Abstract
Objective
To evaluate the current incidence and economic cost and to estimate the future burden of periprosthetic fracture (PF) after joint arthroplasties in South Korea.
Methods
This study was a retrospective registry‐based study of patients who were diagnosed as periprosthetic fractures (PFs) in South Korea. Cases of PF from 2010 to 2017 in South Korea using Health Insurance and Review and Assessment (HIRA) database, which contains all medical claims for all South Korean patients, were identified. The operational definitions of PFs were identified from the Electronic Data Interchange (EDI) code of the Korean National Health Insurance Program (KHNIP). The annual incidence and medical costs during the period were calculated and the future increase of PF and its cost were projected through 2030 using generalized linear model with quasi‐poisson link.
Results
During the 8‐year period, 14,456 patients were treated due to PFs. The annual number of patients with PF remarkably increased from 1,322 in 2010 to 2,636 in 2017. The increment was prominent in age groups of 70–79 and ≧80. Total number of patients with PF were 9752 in women and 4704 in men during the study period. Mean personal costs were 1,155.4 USD in women and 1,185.5 USD in men. The total cost of PFs increased from 779,533 USD in 2010 to 3,888,402 USD in 2017. The personal cost of PFs also increased from 589.7 USD in 2010 to 1,475.1 USD in 2017. In 2017, the number of PF patients exponentially increased after 50 years of age especially in women. Estimated with our projection model, the number of PFs will increase by 2.5 times and the cost will increase by 10 times in the next 10 years.
Conclusion
The incidence and cost of PFs are rising and will represent a serious socioeconomic burden in South Korea.
Keywords: Arthroplasty, Epidemiology, Incidence, Periprosthetic fractures, Republic of Korea
To evaluate and predict the burden of PF after joint arthroplasties in South Korea, we identified cases of PF from 2010 to 2017 in South Korea using Health Insurance and Review and Assessment (HIRA) database. The annual number of patients with PF remarkably increased from 1,322 to 2,636 and the increment was prominent in age groups of 70–79 and ≧80. In our projection model, the number of PF will increase by 2.5 times and the cost will increase by 10 times in the next 10 years.

Introduction
Periprosthetic fractures (PFs) are fractures which occur around prosthesis after joint replacement arthroplasty. Along with the increase of life expectancy and the number of joint arthroplasties, the number of PFs is increasing worldwide 1 . Among patients undergoing hip arthroplasty, 0.8% to 2.4% will suffer a PF within 5 years after the procedure 2 , 3 , 4 , 5 , 6 . Periprosthetic fractures are associated with significant morbidity and mortality. These fractures frequently require surgical management and cause a serious financial burden 5 , 7 , 8 , 9 . Not only do these PFs normally require surgery, but the difficulty of the required surgeries is a challenge to orthopaedic surgeons 10 . Arthroplasty surgeons have made various efforts to prevent the PFs during the primary arthroplasty and evaluate the risks of PFs in the follow‐up 11 , 12 , 13 . It has been suggested that age, gender, use of corticosteroids, poor bone quality, number of previous surgeries, stiff joints, neurological comorbidities, inflammatory arthropathy, and type of implants used in primary arthroplasties could increase the risk of PFs 2 , 4 , 6 , 14 , 15 , 16 , 17 . Prior to finding out the risk factors and figuring out whether it is controllable, the precise evaluation of incidence and burden of PFs is crucial.
The most common types of currently performed arthroplasty surgeries are total hip arthroplasty (THA) and total knee replacement (TKR). Therefore, PFs following these two types of total joint arthroplasties are most common among the PFs as well. Since most of these PFs after the arthroplasty in lower limbs would disable the capability to walk, they would cause higher morbidity and graver prognosis compared to PFs in upper limbs. Traditionally, the incidence of these two most common PFs are known as 1% after primary THA, 4% after revision THA, and 2% after TKA 4 .
There have been several studies on the incidence, morbidity, mortality, and medical cost of PF from the USA, Scotland, and Scandinavian countries 5 , 6 , 18 , 19 , 20 . The trend of PF incidence was quite different among the studies. While some studies reported an increase of PF incidence, the incidence decreased in other studies. Thus, it is not clear whether the incidence of PF is increasing. To date, national burden of PF has not been reported from East Asia. Furthermore, to our knowledge, the future burden of PFs has not been studied despite the significant socioeconomic problem and severe morbidity.
Therefore, the purpose of this study was (i) to evaluate the current incidence and economic cost of PF and (ii) to estimate the future burden of PF in South Korea.
Methods
Data Sources
This study was a retrospective registry‐based study of patients who were diagnosed as periprosthetic fractures in South Korea. Periprosthetic fractures were identified from the Electronic Data Interchange (EDI) code of the KNHIP, the principal codes of diagnoses and procedures in the HIRA database. From 2010 to 2017, all patients who had the code of PF (ICD‐10 (M966)) as primary diagnosis were selected.
The Health Insurance and Review and Assessment (HIRA) database includes medical claims for all South Korean citizens. In South Korea, 97% of the population is legally obliged to enroll in the Korean National Health Insurance Program (KNHIP) and the remaining 3% are covered by a medical aid program. Thus, almost all information about claims of South Korean patients is available from the HIRA database, which has been used for nationwide epidemiological studies 21 , 22 , 23 .
Current Burden of Periprosthetic Fractures
The annual number of patients with a diagnosis of PF was identified during a period from 2010 to 2017. The patients were divided into groups according to their age (subdivided into 10‐year increments) and gender.
Total and personal costs for the treatment of PF were also evaluated during the study period.
Future Projection of Periprosthetic Fractures
The annual frequency and medical cost of PF was predicted through 2030.
In order to adjust the confounding effect of changing numbers of the general population in the future, the age and sex distributions of the entire South Korean population over the study period and the projections through 2030 were obtained from the web site KOSIS (http://www.kosis.kr), which is run by the Central Government Organization for Statistics 24 .
Statistical Analysis
A quasi‐poisson regression was used to predict the annual frequency and medical cost of PF through 2030 25 . The quasi‐poisson regression model was given by the following formula.
where m is the month of surgery; E() is an expected count of annual surgery procedure; α is intercept; are coefficients of variables. Census of Korea was set as an offset that adjusted the confounding effect from oscillating number of people in time‐series data. All data and statistics were analyzed by using R software (version 3.5.3) 26 .
Results
Current Burden of Periprosthetic Fractures
From 2010 to 2017, 14,456 PF patients were identified in South Korea (Table 1). The demographic characteristics of the PF patients are summarized in Table 2. The annual number of PF patients increased in both genders during the study period (Figure 1). Total cost and personal cost also increased during the study period (Figure 2A,B). The increment was prominent in age groups of 70–79 and ≧80 (Figure 3). In 2017, the number of PF patients exponentially increased after 50 years, especially in women (Figure 4).
TABLE 1.
Number of patients who had periprosthetic fractures in South Korea from 2010 to 2017
| Cost | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|
| Number of periprosthetic fractures | 1,322 | 1,425 | 1,391 | 1,414 | 1,727 | 2,059 | 2,482 | 2,636 |
| Total cost (USD) | 779,533 | 992,309 | 1,218,582 | 1,435,815 | 2,133,629 | 2,765,132 | 3,630,445 | 3,888,402 |
| Personal cost (USD) | 589.7 | 696.4 | 876 | 1015.4 | 1235.5 | 1342.9 | 1462.7 | 1475.1 |
TABLE 2.
Demographic characteristics of patients who had periprosthetic fractures in South Korea from 2010 to 2017
| Periprosthetic fractures | Total cost (USD) | Personal cost (USD) | |
|---|---|---|---|
| Total | 14,456 | 16,843,846 | 1165.2 |
| Gender | |||
| Female | 9,752 | 11,267,075 | 1155.4 |
| Male | 4,704 | 5,576,772 | 1185.5 |
| Age (years) | |||
| 10–19 | 87 | 74,012 | 850.7 |
| 20–29 | 152 | 129,301 | 850.7 |
| 30–39 | 220 | 176,673 | 803.1 |
| 40–49 | 384 | 428,843 | 1,116.8 |
| 50–59 | 1,130 | 833,660 | 737.8 |
| 60–69 | 2,934 | 2,762,124 | 941.4 |
| 70–79 | 5,994 | 6,701,578 | 1,118 |
| ≧80 | 3,555 | 5,737,656 | 1,614 |
Fig. 1.
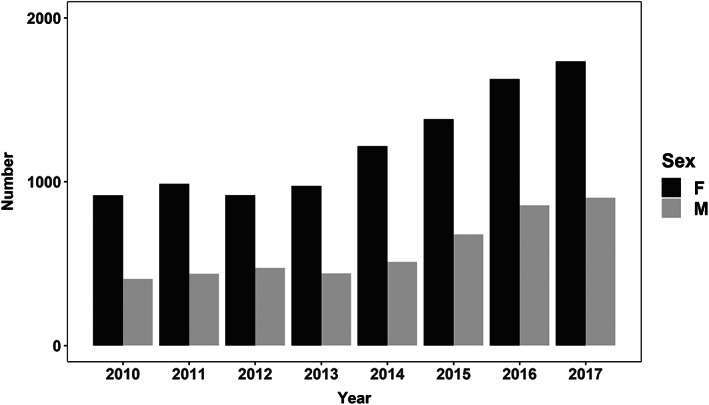
Number of patients with periprosthetic fracture in South Korea from 2010 to 2017.
Fig. 2.
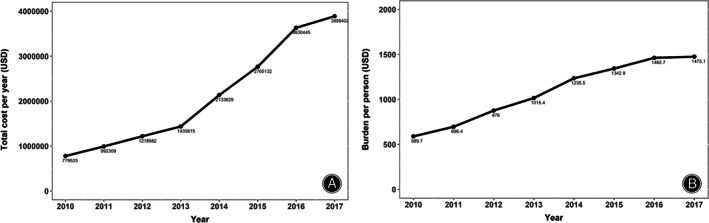
(A) Total cost of treatment for periprosthetic fracture in South Korea from 2010 to 2017. (B) Personal cost of treatment for periprosthetic fracture in South Korea from 2010 to 2017.
Fig. 3.
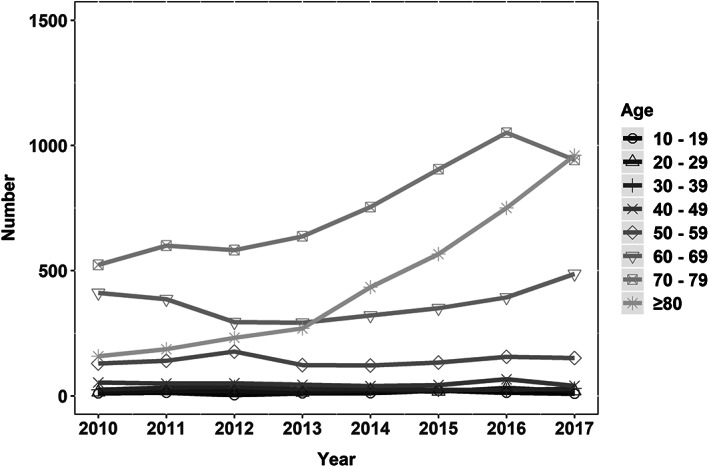
Number of patients with periprosthetic fractures stratified by age group from 2010 to 2017.
Fig. 4.
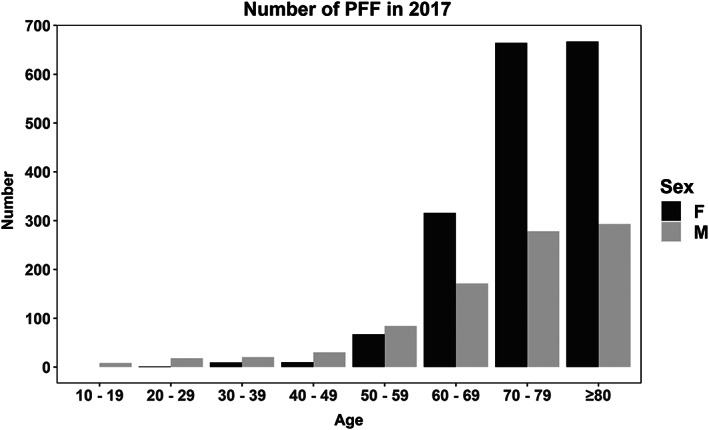
Number of patients who had periprosthetic fracture in each age group in 2017.
Future Projection of Periprosthetic Fractures
The projection model predicted that the number PF patients will increase by 2.5 times (Fig. 5), and total cost for PF will increase by 10 times in the next 10 years (Fig 6).
Fig. 5.
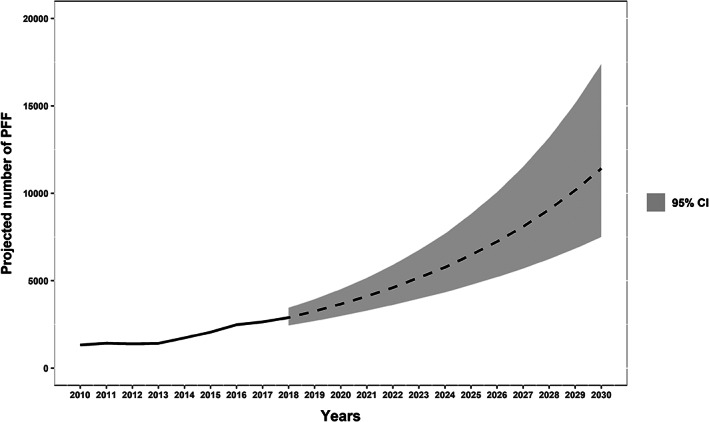
Projected number of patients who have periprosthetic fracture.
Fig. 6.
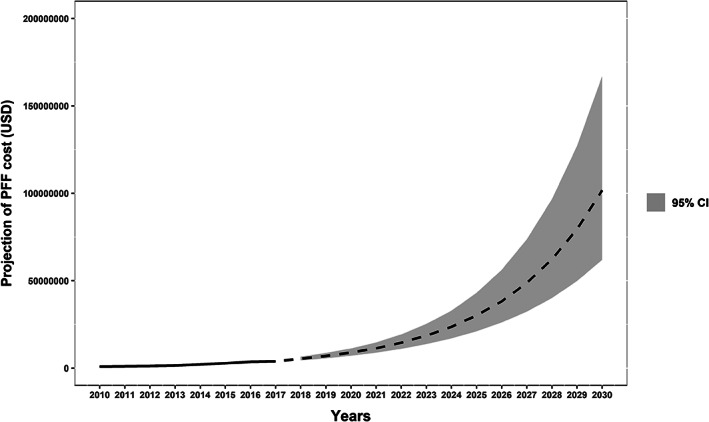
Projected total cost of treatment for periprosthetic fracture.
Discussion
Burden of Periprosthetic Fractures
The number of patients with PF has increased from 1,322 in 2010 to 2,636 in 2017 in South Korea and is projected to increase through 2030 by 2.5 times in this study.
Overall cost for PF treatment has increased from 779,533 to 3.888.402 USD and is predicted to increase by 10 times during next 10 years.
To date, several studies from western countries reported the trends related to the frequency and hospital charges of PF, especially after hip arthroplasty. However, the results were different among the studies (Table 3).
TABLE 3.
Periprosthetic fractures in previous studies
| Authors | Country | Study period | Number of PF | Economic cost |
|---|---|---|---|---|
| Cox et al. 18 | USA | 2006–2010 | Stationary | Increased |
| Meek et al. 6 | Scotland | 1997–2008 | Stable | NA |
| Sarvilinna et al. 19 | Finland | 1990–1999 | Decreased | NA |
| Thien et al. 27 | Norway | 1995–2009 | Increased | NA |
| Lindahl et al. 20 | Sweden | 1979–2000 | Increased | NA |
Abbreviations: NA, not applicable; PF, periprosthetic fracture.
An epidemiologic study using US Nationwide Inpatient Sample (NIS) analyzed the trend of PF frequency and showed that number of admissions due to PF after THA remained stationary from 2006 to 2010 18 .
Another study based on Scottish national registry data investigated the incidence of PF after THA and TKR over a 10‐year period from 1997 to 2008. In that study, the number of revision surgeries due to PF remained relatively stable during the study period 6 .
However, a study from the Finnish Arthroplasty Register reported a decrease of PF incidence. The authors calculated separately the PF incidence for the years 1990–1994 and 1995–1999. The incidence in the second period (15.43 [CI = 9.14–26.05] per 100,000 person years) was lower than in the first (20.45 [CI = 13.93–30.04] per 100,000 person years) 19 .
On the contrary, several studies have recently reported an increase in the incidence of PF.
Pivec et al. estimated the incidence of PF following THA based on 12 national joint registries data and created a projection model to predict the future PF burden. In the United States, the mean incidence of postoperative PFs requiring revision was 0.8%. They expected the number of PFs would rise steadily by mean 4.6% every decade over the next 30 years 8 .
Thien et al. evaluated the incidence of PF after THA using the Nordic Arthroplasty Register Association database. The risk for revision due to early PF increased during the 2003 to 2009 period compared with the 1995 to 2002 period (relative risk, 1.44 [95% CI, 1.18 to 1.69]; P < 0.0005). The incidence of revision due to PF within postoperative 2 years was 0.47% for cementless stems and 0.07% for cemented stems 27 .
Cause of the Increase in the Burden of Periprosthetic Fractures
Reportedly, there is a regional difference in the PF incidence. The difference might be related to the type of prostheses, fixation method (cemented vs cementless) and demographic characteristics in each country.
Cementless hip fixation is associated with higher rate of PF compared to cemented fixation. However, on‐table and very early postoperative death, so called bone cement implantation syndrome (BCIS), is implicated with cemented fixation 28 , 29 .
During the past decade, cementless fixation has been increasingly used in hip arthroplasty due to BCIS risk of cemented stems 17 . This indicated an increase in utilization of cementless femoral fixation for THA and hemiarthroplasty despite the association between cementless fixation and risk of PF.
In the current study, the number and economic burden of PFs increased during the last 8 years. This increase seems to be related to aging of our population, increase in the number of joint arthroplasties, and popular use of cementless stems in South Korea.
The features of PFs closely resemble those of osteoporotic fractures, especially in higher occurrence and morbidity in the elderly population 30 . In our study, 86% of periprosthetic fracture patients from 2010 to 2017 were older than 60 years of age. Many anti‐osteoporosis medications have been reported to be clinically effective in preserving periprosthetic bone mineral density, and thus effective in preventing PFs 31 , 32 , 33 , 34 . This suggests that patient education including fall prevention as well as anti‐osteoporotic medication could be an option for prevention of PFs, particularly in the elderly patients.
Limitations
A de‐identified database was used in this study. Thus, we could not identify the type of arthroplasty (THA, TKA, or arthroplasty of other joints) and the associated risk factors for PF.
In spite of these limitations, this is the first nationwide study on the future projection as well as the current trends of PF in East Asia.
Conclusion
The number of PFs and cost for treatment have risen and will be steadily rising, and PF will lead to a serious burden on the healthcare system. Further consideration to prevent PF after arthroplasty is urgently warranted.
Acknowledgments
This study was funded by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI18C0284).
Disclosure: Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1. Shields E, Behrend C, Bair J, Cram P, Kates S. Mortality and financial burden of periprosthetic fractures of the femur. Geriatr Orthop Surg Rehabil, 2014, 5: 147–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yoon BH, Lee YK, Jo WL, Ha YC, Choi DH, Koo KH. Incidence and risk period of periprosthetic femoral fracture after cementless bipolar hemiarthroplasty in elderly patients. J Arthroplasty, 2016, 31:1326–30. [DOI] [PubMed] [Google Scholar]
- 3. Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am, 2012, 94: 577–83. [DOI] [PubMed] [Google Scholar]
- 4. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am, 1999, 30:183–90. [DOI] [PubMed] [Google Scholar]
- 5. Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury, 2007, 38: 651–4. [DOI] [PubMed] [Google Scholar]
- 6. Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri‐prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br, 2011, 93: 96–101. [DOI] [PubMed] [Google Scholar]
- 7. Della Rocca GJ, Leung KS, Pape HC. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma, 2011, 25(Suppl 2): S66–70. [DOI] [PubMed] [Google Scholar]
- 8. Pivec R, Issa K, Kapadia BH, Cherian JJ, Maheshwari AJ, Bonutti PM, et al. Incidence and future projections of periprosthetic femoral fracture following primary total hip arthroplasty: an analysis of international registry data. J Long Term Eff Med Implants, 2015, 25: 269–75. [DOI] [PubMed] [Google Scholar]
- 9. Kang JS, Moon KH, Ko BS, Roh TH, Na Y, Youn YH, et al. Prognostic factors and clinical outcomes after treatment of periprosthetic femoral fractures using a cable‐plate. Hip Pelvis, 2019, 31: 166–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee JM, Kim TS, Kim TH. Treatment of periprosthetic femoral fractures following hip arthroplasty. Hip Pelvis, 2018, 30: 78–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yoshikawa R, Hiranaka T, Okamoto K, Fujishiro T, Hida Y, Kamenaga T, et al. The medial eminence line for predicting tibial fracture risk after unicompartmental knee arthroplasty. Clin Orthop Surg, 2020, 12: 166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Correa‐Valderrama A, Stangl‐Herrera W, Echeverry‐Vélez A, Cantor E, Ron‐Translateur T, Palacio‐Villegas JC. Relationship between body mass index and complications during the first 45 days after primary total hip and knee replacement: a single‐center study from South America. Clin Orthop Surg, 2019, 11: 159–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kamo K, Kido H, Kido S. Comparison of the incidence of intra‐operative fractures in hip hemi‐arthroplasty performed in supine and lateral positions. Hip Pelvis, 2019, 31: 33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cordeiro EN, Costa RC, Carazzato JG, Silva JS. Periprosthetic fractures in patients with total knee arthroplasties. Clin Orthop Relat Res, 1990, 252: 182–9. [PubMed] [Google Scholar]
- 15. Healy WL, Siliski JM, Incavo SJ. Operative treatment of distal femoral fractures proximal to total knee replacements. J Bone Joint Surg Am, 1993, 75: 27–34. [DOI] [PubMed] [Google Scholar]
- 16. Merkel KD, Johnson EW Jr. Supracondylar fracture of the femur after total knee arthroplasty. J Bone Joint Surg Am, 1986, 68: 29–43. [PubMed] [Google Scholar]
- 17. Springer BD, Etkin CD, Shores PB, Gioe TJ, Lewallen DG, Bozic KJ. Perioperative periprosthetic femur fractures are strongly correlated with fixation method: an analysis from the American Joint Replacement Registry. J Arthroplasty, 2019, 34: S352–4. [DOI] [PubMed] [Google Scholar]
- 18. Cox JS, Kowalik TD, Gehling HA, DeHart ML, Duwelius PJ, Mirza AJ. Frequency and treatment trends for periprosthetic fractures about Total hip arthroplasty in the United States. J Arthroplasty, 2016, 31: 115–20. [DOI] [PubMed] [Google Scholar]
- 19. Sarvilinna R, Huhtala HS, Puolakka TJ, Nevalainen JK, Pajamäki KJ. Periprosthetic fractures in total hip arthroplasty: an epidemiologic study. Int Orthop, 2003, 27: 359–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty, 2005, 20: 857–65. [DOI] [PubMed] [Google Scholar]
- 21. Park C, Ha YC, Jang S, Jang S, Yoon HK, Lee YK. The incidence and residual lifetime risk of osteoporosis‐related fractures in Korea. J Bone Miner Metab, 2011, 29: 744–51. [DOI] [PubMed] [Google Scholar]
- 22. Lee YK, Ha YC, Park C, Yoo JJ, Shin CS, Koo KH. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int, 2013, 24: 707–11. [DOI] [PubMed] [Google Scholar]
- 23. Lee YK, Ha YC, Park C, Koo KH. Trends of surgical treatment in femoral neck fracture: a nationwide study based on claim registry. J Arthroplasty, 2013, 28: 1839–41. [DOI] [PubMed] [Google Scholar]
- 24. Korea National Statistical Office Projected Population by Age(Korea). [Cited 2020 Mar 4]. Available from: http://www.kosis.kr/.
- 25. Ver Hoef JM, Boveng PL. Quasi‐Poisson vs. negative binomial regression: how should we model overdispersed count data. Ecology, 2007, 88: 2766–72. [DOI] [PubMed] [Google Scholar]
- 26. Gentric G, Kieffer Y, Mieulet V, Goundiam O, Bonneau C, Nemati F, et al. PML‐regulated mitochondrial metabolism enhances chemosensitivity in human ovarian cancers. Cell Metab, 2019, 29: 156–73.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thien TM, Chatziagorou G, Garellick G, Furnes O, Havelin LI, Mäkelä K, et al. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the nordic arthroplasty register association database. J Bone Joint Surg Am, 2014, 96: e167. [DOI] [PubMed] [Google Scholar]
- 28. Costain DJ, Whitehouse SL, Pratt NL, Graves SE, Ryan P, Crawford RW. Perioperative mortality after hemiarthroplasty related to fixation method. Acta Orthop, 2011, 82:275–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Middleton RG, Uzoigwe CE, Young PS, Smith R, Gosal HS, Holt G. Peri‐operative mortality after hemiarthroplasty for fracture of the hip: does cement make a difference. Bone Joint J, 2014, 96: 1185–91. [DOI] [PubMed] [Google Scholar]
- 30. Haughom BD, Basques BA, Hellman MD, Brown NM, Della Valle CJ, Levine BR. Do mortality and complication rates differ between periprosthetic and native hip fractures. J Arthroplasty, 2018, 33: 1914–8. [DOI] [PubMed] [Google Scholar]
- 31. MacKenzie SA, Ng RT, Snowden G, Powell‐Bowns M, Duckworth AD, Scott C. Periprosthetic atypical femoral fractures exist and are associated with duration of bisphosphonate therapy. Bone Joint J, 2019, 101: 1285–91. [DOI] [PubMed] [Google Scholar]
- 32. Aro HT, Nazari‐Farsani S, Vuopio M, Löyttyniemi E, Mattila K. Effect of denosumab on femoral periprosthetic BMD and early femoral stem subsidence in postmenopausal women undergoing cementless total hip arthroplasty. JBMR Plus, 2019, 3: e10217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nagoya S, Tateda K, Okazaki S, Kosukegawa I, Shimizu J, Yamashita T. Restoration of proximal periprosthetic bone loss by denosumab in cementless total hip arthroplasty. Eur J Orthop Surg Traumatol, 2018, 28: 1601–7. [DOI] [PubMed] [Google Scholar]
- 34. Suzuki T, Sukezaki F, Shibuki T, Toyoshima Y, Nagai T, Inagaki K. Teriparatide administration increases periprosthetic bone mineral density after Total knee arthroplasty: a prospective study. J Arthroplasty, 2018, 33: 79–85. [DOI] [PubMed] [Google Scholar]


