Abstract
Background
End-Stage Renal Disease (ESRD) is a significantly increasing condition warranting renal replacement therapy. Gaining vascular access for catheter placement for this procedure is of paramount importance. These can be done by temporary and permanent cuffed tunnelled catheters. The present study aims to analyze the outcome of permanent hemodialysis catheters and their efficacy in the case of patients suffering from end-stage renal disease.
Materials and methods
A cross-sectional study was conducted on 32 patients who underwent permanent tunnelled catheter intervention along with details of follow-up from January 1st, 2021 till December 31st, 2021.
Results
Among 32 patients, the mean age of the patient was 50.25 ± 18.10 years with 62.5% females. The site of insertion was right 27(84.37%) and left internal jugular vein in 4 (12.50%) and 1 patient (3.12%) in the left common femoral vein. Bleeding the peri-catheter site was observed in 4 (12.5%), infection was found among 2 patients (6.25%), thrombosis in the catheter in 7 (21.87%) patients. Indication for the procedure was due to failure of arteriovenous fistula in 21 (65.62%), lack of maturation of the AVF in 9 (28.12%) and patients awaiting transplantation in 2 (6.25%). The mean months of follow-up of the patients were 5.9 months (SD 4.4 months, range 1 month–12 months). Total 25 (78.1%) of the catheters were patent till the time of follow-up. Seven (21.9%) of the patients required manipulation once after which they also had functioning permanent catheters. The mean month on which manipulation was required was 4.1 months (SD 2.3months, range one month to seven months).
Conclusion
Permanent cuffed tunnelled catheter has good patency and can be an alternative to an arteriovenous fistula.
Keywords: Arteriovenous fistulas, End-stage renal disease, Hemodialysis, Vascular catheters
Highlights
-
•
Experience of cuffed tunnelled permanent hemodialysis catheter and details on manipulation.
-
•
Details on denovo catheter insertion and exchange with a previous internal jugular catheter.
-
•
Study on patency of cuffed tunnelled permanent hemodialysis catheter.
1. Introduction
Hemodialysis is one of the major modality renal replacement therapy in patients suffering from end-stage renal disease [1]. For hemodialysis vascular access has its prime importance. There are currently three modalities of vascular access for hemodialysis: temporary jugular catheter, permanent catheters and the creation of an arteriovenous fistula [2]. All the modalities have their own merits and demerits. To date, arteriovenous fistula is known as the best modality for hemodialysis access due to its long term use and low level of complications [2,3]. However it has its own limitations such as it requires more than 6 weeks for its maturation, failure of maturation, it may not be appropriate for the patients with heart failure, chronic respiratory problem patients, patients with many comorbidities, and patients with sclerotic vessels [4]. Hence, temporary and permanent cuffed tunnelled catheters should be used in these patients and those who need acute hemodialysis [5]. Compared to temporary catheters permanent tunnelled catheters have decreased the rates of malfunction, infection, and thrombosis significantly and should be preferred if the patient would need this access for more than 1 month [6]. Similarly, permanent tunnelled catheters also have their own complications such as central venous stenosis, thrombosis and infection with immediate complications such as arterial puncture, pneumothorax and hematoma.[[6], [7]] To prevent these complications it requires proper aseptic conditions with fluoroscopy and ultrasonography guidance.
As the permanent cuffed tunnelled catheters are being used by more than one-third of the population who are suffering from end-stage renal disease we aim to analyze the outcome of these catheters and their efficacy in the case of patients suffering from end-stage renal disease.
2. Methods
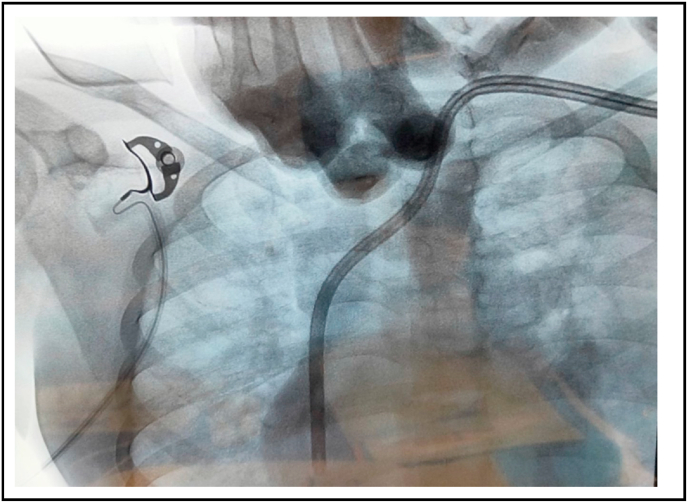
A cross-sectional study was conducted in the Cardiothoracic and Vascular Surgery Unit, Department of Surgery in Kathmandu University Dhulikhel Hospital with patients who underwent permanent tunnelled catheter intervention or manipulation of the existing permanent tunnelled catheter from January 1st, 2021 till December 31st, 2021. For permanent tunnelled catheter, because of availability, Newtech Permanent Hemodialysis Catheter (company details) with 15 F of size with 36 cm length for right and 40 cm for left side was used and similarly 40 cm catheter length was used for femoral catheter placement. The procedure was done on a daycare basis. In the case of an existing temporary internal jugular catheter, a guidewire of 4F size and 15 cm length was inserted via one of the ports as mentioned in the “over-the guidewire exchange” technique [8]. If the existing IJ catheter is high up, cannulation in a favourable site in the internal jugular vein is done. For the new case, the right internal jugular vein was punctured by a “Geometry based” cannulation technique using ultrasound guidance [9]. We used Acuson P300 (Siemens corporation) for ultrasonography with a linear probe of 6.5–10 MHz. All the procedures were done in the cath lab under fluoroscopy guidance by two experienced vascular surgeons with experience of 9 years and two years. 2% lignocaine was used for the local anaesthesia at the puncture site and along the line of the tunnel formation for local anaesthesia. Proper aseptic technique as per institute policy was followed. All the catheters were handled with care and diluted unfractionated heparin was flushed in the lumen of the catheter before the beginning of the procedure. Confirmation of the placement of the catheter at the right atrium was done with the help of fluoroscopy in the cath lab. At the end of the procedure also concentrated heparin of the required amount was flushed in each port of the catheter. Relevant pictures describing the catheter setup and process of insertion are shown in the picture collage (Fig. 1, Fig. 2).
Fig. 1.
Permanent catheter through the left internal jugular vein.
Fig. 2.
Overriding guidewire technique.
All the data of the procedure and patients' information were taken from the hospital software after proper consent from the patients and concerned authority from the hospital and clinical manifestations and complications were analyzed retrospectively. Monthly follow-up of the cases was done to note the patency. The study was conducted according to the guidelines of Strengthening the reporting of cohort studies in surgery (STROCSS) 2019 [10].
3. Results
Total of 271 cases were done in Cath Lab during the time frame. Among which 32 patients (11.8%) underwent tunnelled permanent hemodialysis catheter insertion. The average mean age was 50.25 ± 18.10 years and 37.5% of the patients were male and 62.5% were female patients. Of them, 20 cases (62.5%) had denovo catheter insertion while in 12 patients (37.5%) permanent catheter was exchanged in the previous IJ catheter. In the case of permanent catheter exchange over IJ catheter, 10 cases (83.3%) were done by the “over the guidewire exchange” method. In two cases (16.6%), as the IJ catheter was inserted high up, new cannulation was done in the internal jugular vein (Fig. 1) for insertion of a permanent catheter. The permanent catheter was placed in the right internal jugular vein in 26 patients (81.3%) while that was placed in the left internal jugular vein in five patients (15.6%) and one (3.1%) in the left femoral vein. In the case where a Permanent catheter was placed in the left femoral vein, it was initially tried in the right internal jugular vein followed by the left internal jugular vein but the guidewire could not be negotiated in the right atrium, hence the insertion site was changed.
The most common indication for the tunnel permanent catheter was the failure of AVF access and unavailability of veins for the creation of new fistula 21 (65.6%), second most common were waiting for the maturation of the AVF 9 (28.12%) and 2 (6.2%) were waiting for there transplantation. The common site of insertion of permanent tunnel catheter was the right internal jugular vein which was among 27(84.3%) patients and 4 (12.5%) patients had a placement in the left side and 1 (3.1%) had in the left common femoral vein.
The mean months of follow-up of the patients in which the catheter was inserted were 5.9 months (SD 4.4 months, range 1 month–12 months). Total 25 (78.1%) of the catheters were patent till the time of follow-up. Seven (21.9%) of the patients required manipulation once after which they also had functioning permanent catheters. The mean month on which manipulation was required was 4.1 months (SD 2.3months, range one month to seven months). Following manipulation, the mean months of follow up were 2.7 months (SD 1.6 months, ranging from one month to five months). All the patients in which manipulation was done had a patent catheter till the time of follow-up.
As an immediate complication bleeding from the peri-catheter site was present among 4 (12.5%) patients which was stopped post-correction of the underlying causes such as deranged coagulation factors, local compression and suturing in peri-catheter region. On long term complications, catheter thrombus was found among 7 (21.87%) patients, all of which required manipulation and intervention. In one patient, following successful cannulation of the right internal jugular vein, the guidewire could not be negotiated to the right atrium. Following that, the left internal jugular vein was cannulated but guidewire could not be negotiated in the right atrium. Thus, the Permanent catheter was inserted in the left femoral vein. Two cases (6.25%) had evidence of infection due to catheter management by IV antibiotics. As all the cases were done with the help of ultrasonography and under fluoroscopy guidance none of the cases had arterial puncture and displacement of the catheters. The summary of the findings of the study is mentioned in Table 1.
Table 1.
Summary of the results.
| Patients Demographics | |
|---|---|
| Average Age | 50.25 ± 18.10 years |
| Gender Distribution [n = 32 (%)] | |
| Male | 12 (37.5) |
| Female | 20 (62.5) |
| Catheter Insertion [n = 32 (%)] | |
| Denovo Insertion | 20 (62.5) |
| IJ exchange | 12 (37.5) |
| Among IJ exchange [n = 12 (%)] | |
| Over the guidewire exchange method | 10(83.33) |
| New cannulation below IJ | 2(16.66) |
| Site of insertion of catheters [n (%)] | |
| Right Internal Jugular | 27 (84.3) |
| Left Internal Jugular | 4 (12.5) |
| Femoral vein | 1 (3.1) |
| Immediate Complications [n (%)] | |
| Bleeding | 4 (12.5) |
| Infection | 2 (6.25) |
| Late Complications [n (%)] | |
| Thrombus in catheter | 7(21.87) |
| Patency [n = 32 (%)] | |
| Number of cases patent till the followup period. | 25 (78.1) |
| Patency in cases where manipulation was done [n = 7(%)] | |
| Number of cases post manipulation which was patent till the follow-up period. | 7 (100) |
4. Discussion
For patients suffering from end-stage renal disease hemodialysis has been proven as the best way of renal replacement therapy to date. Among many modalities, arteriovenous fistula has been determined as the best modality to perform the procedure. Among all the others, a permanent tunnelled catheter has been proven as one of the best alternatives for patients who cannot undergo hemodialysis with arteriovenous fistula. In our study, we have successfully inserted 31 (96.87%) catheters in a period of one year however we have failed to insert the catheter in one patient using a central vein.
The average age of the patients who underwent catheter placement was 50.25 ± 18.10 years. In a prevalence study done among the end-stage renal disease in Nepal, the average age was 49.6 ± 15.5 years [11], however in a similar study done in another centre in Nepal the average age group who had undergone tunnelled catheter was 67.57 ± 12.77 years [12]. Similarly females (62.5%) were common in our study compared to males (37.5%). It was also known that females are more prone to chronic kidney disease compared to male [13].
Regarding the site of the catheter placement, the common site was right side 27 (84.37%) and 4 (12.50%) patients had a placement in the left side and 1 (3.12%) had in the left common femoral vein, due to failure to of placement in right and left internal jugular vein. Subclavian was avoided as the guidelines also suggested avoiding the placement in the subclavian vein due to chances of stenosis and failure of AVF. Similarly, KDOQI guidelines also suggested the placement of catheters first in the right internal jugular vein followed by the left-sided one and then femoral vein, external vein, subclavian vein and translumbar vein and inferior vena cava. It is also suggested to avoid the placement in the subclavian vein as mentioned above [14]. In cases where an existing IJ catheter was present, we inserted guidewire via the IJ catheter and avoided separate cannulation. This technique has been documented as the “over-the-guidewire exchange method” and considered as a safe technique in terms of patency, chances of infection [8]. However, if IJ is placed high up, we prefer re-puncture of the internal jugular vein in the lower favourable site.
In a study done by Sepas et al., in 2019 in Iran, it has suggested the patency of the permanent tunnelled catheters were 5.65 ± 4.57 months [15]. Similarly in another study done in 1994 among 108 patients by Tesio et al. suggested one-year patency ranged from 91% to 93% [16]. As in our case among 32 patients patency ranged from 78.12% to 100% after manipulation among 7 patients. Varying in range of the patency may be due to failure of proper management of catheter, failure to create a proper aseptic environment and sometimes failure of treatment of infection.
On immediate complication, bleeding was found to be 12.50% among 32 patients on a study done among 59 patients by Abu Shark et al., in 2020 suggested 5.1% of patients had bleeding from the peri-catheter site [17], possible reasons might be due to underlying coagulation disorder in our cases. and infection being 6.25%, similarly, a study done by Rackoff et al., it has also suggested the rate of infection was 6.28% which was similar to our study [18]. On long term complications, there were 7 (21.87%) patients who had thrombus in the catheter. For this problem manipulation of the catheter with stiff guidewire insertion (Fig. 2) and thrombus suction with 50 ml syringe and heparin flush was done. In a study done in 2001 by Jean et al. on long term complications of the permanent catheter, it has also concluded that thrombosis of the central vein was found in 20.9% [19] which is also similar to our study. In one case there was a failure to insert in both right and left-sided internal jugular vein for which a permanent catheter was placed in the left femoral vein.
5. Limitation of the study
Details on the long term follow-up including duration of patency of the catheters was not studied.
6. Conclusion
Permanent cuffed tunnelled catheter is a viable option for dialysis access in selected patients due to longer patency and safety. However, regular monitoring of patency needs to be noted and when required manipulation can be done with good outcomes.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Sources of funding
No funding was secured for this study.
Consent for publication
Informed consent was obtained from each participant.
Availability of data and materials
All relevant data and materials are provided within the manuscript.
Funding
None.
Provenance and peer review
Not commissioned; externally peer-reviewed.
Consent
Consent was taken from all the participants and none of the identifying characteristics were included in the original article.
Author contribution
Satish Vaidya: Surgical procedure, patient care, manuscript writing.
Robin Man Karmacharya: Surgical procedure, Patient care, manuscript writing.
Swechha Bhatt: manuscript writing and editing.
Niroj Bhandari: Manuscript writing.
Sarita Duwal: Surgical procedure, Patient care.
Yashoda Devi Karki: Surgical procedure, Patient care.
Rashmi Maharjan: Surgical procedure, Patient care.
Registration of research studies
1. Name of the registry: researchregistry7556.
2. Unique identifying number or registration ID: 7556.
3. Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#home/
Guarantor
Dr. Robin Man Karmacharya.
Associate Professor and unit chief.
Cardio Thoracic and Vascular Surgery Unit.
Department of Surgery.
Dhulikhel Hospital.
Kathmandu University Hospital.
Declaration of competing interest
None.
Contributor Information
Satish Vaidya, Email: satish.vaidya.nep@gmail.com.
Robin Man Karmacharya, Email: reachrobin773@gmail.com.
Swechha Bhatt, Email: swechhabhatt48@gmail.com.
Niroj Bhandari, Email: bhandariniroj15@gmail.com.
Sarita Duwal, Email: duwalsarta67@gmail.com.
Yashoda Devi Karki, Email: yasodhakarki370@gmail.com.
Rashmi Maharjan, Email: rashmimaharjan@kusms.edu.np.
References
- 1.End-stage renal (kidney) disease. https://my.clevelandclinic.org/health/diseases/16243-end-stage-renal-kidney-disease
- 2.Santoro D., Benedetto F., Mondello P., et al. Vascular access for hemodialysis:current perspectives. Int. J. Nephrol. Renovascular Dis. 2014;7:281–294. doi: 10.2147/IJNRD.S46643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moureau N.L. Springer; 2019. Vessel Health and Preservation:The Right Approach for Vascular Access. [Google Scholar]
- 4.Lomonte C., Basile C., Mitra S., et al. Should a fistula first policy be revisited in elderly haemodialysis patients? Nephrol. Dial. Transplant. 2019;34:1636–1643. doi: 10.1093/ndt/gfy319. [DOI] [PubMed] [Google Scholar]
- 5.Rayner H.C., Pisoni R.L., Gillespie B.W., et al. Creation, cannulation and survival of arteriovenous fistulae:data from the dialysis outcomes and practice patterns study. Kidney Int. 2003;63:323–330. doi: 10.1046/j.1523-1755.2003.00724.x. [DOI] [PubMed] [Google Scholar]
- 6.Weijmer M.C., Vervloet M.G., ter Wee P.M. Compared to tunnelled cuffed haemodialysis catheters, temporary untunnelled catheters are associated with more complications already within 2 weeks of use. Nephrol. Dial. Transplant. 2004;19:670–677. doi: 10.1093/ndt/gfg581. [DOI] [PubMed] [Google Scholar]
- 7.Rayner H.C., Pisoni R.L. The increasing use of hemodialysis catheters:evidence from the DOPPS on its significance and ways to reverse it. Semin. Dial. 2010;23:6–10. doi: 10.1111/j.1525-139X.2009.00675.x. [DOI] [PubMed] [Google Scholar]
- 8.Park H.S., Choi J., Kim H.W., et al. Exchange over the guidewire from non-tunneled to tunneled hemodialysis catheters can be performed without patency loss. J. Vasc. Access. 2018;19:252–257. doi: 10.1177/1129729817747541. [DOI] [PubMed] [Google Scholar]
- 9.Karmacharya R.M. Geometry-based cannulation technique” for cannulation of great saphenous vein during radiofrequency ablation of varicose veins at a university hospital of Nepal. Indian J. Vasc. Endovasc. Surg. 2020;7:18. [Google Scholar]
- 10.Mathew G., Agha R., STROCSS Group STROCSS 2021:Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Ann. Med. Surg. (Lond) 2021;72:103026. doi: 10.1016/j.amsu.2021.103026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghimire M., Vaidya S., Upadhyay H.P. Prevalence of newly diagnosed end-stage renal disease patients in a tertiary hospital of Central Nepal, chitwan:A descriptive cross-sectional study. JNMA J. Nepal Med. Assoc. 2021;59:61–64. doi: 10.31729/jnma.4971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrestha K.R., Gurung D., Shrestha U.K. Outcome of cuffed tunneled dialysis catheters for hemodialysis patients at a tertiary care hospital:A descriptive cross-sectional study. JNMA J. Nepal Med. Assoc. 2020;58:390–395. doi: 10.31729/jnma.4795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kidney failure risk factor:gender (sex) 2020. https://www.kidney.org/content/kidney-failure-risk-factor-gender-sex
- 14.National Kidney Foundation KDOQI clinical practice guideline for hemodialysis adequacy:2015 update. Am. J. Kidney Dis. 2015;66:884–930. doi: 10.1053/j.ajkd.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Sepas H.N., Negahi A., Mousavie S.H., et al. Patency and outcomes of tunneled hemodialysis catheter via femoral versus jugular vein access. "J. Adv. Pharm. Technol. Research"" (JAPTR)". 2019;10:81–84. doi: 10.4103/japtr.JAPTR_383_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tesio F., De Baz H., Panarello G., et al. Double catheterization of the internal jugular vein for hemodialysis:indications, techniques, and clinical results. Artif. Organs. 1994;18:301–304. doi: 10.1111/j.1525-1594.1994.tb02200.x. [DOI] [PubMed] [Google Scholar]
- 17.Abuward A.-S.I., Puello M.S., Janeiro M.L., et al. Tunneled femoral catheters and tunneled jugular catheters, our experience, efficacy and complications. Archives of Clinical Nephrology. 2020;6:1–4. [Google Scholar]
- 18.Rackoff W.R., Weiman M., Jakobowski D., et al. A randomized, controlled trial of the efficacy of a heparin and vancomycin solution in preventing central venous catheter infections in children. J. Pediatr. 1995;127:147–151. doi: 10.1016/s0022-3476(95)70276-8. [DOI] [PubMed] [Google Scholar]
- 19.Jean G., Charra B., Chazot C., et al. Long-term outcome of permanent hemodialysis catheters:a controlled study. Blood Purif. 2001;19:401–407. doi: 10.1159/000046971. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data and materials are provided within the manuscript.