Abstract
Introduction.
Although the majority of patients with myelomeningocele have hydrocephalus, reported rates of treatment of hydrocephalus vary widely. The purpose of this study was to determine the rate of surgical treatment for hydrocephalus in patients with myelomeningocele in the National Spina Bifida Patient Registry (NSBPR). In addition, we explored the variation in shunting rates across NSBPR institutions, examined the relationship between hydrocephalus and the functional lesion level of the myelomeningocele, and evaluated for temporal trends in rates of treated hydrocephalus.
Methods.
We queried the NSBPR to identify all patients with myelomeningoceles. Individuals were identified as having treated hydrocephalus if they had undergone at least one hydrocephalus-related operation. For each participating NSBPR institution, we calculated the proportion of patients enrolled at that site with treated hydrocephalus. Logistic regression was performed to analyze the relationship between hydrocephalus and the functional lesion level of the myelomeningocele as well as to compare the rate of treated hydrocephalus in children born before 2005 to those born in 2005 or later.
Results.
A total of 4448 patients with myelomeningocele were identified from 26 institutions, of whom 3558 patients (79.99%) had undergone at least one hydrocephalus-related operation.
The rate of treated hydrocephalus ranged from 72% to 96% among institutions enrolling more than 10 patients. This difference in treatment rates between centers was statistically significant (p<0.001). Insufficient data were available in the NSBPR to analyze reasons for the different rate of hydrocephalus treatment between sites.
Multivariate logistic regression demonstrated that more rostral functional lesion levels were associated with higher rates of treated hydrocephalus (p < 0.001) but demonstrated no significant difference in hydrocephalus treatment rates between children born before versus after 2005.
Conclusion.
The rate of hydrocephalus treatment in patients with myelomeningocele in the NSBPR is 79.99%, which is consistent with previously published literature. Our data demonstrate a clear association between functional lesion level of the myelomeningocele and the need for hydrocephalus treatment.
Keywords: myelomeningocele, spina bifida, hydrocephalus, VP shunt
Introduction
The majority of patients with a diagnosis of myelomeningocele have concomitant hydrocephalus. Rates of cerebrospinal fluid (CSF) diversion for treatment of hydrocephalus vary widely, ranging from 40% to 91% in the published literature (52% to 91% for post-natal myelomeningocele closures).1–4,6,9,12 In the randomized trial Management of Myelomeningocele Study (MOMS), rates of shunting were 40% in the prenatal-surgery group and 82% in the postnatal-surgery group at 12 months of age, but this trial included only mothers who met stringent selection criteria, and fewer than 20% of screened mothers were enrolled.1
Although the association between myelomeningoceles and hydrocephalus is well established, there are far fewer data on the relationship between the functional lesion level of the myelomeningocele and the need for hydrocephalus treatment. One large retrospective review of 297 individuals found that rates of shunt placement varied with both the functional and anatomic level of the myelomeningocele, with higher rates of shunting required in patients with more rostral lesion levels.9 However, another retrospective analysis of 72 patients found no difference in shunting rates by anatomic level.7
In 2008 the Centers for Disease Control and Prevention established a National Spina Bifida Patient Registry (NSBPR) to facilitate research and improve clinical care for children and adults with spina bifida.11,13 The NSBPR collects data longitudinally, using both family/patient report and medical record review at the time of routine clinic visits. It includes multiple checks on data integrity and quality (see Appendix for details of the NSBPR and data collection techniques). The majority participants in the NSBPR have myelomeningocele, with other forms of spinal dysraphism making up less than 20% of the total participants.11
The goal of this study was to use data collected in the NSBPR to better understand the treatment of hydrocephalus among individuals with myelomeningocele. In addition, we sought to examine the variation in rates of treated hydrocephalus between centers participating in the NSBPR. We also explored the relationship between rates of CSF shunting and the functional lesion level of the myelomeningocele. Lastly, we evaluated for any temporal trends in the rates of hydrocephalus treatment for patients with myelomeningocele.
Methods
Much of the methods in this study have been reported in another paper by our grou (citation of Chiari II paper). Data collection for the NSBPR is performed at each site by a designated coordinator. Variables to be collected are noted at the time of the clinic visit on standardized case report forms (either an Initial Encounter Form or an Annual Collection Form) following the NSBPR Manual of Procedures. Data are obtained from query of the patient/family, review of the medical record, or both. Data are then uploaded to a NSBRP electronic record. Here they are automatically subjected to data quality checks. Additional checks are performed by NSBPR administrators and requests for clarification sent to each site. Full details of the NSBPR data collection procedure can be found in the Appendix.
Per the established protocol for studying the aggregate data collected in the NSBPR, the data analysis proposal outlining this study was reviewed by the CDC Committee for Science and Publication. We then queried the NSBPR to identify all patients with myelomeningocele enrolled in the registry between March 2009 and October 2015. We collected demographic and clinical variables, and records of all included operative procedures. Operative procedures may have been performed outside of the 2009–2015-time range, since those performed prior to NSBRP enrollment would be recorded at the time of enrollment. The functional lesion level was determined by direct bilateral lower extremity neurological examination. If the lesion differed by side, then the more rostral level was used to represent functional lesion level. We defined individuals as having treated hydrocephalus if they had a history of one or more qualifying hydrocephalus-related operations (Table 1).
Table 1.
| List of hydrocephalus-related procedures |
|---|
| Ventriculoperitoneal shunt |
| Creation of ventriculo-atrial shunt |
| Ventriculopleural shunt with valve |
| Shunt of cerebral ventricle to gallbladder |
| Creation of lumboperitoneal shunt |
| Revision of cerebral ventricular shunt |
| Replacement of ventricular shunt |
| Removal of ventriculoperitoneal shunt |
| Removal of cerebral ventricular shunt |
| Endoscopic exteriorization of third ventricle |
| Endoscopic third ventriculostomy |
We calculated the rate of treated hydrocephalus among all patients with myelomeningocele. We assume that hydrocephalus is treated within the first few months of age, and therefore, that including all patients in the analysis is valid. However, to control for the possibility that very young children may not yet have received treatment, we also determined the rate of hydrocephalus treatment excluding all children under age 12 months.
Univariate logistic regression was used to examine the relationship between treatment of hydrocephalus and the functional lesion level of the myelomeningocele. For each participating NSBPR institution, we calculated the proportion of patients enrolled at that site with treated hydrocephalus. Chi square analysis was performed to determine if the difference in hydrocephalus treatment rate between institutions was statistically significant.
It is the perception of the authors that there has been a trend towards a higher threshold for treatment of hydrocephalus in patients with myelomeningocele in recent years. To explore this, univariate logistic regression was used to compare the rates of treated hydrocephalus between children born before 2005 and children born in 2005 or later. The year 2005 was selected by consensus opinion of the authors. Because 2005 was chosen by consensus and without empiric support, sensitivity analysis was performed by repeating analysis using 2002 and 2008 as the cutoff year. Additional sensitivity analysis was performed comparing rates of hydrocephalus treatment for children born in 2003 or earlier to those born in 2006 or later, thus separating the comparison groups by excluding all children born in 2004 or 2005.
Finally, post hoc analysis was performed using multivariate logistic regression to control for the effect of lesion level on observations made about hydrocephalus treatment rates by study site and by year of birth.
Results
We identified 4448 individuals with myelomeningocele from 26 institutions in the NSBPR (Table 2). 2308 (51.89%) of whom were female and 2140 (48.11%) of whom were male. The mean age as of the time of the most recent clinic visit was 13.9 years (y) (median 12.3y, standard deviation (SD) 10.3y). Figure 1 shows the age distribution of included individuals (range 0 to 82 years). Children under 1 year of age made up 12.5% of the total sample (558).
Table 2.
Patient Demographics.
| Age, years | |
|---|---|
| Mean (SD) | 13.9 (10.3) |
| Median | 12.3 |
| Gender (%) | |
| Female | 2308 (51.9) |
| Male | 2140 (48.1) |
| Functional Lesion Level (%) | |
| Thoracic (flaccid lower extremities) | 856 (19.2) |
| High-lumbar (hip flexion present) | 508 (11.4) |
| Mid-lumbar (knee extension present) | 1325 (29.8) |
| Low-lumbar (foot dorsiflexion present) | 877 (19.7) |
| Sacral (foot plantar flexion present) | 882 (19.8) |
Figure 1.
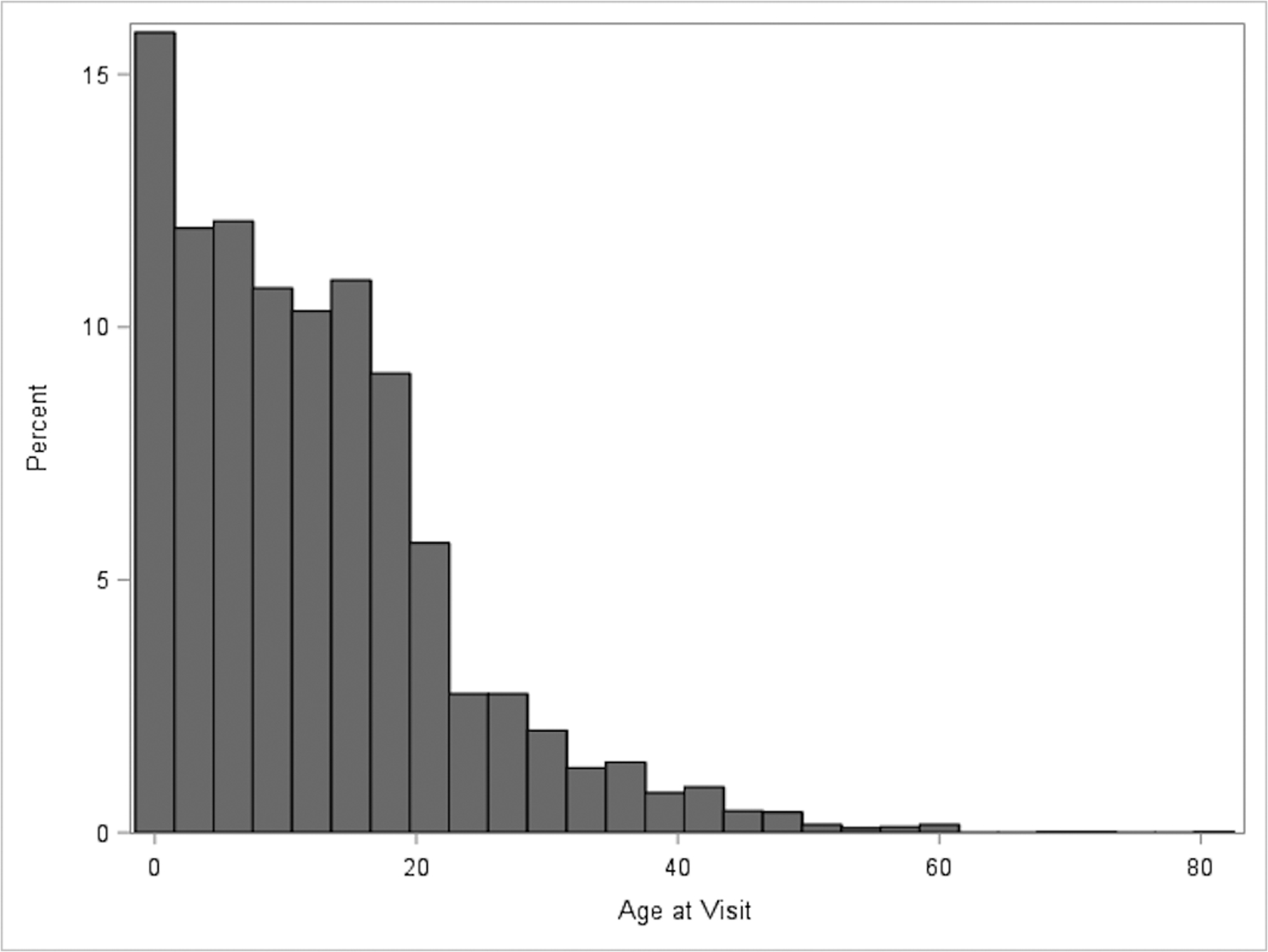
Age of included patients
We used functional lesion level (as defined by the NSBPR) as an assessment of neurological function. There were 856 patients (19.2%) with thoracic functional level (flaccid lower extremities); 508 patients (11.4%) with high-lumbar level (hip flexion present), 1325 patients (29.8%) with mid-lumbar level (knee extension present), 877 patients (19.7%) with low-lumbar level (foot dorsiflexion present), and 882 patients (19.8%) with sacral level (foot plantar flexion present).
Of all subjects, a total of 3558 patients (79.99%) had undergone at least one surgical procedure for treatment of hydrocephalus. There was no difference in the rates of treated hydrocephalus between male and female patients (79.11% vs. 80.81% respectively, p=0.158). When considering only participants over age 12 months, the overall rate of hydrocephalus treatment was 80.90%.
Univariate logistic regression demonstrated a significant association between the functional lesion level of myelomeningocele and treated hydrocephalus (Table 3). 789 of 856 patients (92.2%) of patients with thoracic level, 454 of 508 patients (89.4%) with high-lumbar level, 1104 of 1325 patients (83.3%) with mid-lumbar level, 676 of 877 patients (77.1%) with low-lumbar level, and 535 of 882 patients (60.7%) patients with sacral level myelomeningocele required treatment for hydrocephalus. More rostral functional lesion levels were associated with higher rates of hydrocephalus treatment (p < 0.0001). The odds ratio for hydrocephalus treatment (with sacral functional lesion level as the reference), was 7.64 (5.75–10.14, 95% confidence interval (CI)) in thoracic level, 5.45 (3.99–7.46, 95% CI) in high-lumbar level, 3.24 (2.66–3.95, 95% CI) in mid-lumbar level, and 2.18 (1.77–2.68, 95% CI) in low-lumbar level myelomeningocele patients. Thus, there is a statistically significant increase in the odds for hydrocephalus treatment when any more rostral functional lesion level is compared to sacral lesion level. This relationship is maintained with negligible change in odds ratios or confidence intervals when analysis is performed using only children age 12 months or older.
Table 3.
Relationship between functional lesion level of myelomeningocele and treated hydrocephalus
| Functional Lesion Level | Treated Hydrocephalus | Total | Percentage (%) | Odds Ratio (vs. Sacral Level) |
95% Confidence Interval |
|---|---|---|---|---|---|
| Thoracic | 789 | 856 | 92.2 | 7.64 | 5.75–10.14 |
| High-lumbar | 454 | 508 | 89.4 | 5.45 | 3.99–7.46 |
| Mid-lumbar | 1104 | 1325 | 83.3 | 3.24 | 2.66–3.95 |
| Low-lumbar | 676 | 877 | 77.1 | 2.18 | 1.77–2.68 |
| Sacral | 535 | 882 | 60.7 | Ref | Ref |
| Total | 3558 | 4448 | 80.0 |
There were 26 sites participating in the NSBPR, with a mean enrollment of 159 individuals (range 1–363, SD 117, Figure 2). Among institutions enrolling more than 10 patients (23 of 26 institutions), the rate of treated hydrocephalus ranged from 72% to 96%. This difference in hydrocephalus treatment rate is statistically significant by Chi square analysis (p<0.001). There is also a statistically significant difference in proportion of patients with each functional lesion level at each site (p<0.001 by Chi Square). Nevertheless, when controlling for functional lesion level, the difference between sites remains statistically significant.
Figure 2.
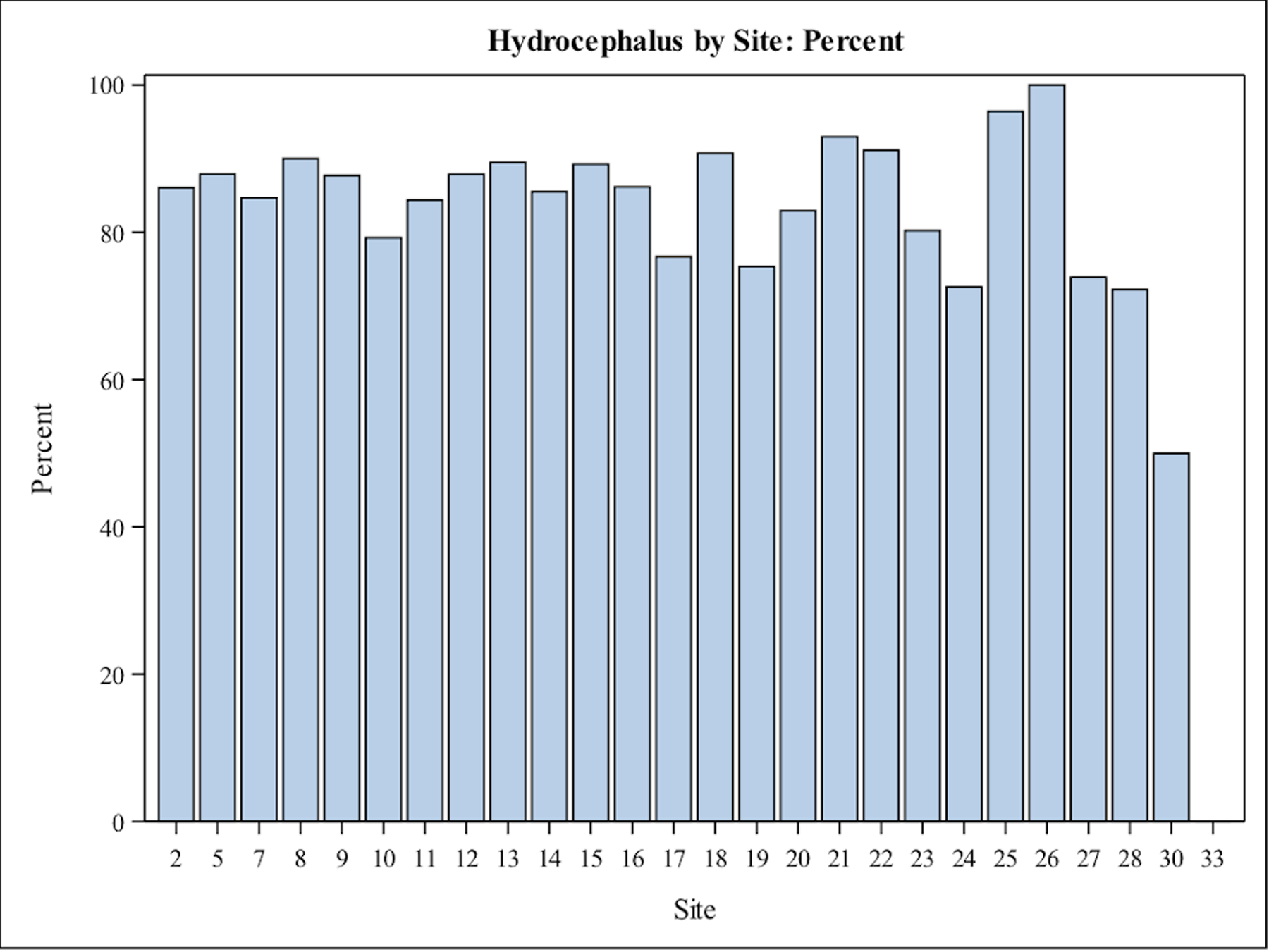
Distribution of treated hydrocephalus by site
Univariate logistic regression analysis also demonstrated a significant decrease in the rates of treated hydrocephalus in children born in 2005 or later. Of the 2796 individuals born before 2005, 2296 (82.1%) had treated hydrocephalus. Of the 1652 individuals born in 2005 or later, 1262 (76.4%) had hydrocephalus treatment (OR 1.42, 1.22–1.65, 95% CI, p<0.001). When this analysis is repeated with 2002 and 2008 as the threshold years, there continues to be a statistically significantly higher rate of hydrocephalus treatment in the earlier period. However, when combined with gender and functional lesion level in a multivariate logistic regression model, only functional lesion level remains significant. Gender (p=0.25) and year of birth (p=0.086) do not show statistically significant association with hydrocephalus treatment (Table 4). When this analysis is repeated comparing children born in 2003 or earlier to those born in 2006 or later, we see a significant difference on univariate analysis (OR 1.30, 95% CI 1.10–1.54, p=0.0018), but no difference when controlling for lesion level (p=0.49). As expected given these findings, there is a statistically significant higher proportion of more rostral functional lesion level among children born in earlier epoch compared to later epochs (p<0.001 by Chi square).
Table 4.
Relationship between functional lesion level, gender, and year of birth with treated hydrocephalus (multivariate logistic regression)
| Variable | Odds Ratio | 95% Confidence Interval | p-value |
|---|---|---|---|
| Functional Lesion Level | |||
| Thoracic | 7.33 | 5.51–9.77 | <0.0001 |
| High-lumbar | 5.41 | 3.96–7.40 | <0.0001 |
| Mid-lumbar | 3.20 | 2.63–3.90 | <0.0001 |
| Low-lumbar | 2.19 | 1.78–2.70 | <0.0001 |
| Sacral | Ref | Ref | |
| Gender | |||
| Female | 1.10 | 0.94–1.28 | 0.25 |
| Male | Ref | Ref | |
| Year of Birth | |||
| Before 2005 | 1.15 | 0.98–1.34 | 0.086 |
| 2005 or later | Ref | Ref |
Discussion
The overall rate of treated hydrocephalus in patients with myelomeningocele enrolled in the NSBPR is 80%, which is consistent with reported rates in the published literature. As expected, there is some variability among the institutes participating in NSBPR. However, among sites enrolling more than 10 patients, the rates of treated hydrocephalus vary from 72 to 96%, which appears to be slightly less than in the published literature.1–7
Unfortunately, the available data in the NSBPR do not contain enough detail to explain this variation between sites. The version of registry questionnaire in use at the time of this analysis did not record the indication for treatment of hydrocephalus, nor did it collect data on clinical or radiographic patient parameters related to hydrocephalus such as fontanelle characteristics, splayed sutures, biventricular diameter, or bradycardic/apneic episodes.7,14 In addition, very limited data on head circumference were collected (at the time of enrollment and annually if the child was less than 3 years of age), which is insufficient for analysis.
It should also be noted that the registry questionnaire in use at that time did not record any data regarding timing of myelomeningocele closure. Although we estimate that fewer than 1% of patients enrolled in the NSBPR have undergone prenatal closure, the available data do not allow us to compare rates of treated hydrocephalus between patients who have undergone prenatal surgery to those who have undergone postnatal surgery.
The data did demonstrate a clear correlation between functional lesion level of the myelomeningocele and the need for hydrocephalus treatment. By combining all of patients with a functional lumbar level (high, mid, and low), we found that overall rates of treated hydrocephalus were 92.2% for thoracic level, 82.4% for lumbar level, and 60.7% for sacral level myelomeningoceles. This can be compared to the single-institution data from Children’s Hospital of Philadelphia, which reported shunting rates of 97%, 87%, and 37%, respectively, by functional level.9 The rates of treated hydrocephalus in the present study were similar but slightly lower in the thoracic and lumbar functional levels, but much higher in the sacral functional levels when compared to the published single-center data. The reason for this difference is not clear. While the correlation between functional lesion level and hydrocephalus is not unexpected, it has not previously been explored with this large a sample size.
The data also suggest a decrease in the rate of treated hydrocephalus in individuals born in 2005 or later compared to those born before 2005. This is consistent with the authors’ perception of a trend towards a higher threshold for treatment of hydrocephalus. In recent years, there has been a growing discussion about reducing treatment rates for hydrocephalus in patients with myelomeningoceles, arising in part due to concerns about the long-term sequelae of shunted hydrocephalus and the morbidity of multiple shunt operations in conjunction with the lower rates of CSF shunting reported in patients undergoing prenatal closure of myelomeningocele.1,3,7,8,10 However, in multivariate analysis, when controlling for lesion level, the effect of year of birth is lost. Therefore, we can report no such declining trend in hydrocephalus treatment rate.
Since it was established in 2008, the NSBPR questionnaire has been updated and expanded. Data are currently being collected in the third version of the registry questionnaire, which includes much more data on hydrocephalus, including clinical and radiographic parameters of the patient as well as the indications for some surgical procedures, including treatment of hydrocephalus. More analysis is indicated in the future to better understand the variation in the rates of treated hydrocephalus among institutions as well as the ultimate effect of neurocognitive parameters.
Limitations
In addition to the limitations on data included in the NSBPR noted above, there are important additional limitations. Individuals may be lost to follow up or move to a different NSBPR site. If an individual moves to a different participating site, their records are forwarded and they would be counted as a patient in the new site (site of most recent clinic visit). This may lead to inaccuracies in the analysis of hydrocephalus treatment rate by site. We estimate that fewer than 1% of patients move between centers each year. Therefore, this should be a minor error.
There is no validated assessment of the functional lesion level. While the NSBPR provides guidelines and descriptions of functional level, personnel at each site make a judgement about the level. Similarly, the decision to treat a patient’s hydrocephalus is made by local surgeons and may vary between sites. While guidelines exist for making treatment decisions, for example those from the MOMS trial, there may be variation in how these standards are applied.1,5
Conclusion
The rate of hydrocephalus treatment in patients with myelomeningocele in the NSBPR is 80%, which is consistent with previously published literature. Our data demonstrate a clear association between functional lesion level of the myelomeningocele and the need for hydrocephalus treatment. While we hypothesized that hydrocephalus treatment had decreased over time, we see no evidence that this is the case.
Supplementary Material
Acknowledgements:
The development of the National Spina Bifida Patient Registry has been successful due to the contributions of all the members of the NSBPR Coordinating Committee. Members of this committee during the collection of the data reported here were William Walker, Seattle Children’s Hospital; Kathryn Smith, Children’s Hospital, Los Angeles; Kurt Freeman, Oregon Health & Science University, Portland; Pamela Wilson, Children’s Hospital Colorado, Aurora; Kathleen Sawin, Children’s Hospital of Wisconsin and Froedtert Hospital, Milwaukee (adult clinic); Jeffrey Thomson, Connecticut Children’s Medical Center, and Shriners Hospital for Children, Springfield; Heidi Castillo, Texas Children’s Hospital/Baylor College of Medicine, Houston; David Joseph, Children’s Hospital of Alabama and University of Alabama at Birmingham; Jacob Neufeld, St. Luke’s Boise Medical Center, Boise; Robin Bowman, Lurie Children’s Hospital of Chicago, Chicago; Karen Ratliff-Schaub, Nationwide Children’s Hospital, Columbus; Jim Chinarian, Children’s Hospital of Michigan, Detroit; John Wiener, Duke University Medical Center, Durham; Mark Dias, Hershey Medical Center, Hershey; Tim Brei, Riley Hospital for Children, Indianapolis; Brad Dicianno, Children’s Hospital of Pittsburgh, and University of Pittsburgh Medical Center, (adult clinic) Pittsburgh; Paula Peterson, Primary Children’s Medical Center, Salt Lake City; Elaine Pico, UCSF, San Francisco, and Children’s Hospital and Research Center, Oakland. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding:
The National Spina Bifida Patient Registry is funded by the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, Georgia. Preparation of this manuscript was supported by grants #1UO1DDD000742.01; 1UO1DDD000766.01; 1UO1DDD000772.01.
Footnotes
Data included in this manuscript have been presented at the AANS/CNS Joint Section on Pediatric Neurosurgery Meeting, Orlando, Florida, December 2016 and at the Third World Congress on Spina Bifida Research and Care, San Diego, California, March 2017. No part of this manuscript has been previously published.
References
- 1.Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, et al. : A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364:993–1004, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bowman RM, Boshnjaku V, McLone DG: The changing incidence of myelomeningocele and its impact on pediatric neurosurgery: a review from the Children’s Memorial Hospital. Childs Nerv Syst 25:801–806, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Chakraborty A, Crimmins D, Hayward R, Thompson D: Toward reducing shunt placement rates in patients with myelomeningocele. J Neurosurg Pediatr 1:361–365, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Johnson MP, Sutton LN, Rintoul N, Crombleholme TM, Flake AW, Howell LJ, et al. : Fetal myelomeningocele repair: short-term clinical outcomes. Am J Obstet Gynecol 189:482–487, 2003 [DOI] [PubMed] [Google Scholar]
- 5.Laskay NMB, Arynchyna AA, McClugage SG 3rd, Hopson B, Shannon C, Ditty B, et al. : A comparison of the MOMS trial results to a contemporaneous, single-institution, postnatal closure cohort. Childs Nerv Syst 33:639–646, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patet JD, Lapras C, Guilburd JN, Lapras C: [Spina bifida aperta--myelomeningocele. Hydrocephalus]. Neurochirurgie 34 Suppl 1:47–52, 1988 [PubMed] [Google Scholar]
- 7.Phillips BC, Gelsomino M, Pownall AL, Ocal E, Spencer HJ, O’Brien MS, et al. : Predictors of the need for cerebrospinal fluid diversion in patients with myelomeningocele. J Neurosurg Pediatr 14:167–172, 2014 [DOI] [PubMed] [Google Scholar]
- 8.Piatt JH Jr.: Treatment of myelomeningocele: a review of outcomes and continuing neurosurgical considerations among adults. J Neurosurg Pediatr 6:515–525, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Rintoul NE, Sutton LN, Hubbard AM, Cohen B, Melchionni J, Pasquariello PS, et al. : A new look at myelomeningoceles: functional level, vertebral level, shunting, and the implications for fetal intervention. Pediatrics 109:409–413, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Sankhla S, Khan GM: Reducing CSF shunt placement in patients with spinal myelomeningocele. J Pediatr Neurosci 4:2–9, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawin KJ, Liu T, Ward E, Thibadeau J, Schechter MS, Soe MM, et al. : The National Spina Bifida Patient Registry: profile of a large cohort of participants from the first 10 clinics. J Pediatr 166:444–450 e441, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stein SC, Schut L: Hydrocephalus in myelomeningocele. Childs Brain 5:413–419, 1979 [DOI] [PubMed] [Google Scholar]
- 13.Thibadeau JK, Ward EA, Soe MM, Liu T, Swanson M, Sawin KJ, et al. : Testing the feasibility of a National Spina Bifida Patient Registry. Birth Defects Res A Clin Mol Teratol 97:36–41, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tulipan N, Wellons JC 3rd, Thom EA, Gupta N, Sutton LN, Burrows PK, et al. : Prenatal surgery for myelomeningocele and the need for cerebrospinal fluid shunt placement. J Neurosurg Pediatr 16:613–620, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


