Abstract
Purpose
Molar Incisor Hypomineralization (MIH) are first molars with developmental enamel defects and are common findings in many child populations. The porous nature of MIH enamel and the presence of post-eruptive enamel breakdown leads to the presence of hypersensitivity and pain, which is often the patient’s main complaint and can result in dental fear and affect the quality of life.
The present review aims to summarise the evidence for the ability of MIH to cause problems, such as dental fear and anxiety (DFA) and to summarise the evidence for a possibly negative impact on the oral health-related quality of life (OHRQoL) of MIH affected children and adolescents, in a systematic review.
Method
Two searches, (1) MIH AND dental anxiety and (2) MIH AND Quality of life, were performed in MEDLINE/PubMed and Scopus. Selection demands were fulfilling the MIH diagnosis criteria using validated instruments and questionnaires for assessing DFA and OHRQoL, respectively.
Results
After removing duplicates and articles not fulfilling the selection demands, 6 studies concerning MIH and DFA and 8 studies concerning MIH and OHRQoL remained.
Conclusion
Children and adolescents with diagnosed MIH did not seem to suffer from increased dental fear and anxiety, but indicated an impaired oral health-related quality of life.
Keywords: Molar incisor hypomineralization (MIH), Dental fear and anxiety, Review
Introduction
First permanent molars (FPM), which at eruption show areas of hypomineralised enamel, were primarily observed in the 1980s (Koch et al. 1987, Suckling et al. 1987). For the past 20 years, the condition, which has been termed Molar-Incisor Hypomineralization (MIH) (Weerheijm et al. 2001), has attracted increasing attention and proved to occur all over the world. A comprehensive literature research, with 70 eligible prevalence studies included, found a pooled MIH prevalence of 14.2%, globally (Zhao et al. 2018).
Clinically, the porous hypomineralised areas appear as white–yellow to brownish, well-defined opaque spots. In these areas, the enamel is insufficiently mineralised with varying degrees and can fall apart, especially on the occlusal surfaces of the teeth (Weerheijm et al. 2003). The severity of MIH has a significant impact on the treatment need in the FPM. Already restored MIH molars remain within short re-treatment cycles. (Leppaniemi et al. 2001). It has been shown that children with MIH have undergone dental treatment of their FPMs approximately ten times as often as children without MIH (Jälevik and Klingberg 2012).
The porous nature of MIH enamel and the presence of post-eruptive enamel breakdown leads to hypersensitivity and pain, which is often the patient’s main complaint and can affect the quality of life. There is also the increased risk of dental fear and anxiety (Jälevik and Klingberg 2002).
Teeth with hypersensitivity not only create problems for patients, but also for the dentists. The sensitivity becomes problematic when it hinders the possibility of obtaining sufficient pain control with, consequently, behavioural management problems due to dental fear and anxiety, which is related to the pain experienced by the patients during multiple treatment appointments (Raposo et al. 2019; Jälevik and Klingberg 2012).
Today, approximately 500 scientific articles have been published concerning various aspects of MIH, including biochemical and histomorphological properties, diagnostics, prevalence, aetiology, treatment, dental fear and quality of life (D3 group). Approximately, 40 review articles have been published on various aspects of MIH (D3-group).
Conditions that mainly affect the oral health-related quality of life are untreated dental caries, dental trauma, increased dental protrusion, wearing orthodontic appliances and severe periodontal disease (De Stefani 2019). However, there are no reviews regarding the impact of MIH on dental fear, treatment problems and quality of life.
In the literature, it is often stated that MIH has created problems for both the affected children and treating dentists in the form of dental fear, treatment problems and that MIH has contributed to a poorer quality of life for the affected children (Jälevik and Klingberg 2002). It has been suggested that children, affected by oral and orofacial disorders, such as MIH, have compromised functioning, well being and quality of life (QoL) (Kalkani et al. 2016, Barbosa and Gavião 2008). The evidence for these proposals is regarded as weak since it is mainly based on the observations by the treating dentists and occasionally by the parents, yet seldom by the affected children.
The present research question is: Are children and adolescents with diagnosed MIH more anxious in the dental context and/or do the impaired teeth influence their oral health-related quality of life?
Systematic reviews are essential tools for summarising evidence accurately and reliably. This review aims to summarise the evidence for the ability of MIH to cause problems, such as dental fear and anxiety and to summarise the evidence for a possibly negative impact on the oral health-related quality of life (OHRQoL) of MIH affected children and adolescents, in a systematic review.
Assessment of behaviour management problems has been partly based on observations of the child's behavior during treatment and partly based on the dentist's notes in the dental records, clearly expressing delay of treatment or rendering treatment impossible. This type of registration is subjective and almost certainly biased; therefore, this review has refrained from including this item.
Methods
This systematic review followed a protocol in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). Registered in PROSPERO: CRD42021233962.
Searches
Searches were performed in MEDLINE/PubMed and Scopus. To find the eligible articles, a search strategy was performed combining MeSH terms, MeSH synonyms and free terms. The ‘AND’ and ‘OR’ Boolean operators were applied to combine keywords (Tables 1, 2). Searches performed from inception dates to date noted. Once selected, the references were analysed according to the eligibility criteria.
Table 1.
Search 1 MIH AND dental anxiety
| Search order | Search string | No results |
|---|---|---|
| PubMed 2020–11-03 | ||
| #13 | #9 AND #12 | 34 |
| #12 | #10 OR #11 | 255,913 |
| #11 | Anxiety[tiab] OR anxieties[tiab] OR fear[tiab] OR odontophobia[tiab] OR phobia[tiab] OR phobias[tiab] OR DAQ[tiab] OR CFSS-DS[tiab] | 255,158 |
| #10 | Dental anxiety[mesh] | 2683 |
| #9 | #3 OR #8 | 8485 |
| #8 | #6 AND #7 | 5633 |
| #7 | Hypominerali*[tiab] OR mottling[tiab] OR opacit*[tiab] OR cheese[tiab] OR hypoplasia*[tiab] OR idiopathic enamel[tiab] OR opaque[tiab] OR calcification[tiab] OR discoloration[tiab] | 121,128 |
| #6 | #4 OR #5 | 271,505 |
| #5 | Molar*[tiab] OR tooth[tiab] OR teeth[tiab] | 245,897 |
| #4 | Molar[mesh] OR tooth[mesh] | 89,132 |
| #3 | #1 OR #2 | 4393 |
| #2 | Dental enamel hypoplasia[tiab] OR hypoplastic Enamel[tiab] OR enamel agenesis[tiab] OR enamel ageneses[tiab] OR enamel hypoplasia[tiab] OR enamel hypoplasias[tiab] OR Molar Incisor Hypomineralization[tiab] OR enamel hypomineralization[tiab] OR MIH[tiab] OR molar Hypomineralization[tiab] OR molar Incisor Hypomineralisation[tiab] OR enamel hypomineralisation[tiab] OR Molar hypomineralisation[tiab] OR enamel defect[tiab] OR enamel defects[tiab] | 2810 |
| #1 | Dental enamel hypoplasia[mesh] | 2792 |
| Scopus 2020–11-03 | ||
| #8 | Limit to article, review | 80 |
| #7 | #5 AND #6 | 91 |
| #6 | TITLE-ABS-KEY(anxiety OR anxieties OR fear OR odontophobia OR phobia* OR DAQ OR CFSS-DS) | 536,099 |
| #5 | #1 OR #4 | 18,611 |
| #4 | #2 AND #3 | 16,203 |
| #3 | TITLE-ABS-KEY (molar* OR tooth OR teeth) | 659,774 |
| #2 | TITLE-ABS-KEY(hypominerali* OR mottling OR opacit* OR cheese OR hypoplasia* OR “idiopathic enamel” OR opaque OR calcification OR discoloration) | 289,257 |
| #1 | TITLE-ABS-KEY(“dental enamel hypoplasia” OR “hypoplastic enamel” OR “enamel agenesis” OR “enamel ageneses” OR “enamel hypoplasia*” OR “Molar Incisor Hypomineralization” OR “enamel hypomineralization” OR MIH OR “molar Hypomineralization” OR “Molar Incisor Hypomineralisation” OR “enamel hypomineralisation” OR “molar Hypomineralisation” OR “enamel defect*”) | 5235 |
Table 2.
Search 2 MIH AND Quality of life
| Search order | Search string | No results |
|---|---|---|
| PubMed 2020–11-03 | ||
| #13 | #9 AND #12 | 156 |
| #12 | #10 OR #11 | 540,874 |
| #11 | Life quality[tiab] OR life qualities[tiab] OR QoL[tiab] OR HRQoL[tiab] OR HRQL[tiab] OR OHRQoL[tiab] OR personal satisfaction[tiab] OR patient satisfaction[tiab] OR Activities of Daily Living[tiab] OR personal autonomy[tiab] OR patient preference[tiab] OR patient preferences[tiab] OR self-concept[tiab] OR CPQ11-14[tiab] | 144,445 |
| #10 | Quality of Life[mesh] OR personal satisfaction[mesh] OR patient satisfaction[mesh] OR Activities of Daily Living[mesh] OR personal autonomy[mesh] OR self-concept[mesh] | 484,730 |
| #9 | #3 OR #8 | 8485 |
| #8 | #6 AND #7 | 5633 |
| #7 | Hypominerali*[tiab] OR mottling[tiab] OR opacit*[tiab] OR cheese[tiab] OR hypoplasia*[tiab] OR idiopathic enamel[tiab] OR opaque[tiab] OR calcification[tiab] OR discoloration[tiab] | 121,128 |
| #6 | #4 OR #5 | 271,505 |
| #5 | Molar*[tiab] OR tooth[tiab] OR teeth[tiab] | 245,897 |
| #4 | Molar[mesh] OR tooth[mesh] | 89,132 |
| #3 | #1 OR #2 | 4393 |
| #2 | Dental enamel hypoplasia[tiab] OR hypoplastic Enamel[tiab] OR enamel agenesis[tiab] OR enamel ageneses[tiab] OR enamel hypoplasia[tiab] OR enamel hypoplasias[tiab] OR Molar Incisor Hypomineralization[tiab] OR enamel hypomineralization[tiab] OR MIH[tiab] OR molar Hypomineralization[tiab] OR Molar Incisor Hypomineralisation[tiab] OR enamel hypomineralisation[tiab] OR molar hypomineralisation[tiab] OR enamel defect[tiab] OR enamel defects[tiab] | 2810 |
| #1 | Dental enamel hypoplasia[mesh] | 2792 |
| Scopus 2020–11-03 | ||
| #8 | Limit to article, review | 378 |
| #7 | #5 AND #6 | 399 |
| #6 | TITLE-ABS-KEY ("Quality of Life" OR "life quality" OR "life qualities" OR "personal satisfaction" OR QoL OR HRQoL OR HRQL OR OHRQoL OR "patient satisfaction" OR "Activities of Daily Living" OR "personal autonomy" OR "patient preference” OR "self-concept” OR CPQ11-14) | 869,714 |
| #5 | #1 OR #4 | 18,611 |
| #4 | #2 AND #3 | 16,203 |
| #3 | TITLE-ABS-KEY (molar* OR tooth OR teeth) | 659,774 |
| #2 | TITLE-ABS-KEY(hypominerali* OR mottling OR opacit* OR cheese OR hypoplasia* OR “idiopathic enamel” OR opaque OR calcification OR discoloration) | 289,257 |
| #1 | TITLE-ABS-KEY(“dental enamel hypoplasia” OR “hypoplastic enamel” OR “enamel agenesis” OR “enamel ageneses” OR “enamel hypoplasia*” OR “Molar Incisor Hypomineralization” OR “enamel hypomineralization” OR MIH OR “molar hypomineralization” OR “Molar Incisor Hypomineralisation” OR “enamel hypomineralisation” OR “molar hypomineralisation” OR “enamel defect*”) | 5235 |
Selection process
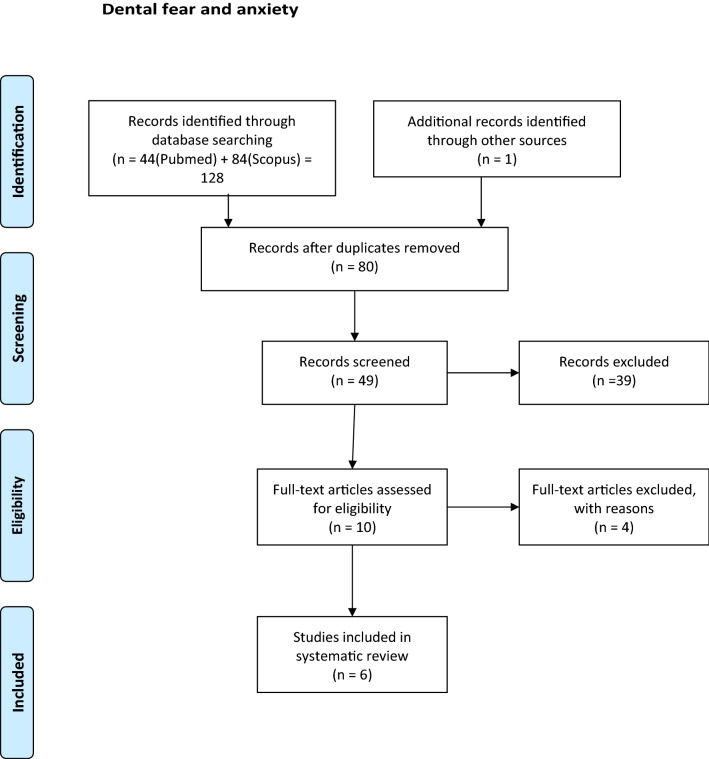
Duplicates were removed and after the screening of abstracts, possible articles for inclusion were read by three authors (BJ, NS, AR) in full text. After reading, discussions and agreement, articles not fulfilling the inclusion criteria were removed (Figs. 1, 2).
Fig. 1.
Flow fear. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
Fig. 2.
Flow chart quality of life. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
Inclusion criteria
Full text articles published in peer reviewed journals
MIH diagnosis in accordance with established MIH criteria, e.g., DDE index (FDI Working Group 1992) or EAPD index (Weerheijm et al. 2003)
Dental fear and anxiety (DFA) and oral health-related quality of life (OHRQoL) registered in accordance with validated scales or questionnaires
Written in the English language
The PICOT strategy applied for inclusion criteria:
Population (P): 6-to 18-year-old children.
Intervention (I): Not applicable.
Comparator (C): MIH.
Outcome (O): (a) Dental Fear and Anxiety (DFA), (b) Oral Health-Related Quality of Life (OHRQoL).
Type of study (T): Case–Control and Cross-Sectional studies.
Exclusion criteria
MIH diagnosis not in accordance with established MIH indices
DFA or OHRQoL not measured with validated scales or questionnaires
Reviews, case reports, letters to editor
Assessment of risk of bias in included studies
All three authors (BJ, NS, AR), independently, assessed the risk of bias for the eligible articles using a modified version of the quality assessment for prevalence studies tool developed by Munn et al. (2015).
Data extraction
Population
The country where the study was conducted.
Type of study.
Size and age of the study group.
Criteria for MIH diagnosis
Number of children with MIH diagnosis and degree of disorder.
Method for reporting Dental Fear and Anxiety and/or Oral Health-Related Quality of Life.
Respondent: Child or parents.
Results
Data searches
After duplicates were removed, the number of articles identified in database searches was 80 for DFA (Dental Fear and Anxiety) and 511 for OHRQoL (Oral Health-Related Quality of Life). After screening the abstracts, 10 articles for DFA and 22 articles for OHRQoL remained for complete reading. The articles were read by two authors: DFA (AR and BJ) and OHRQoL (NS and BJ). After reading and discussions, 4 DFA articles and 14 OHRQoL articles were excluded. The most common reason for exclusion (10 articles) was that nonvalidated instruments/questionnaires were used. Four articles were excluded as it was not the effect of having MIH but the result after treatment of MIH that was measured and 4 because there was no valid MIH diagnosis (Tables 3, 4). Six articles remained regarding how MIH affected DFA (Tables 5, 6). Eight articles dealt with MIH's impact on OHRQoL (Table 7).
Table 3.
Excluded papers: dental fear and anxiety
| Authors | Articles | Motives |
|---|---|---|
| Crombie et al. (2008) | Molar incisor hypomineralization: a survey of members of the Australian and New Zealand Society of Paediatric Dentistry | No fear measure instrument |
| Kalkani et al. (2016) | Molar incisor hypomineralization: experience and perceived challenges among dentists specialising in paediatric dentistry and a group of general dental practitioners in the UK | No fear measure instrument |
| Mahoney (2012) | Molar incisor hypomineralization | No fear measure instrument |
| Rolim et al. (2021) | Adhesive restoration of molars affected by molar incisor hypomineralization: a randomised clinical trial | Treatment evaluation |
Table 4.
Excluded papers: quality of life
| Authors | Article | Motives |
|---|---|---|
| Almuallem et al. (2018) | Molar incisor hypomineralization (MIH) – an overview | OHRQoL vs MIH not measured |
| Andrade et al. (2019) | Impact of developmental enamel defects on quality of life in 5‐year‐old children | 5-year-olds, no MIH diagnosis |
| Ebel et al. (2018) | The severity and degree of hypomineralization in teeth and its influence on oral hygiene and caries prevalence in children | OHRQoL vs MIH not measured |
| Elhennawy et al. (2019) | Outcome and comparator choice in molar incisor hypomineralization (MIH) intervention studies: a systematic review and social network analysis | Review, OHRQoL vs MIH, not measured |
| Fütterer et al. (2020) | Influence of customised therapy for molar incisor hypomineralization on children's oral hygiene and quality of life | OHRQoL vs MIH not measured. Treatment evaluation |
| Hasmun et al. (2020) | Determinants of children’s oral health-related quality of life following T aesthetic treatment of enamel opacities | OHRQoL vs MIH not measured. Treatment evaluation |
| Hasmun et al. (2018) | Change in Oral Health-Related Quality of Life Following Minimally Invasive Aesthetic Treatment for Children with Molar Incisor Hypomineralization: A Prospective Study | OHRQoL vs MIH not measured. Treatment evaluation |
| Kalkani et al. (2016) | Molar incisor hypomineralization: experience and perceived challenges among dentists specialising in paediatric dentistry and a group of general dental practitioners in the UK | Evaluation of dentist perception |
| Large et al. (2020) | What children say and clinicians hear: accounts relating to incisor hypomineralization of cosmetic concern | Estetic evaluation |
| Marshman et al. (2009) | The impact of developmental defects of enamel on young people in the UK | No MIH diagnosis. Qualitative study, no questionnaire |
| Oyedele et al. (2015) | Co-morbidities associated with molar-incisor hypomineralization in 8 to 16 year old pupils in Ile-Ife, Nigeria | No validated QoL questionnaire |
| Paglia (2018) | Molar Incisor Hypomineralization: paediatricians should be involved as well! | Letter to editor |
| Sujak et al. (2004) | Esthetic perception and psychosocial impact of developmental enamel defects among Malaysian adolescents | No validated QoL questionnaire, no MIH diagnosis |
| Vargas-Ferreira and Ardenghi (2011) | Developmental enamel defects and their impact on child oral health-related quality of life | No MIH diagnosis |
Table 5.
Dental fear and anxiety description
| Authors | Country | Study design | Sample size | Age years | Boys N | Girls N | MIH diagnos | Severe MIH N | Mild MIH N | MIH (severe/mild) % |
|---|---|---|---|---|---|---|---|---|---|---|
| Arrow (2017) | Australia | Cross sectional | 88 | 15 | DDE index | 18* | 20 | |||
| Laureno et al. (2020) | Brazil | Cross sectional | 466 | 8–10 | Ghamin 2015 | 19 | 37 | 12 (4/8) | ||
| Jälevik et al. (2002) | Sweden | Case control | 73 | 9 | 35 | 38 | DDE index | 32 | ||
| Jälevik et al. (2012) | Sweden | Case control | 67 | 18 | 31 | 36 | DDE index | 30 | ||
| Kosma et al. 2016 | Greece | Cross sectional | 1179 | 8 | 1139 | 1196 | EAPD 2003 | 33 | 221 | 22 (3/19) |
| 1156 | 14 | 85 | 159 | 21 (7/14) | ||||||
| Menoncin et al. (2019) | Brazil | Cross sectional | 731 | 8 | 357 | 374 | EAPD 2003 | 88* | 12 | |
*p < 0.05
Table 6.
Dental fear and anxiety, findings
| Authors | CFSS-DS mean (SD) | DAQ reported DA | DVSS mean | MCDAS mean (SD) | Respondent | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No MIH | MIH | no MIH N (%) | MIH N (%) | No MIH | MIH | No MIH | MIH | ||||||
| Arrow (2017) | 21.0 (8.2) | 18.9 (7.1) | NS | Parent | |||||||||
| Carvalho Laureno et al. (2020) | 29.87 (0.92) | NS | Child | ||||||||||
| Jälevik et al. (2002) | 20.8 (5.4) | 23.3 (7.5) | NS | 8 (20) | 14 (44) | * | Parent | ||||||
| Jälevik et al. (2012) | 21.7 (5.8) | 22.0 (6.2) | NS | 39.6 | 38.2 | NS | Child | ||||||
| Kosma et al. 2016 | 25.3 (10.5) | 25.0 (9.5) | NS | Child | |||||||||
| 27.2 (9.2) | 28.1 (9.2) | NS | |||||||||||
| Menoncin et al. (2019) | 348 (48) | 57 (64) | NS | Parent | |||||||||
CFSS-DS Dental Subscale of Children’s Fear Survey Schedule; DAQ Dental Anxiety Question; DVSS Dental Visit Satisfaction Scale; MCDAS Modified Child Dental Anxiety Scale; NS No significance
*p < 0.05
Table 7.
QoL studies
| Authors | Country | Study design | Sample size N | Age years | Boys N | Girls N | MIH diagnos | Severe MIH N | Mild MIH N | Presence of MIH (severe/mild) % | COHQoL | Responder | Summary of finding |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arrow (2013) | Austr | Cross Sectional | 550 | 7 | ? | ? | DDE index | 32 | 86 | 21% (6%/16%) | P-CPQ | P | No impact of MIH on OHRQoL is shown |
| Arrow (2017) | Austr | Cross Sectional | 88 | 14–16 | ? | ? | DDE index | 18 | 20% | CPQ11-14 | C | No impact of MIH on OHRQoL is shown | |
| Dantas-Neta et al. (2016) | Brazil | Cross Sectional | 594 | 11–14 | ? | ? | EAPD 2003 | 25 | 84 | 18% (4%/14%) | P-CPQ | P | Severe MIH was significantly associated with a greater negative impact of the ‘functional limitation domain’ according to parents’/caregivers’ perceptions. According to the children, severe MIH was significantly associated with a greater negative impact of the ‘oral symptom domain’ and ‘functional limitation domain’ |
| CPQ11-14 | C | ||||||||||||
| Dias et al. (2020) | Brazil | Cross Sectional | 42 | 6–7 | 125 | 128 |
EAPD 2003 |
15 | 238 | CPQ8-10 | C | Those with severe MIH are compared to those with mild. The results of OHRQoL questionnaire indicate a certain but not significant impact on the domains: ‘Oral symptoms’, ‘Functional limitations’ and also ‘Emotional wellbeing’ (the parents) | |
| 211 | 8–12 | CPQ11-14 | C | ||||||||||
| P-CPQ | P | ||||||||||||
| Folayan et al. (2018) | Nigeria | Cross Sectional | 428 | 6–9 | 438 | 415 |
EAPD 2003 |
20 | 3% | Child OIPD | C | No impact of MIH on OHRQoL is shown | |
| 425 | 10–16 | 5 | |||||||||||
| Gutiérrez et al. (2019) | Mexico | Cross Sectional | 411 | 8–10 | 194 | 217 |
EAPD 2003 |
166 | 40% | CPQ8-10 | C | MIH, severe as well as mild, impact on OHRQoL in all domains (p < 0.001) | |
| Portella et al. (2019) | Brazil | Cross Sectional | 728 | 8–10 | 372 | 356 |
EAPD 2003 |
25 | 63 |
12% (3%/9%) |
CPQ8-10 | C | MIH, severe as well as mild, impact on OHRQoL the domain ‘oral symptoms’ (p < 0.001) |
| Velandia et al. (2018) | Colomb | Case Control | 88 | 8–10 | 41 | 47 |
EAPD 2003 |
44 | CPQ8-10 | C | MIH, severe as well as mild, impact on OHRQoL in all domains (p < 0.001) | ||
Description and findings
C Children, P Parent, ? not given
Populations
Most studies are of the cross-sectional type. Three studies are case–control studies (Jälevik and Klingberg 2002, 2012; Velandia et al. 2018).
The study groups varied in age and size. The age range in the study groups within the OHRQoL articles varied between 6 and 16 years to only one age. The most common age group was 8–10 years.
Within the DFA articles, all but one study included only one age group. In one DFA article, the study group was 8–10 years old (Table 5).
Latin America dominates as a country of origin for studies on OHRQoL (Table 7). Regarding DFA, studies have been conducted in Europe, Brazil and Australia (Table 5).
MIH diagnosis
Regarding MIH diagnosis, most studies use the EAPD index (Weerheijm 2003). Four articles (Jälevik and Klingberg 2002, 2012, Arrow 2013, 2017) use the DDE index (FDI Commision on Oral Health 1992).
Five out of 14 articles did not report if the MIH disorder was mild or severe. Instruments and Questionnaires.
DFA
In 4 out of 6 DFA studies, CFSS-DS (Dental Subscale of Children’s Fear Survey Schedule) was used as a measuring instrument. Two of these studies were supplemented with other instruments, DAQ (Dental Anxiety Question) (Neverlien 1990) and DVSS (Dental Visit Satisfaction Scale) (Corah et al. 1988), respectively.
Another study used DAQ and one used MCDAS (Modified Child Dental Anxiety Scale) (Howard and Freeman 2007).
The CFSS-DS is the most frequently used measure of DFA in children and adolescents (Klingberg and Broberg 2007) and comprises 15 items scored on a Likert-type scale, ranging from 1 (not afraid at all) to 5 (very afraid). The total score ranges between 15 and 75.
DAQ consists of one question: “Do you think that your child is afraid of going to the dentist?” with four possible answers: no = 1; a little = 2; yes, he/she is afraid = 3; and yes, he/she is very afraid = 4.
DVSS has been developed to measure different aspects of the dentist–patient relationship from the patient´s point of view.
Modified Child Dental Anxiety Scale (MCDAS) was utilised in one study (Tables 5, 6).
OHRQoL
To evaluate MIH's impact on the affected children's quality of life, CPQ8-10 and CPQ11–14 (Jokovic et al. 2002) were mainly used. In two of these studies, a questionnaire for parents (P-CPQ) (Jokovic et al. 2003) was added and in one study, only the parental questionnaire was used. One study used Child-OIPD (Gherunpong et al. 2004).
Oral Health-Related Quality of Life focuses on oral health and orofacial concerns. It describes the way in which oral health affects a person’s ability to function, psychological status, social factors and pain or discomfort. Therefore, the OHRQoL attempts to represent the subjective side of oral health (Bekes and Hirsch 2013).
CPQ8-10, CPQ11–14 and P-CPQ are questionnaires within the entity OHRQoL, which was developed to suit different groups of responders. It contains questions in four domains: Oral symptoms, functional limitations, emotional well-being and social well-being.
Child-OIPD is another questionnaire within the OHRQoL entity developed by Gherunpong et al. (2004) (Table 7).
Respondents
The parents responded in 3 out of 6 articles regarding DFA.
Concerning OHRQoL, the parent was the only respondent in one article; in two articles, parents and the child responded to one adjusted questionnaire each. In the remaining articles, the child was the respondent.
Outcomes
DFA
A significant connection between MIH and DFA is only shown by DAQ in Jälevik & Klingberg (2002). The same study also showed a significant association of MIH and DFA with CFSS-DS, when using a cutoff value for DFA. CFSS-DS as well as DAQ were answered by the parents. Other studies only showed a tendency for increased DFA in MIH, but without significance (Table 6).
OHRQoL
Two of the articles showed a significant impact of MIH on all domains of OHRQoL (Gutiérrez et al. 2019; Velandia et al. 2018). Portella et al. (2019) found a significant impact on the domain "oral symptoms". Two studies (Dantas-Neta et al. 2016; Dias et al. 2020) demonstrated some influence in the domains Oral Symptoms and Functional Limitations. In the latter study, those with severe MIH were compared with those with severe MIH. In all other studies, those with MIH were compared with those without MIH regarding DFA as well as OHRQoL.
The results in the studies where both the parents and the children were respondents, in their respective questionnaires, indicated good consensus (Table 7).
Discussion
In the present literature research, few articles were found that describe the ability of the condition Molar Incisor Hypomineralization (MIH) to cause dental fear and anxiety (DFA) and to impact on the quality of life (QoL) negatively in the affected children.
Comparison between the selected studies should be interpreted with caution due to the lack of uniformity in sample size and selection, diagnostics and age groups. Furthermore, the demographic and socioeconomic aspects, as well as the organisation of dental service for children, differ substantially around the world.
Most studies used the EAPD index when diagnosing MIH. A few older studies used the DDE index. As the EAPD index is based entirely on the DDE index, it is unproblematic.
DFA
Most studies in the present review used the CFSS-DS instrument when searching for DFA among children with MIH. When comparing mean values between the groups (MIH vs no MIH), none of these studies found a significant difference. One study showed a significant difference when calculating a cutoff value for DFA, defined by total sample mean score plus one standard deviation, where the parents filled in the questionnaires (Jälevik and Klingberg 2002).
However, more recent studies have shown that a lot of surrounding factors can influence the CFSS-DS value. The parent as the informant has been questioned; the child alone as the informant has been advocated (Klingberg and Broberg 2007, Gustafson et al. 2010). Also, the calculation of the cutoff value for CFSS-DS is now being challenged. It should be adapted to age and gender (Lopes et al. 2013).
Moreover, a more recent review study (Cianetti et al. 2017) has shown that in studies using CFSS-DS ratings, the prevalence and the mean score of dental fear/anxiety was lower in Northern Europe than the remaining countries, the prevalence decreased with increasing age and the frequency was higher in females than in males. It can be questioned whether the measuring instrument CFSS-DS is reliable when it comes to studying specified dental disorders influencing dental fear.
Of the 15 questions, only a small number of questions can be linked to poor experience with MIH teeth. This is especially true in those parts of the world where dental health is good and where children's contact with dental care is established at a young age.
According to Klingberg et al. (1995), only approximately one-fourth of the children with BMP suffered dental fear. Consequently, the perceived difficulties in treating MIH teeth mainly does not reflect fear of dental care, but problems due to sensitivity of the teeth and the problem of obtaining adequate anesthesia (Rodd et al. 2007).
QoL
Oral Health-Related Quality of Life (OHRQoL) focuses on oral health and orofacial concerns. It describes the way in which oral health affects a person’s ability to function, psychological status, social factors and pain or discomfort. Therefore, the OHRQoL attempts to represent the subjective side of oral health (Bekes and Hirsch 2013).
The articles in the present review concerning the effect of MIH on OHRQoL are all recent and reflect a relatively new, but rapidly growing concept in dentistry. It is an aspect of dental health, addressing the patient's perception of whether his/her current oral health status has an impact upon his/her actual quality of life.
The results indicate that the MIH condition can impact OHRQoL, in particularly the domains ‘Oral symptoms’ and ‘Functional limitations’.
It is a common perception that treatment of children with MIH can be problematic (Garg et al. 2012; Gamboa et al. 2018). Teeth with decay are quickly attacked by caries, difficult to anesthetise and restore and children have difficulties in cooperating. The impact in daily life is of great concern when it comes to the holistic perspective of MIH.
In a recent questionnaire about perception and clinical management of molar incisor hypomineralization among dentists, the most cited barrier to care was the child’s behaviour, followed by difficulty in achieving local anesthesia (Wall and Leith 2020).
In a similar questionnaire, dentists reported increased sensitivity of the affected teeth as the most frequently encountered problem. They also recognise the negative effect this condition has on the quality of life of the affected children and their families (Kalkani et al. 2016).
It has been shown that patients benefit from desensitising therapy for MIH-damaged teeth and that treatment can reduce hypersensitivity and improve the ability to ensure oral hygiene, but also has a positive impact on the quality of life (Fütterer et al. 2020). These results underline the importance of treating MIH-damaged teeth to help relieve children's suffering and improve their quality of life (Raposo et al 2019).
Conclusion
Children and adolescents with diagnosed MIH did not seem to suffer from increased dental fear and anxiety, but indicated an impaired oral health-related quality of life.
Most previous studies on the treatment of MIH are the views of the dentists, with just a few from the child's perspective. To help dentists manage optimal treatment of MIH teeth, more studies from different countries regarding the impact of MIH on OHRQoL is desirable.
Acknowledgements
The authors gratefully acknowledge Linda Hammarberg and Helen Sjöblom, librarians at the Biomedical Library, University of Gothenburg, for valuable assistance with the electronic literature search.
Funding
Open access funding provided by University of Gothenburg. This study is not funded.
Declarations
Conflict of interest
The authors have no conflict of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Almuallem Z, Busuttil-Naudi A. Molar incisor hypomineralisation (MIH) - an overview. Br Dent J. 2018 doi: 10.1038/sj.bdj.2018.814. [DOI] [PubMed] [Google Scholar]
- Andrade NS, Dos Santos IT, Lima LMS, Lima CCB, Moura LFAD, Barros SSLV, Moura MS, Lima MDM. Impact of developmental enamel defects on quality of life in 5-year-old children. Int J Paediatr Dent. 2019;29(5):557–565. doi: 10.1111/ipd.12498. [DOI] [PubMed] [Google Scholar]
- Arrow P. Child oral health-related quality of life (COHQoL), enamel defects of the first permanent molars and caries experience among children in Western Australia. Community Dent Health. 2013;30(3):183–188. [PubMed] [Google Scholar]
- Arrow P. Dental enamel defects, caries experience and oral health-related quality of life: a cohort study. Aust Dent J. 2017;62(2):165–172. doi: 10.1111/adj.12449. [DOI] [PubMed] [Google Scholar]
- Barbosa TS, Gavião MB. Oral health-related quality of life in children: part II. Effects of clinical oral health status. A systematic review. Int J Dent Hyg. 2008;6(2):100–107. doi: 10.1111/j.1601-5037.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- Bekes K, Hirsch C. What is known about the influence of dentine hypersensitivity on oral health-related quality of life? Clin Oral Investig. 2013;17(Suppl 1):S45–51. doi: 10.1007/s00784-012-0888-9. [DOI] [PubMed] [Google Scholar]
- Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, Caruso S, Gatto R, De Giorgio S, Salvato R. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017;18(2):121–130. doi: 10.23804/ejpd.2017.18.02.07. [DOI] [PubMed] [Google Scholar]
- Corah NL, O'Shea RM, Bissell GD, Thines TJ, Mendola P. The dentist-patient relationship: perceived dentist behaviors that reduce patient anxiety and increase satisfaction. J Am Dent Assoc. 1988;116(1):73–76. doi: 10.14219/jada.archive.1988.0162. [DOI] [PubMed] [Google Scholar]
- Crombie FA, Manton DJ, Weerheijm KL, Kilpatrick NM. Molar incisor hypomineralization: a survey of members of the Australian and New Zealand Society of Paediatric Dentistry. Aust Dent J. 2008;53(2):160–166. doi: 10.1111/j.1834-7819.2008.00026.x. [DOI] [PubMed] [Google Scholar]
- Dantas-Neta NB, Moura LF, Cruz PF, Moura MS, Paiva SM, Martins CC, Lima MD. Impact of molar-incisor hypomineralization on oral health-related quality of life in schoolchildren. Braz Oral Res. 2016;30(1):e117. doi: 10.1590/1807-3107BOR-2016.vol30.0117. [DOI] [PubMed] [Google Scholar]
- De Stefani A, Bruno G, Irlandese G, Barone M, Costa G, Gracco A. Oral health-related quality of life in children using the child perception questionnaire CPQ11-14: a review. Eur Arch Paediatr Dent. 2019;20(5):425–430. doi: 10.1007/s40368-019-00418-8. [DOI] [PubMed] [Google Scholar]
- Dias FMCS, Gradella CMF, Ferreira MC, Oliveira LB. Molar-incisor hypomineralization: parent's and children's impact perceptions on the oral health-related quality of life. Eur Arch Paediatr Dent. 2020 doi: 10.1007/s40368-020-00556-4. [DOI] [PubMed] [Google Scholar]
- Ebel M, Bekes K, Klode C, Hirsch C. The severity and degree of hypomineralisation in teeth and its influence on oral hygiene and caries prevalence in children. Int J Paediatr Dent. 2018;28(6):648–657. doi: 10.1111/ipd.12425. [DOI] [PubMed] [Google Scholar]
- Elhennawy K, Krois J, Jost-Brinkmann PG, Schwendicke F. Outcome and comparator choice in molar incisor hypomineralisation (MIH) intervention studies: a systematic review and social network analysis. BMJ Open. 2019;9(8):e028352. doi: 10.1136/bmjopen-2018-028352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FDI Commision on Oral Health, Research and Epidemiology. A review of the developmental defects of enamel index (DDE Index). Int Dent J 1992; 42: 411–426. [PubMed]
- Folayan MO, Chukwumah NM, Popoola BO, Temilola DO, Onyejaka NK, Oyedele TA, Lawal FB. Developmental defects of the enamel and its impact on the oral health quality of life of children resident in Southwest Nigeria. BMC Oral Health. 2018;18(1):160. doi: 10.1186/s12903-018-0622-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fütterer J, Ebel M, Bekes K, Klode C, Hirsch C. Influence of customized therapy for molar incisor hypomineralization on children's oral hygiene and quality of life. Clin Exp Dent Res. 2020;6(1):33–43. doi: 10.1002/cre2.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamboa GCS, Lee GHM, Ekambaram M, Yiu CKY. Knowledge, perceptions, and clinical experiences on molar incisor hypomineralization among dental care providers in Hong Kong. BMC Oral Health. 2018;18(1):217. doi: 10.1186/s12903-018-0678-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg N, Jain AK, Saha S, Singh J. Essentiality of early diagnosis of molar incisor hypomineralization in children and review of its clinical presentation, etiology and management. Int J Clin Pediatr Dent. 2012;5(3):190–196. doi: 10.5005/jp-journals-10005-1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gherunpong S, Tsakos G, Sheiham A. Developing and evaluating an oral health related quality of life index for children; the CHILD-OIDP. Community Dent Health. 2004;21:161–169. [PubMed] [Google Scholar]
- Gustafsson A, Arnrup K, Broberg AG, Bodin L, Berggren U. Child dental fear as measured with the Dental Subscale of the Children's Fear Survey Schedule: the impact of referral status and type of informant (child versus parent) Community Dent Oral Epidemiol. 2010;38(3):256–266. doi: 10.1111/j.1600-0528.2009.00521.x. [DOI] [PubMed] [Google Scholar]
- Gutiérrez TV, Ortega CCB, Pérez NP, Pérez AG. Impact of molar incisor hypomineralization on oral health-related quality of life in mexican schoolchildren. J Clin Pediatr Dent. 2019;43(5):324–330. doi: 10.17796/1053-4625-43.5.4. [DOI] [PubMed] [Google Scholar]
- Hasmun N, Lawson J, Vettore MV, Elcock C, Zaitoun H, Rodd H. Change in oral health-related quality of life following minimally invasive aesthetic treatment for children with molar incisor hypomineralisation: a prospective study. Dent J (Basel) 2018;6(4):61. doi: 10.3390/dj6040061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasmun N, Vettore MV, Lawson JA, Elcock C, Zaitoun H, Rodd HD. Determinants of children’s oral health-related quality of life following aesthetic treatment of enamel opacities. J Dent. 2020;98:103372. doi: 10.1016/j.jdent.2020.103372. [DOI] [PubMed] [Google Scholar]
- Howard KE, Freeman R. Reliability and validity of a faces’ version of the Modified Child Dental Anxiety Scale. Int J Paediatr Dent. 2007;17(4):281–288. doi: 10.1111/j.1365-263X.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- Jälevik B, Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002;12(1):24–32. [PubMed] [Google Scholar]
- Jälevik B, Klingberg G. Treatment outcomes and dental anxiety in 18-year-olds with MIH, comparisons with healthy controls—a longitudinal study. Int J Paediatr Dent. 2012;22(2):85–91. doi: 10.1111/j.1365-263X.2011.01161.x. [DOI] [PubMed] [Google Scholar]
- Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81(7):459–463. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Measuring parental perceptions of child oral health-related quality of life. J Public Health Dent. 2003;63(2):67–72. doi: 10.1111/j.1752-7325.2003.tb03477.x. [DOI] [PubMed] [Google Scholar]
- Kalkani M, Balmer RC, Homer RM, Day PF, Duggal MS. Molar incisor hypomineralisation: experience and perceived challenges among dentists specialising in paediatric dentistry and a group of general dental practitioners in the UK. Eur Arch Paediatr Dent. 2016;17:81–88. doi: 10.1007/s40368-015-0209-5. [DOI] [PubMed] [Google Scholar]
- Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007;17(6):391–406. doi: 10.1111/j.1365-263X.2007.00872.x. [DOI] [PubMed] [Google Scholar]
- Klingberg G, Berggren U, Carlsson SG, Noren JG. Child dental fear: cause-related factors and clinical effects. Eur J Oral Sci. 1995;103(6):405–412. doi: 10.1111/j.1600-0722.1995.tb01865.x. [DOI] [PubMed] [Google Scholar]
- Koch G, Hallonsten AL, Ludvigsson N, Hansson BO, Holst A, Ullbro C. Epidemiologic study of idiopathic enamel hypomineralization in permanent teeth of Swedish children. Community Dent Oral Epidemiol. 1987;15(5):279–285. doi: 10.1111/j.1600-0528.1987.tb00538.x. [DOI] [PubMed] [Google Scholar]
- Kosma I, Kevrekidou A, Boka V, Arapostathis K, Kotsanos N. Molar incisor hypomineralisation (MIH): correlation with dental caries and dental fear. Eur Arch Paediatr Dent. 2016;17(2):123–129. doi: 10.1007/s40368-016-0221-4. [DOI] [PubMed] [Google Scholar]
- Large JF, Hasmun N, Lawson JA, Elcock C, Vettore MV, Rodd HD. What children say and clinicians hear: accounts relating to incisor hypomineralisation of cosmetic concern. Eur Arch Paediatr Dent. 2020;21(2):185–191. doi: 10.1007/s40368-019-00465-1. [DOI] [PubMed] [Google Scholar]
- Laureano ICC, Farias L, Fernandes LHF, Alencar CRB, Forte FDS, Honório DR, Cavalcanti AL. Dental fear in children: association with dental caries and molar incisor hypomineralization. Braz Dent J. 2020;31(6):673–679. doi: 10.1590/0103-6440202003880. [DOI] [PubMed] [Google Scholar]
- Leppaniemi A, Lukinmaa PL, Alaluusua S. Nonfluorid hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res. 2001;35:36–40. doi: 10.1159/000047428. [DOI] [PubMed] [Google Scholar]
- Lopes D, Arnrup K, Robertson A, Lundgren J. Validating the dental subscale of the children’s fear survey schedule using Rasch analysis. Eur J Oral Sci. 2013;121(3 Pt 2):277–282. doi: 10.1111/eos.12040. [DOI] [PubMed] [Google Scholar]
- Mahoney E. Molar incisor hypomineralization. Ann R Austral Coll Dent Surg. 2012;21:56–57. [PubMed] [Google Scholar]
- Marshman Z, Gibson B, Robinson PG. The impact of developmental defects of enamel on young people in the UK. Community Dent Oral Epidemiol. 2009;37(1):45–57. doi: 10.1111/j.1600-0528.2008.00453.x. [DOI] [PubMed] [Google Scholar]
- Menoncin BLV, Portella PD, Ramos BLM, Assunção LRDS, de Souza JF, Menezes JVNB. Dental anxiety in schoolchildren with molar incisor hypomineralization-A population-based cross-sectional study. Int J Paediatr Dent. 2019;29(5):615–623. doi: 10.1111/ipd.12503. [DOI] [PubMed] [Google Scholar]
- Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- Neverlien PO. Assessment of a single-item dental anxiety question. Acta Odontol Scand. 1990;48(6):365–369. doi: 10.3109/00016359009029067. [DOI] [PubMed] [Google Scholar]
- Oyedele TA, Folayan MO, Adekoya-Sofowora CA, Oziegbe EO. Co-morbidities associated with molar-incisor hypomineralisation in 8 to 16 year old pupils in Ile-Ife, Nigeria. BMC Oral Health. 2015;15:37. doi: 10.1186/s12903-015-0017-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paglia L. Molar Incisor Hypomineralization: paediatricians should be involved as well! Eur J Paediatr Dent. 2018;19(3):173. doi: 10.23804/ejpd.2018.19.03.1. [DOI] [PubMed] [Google Scholar]
- Portella PD, Menoncin BLV, de Souza JF, de Menezes JVNB, Fraiz FC, Assunção LRDS. Impact of molar incisor hypomineralization on quality of life in children with early mixed dentition: a hierarchical approach. Int J Paediatr Dent. 2019;29(4):496–506. doi: 10.1111/ipd.12482. [DOI] [PubMed] [Google Scholar]
- Raposo F, de Carvalho Rodrigues AC, Lia ÉN, Leal SC. Prevalence of hypersensitivity in teeth affected by molar-incisor hypomineralization (MIH) Caries Res. 2019;53(4):424–430. doi: 10.1159/000495848. [DOI] [PubMed] [Google Scholar]
- Rodd HD, Morgan CR, Day PF, Boissonade FM. Pulpal expression of TRPV1 in molar incisor hypomineralisation. Eur Arch Paediatr Dent. 2007;8(4):184–188. doi: 10.1007/BF03262594. [DOI] [PubMed] [Google Scholar]
- Rolim TZC, da Costa TRF, Wambier LM, Chibinski AC, Wambier DS, da Silva Assunção LR, de Menezes JVBN, Feltrin-Souza J. Adhesive restoration of molars affected by molar incisor hypomineralization: a randomized clinical trial. Clin Oral Investig. 2021;25:1513–1524. doi: 10.1007/s00784-020-03459-2. [DOI] [PubMed] [Google Scholar]
- Suckling GW, Herbison GP, Brown RH. Etiological factors influencing the prevalence of developmental defects of dental enamel in nine-year-old New Zealand children participating in a health and development study. J Dent Res. 1987;66(9):1466–1469. doi: 10.1177/00220345870660091101. [DOI] [PubMed] [Google Scholar]
- Sujak SL, Abdul Kadir R, Dom TN. Esthetic perception and psychosocial impact of developmental enamel defects among Malaysian adolescents. J Oral Sci. 2004;46(4):221–226. doi: 10.2334/josnusd.46.221. [DOI] [PubMed] [Google Scholar]
- Vargas-Ferreira F, Ardenghi TM. Developmental enamel defects and their impact on child oral health-related quality of life. Braz Oral Res. 2011;25(6):531–537. doi: 10.1590/S1806-83242011000600010. [DOI] [PubMed] [Google Scholar]
- Velandia LM, Álvarez LV, Mejía LP, Rodríguez MJ. Oral health-related quality of life in Colombian children with molar-incisor hypomineralization. Acta Odontol Latinoam. 2018;31(1):38–44. [PubMed] [Google Scholar]
- Wall A, Leith R. A questionnaire study on perception and clinical management of molar incisor hypomineralisation (MIH) by Irish dentists. Eur Arch Paediatr Dent. 2020;21(6):703–710. doi: 10.1007/s40368-020-00519-9. [DOI] [PubMed] [Google Scholar]
- Weerheijm KL, Jälevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35(5):390–391. doi: 10.1159/000047479. [DOI] [PubMed] [Google Scholar]
- Weerheijm KL, Duggal M, Mejàre I, Papagiannoulis L, Koch G, Martens LC, Hallonsten AL. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4(3):110–113. [PubMed] [Google Scholar]
- Zhao D, Dong B, Yu D, Ren Q, Sun Y. The prevalence of molar incisor hypomineralization: evidence from 70 studies. Int J Paediatr Dent. 2018;28(2):170–179. doi: 10.1111/ipd.12323. [DOI] [PubMed] [Google Scholar]