davis Medical Center: Timothy E. Albertson*, Jason Y. Adams; University of California-Los Angeles Medical Center: Ronald Reagan-UCLA Medical Center - Steven Y. Chang*, Rebecca M. Beutler; Santa Monica-UCLA Medical Center – Carl E. Schulze; University of California-San Diego Medical Center: Etienne Macedo*, Harin Rhee; University of California-San Francisco Medical Center: Kathleen D. Liu*, Vasantha K. Jotwani; University of Chicago Medical Center: Jay L. Koyner*, Alissa Kunczt; University of Florida Health-Gainesville: Chintan V. Shah*; University of Florida-Health-Jacksonville: Vishal Jaikaransingh*; University of Illinois Hospital and Health Sciences System: Stephanie M. Toth-Manikowski*, Min J. Joo*, James P. Lash; University of Kentucky Medical Center: Javier A. Neyra*, Nourhan Chaaban, Madona Elias, Yahya Ahmad; University Medical Center of Southern Nevada: Rajany Dy*, Alfredo Iardino, Elizabeth H. Au, Jill H. Sharma; University of Miami Health System: Marie Anne Sosa*, Sabrina Taldone, Gabriel Contreras, David De La Zerda, Alessia Fornoni, Hayley B. Gershengorn; University of Michigan: Salim S. Hayek*, Pennelope Blakely, Hanna Berlin, Tariq U. Azam, Husam Shadid, Michael Pan, Patrick O” Hayer, Chelsea Meloche, Rafey Feroze, Kishan J. Padalia, Abbas Bitar, Jeff Leya, John P. Donnelly, Andrew J. Admon; University of North Carolina School of Medicine: Jennifer E. Flythe*, Matthew J. Tugman, Emily H. Chang; University of Oklahoma Health Sciences Center: Brent R. Brown*; University of Pennsylvania Health System: Amanda K. Leonberg-Yoo*, Ryan C. Spiardi, Todd A. Miano, Meaghan S. Roche, Charles R. Vasquez; University of Pittsburgh Medical Center: Amar D. Bansal*, Natalie C. Ernecoff, Sanjana Kapoor, Siddharth Verma, Huiwen Chen; University of Tennessee Health Science Center and Memphis VA Medical Center/Methodist University Hospital – Csaba P. Kovesdy*, Miklos Z. Molnar*, Ambreen Azhar; University of Texas Southwestern Medical Center and Parkland Health and Hospital System: S. Susan Hedayati*, Mridula V. Nadamuni, Shani Shastri, Duwayne L. Willett; University of Vermont Larner College of Medicine: Samuel A.P. Short; University of Virginia Health System: Amanda D. Renaghan*, Kyle B. Enfield; University of Washington Medical Center: Pavan K. Bhatraju*, A. Bilal Malik; Vanderbilt University Medical Center: Matthew W. Semler; Washington University in St. Louis/Barnes Jewish Hospital: Anitha Vijayan*, Christina Mariyam Joy, Tingting Li, Seth Goldberg, Patricia F. Kao; Wellforce Health System: Lowell General Hospital - Greg L. Schumaker*, Tufts Medical Center - Nitender Goyal*, Anthony J. Faugno, Greg L. Schumaker, Caroline M. Hsu, Asma Tariq, Leah Meyer, Ravi K. Kshirsagar, Aju Jose, Daniel E. Weiner; Westchester Medical Center: Marta Christov*, Savneek Chugh, Jennifer Griffiths, Sanjeev Gupta, Aromma Kapoor, Savneek Chugh; Yale School of Medicine: Perry Wilson,* Tanima Arora, Ugochukwu Ugwuowo.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: HBG receives funding from the University of Miami Hospital and Clinics in support of the UHealth-DART Research Group. AJA receives funding from the National Institutes of Health / National Heart, Lung, and Blood Institute. The funders had no role in the design, execution, or presentation of the study. ABK, SKB, SG, DL, and DEL received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: HBG serves on COVID-19 Advisory Boards for Gilead Sciences, Inc.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Heart, Lung, and Blood Institute (grant number K08HL155407-01, n/a).
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
ORCID iDs: Adam B. Keene https://orcid.org/0000-0003-3382-7146
Hayley B. Gershengorn https://orcid.org/0000-0002-7360-2489
Supplemental Material: Supplemental material for this article is available online.
References
- 1.World Health Organization. Novel Coronavirus (2019-nCoV) Situation Report 1; 2021.
- 2.Belluck P, Weiland N. C.D.C. Officials Warn of Coronavirus Outbreaks in the U.S. The New York Times; 2020.
- 3.Coronavirus now spreading faster outside China. BBC News; 2020.
- 4.Kobokovich A. Ventilator stockpiling and availability in the US: Johns Hopkins Center for Health Security; 2020.
- 5.Ranney ML, Griffeth V, Jha AK. Critical supply shortages - The need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med. Apr 2020;382(18):e41. [DOI] [PubMed] [Google Scholar]
- 6.Widdicombe L. The coronavirus pandemic peaks in New York's Hospitals. The New Yorker. April 15 2020. [Google Scholar]
- 7.Keene AB, Shiloh AL, Eisen L, et al. Critical care surge during the COVID-19 pandemic: implementation and feedback from frontline providers. J Intensive Care Med. Feb 2021;36(2):233‐240. [DOI] [PubMed] [Google Scholar]
- 8.Gershengorn HB. ICU capacity is more about the clinicians than the number of beds. statnews.com; 2020.
- 9.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 07 2020;180(7):934‐943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323(20):2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 04 2020;323(16):1612‐1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrot L, Asfar P, Mauny F, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 03 2020;382(11):999‐1008. [DOI] [PubMed] [Google Scholar]
- 13.Beitler JR, Sarge T, Banner-Goodspeed VM, et al. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy versus an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 03 2019;321(9):846‐857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moss M, Huang DT, Brower RG, et al. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 05 2019;380(21):1997‐2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fowler AA, Truwit JD, Hite RD, et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: the CITRIS-ALI randomized clinical trial. JAMA. 10 2019;322(13):1261‐1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wendel Garcia PD, Fumeaux T, Guerci P, et al. Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: initial report of the international RISC-19-ICU prospective observational cohort. EClinicalMedicine. Aug 2020;25:100449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Auld SC, Caridi-Scheible M, Blum JM, et al. ICU and ventilator mortality among critically ill adults with coronavirus disease 2019. Crit Care Med. 09 2020;48(9):e799‐e804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US department of veterans affairs hospitals during the COVID-19 pandemic. JAMA Netw Open. 01 2021;4(1):e2034266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gupta S, Hayek SS, Wang W, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;180(11):1436–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vincent JL, Moreno R, Takala J, et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. Jul 1996;22(7):707‐710. [DOI] [PubMed] [Google Scholar]
- 21.American Hospital Association Regions. American Hospital Association. Accessed February 1, 2021. Available at: https://www.ahvrp.org/sites/default/files/aha-regional-map.pdf [Google Scholar]
- 22.Stuart EA, Huskamp HA, Duckworth K, et al. Using propensity scores in difference-in-differences models to estimate the effects of a policy change. Health Serv Outcomes Res Methodol. Dec 2014;14(4):166‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanner-Smith EE, Tipton E. Robust variance estimation with dependent effect sizes: practical considerations including a software tutorial in stata and spss. Res Synth Methods. Mar 2014;5(1):13‐30. [DOI] [PubMed] [Google Scholar]
- 24.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002 Oct 23-30 2002;288(16):1987‐1993. [DOI] [PubMed] [Google Scholar]
- 25.Dang D, Johantgen ME, Pronovost PJ, Jenckes MW, Bass EB. Postoperative complications: does intensive care unit staff nursing make a difference? Heart Lung. 2002 May-Jun 2002;31(3):219‐228. [DOI] [PubMed] [Google Scholar]
- 26.McGahan M, Kucharski G, Coyer F. Elsevier WABNRPsb. Nurse staffing levels and the incidence of mortality and morbidity in the adult intensive care unit: a literature review. Aust Crit Care. May 2012;25(2):64‐77. [DOI] [PubMed] [Google Scholar]
- 27.Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Crit Care Med. Jul 2010;38(7):1521‐1528. quiz 1529. [DOI] [PubMed] [Google Scholar]
- 28.Gershengorn HB, Harrison DA, Garland A, Wilcox ME, Rowan KM, Wunsch H. Association of intensive care unit patient-to-intensivist ratios with hospital mortality. JAMA Intern Med. Mar 2017;177(3):388‐396. [DOI] [PubMed] [Google Scholar]
- 29.Dara SI, Afessa B. Intensivist-to-bed ratio: association with outcomes in the medical ICU. Chest. Aug 2005;128(2):567‐572. [DOI] [PubMed] [Google Scholar]
- 30.Wilcox ME, Chong CA, Niven DJ, et al. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. Oct 2013;41(10):2253‐2274. [DOI] [PubMed] [Google Scholar]
- 31.Kashiouris MG, Sessler CN, Qayyum R, et al. Near-simultaneous intensive care unit (ICU) admissions and all-cause mortality: a cohort study. Intensive Care Med. 11 2019;45(11):1559‐1569. [DOI] [PubMed] [Google Scholar]
- 32.Neuraz A, Guérin C, Payet C, et al. Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit Care Med. Aug 2015;43(8):1587‐1594. [DOI] [PubMed] [Google Scholar]
- 33.Gabler NB, Ratcliffe SJ, Wagner J, et al. Mortality among patients admitted to strained intensive care units. Am J Respir Crit Care Med. Oct 2013;188(7):800‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhonagiri D, Pilcher DV, Bailey MJ. Increased mortality associated with after-hours and weekend admission to the intensive care unit: a retrospective analysis. Med J Aust. Mar 2011;194(6):287‐292. [DOI] [PubMed] [Google Scholar]
- 35.Groenland CNL, Termorshuizen F, Rietdijk WJR, et al. Emergency department to ICU time is associated with hospital mortality: a registry analysis of 14,788 patients from six university hospitals in the Netherlands. Crit Care Med. 11 2019;47(11):1564‐1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang Z, Bokhari F, Guo Y, Goyal H. Prolonged length of stay in the emergency department and increased risk of hospital mortality in patients with sepsis requiring ICU admission. Emerg Med J. Feb 2019;36(2):82‐87. [DOI] [PubMed] [Google Scholar]
- 37.Butler CR, Wong SPY, Wightman AG, O’Hare AM. US clinicians’ experiences and perspectives on resource limitation and patient care during the COVID-19 pandemic. JAMA Netw Open. 11 2020;3(11):e2027315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kadri SS, Sun J, Lawandi A, et al. Association between caseload surge and COVID-19 survival in 558 U.S. hospitals, March to August 2020. Ann Intern Med. Jul 06 2021.174(9):1240–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jicm-10.1177_08850666211067509 for Association of Surge Conditions with Mortality Among Critically Ill Patients with COVID-19 by Adam B. Keene, Andrew J. Admon, Samantha K. Brenner, Shruti Gupta, Deepa Lazarous, David E. Leaf, Hayley B. Gershengorn and in Journal of Intensive Care Medicine