Abstract
Background
The COVID-19 pandemic raised major challenges to the management of patient flows and medical staff resource allocation. To prevent the collapse of medical facilities, elective diagnostic and surgical procedures were drastically reduced, canceled or rescheduled.
Methods
We recorded all in-hospital treated patients and outpatient clinics visits of our neurosurgical department from March 2017 to February 2021. Changes of OR capacity, in-hospital neurosurgical treatments and outpatient clinics visits during the pandemic episode was compared on a monthly bases to the previous years.
Results
A total of 3′214 data points from in-house treated patients and 11′400 outpatient clinics visits were collected. The ratio of elective (73.5% ± 1.5) to emergency surgeries (26.5% ± 1.5) remained unchanged from 2017 to 2021. Significantly less neurosurgical interventions were performed in April 2020 (−42%), significantly more in July 2020 (+36%). Number of outpatient clinics visits remained in the expected monthly range (mean n = 211 ± 67). Total OR capacity was reduced to 30% in April 2020 and 55% in January 2021. No significant delay of urgent surgical treatments was detected during restricted (<85%) OR capacity. On average, the delay of rescheduled consultations was 58 days (range 3 – 183 days), three (6.5%) were referred as emergencies.
Conclusions
Dynamic monitoring and adjustment of resources is essential to maintain surgical care. The sharp restrictions of surgical activities resulted in significant fluctuations and 5% decrease of treated neurosurgical patients during the COVID-19 pandemic. However, urgent neurosurgical care was assured without significant time delay during periods of reduced OR capacity.
Abbreviations: FOPH, federal office of public health; HRA, Human Research Act; ICU, Intensive Care Unit; OR, operating room
Keywords: Hospital outpatient clinics, Neurosurgery, Non-COVID-19 patients, Operating room capacity, Pandemic care management
1. Introduction
The COVID-19 pandemic has led to major changes in patient and staff resources management worldwide [1], [2], [3]. Elective surgeries, routine diagnostics and time of in-hospital stays were reduced in the interest of patient safety and as a measure to prevent the collapse of medical institutions [4], [5]. The expected onslaught of COVID-19 positive patients resulted in a reduction of elective surgical activities to free up beds in the ward and Intensive Care Unit (ICU) [3]. In addition, the postoperative recovery areas and operating rooms were repurposed as overflow ICUs. Surgeons and operating room (OR) teams were reassigned to support other critical areas of the hospital. Continued suspension of scheduled, non-emergent outpatient visits shifted freed-up staff resources to the COVID-19 triage and screening centers [2].
However, the insufficiency of facility and staff resources during the pandemic with consequent cancelling of elective operations hazards the high standards of elective care to patients with an extensive impact on patients and the healthcare system overall [1], [4]. The delay of urgent surgeries results in worsening of health conditions and quality of life, increased social costs and probably unnecessary deaths [6], [7], [8], [9]. Surgical disciplines had to define and implement triage strategies within a very short time during the pandemic in order to cope with the ongoing surge of urgent operations of non-COVID-19 patients [1], [10]. This study aimed to quantify OR capacity resources, the changes as well as fluctuations of neurosurgical treated patients and outpatient clinics visits during the global COVID-19 pandemic in 2020 and 2021 compared to previous years. Further we compared the time-delay of urgent cranial and spinal surgical operations during the pandemic episode in times of “reduced (<85%)” and “normal (>85%)” OR capacity.
2. Materials and Methods
All consecutive outpatient clinics visits and number of in-hospital treated neurosurgical patients at our institution from March 2017 to February 2021 were retrospectively enrolled. We compared the data of the pandemic episode (March 2020 to February 2021) on a monthly bases to the corresponding month of the previous three years (March 2017 to February 2020). Numbers of surgical and conservatively treated neurosurgical in-hospital patients were recorded as well as site of pathology (cranial, spinal, other) and the ratio of elective to emergency treatments. Cancelled and rescheduled outpatient clinics visits were analyzed as well as the delay of consultations caused by the restrictions during the pandemic year. Descriptive statistics for continuous variables were reported as means (±standard deviation [σ]). A value ± 2σ was considered as an outlier value and hence statistically significant. Furthermore, the delay of urgent neurosurgical treatment of cranial and spinal pathologies during reduced (<85%) and normal (>85%) OR capacity was analyzed. Statistical analyses and graphical illustrations were performed using GraphPad 8.1 software (GraphPad Software, La Jolla California USA). The unpaired, nonparametric Mann-Whitney test was used for group comparison. All patient visits and the number of surgical procedures were obtained from the hospital's administrative databases in anonymized form without individual patient data. The research project did not fall within the scope of the Human Research Act (HRA) and was therefore approved by the Cantonal Ethics Committee of Zurich (BASEC-Nr. Req-2021-01067). The data of COVID-19 infections in Switzerland was acquired from the federal office of public health (FOPH, online source, https://www.bag.admin.ch/bag/en/home, Mai 2021). We used the STROBE checklist as study guideline [11].
3. Results
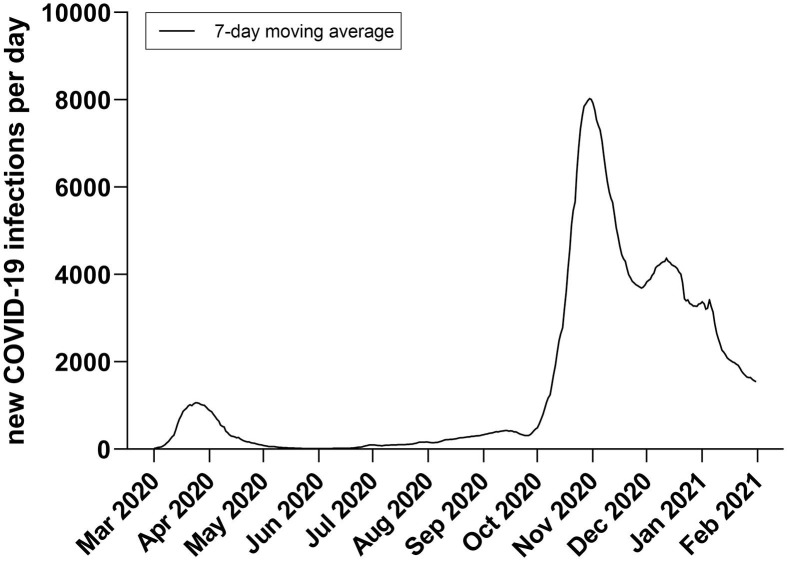
A total of 3′214 data points from in-house treated patients and 11′400 outpatient clinics visits were collected. A first (March to May 2020) and second (October 2020 to January 2021) COVID-19 infection peak was detected in Switzerland. During the first wave, the daily new COVID-19 infections peaked at 1065 cases and 8029 during the second wave (Fig. 1 ). Our department experienced an overall 5% decrease in neurosurgical treated patients during the global pandemic episode from March 2020 to February 2021 (Table 1 ). This compares to the previous episodes, which saw an annual increase of 15.7% and 6.5%. The continuous average annual increase of 2.0% in the treatment of cranial pathologies (brain tumors) remained during the pandemic. The ratio of elective surgeries (73.5% ± 1.5) to emergencies (26.5% ± 1.5) did not change.
Fig. 1.
7-day moving average of daily new COVID-19 infections in Switzerland from March 2020 to February 2021 showing the first (peak n = 1065 end of March 2020) and second wave (peak n = 8029 begin of November 2020).
Table 1.
Neurosurgical treated in-hospital patients cohort from March 2017 to February 2021. There was a decrease of 5% in patient volume during the COVID-19 pandemic episode (March 2020 – February 2021) without significant changes in hospital allocation and pathology mix distribution over the last 4 years.
| Mar 2017 - Feb 2018 | Mar 2018 - Feb 2019 | Mar 2019 - Feb 2020 | Mar 2020 - Feb 2021 | |
|---|---|---|---|---|
| Patients treated (n) | 704 | 815 | 868 | 827 |
| surgical (n, [%]) | 563 [80] | 668 [82] | 684 [79] | 645 [78] |
| conservative (n, [%]) | 141 [20] | 147 [18] | 184 [21] | 182 [22] |
| Hospital allocation | ||||
| elective (n, [%]) | 507 [72] | 604 [74] | 647 [75] | 604 [73] |
| emergencies (n, [%]) | 197 [28] | 211 [26] | 221 [25] | 223 [27] |
| Pathology | ||||
| cranial (n, [%]) | 141 [20] | 187 [23] | 201 [25] | 223 [27] |
| brain tumors (n, [%]) | 45 [32] | 64 [34] | 72 [36] | 67 [39] |
| head trauma, ICB (n, [%]) | 78 [55] | 101 [54] | 109 [54] | 136 [60] |
| other cranial (n, [%]) | 18 [13] | 22 [12] | 20 [10] | 27 [11] |
| spinal (n, [%]) | 549 [78] | 609 [75] | 630 [73] | 587 [71] |
| stenosis / disc herniation (n, [%]) | 433 [79] | 469 [77] | 478 [76] | 440 [74] |
| spine trauma (n, [%]) | 93 [17] | 79 [13] | 95 [15] | 97 [16] |
| other spine (n, [%]) | 23 [4] | 61 [10] | 57 [9] | 60 [10] |
| other, interdisciplinary (n, [%]) | 14 [2] | 19 [2] | 37 [2] | 17 [2] |
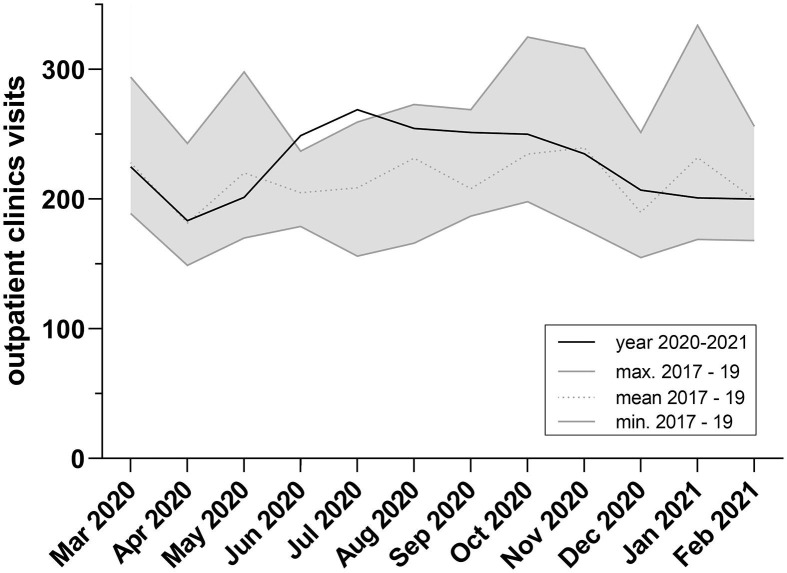
Monthly outpatient clinics visits during the global COVID-19 pandemic showed no outliers and stayed in the expected range (mean n = 211, σ ± 67) (Fig. 2 ). Of n = 714 planned consultations in March, April and November 2020 combined, n = 59 (8.3%) were cancelled and n = 46 (6.4%) rescheduled after medical consultation by phone (Table 2 ). On average the delay of rescheduled consultations was 58 days (range 3 – 183 days). Three (6.5%) of the rescheduled patients were referred as emergencies in the course of the pandemic due to immobilizing pain caused by spinal pathologies.
Fig. 2.
Outpatient clinics visits on a monthly basis from 2017 to 2021 - no significant outlier month (±2σ, mean n = 211, σ ± 67) was detected during the COVID-19 pandemic episode.
Table 2.
From planed n = 513 outpatient clinics consultations in March and April 2020, n = 105 (20.5%) were cancelled or rescheduled. Overall delay of rescheduled consultations was 60 days (range 3–183 days). During the second COVID-19 wave (November 2020), only n = 7 (3.5%) of scheduled consultations were cancelled.
| Month | Planed consultations | Cancelled initial consultations | Cancelled follow ups | Rescheduled initial consultations | Rescheduled follow ups | Delay of rescheduled consultations (days) |
|---|---|---|---|---|---|---|
| Mar 2020 | n = 295 | 12 (4.1%) | 24 (8.1%) | 18 (6.1%) | 16 (5.4%) | 64 (range 3–183) |
| Apr 2020 | n = 218 | 7 (3.2%) | 16 (7.3%) | 6 (2.8%) | 6 (2.8%) | 52 (range 7–105) |
| Nov 2020 | n = 201 | 0 | 7 (3.5%) | 0 | 0 | n/a |
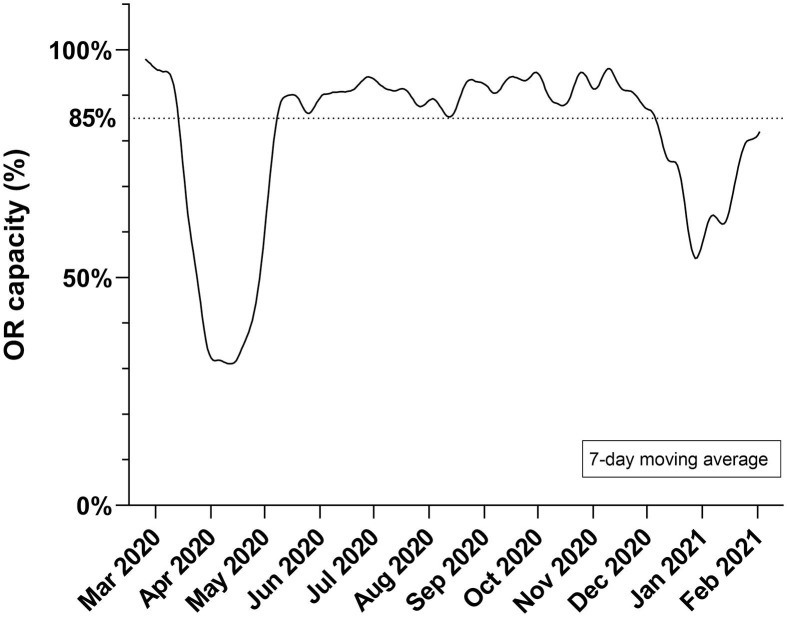
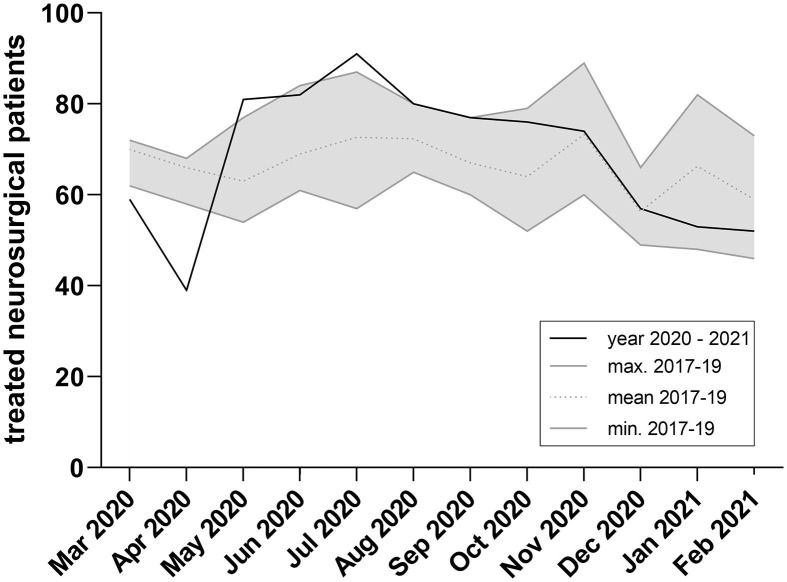
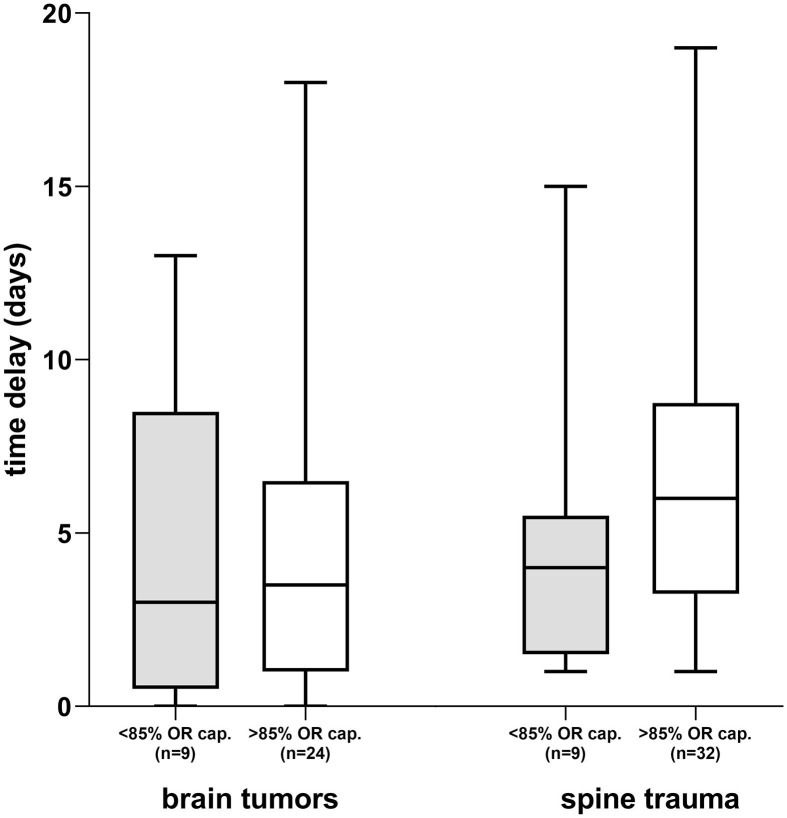
Due to the operational restrictions during the pandemic, OR capacity was reduced to an all-time low of 30% in April 2020 and to 55% in January 2021 (Fig. 3 ). Hence, significantly less neurosurgical patients (n = 39, −42%) were treated in our department in April 2020 compared to an expected monthly average of 67 patients (σ ± 11) in the last three years. In contrast, significantly more neurosurgical patients underwent neurosurgical treatment in July 2020 (n = 91, +36%) after guidelines for elective surgical activities were relaxed (Fig. 4 ). Urgent neurosurgical treatment of cranial or spinal pathologies were not significantly postponed during times of operational restrictions (OR capacity < 85%) compared to periods of normal surgical activities (OR capacity > 85%). Patients with symptomatic brain tumors were treated on average after 3 days of initial diagnosis during reduced OR capacity and 3.5 days during normal OR capacity (p = 0.928, 95% CI: −4 to 4). Accordingly, no significant delay (p = 0.069, 95% CI: 0 to 5) of neurosurgical treatment of spine pathologies was detected (Fig. 5 ).
Fig. 3.
OR capacity during COVID-19 with capacity reduction in April 2020 (all-time low of 30%) and in January 2021 (55%). Normal OR capacity utilization remained above 85% from mid Mai to mid December 2020.
Fig. 4.
Treated neurosurgical patients at our institution from 2017 to 2021 (mean n = 67, σ ± 11). Significantly less patients were treated in April (n = 39), significantly more in July 2021 (n = 91).
Fig. 5.
During reduced OR capacity (<85%), neither in brain tumor (p = 0.928) nor spine trauma (p = 0.069) patients a significant delay from initial diagnosis to urgent operative treatment was detected (excluded patients / outliers n = 13).
4. Discussion
The dynamic shift and monitoring of resources was, and still is, necessary to prevent the collapse of the health care system during the global COVID-19 pandemic. The aim of this study was to evaluate the accessibility to the neurosurgical resources during the first waves of the COVID-19 epidemic, when the reduction of surgical procedures was at the center of public health policies. To deal with the neurosurgical patients requiring an operative treatment or a clinic visit the judiciously making use of the available resources was essential. At our neurosurgery department, the limited access to elective surgeries was reflected by an overall decrease of −5% in the pandemic year compared to a steady increase the years prior (+15.7%, +6.5%). The fear of uncertainty in the beginning of the pandemic resulted in an abrupt reduction of elective surgeries and outpatient clinics visits. The significant decrease of patients treated (−42%) in our neurosurgical department in April 2020 is comparable with the known literature. Hübner et al. recorded a 43% decrease of elective visceral surgical procedures in the beginning of the pandemic, while the urgent operations decreased by 39% [9]. Dinmohamed et al. showed a notable decrease in skin cancer diagnoses compared to the period before the COVID-19 outbreak [12]. Other Neurosurgery centers reported an operative volume that was only modestly diminished and essential neurosurgical needs were unaffected [1], [7]. However, long-term data of larger centers does not exist. Overall, our data showed that i) ratio of cranial to spinal operative cases, ii) ratio of emergency to elective patients and iii) pathology case-mix did not significantly change and stabilized on levels compared to prior years.
Under normal (>85%) and reduced (<85%) OR capacity utilization, we did not observe any significant delay in urgent neurosurgical treatment of patients with brain tumors (p = 0.928) or spinal trauma (p = 0.069). Neurosurgical treatments of acute life-threatening emergencies were continued unaltered and hence not affected by OR capacity reduction. Our findings are comparable with the report of Wali et al. where neuro-oncological surgeries with high risk of a permanent or progressive neurological deficits or substantial threat to life remained unchanged during first stages of the pandemic [7]. Ashkan et al. reported that, by shifting additional surgical capacity to the private health sector, urgent neurovascular or neuro-oncological treatments in public health facilities were not delayed [1].
At the time of writing, the COVID-19 pandemic is still on the surge and the next wave of infections is expected. Although vaccination programs have been launched around the world, the healthcare sector remains under pressure to provide medical care for non-COVID-19 and COVID-19 patients. New variants of the COVID-19 virus, geopolitical and socioeconomic tensions are unknown factors to reliably predict future developments [13], [14]. Therefore, it is necessary to monitor and dynamically adjust medical resources in order to quickly detect changes in the current situation and avoid the risk of large patient fluctuations.
As a tertiary referral center of neurosurgical patients, we are aware of the limitation of this study i.e. small sample size and retrospective design. We further did not analyze the impact on mortality during the pandemic year. Unknown factors not mentioned in this report may have influenced our findings.
5. Conclusion
Overall, in this retrospective observational study performed in a single tertiary care center, the number of patients treated in our neurosurgery department decreased by 5% from March 2020 to February 2021 compared to the year 2019. The accessibility to neurosurgical procedures of non-COVID-19 patients during the first waves of the COVID-19 pandemic did not differ significantly from the availableness during the previous year, because of the flexibility and reorganization of the health system. The severe shortening of surgical activities during the first half of the COVID-19 pandemic year resulted in significant fluctuations in neurosurgical patients treated. Effective and dynamic adjustment of OR capacity during the second COVID-19 wave did not result in significant outlier months in neurosurgical patient volume. No significant delay of urgent neurosurgical treatments was observed during the periods of OR capacity reduction. Dynamic monitoring and adjustment of medical resources allowed for the reduction of major patient fluctuations, the provision of medical care, and the prevention of the impending collapse of the health care system.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Daniel Schöni: Conceptualization, Methodology, Software, Data curation, Writing – original draft, Writing – review & editing. Marc-Eric Halatsch: Data curation, Writing – original draft, Supervision. Alex Alfieri: Supervision, Validation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ashkan K., Jung J., Velicu A.M., Raslan A., Faruque M., Kulkarni P., Bleil C., Hasegawa H., Kailaya-Vasan A., Maratos E., Grahovac G., Vergani F., Zebian B., Barazi S., Malik I., Bell D., Walsh D., Bhangoo R., Tolias C., Bassi S., Selway R., Thomas N., Chandler C., Gullan R. Neurosurgery and coronavirus: impact and challenges—lessons learnt from the first wave of a global pandemic. Acta Neurochir. (Wien). 2021;163(2):317–329. doi: 10.1007/s00701-020-04652-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mallah S.I., Ghorab O.K., Al-Salmi S., Abdellatif O.S., Tharmaratnam T., Iskandar M.A., Sefen J.A.N., Sidhu P., Atallah B., El-Lababidi R., Al-Qahtani M. COVID-19: breaking down a global health crisis. Ann. Clin. Microbiol. Antimicrob. 2021;20(1) doi: 10.1186/s12941-021-00438-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spinelli A., Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br. J. Surg. 2020;107(7):785–787. doi: 10.1002/bjs.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santi L., Golinelli D., Tampieri A., Farina G., Greco M., Rosa S., Beleffi M., Biavati B., Campinoti F., Guerrini S., Ferrari R., Rucci P., Fantini M.P., Giostra F., Manzoli L. Non-COVID-19 patients in times of pandemic: Emergency department visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS One. 2021;16(3 March):1–14. doi: 10.1371/journal.pone.0248995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vanni G., Legramante J.M., Pellicciaro M., De carolis G., Cotesta M., Materazzo M., Buonomo C., Farinaccio A., Santori F., Saraceno F., Ielpo B., Aiello F., Paganelli C., Grande M., De andreis G., Chiocchi M., Palombi L., Buonomo O.C. Effect of lockdown in surgical emergency accesses: Experience of a COVID-19 hospital. In Vivo (Brooklyn) 2020;34(5) doi: 10.21873/invivo.12137. 3033-3038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agarwal N., Raheja A., Suri A. Guidelines for Preoperative testing for neurosurgery in coronavirus disease 2019 (COVID-19) era: indian viewpoint amidst global practice. World Neurosurg. 2021;146(January):103–112. doi: 10.1016/j.wneu.2020.10.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wali A.R., Ryba B.E., Kang K., Santiago-Dieppa D.R., Steinberg J., Diaz-Aguilar L.D., Stone L.E., Brandel M.G., Longhurst C.A., Taylor W., Khalessi A.A. Impact of COVID-19 on a neurosurgical service: lessons from the university of California San Diego. World Neurosurg. 2021;148:e172–e181. doi: 10.1016/j.wneu.2020.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rommel A., von der Lippe E., Plaß D., Ziese T., Diercke M., an der Heiden M., Haller S., Wengler A. The COVID-19 Disease Burden in Germany in 2020. Dtsch Arztebl Int. 2021;118(9):145–151. doi: 10.3238/arztebl.m2021.0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hübner M., Zingg T., Martin D., Eckert P., Demartines N., Ashkenazi I. Surgery for non-Covid-19 patients during the pandemic. PLoS One. 2020;15(10 October):1–10. doi: 10.1371/journal.pone.0241331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh R., Sahu A., Singh K., Prasad R.S., Pandey N., Singh R.C. Impact of COVID-19 Pandemic on Neurosurgical Practice in a Tertiary Care Center in India. J. Neurosci. Rural Pract. 2021;12(1):24–32. doi: 10.1055/s-0040-1716455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Dinmohamed A.G., Visser O., Verhoeven R.H.A., Louwman M.W.J., van Nederveen F.H., Willems S.M., Merkx M.A.W., Lemmens V.E.P.P., Nagtegaal I.D., Siesling S. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020;21(6):750–751. doi: 10.1016/S1470-2045(20)30265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salian V.S., Wright J.A., Vedell P.T., Nair S., Li C., Kandimalla M., Tang X., Carmona Porquera E.M., Kalari K.R., Kandimalla K.K. COVID-19 transmission, current treatment, and future therapeutic strategies. Mol. Pharm. 2021;18(3):754–771. doi: 10.1021/acs.molpharmaceut.0c00608. [DOI] [PubMed] [Google Scholar]
- 14.Callaway E. Could new COVID variants undermine vaccines? Labs scramble to find out. Nature. 2021;589(7841):177–178. doi: 10.1038/d41586-021-00031-0. [DOI] [PubMed] [Google Scholar]