Abstract
Introduction and importance
Distal femoral growth plate fracture is one of the most common growth plate fractures in the pediatric age, and associated with growth disturbance risk. Consequences that may arise are hindered growth, irreversible decrease in range of motion, instability, angular deformity and neurovascular issues. Fractures of the lateral condyle show a higher risk of developing sequelae compared to the medial side.
Case presentation
Corrective osteotomy of the distal femur was performed in patient with history of femoral fracture which undergone an ORIF procedure for the shaft at the previous hospital, while the lateral condyle fracture was treated conservatively. We did close wedge osteotomy medially and transferred the bone fragment to the lateral side as an open wedge to lengthen the lateral cortex. The leg-length discrepancy was reduced from 5 to 2 cm even though subsequent deformities may possibly occur.
Clinical discussion
The management approach for fracture of distal femoral physis can be done conservatively or surgically. Unfavorable outcomes from the conservative approach gave more reasons to opt for a surgical approach. The growth plate location should be considered when deciding which level of osteotomy is best and the fixation points in younger patients. When physeal bars are formed due to the fracture stress on the growth plate, the treatment is based on the patient's age and the bar's size.
Conclusion
Fractures of the distal femur involving a growth plate in children should not be considered a trivial case, and a comprehensive treatment plan should be coordinated.
Keywords: Case report, Neglected pediatric fracture, Distal femoral fracture, Physeal plate, Osteotomy
Highlights
-
•
Distal femoral fracture is one of the most common growth plate fracture in pediatric associated with growth disturbance and growth arrest
-
•
Fracture occurring on the lateral condyle show a higher risk of developing sequelae compared to the medial condyle fracture
-
•
Pediatric distal femoral fractures managed conservatively using a long-leg cast only would not sustain reduction and often ended up losing the reduction
-
•
Internal fixation being recommended to be done regardless of displacement severity occurring with distal femoral fracture
-
•
Growth plate location should be considered when deciding the level of osteotomy and fixation points
1. Introduction
The distal femoral epiphysis is an anatomical feature developed congenitally and present since birth bilaterally. The distal epiphysis contributes to both medial and lateral femoral condyles, acting as an anatomical site for gastrocnemius muscle insertion. It fuses proximally with the metaphysis around mid-teen, with girls occurring approximately two years earlier than boys. As distal femoral epiphysis comprises a physeal plate, it is responsible for the growth of the majority of the femur and more than a third of the lower extremity's total length. Compared to other existing physis in the body, the distal femoral epiphysis is the fastest-growing physis with a growth rate of 1.0 cm annually [1], [2], [3], [4].
The distal femoral growth plate fracture is the third most common growth plate fracture in the pediatric age group and is, unfortunately, associated with growth disruption risk in up to 90% of cases. When distal femoral epiphysiolysis occurs, growth disturbance, angular deformities, reduced range of movement, instability, and neurovascular issues are the most commonly seen consequences. A meta-analysis data showed that 52% of reported growth plate fractures developed growth disturbance. Fractures accompanied with a displaced fragment were shown to have a higher incidence of more than twice in developing growth disturbance and growth arrest by four times compared to growth plate fracture without displacement [1], [5], [6].
In classifying physeal fractures, the Salter-Harris (SH) classification remains the most extensively utilized classification system which aids in assuming probable injury mechanisms and predicting possible following complications. Out of the five possible types in the classification, distal femoral physeal fractures are commonly seen with SH type II fractures, not excluding possibilities of other fracture types occurring. Complications that may arise are hindered growth, irreversible decrease in range of motion, and angular deformity [1], [7], [8].
Although SH Type II fracture is the most commonly reported physeal fracture, SH type IV fracture seems to have the worst impact on bone growth demonstrated by having the highest incidence of growth rate disturbance compared to other SH fracture types. Overall, more than one-fifth of the growth plate fracture occurring on distal femurs exhibited leg length discrepancy of more than 1.5 cm as a sequela, reported from pooled data [1], [7], [8].
Leaving out fixation as part of the treatment plan has shown to progress into growth abnormality in almost 60% of fractures reported, with more than a third overall being severe. Although another study revealed a higher proportion of growth disturbance seen in patients treated with fixation, there seems to be a significant reduction of severe growth disturbance cases than those without fixation (27% vs. 37%). As mentioned before, distal femoral physeal fractures commonly co-occur with displacement, more often in the coronal plane. Compared to whichever treatment plan chosen, the presence of displacement along with fracture pattern is believed to have a more superior role in determining the outcome [1], [5], [9].
As a complex consequence of distal femoral physis fracture, physeal bar formation may develop due to the stress-strain targeted on the growing physeal plate. Early physeal closure is likely to occur, resulting in angled deformity and discrepancy in leg length. Development of physeal bar occurs in more than one-fifth of distal femoral epiphysis fracture patients, with prepubescent patients having a greater contribution to this incidence. As prepubescent patients tend to have thicker layers surrounding their bone and cartilage, a higher magnitude of trauma is necessary to cause disorder to these and deeper structures and is usually related to crushing injuries. In contrast, with thinner periosteum, the teenage population and older tend to require less impact energy to cause such trauma [1], [2], [3], [5].
Although both are formed from distal femoral epiphysis, fracture occurring on the lateral condyle was reported to show a higher risk of developing sequelae by almost five times compared to the medial condyle fracture. Higher complication risk subsequent to lateral condyle fracture includes the likelihood of requiring surgery in the future, followed by early physeal closures. The required magnitude of force placed during an injury may explain why lateral femoral condyle fracture would lead to a worse outcome like it did on prepubescent subjects. Knock knees and poor feet posture observed on gait are possible consequences of a genu valgum deformity. This increase in Q angle eventually leads to patellofemoral joint instability as the joint subluxated laterally. Finally, osteoarthritis may develop after prolonged strain on the lateral knee compartment. The importance of knee misalignment revision by evening the weight distribution is ever so highlighted to avoid this implicated domino effect [1], [2], [3].
2. Case presentation
An 11-year old girl with a closed fracture of middle third of the left femoral shaft due to a motorcycle traffic accident had undergone a surgical procedure of open reduction and internal fixation with plate and screws for the fracture at a local district hospital. Several days after the surgery, the patient still complained of pain on the lateral side of her knee joint. Radiograph evaluation, including her distal femur area, revealed a lateral condyle fracture Salter-Harris type III and was treated conservatively 6 months before at the previous hospital.
Several months after the surgery, the patient still reported pain in her thigh, with visual analogue scale 5, and her knee had become valgus. Then she had another deformity correction by the other surgeon. After 18 months, the patient perceived worsening leg length discrepancy, and her thighs had returned to valgus alignment.
The corrective osteotomy of the distal femur was performed at our Pediatric Orthopaedics division of Hasan Sadikin General Hospital in Bandung, Indonesia. Removal of the implant was done from the previous medial incision, and we did close wedge osteotomy medially and transferred the bone fragment to the lateral side as an open wedge to lengthen the lateral cortex. The leg-length discrepancy was reduced from 5 to 2 cm. After the procedure, there was no complication observed. The patient was then discharged from the hospital for outpatient follow-up. This report is in line with the updated SCARE (Surgical Case Report) 2020 guidelines [10] (Fig. 1).
Fig. 1.
Plain radiograph of the patient from the previous hospital: (A) Post-operative revealed a lateral condyle fracture treated conservatively; (B) valgus knee seen; (C) after the second surgical procedure for deformity correction.
3. Discussion
The management approach for fracture of distal femoral physis can be done in numerous techniques, conservatively or surgically. Conservative approaches include placement of casting and traction, or even both, followed by constant monitoring of whether fragment displacement is present or not. Case reviews have shown that a single approach of only using a long-leg cast would not sustain reduction and that seven out of 10 distal femoral fractures managed conservatively ended up losing the reduction as early as the following couple of weeks. More than half of patients with fractures accompanied by displacement had varying fair to poor end-results, described as having reduced range of movement of at least 10 degree, LLD of more than 1 cm, or knee joint deformity angled more than 5°, whether it is varus or valgus. These complications were also seen within less than a year after the initial trauma in up to 90% of pediatric patients managed conservatively [7], [9], [11], [12].
These unfavorable outcomes gave more reasons to opt for a surgical approach, which a study has recommended for internal fixation to be done regardless of displacement severity occurring with distal femoral fracture. Different surgical approaches encompass a screw-only construct, plate and screw construct, and a screw and cross-pin Kirschner wire construct, a percutaneous procedure, an open arthrotomy, or arthroscope-aided techniques. Compared to procedures that cross the physeal plate, such as crossed Steinmann pins, fixation approaches like metaphyseal cannulated screws showed a lower incidence rate of long-term problems by avoiding interference to the plate (30% vs. 65%) [13], [14], [15], [16].
Unlike adult patients, whose osteotomy site can be near the joint line, growth plate location should be considered when deciding which level of osteotomy is best and the fixation points in younger patients. When physeal bars are formed due to the fracture stress on the growth plate, removal of them and complete and contralateral epiphysiodesis are practicable to treat failed excisions. These can be done in children with five years, or even less, growth potential left and physeal bar that occupies more than one-third of physeal plate area [11], [12], [13], [17].
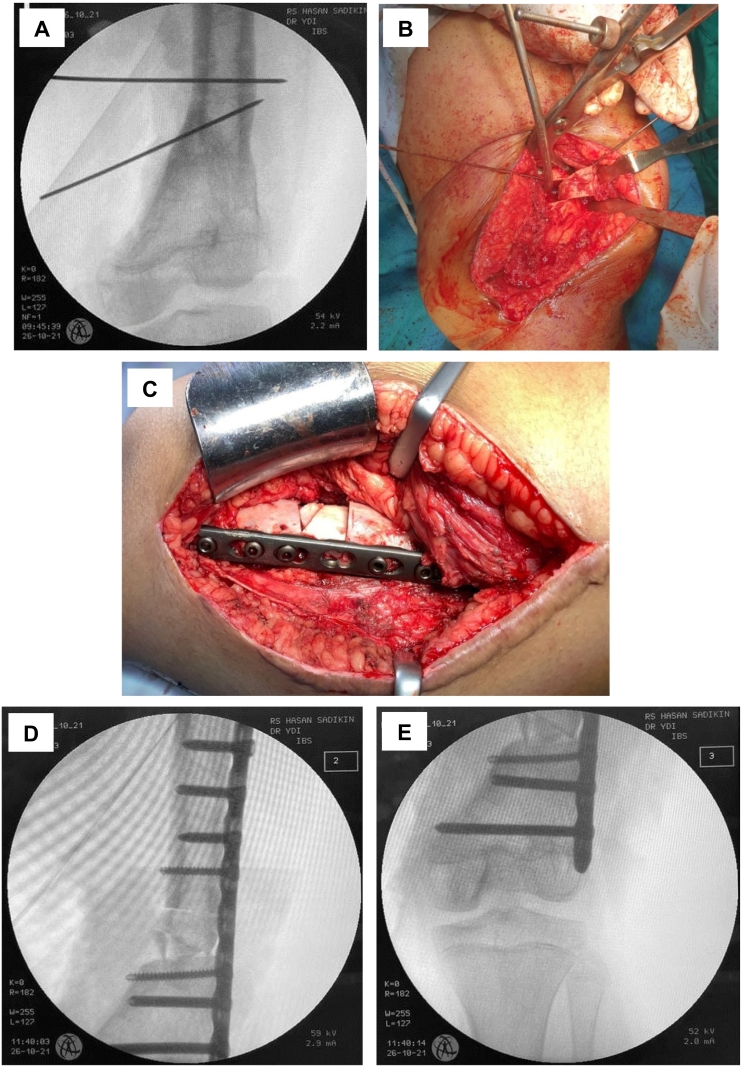
In our patient discussed earlier, we performed corrective osteotomy of the distal femur. Removal of the implant was done from the previous medial incision, and we did close wedge osteotomy medially and transferred the bone fragment to the lateral side as a close wedge to lengthen the lateral cortex. The leg-length discrepancy was reduced from 5 to 2 cm. However, subsequent deformities may still occur, and, thus, a hemiepiphysiodesis is planned to be performed in the near future (Fig. 2).
Fig. 2.
Corrective osteotomy which performed in the patient: (A) Osteotomy marking using wires; (B) slide the wedge-bone fragment laterally; (C) intraoperative wedge-bone fragment position after fixation with a locking plate; (D, E) intraoperative fluoroscopy evaluation.
4. Conclusion
A distal femoral fracture involving a growth plate should not be considered a trivial case, and a comprehensive treatment plan should be coordinated. The risk of future complications, which extends beyond just growth disruption, should be meticulously informed to the patient and their families.
Sources of funding
The authors declare that this study had no funding resource.
Ethical approval
The informed consent form was declared that patient data or samples will be used for educational or research purposes. Our institutional review board also do not provide an ethical approval in the form of case report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Hilmi Muhammad: Conceptualization, Methodology, Writing- Reviewing and Editing.
Muhammad Riyad Filza and Afrisya Bimo Siwendro: Data curation, Investigation, Writing- Original draft preparation.
Yoyos Dias Ismiarto Supervision, Writing- Reviewing and Editing.
Research registration
Not applicable.
Guarantor
Hilmi Muhammad.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We thank patient family, the surgical team and the nursing staff who were involved in the surgery and patients care.
References
- 1.Wall E.J., May M.M. Growth plate fractures of the distal femur. J. Pediatr. Orthop. 2012;32(Suppl. 1):S40–S46. doi: 10.1097/BPO.0b013e3182587086. [DOI] [PubMed] [Google Scholar]
- 2.Loder R.T., O'Donnell P.W., Feinberg J.R. Epidemiology and mechanisms of femur fractures in children. J. Pediatr. Orthop. 2006;26(5):561–566. doi: 10.1097/01.bpo.0000230335.19029.ab. [DOI] [PubMed] [Google Scholar]
- 3.John R., Sharma S., Raj G.N., Singh J., Varsha C., Arjun R.H.H., et al. Current concepts in paediatric femoral shaft fractures. Open Orthop. J. 2017;11:353–368. doi: 10.2174/1874325001711010353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pennock A.T., Ellis H.B., Willimon S.C., Wyatt C., Broida S.E., Dennis M.M., et al. Intra-articular physeal fractures of the distal femur: a frequently missed diagnosis in adolescent athletes. Orthop. J. Sports Med. 2017;5(10) doi: 10.1177/2325967117731567. 2325967117731567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basener C.J., Mehlman C.T., DiPasquale T.G. Growth disturbance after distal femoral growth plate fractures in children: a meta-analysis. J. Orthop. Trauma. 2009;23(9):663–667. doi: 10.1097/BOT.0b013e3181a4f25b. [DOI] [PubMed] [Google Scholar]
- 6.Arkader A., Warner W.C., Jr., Horn B.D., Shaw R.N., Wells L. Predicting the outcome of physeal fractures of the distal femur. J. Pediatr. Orthop. 2007;27(6):703–708. doi: 10.1097/BPO.0b013e3180dca0e5. [DOI] [PubMed] [Google Scholar]
- 7.Kocher M.S., Sink E.L., Blasier R.D., Luhmann S.J., Mehlman C.T., Scher D.M., et al. Treatment of pediatric diaphyseal femur fractures. J. Am. Acad. Orthop. Surg. 2009;17(11):718–725. doi: 10.5435/00124635-200911000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Bellamy J.T., Ward L.A., Fletcher N.D. Evaluation of pediatric distal femoral physeal fractures and the factors impacting poor outcome requiring further corrective surgery. J. Pediatr. Orthop. B. 2021;30(1):6–12. doi: 10.1097/BPB.0000000000000733. [DOI] [PubMed] [Google Scholar]
- 9.Adams A.J., Mahmoud M.A.H., Wells L., Flynn J.M., Arkader A. Physeal fractures of the distal femur: does a lower threshold for surgery lead to better outcomes? J. Pediatr. Orthop. B. 2020;29(1):40–46. doi: 10.1097/BPB.0000000000000664. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Heerwaarden R., Brinkman J.M., Pronk Y. Correction of femoral valgus deformity. J. Knee Surg. 2017;30(8):746–755. doi: 10.1055/s-0037-1602138. [DOI] [PubMed] [Google Scholar]
- 12.Brinkman J.M., Freiling D., Lobenhoffer P., Staubli A.E., Heerwaarden R.J. Supracondylar femur osteotomies around the knee: patient selection, planning, operative techniques, stability of fixation, and bone healing. Orthopade. 2014;43(Suppl. 1):S1–S10. doi: 10.1007/s00132-014-3007-6. [DOI] [PubMed] [Google Scholar]
- 13.Khoriati A., Jones C., Gelfer Y., Trompeter A. The management of paediatric diaphyseal femoral fractures: a modern approach. Strategies Trauma Limb. Reconstr. 2016;11(2):87–97. doi: 10.1007/s11751-016-0258-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker P., McMurtry I., Port A. The treatment of distal femoral fractures in children using the liss plate: a report of two cases. Ann. R. Coll. Surg. Engl. 2008;90(4):W4–W6. doi: 10.1308/147870808X302985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garrett B.R., Hoffman E.B., Carrara H. The effect of percutaneous pin fixation in the treatment of distal femoral physeal fractures. J. Bone Joint Surg. (Br.) 2011;93(5):689–694. doi: 10.1302/0301-620X.93B5.25422. [DOI] [PubMed] [Google Scholar]
- 16.Raffaele V., Marco L., Fabrizio D., Giulia M., Giovanni N., Vincenzo D.S., et al. Locking plate fixation in pediatric femur fracture: evaluation of the outcomes in our experience. Acta Biomed. 2019;90(Suppl. 1):110–115. doi: 10.23750/abm.v90i1-S.8109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cameron J.I., McCauley J.C., Kermanshahi A.Y., Bugbee W.D. Lateral opening-wedge distal femoral osteotomy: pain relief, functional improvement, and survivorship at 5 years. Clin. Orthop. Relat. Res. 2015;473(6):2009–2015. doi: 10.1007/s11999-014-4106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]