Abstract
An increasing number of people are seeking elective cosmetic change of eye color. We review the surgical techniques, outcomes and complications arising from the various existing surgical alternatives, including cosmetic iris implants—which based on the available evidence should be considered malpractice—as well as laser iris depigmentation and cosmetic keratopigmentation. Laser iris depigmentation has been used clinically for aesthetic purposes without receiving official approval or licensing. The technique can be performed in an outpatient clinic thanks to the use of neodymium: yttrium–aluminum–garnet (Nd:YAG) lasers, but scientific literature data about this treatment is very limited. Cosmetic iris implants are neither CE-marked nor Food and Drug Administration (FDA)-approved, and lead to severe complications arising from their placement including uveitis, hyphema, glaucoma, cataract, corneal endothelial damage and severe vision loss. Management of complications resulting from iris implants might require several surgical procedures, and the follow-up is difficult among these poorly informed patients. Keratopigmentation is the most extensively studied technique and had long been investigated before being introduced into clinical practice: already introduced centuries ago, it was recently developed, reporting adequate levels of safety and efficacy. The medium- and long-term cosmetic outcomes of keratopigmentation and patient satisfaction have been the subject of recent reports. The available level of evidence suggests that cosmetic keratopigmentation is the best evidence-supported surgical choice for patients seeking a permanent cosmetic eye color change. Still, additional investigation is needed to optimize the outcomes, minimize postoperative complications and further develop this and other new surgical alternatives such as laser procedures.
Keywords: Cosmetic iris implants, Eye color change, Keratopigmentation, Laser depigmentation
Key Summary Points
| Cosmetic iris implants (not yet FDA-approved or CE-marked) lead to severe loss of visual function in many cases, and their implantation should be considered malpractice. |
| Laser iris depigmentation represents a promising new surgical approach to change eye color but still lacks strong evidence about outcomes and complications in the short and medium term. |
| Femtosecond-assisted cosmetic keratopigmentation is the most widely studied technique to accomplish cosmetic eye color change by injecting mineral micronized pigments inside a stromal pocket. Medium- and long-term evidence is available for this technique. |
Introduction
Various surgical techniques have been proposed for the treatment of patients seeking an elective and permanent change of eye color. Keratopigmentation (KTP) [1–3] was comprehensively investigated before being introduced into clinical practice, but other techniques such as laser iris depigmentation, even if noting interesting results , have been used clinically even before there are relevant data in the literature [4–6]. Finally, cosmetic iris implants have been surrounded by growing malpractice controversy: even if not approved, they continue to be used in some countries, leading to tremendous complications [7–10]. No previous review reports are available on the different surgical alternatives for changing the apparent color of the eye. In the current review, we provide the technical and surgical characteristics of the various alternatives, the level of evidence existing today for their practice, and a broad view of what is reported in the literature concerning the corresponding outcomes and complications. This article is based mainly on previously conducted studies and was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Informed consent to include potentially identifiable data was acquired from all the participants. This review is important to help doctors and patients choose wisely among the different surgical alternatives, understanding the state of the art of each of them and their level of effectiveness and any eventual associated complications.
Laser Depigmentation
Surgical Techniques
The procedure uses a device mounted onto a slit-lamp biomicroscope that produces a frequency-doubled 532-nm wavelength neodymium: yttrium–aluminum–garnet (Nd:YAG) laser with different spot diameters. Yildrim et al. [4] conducted an animal study using a 900-μm spot size: they applied 200 laser shots (A.R.C. Laser, Germany) in two groups of rabbits divided according to the energy levels (group A, 0.8 mJ; group B, 1.2 mJ) with a laser application time of 3 ns. A total of 120 pulses were administered at the first session; the same dose and pulses were repeated at the second session, which was 2 weeks after the first application. Finally, both groups received 200 laser pulses at the third session to fill the gap between spots. Thus, in total, the laser was applied minimally as 352 mJ in group A (0.8 mJ × 440 pulses/three sessions) and maximally as 660 mJ in group B (1.5 mJ × 440 pulses/three sessions).
Basoglu et al. [5] treated sectorial heterochromia in a 22-year-old man with a 400-mm spot diameter. The energy level was adjusted to 0.5 mJ. The authors divided the area of treatment into three zones, and 100 pulses/day were applied on each zone to complete the treatment in 3 days. One month after the first session, the patient returned to repeat the session and complete the treatment. In both studies, pupils were constricted before laser application with miotic eye drops.
Grimaldos Ruiz [6] studied the efficacy, safety and predictability of photoablative cosmetic iridoplasty (PCI) for depigmentation of the anterior epithelium of the iris in cases of heterochromia, nevus or cosmetic indications. Treatments were performed with a 532-nm Q-switched crystal laser, with 3–4-ns pulses. Each phase consisted of four or five consecutive daily sessions, repeated every 4–6 months until finalization, with the treatment completed in two or three phases.
The STRŌMA® Laser System (available at https://www.stromamedical.com) is another investigational device that is not currently approved for commercial use. It uses a laser procedure that generates a low-energy laser beam that heats the brown pigment on the front surface of the iris, revealing the natural underlying blue or green eye. However, the STRŌMA laser procedure is not commercially available anywhere in the world and does not have a commercial release date because it is under investigation and there is no available literature on the device.
Clinical Application, Outcomes and Complications
Laser iris depigmentation has been in clinical use for aesthetic purposes without official licensing, and literature data about this treatment are sparse. It was introduced based on the satisfactory cosmetic results observed in the treatment of oculodermal melanocytosis [11] and in the dermatological treatment of cutaneous pigmentation [12]. It is proposed that eye color can be changed with this laser by reduction or elimination of melanin pigments on the anterior iris surface; however, because the procedure can only reveal the natural underlying gray stromal fibers, the patient cannot choose a blue or green eye, as the procedure cannot change a blue eye to green or a green eye to blue [6].
In an animal investigation of this novel technique, the authors reported the presence of a patchy appearance in iris tissue at the first week in group A, as well as areas showing hyperpigmentation, which diminished at the end of the eighth week. In group B, mottling became more extensive on day 30, with a grayish appearance; hyperpigmented granular areas diminished on day 60, with a broken white appearance. The authors also observed ciliary injection and mild anterior chamber reaction in all groups on the first day, which became more prominent in group B and eventually disappeared after the first week. Nevertheless, they did not administer anti-inflammatory treatment, and there was no hypopyon or prolonged anterior chamber reaction [4].
In a single case study on human treatment with a Nd:YAG laser, the authors reported an excellent cosmetic result with no side effects, and flare formation that disappeared after 3 days; however, data about intraocular pressure (IOP) and other safety parameters are missing [5]. In a prospective clinical study on 1176 eyes, the author reported high effectiveness for selective depigmentation of superficial melanin of the iris, with high predictability and patient satisfaction and no remarkable long-term complications. The only notable complication reported by the author was brief iritis in 25% of the patients, which was resolved on topical treatment [6].
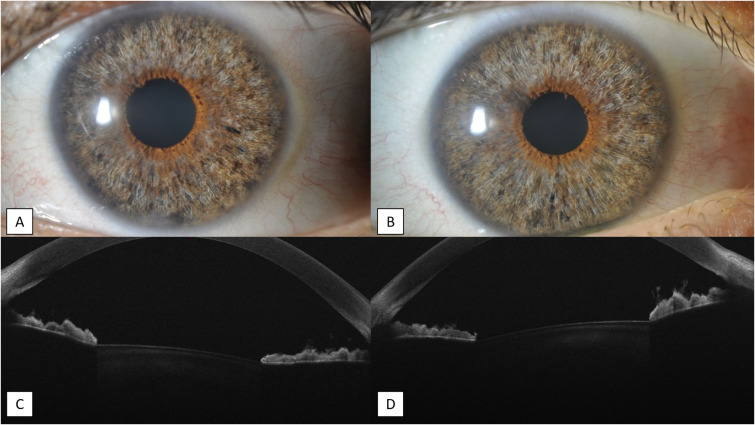
We documented the case of a 25-year-old Caucasian female who was referred to our clinic because of binocular photophobia. She had been treated in another clinic with laser iris depigmentation to change the apparent color of the eyes. At the slit-lamp examination, extensive iris stromal atrophy was present in both eyes and was confirmed with anterior segment optical coherence tomography (AS-OCT) (Fig. 1). The patient was also dissatisfied with the eye color achieved: we performed a cosmetic KTP to reduce the photophobia and, at the same time, achieved the desired cosmetic aspect.
Fig. 1.
Twenty-five-year-old female who underwent laser iris depigmentation. a, b Iris stromal severe atrophy in both eyes, only sparing the peripupillary area. c, d AS-OCT shows the loss of iris tissue corresponding to the treated areas
Cosmetic Iris Implants
Surgical Techniques
A variety of prosthetic iris implants have been used for functional, traumatic or congenital iris deficiencies since the first prosthetic iris was implanted in 1956 [13, 14]. nowadays, two medical devices are used for cosmetic purposes. The NewColorIris (Kahn Medical Devices, US patent 2006 #7025781 2B, available at https://www.google.com/patents/US7025781) is a silicone iris diaphragm with six rounded flaps at the periphery designed to hold it in place, and is between 11.0 and 13.0 mm in diameter, with a pupillary aperture of 3.5 mm and thickness of 0.16 mm. The BrightOcular (Stellar Devices LLC, US patent 2012 #8197540, available at http://www.google.com/patents/US8197540) presents some slight differences in size (11.5–13.5 mm in diameter and 0.16–0.18 mm in thickness). It is held in place by five peripheral triangular flaps, and its posterior face presents grooves to facilitate the flow of the aqueous humor [7, 9].
Neither implant has received a CE mark or Food and Drug Administration (FDA) approval, and as will be discussed later in the review, they can lead to disastrous postoperative complications. Their use is strongly discouraged; therefore, we do not consider it in the interest of this review to proceed with the specifics about the surgical implant technique and their clinical application, but only with the management of their complications.
Clinical Application, Outcomes and Complications
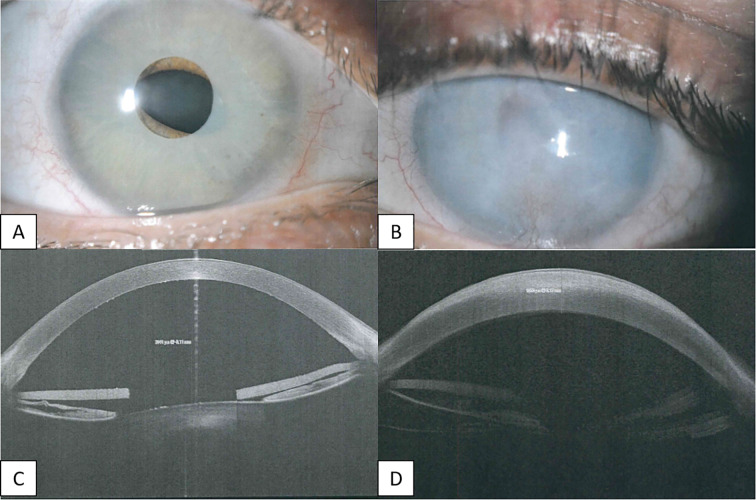
Complications arising from the placement of cosmetic iris implants are serious and include uveitis, hyphema, glaucoma, cataract, corneal endothelial damage and severe vision loss [7–10, 15–24]. Corneal complications are the most common (Fig. 2), related to corneal edema due to loss of endothelial cells (caused by low-grade chronic inflammation and anterior chamber turbulence as a result of cosmetic iris implants), which may require a corneal transplant, as well as ocular hypertension attributable to three main mechanisms: direct trauma to the trabecular meshwork, peripheral anterior synechiae (Fig. 3) and iris pigment dispersion [9, 10]. Corneal graft surgery may be required in eyes with previous glaucoma surgery, which is more challenging because the anterior segment is usually abnormal due to either synechiae or the presence of a glaucoma tube [25].
Fig. 2.
Thirty-two-year-old female with iris implant in both eyes. a, b Slit-lamp image of both eyes, showing the cosmetic iris implants with severe corneal edema in the left eye. c AS-OCT of the right eye shows the endothelial cell loss with the implant resting on the iris. d AS-OCT of the left eye shows the corneal edema
Fig. 3.
Forty-one-year-old female with iris implant in both eyes. a, b Postoperative condition of both eyes, showing severe bilateral iris atrophy. c Right eye had cataract surgery with Morcher iris-IOL device placement and Ahmed valve. d Left eye had Descemet membrane endothelial keratoplasty (DMEK). e AS-OCT of the left eye showing clear cornea with resolution of the edema after DMEK surgery, iris atrophy and peripheral anterior synechiae
Despite the lack of CE mark or FDA approval for either implant, growing malpractice has led to continued implantation of these devices, and it is common to deal with patients reporting associated complications. Hoguet et al. [10] reported the presentation and management of 14 eyes of seven patients who had NewColorIris cosmetic iris implants in Panama City, Panama: all 14 eyes were eventually treated with explantation of the iris prosthesis (between 4 and 33 months after implant placement). Intraoperative complications included suprachoroidal hemorrhage during explantation in one eye, with vision limited to hand motion. Postoperative complications included corneal edema in eight eyes, early cataract development in nine eyes and increased IOP/glaucoma in seven eyes. Descemet-stripping automated endothelial keratoplasty was performed in five eyes, penetrating keratoplasty (PKP) in one eye, cataract extraction with intraocular lens placement in seven eyes, trabeculectomy in three eyes, and glaucoma drainage implant placement in three eyes.
Mansour et al. [6] collected a collaborative case series of 12 patients who had bilateral cosmetic iris implant placement by contacting authors who had previously published reports on this topic: three cases of this series were previously presented in part as surgical videos or on PubMed [26, 27]. Eleven subjects had ocular manifestations including anterior uveitis (83.3%), glaucoma (58.3%) and corneal decompensation (50%). Despite being advised of the need for explantation of the prosthesis, four patients refused because of the positive cosmetic effect achieved. A single patient had no ocular signs and symptoms but requested prophylactic removal of the implants.
Recently, El Chehab et al. [9] reported a multicenter retrospective observational questionnaire-based study about the safety, complications and therapeutic management in a large French series of 65 eyes that underwent cosmetic iris implant placement. Of the 65 eyes analyzed, only five eyes (7.7%) did not experience any complication, and 60 eyes (92.3%) had at least one complication. The most commonly reported complication was corneal decompensation (78.5%), and 13 eyes (20%) underwent keratoplasty: of these, 11 eyes had Descemet membrane endothelial keratoplasty (DMEK), and two eyes (one patient) had PKP. Diagnosis of glaucoma was made in over half of the cases (52.3%), and filtering surgery was needed in 15 eyes (21%). Sixteen eyes had cataract surgery, with a mean patient age of 34.2 years. Explantation was needed in 81.5% of cases on average 2.3 ± 0.4 years after implantation. Among all cases, 51 eyes had a complication, and two eyes were explanted preventively. In the remaining patients, explantation was advised but was refused. The mean final visual acuity was 0.45 ± 0.08 logarithm of the minimum angle of resolution (logMAR) (0 to 2 logMAR).
Table 1 shows our series of 10 eyes of five patients referred for the management of complications arising from cosmetic iris implants (two eyes had implantation of NewColorIris, and eight eyes had implantation of BrightOcular). All the eyes were eventually explanted because of dangerous postoperative complications between 1 to 60 months after implantation. Endothelial cell density (ECD) was 848 ± 227.5, and 30% of eyes required a corneal transplant: of these, two eyes had DMEK and one eye had PKP, while three patients were advised of the need to perform corneal transplant surgery (one PKP and two DMEK) but it has not yet been performed (Fig. 4). Ninety percent of the eyes had ocular hypertension or showed signs of glaucomatous neuropathy, and filtering surgery was needed in two cases (20%) to control elevated IOP. Early development of cataract was a common complication, as 40% of our patients required cataract surgery, in one case with the implant of a Morcher iris-intraocular lens (IOL) device (Morcher GMBH, Stuttgart, Germany) because of severe iris atrophy (Fig. 3c); the mean age at the time of cataract surgery was 36 years.
Table 1.
Clinical summary of five patients with cosmetic iris implants
| Patient/eye | Age at implant | Model | Explantation/months after implantation | ECD (cells/mm2) | Corneal transplant | Iris atrophy | Cataract surgery | HTO | Glaucoma surgery |
|---|---|---|---|---|---|---|---|---|---|
| 1/R | 35 | NewColorIris | Yes/1 | 778 | No | Yes | No | No | No |
| 1/L | 35 | NewColorIris | Yes/2 | 1026 | No | Yes | No | Yes | No |
| 2/R | 37 | BrightOcular | Yes/12 | 444 | DMEK | Yes | No | Yes | No |
| 2/L | 37 | BrightOcular | Yes/12 | 1054 | Advised | No | No | Yes | No |
| 3/R | 44 | BrightOcular | Yes/32 | 814 | PKP | No | Yes | Yes | Trabeculectomy + ExPRESS shunt |
| 3/L | 44 | BrightOcular | Yes/32 | NA | No | No | Yes | Yes | No |
| 4/R | 41 | BrightOcular | Yes/40 | NA | Advised | Yes | Yes | Yes | No |
| 4/L | 41 | BrightOcular | Yes/40 | NA | DMEK | Yes | Yes | Yes | 1° Trabeculectomy + ExPRESS shunt; 2° Ahmed valve |
| 5/R | 27 | NewColorIris | Yes/60 | 972 | No | Yes | No | Yes | No |
| 5/L | 27 | NewColorIris | Yes/60 | NA | Advised | Yes | No | Yes | No |
DMEK Descemet membrane endothelial keratoplasty, ECD endothelial cell density, HTO hypertension L left eye, NA information not available, PKP penetrating keratoplasty, R right eye
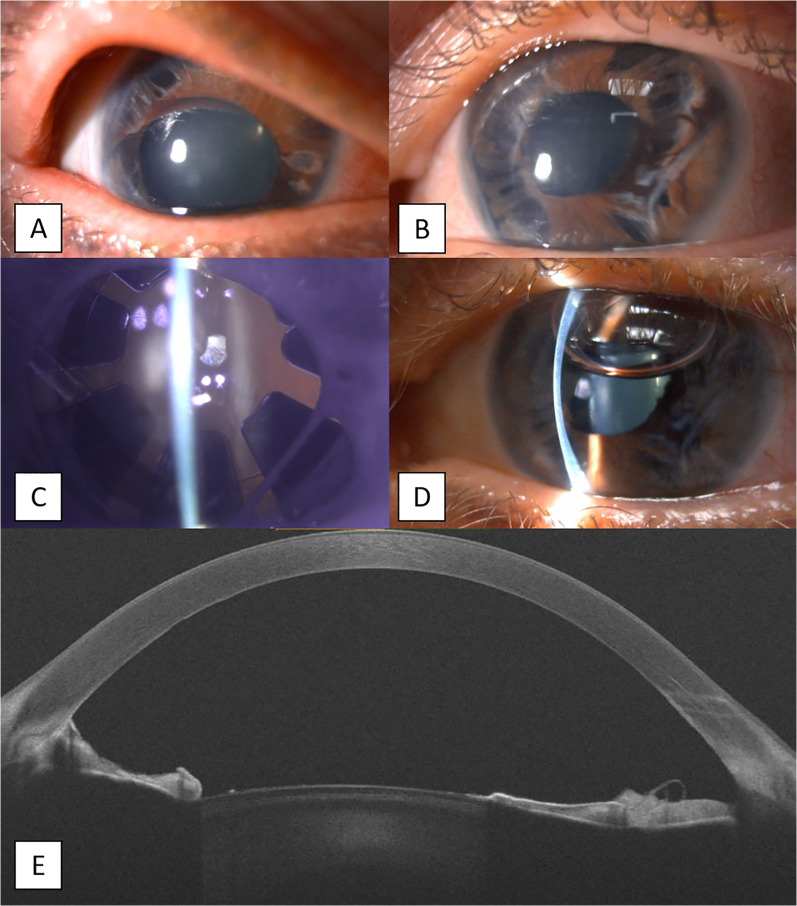
Fig. 4.
Thirty-seven-year-old female with a cosmetic implant in her left eye. a, b Preoperative condition of the eye, showing the presence of the cosmetic device and an apparent clear cornea with dramatic endothelial cell loss (1163 cells/mm2); c, d postoperative presentation, with iris atrophy most evident in the superior sector and relatively conserved endothelial cell density after the explant (1054 cells/mm2)
Cosmetic Keratopigmentation
Surgical Techniques
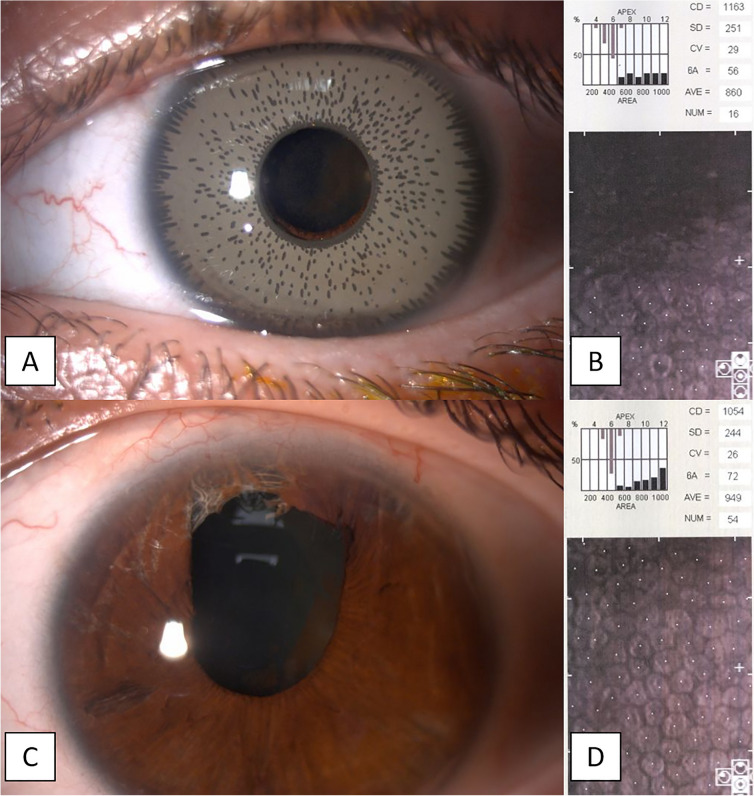
Three main surgical techniques have been described for KTP, which can be divided between intrastromal and superficial KTP. The recommended and most commonly used in cases of cosmetic KTP is femtosecond laser-assisted intrastromal KTP (FAK) [1], in which a circular stromal tunnel is created with a femtosecond laser, with pupil diameter set to an inner diameter of 5.5 mm and an outer diameter of 9.5 mm: the tunnel is eventually opened to the periphery of the cornea with a lamellar dissector until reaching the limbus (KTP corneal dissector; Epsilon, Irvine, CA), followed by the injection of the pigment through the superior incision using a 27-gauge flat cannula (Fig. 5) [1–3, 28, 29].
Fig. 5.

Postoperative appearance of a sample of three patients after femtosecond laser-assisted cosmetic keratopigmentation
Manual intralamellar KTP (MIK) is a surgical alternative for those clinics that do not have a femtosecond laser. Two to four freehand incisions are performed from the limbus to the border of a previously marked pupil. The cornea is then dissected intralamellarly and circumferentially using a microcrescent blade and helicoidal intrastromal corneal dissectors [2].
Afterward, the pigment is injected as described above [30, 31]. We recommend the use of a femtosecond laser for the creation of the stromal tunnel, as it allows a precise cut that can be created at any stromal depth.
Finally, superficial automated KTP (SAK) uses a special micropuncture device [Vissum Eye MP System, Madrid, Spain (Apl. No. 2.949.539), provided by BIOTIC Phocea, France] with a customized set of power and depth according to the individual case, to deliver the pigments to the superficial layers of the cornea [2, 32–34]. The center of the cornea is previously marked with a caliper, and the pupil size is determined by an optic zone marker (Katena, NY, USA). SAK is recommended in cases of deep and dense corneal opacities or for fine-tuning the details of the iris pattern, but not as the first treatment choice for a patient seeking an elective change of eye color.
Third-generation customized mineral micronized pigments were manufactured following the Ministry of Health and Annex IV of European Regulation of Cosmetics: the CE mark certified that pigments (BIOTIC Phocea, France) are composed of different amounts of lactic acid, propanediol and micronized mineral pigments [color index: 77,007, 77,491, 77,499, 77,492, 77,288 and 77,891]. Mineral micronized pigments were prepared according to the cosmetic desires of the patients based on a proposed list of colors, and computer simulations were also performed in most cases using the patient’s picture and the proposed or selected color to determine the most suitable one in agreement with the surgeon [1].
Clinical Application, Outcomes and Complications
This technique has the greatest volume of scientific evidence, in addition to high quality in its therapeutic and cosmetic application. Alio et al. in 2016 reported for the first time the outcomes of seven patients treated with cosmetic KTP for elective change of eye color [3]. The authors reported excellent stability of the pigmentation pattern over a follow-up of up to 2.5 years, with no signs of ocular toxicity or changes in patients' vision and astigmatism, thus representing a valid and safe surgical option for patients motivated to change their eye color. In 2021, D'Oria et al. prospectively reported the medium- and long-term outcomes of 79 normally sighted eyes of 40 patients who underwent cosmetic KTP, with an average follow-up of 29 months up to a maximum of 69 months [1]. The observer’s evaluation was excellent in 90% of cases, defined as agreement between the proposed and the achieved color and a very natural appearance. Patient satisfaction was excellent in 92.5% of cases, and all the patients indicated that they would repeat the surgery. No significant changes in topographic, pachymetric or refractive values or visual acuity were reported, thus confirming the safety of the procedure. With regard to complications, two patients experienced intraoperative pigment dispersion at the site of a previous laser-assisted in situ keratomileusis (LASIK) flap interface; no other intraoperative complications or any other intraoperative problems related to the surgical procedure were observed in any case. Twelve patients (30%) complained of excessive light sensitivity, which eventually disappeared during the first postoperative month and was absent in the newest patients treated by deepening the stromal pocket at more than 250 µm to avoid stimulating the subbasal corneal nerve plexus. One patient (2.5%), who had prior LASIK surgery, developed bilateral and progressive corneal ectasia after 6 months which was successfully treated with a standard epithelium-off corneal collagen cross-linking (CXL), being stable throughout 2 years of follow-up after the CXL procedure. We recommend against performing KTP in a LASIK patient, as LASIK might represent a contraindication according to our evidence. Nevertheless, our evidence shows that photorefractive keratectomy (PRK) does not represent a contraindication to KTP. Failure to meet the cosmetic expectation can cause dissatisfaction for patients after cosmetic procedures; we recommend using preoperative photo-editing software and discussing the color in consultation with the patient.
Discussion
Individuals who wish to change the cosmetic appearance of their eyes can resort to various surgical techniques that achieve this through a permanent change of the apparent eye color. Although different techniques have been described, some are not yet advisable or are contraindicated due to the low level of evidence available, the level of development, and their safety profile. Complications arising from the placement of cosmetic iris implants are serious and have been described secondary to both BrightOcular and NewColorIris implantation [7–10, 20–22]. The reported case series have documented the occurrence of severe complications related to anterior segment damage, such as uveitis glaucoma and corneal decompensation, which can lead to severe and permanent visual loss and the need for secondary treatments [7–10]; also, patients usually reported no follow-up after surgery in the country where implantation was performed, as they were poorly informed [9]. Based on the retrospective nature of the available literature, it is not possible to determine the exact incidence of complications; however, since this is a cosmetic procedure, the presence of serious complications with devastating visual consequences would be considered unacceptable, and argues against this cosmetic implant for any patient. Laser iris depigmentation represents an innovative technique that is emerging in the clinical panorama, but it has not yet been studied extensively by several authors: data on animal studies, a single human case report, and one prospective clinical study are available in the literature [4–6]. Therefore, this technique still needs to be validated by different “external” authors. KTP is the most widely studied of all techniques: introduced centuries ago, it was developed and perfected by our research team to achieve an excellent safety and efficacy profile, and has been used for a wide range of therapeutic, functional and cosmetic applications [1–3, 28–30, 35–38]. The outcomes of 79 eyes treated for purely cosmetic purposes have been reported by the authors [1], showing the complications that have emerged along the learning and study curve of this new technique and which have now disappeared in its most recent version: the functional, topographical and pachymetric parameters of the treated eyes are not modified by this technique, no eye has suffered complications that permanently compromise vision, and all patients have been extremely satisfied with the aesthetic outcome, thanks to the duration and resistance of the new micronized mineral pigments in use [30, 31].
Conclusion
Patients seeking to permanently change eye color can resort to various surgical techniques. Placement of cosmetic iris implants represents a surgical option that carries a high risk of definitive loss of vision as well as other serious complications that should be emphasized to patients. Such a procedure can definitely be considered as malpractice and should be discouraged. However, this surgical practice is still used in many countries, and it is necessary to be prepared to face any problems connected with it. Laser iris depigmentation represents an innovative and promising technique that is emerging in the clinical panorama. It has the advantage of being able to be performed in an outpatient clinic thanks to the use of Nd:YAG lasers, but it has not yet been studied extensively. KTP is the most widely studied of all techniques: the high safety and efficacy of this technique make its elective application the best option for a suitably selected patient who wishes to change the apparent color of the eye. Nevertheless, more studies are needed to develop pigments that are more natural and do not change with time.
Acknowledgments
Funding
This study has been financed in part by the Network for Cooperative Research in Health “OFTARED”—Reference: RD16/0008/0012. Funded by Instituto de Salud Carlos III and co-funded by European Regional Development Fund (ERDF), Project “A way to make Europe". No funding or sponsorship was received for publication of this article.
Authorship
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Manuscript writing (Francesco D'Oria and Jorge L. Alio). Data generation & analysis (Francesco D'Oria, Sabat K. Abu-Mustafa and Jorge L. Alio). Critical review (Sabat K. Abu-Mustafa and Jorge L. Alio).
Disclosures
Francesco D’Oria, Sabat K. Abu-Mustafa and Jorge L. Alio confirm that they have nothing to disclosure.
Compliance with Ethics Guidelines
The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. Informed consent to include potentially identifiable data was acquired from all the participants.
Data Availability
Data generated or analysed during this study are included in the manuscript.
References
- 1.D’Oria F, Alio JL, Rodriguez AE, Amesty MA, Abu-Mustafa SK. Cosmetic keratopigmentation in sighted eyes: medium and long-term clinical evaluation. Cornea. 2021;40(3):327–333. doi: 10.1097/ICO.0000000000002417. [DOI] [PubMed] [Google Scholar]
- 2.Alio JL, Rodriguez AE, Toffaha BT. Keratopigmentation (corneal tattooing) for the management of visual disabilities of the eye related to iris defects. Br J Ophthalmol. 2011;95:1397–1401. doi: 10.1136/bjophthalmol-2011-300170. [DOI] [PubMed] [Google Scholar]
- 3.Alió JL, Rodriguez AE, El Bahrawy M, Angelov A, Zein G. Keratopigmentation to change the apparent color of the human eye: a novel indication for corneal tattooing. Cornea. 2016;35:431–437. doi: 10.1097/ICO.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 4.Yildirim Y, Duzgun E, Kar T, et al. Evaluation of color-changing effect and complications after Nd:YAG laser application on iris surface. Med Sci Monit. 2016;22:107–114. doi: 10.12659/MSM.895086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basoglu A, Çelik U. The effect of SLT laser application on iris to treat sectorial heterochromia: a promising technique. Eye Contact Lens. 2018;44(Suppl 1):S352–S354. doi: 10.1097/ICL.0000000000000374. [DOI] [PubMed] [Google Scholar]
- 6.Grimaldos Ruiz P. Photoablative cosmetic iridoplasty: effective, safe, and predictable-eye color change in 1176 eyes. Int Ophthalmol. 2021 doi: 10.1007/s10792-021-01693-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mansour AM, Ahmed IIK, Eadie B, et al. Iritis, glaucoma and corneal decompensation associated with BrightOcular cosmetic iris implant. Br J Ophthalmol. 2016;100:1098–1101. doi: 10.1136/bjophthalmol-2015-307295. [DOI] [PubMed] [Google Scholar]
- 8.Galvis V, Tello A, Corrales MI. Postoperative results of cosmetic iris implants. J Cataract Refract Surg. 2016;42:1518–1526. doi: 10.1016/j.jcrs.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 9.El Chehab H, Gatinel D, Baudouin C. Complications of cosmetic iris implants: French series of 87 eyes. J Cataract Refract Surg. 2020;46(1):34–39. doi: 10.1097/j.jcrs.0000000000000032. [DOI] [PubMed] [Google Scholar]
- 10.Hoguet A, Ritterband D, Koplin R, et al. Serious ocular complications of cosmetic iris implants in 14 eyes. J Cataract Refract Surg. 2012;38:387–393. doi: 10.1016/j.jcrs.2011.09.037. [DOI] [PubMed] [Google Scholar]
- 11.Park JH, Kim JY, Kim MJ, Tchah H. Efficacy and safety of combination treatment for oculodermalmelanocytosis: surgical reduction and use of 532-nm Q-switched Nd: YAG laser. Cornea. 2014;33:832–837. doi: 10.1097/ICO.0000000000000159. [DOI] [PubMed] [Google Scholar]
- 12.Anderson RR, Margolis RJ, Watenabe S, et al. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd:YAG laser pulses at 1064, 532, and 355 nm. J Invest Dermatol. 1989;93:28–32. doi: 10.1111/1523-1747.ep12277339. [DOI] [PubMed] [Google Scholar]
- 13.Burk SE, Da Mata AP, Snyder ME, Cionni RJ, Cohen JS, Osher RH. Prosthetic iris implantation for congenital, traumatic, or functional iris deficiencies. J Cataract Refract Surg. 2001;27:1732–1740. doi: 10.1016/S0886-3350(01)01124-5. [DOI] [PubMed] [Google Scholar]
- 14.Pozdeyeva NA, Pashtayev NP, Lukin VP, Batkov YN. Artificial iris-lens diaphragm in reconstructive surgery for aniridia and aphakia. J Cataract Refract Surg. 2005;31:1750–1759. doi: 10.1016/j.jcrs.2005.02.037. [DOI] [PubMed] [Google Scholar]
- 15.Anderson JE, Grippo TM, Sbeity Z, Rich R. Serious complications of cosmetic NewColorIris implantation. Acta Ophthalmol. 2010;88:700–704. doi: 10.1111/j.1755-3768.2008.01499.x. [DOI] [PubMed] [Google Scholar]
- 16.Thiagalingam S, Tarongoy P, Hamrah P, et al. Complications of cosmetic iris implants. J Cataract Refract Surg. 2008;34:1222–1224. doi: 10.1016/j.jcrs.2008.02.035. [DOI] [PubMed] [Google Scholar]
- 17.Arthur SN, Wright MM, Kramarevsky N, Kaufman SC, Grajewski AL. Uveitis-glaucoma-hyphema syndrome and corneal decompensation in association with cosmetic iris implants. Am J Ophthalmol. 2009;148:790–793. doi: 10.1016/j.ajo.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 18.George MK, Tsai JC, Loewen NA. Bilateral irreversible severe vision loss from cosmetic iris implants. Am J Ophthalmol. 2011;151:872–875. doi: 10.1016/j.ajo.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Ali MH, Traish AS. Elevated intraocular pressure and endothelial cell loss following iris color change. JAMA Ophthalmol. 2016;134(8):939–940. doi: 10.1001/jamaophthalmol.2015.6145. [DOI] [PubMed] [Google Scholar]
- 20.Chaurasia S. Devastating complication of cosmetic iris implants. Indian J Ophthalmol. 2017;65(8):771–772. doi: 10.4103/ijo.IJO_537_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bore M, Choudhari N, Chaurasia S. Management of complications of cosmetic iris implants in a phakic eye: a case report and literature review. Int Ophthalmol. 2019;39(5):1141–1146. doi: 10.1007/s10792-018-0893-3. [DOI] [PubMed] [Google Scholar]
- 22.Narang P, Mehta K, Agarwal A. Phacoemulsification with single-pass four-throw pupilloplasty and pre-Descemet's endothelial keratoplasty for management of cosmetic iris implant complication. Indian J Ophthalmol. 2018;66:841–844. doi: 10.4103/ijo.IJO_559_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kerr NM, Kong YXG, Skalicky SE, Green C. Sight-threatening complications of cosmetic iris implants. Clin Exp Ophthalmol. 2018;46:955–956. doi: 10.1111/ceo.13194. [DOI] [PubMed] [Google Scholar]
- 24.Shalash A, El Bahrawy M. Five-slice technique for the explantation of complicated BrightOcular© cosmetic iris implants. Int Ophthalmol. 2020;40:1565–1570. doi: 10.1007/s10792-020-01328-1. [DOI] [PubMed] [Google Scholar]
- 25.Abdelghany A, D’Oria F, Alio JL. Surgery of glaucoma in modern corneal graft procedures. Surv Ophthalm. 2021;66(2):276–289. doi: 10.1016/j.survophthal.2020.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Kelly A, Kaufman SC. Corneal endothelial cell loss and iritis associated with a new cosmetic iris implant. JAMA Ophthalmol. 2015;133:723–724. doi: 10.1001/jamaophthalmol.2015.0488. [DOI] [PubMed] [Google Scholar]
- 27.Luk S, Spiteri A, Muthusamy K, Mearza AA. Cosmetic iris implantation complicated by secondary angle closure. Cont Lens Anterior Eye. 2015;38:142–143. doi: 10.1016/j.clae.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 28.Alió JL, Rodriguez AE, Toffaha BT, Pinero D, Moreno LJ. Femtosecond assisted keratopigmentation for functional and cosmetic restoration in essential iris atrophy. J Cataract Refract Surg. 2011;37:1744–1747. doi: 10.1016/j.jcrs.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Alio JL, Rodriguez AE, Toffaha BT, El Aswad A. Femtosecond-assisted keratopigmentation double tunnel technique in the management of a case of Urrets-Zavalia syndrome. Cornea. 2012;31:1071–1074. doi: 10.1097/ICO.0b013e318243f6b1. [DOI] [PubMed] [Google Scholar]
- 30.Amesty MA, Rodriguez AE, Hernández E, De Miguel MP, Alio JL. Tolerance of micronized mineral pigments for intrastromal keratopigmentation: a histopathology and immunopathology experimental study. Cornea. 2016;35:1199–1205. doi: 10.1097/ICO.0000000000000900. [DOI] [PubMed] [Google Scholar]
- 31.Amesty MA, Alio JL, Rodriguez AE. Corneal tolerance to micronised mineral pigments for keratopigmentation. Br J Ophthalmol. 2014;98:1756–1760. doi: 10.1136/bjophthalmol-2014-305611. [DOI] [PubMed] [Google Scholar]
- 32.Al-Shymali O, Rodriguez AE, Amesty MA, Alio JL. Superficial keratopigmentation: an alternative solution for patients with cosmetically or functionally impaired eyes. Cornea. 2019;38:54–61. doi: 10.1097/ICO.0000000000001753. [DOI] [PubMed] [Google Scholar]
- 33.Alio J, Agdeppa M, Uceda-Montanes A. Femtosecond laser-assisted superficial keratectomy for the treatment of superficial corneal leukomas. Cornea. 2011;30:301–307. doi: 10.1097/ICO.0b013e3181eeb0c1. [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez AE, Amesty MA, El Bahrawy M, Rey S, Alio del Barrio JL, Alio JL. Superficial automated keratopigmentation for Iris and pupil simulation using micronized mineral pigments and a new puncturing device: an experimental study. Cornea. 2017;36:1069–1075. doi: 10.1097/ICO.0000000000001249. [DOI] [PubMed] [Google Scholar]
- 35.Alio JL, Sirerol B, Walewska-Szafran A, et al. Corneal tattooing (keratopigmentation) with new mineral micronised pigments to restore cosmetic appearance in severely impaired eyes. Br J Ophthalmol. 2010;94:245–249. doi: 10.1136/bjo.2008.149435. [DOI] [PubMed] [Google Scholar]
- 36.Laria C, Alio J, Pinero D. Intrastromal corneal tattooing as treatment in a case of intractable strabismic diplopia (double binocular vision) Binocul Vis Strabismus Q. 2010;25:238–242. [PubMed] [Google Scholar]
- 37.Alio J, Al-Shymali O, Amesty MA, et al. Keratopigmentation with micronised mineral pigments: complications and outcomes in a series of 234 eyes. Br J Ophthalmol. 2018;102:742–747. doi: 10.1136/bjophthalmol-2017-310591. [DOI] [PubMed] [Google Scholar]
- 38.D'Oria F, Barraquer R, Alio JL. Crystalline lens alterations in congenital aniridia. Arch Soc Esp Oftalmol (Engl Ed). 2021 doi: 10.1016/j.oftal.2020.12.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data generated or analysed during this study are included in the manuscript.